Abstract
Empathic accuracy, the ability to accurately understand others’ emotions, is typically viewed as beneficial for mental health. However, empathic accuracy may be problematic when a close relational partner is depressed because it promotes shared depression. Across two studies, we measured empathic accuracy using laboratory tasks that capture the ability to rate others’ emotional valence accurately over time: first, in a sample of 156 neurotypical married couples (Study 1; Total N=312), and then in a sample of 102 informal caregivers of individuals with dementia (Study 2). Across both studies, the association between empathic accuracy and depressive symptoms varied as a function of a partner’s level of depressive symptoms. Greater empathic accuracy was associated with (a) fewer depressive symptoms when a partner lacked depressive symptoms, but (b) more depressive symptoms when a partner had high levels of depressive symptoms. Accurately detecting changes in others’ emotional valence may underpin shared depressive symptoms.
Keywords: depression, empathy, contagion, dementia caregiving
Empathy, the ability to share and understand others emotions, helps us build and maintain social relationships (Eisenberg & Miller, 1987; Ickes, 1997). Empathy has been linked to better social connectedness and mental health, spurring large scale interventions aimed at enhancing empathic skills (Morelli et al., 2017; Weisz & Zaki, 2017; Weisz & Zaki, 2018). However, a growing body of research has begun to highlight potential adverse consequences of empathy for mental health. Empathizing can be effortful and costly, sometimes leading to heightened stress and negative affect for the empathizer (Brown, West, et al., 2020; Cameron et al., 2019). Consistent with this, mental health problems have been found to be more common among physicians and caregivers who regularly empathize with others’ suffering (Gleichgerrcht & Decety, 2011; Hua et al., 2021). Such findings contribute to an ongoing debate over whether empathy is beneficial or harmful (Bloom, 2017; Zaki, 2017). Rather than viewing this as an “either-or” issue, the current studies takes a more nuanced approach, and heed recent calls in the literature to understand when certain aspects of empathy are beneficial and when they are harmful for mental health (Hittner & Haase, 2021; Weisz & Cikara, 2021).
In daily life, empathy occurs most commonly with close relational partners, and in response to others’ positive emotions (Depow et al., 2020). Empathic accuracy is a key component of empathy in close relationships, and refers to the ability to accurately understand what another person feels. Empathic accuracy is generally thought to improve relationship satisfaction and promote mental health and well-being (Ickes, 1997; Sened et al., 2017). However, when a close relational partner has high levels of depressed or negative affect, accurately recognizing that partner’s depressed emotions (i.e., empathic accuracy) may be detrimental for one’s own mental health insofar as accurate recognition leads to a shared or common experience between partners. The current studies examine if empathic accuracy is associated with better mental health when a partner has fewer depressive symptoms, but worse mental health when a partner has more depressive symptoms.
Empathic Accuracy as a Risk Factor for Depression Contagion
Measures of empathic accuracy are typically based on performance and capture the degree of agreement between: (a) what a perceiver thinks a person is feeling, and (b) what that person actually reports feeling (Ickes & Hodges, 2013). These performance or skill-based measures of empathic accuracy do not usually correspond to self-reported empathic tendencies (e.g., empathic concern, the tendency to have concerned feelings for others, or perspective taking, the tendency to take others’ point of view; Levenson & Ruef, 1992; Zaki et al., 2008). To put it simply, empathically accurate perceivers are those who can read others’ emotions correctly, whether it is their close partner or a stranger (Ickes & Hodges, 2013).
Empathic accuracy is sometimes categorized as a cognitive or “cold” form of empathy because it results from an accurate cognitive processing or understanding of another person’s emotions (Hua et al., 2021). However, a number of studies suggest that empathic accuracy in fact relies on neural networks critical for emotional or “hot” forms of empathy like affect contagion and embodying others’ emotional states (Brown, Hua, et al., 2020; Zaki, Weber, et al., 2009). Empathic accuracy may lead to shared experience and shared physiology, especially in close relationships or when empathic concern is high (Brown, West, et al., 2020; Levenson & Ruef, 1992, 1997). Several theories of empathy argue that an accurate understanding of others’ emotions may be necessary to engender shared experience and physiology (Dezecache et al., 2015; Hatfield et al., 1993). Taken together, past theory and research suggest that individuals high in empathic accuracy may be especially likely to recognize and be influenced by the distress of their close relational partners.
Similar themes are found in interpersonal theories of depression, which posit that interacting with a depressed person is a risk factor for developing depression (Coyne, 1976; Hames et al., 2013). Indeed, research and meta-analyses demonstrate that depressive symptoms can be “contagious” and spread across individuals (Joiner & Katz, 1999). A number of cognitive and behavioral mechanisms have been proposed to explain shared depression in dyads (e.g., adopting a partner’s cognitive style; Haeffel & Hames, 2014; Paukert et al., 2008). Accurately recognizing a partner’s depression could precipitate and promote one’s own depression in a variety of ways, for example, via feelings of guilt or failure that one cannot resolve a partner’s depressive symptoms. Yet, no studies to our knowledge have examined whether individuals with greater empathic accuracy are more likely to share their partner’s level of depressive symptoms.
Moreover, the specific kinds of depressive symptoms that could spread to individuals with high empathic accuracy remain unclear. Depressed affect is a central emotional feature of depression that seems likely to spread to a partner who has high empathic accuracy. But depression can also involve other symptoms that are less closely tied to negative emotion (e.g., somatic symptoms, interpersonal problems, low positive affect; Hays et al., 1998). It is unclear whether these other symptoms of depression can spread within dyads to the extent that depressed affect can (Joiner & Katz, 1999). For example, in the context of a partner’s depressive symptoms, empathic accuracy may promote heightened depressed affect, but not heightened somatic symptoms. The current study will determine whether specific kinds of depressive symptoms spread to individuals with high empathic accuracy.
Similar to depression, anxiety is characterized by negative affect that may spread between individuals (Gorman, 1996). Relative to the number of studies on shared depression, fewer studies have focused on shared anxiety (Joiner & Katz, 1999). There are hints in the literature that depression is more likely than anxiety to be shared between partners. For example, Joiner (1994) found that depression, but not anxiety, spreads between college roommates. However, in laboratory settings, greater subjective emotional empathy has been linked to more vicarious distress and anxiety within dyads (Dimitroff et al., 2017; Shu et al., 2017). The current research will examine both anxiety and depressive symptoms, and determine whether individuals higher in empathic accuracy are more likely to mirror their close relational partner’s anxiety and depressive symptoms.
A Dyadic Context Ripe for Shared Depression: Dementia Caregiving
Mental health problems such as depression and anxiety become less common as adults age, but can emerge in mid- to late-life as a result of neurobiological changes or stressful circumstances (Fiske et al., 2009; Schuurmans & Van Balkom, 2011). Depression and anxiety symptoms commonly arise as an early indicator of various neurodegenerative diseases that profoundly impair cognitive, emotional, and motor functioning (e.g., Alzheimer’s disease [AD], frontotemporal dementia [FTD]; Lyketsos et al., 2002; Woolley et al., 2011). Close relational partners of individuals with neurodegenerative disease evidence increased rates of depression and anxiety compared to same-aged non-caregiving adults (Brodaty & Donkin, 2009; Coope et al., 1995; Cuijpers, 2005).
Caregivers’ mental health can be profoundly influenced by impairments in the care recipients’ emotional functioning (Brown et al., 2018; Brown, Wells, et al., 2020; Chen et al., 2017; Otero & Levenson, 2017). Research also highlights emotional qualities within caregivers that indicate elevated risk for mental health problems, such as poor emotion regulation (Wells et al., 2020) and high levels of emotional empathy (Hua et al., 2021). Both self-reported emotional empathy and greater self-reported negative affect in response to images of suffering individuals have been linked to poor mental health in caregivers (Hua et al., 2021; Jütten et al., 2019; Lee et al., 2001). However, past research has failed to uncover direct associations between caregiver empathic accuracy and caregiver mental health (Hua et al., 2021).
We suspect the lack of direct associations between caregiver empathic accuracy and caregiver mental health may occur because this association varies depending on characteristics of the care recipient. When an individual with dementia is depressed or anxious, possessing greater empathic accuracy may be detrimental for caregivers because accurately recognizing negative affect in their close relational partner may lead to a shared experience of depression and anxiety. However, when an individual with dementia is not depressed or anxious, caregivers’ empathic accuracy may be beneficial for their mental health because it provides peace of mind that their close relational partner is not suffering with depressed affect. Thus, the answer to the question of whether caregivers’ empathic accuracy is good or bad for their mental health may depend upon the care recipient’s levels of depression and anxiety.
The Current Studies
The current studies utilize two dyadic datasets to examine whether a close relational partner’s depression and anxiety symptoms impact the associations between empathic accuracy and mental health. The first study included neurotypical heterosexual middle-aged and elderly married couples, and the second study included middle-aged and elderly dementia care recipient-caregiver dyads. In both studies, empathic accuracy was measured using laboratory tasks in which participants continuously rate the valence of others’ emotions using a rating dial (Ruef & Levenson, 2007). In Study 1, empathic accuracy was computed for both husbands and wives based on each participant’s ratings of their spouse’s affect during a naturalistic conversation involving a relationship conflict. Given that empathic accuracy can be influenced by factors related to the target (i.e., the person whose affect is being rated; Zaki et al., 2008), in Study 2, we had caregivers rate standardized films of unfamiliar targets expressing emotions during conflict. This enabled us to better capture trait-like individual differences in the ability to accurately identify others’ emotions. It also enabled us to avoid having individuals with dementia provide self-reports of affect, which can be unreliable due to their cognitive impairments. Thus, we used two different kinds of targets for assessing empathic accuracy, spouses (in Study 1) and strangers (in Study 2).
The two studies also differed in the method used for measuring depressive and anxiety symptoms. In Study 1, husbands and wives independently reported on their own symptoms. In Study 2, caregivers reported on their own depressive symptoms and anxiety, and a standardized clinical interview with caregivers was used to assess care recipients’ level of depressive and anxiety symptoms. These kinds of clinical interviews are a gold standard method for assessing psychopathology for individuals with dementia, who often lack the capacity or insight to report on their own psychiatric symptoms (Cummings, 1997).
For both studies, we hypothesized that a partner’s level of depressive symptoms would moderate the association between empathic accuracy and depressive symptoms in the empathizer. Specifically, we predicted that greater empathic accuracy would be associated with better mental health when a partner lacks depressive symptoms, whereas greater empathic accuracy would be associated with poorer mental health when a partner has high levels of depressive symptoms. We hypothesized a similar relationship for anxiety (i.e., that a partner’s level of anxiety symptoms would moderate the association between empathic accuracy and anxiety).
Study 1 Method
Participants were drawn from a longitudinal study of 156 heterosexual middle-aged and elderly married couples in long-term marriages (Mean length of marriage= 30.59, Mean age= 52.95). Participants were primarily White (86%; 7% Black; 2% Hispanic; 4% Asian; 1% other), relatively well-off socioeconomically, resided in California, and had children (95% had at least one child). See Table 1 for additional demographics and Supplemental Content for sampling and recruitment details and a list of prior publications using this dataset. The University of California, Berkeley Committee for the Protection of Human Subjects approved all procedures used in this research.
Table 1. Additional demographic and clinical characteristics.
Means and standard deviations provided, unless otherwise noted.
| Study 1 | ||
| Husbands | Wives | |
| Age | 53.61(10.10) | 52.29(10.01) |
| Years of Education | 16.51(2.78) | 15.23(2.47) |
| Depression (SCL-90) | 0.22(0.30) | 0.35(0.45) |
| Anxiety (SCL-90) | 0.11(0.23) | 0.21(0.37) |
| Empathic Accuracy | 0.26(0.26) | 0.25(.26) |
| Study 2 | ||
| Care recipients | Caregivers | |
| Age | 64.53 (10.12) | 63.3 (8.82) |
| Gender (% Female) | 41.2 | 57.8 |
| Diagnosis (n=) | ||
| FTD | 39 | - |
| AD | 18 | - |
| Motor | 25 | - |
| MCI or mixed | 20 | - |
| Clinical Dementia Severity | 3.93 (2.51) | - |
| iADLs | 2.87 (.78) | |
| Depression (NPI) | - | 1.92 (2.0) |
| Anxiety (BAI) | - | 6.30 (6.71) |
| Depression (CESD) | - | 12.45 (8.54) |
| Empathic Accuracy | - | 0.45(0.33) |
Notes. SCL-90 = Symptom Checklist- 90; iADLs = Instrumental activities of daily living; NPI = Neuropsychiatric Inventory; BAI = Beck Anxiety Inventory; CESD = Center for Epidemiological Studies Depression Scale.
Procedure
Couples completed questionnaires and a laboratory session based on a well-validated protocol for studying emotion during dyadic interactions (Levenson & Gottman, 1983). Data were collected at four time points over the course of 20 years. The current analyses are based on data collected at the first time point (from 1989–1990) in which couples visited the laboratory and engaged in a 15-minute conversation on a topic of ongoing conflict in their marriage (Levenson et al., 1994).
Empathic Accuracy
Several days after the laboratory session, participants returned to the laboratory and individually watched a video-recording of their conversation twice, first rating their own emotional valence during the interaction, and then rating their partner’s emotional valence during the interaction. To rate emotions, participants used a dial that traversed a 180° path, with the dial pointer moving over a 9-point scale anchored by the legends “extremely negative” (1) and “extremely positive” (9), with a line labeled “neutral” in the middle (5).1 Spouses were instructed to change the position of the dial as often as necessary so that it always represented how either they or their partner felt during the interaction (Ruef & Levenson, 2007). This procedure for obtaining continuous self-reports of affect is well-validated (Gottman & Levenson, 1985). The rating dial generated a position-dependent electrical voltage that was sampled by a computer every 3 msec and averaged every second. For each spouse, this resulted in two second-by-second time-series reflecting (a) their affective valence during the conversation, and (b) their perception of their partner’s affective valence during the interaction. For each spouse, empathic accuracy was computed as the correlation between their rating of their partner’s affect and their partner’s self-rated affect during the interaction2. Higher scores indicate greater accuracy.
Depressive Symptoms and Anxiety Symptoms
Participants completed the Symptom Checklist-90 (SCL-90; Derogatis et al., 1973; Derogatis & Cleary, 1977), including the 13-item depression subscale (α = .85) and the 9-item anxiety subscale (α = .80). Participants rated the extent to which they were bothered by each item using a scale of 0 (not at all) to 4 (extremely). Items within subscales were averaged, with higher scores indicating greater depression or anxiety.
Analytic Approach
Data were analyzed using the structural equation modeling (SEM) framework with the lavaan package in R Version 4.0.4 (Rosseel, 2012).
To evaluate model fit, we inspected the χ2 test of model fit and the standardized root mean squared residual (SRMR) as measures of absolute fit, as well as the comparative fit index (CFI) as a measure of incremental fit, following established guidelines (Hu & Bentler, 1999). The following values indicated adequate model fit: nonsignificant χ2 values (ps > 0.05), CFI values greater than 0.95, and SRMR values less than .08.
We constructed a multi-group structural equation model (MG-SEM) estimated using maximum likelihood, with gender as the grouping variable. To test our hypothesis that a partner’s level of depressive symptoms would moderate the association between one’s own empathic accuracy and depressive symptoms, we regressed participants’ depressive symptoms on the participant’s empathic accuracy, his/her partner’s depressive symptoms, and the product between the two in order to examine their interactive effect. Similarly, to test our hypothesis that a partner’s level of anxiety symptoms would moderate the association between one’s own empathic accuracy and anxiety symptoms, we re-ran the same model replacing depressive symptoms with anxiety symptoms.
For each model, we set equality constraints on slopes for husbands and wives and then compared this model with one in which slopes for husbands and wives were freely estimated. We compared the fit of these two models using a likelihood ratio test. If the two models did not differ significantly, we chose the more parsimonious model in which the slopes were constrained to be equal across groups. For models in which the significant hypothesized interaction of empathic accuracy X partner symptom level emerged, simple slopes analysis was conducted to understand and describe the nature of the interaction.3 We examined simple slopes at plus and minus one standard deviation above and below the mean of each predictor variable. Because means and variances were allowed to vary for husbands and wives, we report four unique simple slopes for husbands and wives, including slopes at: (a) higher levels of partner depressive symptoms, (b) lower levels of partner depressive symptoms, (c) higher levels of empathic accuracy, and (d) lower levels of empathic accuracy. For significant interaction effects, we also conducted additional sensitivity analyses to examine whether the interaction effects were robust to the inclusion of covariates, including age, education, length of marriage, and partner expressivity captured via behavioral coding (See Supplemental Content for details). For all models, we allowed the means and variances of predictors to be freely estimated across groups, and allowed predictors to correlate freely with one another.
Sample size was pre-determined because the data are archival. De-identified data and syntax used for analyses are available through the Open Science Framework (OSF) at https://osf.io/35un9/?view_only=39c5b572a7524de78d03ca874513e74c.
Study 1 Results
Correlations among key study variables are presented in Table 2. The MG-SEM with equality constraints on the slopes that examined whether the association between empathic accuracy and depressive symptoms is moderated by a partner’s depressive symptoms indicated excellent fit, χ2(3) = 0.831; p = .842; CFI = 1.01; SRMR = .013. Partner depressive symptoms significantly moderated the association between empathic accuracy and depressive symptoms (B = .290, SE = .121, p = .016), with no main effects of empathic accuracy (B = −.076, SE = .100, p = .446) nor partner depressive symptoms (B = .074, SE = .049, p = .133). Model fit did not improve by removing equality constraints between husbands and wives (χ2(3) = 0.83, p = .84), therefore we retained these constraints in the model. The interaction between empathic accuracy and partner depressive symptoms remained significant when additional covariates including age, education, length of marriage, and partner emotional expressivity were included in the model (B = .30, SE = .12, p = .012; See Supplemental Content for details). See Figure 1 for a depiction of the interactive effects, and Supplemental Figure 1 for a depiction of the same interactive effects with an alternative orientation of the independent variables.
Table 2.
Intercorrelations between primary variables of interest.
| Study 1 | ||||||
| 1 | 2 | 3 | 4 | 5 | 6 | |
|
| ||||||
| 1. Husbands’ Empathic Accuracy | 1.00 | |||||
| 2. Wives’ Empathic Accuracy | .07 | 1.00 | ||||
| 3. Husbands’ Depressive Symptoms (SCL-90) | .08 | −.04 | 1.00 | |||
| 4. Wives’ Depressive Symptoms (SCL-90) | −.23** | −.05 | .11 | 1.00 | ||
| 5. Husbands’ Anxiety (SCL-90) | .13 | .01 | .66** | .11 | 1.00 | |
| 6. Wives’ Anxiety (SCL-90) | −.15+ | −.01 | −.04 | .69** | .04 | 1.00 |
|
| ||||||
| Study 2 | ||||||
| 1 | 2 | 3 | 4 | 5 | ||
|
| ||||||
| 1. Caregivers’ Empathic Accuracy | 1.00 | |||||
| 2. Caregivers’ Depressive Symptoms (CESD) | .08 | 1.00 | ||||
| 3. Care Recipients’ Depressive Symptoms (NPI) | .06 | .19* | 1.00 | |||
| 4. Caregivers’ Anxiety Symptoms (BAI) | .04 | .68** | .22* | 1.00 | ||
| 5. Care Recipients’ Anxiety Symptoms (NPI) | .06 | .07 | .28** | .14 | 1.00 | |
Notes.
p<.1
p < .05
p < .01
SCL-90 = Symptom Checklist- 90; iADLs = Instrumental activities of daily living; NPI = Neuropsychiatric Inventory; BAI = Beck Anxiety Inventory; CESD = Center for Epidemiological Studies Depression Scale.
Figure 1.
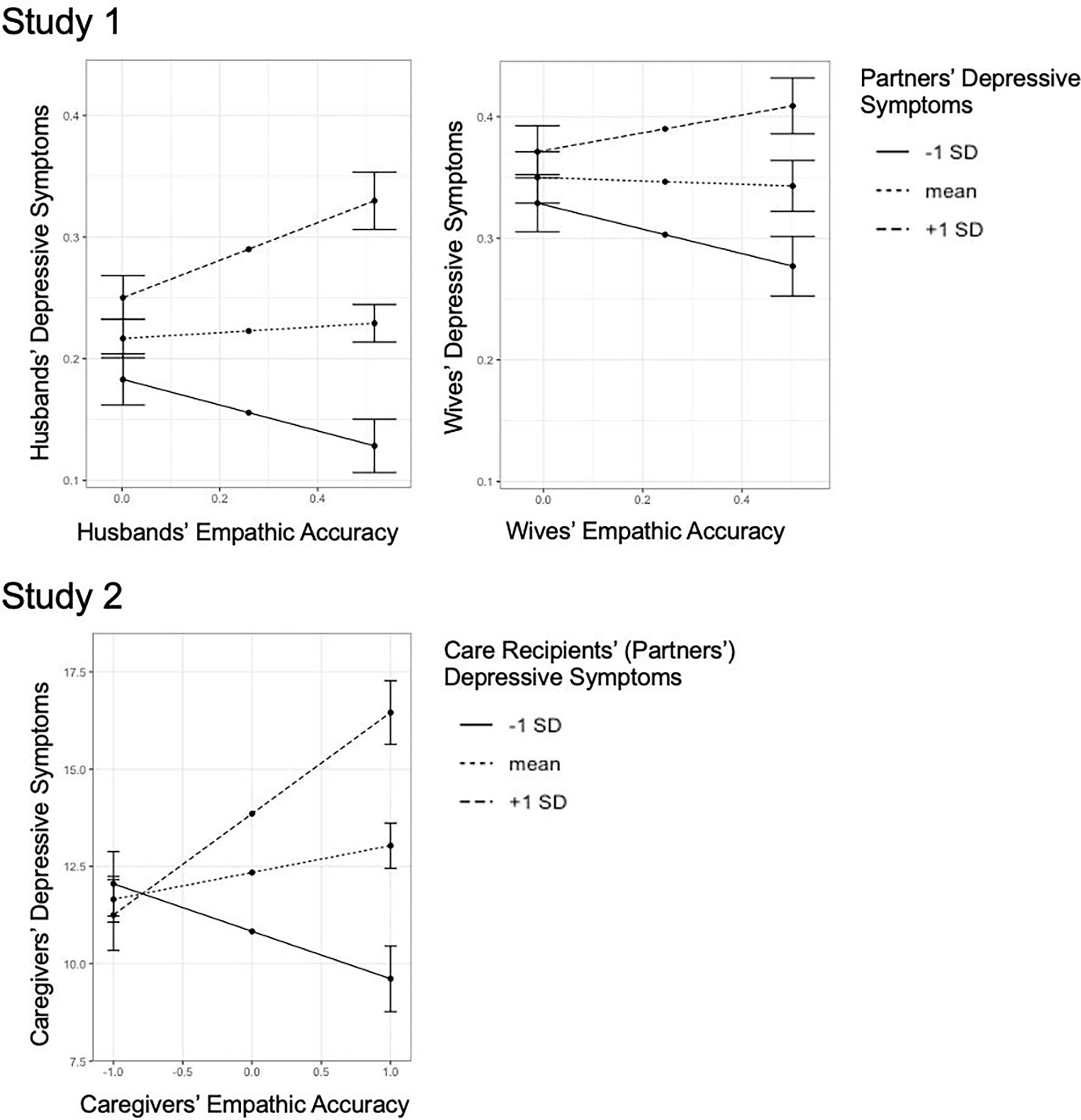
Note. A close relational partner’s level of depressive symptoms moderates the association between empathic accuracy and depressive symptoms in heterosexual married couples (Study 1) and in a sample of informal caregivers of close relational partners with dementia (Study 2).
An examination of simple slopes to understand the nature of the significant interaction revealed that when a partner had relatively high levels of depressive symptoms (1 SD above the mean), the slope of empathic accuracy on depressive symptoms was positive but non-significant (husbands: B = .16, SE = .09, p = .082; wives: B = .07, SE = .08, p = .36); however, when a partner had relatively low levels of depressive symptoms (1 SD below the mean), the effect of empathic accuracy on depressive symptoms was negative but non-significant (husbands: B = −.11, SE = .11, p = .323; wives: B = −.10, SE = .11, p = .343). Thus, the significant difference between slopes (the significant interaction effect) is characterized by a more positive association between empathic accuracy and depressive symptoms when a partner had relatively high levels of depressive symptoms, in contrast to a more negative association between empathic accuracy and depressive symptoms when a partner had relatively low levels of depressive symptoms. An examination of simple slopes from the same interaction at higher and lower levels of empathic accuracy revealed that, for individuals with relatively high empathic accuracy (1 SD above the mean), the association between husbands’ and wives’ depressive symptoms was significant and positive (husbands: B = .22, SE = .07, p = .002; wives: B = .22, SE = .07, p = .002). In contrast, for individuals with relatively low empathic accuracy (1 SD below the mean), the association between husbands’ and wives’ depressive symptoms was non-significant and near zero (husbands: B = .08, SE = .05, p = .126; wives: B = .07, SE = .05, p = .154). Thus, at high levels of empathic accuracy, individuals had higher levels of depressive symptoms if their spouse had higher levels of depressive symptoms, but lower levels of depressive symptoms if their spouse had lower levels of depressive symptoms. In other words, husbands and wives only shared their partner’s level of depressive symptoms when they were high on empathic accuracy.4
The MG-SEM to examine whether the association between empathic accuracy and anxiety was moderated by a partner’s anxiety indicated excellent fit when the slopes were constrained to be equal, χ2(3) = 0.486; p = .922; CFI = 1.0; SRMR = .011. Model fit did not improve by removing equality constraints between husbands and wives (χ2 (3) = 0.49, p = .92). No evidence for the hypothesized moderating role of a partner’s anxiety in the association between empathic accuracy and anxiety was found (B = .170, SE = .119, p = .152). Neither empathic accuracy (B = .031, SE = .073, p = .67) nor partner anxiety symptoms (B = .020, SE = .049, p = .688) were associated with anxiety.
Preliminary Discussion
Results of Study 1 indicate that individuals’ depressive symptoms were predicted by the interaction between their own empathic accuracy and their partner’s level of depressive symptoms. Individuals high in empathic accuracy report greater depressive symptoms when their partner was depressed, but fewer depressive symptoms when their partner was lower in depressive symptoms. These results suggest that the degree to which high empathic accuracy is beneficial or harmful in terms of depressive symptoms depends on one’s partner’s depressive symptoms. Importantly, we did not find similar results for anxiety. That is, the association between empathic accuracy and anxiety was not moderated by a partner’s level of anxiety.
Taken at face value, these results suggest that depression contagion only occurs in the context of high empathic accuracy. However, participants in Study 1 rated the emotions of their own spouse as a measure of empathic accuracy. Performance on measures of empathic accuracy can be influenced by the expressivity of the target (i.e., the person whose emotions are being rated; Zaki, Bolger, et al., 2009) and by the amount of exposure to the target (Colvin et al., 1997). Although results remained significant after controlling for length of marriage and partner emotional expressivity, Study 1 leaves open the possibility that some other feature of the spouse or the relationship may be mechanisms driving the observed interaction (promoting both empathic accuracy and shared depressive symptoms). Therefore, in a second study (Study 2), we assessed the robustness of the interactive effects observed in Study 1 by measuring empathic accuracy using a standardized laboratory task where all participants rate videos of the same targets, such that individual differences in empathic accuracy are not influenced by factors related to the spouse/target.
Additionally, in Study 2 we focused on a clinical population of dementia care recipient-caregiver dyads for whom depressive symptoms are more common (Brodaty & Donkin, 2009). We measured a variety of factors previously linked to caregiver depression in the literature (e.g., care recipient diagnosis, disease severity, and functional impairments). Moreover, we utilized a depression scale that demonstrates adequate within-scale structural validity to capture four distinct symptom clusters of depression in older adults: depressed affect, low positive affect, somatic complaints, and interpersonal problems (Hays et al., 1998). This enabled us to explore which of these symptom clusters of depression were elevated for caregivers high in empathic accuracy when their care recipient had greater depression.
Study 2 Materials and Methods
Participants
Informal caregivers (N = 102)5 of close relational partners with dementia were recruited from the Memory and Aging Center at the University of California, San Francisco (UCSF) where the care recipients underwent a full diagnostic evaluation, including neurological, neuropsychological, and neuroimaging assessment. On average, caregivers were 63.3 years old and care recipients were 64.53 years old. Most caregivers were spouses of the care recipients (89.9%), but the sample also included unmarried partners (2%), family members (4.9%), and friends (3%). Approximately 60% of caregivers identified as female. Participants were primarily White (82.1%; 4.4% Latino; 2.9% Black; 3% Native American, 1.4% Middle Eastern, 1.5% Southeast Asian). Caregivers and their care recipients resided together within the United States. The sample of 102 care recipients included: (a) 39 diagnosed with frontotemporal dementia (FTD); (b) 18 diagnosed with Alzheimer’s disease (AD), which predominantly affects memory functioning; (c) 25 with diagnoses that were characterized by motor symptoms (Motor; e.g., corticobasal syndrome, progressive supranuclear palsy); and (d) 20 individuals diagnosed with developing dementia, mild cognitive impairment, or mixed symptoms (Other). Diagnoses were based on consensus criteria for these disorders (Armstrong et al., 2013; Budka et al., 1995; Gorno-Tempini et al., 2011; Litvan et al., 1996; McKeith, 2004; McKhann et al., 2011; Rascovsky et al., 2011). For additional demographic details, see Table 1.
Procedure
Caregivers consented to participate in an assessment of socioemotional functioning at the Berkeley Psychophysiology Laboratory at the University of California, Berkeley that consisted of a number of tasks designed to measure emotional functioning (Levenson et al., 2008), including the empathic accuracy task described below. Caregivers completed clinical interviews and questionnaires online and at UCSF within 4 months of completing the empathic accuracy task at UC Berkeley. All procedures were approved by the Committee for the Protection of Human Subjects at the University of California, Berkeley.
Caregivers’ Empathic Accuracy
Caregivers watched videos of two different heterosexual married couples having conversations about an area of disagreement in their relationship. For each video, participants were asked to rate the emotions of a target individual who was highlighted with a green dot above his or her head. To rate emotions, participants used a dial similar to the one described in Study 1, which traversed a 180° path, with the dial pointer moving over a 9-point scale ranging from “very bad” at the far left (shown with a schematic frowning face), with “neutral” in the middle, and “very good” (shown with a schematic smiling face) at the far right. Caregivers were instructed to change the position of the dial as often as necessary so that it always represented how the target person in the video felt. Each video lasted 240 seconds. The videos and target’s emotional ratings were drawn from Study 1 data, and have been used in earlier studies on emotion recognition (Sze et al., 2012). In line with past studies on empathic accuracy, we ensured that the target individual: (a) experienced sufficient variability and range of emotion (i.e., rated him or herself as feeling positive or negative); and (b) rated his or her own emotion in a way that was reasonable and not unduly idiosyncratic (determined by comparing the target’s own ratings with those of a panel of four expert raters; Levenson & Ruef, 1992; Soto & Levenson, 2009).
As in Study 1, accuracy on this task was calculated using time-series correlations to determine the agreement between: (a) the caregiver’s moment-to-moment ratings of the target person’s emotions, and (b) the target’s ratings of his or her own emotions. Accuracy scores were reliable across the videos (α = .71), thus we averaged the correlation coefficients from each video to derive a single measure of each caregiver’s empathic accuracy, with higher scores reflecting greater accuracy.
Caregiver Depressive Symptoms and Anxiety Symptoms
Caregivers completed the Center for Epidemiologic Studies Depression (CESD; Radloff, 1977), a 20-item self-report assessment of depressive symptoms (α = .88). The presence of symptoms in the past week was rated on a 4-point scale ranging from “not at all” to “a lot”. Scores were reversed where appropriate and summed, with higher scores indicating greater depression.6 Additionally, to examine different symptom clusters of depression, we computed four subscales by summing item responses related specifically to: (a) depressed affect [α = .81], (b) low positive affect [α = .76], (c) somatic complaints [α = .69], and (d) interpersonal problems [α = .76]). These clusters and the associated subscales are based on prior research on social determinates of depression in older adults (Hays et al., 1998).
Caregivers also completed the Beck Anxiety Inventory (BAI; Steer & Beck, 1997), a 20-item self-report assessment of anxiety symptoms (α = .87). Caregivers reflected on the past month and rated themselves on a scale from 0 (“not at all”) to 3 (“a lot”) for 21 items (e.g., “Unable to relax”). Scores were summed, with higher scores indicating greater anxiety.
Care Recipients’ Depressive Symptoms and Anxiety Symptoms
At UCSF, care recipients’ neuropsychiatric symptoms were assessed via a clinical interview conducted by a nurse with the caregiver using the Neuropsychiatric Inventory, a well-validated measure of care recipients’ neuropsychiatric symptoms, which includes subscales focused on the domains of depression and anxiety (Cummings, 1997). For each domain, an interviewer probed for the presence of a variety of symptoms (e.g., feelings of sadness, low spirits, burdening social partners). If symptoms were present, their frequency and severity were rated. Frequency scores ranged from 1 (rarely) to 4 (very often) and severity scores ranged from 1 (mild) to 3 (severe). Frequency and severity scores were multiplied to create a total score in each domain, with higher scores indicating greater symptomatology.
Care Recipients’ Disease Severity
At UCSF, the Clinical Dementia Rating Scale (CDR) was completed by having clinicians administer a semi-structured interview to caregivers (Morris, 1997). The CDR assesses functional performance in six domains: (a) memory, (b) orientation, (c) judgement and problem-solving, (d) community affairs, (e) home and hobbies, and (f) personal care. Scores in each domain ranged from 0 (none) to 3 (severe) (α = .82) and were summed to create a composite score, ranging from 0 to 18, with higher scores indicating greater disease severity.
Care Recipients’ Functional Impairments
Functional impairments were measured using an adapted version of the Lawton-Brody Instrumental activities of daily living (iADL) Scale (Lawton & Brody, 1969), in which caregivers reported on the extent to which care recipients are able to perform each of 8 activities (e.g., food preparation, laundry, managing finances, α = .88). Specifically, for each activity, caregivers were asked to choose an item that most closely reflected their care recipient’s highest level of functioning (e.g., for laundry: a] does laundry completely, b] launders small items…, c] all laundry must be done by others). Responses were summed, with lower scores reflecting poorer performance of iADLs.
Analytic Approach
To test our first hypothesis that care recipient depressive symptoms would moderate the association between caregiver empathic accuracy and caregiver depressive symptoms, we used linear regression. We regressed caregiver depressive symptoms onto caregiver empathic accuracy, care recipient depressive symptoms, and the product between the two in order to examine their interactive effect. To test our second hypothesis that care recipient anxiety symptoms would moderate the association between caregiver empathic accuracy and caregiver anxiety symptoms, we repeated the aforementioned model, replacing depressive symptoms with anxiety symptoms.
For all models in which the significant hypothesized interactions emerged, in order to understand and describe the nature of the interaction, we examined simple slopes at one standard deviation above and below the mean for each predictor variable. Thus, for the significant interaction, we report four simple slopes at: (a) higher levels of care recipient depressive symptoms, (b) lower levels of care recipient depressive symptoms, (c) higher levels of caregiver empathic accuracy, and (d) lower levels of caregiver empathic accuracy. We also conducted additional analyses to examine whether the interaction effects were robust to the inclusion of covariates previously linked to caregiver depression in the literature, including caregiver age and sex, and care recipient diagnosis, disease severity, and functional impairments.
Additionally, we conducted a series of 4 linear regressions to explore whether the interaction between caregiver empathic accuracy and care recipient depressive symptoms predicted each of the four symptom clusters of depression on the CESD (Hays et al., 1998): (a) depressed affect, (b) low positive affect, (c) somatic complaints, and (d) interpersonal problems.
Study 2 Results
Correlations among key study variables are presented in Table 2. In line with our first hypothesis, regression analysis revealed that the association between caregiver empathic accuracy and caregiver depressive symptoms was moderated by care recipient depressive symptoms (significant empathic accuracy by care recipient depressive symptoms interaction) (β = .22, t(98) = 2.05, p = .043), with no main effect of caregiver empathic accuracy (β = .08, t(98) = 0.84, p = .41) nor care recipient depressive symptoms (β = .18, t(98) = 1.82, p = 072). The interaction between care recipient depressive symptoms and caregiver empathic accuracy remained significant after controlling for a variety of factors relevant to caregiver depressive symptoms (i.e., caregiver age and gender, and care recipients’ diagnosis, disease severity, and functional impairments; β = .25, t(86) = 2.42, p = .017).7 See Figure 1 for a depiction of the interactive effect, and Supplemental Figure 1 for an alternative orientation of this effect.
Simple slopes at higher and lower levels of care recipient depressive symptoms revealed that, when a care recipient had relatively high levels of depressive symptoms (1 SD above the mean), the effect of caregiver empathic accuracy on caregiver depressive symptoms was positive and significant (β = .31, t(98) = 2.03, p = .045). However, when a care recipient was relatively low in depressive symptoms (1 SD below the mean), the effect of caregiver empathic accuracy on caregiver depressive symptoms was negative and non-significant (β = −.14, t(98) = −1.00, p = .32). Thus, the significant difference between slopes (the significant interaction effect) was characterized by a more positive association between caregivers’ empathic accuracy and depressive symptoms when care recipients had relatively high levels of depressive symptoms, in contrast to a more negative association between caregivers’ empathic accuracy and depressive symptoms when care recipients had relatively low levels of depressive symptoms. Examining simple slopes from the same interaction at higher and lower levels of empathic accuracy revealed that for caregivers relatively high on empathic accuracy (1 SD above the mean), the association between care recipients’ depressive symptoms and caregivers’ depressive symptoms was significant and positive (β = .40, t(98) = 2.86, p = .005). In contrast, for caregivers relatively low on empathic accuracy (1 SD below the mean), the association between care recipients’ depressive symptoms and caregivers’ depressive symptoms was non-significant and near zero (β = −.04, t(98) = −0.31, p = .76). Thus, when a caregiver had relatively high levels of empathic accuracy, the caregiver had higher levels of depressive symptoms if their care recipient had higher levels of depressive symptoms, and lower levels of depressive symptoms if their care recipient had lower depressive symptoms. In other words, caregivers only shared their care recipient’s level of depressive symptoms when caregivers were high on empathic accuracy.8
Examining specific symptom clusters of caregiver depression (i.e., depressed affect, interpersonal problems, low positive affect, and somatic symptoms), we found that caregiver empathic accuracy significantly moderated the association between care recipient depressive symptoms and caregiver depressed affect (β = .24, t(98) = 2.20, p = .030). Caregiver empathic accuracy also significantly moderated the association between care recipient depressive symptom and caregiver interpersonal problems (β = .23, t(97) = 2.30, p = .042). The pattern of simple slopes for both of these significant interactions were similar to those observed for the interaction with caregivers’ overall depressive symptoms. In contrast, empathic accuracy did not significantly moderate the association between care recipient depressive symptoms and caregiver low positive affect, β = .14, t(95) = 1.28, p = .20. Similarly, empathic accuracy did not significantly moderate the association between care recipient depressive symptoms and caregiver somatic symptoms, β = .15, t(98) = 1.37, p = .175).
Contrary to our second hypothesis, the association between caregiver empathic accuracy and caregiver anxiety was not significantly moderated by care recipient anxiety (β = .07, t(98) = 0.64, p = .53). In this model, neither the main effect of care recipient anxiety (β = .14, t(98) = 1.33, p = .19) nor the main effect of caregiver empathic accuracy were significant (β = .03, t(98) = 0.33, p = .74).
Discussion
The present study examined whether the association between one’s own empathic accuracy and mental health is moderated by a close relational partner’s level of depression and anxiety. We predicted that one’s own greater empathic accuracy would be associated with better mental health when a partner lacks depressive symptoms, whereas one’s own greater empathic accuracy would be associated with poorer mental health when a partner has high levels of depressive symptoms. In Study 1, we examined this hypothesis in heterosexual married couples using an empathic accuracy task in which participants rated the emotional valence of their own spouse. In Study 2, we examined this hypothesis in a sample of caregivers for individuals with dementia using an empathic accuracy task in which caregivers rated the emotional valence of a stranger. Across both studies, we found that a partner’s level of depressive symptoms significantly moderates the association between one’s own empathic accuracy and depression, such that higher empathic accuracy is linked with more depressive symptoms when a partner has high levels of depressive symptoms, but fewer depressive symptoms when a partner has low levels of depressive symptoms. These results demonstrate that high levels of empathic accuracy can correspond with better or worse mental health, depending on a partner’s level of depressive symptoms. We believe these findings reflect the critical role for empathic accuracy in depression contagion in close relationships, and the benefits of one’s own empathic accuracy for one’s own mental health in the absence of a partner’s depressive symptoms.
Contrary to our hypotheses in both Study 1 and Study 2, results were specific to depression; comparable results did not emerge for anxiety. This finding fits with previous literature that suggests symptoms of depression may be more contagious than symptoms of anxiety in close relationships (Joiner, 1994). The relational attributions individuals make regarding a partner’s depression may differ from those of anxiety. While research suggests that, in general, shared negative affect in dyads is associated with negative views regarding the relationship (Brown et al., 2021), unlike anxiety, depression is more strongly tied to feelings of loneliness and isolation. As a result, individuals may be more likely to attribute their partner’s depressed affect to problems in their relationship, whereas anxiety may be more attributable to the external environment. Future research should explore this possibility.
Using the measure of caregiver depression from Study 2 (CESD), past research has highlighted distinct symptom clusters of depression in older adults, including somatic symptoms, low positive affect, depressed affect, and interpersonal problems. We explored whether care recipients’ depression was associated with higher levels of each of these symptom clusters in caregivers who had higher empathic accuracy. Results revealed that caregivers high in empathic accuracy caring for an individual with high levels of depressive symptoms had the highest levels of depressed affect and interpersonal problems, but not somatic symptoms or low positive affect. These differences may emerge due to limitations in the measurement of constructs (e.g., the measure of care recipient depression may capture depressed affect better than somatic symptoms). Alternatively, empathic accuracy may specifically promote the transmission of depressed affect and promote interpersonal problems with a depressed partner, including feelings of loneliness and isolation. It is possible that somatic symptoms and low positive affect are less likely to result from depression contagion or that these symptoms are simply more heavily determined by other factors we did not measure (e.g., lack of sleep or enjoyable activities; Talbot et al., 2010).
The current findings contribute to our understanding of the interpersonal emotional concomitants of depressive symptoms in middle and late adulthood, periods where overall rates of depression usually drop (Fiske et al., 2009). Marriage is the closest relationship most adults experience, and emotions within close relationships become especially important for mental health with older age (Rook & Charles, 2017). In middle to late life, although the ability to understand a spouse’s changing emotional valence may be beneficial under many circumstances, emotional understanding may have deleterious effects when a spouse is depressed.
Findings from Study 2 exemplify how qualities of a caregiver and qualities of a care recipient interact to predict caregiver mental health (Wells et al., 2019). With the rapidly aging worldwide population, and the increasing prevalence of dementia with age, mental health problems associated with dementia caregiving will be a major public health issue with increasing implications for psychological science (Kawas & Brookmeyer, 2009). Emotional problems and suffering in care recipients are known to be problematic for caregiver mental health (Schulz et al., 2008), and the current findings suggest that empathically accurate caregivers may be most susceptible to the mental health consequences of care recipients’ depressive symptoms. Poor mental health in caregivers has been associated with greater mortality in their care recipients (Lwi et al., 2017), highlighting the need for targeted interventions that can stop the spread of depression in these vulnerable dyads (Hua et al., 2021).
Strengths, Limitations, and Future Directions
The current studies advance our understanding of the conditions under which empathic skills are associated with good or bad mental health, and highlight empathic accuracy as a factor that may promote shared depression in dyads. Strengths of the current studies include (a) the use of two objective measures of empathic accuracy derived from naturalistic social interactions, which do not rely on subjective perspectives on empathic traits, (b) a large community sample of heterosexual married couples and a unique clinical population in which depressive symptoms are heightened, and (c) well-validated measures of depressive symptoms. In addition, these findings add diversity to the literature on empathy by focusing on middle-aged and elderly dyads.
In Study 1, where the measure of empathic accuracy required participants to accurately rate their own spouse, it is possible that more expressive spouses were rated more accurately. Thus, greater expressivity, rather than individual differences in empathic skills could have been a driving force underlying shared depression for individuals high in empathic accuracy. We explicitly addressed this possibility in Study 1 by controlling for a partner’s level of expressivity, and observed a significant moderating effect of empathic accuracy. Nonetheless, the measure of empathic accuracy in Study 1 remains inherently dyadic, and factors other than a participant’s skill in reading other’s emotions could increase their accuracy score. For example, characteristics of the spouse (like having more or less predictable and idiosyncratic self-ratings) could influence empathic accuracy. We addressed this possibility in Study 2 by having all caregivers rate the same standardized videos of unfamiliar targets expressing emotions during naturalistic social interactions, and continued to observe significant moderating effects of empathic accuracy. Even so, our measures of empathic accuracy capture the ability to accurately detect changes in another person’s emotional valence, and results may not generalize to other forms of empathic accuracy (e.g., rating a monologue or accurately identifying specific emotions like anger and sadness).
In Study 2, we used structured clinical interviews with caregivers to capture care recipient depression. Clinical interviews with caregivers are the gold standard for measuring depression in individuals with neurodegenerative disease, because these individuals often lack the ability to report on their own depressive symptoms. Although the trained interviewers (in this case licensed nurses) ultimately rate care recipients’ level of depression, both the reports of caregivers’ depression and their care recipient’s depression are based on caregiver reports. As a result, it remains possible that greater care recipient depression corresponds with greater caregiver depression for all dyads, but this association only emerged for caregivers higher in empathic accuracy because only these caregivers could accurately report on their care recipient’s depressive psychiatric symptoms. We find this possibility unlikely considering that results did not extend to anxiety, and considering that a similar interaction was observed in Study 1, in which spouses each reported on their own depressive symptoms independently.
Because results from both studies are correlational in nature, we cannot conclude that empathic accuracy necessarily leads to depression contagion. Depression can influence the accuracy of social judgements (Moore & Fresco, 2012), and we must consider the possibility that the current results emerge because individuals high in both depression and empathic accuracy somehow make their partners more depressed. Given the wealth of research linking greater empathic accuracy to positive outcomes for close relational partners (including less depression), (Brown et al., 2018; Brown, Wells, et al., 2020; Gordon et al., 2013), this possibility seems unlikely.
Findings from the present study point to several important areas for future research. The current research largely focused on negative states (i.e., depression, anxiety). Future studies should examine whether similar effects are found for positive states (e.g., positive affect and well-being; c.f., Brown & Fredrickson, 2021). For example, does empathic accuracy moderate the extent to which individuals share and benefit from their partner’s positive affect and well-being? Research should also explore whether other people’s depressive symptoms influence the association between empathic accuracy and mental health at earlier points in the lifespan (i.e., before middle and older adulthood), and in other types of relationships (e.g., coworkers, teacher-student relationships, non-familial caregivers, etc.). Relevant to the issue of other types of relationships, a similar pattern of effects has been found for physical health in parent-child relationships. In this study, greater cognitive empathy in parents was associated with greater inflammatory cytokine production, but only if their child was depressed (Manczak et al., 2015). Finally, we note that in both of our studies, participants were primarily white and lived within western culture. Given known cultural differences in emotional understanding and expression (Sun & Lau, 2018), future research should examine these topics in diverse populations.
Although shared depression can be cast in a negative light, it is important to consider the potential benefits and short-term value of sharing a partner’s depressive symptoms. Research has begun to highlight how sharing a partner’s negative affect can help that partner feel better (Brown, West, et al., 2020). Future research should explore whether shared depressive states help pull a couple out of a depressive episode, or create a downward spiral of negative affect that can lead to relationship dissolution. While more research is needed to understand how empathic accuracy influences the spread of mental health problems in dyads and social groups, the current findings suggest that in marriages and close caregiving relationships, individuals with the most depressive symptoms are those who are high on empathic accuracy and whose partners are most depressed.
Conclusions
Although empathic accuracy is typically viewed as beneficial for social functioning and mental health, results from the current studies demonstrate that greater empathic accuracy is linked with worse mental health for individuals enmeshed in a depressive milieu. Findings sound a cautionary note for researchers actively developing and implementing interventions aimed at increasing empathic accuracy because individuals high in empathic accuracy may be more likely to share their close relational partners’ depressive symptoms. Future research examining the ramifications of empathic accuracy for mental health should take into account the extent to which the individual’s close relational partners are depressed.
Supplementary Material
Acknowledgements
We would like to thank our participants, Scott Newton, Deepak Paul, and other members of the Berkeley Psychophysiology lab, as well as the UCSF Memory and Aging Center for their help conducting the studies.
Funding
Preparation of this manuscript was supported by National Institute on Aging grants 4R01AG041762 and 1R01AG062639 to R.W.L., P01AG019724, and K99AG073617 to C.L.B. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
The rating dial mirrors the affective circumplex model of valence, in which positive and negative affect fall along a unidimensional scale (Posner et al., 2005).
This correlational approach for computing empathic accuracy captures the degree to which an individual accurately detects changes in another’s emotional valence, and has been widely used in studies on empathic accuracy (Brown, Hua, et al., 2020; Hua et al., 2021; Kern et al., 2013; Zaki et al., 2008; Zaki, Weber, et al., 2009).
Although simple slopes analysis is a convention that is useful for understanding and describing the nature of significant interactions, the significance of simple slopes at an arbitrary threshold of 1 standard deviation above and below the mean is not particularly informative because the significance of simple slopes can vary at different thresholds (Finsaas & Goldstein, 2021). Even when simple slopes are not significant (meaning slopes do not differ significantly from zero), the presence of a significant interaction should still be interpreted as a significant difference between two slopes. The simple slopes analysis reveals which slope is more negative or positive relative to the other slope, and this difference should be interpreted even if the slopes are non-significant.
For all simple slope analyses, we compared models with and without equality constraints across genders at high and low levels of the IVs to ensure that simple slopes did not differ significantly by gender at relatively high and low levels of the predictors.
The sample size for Study 2 was smaller than intended because data collection ended due to the COVID-19 pandemic. We conducted post-hoc, retrospective power simulations using R with the data collected for Study 2, focused on the significant interaction effect, which revealed 61% achieved power.
For the CESD, a score of 16 is the most widely used clinical cutoff, however, recent research suggests the optimal cutoff score ranges from 15 to 23 depending on gender, ethnicity, and other factors (Henry et al., 2018).
Disease severity was the only other significant predictor of caregiver depression in this model, β = .44, t(86) = 3.23, p = .001. Additionally, when we limited the sample to include only romantic partners, the interaction between care recipient depressive symptoms and caregiver depressive symptoms remained a significant predictor of caregiver depressive symptoms, β = .21, t(77) = 2.08, p = .041. The interaction between care recipient anxiety and caregiver empathic accuracy remained a non-significant predictor of caregiver anxiety, β = −.01, t(77) = −.06, p = .95.
We conducted exploratory analyses for both studies to examine whether a partner’s anxiety symptoms moderated the association between empathic accuracy and depressive symptoms. In these analyses the interaction effects were not significant: Study 1: (B = .191, SE = .155, p = .218); Study 2: (β = .160, t(98) = 1.46, p = .147). Similarly, partner’s depressive symptoms did not moderate the association between empathic accuracy and anxiety: Study 1: (B = .164, SE = .093, p = .078); Study 2: (β = .162, t(98) = 1.55, p = .124).
Conflict of Interest
The authors declare no conflicts of interest with respect to the authorship or the publication of this article.
References
- Armstrong MJ, Litvan I, Lang AE, Bak TH, Bhatia KP, Borroni B, Boxer AL, Dickson DW, Grossman M, Hallett M, Josephs K. a., Kertesz A, Lee SE, Miller BL, Reich SG, Riley DE, Tolosa E, Tröster AI, Vidailhet M, & Weiner WJ (2013). Criteria for the diagnosis of corticobasal degeneration. Neurology, 80(5), 496–503. 10.1212/WNL.0b013e31827f0fd1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloom P (2017). Empathy and Its Discontents. Trends in Cognitive Sciences, 21(1), 24–31. 10.1016/J.TICS.2016.11.004 [DOI] [PubMed] [Google Scholar]
- Brodaty H, & Donkin M (2009). Family caregivers of people with dementia. In Dialogues in Clinical Neuroscience (Vol. 11, Issue 2, pp. 217–228). 10.1002/gps [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown CL, Chen K, Wells JL, Otero MC, Connelly DE, Levenson RW, & Fredrickson BL (2021). Shared emotions in shared lives: Moments of co-experienced affect, more than individually-experienced affect, linked to relationship quality. Emotion. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown CL, & Fredrickson BL (2021). Characteristics and consequences of co-experienced positive affect: understanding the origins of social skills, social bonds, and caring, healthy communities. Current Opinion in Behavioral Sciences, 39, 58–63. 10.1016/J.COBEHA.2021.02.002 [DOI] [Google Scholar]
- Brown CL, Hua AY, De Coster L, Sturm VE, Kramer JH, Rosen HJ, Miller BL, & Levenson RW (2020). Comparing two facets of emotion perception across multiple neurodegenerative diseases. Social Cognitive and Affective Neuroscience, 15(5), 511–522. 10.1093/scan/nsaa060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown CL, Lwi SJ, Goodkind MS, Rankin KP, Merrilees J, Miller BL, & Levenson RW (2018). Empathic accuracy deficits in patients with neurodegenerative disease: Association with caregiver depression. American Journal of Geriatric Psychiatry, 26(4), 484–493. 10.1016/j.jagp.2017.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown CL, Wells JL, Hua AY, Chen K-H, Merrilees J, Miller BL, & Levenson RW (2020). Emotion recognition and reactivity in persons with neurodegenerative disease are differentially associated with caregiver health. The Gerontologist, 60(7), 1233–1243. 10.1093/geront/gnaa030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown CL, West TV, Sanchez AH, & Mendes WB (2020). Emotional Empathy in the Social Regulation of Distress: A Dyadic Approach: 10.1177/0146167220953987, 47(6), 1004–1019. 10.1177/0146167220953987 [DOI] [PubMed] [Google Scholar]
- Budka H, Aguzzi A, Brown P, Brucher J-M, Bugiani O, Gullotta F, Haltia M, Hauw J-J, Ironside JW, Jellinger K, Kretzschmar HA, Lantos PL, Masullo C, Schlote W, Tateishi J, & Weller RO (1995). Neuropathological Diagnostic Criteria for Creutzfeldt-Jakob Disease (CJD) and Other Human Spongiform Encephalopathies (Prion Diseases). Brain Pathology, 5(4), 459–466. 10.1111/J.1750-3639.1995.TB00625.X [DOI] [PubMed] [Google Scholar]
- Cameron CD, Hutcherson CA, Ferguson AM, Scheffer JA, Hadjiandreou E, & Inzlicht M (2019). Empathy Is Hard Work: People Choose to Avoid Empathy Because of Its Cognitive Costs. Journal of Experimental Psychology: General. 10.1037/xge0000595.supp [DOI] [PubMed] [Google Scholar]
- Chen K-H, Wells JL, Otero MC, Lwi SJ, Haase CM, & Levenson RW (2017). Greater experience of negative non-target emotions by patients with neurodegenerative diseases is related to lower emotional well-being in caregivers. Dementia and Geriatric Cognitive Disorders, 44(5–6), 245–255. 10.1159/000481132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colvin CR, Vogt D, & Ickes W (1997). Why do friends understand each other better than strangers do? In Empathic accuracy. (pp. 169–193). The Guilford Press. [Google Scholar]
- Coope B, Ballard C, Saad K, Patel A, Bentham P, Bannister C, Graham C, & Wilcock G (1995). The prevalence of depression in the carers of dementia sufferers. International Journal of Geriatric Psychiatry, 10(3), 237–242. 10.1002/gps.930100310 [DOI] [Google Scholar]
- Coyne JC (1976). Toward an Interactional Description of Depression. Psychiatry, 39(1), 28–40. 10.1080/00332747.1976.11023874 [DOI] [PubMed] [Google Scholar]
- Cuijpers P (2005). Depressive disorders in caregivers of dementia patients: a systematic review. Aging & Mental Health, 9(4), 325–330. 10.1080/13607860500090078 [DOI] [PubMed] [Google Scholar]
- Cummings JL (1997). The Neuropsychiatric Inventory: Assessing psychopathology in dementia patients. Neurology, 48(Issue 5, Supplement 6), 10S–16S. 10.1212/WNL.48.5_Suppl_6.10S [DOI] [PubMed] [Google Scholar]
- Depow GJ, Francis ZL, & Inzlicht M (2020). The Experience of Empathy in Everyday Life. PsyArXiv 10.31234/OSF.IO/HJUAB [DOI] [PubMed] [Google Scholar]
- Derogatis L, Lipman R, & Covi L (1973). SCL-90: An outpatient psychiatric rating scale-preliminary report. Psychopharmacology Bulletin, 9(1), 13–29. [PubMed] [Google Scholar]
- Derogatis LR, & Cleary PA (1977). Confirmation of the dimensional structure of the SCL-90: A study in construct validation. Journal of Clinical Psychology, 33(4), 981–989. 10.1002/1097-4679 [DOI] [Google Scholar]
- Dezecache G, Jacob P, & Grèzes J (2015). Emotional contagion: its scope and limits. Trends in Cognitive Sciences, 19(6), 297–299. 10.1016/J.TICS.2015.03.011 [DOI] [PubMed] [Google Scholar]
- Dimitroff SJ, Kardan O, Necka EA, Decety J, Berman MG, & Norman GJ (2017). Physiological dynamics of stress contagion. Scientific Reports, 7(1), 6168. 10.1038/s41598-017-05811-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg N, & Miller PA (1987). The relation of empathy to prosocial and related behaviors. Psychological Bulletin, 101(1), 91–119. 10.1037/0033-2909.101.1.91 [DOI] [PubMed] [Google Scholar]
- Finsaas MC, & Goldstein BL (2021). Do simple slopes follow-up tests lead us astray? Advancements in the visualization and reporting of interactions. Psychological Methods, 26(1), 38–60. 10.1037/MET0000266 [DOI] [PubMed] [Google Scholar]
- Fiske A, Wetherell JL, & Gatz M (2009). Depression in Older Adults. Annual Review of Clinical Psychology, 5(1), 363–389. 10.1146/annurev.clinpsy.032408.153621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gleichgerrcht E, & Decety J (2011). The costs of empathy among health professionals. In Decety J (Ed.), Empathy: From Bench to Bedside (p. 245). https://books.google.com/books?hl=en&lr=&id=qO_uCwAAQBAJ&oi=fnd&pg=PA245&dq=the+costs+of+empathy+among+health+professionals&ots=mljN91zfS4&sig=DpyiwvYNeHqOUhws308B2K2sDw0 [Google Scholar]
- Gordon AM, Tuskeviciute R, & Chen S (2013). A multimethod investigation of depressive symptoms, perceived understanding, and relationship quality. Personal Relationships. 10.1111/pere.12005 [DOI] [Google Scholar]
- Gorman JM (1996). Comorbid depression and anxiety spectrum disorders. Depression and Anxiety, 4(4), 160–168. [DOI] [PubMed] [Google Scholar]
- Gorno-Tempini ML, Hillis a E., Weintraub S, Kertesz a, Mendez M, Cappa SF, Ogar JM, Rohrer JD, Black S, Boeve BF, Manes F, Dronkers NF, Vandenberghe R, Rascovsky K, Patterson K, Miller BL, Knopman DS, Hodges JR, Mesulam MM, & Grossman M (2011). Classification of primary progressive aphasia and its variants. Neurology, 76, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottman JM, & Levenson RW (1985). A valid procedure for obtaining self-report of affect in marital interaction. Journal of Consulting and Clinical Psychology, 53(2), 151–160. http://psycnet.apa.org/buy/1985-22469-001 [DOI] [PubMed] [Google Scholar]
- Haeffel GJ, & Hames JL (2014). Cognitive Vulnerability to Depression Can Be Contagious. Clinical Psychological Science, 2(1), 75–85. 10.1177/2167702613485075 [DOI] [Google Scholar]
- Hames JL, Hagan CR, & Joiner TE (2013). Interpersonal Processes in Depression. 10.1146/Annurev-Clinpsy-050212-185553, 9, 355–377. [DOI] [PubMed] [Google Scholar]
- Hatfield E, Cacioppo JT, & Rapson RL (1993). Emotional Contagion. Current Directions in Psychological Science, 2(3), 96–100. 10.1111/1467-8721.ep10770953 [DOI] [Google Scholar]
- Hays JC, Landerman LR, George LK, Flint EP, Koenig HG, Land KC, & Blazer DG (1998). Social Correlates of the Dimensions of Depression in the Elderly. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 53B(1), P31–P39. 10.1093/geronb/53B.1.P31 [DOI] [PubMed] [Google Scholar]
- Henry SK, Grant MM, & Cropsey KL (2018). Determining the optimal clinical cutoff on the CES-D for depression in a community corrections sample. Journal of Affective Disorders, 234, 270–275. 10.1016/J.JAD.2018.02.071 [DOI] [PubMed] [Google Scholar]
- Hittner EF, & Haase CM (2021). Empathy in context: Socioeconomic status as a moderator of the link between empathic accuracy and well-being in married couples, 38(5), 1633–1654. 10.1177/0265407521990750 [DOI] [Google Scholar]
- Hu LT, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6(1), 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Hua AY, Wells JL, Brown CL, & Levenson RW (2021). Emotional and Cognitive Empathy in Caregivers of People With Neurodegenerative Disease: Relationships With Caregiver Mental Health: 10.1177/2167702620974368, 9(3), 449–466. 10.1177/2167702620974368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ickes. (1997). Empathic Accuracy. Guilford Press. [Google Scholar]
- Ickes W, & Hodges S (2013). Empathic Accuracy in Close Relationships. In Oxford handbook of close relationships; (pp. 349–373). [Google Scholar]
- Joiner TE (1994). Contagious Depression: Existence, Specificity to Depressed Symptoms, and the Role of Reassurance Seeking. Journal of Personality and Social Psychology, 67(2), 287–296. 10.1037/0022-3514.67.2.287 [DOI] [PubMed] [Google Scholar]
- Joiner TE, & Katz J (1999). Contagion of Depressive Symptoms and Mood: Meta-analytic Review and Explanations from Cognitive, Behavioral, and Interpersonal Viewpoints. Clinical Psychology: Science and Practice, 6(2), 149–164. 10.1093/clipsy.6.2.149 [DOI] [Google Scholar]
- Jütten LH, Mark RE, & Sitskoorn MM (2019). Empathy in informal dementia caregivers and its relationship with depression, anxiety, and burden. International Journal of Clinical and Health Psychology, 19(1), 12–21. 10.1016/J.IJCHP.2018.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawas CH, & Brookmeyer R (2009). Aging and the Public Health Effects of Dementia. 10.1056/NEJM200104123441509, 344(15), 1160–1161. 10.1056/NEJM200104123441509 [DOI] [PubMed] [Google Scholar]
- Kern RS, Penn DL, Lee J, Horan WP, Reise SP, Ochsner KN, Marder SR, & Green MF (2013). Adapting Social Neuroscience Measures for Schizophrenia Clinical Trials, Part 2: Trolling the Depths of Psychometric Properties. Schizophrenia Bulletin, 39(6), 1201–1210. 10.1093/SCHBUL/SBT127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawton MP, & Brody EM (1969). Assessment of Older People: Self-Maintaining and Instrumental Activities of Daily Living 1. Gerontologist, 9(3), 179–186. 10.1093/geront/9.3_Part_1.179 [DOI] [PubMed] [Google Scholar]
- Lee HS, Flatley Brennan P, & Daly BJ (2001). Relationship of Empathy to Appraisal, Depression, Life Satisfaction, and Physical Health in Informal Caregivers of Older Adults. Research in Nursing & Health, 24, 44–56. 10.1002/1098-240X(200102)24:1 [DOI] [PubMed] [Google Scholar]
- Levenson RW, Ascher E, Goodkind M, McCarthy M, Sturm V, & Werner K (2008). Laboratory testing of emotion and frontal cortex. In Miller B & Goldenberg G (Eds.), Handbook of Clinical Neurology, Third Series (Vol. 88, pp. 489–498). Elsevier. 10.1016/S0072-9752(07)88025-0 [DOI] [PubMed] [Google Scholar]
- Levenson RW, Carstensen LL, & Gottman JM (1994). Influence of age and gender on affect, physiology, and their interrelations: A study of long-term marriages. Journal of Personality and Social Psychology, 67(1), 56–68. 10.1037/0022-3514.67.1.56 [DOI] [PubMed] [Google Scholar]
- Levenson RW, & Ruef AM (1992). Empathy: A Physiological Substrate. Journal of Personality and Social Psychology, 63(2), 234–246. 10.1037/0022-3514.63.2.234 [DOI] [PubMed] [Google Scholar]
- Levenson RW, & Ruef AM (1997). Physiological aspects of emotional knowledge and rapport. Guilford Press. [Google Scholar]
- Litvan I, Agid Y, Calne D, Campbell G, Dubois B, Duvoisin RC, Goetz CG, Golbe LI, Grafman J, Growdon JH, Hallett M, Jankovic J, Quinn NP, Tolosa E, & Zee DS (1996). Clinical research criteria for the diagnosis of progressive supranuclear palsy (Steele-Richardson-Olszewski syndrome): report of the NINDS-SPSP international workshop. [Review] [88 refs]. Neurology, 47(1), 1–9. [DOI] [PubMed] [Google Scholar]
- Lwi SJ, Ford BQ, Casey JJ, Miller BL, & Levenson RW (2017). Poor caregiver mental health predicts mortality of patients with neurodegenerative disease. Proceedings of the National Academy of Sciences of the United States of America, 114(28), 7319–7324. 10.1073/pnas.1701597114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyketsos CG, Lopez O, Jones B, Fitzpatrick AL, Breitner J, & DeKosky S (2002). Prevalence of Neuropsychiatric Symptoms in Dementia and Mild Cognitive Impairment. JAMA, 288(12), 1475. 10.1001/jama.288.12.1475 [DOI] [PubMed] [Google Scholar]
- Manczak EM, Basu D, & Chen E (2015). The Price of Perspective Taking: Child Depressive Symptoms Interact With Parental Empathy to Predict Immune Functioning in Parents. 10.1177/2167702615595001, 4(3), 485–492. 10.1177/2167702615595001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKeith I (2004). Dementia with Lewy bodies. Dialogues in Clinical Neuroscience, 6(3), 333. 10.31887/DCNS.2004.6.3/IMCKEITH [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR, Kawas CH, Klunk WE, Koroshetz WJ, Manly JJ, Mayeux R, Mohs RC, Morris JC, Rossor MN, Scheltens P, Carrillo MC, Thies B, Weintraub S, & Phelps CH (2011). The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s & Dementia, 7(3), 263–269. 10.1016/j.jalz.2011.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore MT, & Fresco DM (2012). Depressive realism: A meta-analytic review. Clinical Psychology Review, 32(6), 496–509. 10.1016/J.CPR.2012.05.004 [DOI] [PubMed] [Google Scholar]
- Morelli SA, Ong DC, Makati R, Jackson MO, & Zaki J (2017). Empathy and well-being correlate with centrality in different social networks. Proceedings of the National Academy of Sciences of the United States of America, 114(37), 9843–9847. 10.1073/pnas.1702155114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris JC (1997). Clinical dementia rating: a reliable and valid diagnostic and staging measure for dementia of the Alzheimer type. International Psychogeriatrics, 9 Suppl 1, 173–176; discussion 177–178. 10.1017/S1041610297004870 [DOI] [PubMed] [Google Scholar]
- Otero MC, & Levenson RW (2017). Lower visual avoidance in dementia patients Is associated with greater psychological distress in caregivers. Dement Geriatr Cogn Disord, 43, 247–258. 10.1159/000468146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paukert AL, Pettit JW, & Amacker A (2008). The Role of Interdependence and Perceived Similarity in Depressed Affect Contagion. Behavior Therapy, 39(3), 277–285. 10.1016/j.beth.2007.08.001 [DOI] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D Scale: A Self Report Depression Scale for Research in the General. Applied Psychological Measurement, 1, 385–401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- Rascovsky K, Hodges JR, Knopman D, Mendez MF, Kramer JH, Neuhaus J, Van Swieten JC, Seelaar H, Dopper EGP, Onyike CU, Hillis AE, Josephs KA, Boeve BF, Kertesz A, Seeley WW, Rankin KP, Johnson JK, Gorno-Tempini M-L, Rosen H, … Miller BL (2011). Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain, 134(9), 2456–2477. 10.1093/brain/awr179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rook KS, & Charles ST (2017). Close social ties and health in later life: Strengths and vulnerabilities. The American Psychologist, 72(6), 567–577. 10.1037/amp0000104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosseel Y (2012). lavaan: An R Package for Structural Equation Modeling. Journal of Statistical Software, 48(2), 1–36. 10.18637/jss.v048.i02 [DOI] [Google Scholar]
- Ruef AM, & Levenson RW (2007). Continuous measurement of emotion: The affect rating dial. In Coan JA& Allen JJB (Eds.), The Handbook of Emotion Elicitation and Assessment (pp. 286–297). Oxford University Press. [Google Scholar]
- Schulz R, McGinnis KA, Zhang S, Martire LM, Hebert RS, Beach SR, Zdaniuk B, Czaja SJ, & Belle SH (2008). Dementia Patient Suffering and Caregiver Depression. Alzheimer Disease and Associated Disorders, 22(2), 170. 10.1097/WAD.0B013E31816653CC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuurmans J, & Van Balkom A (2011). Late-life Anxiety Disorders: A Review. Curr Psychiatry Rep, 13, 267–273. 10.1007/s11920-011-0204-4 [DOI] [PubMed] [Google Scholar]
- Sened H, Lavidor M, Lazarus G, Bar-Kalifa E, Rafaeli E, & Ickes W (2017). Empathic accuracy and relationship satisfaction: A meta-analytic review. Journal of Family Psychology, 31(6), 742–752. 10.1037/fam0000320 [DOI] [PubMed] [Google Scholar]
- Shu J, Hassell S, Weber J, Ochsner KN, & Mobbs D (2017). The role of empathy in experiencing vicarious anxiety. Journal of Experimental Psychology: General, 146(8), 1164–1188. 10.1037/xge0000335 [DOI] [PubMed] [Google Scholar]
- Soto JA, & Levenson RW (2009). Emotion recognition across cultures: The influence of ethnicity on empathic accuracy and physiological linkage. Emotion, 9(6), 874–884. 10.1037/a0017399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steer RA, & Beck AT (1997). Beck Anxiety Inventory. [Google Scholar]
- Sun M, & Lau AS (2018). Exploring Cultural Differences in Expressive Suppression and Emotion Recognition: 10.1177/0022022118763749, 49(4), 664–672. 10.1177/0022022118763749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sze JA, Goodkind MS, Gyurak A, & Levenson RW (2012). Aging and Emotion Recognition: Not Just a Losing Matter. Psychol Aging, 27(4), 940–950. 10.1037/a0029367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talbot LS, McGlinchey EL, Kaplan KA, Dahl RE, & Harvey AG (2010). Sleep Deprivation in Adolescents and Adults: Changes in Affect. Emotion (Washington, D.C.), 10(6), 831. 10.1037/A0020138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisz E, & Zaki J (2017). Empathy building interventions: A review of existing work and suggestions for future directions. In Seppala E, Simon-Thomas E, Brown S, Worline M, Cameron D, & Doty J (Eds.), The Oxford Handbook of Compassion Science. Oxford University Press. [Google Scholar]
- Weisz E, & Cikara M (2021). Strategic Regulation of Empathy. Trends in Cognitive Sciences, 25(3), 213–227. 10.1016/J.TICS.2020.12.002 [DOI] [PubMed] [Google Scholar]
- Weisz E, & Zaki J (2018). Motivated empathy: a social neuroscience perspective. Current Opinion in Psychology, 24, 67–71. 10.1016/J.COPSYC.2018.05.005 [DOI] [PubMed] [Google Scholar]
- Wells JL, Hua AY, & Levenson RW (2020). Poor Disgust Suppression is Associated with Increased Anxiety in Caregivers of People with Neurodegenerative Disease. J Gerontol B Psychol Sci Soc Sci 10.1093/geronb/gbaa056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells Jenna L., Brown CL, Hua AY, Soyster PD, Chen K-H, Dokuru DR, Coppola G, Haase CM, & Levenson RW (2019). Neurodegenerative disease caregivers’ 5-HTTLPR genotype moderates the effect of patients’ empathic accuracy deficits on caregivers’ well-being. The American Journal of Geriatric Psychiatry, 27(10), 1046–1056. 10.1016/J.JAGP.2019.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolley JD, Khan BK, Murthy NK, Miller BL, & Rankin KP (2011). The diagnostic challenge of psychiatric symptoms in neurodegenerative disease: rates of and risk factors for prior psychiatric diagnosis in patients with early neurodegenerative disease. The Journal of Clinical Psychiatry, 72(2), 126–133. 10.4088/JCP.10m06382oli [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaki J (2017). Moving beyond Stereotypes of Empathy. Trends in Cognitive Sciences, 21(2), 59–60. 10.1016/J.TICS.2016.12.004 [DOI] [PubMed] [Google Scholar]
- Zaki J, Bolger N, & Ochsner K (2008). It takes two: The interpersonal nature of empathic accuracy: Research article. Psychological Science, 19(4), 399–404. 10.1111/j.1467-9280.2008.02099.x [DOI] [PubMed] [Google Scholar]
- Zaki J, Bolger N, & Ochsner K (2009). Unpacking the informational bases of empathic accuracy. Emotion, 9(4), 478–487. 10.1037/a0016551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaki J, Weber J, Bolger N, & Ochsner K (2009). The neural bases of empathic accuracy. Proceedings of the National Academy of Sciences of the United States of America, 106(27), 11382–11387. 10.1073/pnas.0902666106 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


