Abstract
Objective
The purpose of this study is to examine the regional distribution of the pediatric surgery workforce and the expected local demand for pediatric surgical procedures in Brazil.
Methods
We collected data on the pediatric surgical workforce, surgical volume, Gross Domestic Product per capita, and mortality for gastrointestinal tract malformations (MGITM) across the different regions of Brazil for 2019.
Results
Data from the Federal Medical Council reported 1515 pediatric surgery registries in Brazil, corresponding to 1414 pediatric surgeons (some pediatric surgeons are registered in more than one state), or 2.4 pediatric surgeons per 100 000 children 14 years of age and younger. There were 828 men and 586 women. The mean age was 51.5±12.8 years, and the mean time from graduation was 3.4±5.7 years. There is a higher concentration of pediatric surgeons in the wealthier Central-West, South, and Southeast regions. Individual surgical volume ranged from 88 to 245 operations/year (average 146 operations/year) depending on the region. Of these, only nine (6.1%) were high-complexity (including neonatal) operations. MGITM tended to be higher in the poorer North and Northeast regions than in other regions of Brazil.
Conclusions
Our findings suggest significant disparities in the surgical workforce and workload across Brazil related to socioeconomic status. Regions with an increased surgical workforce were associated with lower MGITM. The average number of complex operations performed annually by each pediatric surgeon was considerably low. Strategic investment and well-defined health policies are imperative to enhance the quality of surgical care in the different regions of Brazil.
Level of evidence
Retrospective review; level IV.
Keywords: Child Health, Health Services, Mortality
WHAT IS ALREADY KNOWN ON THIS TOPIC
It is well-known that there are profound differences in the distribution of wealth and basic resources among the different geographic regions in Brazil. However, it is unclear how this impacts the distribution of the pediatric surgery workforce and surgical needs across those regions.
WHAT THIS STUDY ADDS
There is wide variation in the concentration of pediatric surgeons in the different regions of Brazil, which correlates positively with Gross Domestic Product per capita.
Although the expected number of operations for each pediatric surgeon seems adequate (88–245 operations per surgeon per year), the expected number of complex operations (especially neonatal surgery) is very small (2.1–5.9 operations per surgeon per year), possibly jeopardizing the quality of surgical care.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Governmental and social strategies must be implemented to try to correct the inequalities in the distribution of pediatric surgeons in Brazil as well as to try to rationalize the distribution of complex operations, aiming to offer the best possible standard of surgical care in all regions of Brazil.
Introduction
In recent years, there has been an increase in the publication of general data on the demand and workforce of pediatric surgery in several countries.1–7
In Brazil, despite some recent publications,8–11 information regarding the exact size of the pediatric surgery workforce, as well as the regional demands for pediatric operations, is scarce and often ambiguous, depending on the source of the information. This lack of reliable information makes it challenging to plan the needs of these professionals across the different regions of Brazil and estimate the annual requirement for training new pediatric surgeons.
The purpose of this study is to present data on the regional distribution of the pediatric surgical workforce, seeking to correlate it with the expected local demand for pediatric surgical procedures and propose potential alternatives.
Methods
This study is an ecological, cross-sectional descriptive analysis using data from the Brazilian public health system (Sistema Unico de Saude) and the Brazilian Institute of Geography and Statistics (IBGE).
Data from the IBGE show that in 2019, Brazil had 213 million inhabitants and a Gross Domestic Product (GDP) per capita of US$6277.86. It comprises 26 states and a federal district, which are grouped into five major regions (North, Northeast, Southeast, South, and Central-West). From the economic point of view, the North and Northeast regions are poorer, displaying an average GDP of approximately US$3580.00, whereas the remaining regions display an average GDP of US$7678.57.
Estimates of the pediatric surgery workforce and surgical volume were obtained from the databases available at IBGE (http://tabnet.datasus.gov.br/cgi/deftohtm.exe?ibge/cnv/popbr.def),12 taking 2019 as a reference, as well as the data from the Federal Medical Council (CFM) contained in the document MEDICAL DEMOGRAPHY IN BRAZIL 2020.13 Pediatric surgical workforce density (PSWD) was defined as the number of pediatric surgeons for every 100 000 children 14 years of age or younger. To determine the PSWD, data from this last publication were used. This is because this document derives data from CFM, which is the official registry where doctors are required to be registered to practice their specialty.
To assess the surgical demand in the different states and regions of Brazil, a set of index surgical procedures was employed. This set was adapted from previously published data and was divided into two levels of complexity. Low-complexity operations consisted of procedures such as hernia repair, orchidopexy, appendicitis, vascular access, hypospadias repair, congenital megacolon management, pyloromyotomy for pyloric stenosis, and pediatric gastroesophageal reflux repair. Complex operations included neonatal surgery (intestinal atresia, anorectal malformation, esophageal atresia, abdominal wall defects, diaphragmatic hernia, neonatal enterocolitis), correction of biliary atresia, and choledochal cysts. The expected number of surgeries was estimated based on the published incidence of each corresponding pathology.9 14–17 Surgeries performed because of trauma, oncologic surgeries, transplants, or reoperations were not included in the demand estimate.
To obtain a preliminary assessment of the outcomes of neonatal surgery in the various regions of Brazil, we evaluated the mortality rate associated with a consolidated diagnosis of malformations of the digestive system, which comprised International Classification of Diseases-10 codes ranging from Q38 to Q45.
The data are presented in tables and graphs. Due to the descriptive nature of this study, no attempt was made to perform any statistical calculations with the data.
Results
According to the data from CFM,13 there are a total of 1515 pediatric surgery registries in Brazil, corresponding to 1414 pediatric surgeons (some pediatric surgeons are registered in more than one state), or 2.4 pediatric surgeons per 100 000 inhabitants ≤14 years of age. Of these, 828 were men and 586 were women, with a ratio of 1.41:1. The mean age was 51.5±12.8 years, and the mean time from graduation was 3.4±5.7 years.
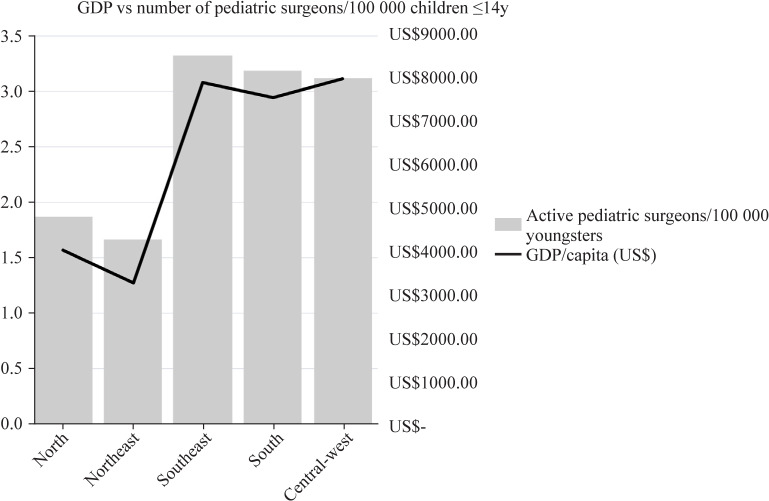
The distribution of pediatric surgeons in Brazil is not equal (table 1 and figure 1). PSWD was higher in the Southeast, South, and Central-West regions of Brazil, which tended to have the highest GDP/capita. Conversely, the North and Northeast regions have roughly half the concentration of pediatric surgeons compared to the other regions.
Table 1.
Distribution of the demographic and pediatric surgery workforce and workload across the different regions of Brazil
| Region | North | Northeast | Southeast | South | Central-West | Brazil |
| Number of inhabitants (IBGE) | 18 906 962 | 57 667 842 | 89 632 957 | 30 402 587 | 16 707 336 | 213 317 684 |
| Number of live births | 301 635 | 770 688 | 2 093 142 | 796 536 | 230 474 | 4 192 475 |
| Childhood mortality (number/1000 births) | 16.6 | 15.3 | 11.7 | 10.1 | 13.0 | 13.3 |
| Number of children <1 year old | 296 628 | 758 896 | 2 068 652 | 788 491 | 227 478 | 4 136 715 |
| Number of children ≤14 years (IBGE) | 3 483 144 | 15 397 314 | 23 932 000 | 8 117 491 | 4 460 859 | 56 955 822 |
| GDP per capita (US$) | 4024.43 | 3278.53 | 7917.89 | 7579.26 | 8014.17 | 6277.89 |
| Pediatric surgery workforce | ||||||
| Active pediatric surgeons | 65 | 256 | 796 | 259 | 139 | 1515 |
| Active pediatric surgeons/100 000 children | 1.9 | 1.7 | 3.3 | 3.2 | 3.1 | 2.7 |
| Number of children ≤14/pediatric surgeon | 536 | 601 | 301 | 313 | 321 | 376 |
| Number of children <1 year/pediatric surgeon | 4564 | 2964 | 2599 | 3044 | 1637 | 2731 |
| Expected number of operations/pediatric surgeon/year | ||||||
| Low complexity | 230.0 | 149.4 | 131.0 | 153.4 | 82.5 | 137.6 |
| High complexity | 15.1 | 9.8 | 8.6 | 10.0 | 5.4 | 9.0 |
| High complexity except for NEC | 5.9 | 3.9 | 3.4 | 4.0 | 2.1 | 3.5 |
| Total annual surgical volume/pediatric surgeon | 245.5 | 159.5 | 139.8 | 163.8 | 88.0 | 146.9 |
| Weekly surgical volume/pediatric surgeon | 5.1 | 3.3 | 2.9 | 3.4 | 1.8 | 3.1 |
| Mortality secondary to gastrointestinal tract malformations | ||||||
| Number of admissions in 2019 | 514 | 1317 | 2620 | 898 | 497 | 5846 |
| Number of deaths in 2019 | 16 | 54 | 54 | 19 | 8 | 152 |
| Mortality rate (%) | 3.11 | 4.10 | 2.06 | 2.12 | 1.61 | 2.60 |
GDP, Gross Domestic Product; IBGE, Brazilian Institute of Geography and Statistics; NEC, neonatal necrotizing enterocolitis.
Figure 1.
Graphic display of the distribution of the pediatric surgery workforce across the different regions of Brazil. GDP, Gross Domestic Product.
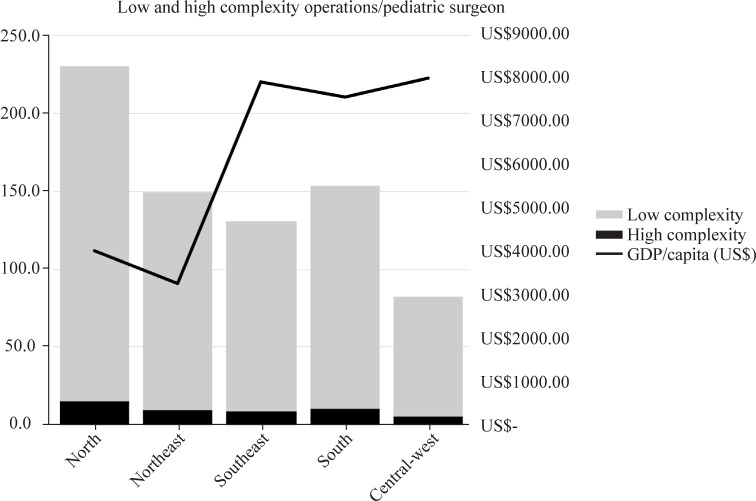
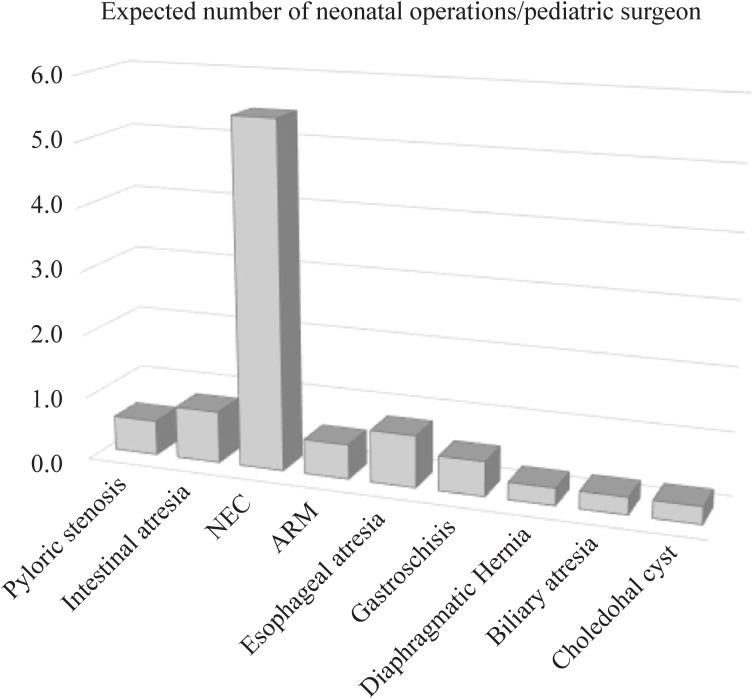
Accordingly, the workload in North and Northeast regions is greater than that in the Central and Southern regions due to the low number of pediatric surgeons (figure 2). Based on the demographic data, a Brazilian pediatric surgeon is expected to perform an average of 147 pediatric operations per year, or 3.1 per week. Of these operations, only nine (6.1%) were highly complex operations. For most neonatal operations, the expected number per pediatric surgeon is less than one per year (figure 3).
Figure 2.
Graphic representation of the distribution of surgical workload of pediatric surgeons across the different regions of Brazil. GDP, Gross Domestic Product.
Figure 3.
Graphic representation of the expected number of complex operations per pediatric surgeon per year in Brazil. ARM, anorectal malformation; NEC, neonatal necrotizing enterocolitis.
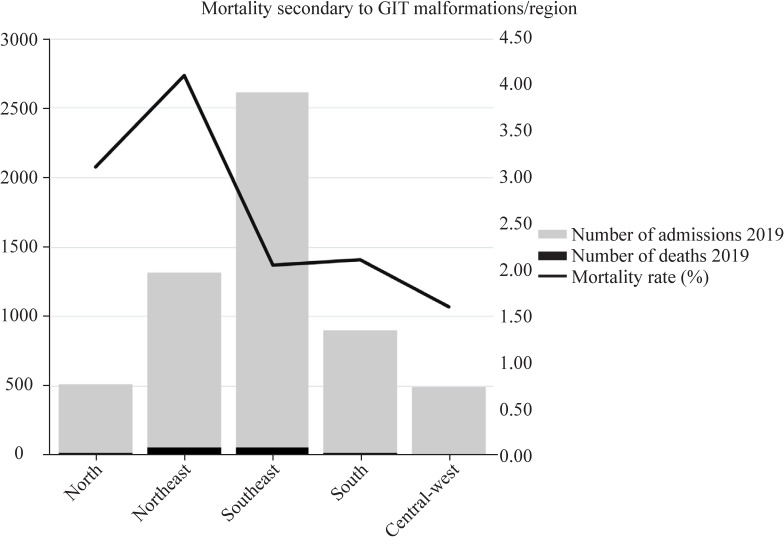
Figure 4 indicates that the mortality rate of neonatal surgery in the Southern States (Southeast, South, and Central-West) is roughly half of that observed in the Northern States (North and Northeast).
Figure 4.
Graphic representation of the mortality secondary to malformations of the gastrointestinal tract (GIT) across the different regions of Brazil in 2019.
Discussion
Data from the present study indicate that pediatric surgery is a minor surgical specialty in Brazil compared with other surgical specialties. The number of pediatric surgeons in Brazil represents approximately 0.31% of the total number of doctors in the country.
As previously mentioned, data may be conflicting depending on the source of information. In 2019, while the CFM counted 1515 pediatric surgeons, the IBGE reported the existence of only 674 pediatric surgeons in Brazil. This data disparity has been reported before, but the cause is still unclear.9
Additionally, in 2019, the Brazilian Association of Pediatric Surgeons (CIPE) had only 454 registered members, implying that nearly half of the surgeons performing surgeries on children in Brazil are not certified by the CIPE. It is noteworthy to mention that, theoretically, Brazilian regulations only require a diploma from the CFM to practice any medical or surgical specialty. However, although not mandatory, it is strongly believed that obtaining certification from a medical association, such as CIPE, is perceived as a seal of quality in the professional activity of pediatric surgeons.
According to the data from the CFM, the Brazilian PSWD is slightly lower than that observed in developed countries (2.65 vs 3.28/100 000 children ≤14 years of age). A European Census regarding pediatric surgery indicates that in the European Union, there are 3.9 pediatric surgeons/100 000 children and approximately 1662 neonates for each pediatric surgeon.18 On the other hand, middle-income and low-income countries have 0.94 and 0.05 pediatric surgeons/100 000 children under 15 years of age.4 Recent research suggests that there is a correlation between PSWD <0.37/100 000 and decreased odds of survival for specific pediatric conditions.1 Accordingly, our findings reveal that the mortality rate for congenital gastrointestinal tract malformations is higher in the lower PSWD regions.
The distribution of pediatric surgeons across the different regions of Brazil is highly unequal, with the North and Northeast regions having the lowest PSWD (1.9 and 1.7 pediatric surgeons/100 000 children, respectively). This disparity is particularly evident in the North region, where one state, Acre, has only one registered pediatric surgeon serving a population of approximately 900 000 inhabitants. This disparity has been previously associated with GDP per capita,19 as well as with the mortality rate of children under 5 years old.11 There is a need for governmental policies to address these disparities and to allocate surgical resources accordingly.
Our findings, based on the incidence of pediatric surgical diseases, show that a Brazilian pediatric surgeon performs an average of 147 operations per year, ranging from 88 to 246 operations annually, depending on the region. However, only 6.1% of these surgeries are high-complexity (including neonatal) surgical procedures. The expected number of specific neonatal operations performed each year by the individual pediatric surgeon is very small, averaging less than one operation/year/pediatric surgeon, for instance, for esophageal atresia or diaphragmatic hernia.
These numbers are not exclusive to our country. Similar trends can be observed in other countries. The European Census on Pediatric Surgery showed that the European surgeon performs an average of 202 procedures per year, of which 11 procedures are on neonates.18 A 2016 study in the USA indicated that many surgeons do not perform any ‘complex index cases’ for extensive periods. In that study, over the preceding year before recertification, the median number of cases per surgeon was one for esophageal atresia repair, with almost 40% of surgeons doing none. Similarly, 40% of surgeons had not performed any pull-through operations for Hirschsprung’s disease, and 60% had not performed any cases of either biliary atresia or choledochal cyst in the same period.20 These findings suggest a necessity to re-evaluate the current approach to pediatric surgical care and to consider alternative models, as there may not be enough cases for the average surgeon to maintain competence to repair complex congenital anomalies.
Although a controversial issue, it would be ideal to start a national debate regarding the best healthcare pathway to be offered to those children in need of complex surgical attention.2 21–23 Care for these children is dependent not only on the presence of well-trained and skilled pediatric surgeons but also on the existence of adequate facilities and highly specialized interdisciplinary pediatric teams (including pediatric anesthesiologists, neonatologists, radiologists, surgically trained nurses, etc) to successfully face the challenges posed by these patients.24 25
International experience suggests that creating decentralized regional centers for pediatric surgical care could improve outcomes and reduce costs.21 26–29
In 2008, the American Pediatric Surgical Association published a position statement saying that ‘Because neonatal and infant surgical conditions are relatively uncommon and teams of appropriately skilled professionals and health systems properly resourced for expert perioperative care of infants are limited in number, the association strongly advocates that the surgical care of high-intensity infants occur within facilities with the human and institutional resources outlined. We view this approach as offering the greatest likelihood of providing optimal medical and surgical care to infants who have significant surgical conditions.’30 This position has been supported by several studies, which have confirmed that regionalization of neonatal surgical care is associated with improved surgical outcomes.31 32
In the UK, all patients with biliary atresia are cared for in three centers: Leeds, Birmingham, and King’s College in London. Notably, numerous well-known hospitals are not on that list.33 As a result of this centralization, each of the three centers sees a substantial number of cases, with an average of more than 30 patients diagnosed with biliary atresia per year. This concentration of cases has led to an improvement in transplant-free survival rates and has allowed the UK to achieve results that are on par with, or even surpass, the best outcomes in Europe.34 35
It is noteworthy that there is already an internal spontaneous ‘regionalization’ within most pediatric surgery groups worldwide, with some surgeons performing or supervising specific complex operations more often than others.36 The development and growth of pediatric urology as a pediatric surgery subspecialty serve as a prime example of the spontaneous trend toward subspecialization, as does the evolution of fetal surgery.37
Arguments against the regionalization of healthcare include the potential for social dislocation for families, the risk of increased incidental expenses, and the likelihood of pediatric surgeons losing their expertise and income.21–23
However, experiences such as the center for anorectal malformations or the hepatobiliary surgery in Cincinnati demonstrate that concentrating the treatment of certain complex issues in resource-rich children’s environments may be better than approaching these problems as a yearly event at a general county hospital by a general pediatric surgeon. These centers have reported that most of the complex cases they handle are children who have been referred after failed primary surgical correction attempts performed at county hospitals by local pediatric surgeons who have received training to treat those patients.38–40
The primary objective is not to restrict the practice of pediatric surgery at any center, which would be unethical, but rather to identify ways to stimulate the development of resource-rich children’s environments devoted to the care of these children. In Brazil, the well-succeeded administration model of the liver transplant program, in which hospitals wishing to start a liver transplant program must meet a comprehensive list of standards to be accredited by the National Health Service and receive payment for their services, can serve as a reference for the establishment of several regional resource-rich pediatric surgery centers. These centers should be strategically distributed in the different regions of the country according to the expected number of patients and the existing workforce.
Additionally, it is of utmost importance to rethink how we train new pediatric surgeons to work in a situation where they shall perform a significant number of low-complexity operations yearly but only a few complex surgeries. The declining availability of complex procedures increases the cost and duration of pediatric surgery training and drastically changes the job market.41–44 A survey of pediatric surgeons in the USA revealed that while the number of simple procedures is increasing, the number of complex operations is decreasing.45 In Brazil, pediatric surgeons often hold multiple jobs and are constantly on call at multiple hospitals, leading to a lack of comprehensive patient postoperative follow-up. Although this is far from ideal care, it is the reality that the organization of health services in Brazil has led us into. The question then arises: What are we doing to address these issues, and, most importantly, how are we preparing future pediatric surgeons to work within this scenario or, perhaps, to change it?
In the context of this potential scenario, it would be advisable to consider implementing two levels of training of pediatric surgeons in Brazil. The first would comprise a general pediatric surgeon trained over a period of 2 years in general pediatric surgery. A smaller number of specialized pediatric surgeons, selected among those who complete this general training, would undergo 1 or 2 additional years of specialized training in the above-mentioned specialized centers. These latter professionals would be prepared to work with advanced pediatric surgery in the high-complexity pediatric surgery centers scattered around the country. This could result in a rationalization of costs and better-trained experts, improving the quality of the care offered to children needing complex surgical procedures.31 Although controversial by nature, this is an important subject that needs to be objectively examined.
Data from the present study must be regarded with caution, as the results are based only on the activities of individual surgeons. It is acknowledged that pediatric surgeons, in most pediatric hospitals, work together in variable-size groups. Therefore, it would be more accurate to evaluate the volume of the pediatric surgery departments or services instead of that of individual surgeons, as done by the European Census on Pediatric Surgery.17 This would result in a more realistic picture of the present situation. Efforts to perform a national survey for this purpose are underway.
Moreover, it is possible that the surgical department’s expected volume might have been underestimated, as it has been based on a list of index operations that does not include oncologic surgery, trauma, reoperations, or the time to care for the children outside the operating room. Another limitation of this study is the noticeable disparity of information obtained from different sources. To effectively address the problems and to appropriately plan the activities and training programs of pediatric surgeons in Brazil, it is paramount to accurately determine the size and professional organization of the pediatric surgery workforce in the different regions of Brazil. To achieve this, standardization of information must be implemented.
The data presented in this paper highlight that despite a seemingly adequate number of pediatric surgeons in Brazil, there are profound regional disparities that lead to unequal standards of care in the different regions of Brazil. Furthermore, the expected individual volume of complex surgical procedures is very low, indicating the need to discuss innovative approaches to the care of children with complex surgical needs and redesign pediatric surgical residents’ training.
This study aims to offer a more grounded basis for the future planning of pediatric surgery in Brazil. It is imperative that CIPE acknowledge these issues, actively participate in improving data collection, and engage in the debate needed to safeguard the quality of pediatric surgical healthcare. The information provided in this study may assist pediatric surgeons, healthcare professionals, and national policymakers in making informed decisions and pursuing improvements in the field of pediatric surgery in Brazil.
Footnotes
Presented at: Parts of this paper have been presented as an oral presentation at the Brazilian Congress of Pediatric Surgery, held in Belo Horizonte, Minas Gerais, Brazil, on October 25–28, 2022.
Contributors: JB-S—project administration, conceptualization, supervision, methodology, writing (review and editing). MLM—formal analysis, writing (review and editing). AR—writing (original draft), data curation. AG—data analysis, writing, review of final draft. AGO-F—data curation, validation, writing (review and editing). JB-S is responsible for the overall content as guarantor. We hereby declare that none of the authors serves as a current Editorial Team member (such as Chief Editors, Associate Editors, Editorial Board Member) for this journal.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available in a public, open access repository. Data are available in a public, open-access repository. All data used for this analysis were obtained from the open-access DATASUS system from the Brazilian Ministry of Health. Data can be obtained freely from: http://tabnet.datasus.gov.br/.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
Ethics approval is waived, in face of the fact that the study does not involve either human or animal participants.
References
- 1.Bouchard ME, Tian Y, Justiniano J, et al. A critical threshold for global pediatric surgical workforce density. Pediatr Surg Int 2021;37:1303–9. 10.1007/s00383-021-04939-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fonkalsrud EW, O’Neill JA, Jabaji Z, et al. Changing relationship of pediatric surgical workforce to patient demographics. Am J Surg 2014;207:275–80. 10.1016/j.amjsurg.2013.07.026 [DOI] [PubMed] [Google Scholar]
- 3.Concepcion T, Mohamed M, Dahir S, et al. Prevalence of pediatric surgical conditions across somaliland. JAMA Netw Open 2019;2:e186857. 10.1001/jamanetworkopen.2018.6857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hamad D, Yousef Y, Caminsky NG, et al. Defining the critical pediatric surgical workforce density for improving surgical outcomes: a global study. J Pediatr Surg 2020;55:493–512. 10.1016/j.jpedsurg.2019.11.001 [DOI] [PubMed] [Google Scholar]
- 5.Niconchuk JA, Newton MW. Global pediatric surgery and anesthesia inequities: how do we have a global effort? Curr Opin Anaesthesiol 2022;35:351–6. 10.1097/ACO.0000000000001122 [DOI] [PubMed] [Google Scholar]
- 6.Krishnaswami S, Nwomeh BC, Ameh EA. The pediatric surgery workforce in low- and middle-income countries: problems and priorities. Semin Pediatr Surg 2016;25:32–42. 10.1053/j.sempedsurg.2015.09.007 [DOI] [PubMed] [Google Scholar]
- 7.Magwesela FM, Rabiel H, Mung’ong’o CM. Pattern of congenital anomalies among pediatric surgical patients in a tertiary care hospital in Northern Tanzania. World J Pediatr Surg 2022;5:e000410. 10.1136/wjps-2021-000410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.TSd C, Piazi MD, CRLd S. Clinical-epidemiological profile of children and adolescents hospitalized in the pediatric surgery nurse in a reference hospital in Rio De Janeiro. Res Soc Dev 2022;11:e33411225645. 10.33448/rsd-v11i2.25645 [DOI] [Google Scholar]
- 9.de Jesus LE, Aguiar AS, de Campos M do S, et al. Needs and specialization for pediatric surgeons in Brazil. Rev Col Bras Cir 2009;36:356–61. 10.1590/s0100-69912009000400016 [DOI] [PubMed] [Google Scholar]
- 10.Rocha TAH, da Silva NC, Amaral PV, et al. Addressing geographic access barriers to emergency care services: a national ecologic study of hospitals in Brazil. Int J Equity Health 2017;16:149. 10.1186/s12939-017-0645-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rocha TAH, Vissoci J, Rocha N, et al. Towards defining the surgical workforce for children: a geospatial analysis in Brazil. BMJ Open 2020;10:e034253. 10.1136/bmjopen-2019-034253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Departamento de informática do SUS - DATASUS. Informações de saúde (TABNET). Brasil, Available: http://www2.datasus.gov.br/DATASUS/index.php?area=02 [Accessed Jun 2022]. [Google Scholar]
- 13.Scheffer ea M. Demografia Médica no brasil 2020. São paulo - SP: FMUSP, CFM, 2020. Available: https://www.fm.usp.br/fmusp/conteudo/DemografiaMedica2020_9DEZ.pdf [Accessed Jun 2022]. [Google Scholar]
- 14.Correa C, Mallarino C, Peña R, et al. Congenital malformations of pediatric surgical interest: prevalence, risk factors, and prenatal diagnosis between 2005 and 2012 in the capital city of a developing country. bogotá, colombia. J Pediatr Surg 2014;49:1099–103. 10.1016/j.jpedsurg.2014.03.001 [DOI] [PubMed] [Google Scholar]
- 15.Silvestri EF, Oliveira EJF, Chiedde M, et al. Epidemiological characteristics of live births with esophageal atresia in Sao Paulo state, Brazil, from 2005 to 2018. World Jnl Ped Surgery 2023;6:e000455. 10.1136/wjps-2022-000455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Toobaie A, Yousef Y, Balvardi S, et al. Incidence and prevalence of congenital anomalies in low- and middle-income countries: a systematic review. J Pediatr Surg 2019;54:1089–93. 10.1016/j.jpedsurg.2019.01.034 [DOI] [PubMed] [Google Scholar]
- 17.Zarante I, Franco L, López C, et al. Frecuencia de malformaciones congénitas: evaluación y pronóstico de 52.744 nacimientos en tres ciudades colombianas. Biomedica 2010;30:65. 10.7705/biomedica.v30i1.154 [DOI] [PubMed] [Google Scholar]
- 18.Parigi GB, Czauderna P, Rolle U, et al. European census on pediatric surgery. Eur J Pediatr Surg 2018;28:227–37. 10.1055/s-0037-1600524 [DOI] [PubMed] [Google Scholar]
- 19.Vissoci JRN, Ong CT, Andrade L de, et al. Disparities in surgical care for children across Brazil: use of geospatial analysis. PLoS One 2019;14:e0220959. 10.1371/journal.pone.0220959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abdullah F, Salazar JH, Gause CD, et al. Understanding the operative experience of the practicing pediatric surgeon: implications for training and maintaining competency. JAMA Surg 2016;151:735–41. 10.1001/jamasurg.2016.0261 [DOI] [PubMed] [Google Scholar]
- 21.Barnhart DC, Oldham KT. Regionalization of children’s surgery. Ann Surg 2016;263:1067–8. 10.1097/SLA.0000000000001721 [DOI] [PubMed] [Google Scholar]
- 22.Carlisle EM, Rowell EE. Ethical challenges in regionalization of pediatric surgical care. Curr Opin Pediatr 2019;31:414–7. 10.1097/MOP.0000000000000764 [DOI] [PubMed] [Google Scholar]
- 23.Rich BS, Silverberg JT, Fishbein J, et al. Subspecialization in pediatric surgery: results of a survey to the American pediatric surgical association. J Pediatr Surg 2020;55:2058–63. 10.1016/j.jpedsurg.2020.02.006 [DOI] [PubMed] [Google Scholar]
- 24.Surgery GIfCs . Optimal resources for children’s surgical care I. guidelines for different levels of care. 2019. Available: https://static-content.springer.com/esm/art%3A10.1007%2Fs00268-018-04888-7/MediaObjects/268_2018_4888_MOESM1_ESM.pdf [Accessed June 2023].
- 25.Goodman LF, St-Louis E, Yousef Y, et al. The global initiative for children’s surgery: optimal resources for improving care. Eur J Pediatr Surg 2018;28:51–9. 10.1055/s-0037-1604399 [DOI] [PubMed] [Google Scholar]
- 26.Pakarinen M, Bjørland K, Qvist N, et al. Centralized pediatric surgery in the Nordic countries: a role model for Europe? Eur J Pediatr Surg 2017;27:395–8. 10.1055/s-0037-1606635 [DOI] [PubMed] [Google Scholar]
- 27.Rolle U, Ure BM. European pediatric surgical association. Eur J Pediatr Surg 2021;31:1. 10.1055/s-0040-1722224 [DOI] [PubMed] [Google Scholar]
- 28.Ure B. Esophageal atresia, europe, and the future. J Pediatr Surg 2019;54:217–22. 10.1016/j.jpedsurg.2018.10.071 [DOI] [PubMed] [Google Scholar]
- 29.Ure BM, Bax NM. Pediatric surgery in the Netherlands. Eur J Pediatr Surg 2001;11:291–4. 10.1055/s-2001-18556 [DOI] [PubMed] [Google Scholar]
- 30.Stolar CJH, Workforce Committee American Pediatric Surgical Association . Best practice for infant surgery--a position statement from the american pediatric surgical association. J Pediatr Surg 2008;43:1585–6. 10.1016/j.jpedsurg.2008.06.001 [DOI] [PubMed] [Google Scholar]
- 31.Bezner SK, Bernstein IH, Oldham KT, et al. Pediatric surgeons’ attitudes toward regionalization of neonatal surgical care. J Pediatr Surg 2014;49:1475–9. 10.1016/j.jpedsurg.2014.03.002 [DOI] [PubMed] [Google Scholar]
- 32.Shetty S, Kennea N, Desai P, et al. Length of stay and cost analysis of neonates undergoing surgery at a tertiary neonatal unit in England. Ann R Coll Surg Engl 2016;98:56–60. 10.1308/rcsann.2016.0034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Superina R. The shrinking landscape of pediatric surgery: is less more? J Pediatr Surg 2018;53:868–74. 10.1016/j.jpedsurg.2018.02.004 [DOI] [PubMed] [Google Scholar]
- 34.Davenport M, De Ville de Goyet J, Stringer M, et al. Seamless management of biliary atresia in England and Wales (1999–2002). The Lancet 2004;363:1354–7. 10.1016/S0140-6736(04)16045-5 [DOI] [PubMed] [Google Scholar]
- 35.Davenport M, Ong E, Sharif K, et al. Biliary atresia in England and Wales: results of centralization and new benchmark. J Pediatr Surg 2011;46:1689–94. 10.1016/j.jpedsurg.2011.04.013 [DOI] [PubMed] [Google Scholar]
- 36.Langer JC, Gordon JS, Chen LE. Subspecialization within pediatric surgical groups in North America. J Pediatr Surg 2016;51:143–8. 10.1016/j.jpedsurg.2015.10.038 [DOI] [PubMed] [Google Scholar]
- 37.Lopyan NM, Perrone EE, Gadepalli SK, et al. Current status of subspecialization in pediatric surgery: a focus on fetal surgery. J Pediatr Surg 2022;57:610–5. 10.1016/j.jpedsurg.2021.05.008 [DOI] [PubMed] [Google Scholar]
- 38.Peña A, Elicevik M, Levitt MA. Reoperations in hirschsprung disease. J Pediatr Surg 2007;42:1008–13. 10.1016/j.jpedsurg.2007.01.035 [DOI] [PubMed] [Google Scholar]
- 39.Peña A, Grasshoff S, Levitt M. Reoperations in anorectal malformations. J Pediatr Surg 2007;42:318–25. 10.1016/j.jpedsurg.2006.10.034 [DOI] [PubMed] [Google Scholar]
- 40.Raval MV, Lautz TB, Browne M. Bile duct injuries during pediatric laparoscopic cholecystectomy: a national perspective. J Laparoendosc Adv Surg Tech A 2011;21:113–8. 10.1089/lap.2010.0425 [DOI] [PubMed] [Google Scholar]
- 41.Beasley SW. The challenges facing training in pediatric surgery worldwide. Front Pediatr 2013;1:24. 10.3389/fped.2013.00024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cummins CB, Bowen-Jallow KA, Tran S, et al. Education of pediatric surgery residents over time: examining 15 years of case logs. J Pediatr Surg 2021;56:85–98. 10.1016/j.jpedsurg.2020.09.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Esparaz JR, Carter SR, Anderson SA, et al. The diminishing experience in pediatric surgery for general surgery residents in the United States. J Pediatr Surg 2021;56:1219–21. 10.1016/j.jpedsurg.2021.03.042 [DOI] [PubMed] [Google Scholar]
- 44.Nakayama DK. Workforce issues in pediatric surgery. Am Surg 2017;83:660–5. [PubMed] [Google Scholar]
- 45.Bruns NE, Shah MA, Dorsey AN, et al. Pediatric surgery - a changing field: national trends in pediatric surgical practice. J Pediatr Surg 2016;51:1034–8. 10.1016/j.jpedsurg.2016.02.079 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available in a public, open access repository. Data are available in a public, open-access repository. All data used for this analysis were obtained from the open-access DATASUS system from the Brazilian Ministry of Health. Data can be obtained freely from: http://tabnet.datasus.gov.br/.