Abstract
Background
Little research has focused on the performance of mechanical thrombectomy (MT) in carotid terminus occlusions (CTOs). Therefore, the best first-line thrombectomy strategy for CTOs remains unclear.
Purpose
To compare the safety and efficacy outcomes of three first-line thrombectomy techniques in CTOs.
Methods
A systematic literature search was conducted in Ovid MEDLINE, Ovid Embase, Scopus, Web of Science, and Cochrane Central Register of Clinical Trials databases. Studies providing safety and efficacy outcomes for endovascular treatment of CTOs were included. Data regarding successful recanalization, functional independence, symptomatic intracranial hemorrhage (sICH), and first pass efficacy (FPE) were extracted from the included studies. A random-effects model was used to calculate prevalence rates and their corresponding 95% confidence intervals (CI), and subgroup analyses were performed to assess the impact of the initial MT technique on safety and efficacy outcomes.
Results
Six studies with 524 patients were included. The overall successful recanalization rate was 85.84% (95% CI = 77.96–94.52), and subgroup analysis did not show a significant difference among the three first-line MT techniques. Overall rates of functional independence and FPE were 39.73% (95% CI = 32.95–47.89) and 32.09% (95% CI = 22.93–44.92), respectively. The combined stent retriever (SR) and aspiration (ASP) technique achieved significantly higher first-pass efficacy rates compared to SR or ASP alone. The overall sICH rate was 9.89% (95% CI = 4.88–20.07), and subgroup analysis did not demonstrate a significant difference across groups. The sICH rates of SR, ASP, and SR + ASP were 8.49% (95% CI = 1.76–40.93), 6.8% (95% CI = 4.59–10.09), and 7.12% (95% CI = 0.27–100), respectively.
Conclusions
Our results support that MT is highly effective for CTOs with functional independence rates of 39%. Additionally, in our meta-analysis, the SR + ASP technique was associated significantly greater rates of FPE compared to SR or ASP alone, without an increase in sICH rates. Prospective, large-scale studies are necessary to determine the optimal first-line MT technique in the endovascular treatment of CTOs.
Abbrevations
- CTO
Carotid terminus occlusion
- MT
Mechanical thrombectomy
- CI
Confidence interval
- FPE
First-pass efficacy
- SR
Stent retriever thrombectomy
- ASP
Aspiration thrombectomy
- SR + ASP
Combined treatment
- sICH
Symptomatic intracranial hemorrhage
- PLVO
Proximal large vessel occlusions
- ICA
Internal carotid artery
- TICI
Thrombolysis in cerebral infarction
- mRS
Modified Rankin Scale
- ID
Inner diameter
1. Introduction
Several randomized clinical trials (RCTs) have established the utility of mechanical thrombectomy (MT) in proximal large vessel occlusions (PLVOs).1, 2, 3, 4, 5 However, the performance of MT in different internal carotid artery (ICA) occlusion subtypes has not been well studied.
ICA occlusions affecting between supraclinoid segment of the ICA and ICA bifurcation are categorized as carotid terminus occlusions (CTOs).6 CTOs account for 20–30% of ICA occlusions and are associated with severe neurologic deficits.7,8 CTOs can result in higher infarct volume than proximal ICA occlusions due to greater impairment in contralateral blood supply from the circle of Willis.7, 8, 9, 10 Additionally, given the large clot burden, successful recanalization rates may be low,11 and distal embolization rates have been documented to be as high as 40% for CTOs.12 Therefore, determining the most effective first-line MT strategy for CTOs is of paramount importance.
Four RCTs have compared the performance of first-line thrombectomy techniques for PLVOs.13, 14, 15, 16 However, CTOs were significantly underrepresented (<20% of all occlusions), and specific CTO data were not available in these trials.13, 14, 15, 16 To date, little research has compared the performance of first-line MT strategies in CTOs. Thus, the best initial thrombectomy strategy for CTOs remains unclear. This meta-analysis aimed to compare the safety and efficacy outcomes of different thrombectomy techniques in the treatment of CTOs.
2. Methods
This meta-analysis is reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) 2020 guidelines.17 A combination of keywords and standardized index terms was used to develop search strategies for different databases. Searches were run on January 6, 2022 in Ovid Cochrane Central Register of Controlled Trials (1991+), Ovid Embase (1974+), Ovid Medline (1946+ including epub ahead of print, in-process & other non-indexed citations), Scopus (1823+), and Web of Science Core Collection (Science Citation Index Expanded 1975+ & Emerging Sources Citation Index 2015+). After the deduplication process, a total of 189 citations were retrieved. Full search strategies are provided in the appendix for each screened database. The reference lists of all included articles were searched for additional studies.
All relevant original publications reporting safety and efficacy outcomes of MT for CTOs were included. No limitations on publication year were applied, and publications up to January 6, 2022 were screened. Exclusion criteria consisted of 1) non-original studies (review articles, editorials, video reports, correspondence papers, meta-analyses, and post-hoc studies), 2) case series consisting of <10 patients, 3) studies not providing detailed outcomes for CTOs, 4) articles not written in the English language, 5) In vitro and Ex vivo studies, 6) conference papers and abstracts, 7) studies with overlapping datasets, 8) studies employing thrombectomy devices other than stent retrievers (SR) and modern aspiration catheters (ASP).
The systematic literature review performed using the Nested Knowledge (St. Paul, MN, USA) semi-automated software and its AutoLit platform. Two authors (MM, HK) performed the initial title and abstract screening. Following the initial screening, full texts of all included articles were retrieved and reviewed. The initial and full-text screenings were completed on the AutoLit platform. Any disagreement between the reviewers was resolved by the senior author (DFK with more than 20 years of experience).
2.1. Data extraction and study outcomes
Two authors performed data extraction using the AutoLit platform. Extracted data included successful recanalization, first-pass efficacy, functional independence, symptomatic hemorrhage (sICH), and baseline patient characteristics.
Successful recanalization was defined as Thrombolysis in Cerebral Infarction scale (TICI) ≥2b, and first pass efficacy (FPE) was described as TICI ≥ 2b recanalization at the first thrombectomy pass. Functional independence was assessed with the modified Rankin Scale (mRS), and an mRS score of ≤2 at 90 days was defined as functional independence.
2.2. Risk of bias
Two authors performed the quality assessment using the modified Newcastle–Ottawa Scale for case–control studies. Questions regarding selection criteria were modified using four criteria: 1) Did the study include all patients or a selected sample? 2) study design (retrospective or prospective) 3) was the clinical and imaging data satisfactory? 4) Were the treatment protocols described thoroughly?
2.3. Statistical analysis
Using R software version 4.1.3, we calculated prevalence rates and corresponding 95% confidence intervals (CI). A random model was adopted to pool all data due to heterogeneity among the included studies. Thus, the potential outliers' impact on overall effect sizes have been limited. Heterogeneity was assessed using Q statistic and the I2 test, where I2 > 50% or P-value <0.05 were considered significant. We conducted subgroup analyses based on the treatment used to explore possible sources of heterogeneity and to test any associated differences in study outcomes. Overall effect sizes, raw event/total rates, and the degree of inter-study heterogeneity are presented in the forest plots. The number of studies analyzed was less than ten; therefore, publication bias (Egger's regression test) and the impact of sample size (meta-regression) were unable to be tested.18,19
3. Results
3.1. Study characteristics
After deduplication, we identified 189 studies that were eligible for screening. We excluded 183 articles after initial and full-text screenings. A total of 6 articles with 524 patients were included in this meta-analysis (Fig. 1).12,20, 21, 22, 23, 24
Fig. 1.
PRISMA flow chart.
Table 1 summarizes the characteristics of the included studies. Two studies were comparative (SR vs. ASP and ASP vs. SR + ASP).12,20 The remaining 4 studies were single-armed. Functional independence data were available in all six studies. Five studies provided successful recanalization and sICH data.12,20, 21, 22, 23 Finally, FPE data were available in three studies.12,20,22
Table 1.
Characteristics of the studies included within quantitative synthesis.
| Study, year, country | Study characteristics |
CTO sample size for first-line thrombectomy strategies |
||||
|---|---|---|---|---|---|---|
| Study design | Study population | Study focus | SR | ASP | SR + ASP | |
| Lee et al. 2013, South Korea | Single center, retrospective | CTOs | SR + ASP vs IVT | – | – | 10 |
| Rai et al., 2013, USA | Multicenter, retrospective | ICA occlusions | MT vs. IVT in ICA occlusions | 29 | – | – |
| Orton et al. 2014, Canada | Single center, retrospective | CTOs | SR's performance in CTOs | 20 | – | – |
| Xing et al. 2020, China | Single center, retrospective | CTOs | SR vs. ASP | 69 | 40 | – |
| Maus et al. 2021, International | Multicenter, retrospective | CTOs | SR's performance in CTOs | 17 | – | – |
| Diana et al. 2021, Italy | Multicenter, retrospective | CTOs | ASP vs. SR + ASP | – | 304 | 49 |
ASPP, aspiration; SR, stent retriever; SR + ASP, combined stent retriever and aspiration thrombectomy; CTO, carotid terminus occlusions; ICA, internal carotid artery.
3.2. Quality assessment
Two studies had a moderate to high risk of bias, and the risk of bias was low in the remaining four articles. All included articles had a retrospective design. The second most common issue was incomparability. Five studies focused on CTOs, and the remaining study included all ICA occlusions. Two studies directly compared the performance of first-line thrombectomy techniques. Results of the quality assessment were presented in Supplementary Table 1.
3.3. Recanalization (TICI 2b-3)
Five studies with 509 patients reported the recanalization rates following thrombectomy. Overall, successful recanalization was achieved in 85.84% (95% CI = 77.96–94.52) of the patients following thrombectomy; however, significant heterogeneity was observed among the included studies (I2 = 92%; P-value< 0.001). On further subgroup analysis, different techniques yielded comparable recanalization rates (P-value = 0.697), with 87.99%, 85.77%, and 82.41% for SR, ASP, and combined SR + ASP, respectively (Fig. 2).
Fig. 2.
Forest plot of successful recanalization.
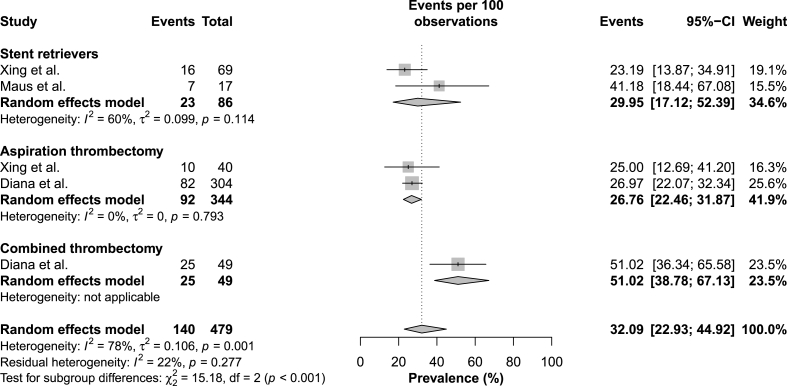
3.4. First pass efficacy
There were three studies with 479 patients reporting MT outcomes for CTOs. Overall, first-pass efficacy was 32.09% (95% CI = 22.93–44.92); however, significant heterogeneity was observed among the included studies (I2 = 78%; P-value< 0.001). On further subgroup analysis, first-line MT techniques’ first-pass efficacy was significantly different, with 29.95%, 26.76%, and 51.02% for SR, AS, and combined SR + ASP, respectively. The heterogeneity was associated with the first-line treatment strategy and significantly decreased after subgroup analysis (residual heterogeneity, I2 = 22%; P-value = 0.277) (Fig. 3).
Fig. 3.
Forest plot of first pass efficacy.
3.5. Functional independence
Six studies with 524 patients reported a functional independence rate for CTOs. Overall, functional independence rate was 39.73% (95% CI = 32.95–47.89); however, moderate heterogeneity was observed among the included studies (I2 = 49%; P-value = 0.055). On further subgroup analysis, there were statistically significant differences across treatment techniques (P-value = 0.486), with 33.58%, 39.38%, and 24.03% for SR, ASP, and combined SR + ASP, respectively (Fig. 4).
Fig. 4.
Forest plot of functional independence.
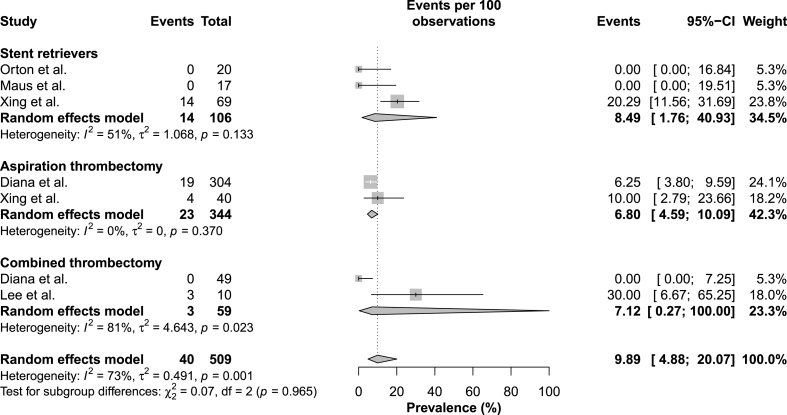
3.6. Symptomatic intracranial hemorrhage
There were 5 studies with 509 patients reporting sICH rates after endovascular treatment. Overall, sICH rate was 9.89% (95% CI = 4.88–20.07); however, significant heterogeneity was present among the included studies (I2 = 73%; P-value< 0.001). On further subgroup analysis, the sICH rates did not significantly differ across groups (P-value< 0.965), with 8.49%, 6.8%, and 7.12% for SR, ASP, and combined SR + ASP, respectively (Fig. 5).
Fig. 5.
Forest plot of symptomatic intracranial hemorrhage.
4. Discussion
Our meta-analysis on carotid terminus thrombectomy identified several important findings. First, the safety and efficacy outcomes of carotid terminus thrombectomy were similar to other comprehensive studies involving PLVOs.1, 2, 3, 4,25 Second, successful recanalization rates did not significantly differ between ASP, SR, and SR + ASP groups. Third, SR + ASP technique provided higher rates of FPE than SR or ASP alone. These findings are important because they indicate that MT may be effective for CTOs. Additionally, our findings suggest that SR + ASP technique may be the favorable treatment option for CTOs due to its low sICH and significantly greater FPE rates. However, further comparative studies are necessary to establish the superiority of the SR + ASP technique in CTOs.
ASTER and COMPASS trials did not find a significant difference in successful recanalization between ASP and SR techniques.14,15 However, in ASTER 2, SR + ASP provided a significantly higher successful recanalization rate than SR alone.13 Additionally, ETIS investigators have recently compared the performance of three first-line thrombectomy strategies in the same prospective large cohort.26 Our systematic review showed that, similar to the results reported in ASTER2, the combined SR + ASP technique was associated with significantly greater successful recanalization rates than SR alone in the ETIS registry.26 However, cohorts of these prospective studies predominantly consisted of M1 occlusions, and subgroup analyses focused on CTOs were not available. In our meta-analysis, the overall successful recanalization rate was 85.47% (95% CI = 75.28–97.03) for CTOs, and it was comparable to those of the four pivotal prospective studies.13, 14, 15,26 However, the differences in successful recanalization rates were insignificant across first-line treatment strategies. ICA terminus is approximately 25% larger than M1, and its occlusions are associated with a large clot burden.7, 8, 9, 10,27 Traditional aspiration catheters are primarily designed for MCA occlusions and have a relatively small inner diameter (ID) for CTOs. This size difference can affect the efficacy of ASP and SR + ASP techniques in CTOs. A recent preliminary study using a larger bore aspiration catheter achieved a successful recanalization rate of 94.7% with ASP only.28 However, despite their theoretical advantages and promising preliminary data, further studies are needed to establish the improved efficacy of larger ID aspiration catheters in CTOs.
CTOs typically present with greater infarct volume compared to MCA or more proximal ICA occlusions and, therefore, are associated with severe neurologic deficits even after MT. However, in our meta-analysis, the overall functional independence rate was 39.83 (95% CI = 32.95–47.89) and was comparable to those of pivotal RCTs.4,13, 14, 15,26 Our promising results suggest that the functional outcome of CTOs may not be different from other well-studied occlusion sites in the era of modern MT.
Despite the similar successful recanalization rates across groups, SR + ASP technique achieved significantly higher FPE than other treatment strategies. Given the large infarct volume associated with CTOs, FPE can be particularly important for CTOs and may affect the severity of the neurologic deficit.7,8,29,30 In our study, the ASP alone group had the highest functional independence rate. However, this finding should be taken with precaution as some of the studies in the SR and SR + ASP groups were published before the landmark MT trials.21,23,24 Differences in patient selection criteria and operator experience might have affected the functional independence outcomes.
Unsuccessful recanalization and device-related vessel injury are the most important predictors of sICH.31,32 The SR technique has been associated with an increased risk of vessel wall injury and endothelial damage.33, 34, 35 Therefore, greater frequencies of hemorrhagic complications have been one of the most important concerns with combined treatment. Interestingly, in our meta-analysis, sICH rates did not differ significantly across MT techniques, and the sICH rate of SR + ASP group remained at 7.12%. There are two possible explanations for this finding. First, the high FPE efficacy of the SR + ASP group might have limited the hemorrhagic transformation.29,30,32 Second, retraction of SR into ASP catheter instead of proximally located distal access catheter might have limited the endothelial injury.
5. Limitations
Our study has several limitations. First, the severity of CTO can substantially vary depending on the occlusion subtype (I, L, or T) and cerebrovascular anatomy. For example, CTOs may affect the contralateral hemisphere via dominant ACA or might even be asymptomatic when robust collateral supply is present through the circle of Willis. Second, thrombectomy device size and model can significantly affect treatment outcomes. However, unfortunately, occlusion morphology, collateral status, device size, and model data were not available in most of the included studies. Third, a few included studies were published before the landmark MT trials, which might have affected the outcomes due to less informed patient selection. Finally, pre-thrombectomy thrombolysis utilization can also affect the safety and efficacy outcomes of the treatment groups.36,37 However, thrombolysis utilization data were not specifically reported for each safety and efficacy outcome in the included articles.
6. Conclusions
CTOs have historically been associated with poor functional outcomes. Yet, in our meta-analysis, successful recanalization and functional independence rates were similar to those of pivotal MT RCTs. Therefore, our meta-analysis indicates that MT may be safe and highly effective for CTOs. Additionally, in our meta-analysis, the combined SR + ASP technique provided significantly higher FPE rates than SR and ASP, without an increase in hemorrhagic complications. Further prospective, large-scale studies are necessary to determine the optimal first-line MT technique in the endovascular treatment of CTOs.
CRediT authorship contribution statement
Cem Bilgin: Conceptualization, Writing – original draft, Writing – review & editing, Methodology. Hassan Kobeissi: Conceptualization, Data curation, Methodology, Validation, Writing – original draft, Writing – review & editing. Sherief Ghozy: Conceptualization, Data curation, Formal analysis, Methodology, Software, Writing – original draft. Marwa A. Mohammed: Conceptualization, Data curation, Methodology, Writing – original draft. Ramanathan Kadirvel: Conceptualization, Methodology, Supervision, Writing – review & editing, Resources. David F. Kallmes: Conceptualization, Investigation, Methodology, Resources, Supervision, Writing – review & editing.
Declaration of competing interest
RK received research support from Cerenovus Inc, Medtronic, Endovascular Engineering, Frontier Bio, Sensome Inc, Endomimetics, Ancure LLC, Neurogami Medical, MIVI Biosciences, Monarch Biosciences, Stryker Inc, Conway Medical, Piraeus Medical, Bionaut Labs. DFK holds equity in Nested Knowledge, Superior Medical Experts, and Conway Medical, Marblehead Medical, and Piraeus Medical; he receives grant support from MicroVention, Medtronic, Balt, and Insera Therapeutics; has served on the Data Safety Monitoring Board for Vesalio; and received royalties from Medtronic.
Acknowledgements
Nested Knowledge, Inc. (St. Paul, MN) has provided software access for this article.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.wnsx.2023.100208.
Appendix A. Supplementary data
The following is the Supplementary data to this article.
References
- 1.Berkhemer O.A., Fransen P.S., Beumer D., et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372(1):11–20. doi: 10.1056/NEJMoa1411587. [DOI] [PubMed] [Google Scholar]
- 2.Goyal M., Demchuk A.M., Menon B.K., et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372(11):1019–1030. doi: 10.1056/NEJMoa1414905. [DOI] [PubMed] [Google Scholar]
- 3.Jovin T.G., Chamorro A., Cobo E., et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015;372(24):2296–2306. doi: 10.1056/NEJMoa1503780. [DOI] [PubMed] [Google Scholar]
- 4.Saver J.L., Goyal M., Bonafe A., et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015;372(24):2285–2295. doi: 10.1056/NEJMoa1415061. [DOI] [PubMed] [Google Scholar]
- 5.Kobeissi H., Ghozy S., Bilgin C., Kadirvel R., Brinjikji W., Kallmes D.F. Are we improving? Temporal trends in outcomes for mechanical thrombectomy for stroke: a systematic review and meta-analysis of randomized trials. Intervent Neuroradiol. 2023 doi: 10.1177/15910199231158938. [DOI] [PubMed] [Google Scholar]
- 6.Gibo H., Lenkey C., Rhoton A.L., Jr. Microsurgical anatomy of the supraclinoid portion of the internal carotid artery. J Neurosurg. 1981;55(4):560–574. doi: 10.3171/jns.1981.55.4.0560. [DOI] [PubMed] [Google Scholar]
- 7.Fischer U., Mono M.L., Schroth G., et al. Endovascular therapy in 201 patients with acute symptomatic occlusion of the internal carotid artery. Eur J Neurol. 2013;20(7):1017–1024. doi: 10.1111/ene.12094. e87. [DOI] [PubMed] [Google Scholar]
- 8.Hong J.M., Lee S.E., Lee S.J., Lee J.S., Demchuk A.M. Distinctive patterns on CT angiography characterize acute internal carotid artery occlusion subtypes. Medicine (Baltim) 2017;96(5) doi: 10.1097/MD.0000000000005722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barreto A.D., Albright K.C., Hallevi H., et al. Thrombus burden is associated with clinical outcome after intra-arterial therapy for acute ischemic stroke. Stroke. 2008;39(12):3231–3235. doi: 10.1161/STROKEAHA.108.521054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saqqur M., Uchino K., Demchuk A.M., et al. Site of arterial occlusion identified by transcranial Doppler predicts the response to intravenous thrombolysis for stroke. Stroke. 2007;38(3):948–954. doi: 10.1161/01.STR.0000257304.21967.ba. [DOI] [PubMed] [Google Scholar]
- 11.Frahm D., Wunderlich S., Schubert M.I., Poppert H., Kleine J.F., Prothmann S. Mechanical thrombectomy in acute occlusion of the carotid-T: a retrospective single centre study in 51 patients. Clin Neuroradiol. 2016;26(1):23–29. doi: 10.1007/s00062-014-0322-6. [DOI] [PubMed] [Google Scholar]
- 12.Xing P.F., Yang P.F., Li Z.F., et al. Comparison of aspiration versus stent retriever thrombectomy as the preferred strategy for patients with acute terminal internal carotid artery occlusion: a propensity score matching analysis. AJNR Am J Neuroradiol. 2020;41(3):469–476. doi: 10.3174/ajnr.A6414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lapergue B., Blanc R., Costalat V., et al. Effect of thrombectomy with combined contact aspiration and stent retriever vs stent retriever alone on revascularization in patients with acute ischemic stroke and large vessel occlusion: the ASTER2 randomized clinical trial. JAMA. 2021;326(12):1158–1169. doi: 10.1001/jama.2021.13827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lapergue B., Blanc R., Gory B., et al. Effect of endovascular contact aspiration vs stent retriever on revascularization in patients with acute ischemic stroke and large vessel occlusion: the ASTER randomized clinical trial. JAMA. 2017;318(5):443–452. doi: 10.1001/jama.2017.9644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Turk A.S., 3rd, Siddiqui A., Fifi J.T., et al. Aspiration thrombectomy versus stent retriever thrombectomy as first-line approach for large vessel occlusion (COMPASS): a multicentre, randomised, open label, blinded outcome, non-inferiority trial. Lancet. 2019;393(10175):998–1008. doi: 10.1016/S0140-6736(19)30297-1. [DOI] [PubMed] [Google Scholar]
- 16.Nogueira R.G., Frei D., Kirmani J.F., et al. Safety and efficacy of a 3-dimensional stent retriever with aspiration-based thrombectomy vs aspiration-based thrombectomy alone in acute ischemic stroke intervention: a randomized clinical trial. JAMA Neurol. 2018;75(3):304–311. doi: 10.1001/jamaneurol.2017.3967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Page M.J., McKenzie J.E., Bossuyt P.M., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol. 2021;134:178–189. doi: 10.1016/j.jclinepi.2021.03.001. [DOI] [PubMed] [Google Scholar]
- 18.Egger M., Davey Smith G., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ghozy S., Nam N.H., Radwan I., et al. Therapeutic efficacy of hepatitis B virus vaccine in treatment of chronic HBV infections: a systematic review and meta-analysis. Rev Med Virol. 2020;30(3) doi: 10.1002/rmv.2089. [DOI] [PubMed] [Google Scholar]
- 20.Diana F., Vinci S.L., Ruggiero M., et al. Comparison of aspiration versus combined technique as first-line approach in terminal internal carotid artery occlusion: a multicenter experience. J Neurointerventional Surg. 2022;14(7):666–671. doi: 10.1136/neurintsurg-2021-017585. [DOI] [PubMed] [Google Scholar]
- 21.Lee J.S., Hong J.M., Lee S.J., Joo I.S., Lim Y.C., Kim S.Y. The combined use of mechanical thrombectomy devices is feasible for treating acute carotid terminus occlusion. Acta Neurochir (Wien) 2013;155(4):635–641. doi: 10.1007/s00701-013-1649-5. [DOI] [PubMed] [Google Scholar]
- 22.Maus V., Hüsken S., Kalousek V., et al. Mechanical thrombectomy in acute terminal internal carotid artery occlusions using a large manually expandable stentretriever (tiger XL device): multicenter initial experience. J Clin Med. 2021;10(17) doi: 10.3390/jcm10173853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Orton T.H., Lum C., Alhazzaa M., et al. Acute stroke patients treated with stent retrievers in carotid "T" occlusions have improved recanalization and outcome. Can J Neurol Sci. 2014;41(6):709–713. doi: 10.1017/cjn.2014.109. [DOI] [PubMed] [Google Scholar]
- 24.Rai A.T., Carpenter J.S., Raghuram K., Roberts T.D., Rodgers D., Hobbs G.R. Endovascular therapy yields significantly superior outcomes for large vessel occlusions compared with intravenous thrombolysis: is it time to randomize? J Neurointerventional Surg. 2013;5(5):430–434. doi: 10.1136/neurintsurg-2012-010429. [DOI] [PubMed] [Google Scholar]
- 25.Goyal M., Menon B.K., van Zwam W.H., et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387(10029):1723–1731. doi: 10.1016/S0140-6736(16)00163-X. [DOI] [PubMed] [Google Scholar]
- 26.Maïer B., Finitsis S., Bourcier R., et al. First-line thrombectomy strategy for anterior large vessel occlusions: results of the prospective ETIS egistry. J Neurointerventional Surg. 2022;14(5) doi: 10.1136/neurintsurg-2021-017505. [DOI] [PubMed] [Google Scholar]
- 27.Rai A.T., Hogg J.P., Cline B., Hobbs G. Cerebrovascular geometry in the anterior circulation: an analysis of diameter, length and the vessel taper. J Neurointerventional Surg. 2013;5(4):371–375. doi: 10.1136/neurintsurg-2012-010314. [DOI] [PubMed] [Google Scholar]
- 28.Romano D.G., Frauenfelder G., Diana F., Saponiero R. JET 7 catheter for direct aspiration in carotid T occlusions: preliminary experience and literature review. Radiol Med. 2022;127(3):330–340. doi: 10.1007/s11547-022-01451-2. [DOI] [PubMed] [Google Scholar]
- 29.Bai X., Zhang X., Yang W., et al. Influence of first-pass effect on recanalization outcomes in the era of mechanical thrombectomy: a systemic review and meta-analysis. Neuroradiology. 2021;63(5):795–807. doi: 10.1007/s00234-020-02586-7. [DOI] [PubMed] [Google Scholar]
- 30.Jadhav A.P., Desai S.M., Budzik R.F., et al. First pass effect in patients with large vessel occlusion strokes undergoing neurothrombectomy: insights from the Trevo Retriever Registry. J Neurointerventional Surg. 2021;13(7):619–622. doi: 10.1136/neurintsurg-2020-016952. [DOI] [PubMed] [Google Scholar]
- 31.Venditti L., Chassin O., Ancelet C., et al. Pre-procedural predictive factors of symptomatic intracranial hemorrhage after thrombectomy in stroke. J Neurol. 2021;268(5):1867–1875. doi: 10.1007/s00415-020-10364-x. [DOI] [PubMed] [Google Scholar]
- 32.Montalvo M., Mistry E., Chang A.D., et al. Predicting symptomatic intracranial haemorrhage after mechanical thrombectomy: the TAG score. J Neurol Neurosurg Psychiatry. 2019;90(12):1370–1374. doi: 10.1136/jnnp-2019-321184. [DOI] [PubMed] [Google Scholar]
- 33.Arai D., Ishii A., Chihara H., Ikeda H., Miyamoto S. Histological examination of vascular damage caused by stent retriever thrombectomy devices. J Neurointerventional Surg. 2016;8(10):992–995. doi: 10.1136/neurintsurg-2015-011968. [DOI] [PubMed] [Google Scholar]
- 34.Peschillo S., Tomasello A., Diana F., et al. Comparison of subacute vascular damage caused by ADAPT versus stent retriever devices after thrombectomy in acute ischemic stroke: histological and ultrastructural study in an animal model. Interv Neurol. 2018;7(6):501–512. doi: 10.1159/000491028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Teng D., Pannell J.S., Rennert R.C., et al. Endothelial trauma from mechanical thrombectomy in acute stroke: in vitro live-cell platform with animal validation. Stroke. 2015;46(4):1099–1106. doi: 10.1161/STROKEAHA.114.007494. [DOI] [PubMed] [Google Scholar]
- 36.Kobeissi H., Adusumilli G., Ghozy S., et al. Mechanical thrombectomy alone versus with thrombolysis for ischemic stroke: a meta-analysis of randomized trials. Intervent Neuroradiol. 2023 doi: 10.1177/15910199231154331. [DOI] [PubMed] [Google Scholar]
- 37.Kobeissi H., Ghozy S., Turfe B., et al. Tenecteplase vs. alteplase for treatment of acute ischemic stroke: a systematic review and meta-analysis of randomized trials. Front Neurol. 2023;14 doi: 10.3389/fneur.2023.1102463. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.