Abstract
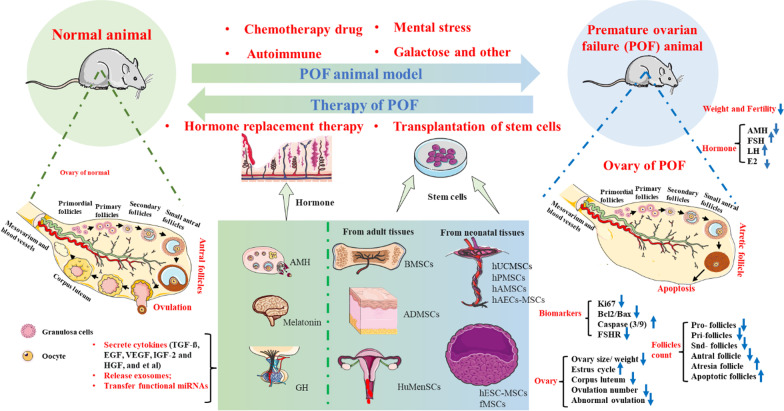
Incidence of premature ovarian failure (POF) is higher with the increase of the pace of life. The etiology of POF is very complex, which is closely related to genes, immune diseases, drugs, surgery, and psychological factors. Ideal animal models and evaluation indexes are essential for drug development and mechanism research. In our review, we firstly summarize the modeling methods of different POF animal models and compare their advantages and disadvantages. Recently, stem cells are widely studied for tumor treatment and tissue repair with low immunogenicity, high homing ability, high ability to divide and self-renew. Hence, we secondly reviewed recently published data on transplantation of stem cells in the POF animal model and analyzed the possible mechanism of their function. With the further insights of immunological and gene therapy, the combination of stem cells with other therapies should be actively explored to promote the treatment of POF in the future. Our article may provide guidance and insight for POF animal model selection and new drug development.
Graphical Abstract
Keywords: Premature ovarian failure, Animal model, Hormone replacement therapy, Transplantation of stem cells, Chemotherapy drug
Introduction
Premature menopause is closely associated with premature ovarian failure (POF), also known as premature insufficient ovarian failure (POI). The incidence of POF was 0.01% in women aged 20 years, 0.1% in women aged 30 years, and 1% in women aged 40 years [1]. The etiology of POF is very complex and closely related to genetics, immune diseases, drugs, surgery, and psychological factors [2]. Currently, according to the etiology of POF, the widely used POF animal models can be classified as chemotherapy drug-induced POF models, autoimmune POF models, POF models of mental stress, and galactose (GAL)-POF models. However, different POF animal model methods have their advantages and disadvantages. For example, the stability of POF animal models of autoimmune and mental stress is low. GAL-induced animal model can better simulate the physiological aging characteristics of clinical POF patients, but the success rate is lower. Hence, it is still a big challenge to select an ideal animal model for drug intervention and mechanism exploration.
Clinically, long-term hormone replacement therapy (HRT), mainly estrogen and progesterone, is the most common treatment for women with POF. The therapeutic and protective effects of some hormones, such as anti-Müllerian hormone (AMH), melatonin, and growth hormone (GH), have been confirmed and accepted. However, long-term use of HRT may increase the risk of cardiovascular disease and cancer [3]. So far, POF is still clinically irreversible. It is an urgent need to find advanced treatment strategies. Recently, the role of stem cells in the treatment of POF animal models has been gradually explored. Stem cells can differentiate into ovarian cells in the microenvironment of POF, to supplement the number of normal ovarian cells [4]. In addition, the regenerated ovarian cells by stem cells can secrete female hormone to maintain the hormone balance and improve women's symptom caused by the decline of ovarian function [5].
In our review, we firstly summarized different POF animal model methods and compared their advantages and disadvantages. Next, we summarized the recently published data on HRT and stem cells in the POF animal model. Our article may provide guidance and insight for POF animal model selection and new drug development.
Comparison of different POF animal models
POF animal model of chemotherapy drugs
It is estimated that more than 6.6 million women are diagnosed with cancer each year, approximately 10% of whom are aged younger than 40 years. The most important and common causes of POF are chemotherapy and radiation therapy in cancer treatment. Cytotoxic chemotherapy and radiotherapy have improved survival in many cases, but alterations in gonadal function are one of the most common long-term side effects of treatment. Some chemotherapeutic agents are associated with gonadal toxicity (e.g., cyclophosphamide (CTX), bucillamine, and nitrogen mustard), while others have minor or unquantifiable effects (e.g., doxorubicin (DOX), vinca alkaloid cisplatin (CIS), and nitrourea). An animal study showed that anticancer drugs (doxorubicin and paclitaxel) reduced the number of primitive and developing follicles in goat preantral follicles [6]. Other studies have also shown that the incidence of POF in women with breast cancer treated with docetaxel + pirarubicin + ifosfamide (DTC) chemotherapy is higher than that in healthy women [7]. Using CTX, methotrexate and fluorouracil (CMF) for more than 4 cycles increase the risk of infertility by more than 80% [8]. The pathophysiological mechanism of chemotherapy-associated POF is that the drugs destroy DNA, induce apoptosis of normal ovarian follicles, and block ovarian vascularization, thus interfering with the functional and structural features of oocytes [8, 9]. Recently, the pathogenesis of POF has been understood to some extent, but an appropriate animal model of POF will benefit the development of new drugs and observation of efficacy. At present, the most common drugs include CTX, tripterygium glycosides (TG), busulfan (BF), CIS, DOX, etc.
CTX inhibits cell proliferation because of its strong immunosuppressive effect. It significantly improves the clinical symptoms of patients with refractory nephropathy and has been widely used in the nephrology field. However, it is associated with serious side effects on female gonads, leading to ovarian damage, manifested as menstrual disorder, secondary amenorrhea, and even POF. The animal model of CTX-induced POF is simple in operation, is short in cycle, and only needs a single dose. TG exists a killing effect on rapidly proliferating cells (such as ovarian follicle cells), the mechanism of which mainly leads to DNA base mismatch and DNA chain rupture. The effect of DNA damage leads to a decrease in estrogen secretion in the ovary, which negatively increases FSH. The disadvantage of the TG-induced POF animal model is that the modeling cycle is long, while the advantage is that oral administration is relatively safe compared with other drug models [10]. CIS induces ovarian injury through the interaction of various factors, including activating apoptosis and the oxidative stress response in ovarian cells. CIS inhibits cellular DNA replication and RNA transcription, arrests cells in G2 phase, and leads to apoptosis. CIS-induced POF animal model has a low cost, a short cycle, low mortality and shows histological and endocrine changes similar to clinical POF ovaries. DOX is an anti-tumor antibiotic that inhibits the synthesis of RNA and DNA, and has the strongest inhibitory effect on RNA. A single intraperitoneal injection of DOX into ICR mice (7.5 mg/kg) resulted in a significant reduction in ovarian size and weight one month after treatment [11]. However, this approach of the POF model has rarely been reported in other articles, it maybe that the effect of this acute injury model is unstable and uncertain.
Clinicially, chemotherapy drugs are widely used, and the damage caused by their toxicity cannot be ignored. How to balance the therapeutic effect and toxic reaction of chemotherapy drugs and improve the safety of clinical drugs are the primary problems. Thus, seeking the prevention and treatment measures, and exploring the occurrence and development mechanism of diseases are beneficial. Animal model studies are helpful to understand the occurrence and development of human diseases more conveniently and effectively.
The autoimmune POF animal model
Immune factors account for 10–30% of POF, which may be simple ovarian autoimmune disease or accompany by other immune diseases. Recent studies have shown that the risk of POF in women of childbearing age with autoimmune diseases is increasing. Early diagnosis of immune POF patients is challenging, and these patients are often in a state of ovarian failure at the time of treatment.
ZP3 glycoprotein is a critical zona pellucida glycoprotein and sperm receptor. Immunizing animals with ZP3 glycoprotein can cause ovaritis by activating T cells, and IgG antibodies against human recombinant ZP3 can lead to follicle destruction [12]. The method of inducing immunocompromised POF mice with ZP3 glycoprotein is easy to establish, with a short cycle, high survival rate of mice (100%), and high success rate (80–90%). In addition, the mouse ZP3 protein shares 67% homology with human ZP3. ZP3 polypeptide induces mice to produce ZP3 polypeptide antibody, which binds to ovarian ZP3 to cause an immune response and interferes with information exchange between oocytes and granulosa cells. The above can induce ovarian atrophy, anovulation, and other manifestations, such as human POF. Hence, the ovarian histomorphology of the ZP3 polypeptide-induced POF mouse model is similar to that of human POF autoimmune ovaritis [12]. The ZP3 glycoprotein-induced POF mouse model is a classical modeling method to explore the pathogenesis and pathological changes of autoimmune POF.
Another method of antoimmune POF animal is that the supernatant protein of ovarian tissue of rats combined with Freund's adjuvant serves as an ovarian antigen. The rat model of autoimmune POF was successfully established by subcutaneous injection of 0.35 mL of ovarian antigen three times every 10 days [13]. Because this method is rarely used, it remains unclear what concentration of ovarian antigen can be used to successfully construct an autoimmune POF model. Moreover, studies have shown that removing the thymus of 3-day-old neonatal mice induces autoimmune ovaritis and leads to complete oocyte loss in adult mice [14]. However, thymectomy for newborn mice is difficult to perform and has a high mortality rate.
The POF animal model of mental stress
Psychological stress, for example chronic anxiety, sadness, fear, and other negative emotions, can lead to POF by altering the function of the hypothalamic–pituitary–target gland axis, leading to the appearance of hypothalamic–pituitary–ovarian axis disorder. The failure of the feedback regulation of the hypothalamic–pituitary–ovarian axis disrupts the balance of the neuroendocrine–immune biomolecular network and ultimately leads to POF. Stress POF animal model can be constructed by alternately administering different frequencies of sound-light-electricity stimulation [15]. The decrease in biomolecules in the hypothalamic–pituitary–adrenal axis led to a significant decrease in biomolecules in the hypothalamus (β-EP, IL-1, NOS and GnRH), leading to a hormone decrease in the target gland layer (E2) in the pituitary–ovarian axis; the pituitary layer (FSH and LH) showed little change [15]. A chronic unpredictable mild stress (CUMS) model was constructed by alternating daily fasting and water deprivation, forced swimming, noise interference, and plantar electrical stimulation for 35 days. The results suggested that the CUMS rat model exhibited depression-like behaviors. CUMS causes psychological stress and decrease ovarian reserve in female rats [16]. The advantages of this modeling approach are that it is consistent with known major causative agents of human POF, and pathogenic pathways and pathological changes are similar to clinical observations.
Galactose and other POF animal models
Galactosemia (GAL) is an autosomal recessive genetic disease caused by the deficiency of galactosidase in the body, resulting in the obstruction of the stereo isomerization process of GAL. Because of the accumulation of GAL and its metabolites in the body, patients eventually develop liver, kidney, eye, nervous, and reproductive system damage. The main clinical manifestation of reproductive system injury is POF or primary amenorrhea. The main mechanism is as follows: the level of GAL in the cell is increased, which is catalyzed by aldose reductase and then is converted to galactol. However, the cell cannot further metabolize GAL, so GAL accumulates in the cell and affects the normal osmotic pressure, causing cell dysfunction. However, the increase in GAL concentration will cause direct damage to granulosa cells, oocytes, and follicular membrane cells of ovarian tissue, while the metabolites of GAL will cause parenchymal damage to the ovary [17]. The offspring of pregnant rats feeding with GAL from Day 3 to Day 21 postpartum showed different manifestations of ovarian dysfunction when they were adults [18]. The model had a success rate of approximately 63%. Aging is the most common cause of POF. D-GAL can accelerate the ageing process, which is similar to observations of normal ageing processes. Hence, the D-GAL-induced model is widely used in aging-induced POF animal model studies [18]. Approximately 75–96% of women have galactosamic gonadal dysfunction. This is because GAL awakens the biological activity of FSH and produces direct ototoxic effects [19]. POF animal model can be successfully constructed by subcutaneously with D-Gal (200 mg/kg/d) daily for 42 days [20]. The process of establishing the model is simple, and the time required is short.
Overall, the chemotherapy drug induced model is a classic and simple animal model for studying POF. However, there still exist many disadvantages. For example, CTX-induced POF animal model may exist many side effects, including myelosuppression and bleeding [21]. TG-induced POF animal model needs long molding time [10]. CIS-induced POF animal model is too toxic and may lead to death [22]. The success rate of DOX-induced POF animal model is uncertain [11]. The autoimmunity-induced model is most related to the etiology of human POF, but the operation of model is relatively complicated. Thymectomy for newborn mice is difficult to operate and has a high mortality rate [14]. The psychological factor-induced model is consistent with the pathogenesis factors of POF. But the model construction time is long, and the stability of this kind of model must be further determined [15]. Although the GAL animal model can better simulate the physiological aging characteristics of clinical POF patients, this model has a lower success rate and longer cycle [18]. Table 1 systematically compares the advantages and disadvantages of different animal models of POF.
Table 1.
The animal model of premature ovarian failure (POF)
| Method of model | Animal | Method of administration | Dosage of administration | Advantages | Disadvantages | The model from References |
|---|---|---|---|---|---|---|
| CTX | Wistar rat (180–200 g) | Ip: 14 days |
1st: 50 mg/kg; 2–14 th: 8 mg/kg |
The most common model; the operation is simple | Myelosuppression and bleeding | [21] |
|
SD rat (150 g) |
Ip: 14 days |
1st: 50 mg/kg; 4–15 th: 5 mg/kg |
[23] | |||
| SD rat (8 weeks) | Ip: 14 days |
1st: 50 mg/kg; 2–14 th: 5 mg/kg |
[24] | |||
| TG |
SD rat (220–250 g) |
Ig: 70 days | For 10 weeks: 40 mg/kg/days | High safety | Long molding time | [10] |
| CTX + BF | Wistar rat (180–220 g) | Ip (CTX) + ih (BF) | 1st: CTX:120 mg/kg + BF 12 mg/kg | Simple operation, short cycle, only a single dose | – | [25] |
| CIS |
SD rat (180–250 g) |
Ip: 6 days | 2 mg/kg, Daily, 6 days | Low-cost, short cycles, low mortality | The lethal dose (50) was 7.4 mg/kg | [22] |
| SD rat (320 ± 10 g) | Ip: 10 days | 1.5 mg/kg, Daily, 10 days | [26] | |||
| DOX |
ICR mice (7–8 weeks) |
Ip: 7.5 mg/kg, | Single dose | The operation is simple | The model success rate is uncertain | [11] |
| ZP3 glycoproteins |
BALB/c mice (18–22 g) |
SI 1st and 14 th |
1st: 0.16 mg/mouse 14th: 0.16 mg/mouse |
Short cycle, high survival rate of mice (100%), and the high success rate (80–90%) | – | [27] |
|
BALB/c mice (7–8 weeks) |
SI 1st and 14 th |
1st: 0.16 mg/mouse 14th: 0.16 mg/mouse |
[28] | |||
| OA + FIA | SD rat (8 weeks) | SI | 3 times, once every 10 days. OA:FIA = 1: 1 | – | This method is rarely used | [13] |
| Thymus removing | BALB/c mice | Surgery | Removing the thymus of 3-day-old neonatal mice | 90% developed autoimmune ovaritis and POF | Thymectomy for newborn mice is difficult to operate and has a high mortality rate | [14] |
| Sound-light-electricity stimulation |
SD rat (200–220 g) |
For 20 days, 5 times per day | The acousto, optical, and electrical stimuli for 20 days | it is consistent with known major causative agents of human POF, and pathogenic pathways and pathological changes are like clinical observations | The success rate of the model is low and large samples are needed | [15] |
| CUMS | Wistar (~ 200 g) | For 35 days | Alternating daily fasting and water deprivation, forced swimming, noise interference, and plantar electrical stimulation | [16] | ||
| GAL |
SD rat (Born 35 days) |
Food pellet: 19 days | Food pellet with 35% galactose: from 3 days of conception continuing through weaning of the litters (21 days), the adult offspring were POF | Success rate:63% | The period is relatively long | [18] |
| D-GAL | Mice (7–8 weeks ) | SI: for 42 days | Daily with d-gal (200 mg/kg/day) | The process of establishing the model is simple | [20] |
CTX cyclophosphamide, TG tripterygium glycosides, BF busulfan, CIS cisplatinum, DOX doxorubicin, ZP3 zona pellucida 3, OA ovarian antigen, FIA: Freund's incomplete adjuvant, CUMS constructed chronic unpredictable mild stress, GAL galactose, D-GAL d-Galactose, Ip intraperitoneal injection, ih hypodermic injection, ig intragastric administration, SI subcutaneous injection
Common evaluation indicators of the POF animal model
Reasonable biological indicators are the key to judging the success of model construction and drug treatment effects. According to CALAS, the identification of experimental animal models requires the evaluation of their overall behavioral characteristics, tissues, organs, cells and molecules [29]. The evaluation of POF animal models mainly includes fertility, hormone, ovary and follicle, and biomarker evaluation.
Fertility in the POF animal model
POF is a fertility decline disease caused by decreased ovarian reserve function, so the most intuitive detection method for animal models is the number of litters produced. In the animal model of POF, reproductive capacity is significantly reduced, including the fertility index (fraction of females that delivered offspring/total females), number of pups, and mean body weight of pups [30]. The drug-induced POF animal model takes advantage of the side effects of chemotherapy drugs on ovarian tissues. In addition to acute damage to the ovaries, toxic side effects on other organs from chemotherapy drugs can markedly affect the survival status of rats. Hence, the rat weight sharply declines [31].
Histological assessment of the ovarian reserve in the POF animal model
The ovarian reserve refers to primordial follicles in the ovarian cortex of human females. Ovarian reserve tests are performed by directly or indirectly assessing the decline in the number of follicles [32]. Ovarian reserve of histological assessment includes the ovary volume and weight, the number of corpuses luteum, the length of the estrous cycle, the follicle count, the ratio of the ovulation number and abnormal ovulation [30]. In the ovarian tissues of the POF animal model, the ovarian volume and weight are decreased. Moreover, the corpus luteum, the ratio of the ovulation number and abnormal ovulation are lower, and the estrous cycle is extended. In addition, Pro-follicles, Pri-follicles, Snd-follicles, and antral follicles are reduced. However, atresia and apoptotic follicles are increased [33].
Endocrine aspects of the ovarian reserve in the POF animal model
Endocrine levels are indirect reflections of decreased ovarian reserve function in POF. Clinically, measurement of AMH levels is useful in assessing the reserve of follicles and may be useful in assessing fertility potential. The lower ofAMH represents a decrease in ovarian reserve function [34]. The main role of FSH is to promote the growth and development of follicles and estrogen secretion. In addition, it can be used to identify the physiological condition of the female ovary. Clinically, an abnormally high value of FSH may indicates POF. LH and E2 can also be used as diagnostic criteria for POF. In the hormone secretion of the POF animal model, AMH and E2 are decreased, while FSH and LH are increased [35].
Biomarkers of granulosa cells in the POF animal model
Most studies claim that ovarian apoptosis caused by oxidative stress and mitochondrial damage is the main cause of POF [30]. In the POF animal model, the expression of Ki67, Bcl2/Bax, and Caspase 3/9 is often used to measure ovarian proliferation and apoptosis levels. Follicle-stimulating hormone receptor (FSHR), a G protein-coupled receptor that binds to FSH, activates many intracellular signaling pathways, playing an important role in female follicle development and estradiol production. The gene mutation and downregulation of FSHR cause POI by preventing follicle development [36].
Overall, in the POF animal model, short-term measures of ovarian reserve function included a reduction in antral/atretic follicles and luteinization, disorder of the estrous cycle and hormone levels, and an increase in apoptotic biomarker expression. The long-term indicators were the decline in the fertility index and number of pups. Table 2 summarizes the common evaluation index of the POF animal model.
Table 2.
Common evaluation index of different POF animal models
| POF model | Body weight | Hormone | Biomarkers of granulosa cells | Fertility | The model from references | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AMH | FSH | LH | E2 | Ki67 | Bcl2 | Bax | Caspase (3/9) | FSHR | Number of litters produced | |||
| CTX | / | ↓ | ↑ | ↑ | ↓ | ↓ | ↓ | ↑ | ↑ | ↓ | ↓ | [30, 33] |
| VCD | ↓ | ↓ | / | / | ↑/↓ | / | / | / | / | / | / | [31] |
| CIS | ns | / | / | / | ↓ | / | / | / | ↑ | / | / | [22] |
| DOX | / | / | / | / | / | / | / | / | ↑ | / | / | [11] |
| GAL | / | / | ↑ | / | ↓ | / | / | / | / | / | / | [18] |
| pZP3 | ↓ | ↓ | ↑ | ↑ | ↓ | / | / | / | / | ↓ | / | [35] |
| OA + FIA | ↓ | ↓ | / | / | ↓ | / | ↓ | / | ↑ | ↓ | / | [13] |
| HFHS | / | / | / | / | ↓ | / | / | / | / | ↓ | / | [37] |
| POF model | Ovary | Follicles count | The model from references | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ovary size | Ovary weight | Estrous cycle | Corpus luteum | Ovulation number | Abnormal ovulation | Pro-follicles | Pri-follicles | Snd-follicles | Antral follicle | Atresia follicle | Apoptotic follicles | ||
| CTX | / | ↓ | - | ↓ | ↓ | ↑ | ↓ | ↓ | ↓ | ↓ | ↑ | ↑ | [30, 33] |
| VCD | ↓ | / | - | / | / | / | ↓ | ↓ | ↓ | / | ↑ | / | [31] |
| CIS | / | / | / | / | / | / | ↓ | ↓ | ↓ | ↓ | / | / | [22] |
| DOX | ↓ | ↓ | / | / | / | / | ns | ns | ns | ns | ns | ns | [11] |
| GAL | / | / | / | / | / | / | / | / | / | ↓ | / | / | [18] |
| pZP3 | / | ↓ | - | / | / | / | ↓ | ↓ | / | ↓ | / | ↑ | [35] |
| OA + FIA | / | / | / | ↓ | / | / | ↓ | ↓ | ↓ | ↓ | ↑ | / | [13] |
| HFHS | / | / | / | / | / | / | / | / | / | ↓ | / | ↑ | [37] |
AMH anti-Müllerian hormone, FSH follicle-stimulating hormone, LH luteinizing hormone, E2 estrogen, BCL2 B cell lymphoma 2, BAX Bcl-2 associated X protein, VCD 4-vinylcyclohexene dicyclic oxide, pZP3 zona pellucida 3 peptides, CTX cyclophosphamide, Pro-follicles primordial follicles, Pri-follicles primary follicles, Snd-follicles secondary follicles. Galactose (GAL), HFHS: High-fat diet,↓:Down-regulation, ↑: Up-regulation, ns: No statistical difference, /: no report; -: Interruption
Current study of POF therapy in an animal model
HRT in the treatment of the POF animal model
AMH is a hormone secreted by granulosa cells in preantral follicles and small antral follicles of the ovary. Detection of AMH can determine the functional status of granulosa cells and number of follicles. It demonstrated that the recombinant AMH protein can increase primordial follicless, rescuing the fertility of a CTX-treated POF animal model. The protective mechanism of AMH on CTX-induced follicular loss may be related to autophagy [38].
Melatonin (N-acetyl-5-methoxytryptamine, honey), a hormone produced primarily by the pineal gland of the brain, can also be produced by peripheral reproductive tissue (the ovary, and the placenta). Many studies have shown that exogenous melatonin has protective effects on the nervous system, kidneys, lungs, testes, uterus, and ovaries [39, 40]. In ovarian tissues, as a free group purifier in follicles, melanin promotes egg maturation, embryo development, and luteinization of granuloma cells [41]. It is reported that intraperitoneal administration of melatonin (15 or 30 mg/kg) for 15 days can successfully rescue CIS-induced primordial follicle loss by inhibiting phosphorylation of PTEN/AKT/FOXO3a pathway components and preventing FOXO3a nuclear shuttling in primordial follicles [42]. Another study showed that melatonin (20 mg/kg/day) taken orally for 34 days can increase the number of primordial follicles and antral follicles, increase body and ovary weight, and enhance the level of AMH by attenuating the activation of SIRT1 signaling pathway [43].
As a member of the growth factor family, GH (a peptide hormone secreted by the anterior pituitary gland) plays a crucial role in regulating growth and development, the gonadal axis, metabolism, and the mental state. Using mouse recombinant mouse GH (rmGH) for CTX-induced POF can significantly reduced ovarian granulocyte injury and the number of atretic follicles, and significantly increased the number of mature oocytes. They confirmed that GH may promoted ovarian tissue repair and estrogen release by activating the Notch-1 signaling pathway in ovarian tissue [44]. Subsequently, it confirmed that GH possesses a protective effect on ovarian tissue in the CTX-induced POF rat model by directly or indirectly promoting the balance between oxidative stress and oxidative detoxification of cells [45].
Table 3 lists the recent research status of HRT in the POF animal model. Although the short-term effects of HRT on POF animal models are effective, the long-term effects on fertility remain unknown. Thus, HRT has been little studied in animal models of POF. However, clinically, the improvement of POF symptoms mostly depends on personalized hormone treatment, aiming to maximize efficacy and reduce the associated risks.
Table 3.
Hormone replacement therapy (HRT) in the POF animal model
| Hormone | POF model | Hormone replacement therapy (HRT) | The HRT from references | ||||
|---|---|---|---|---|---|---|---|
| Animal | Drug | Method | Treatment | Assessment | Mechanism | ||
| AMH | Mice (6 weeks) |
CTX (1st:150 mg/kg, 75 mg/kg once/weeks for 4 weeks) |
0.5 mg/kg, once/weeks for 4 weeks | Ip | Increase primordial follicles and decrease growing follicles. Could not restore the estrous cycle, but could rescue the fertility of CTX-treated mice | Induces autophagy | [38] |
| Melatonin |
CD-1 Mice (5 weeks ) |
CIS (2 mg/kg for 15 days) |
15 or 30 mg/kg daily, for 15 days | Ip |
Increase the number of primordial follicles and antral follicles Decrease granulosa cell apoptosis |
Block the phosphorylation of PTEN/AKT/FOXO3a pathway | [42] |
|
Mice (6 weeks ) |
TG (50 mg/kg/days for 34 days) |
20 mg/kg/day, from day 8 to day 42 | Oral |
Increase the number of primordial follicles and antral follicles Increase body and ovary weight; Increase AMH Improve the estrous cycle |
Attenuates the activation of SIRT1 signaling | [43] | |
|
BALB/c-nu mice (6 weeks) |
CIS (5 mg/kg weekly for 3 weeks ) |
10 mg/kg daily for 3 weeks | Ip |
reduces primordial ovarian follicles loss and depletion caused by CTX protects reproductive endocrine function from CIS damage effectively protects sexually mature protects granulosa cells from damage |
DNA protection and antioxidant effects | [46] | |
| GH | C57BL/6 (4–5 weeks ) |
CTX (70 mg/kg a single) |
100 µL of rmGH daily for 12 days Low dose: 0.4 mg/kg; Medium dose: 0.8 mg/kg; High dose:1.6 mg/kg |
iv |
The number of atretic follicles was reduced in the medium- and high-dose groups Ovarian weight was increased in the medium- and high-dose groups Medium-dose group can reduce FSH level |
Activates the expression of NotCH-1 signaling pathway factors | [44] |
| Rats (6 weeks) |
CTX (1st, 50 mg/kg, 8 mg/kg for 14 days) |
100 µL of rmGH once a week for 28 days Low dose: 0.4 mg/kg; Medium dose: 0.8 mg/kg; High dose:1.6 mg/kg |
ih |
The high-dose group can increase the number of oocytes Ovarian weight was increased in the medium- and high-dose groups did not reverse hormone levels |
Directly or indirectly promotes the balance between oxidative stress and oxidative detoxification of cells | [45] | |
AMH anti-Müllerian hormone, GH growth hormone, rhGH recombinant human PEGylated GH
Stem cells in the treatment of the POF animal model
Stem cells from adult tissues in the treatment of the POF animal model
After using HRT for POF, the risk of cancer and cardiovascular disease is increased. Recently, stem cell therapy has become increasingly popular in POF studies. BMSCs are a member of the adult stem cell family with low immunogenicity and generally exist in the bone marrow microenvironment. BMSCs are isolated from bone marrow extract. Density gradient centrifugation is a common method of preparing BMSCs derived from bone marrow [47]. Under certain circumstances, BMSCs can renew and differentiate into different cells, such as bone, cartilage, and fat cells. Despite the low survival rate and limited differentiation potential of BMSCs after transplantation, cytokines secreted by the ovary can induce BMSCs to migrate to damaged tissues. In the ovarian microenvironment, BMSCs can inhibit inflammation, reduce OS, and regulate immunity to promote ovarian tissue repair by secreting cytokines (VEGF, HGF, IL-6) [48]. The specific mechanism of BMSCs in the treatment of POF has been fully described in this article [48]. However, the number of BMSCs is very limited, and the immunomodulatory properties of BMSCs vary among species. The aggressive procedure is painful for the patient and carries a risk of infection. In addition, their differentiation potential, number, and maximum lifespan significantly decrease with age. These factors greatly limit the clinical application of BMSCs.
ADMSCs have low immunogenicity and can secrete many important growth factors, cytokines, trophic factors, and regenerative factors. Compared with ADSCs from elderly donors, ADSCs from young donors showed a higher proliferation rate, and their differentiation ability still exists with age. Therefore, ADMSCs have advantages over BMSCs. ADSCs also maintain the potential to differentiate into cells of mesodermal origin. Their low immunogenicity makes them suitable for allogeneic transplantation and the treatment of drug-resistant immune diseases [49]. ADMSCs have the advantages of availability and repeatability in autologous cell repair and regeneration [50]. ADMSCs are usually derived from fat tissue during liposuction, lipoplasty, or isolated lipotomy procedures and are digested with collagenase, followed by centrifugation and washing [51]. ADMSCs from the inguinal subcutaneous fat of 6–8-week-old nondiabetic rats can be obtained. It also demonstrated that ADMSC transplantation can reduce the expression of Pannexin1 and Caspase3 molecules to play an anti-apoptotic role in the ovarian tissues of a POF animal model. ADSCs stopped growing at 11~12 subculture, and the number of ADSCs was lower than that of BMSCs. Mazini et al. compared the advantages and disadvantages of ADMSCs as well as the research status of their therapeutic application [52].
HuMenSCs can be isolated from menstrual blood. HuMenSCs are much easier to repair than other adult stem cells, possibly making them a potential clinical donor source. Gargett et al. first extracted HuMenSCs, which can differentiate into adipocytes, osteoblasts, and lung epithelial cells [53]. The therapeutic potential of HuMenSCs has been demonstrated in diabetes [54], myocardial infarction [55] and liver failure [56]. Human endometrial mesenchymal stem cells (ESCs) derived from menstrual blood have the characteristics of mesenchymal stem cells (MSCs). MSC surface markers (CD29, CD44, CD49f, CD90, CD105 and CD117) and ESC markers (Oct4 and SSEA3/4) were highly expressed on the HuMenSC surface [57]. It confirmed the differentiation of HuMenSCs into ovarian-like cells (especially GCs) by injecting HuMenSCs into CTX-induced POF rats through the tail vein [58]. However, the source of HuMenSCs in menstrual blood is limited, and there is a risk of infection.
BMSCs, ADMSCs and HuMenSCs are adult MSCs that have been extensively studied in POF animal models at present. Table 4 summarizes the research status and possible mechanisms of three types of stem cells and their exosomes in POF animal models. Its main advantages are low immunogenicity, strong homing ability and strong ability to split and self-renew. However, most of their extraction procedures are invasive and carry the risk of infection.
Table 4.
The transplantation of stem cells from adult tissues in the POF animal model
| Stem cell types | POF model | The transplantation of stem cells from adult tissues | Stem cell from references | ||||
|---|---|---|---|---|---|---|---|
| Animal | Drug | Stem Cells | Treatment | Main effects of stem cell on POF | Mechanism | ||
| BMSCs | Rats (5 weeks) |
CTX (1st, 50 mg/kg, 8 mg/kg for 14 days) |
BMSCs (1 × 106 cells) in 100μL PBS for 2w |
iv |
Increase E2 and AMH, decrease FSH level; Recover the estrous cycle; Increase the number of basal and sinus follicles |
BMSC-derived exosome Mir-144-5p has a protective effect on the apoptosis of CTX-damaged OGCs | [23] |
|
Rats (3 weeks) |
3.2 Gy radiotherapy (0.48 Gy/min) |
BMSCs (2 × 106 cells) in 150μL PBS |
iv |
Enhances ovarian follicles; Increases serum estradiol- and follicle-stimulating hormone levels; Restores fertility |
Upregulates Wnt/β-catenin and Hippo signaling pathways | [59] | |
| Exosome from BMSCs |
Mice (6–7 weeks) |
CIS (5 mg/kg) |
BMSCs-Exos (125 μg dissolved in 100 μL PBS |
iv |
Inhibit OGCs apoptosis; Increase E2; |
delivering miR-644-5p to granulosa cells to regulate p53 expression of cells | [60] |
| Rats (5 weeks) |
CTX (1st, 50 mg/kg, 8 mg/kg for 14 days ) |
BMSCs-Exos (150 μg dissolved in 100 μL PBS; every other day for 2 weeks) | iv |
Decrease FSH and LH, increase AMH, E2; Inhibit OGCs apoptosis; |
Exosomes miR-144-5p inactivated the PI3K/AKT pathway by suppressing PTEN targeting | [23] | |
| ADMSCs | Rats |
CTX (120 mg/kg) |
ADMSCs (1 × 106 cells, passages 3–4) |
Ip |
Increase the number of primordial follicles and decrease the number of atretic follicles; Increase AMH level; Inhibit the apoptosis of follicle |
Regulate the expression of Connexin43 and pAnnexin1 | [61] |
| Exosome from ADMSCs | Mice (7–8 weeks) |
CTX (120 mg/kg for 2 weeks) |
hADSC-Exos (1 × 106 cells, cocultured with hGCs) |
Ip |
Attenuate ovary damage; Increase the number of follicles; Enhanced the E2 and AMH levels and decreased the FSH levels; Inhibit OGCs apoptosis |
Increase expression of SMAD2, SMAD3, and SMAD5 in vivo and in vitro | [62] |
| HuMenSCs | Mice (7–8 weeks) |
CIS (2 mg/kg for 7 days ) |
HuMenSCs (2 × 106/mL) in 200 μL PBS | iv |
Increase body and ovary weight; Increase the number of follicles; Reduce OGCs apoptosis; repair ovarian injury, Stimulate regeneration, and improve ovarian function |
Protects damaged ovaries by secreting FGF2 | [63] |
| Rats (8 weeks) |
BF (36 mg/kg) |
HuMenSCs (Passages 3) |
iv |
Improve follicle development; Promote AMH and E2 secretion |
NO Report | [64] | |
| Rats (6–8 weeks) |
BF (36 mg/kg) |
HuMenSCs (1 × 106 cells per 200 μL) in 1 mL PBS |
iv |
Increased body and ovary weight; Increase the number of follicles; Reduce OGCs apoptosis |
NO Report | [58] | |
| Mice (18–19 g) |
CTX (120 mg/kg) + BF (30 mg/kg) |
hEnSCs (2 × 106 cells, passages 5) in 20 μL PBS |
Orthotopically inject |
Increased body weight; Improved estrous cycles; Restored fertility |
Reduce chemotherapy-induced depletion of the germline stem cell pool | [57] | |
BMSCs bone marrow mesenchymal stem cells, ADMSCs adipose-derived mesenchymal stem cells, HuMenSCs human menstrual-derived stem cells
Stem cells from neonatal tissues in the treatment of the POF animal model
Compared with adult tissue stem cells, human–neonatal tissue stem cells have lower immunogenicity, fewer ethical issues, a lower risk of infection, and a painless and noninvasive harvesting process and are easy to expand in vitro. Neonatal tissues such as the umbilical cord, placenta, amniotic membrane, or chorionic membrane can be obtained directly after delivery, avoiding invasive procedures and ethical concerns [65]. Moreover, MSCs isolated from these neonatal tissues represent ontogenetic younger cells, at least as attractive candidates for tissue engineering and regenerative medicine. hUCMSCs are the most widely studied MSCs in human–neonatal tissue stem cells and are mainly extracted from different compartments of the human umbilical cord. Compared with BMSCs, hUCMSCs have extensive advantages. On the one hand, the extraction process is noninvasive, preventing the risk of infection. On the other hand, hUCMSCs show higher proliferation and differentiation activity and faster self-renewal. hUCMSCs maintained a stable doubling time (DT) until the 10th generation, and BMSCs showed notably increased DT after only the 6th generation. hUCMSCs have been widely investigated in clinical therapeutic phase I or II trials, such as spinal cord injury, Alzheimer’s disease, and liver failure [66]. In recent years, hUCMSCs have received much attention due to their enormous therapeutic potential in POF therapy. Several studies have shown that the injection of hUCMSCs (1 × 106/mL in 100 μL of PBS) through the tail vein can effectively improve the ovarian status. The method of extracting hUCMSCs from the human umbilical cord is fast, painless, and low immunity. However, there are more moral and ethical issues. The research progress of hUCMSCs in the POF animal model has been detailedly reviewed [4].
HESC-MSCs are cells isolated from an early embryo (before the gastrula stage) or primitive gonad. Compared with other sources of MSCs, hESC-MSCs, they have a higher ability to proliferate and inhibit leukocyte growth [67]. HESC-MSCs show stronger anti-inflammatory properties than BMSCs [68]. HESC-MSCs can also overcome the obstacles encountered in harvesting MSCs from adult tissues, including the lack of appropriate donors, limited number of cells obtained in the acquisition process, limited ability to expand in vitro, and invasive nature of the procedure. HESC-MSCs have been shown to ameliorate chronic liver injury and autoimmune encephalitis. Bahrehbar et al. successfully extracted hESC-MSCs from the placenta and further confirmed that hESC-MSC transplantation was similar to BM-MSC transplantation, which can restore the structure and function of damaged ovarian tissue in CTX-induced POF mice and rescue fertility [69]. hESC-MSC transplantation has long been a controversial area. Proponents argue that it can help cure many intractable diseases because hESC-MSCs can differentiate into multifunctional APSCs, which most closely resemble human development. Opponents argue that hESC-MSC transplantation requires the destruction of embryos, which is anti-bioethical.
HPMSCs contain several stem cells based on placental anatomy: chorionic villi (CV-MSCs), amniotic membrane (AM-MSCs), chorionic plate (CP-MSCs), and umbilical cord Wharton Jelly (WJ-MSCs) [70]. Under the appropriate induction conditions, these placenta-derived MSCs can differentiate into various cell types. Compared with other stem cells from neonatal tissues, hESC-MSCs have the advantages of a convenient source, sufficient cell number, and easy isolation, culture, expansion, and purification, and they still possess the characteristics of stem cells after more than 30 generations. Transplantation of hESC-MSCs can restore the structure of damaged ovarian tissue and their function in CTX combined with BF-induced POF mice and rescue fertility. The possible mechanism is related to the promotion of follicle development, ovarian secretion, fertility, and ovarian cell survival through paracrine effects [69].
Human amniotic cells are divided into human amniotic epithelial cells (hAECs) and human amniotic mesenchymal stem cells (hAMSCs). Both cell types have the potential to differentiate into three layers of germ tissue. HAECs are a class of epithelial cells with stem cell characteristics that are not stem cells in nature because they cannot proliferate indefinitely. When hAECs were passaged to the fifth generation, the cells gradually became larger and older, and their proliferation ability was obviously weakened. However, hAMSCs could be transmitted to approximately the 30th generation without significant changes in cell morphology. hAMSCs had stronger differentiation and proliferation ability than hAECs. The biological characteristics of hAMSCs were superior to those of hAECs but were not superior in the expression of immune molecules. This effect may be because the cellular biological characteristics of hAMSCs, such as telomerase activity, expression level of pluripotent markers, cytokines, and collagen secretion, are superior to those of hAECs [71].
In addition to the above stem cells directly used in POF animal model therapy, other forms of stem cells have been investigated in POF treatment studies. Stem cell exosomes are a hot topic currently. Exosomes carry various microRNAs and proteins into target cells. Presently, exosomes from hUCMSCs and hAMSCs promote ovarian function by regulating the Hippo pathway and carry various microRNAs and proteins [72]. Collagen/hUCMSCs and Matrigel/hUCMSCs can also promote MSC adhesion and increase cell retention in the ovary [73]. In terms of the mode of administration in most animal studies, tail vein injections are the most widely used transplant method to deliver cells to recipients. However, most transplanted cells are trapped in the lungs and cannot reach the target organ. Hence, studies have designed sodium alginate-bioglass (SA-BG)-encapsulated hAECs to promote the adhesion properties, proliferative ability, migration, and homing ability of MSCs in the ovary [74]. Table 5 lists the transplantation of stem cells from neonatal tissues in the POF animal model.
Table 5.
The transplantation of stem cells from neonatal tissues in the POF animal model
| Stem cell type | POF model | The transplantation of stem cells from neonatal tissues | Stem cell from references | ||||
|---|---|---|---|---|---|---|---|
| Animal | Drug | Stem cells | Treatment | Main effects of stem cell on POF | Mechanism | ||
| hUCMSCs |
Rats (8 weeks) |
CTX (1st, 200 mg/kg, 8 mg/kg for 14 days) |
hUCMSCs (1 × 106/mL) in 100 μL PBS | iv |
Improve follicle development and hormone secretion; Reduce ovarian cells’ apoptosis |
NO Report | [75] |
|
Mice (6–7 weeks) |
CTX (120 mg/kg) + BF (30 mg/kg) |
hUCMSCs (1 × 106/mL) in 200 μL PBS | iv |
Increase ovarian size and the number of primary and secondary follicles, decrease the number of atretic follicles; Increase E2 secretion and decrease FSH levels; Exert anti-apoptotic and anti-inflammatory effects |
Activate AKT and P38 pathways; Exert anti-apoptotic and anti-inflammatory effects |
[76] | |
| C57BL/6 (8 weeks) | ZP3 | hUCMSCs (1 × 106/mL) | iv |
Increase serum E2, P, IL-4 levels, and decrease the levels of FSH, IFN-γ, IL-2; Increase the total number of follicles and decrease atretic follicles |
Restored impaired ovarian and endothelial function mediated by changes in the Th1/Th2 cytokine ratio | [77] | |
| SD Rats (12 weeks) |
CTX (1st , 200 mg/kg, 8 mg/kg for 14 days) |
hUCMSCs (5 × 106/mL) in 500 μL PBS | iv |
Restore the disorder of hormone secretion (increase E2 and AMH); Restores follicle production and prevents the loss of secondary follicles); Prolong estrous; Improve pregnant rate and embryos numbers of POF rats |
Improve ovarian failure via NGF/TrkA signaling pathway | [78] | |
|
Wistar rats (180–220 g) |
Paclitaxel (7.5 mg/kg for 1 weeks) | hUCMSCs (2 × 106/mL) in 20 μL PBS | Orthotopically inject |
Increase E2 and AMH, decrease FSH level; Increase antral follicle count |
Regulate the tissue expression of CK 8/18, TGF-ß and PCNA; By directly triggering the ovarian epithelium and/or indirectly enriching the ovarian niche |
[79] | |
| SD Rats (8 weeks) | Freund’s complete adjuvant | 1 mL hUCMSCs with low (0.25 × 106), medium (1 × 106) and high (4 × 106) doses | iv |
Restore estrous cycle; Improve follicle development in rats; Increased serum E2, P4 and AMH; Reduce apoptotic granulomas and promote the proliferation of granuloma cells |
Show dose-dependent effects on improving ovarian follicular development in POF rats | [13] | |
| C57BL/6 (6–8 weeks) | CTX (120 mg/kg) + BF (30 mg/kg) | hUCMSCs (1 × 106/mL) in 100 μL PBS | iv |
Increase levels of FSH and E2 secretion, Decrease follicular atresia, and increased the number of sinus follicles; Improve lymphocyte ratio |
Improve ovarian function through PPAR and cholesterol metabolism pathways | [80] | |
| C57BL/6 (4–6 weeks) | CTX (70 mg/kg) + BF (12 mg/kg) | hUCMSCs (5 × 105/mL) in 10 μL PBS | iv |
Increase ovarian weight and follicle number, Decrease FSH, increase AMH, FSHR; Increase pregnancy rate |
NO Report | [81] | |
| Exosome from hUCMSCs | SD Rat (60–80 g) |
CIS (3 μg/ml) |
huMSC-EXOs (20 µg, 100 µg/ml | – |
Alleviate apoptosis level Increase E2 level |
NO Report | [82] |
| C57BL/6–(8 weeks) | CTX (120 mg/kg two times) | huMSC-EXOs (20 μg/mL, 150 μg) | Ip |
Improve the pregnancy rate (Exo 83.33% vs POF 33.33%) Increase FSHR promoted ovarian cells proliferation |
Promoted ovarian granulosa cell (OGCs) Proliferation In Vitro by Regulating the Hippo Pathway and the Effect Was Inhibited by a YAP Inhibitor | [72] | |
| Wistar Rat (50–60 g) |
CIS (4 µg/ml) |
huMSC-EXOs (30 µg/ml | – | promote resistance to apoptosis and protect OGCs from CIS-induced injury in vitro |
huMSC-EXOs could be incorporated into injured OGCs, accelerating the recovery of OGCs Exosomes carry a variety of microRNAs and proteins into target cells |
[83] | |
| Collagen/hUCMSCs | C57BL/6 (6 weeks) | CTX (40 mg/kg for 15 days) | Collagen/UCMSCs (2 × 105/mL) in 10 μL PBS | Orthotopically inject |
Increase E2 and AMH, decrease FSH level; Promote the formation of granulomatous cell, ovarian angiogenesis |
Promote ovarian angiogenesis with the increase of CD31 expression | [73] |
| Matrigel/hUCMSCs | C57BL/6 (8 weeks) |
CTX (1st , 100 mg/kg, 10 mg/kg for 14 days) |
UCMSCs (5 × 105/mL, passages 3–5) in 2.5 μL saline solution + 2.5 μL Matrigel | Orthotopically inject |
Increase the number of follicles and decrease the rate of tissue fibro-degeneration; Increase the proliferation rate of granuloma cells; Increase the number of vascular radiosensitivity |
Decrease the expression of TGFβ-1 Increase the expression of EGF, TGFβ-3 and VEGF-A |
[84] |
| hESC-MSCs | C57BL/6 (6–8 weeks) | CTX (100 mg/kg) + BF (50 mg/kg) | hESC-MSCs (1 × 106 cells) | iv |
Promotes follicle development; Decrease FSH, increase AMH, E2; Restores fertility |
Through paracrine VEGF, IGF-2 and HGF | [69] |
|
ICR or C57BL/DBA (7 weeks) |
CIS (2 mg/kg for 10 days) |
hESC-MSCs (passage 8~10) | iv |
Increase the mean number of primary and primordial follicles, decrease the count of residual zona pellucida (a marker of apoptosis in ovarian follicles), Increase ovulation, embryo formation, and live birth rates |
NO Report | [85] | |
| hPMSCs |
Balb/c (6–8 weeks) |
ZP3 | hPMSCs (1 × 106 cells, passages 6) | iv |
Increased E2 level and decreased FSH and LH levels; Increase follicles and decrease atretic follicles; Inhibit OGCs apoptosis |
By ER stress IRE1α signaling pathway | [27] |
|
Balb/c (7–8 weeks) |
ZP3 | hPMSCs (1 × 106 cells, passages 6) | iv |
Improve Estrous Cycles; Inhibit Ovarian OGCs apoptosis; Increase E2 and FSH Secretion |
Increase CD25+CD4+Treg cell, inflammatory regulations mediated by IFN-g and TGF-b |
[28] | |
| fMSCs |
ICR (7–8 weeks) |
CTX (120 mg/kg for 2 weeks) | fMSCs (1 × 106 cells) | iv |
Increased E2 and AMH level and decreased FSH levels; Increased sinus follicle number; Inhibit apoptosis |
Regulate MT1, JNK1, PCNA and AMPK to reduce the oxidative damage of POI cells, enhance the oxidative protection and improve their anti-apoptosis effect | [86] |
|
ICR (4–6 weeks) |
CTX (200 mg/kg) + BF (20 mg/kg) | fMSCs (5 × 105 cells) in 5μL PBS | Orthotopically inject |
Reduced apoptosis; Increase the number of primordial follicles and decrease the number of atretic follicles |
Exosomal miR-10a derived from fMSCs protect the ovaries | [87] | |
| hAMSCs | C57BL/6 (8 weeks) | Surgery (Hydrogen peroxide burns) | hAECs (1 × 106 cells) in 300 μL PBS | Ip |
Improve the estrous cycle; Decreased FSH levels; Increased the body weight and ovarian; Enhance the fertility Increase the number of primordial follicles and decrease the number of atretic follicles |
Downregulate the expression of TNF-α and IL-1β | [88] |
| C57BL/6 (8 weeks) | CTX (50 mg/kg for 15 days) | hAECs (2 × 106 cells) in 200 μL PBS | iv |
Increased E2 level and decreased FSH level; Increases the number of oocytes; |
NO Report | [89] | |
| Exosome from hAMSCs | C57BL/6 (10 week) | CTX (120 mg/kg for 2 weeks) | hAMSC-Exos (100 μL of PBS containing the 150 μg exosomes) | iv |
Increased follicular numbers; Enhanced the E2 and AMH levels and decreased the FSH levels; Inhibit OGCs apoptosis |
Inhibited the protein expression of SIRT4, ANT2, AMPK, and L-OPA1 | [90] |
| hAECs | C57BL/6 (7–8 weeks) | CTX (120 mg/kg) + BF (30 mg/kg) | hAECs (12 × 106 cells) | iv |
Inhibition of chemotherapy-induced inflammation; Inhibit Ovarian OGCs apoptosis; Increase the number of cumulus oocyte complexes, increase secondary and mature follicles and decrease atretic follicles |
Inhibit TNF-α-mediated cell apoptosis | [91] |
| C57BL/6 (7–8 weeks) | CTX (120 mg/kg) + BF (30 mg/kg) | hAECs (2 × 104 cells) in 10 μL PBS | Orthotopically inject |
Increase secondary and mature follicles and decrease atretic follicles; Increase AMH, MVH, BMP15 and HAS2; Inhibit the apoptosis of primary human granulosa-lutein (hGL) cells; Promote angiogenesis and vasoformation |
Activate TGF-β/Smad pathway in human luteinized OGCs | [92] | |
| ICR mice (7–8 weeks) | CTX (70 mg/kg for 1 weeks + 120 mg/kg for 1 weeks) | hAECs | Orthotopically inject |
Increased E2 and AMH level and decreased FSH levels; Increased ovary weight; Increase secondary and mature follicles and decrease atretic follicles; Increase fertilizing ability; Increase the proliferation rate of OGCs |
NO Report | [71] | |
| Exosome from hAECs |
Mice (7–8 weeks) |
CTX (120 mg/kg) + BF (30 mg/kg) | hAECs Exosome (1st : 9th, orthotopic injection, 10 μL) and 2nd: 10th, tail vein injection, 100 μL)) | Orthotopic injection, iv |
Inhibit OGCs apoptosis; Protect the ovarian vasculature from damage; Maintain the number of primordial follicles |
Transfer functional miRNAs, such as miR-1246 | [93] |
| SA-BG encapsulated hAECs |
Mice (8 weeks) |
CTX (120 mg/kg) + BF (30 mg/kg) | hAECs (6 × 107 cells) in 0.2 mL PBS + 2 mL SA-BG | Orthotopically inject |
promoted the proliferation of granulomatous cells in antral follicles; Enhanced angiogenesis; Promoted the tube formation |
Stimulated the secretion of pro-angiogenic factors | [74] |
hEnSCs human endometrial mesenchymal stem cells, hUCMSCs human umbilical cord mesenchymal stem cells, hESC-MSCs human embryonic stem cell-derived MSCs, hPMSCs human placenta-derived mesenchymal stem cells, hAMSCs human amniotic mesenchymal stem cells, hAECs human amniotic epithelial cells, fMSCs fetal liver mesenchymal stem cell, SA-BG sodium alginate-bioglass
Immunological and gene therapy in POF animal model
In recent years, advances in immunology and genome medicine have improved our understanding of the pathogenesis of POF [94]. An increased number of B cells, CD4+ T cells, Th17 cells, and a decreased CD8+ T cells, Treg cells in POF patients have been reported [95]. Besides, the cytokines (IL-1α, IL-2, IL-6, IL-8, TNF-α, IFN-γ, IL-17 and IL-21) are upregulated [95, 96], and IL-10 is downregulated in POF patients [97]. Based on these advances, many related treatments such as thymopentin (TP-5), Ab4B19, and prednisone have gradually become research hotspots. Zhu et al. demonstrated that thymopentin (TP-5) significantly reduces the proportion of activated T cells (CD3+/CD8+) and M1/M2 macrophages, and the expression of inflammatory factors was decreased [37]. Co-administration of mouse zona pellucida 3 (mZP3) protein in combination with a DNA vaccine encoding the mZP3 gene can meliorate autoimmune ovarian disease through inducing Treg cells and anti-inflammatory cytokine production [98]. A clinical prospective study showed that short-term treatment with a prednisone can increase serum E2 levels and improves follicle growth [99]. However, the study requires a larger sample size.
Currently, most gene therapy research of POF is limited to the cellular and animal levels. These genes, including NEAT1/miR-654, miR-146a, miRNA-190a-5p, miR-146b-5p, miR-133b, and TRERNA1, are transferred into cells to ameliorate the POF symptoms by inhibiting apoptosis of ovarian granulosa cells (OGCs), stimulating estrogen synthesis, increasing the number of normal follicles, and decreasing the number of atretic follicle (Table 6) [100–102]. Gene therapy is still in experimental stage; it is not sure that whether the treatment will have a positive effect on patients.
Table 6.
The immunological and gene therapy in the POF animal model
| Immune agents/genes | POF model | Immunological/gene therapy | Immunological/gene therapy from references | ||||
|---|---|---|---|---|---|---|---|
| Animal | Drug | Method | Treatment | Assessment | Mechanism | ||
| TP-5 | C57BL/6 mice (10 weeks) |
HFHS (High-fat diet 8 g/kg + 200 μL of 30% high fructose syrup once a day via gavage) for 2 m |
TP-5 (5 mg/kg) for 2 m |
Ip |
Decrease atretic follicles Increase ovary weight Increase peripheral blood E2 levels Improve lipid oxidative stress injury and blood lipids Attenuate proportion and activation of CD3+ T cells and type I macrophages |
TP-5 upregulates BMP4/Smad9 signaling pathway to promote the balance and polarization of immune cell, and reduces the release of inflammatory factors and lipid oxidative stress injury | [37] |
| TrkB agonist antibody (Ab4B19) |
C57BL/6 mice (6–8 w) |
CTX (a single, 75 mg/kg, 200–300 μL) for 7 days |
Ab4B19 (1 mg/kg), once every 4 days, for 16 days |
iv |
Promote oocyte maturation and follicle development Attenuate ovarian degradation Normalize gonadal hormone Inhibit apoptosis Enhance fertility |
NO Report | [30] |
| pcD-mZP3 + mZP3 protein vaccine |
C57BL/6 mice (8–10 weeks) |
mZP3 (0.1 ml of 100 µg of CFA emulsified mZP3) | 100 µg DNA and 100 µg protein vaccines per mouse | - |
Ameliorate autoimmune ovarian disease Promote anti-inflammatory function Down-regulate the antigen-specific T-cell responses Induce adaptive Tr cells |
The induction of the CD4+CD25−Foxp3+IL-10+ Treg cells suppress mZP3 antigen-specific T cell responses in vitro with decreasing the anti-inflammatory cytokine production | [98] |
| Prednisone | POF patients | – | 25 mg four times per day for 2 weeks | – | 2/11 patients demonstrated biochemical normalization, evidence of follicular growth by a rise of E2, and visualization on ultrasonography, and both spontaneously ovulated, conceived, had uneventful pregnancies, and delivered healthy children | NO Report | [99] |
| NEAT1/miR-654 |
C57BL/6 mice (8 weeks) |
CTX (30 mg/kg every other day for 3 weeks) | – | Cell transfection | Eliminates the promoting effect of CTX on OGC apoptosis and autophagy | NEAT1 overexpression inhibits miR-654 and further regulates STC2/MAPK pathway | [103] |
| miR-146a | OGCs | – | 80 nM miR‑146a inhibitor/wk | Cell transfection | Inhibit granulosa cell apoptosis | Attenuates the activation of miR‑146a/IRAK1/TRAF6/caspase‑8 signaling | [104] |
| miRNA-190a-5p |
SD rats (12 weeks, 200 ± 20 g) |
VCD (80 mg/kg/d for 15 days ) | No treatment | Promotes primordial follicle hyperactivation | miRNA-190a-5p inhibits the expression of PHLPP1 and key proteins in the AKT-FOXO3a and AKT-LH/LHR pathways | [105] | |
| miR-146b-5p | C57BL/6 mice (10 weeks) | HFHS diet (8 g/kg bodyweight + 400 μL of 30% d-glucose for 30 days ) | 400 μL of miR-146@ PLGA (20 mg/mL) once every 3 days | iv |
Mitigates the HFHS-induced oxidative stress injury and aging in OGCs Increase ovary weight Increase the number of normal follicles, decrease the number of atretic follicle Increase the peripheral blood levels of estradiol, progesterone and 17α-hydroxy pregnenolone Decrease the peripheral blood levels of testosterone and dihydrotestosterone |
miR-146b-5p overexpression attenuates the activation of the Dab2ip/Ask1/p38-Mapk signaling pathway and γH2A.X phosphorylation | [100] |
| miR-133b | ICR mice (21 days ) | – | – | Cell transfection | Stimulates estrogen synthesis in OGCs | miR-133b down-regulates Foxl2 expression in OGCs by directly targeting the 30UTR, and inhibits the Foxl2-mediated transcriptional repression of StAR and CYP19A1 | [101] |
| TRERNA1 | KGN cells | – | 10 mM TRERNA1 vector/107 cells | Cell transfection | Inhibit KGN cells apoptosis | TRERNA1 may sponge miR-23a to suppress OGCs apoptosis in POF | [102] |
TP-5 thymopentin, HFHS high-fat diet, TGs tripterygium glycosides, OGCs ovarian granular cells, VCD 4-vinylcyclohexene dicyclic oxide, HFHS high-fat diet, VCD 4-vinylcyclohexene diepoxide
Conclusion
Suitable and ideal POF animal models are essential carriers for drug development and mechanism research. Chemotherapy drug model is a classic animal model for studying POF. However, chemotherapy-induced POF animal model may exist many side effects, including myelosuppression and bleeding. POF animal model from autoimmunity and mental stress is the largest relationship with the etiology of POF, but the stability of the model needs to be further determined. GAL-induced animal model can better simulate the physiological aging characteristics of clinical POF patients, but the success rate is lower and the cycle time is longer. Hence, the study of the mechanism of POF and drug efficacy should select appropriate models according to the main purpose of the study. An ideal animal model would have the following characteristics: (1) the pathogenic pathways and processes like those observed in humans; (2) the pathological changes in the model can be reversed by drugs; (3) the reproducibility of the results [106]. In the future, a model of POF constructed by injection of chemotherapy drugs and GAL under ultrasound guidance may reduce side effects and improve model success rate. Besides, more efforts should be made to study aging-related POF. For example, constructing aging-induced animal model studies the role of MSCs and their exosomes in restoring ovarian function.
The breakthrough discovery of MSCs makes them an ideal source for POF therapy. Many animal and preclinical studies of MSCs for POF treatment have been conducted; the clinical application of MSCs has big challenges, including insufficient cell sourcing, immunogenicity, subculture, and ethical issues. In addition, the long-term survival and self-renewal of stem cells in ovarian tissue remain to be further studied. In the future, it is necessary to establish a professional quality inspection system of MSC production to ensure the functional potential and microbiological safety of MSCs. More importantly, multicenter, large-sample phase II or III trials are expected to confirm the therapeutic and safety effect of stem cells on POF rather than just POF animal models. Especially, it is also worth considering whether the regenerative properties of MSCs can stimulate tumor regeneration in the future. Exosomes is smaller, easier to produce, and can carry various microRNAs and proteins into target cells without risk of tumor formation [72]. Moreover, stem cell tissue engineering is also an effective strategy. Sodium alginate-bioglass (SA-BG)-encapsulated MSCs can support the survival of the transplanted cells at the initial phase of transplantation [74]. Moreover, the combination of stem cells with other therapies (such as gene and immunotherapy) should be actively explored to promote the treatment of POF in the future.
Acknowledgements
Not applicable.
Abbreviations
- POF
Premature ovarian failure
- POI
Premature insufficient ovarian failure
- GAL
Galactose
- AMH
Anti-Müllerian hormone
- GH
Growth hormone
- CTX
Cyclophosphamide
- BF
Busulfan
- CIS
Cisplatinum
- DOX
Doxorubicin
- TG
Tripterygium glycosides
- FSH
Follicle-stimulating hormone
- LH
Luteinizing hormone
- E2
Estrogen
- HRT
Hormone replacement therapy
- ZP3
Zona pellucida 3
- CUMS
Constructed chronic unpredictable mild stress
- FSHR
Follicle-stimulating hormone receptor
- rmGH
Recombinant mouse GH
- MSCs
Mesenchymal stem cells
- BMSCs
Bone marrow mesenchymal stem cells
- ADMSCs
Adipose-derived mesenchymal stem cells
- HuMenSCs
Human menstrual-derived stem cells
- hEnSCs
Human endometrial mesenchymal stem cells
- hUCMSCs
Human umbilical cord mesenchymal stem cells
- hESC-MSCs
Human embryonic stem cell-derived MSCs
- hPMSCs
Human placenta-derived mesenchymal stem cells
- hAMSCs
Human amniotic mesenchymal stem cells
- hAECs
Human amniotic epithelial cells
- fMSCs
Fetal liver mesenchymal stem cells
- TGF-β
Transforming growth factor-beta
- VEGF
Vascular endothelial growth factor
- EGF
Epidermal growth factor
- IGF2
Insulin-like growth factor 2
- HGF
Human growth factor
Author contributions
FFD, YXC, and RQW designed the study and reviewed the manuscript. FFD was responsible for the first draft of the manuscript. ZMD, DYY, LLW, and MLW were responsible for the concept of the review. RQW and ZMD prepared figures. WH and YXC revised the manuscript. All authors read and approved the final version of the manuscript.
Funding
This research was funded by Key Research and Development Program of Hubei Province (2020BCB023); the National Natural Science Foundation of China, grant number (82071655, 81860276); Young Teacher Qualification Project of the Fundamental Research Funds for the Central Universities (2042020kf0088).
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Fangfang Dai, Ruiqi Wang and Zhimin Deng have contributed equally to this work and share first authorship
Contributor Information
Wei Hu, Email: hwdoct@163.com.
Yanxiang Cheng, Email: yanxiangcheng@whu.edu.cn.
References
- 1.Zhang C. The roles of different stem cells in premature ovarian failure. Curr Stem Cell Res Ther. 2020;15(6):473–481. doi: 10.2174/1574888X14666190314123006. [DOI] [PubMed] [Google Scholar]
- 2.Szeliga A, et al. Autoimmune diseases in patients with premature ovarian insufficiency-our current state of knowledge. Int J Mol Sci. 2021 doi: 10.3390/ijms22052594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Armeni E, et al. Hormone therapy regimens for managing the menopause and premature ovarian insufficiency. Best Pract Res Clin Endocrinol Metab. 2021;35(6):101561. doi: 10.1016/j.beem.2021.101561. [DOI] [PubMed] [Google Scholar]
- 4.Shareghi-Oskoue O, et al. Transplantation of human umbilical cord mesenchymal stem cells to treat premature ovarian failure. Stem Cell Res Ther. 2021;12(1):454. doi: 10.1186/s13287-021-02529-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fu YX, et al. Human mesenchymal stem cell treatment of premature ovarian failure: new challenges and opportunities. Stem Cell Res Ther. 2021;12(1):161. doi: 10.1186/s13287-021-02212-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guerreiro DD, et al. In situ cultured preantral follicles is a useful model to evaluate the effect of anticancer drugs on caprine folliculogenesis. Microsc Res Tech. 2016;79(8):773–781. doi: 10.1002/jemt.22697. [DOI] [PubMed] [Google Scholar]
- 7.Long JP, et al. DTC chemotherapy regimen is associated with higher incidence of premature ovarian failure in women of reproductive age with breast cancer. Eur Rev Med Pharmacol Sci. 2016;20(6):1087–1092. [PubMed] [Google Scholar]
- 8.Mauri D, et al. Chemotherapy associated ovarian failure. Front Endocrinol (Lausanne) 2020;11:572388. doi: 10.3389/fendo.2020.572388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blumenfeld Z, et al. Preservation of fertility and ovarian function and minimization of chemotherapy-induced gonadotoxicity in young women by GnRH-a. J Natl Cancer Inst Monogr. 2005;34:40–43. doi: 10.1093/jncimonographs/lgi015. [DOI] [PubMed] [Google Scholar]
- 10.Fu Y, et al. Therapeutic mechanisms of Tongmai Dasheng Tablet on tripterygium glycosides induced rat model for premature ovarian failure. J Ethnopharmacol. 2012;139(1):26–33. doi: 10.1016/j.jep.2011.08.077. [DOI] [PubMed] [Google Scholar]
- 11.Ben-Aharon I, et al. Doxorubicin-induced ovarian toxicity. Reprod Biol Endocrinol. 2010;8:20. doi: 10.1186/1477-7827-8-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Setiady YY, et al. Maternal autoantibody triggers de novo T cell-mediated neonatal autoimmune disease. J Immunol. 2003;170(9):4656–4664. doi: 10.4049/jimmunol.170.9.4656. [DOI] [PubMed] [Google Scholar]
- 13.Wang Z, et al. Mesenchymal stem cell therapy using human umbilical cord in a rat model of autoimmune-induced premature ovarian failure. Stem Cells Int. 2020;2020:3249495. doi: 10.1155/2020/3249495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tong ZB, et al. A mouse gene encoding an oocyte antigen associated with autoimmune premature ovarian failure. Endocrinology. 1999;140(8):3720–3726. doi: 10.1210/endo.140.8.6911. [DOI] [PubMed] [Google Scholar]
- 15.Wang XF, et al. Biological mechanisms of premature ovarian failure caused by psychological stress based on support vector regression. Int J Clin Exp Med. 2015;8(11):21393–21399. [PMC free article] [PubMed] [Google Scholar]
- 16.Fu XY, et al. Effects of chronic unpredictable mild stress on ovarian reserve in female rats: Feasibility analysis of a rat model of premature ovarian failure. Mol Med Rep. 2018;18(1):532–540. doi: 10.3892/mmr.2018.8989. [DOI] [PubMed] [Google Scholar]
- 17.Azman KF, et al. D-Galactose-induced accelerated aging model: an overview. Biogerontology. 2019;20(6):763–782. doi: 10.1007/s10522-019-09837-y. [DOI] [PubMed] [Google Scholar]
- 18.Bandyopadhyay S, et al. Galactose toxicity in the rat as a model for premature ovarian failure: an experimental approach readdressed. Hum Reprod. 2003;18(10):2031–2038. doi: 10.1093/humrep/deg414. [DOI] [PubMed] [Google Scholar]
- 19.Liu G, et al. Galactose metabolism and ovarian toxicity. Reprod Toxicol. 2000;14(5):377–384. doi: 10.1016/s0890-6238(00)00096-4. [DOI] [PubMed] [Google Scholar]
- 20.He L, et al. Ginsenoside Rg1 improves fertility and reduces ovarian pathological damages in premature ovarian failure model of mice. Exp Biol Med (Maywood) 2017;242(7):683–691. doi: 10.1177/1535370217693323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fu X, et al. Overexpression of miR-21 in stem cells improves ovarian structure and function in rats with chemotherapy-induced ovarian damage by targeting PDCD4 and PTEN to inhibit granulosa cell apoptosis. Stem Cell Res Ther. 2017;8(1):187. doi: 10.1186/s13287-017-0641-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu J, et al. Homing and restorative effects of bone marrow-derived mesenchymal stem cells on cisplatin injured ovaries in rats. Mol Cells. 2014;37(12):865–872. doi: 10.14348/molcells.2014.0145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yang M, et al. Bone marrow mesenchymal stem cell-derived exosomal miR-144-5p improves rat ovarian function after chemotherapy-induced ovarian failure by targeting PTEN. Lab Invest. 2020;100(3):342–352. doi: 10.1038/s41374-019-0321-y. [DOI] [PubMed] [Google Scholar]
- 24.Peng H, et al. Zuogui Pills inhibit mitochondria-dependent apoptosis of follicles in a rat model of premature ovarian failure. J Ethnopharmacol. 2019;238:111855. doi: 10.1016/j.jep.2019.111855. [DOI] [PubMed] [Google Scholar]
- 25.Jiang HL, et al. Protective effects ROS up-regulation on premature ovarian failure by suppressing ROS-TERT signal pathway. Eur Rev Med Pharmacol Sci. 2018;22(19):6198–6204. doi: 10.26355/eurrev_201810_16025. [DOI] [PubMed] [Google Scholar]
- 26.Li D, et al. Differentially expressed genes in cisplatin-induced premature ovarian failure in rats. Anim Reprod Sci. 2013;137(3–4):205–213. doi: 10.1016/j.anireprosci.2012.11.011. [DOI] [PubMed] [Google Scholar]
- 27.Li H, et al. Human placenta-derived mesenchymal stem cells inhibit apoptosis of granulosa cells induced by IRE1alpha pathway in autoimmune POF mice. Cell Biol Int. 2019;43(8):899–909. doi: 10.1002/cbin.11165. [DOI] [PubMed] [Google Scholar]
- 28.Yin N, et al. Restoring Ovarian Function With Human Placenta-Derived Mesenchymal Stem Cells in Autoimmune-Induced Premature Ovarian Failure Mice Mediated by Treg Cells and Associated Cytokines. Reprod Sci. 2018;25(7):1073–1082. doi: 10.1177/1933719117732156. [DOI] [PubMed] [Google Scholar]
- 29.中国实验动物学会 (英文) %J Animal Models and Experimental Medicine. 2021;4(04):426
- 30.Qin X, et al. TrkB agonist antibody ameliorates fertility deficits in aged and cyclophosphamide-induced premature ovarian failure model mice. Nat Commun. 2022;13(1):914. doi: 10.1038/s41467-022-28611-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cao LB, et al. Systemic changes in a mouse model of VCD-induced premature ovarian failure. Life Sci. 2020;262:118543. doi: 10.1016/j.lfs.2020.118543. [DOI] [PubMed] [Google Scholar]
- 32.Cedars MI. Evaluation of female fertility-AMH and ovarian reserve testing. J Clin Endocrinol Metab. 2022;107(6):1510–1519. doi: 10.1210/clinem/dgac039. [DOI] [PubMed] [Google Scholar]
- 33.Liu Z, et al. Esculentoside A rescues granulosa cell apoptosis and folliculogenesis in mice with premature ovarian failure. Aging (Albany NY) 2020;12(17):16951–16962. doi: 10.18632/aging.103609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moolhuijsen LME, et al. Anti-Mullerian hormone and ovarian reserve: update on assessing ovarian function. J Clin Endocrinol Metab. 2020;105(11):3361–3373. doi: 10.1210/clinem/dgaa513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang H, et al. Effects of hPMSCs on granulosa cell apoptosis and AMH expression and their role in the restoration of ovary function in premature ovarian failure mice. Stem Cell Res Ther. 2018;9(1):20. doi: 10.1186/s13287-017-0745-5. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 36.Liu H, et al. A novel homozygous mutation in the FSHR gene is causative for primary ovarian insufficiency. Fertil Steril. 2017;108(6):1050–1055 e1052. doi: 10.1016/j.fertnstert.2017.09.010. [DOI] [PubMed] [Google Scholar]
- 37.Zhu X, et al. Thymopentin treatment of murine premature ovarian failure via attenuation of immune cell activity and promotion of the BMP4/Smad9 signalling pathway. Int J Med Sci. 2021;18(15):3544–3555. doi: 10.7150/ijms.61975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sonigo C, et al. AMH prevents primordial ovarian follicle loss and fertility alteration in cyclophosphamide-treated mice. FASEB J. 2019;33(1):1278–1287. doi: 10.1096/fj.201801089R. [DOI] [PubMed] [Google Scholar]
- 39.Tordjman S, et al. Melatonin: Pharmacology, Functions and Therapeutic Benefits. Curr Neuropharmacol. 2017;15(3):434–443. doi: 10.2174/1570159X14666161228122115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tamtaji OR, et al. Melatonin, a calpain inhibitor in the central nervous system: Current status and future perspectives. J Cell Physiol. 2019;234(2):1001–1007. doi: 10.1002/jcp.27084. [DOI] [PubMed] [Google Scholar]
- 41.Tamura H, et al. Melatonin as a free radical scavenger in the ovarian follicle. Endocr J. 2013;60(1):1–13. doi: 10.1507/endocrj.ej12-0263. [DOI] [PubMed] [Google Scholar]
- 42.Jang H, et al. Melatonin prevents cisplatin-induced primordial follicle loss via suppression of PTEN/AKT/FOXO3a pathway activation in the mouse ovary. J Pineal Res. 2016;60(3):336–347. doi: 10.1111/jpi.12316. [DOI] [PubMed] [Google Scholar]
- 43.Ma M, et al. Melatonin protects premature ovarian insufficiency induced by tripterygium glycosides: role of SIRT1. Am J Transl Res. 2017;9(4):1580–1602. [PMC free article] [PubMed] [Google Scholar]
- 44.Liu TE, et al. Growth hormone treatment of premature ovarian failure in a mouse model via stimulation of the Notch-1 signaling pathway. Exp Ther Med. 2016;12(1):215–221. doi: 10.3892/etm.2016.3326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Feng P, et al. Study on the reparative effect of PEGylated growth hormone on ovarian parameters and mitochondrial function of oocytes from rats with premature ovarian insufficiency. Front Cell Dev Biol. 2021;9:649005. doi: 10.3389/fcell.2021.649005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Huang J, et al. Melatonin provides protection against cisplatin-induced ovarian damage and loss of fertility in mice. Reprod Biomed Online. 2021;42(3):505–519. doi: 10.1016/j.rbmo.2020.10.001. [DOI] [PubMed] [Google Scholar]
- 47.Pittenger MF, et al. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284(5411):143–147. doi: 10.1126/science.284.5411.143. [DOI] [PubMed] [Google Scholar]
- 48.He Y, et al. The therapeutic potential of bone marrow mesenchymal stem cells in premature ovarian failure. Stem Cell Res Ther. 2018;9(1):263. doi: 10.1186/s13287-018-1008-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.McIntosh KR. Evaluation of cellular and humoral immune responses to allogeneic adipose-derived stem/stromal cells. Methods Mol Biol. 2011;702:133–150. doi: 10.1007/978-1-61737-960-4_11. [DOI] [PubMed] [Google Scholar]
- 50.Bourin P, et al. Stromal cells from the adipose tissue-derived stromal vascular fraction and culture expanded adipose tissue-derived stromal/stem cells: a joint statement of the International Federation for Adipose Therapeutics and Science (IFATS) and the International Society for Cellular Therapy (ISCT) Cytotherapy. 2013;15(6):641–648. doi: 10.1016/j.jcyt.2013.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Griffiths MJ, et al. Stem cells of the alveolar epithelium. Lancet. 2005;366(9481):249–260. doi: 10.1016/S0140-6736(05)66916-4. [DOI] [PubMed] [Google Scholar]
- 52.Mazini L, et al. Regenerative capacity of adipose derived stem cells (ADSCs), comparison with mesenchymal stem cells (MSCs) Int J Mol Sci. 2019 doi: 10.3390/ijms20102523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gargett CE. Stem cells in gynaecology. Aust N Z J Obstet Gynaecol. 2004;44(5):380–386. doi: 10.1111/j.1479-828X.2004.00290.x. [DOI] [PubMed] [Google Scholar]
- 54.Santamaria X, et al. Derivation of insulin producing cells from human endometrial stromal stem cells and use in the treatment of murine diabetes. Mol Ther. 2011;19(11):2065–2071. doi: 10.1038/mt.2011.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhang Z, et al. Menstrual blood derived mesenchymal cells ameliorate cardiac fibrosis via inhibition of endothelial to mesenchymal transition in myocardial infarction. Int J Cardiol. 2013;168(2):1711–1714. doi: 10.1016/j.ijcard.2013.03.126. [DOI] [PubMed] [Google Scholar]
- 56.Chen L, et al. Human menstrual blood-derived stem cells ameliorate liver fibrosis in mice by targeting hepatic stellate cells via paracrine mediators. Stem Cells Transl Med. 2017;6(1):272–284. doi: 10.5966/sctm.2015-0265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lai D, et al. Human endometrial mesenchymal stem cells restore ovarian function through improving the renewal of germline stem cells in a mouse model of premature ovarian failure. J Transl Med. 2015;13:155. doi: 10.1186/s12967-015-0516-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Noory P, et al. Human menstrual blood stem cell-derived granulosa cells participate in ovarian follicle formation in a rat model of premature ovarian failure in vivo. Cell Reprogram. 2019;21(5):249–259. doi: 10.1089/cell.2019.0020. [DOI] [PubMed] [Google Scholar]
- 59.El-Derany MO, et al. Bone marrow-derived mesenchymal stem cells reverse radiotherapy-induced premature ovarian failure: emphasis on signal integration of TGF-beta, Wnt/beta-catenin and hippo pathways. Stem Cell Rev Rep. 2021;17(4):1429–1445. doi: 10.1007/s12015-021-10135-9. [DOI] [PubMed] [Google Scholar]
- 60.Sun B, et al. miR-644-5p carried by bone mesenchymal stem cell-derived exosomes targets regulation of p53 to inhibit ovarian granulosa cell apoptosis. Stem Cell Res Ther. 2019;10(1):360. doi: 10.1186/s13287-019-1442-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sen Halicioglu B, et al. Adipose-derived mesenchymal stem cell transplantation in chemotherapy-induced premature ovarian insufficiency: the role of connexin and pannexin. Reprod Sci. 2022;29(4):1316–1331. doi: 10.1007/s43032-021-00718-9. [DOI] [PubMed] [Google Scholar]
- 62.Huang B, et al. Exosomes derived from human adipose mesenchymal stem cells improve ovary function of premature ovarian insufficiency by targeting SMAD. Stem Cell Res Ther. 2018;9(1):216. doi: 10.1186/s13287-018-0953-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wang Z, et al. Study of the reparative effects of menstrual-derived stem cells on premature ovarian failure in mice. Stem Cell Res Ther. 2017;8(1):11. doi: 10.1186/s13287-016-0458-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Manshadi MD, et al. The effects of human menstrual blood stem cells-derived granulosa cells on ovarian follicle formation in a rat model of premature ovarian failure. Microsc Res Tech. 2019;82(6):635–642. doi: 10.1002/jemt.23120. [DOI] [PubMed] [Google Scholar]
- 65.Hass R, et al. Different populations and sources of human mesenchymal stem cells (MSC): A comparison of adult and neonatal tissue-derived MSC. Cell Commun Signal. 2011;9:12. doi: 10.1186/1478-811X-9-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mebarki M, et al. Human umbilical cord-derived mesenchymal stem/stromal cells: a promising candidate for the development of advanced therapy medicinal products. Stem Cell Res Ther. 2021;12(1):152. doi: 10.1186/s13287-021-02222-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mardpour S, et al. Extracellular vesicles derived from human embryonic stem cell-MSCs ameliorate cirrhosis in thioacetamide-induced chronic liver injury. J Cell Physiol. 2018;233(12):9330–9344. doi: 10.1002/jcp.26413. [DOI] [PubMed] [Google Scholar]
- 68.Lotfinia M, et al. Effect of secreted molecules of human embryonic stem cell-derived mesenchymal stem cells on acute hepatic failure model. Stem Cells Dev. 2016;25(24):1898–1908. doi: 10.1089/scd.2016.0244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bahrehbar K, et al. Human embryonic stem cell-derived mesenchymal stem cells improved premature ovarian failure. World J Stem Cells. 2020;12(8):857–878. doi: 10.4252/wjsc.v12.i8.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lee HJ, et al. Comparison of in vitro hepatogenic differentiation potential between various placenta-derived stem cells and other adult stem cells as an alternative source of functional hepatocytes. Differentiation. 2012;84(3):223–231. doi: 10.1016/j.diff.2012.05.007. [DOI] [PubMed] [Google Scholar]
- 71.Ding C, et al. Different therapeutic effects of cells derived from human amniotic membrane on premature ovarian aging depend on distinct cellular biological characteristics. Stem Cell Res Ther. 2017;8(1):173. doi: 10.1186/s13287-017-0613-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Li Z, et al. Human umbilical cord mesenchymal stem cell-derived exosomes improve ovarian function and proliferation of premature ovarian insufficiency by regulating the hippo signaling pathway. Front Endocrinol (Lausanne) 2021;12:711902. doi: 10.3389/fendo.2021.711902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yang Y, et al. Transplantation of umbilical cord-derived mesenchymal stem cells on a collagen scaffold improves ovarian function in a premature ovarian failure model of mice. In Vitro Cell Dev Biol Anim. 2019;55(4):302–311. doi: 10.1007/s11626-019-00337-4. [DOI] [PubMed] [Google Scholar]
- 74.Huang Y, et al. Sodium alginate-bioglass-encapsulated hAECs restore ovarian function in premature ovarian failure by stimulating angiogenic factor secretion. Stem Cell Res Ther. 2021;12(1):223. doi: 10.1186/s13287-021-02280-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Song D, et al. Human umbilical cord mesenchymal stem cells therapy in cyclophosphamide-induced premature ovarian failure rat model. Biomed Res Int. 2016;2016:2517514. doi: 10.1155/2016/2517514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Deng T, et al. Human umbilical cord mesenchymal stem cells improve ovarian function in chemotherapy-induced premature ovarian failure mice through inhibiting apoptosis and inflammation via a paracrine mechanism. Reprod Sci. 2021;28(6):1718–1732. doi: 10.1007/s43032-021-00499-1. [DOI] [PubMed] [Google Scholar]
- 77.Lu X, et al. The effects of human umbilical cord-derived mesenchymal stem cell transplantation on endometrial receptivity are associated with Th1/Th2 balance change and uNK cell expression of uterine in autoimmune premature ovarian failure mice. Stem Cell Res Ther. 2019;10(1):214. doi: 10.1186/s13287-019-1313-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zheng Q, et al. Umbilical cord mesenchymal stem cell transplantation prevents chemotherapy-induced ovarian failure via the NGF/TrkA pathway in rats. Biomed Res Int. 2019;2019:6539294. doi: 10.1155/2019/6539294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Elfayomy AK, et al. Human umbilical cord blood-mesenchymal stem cells transplantation renovates the ovarian surface epithelium in a rat model of premature ovarian failure: Possible direct and indirect effects. Tissue Cell. 2016;48(4):370–382. doi: 10.1016/j.tice.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 80.Zhang L, et al. Comparison of CD146+/− mesenchymal stem cells in improving premature ovarian failure. Stem Cell Res Ther. 2022;13(1):267. doi: 10.1186/s13287-022-02916-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mohamed SA, et al. Umbilical cord blood mesenchymal stem cells as an infertility treatment for chemotherapy induced premature ovarian insufficiency. Biomedicines. 2019 doi: 10.3390/biomedicines7010007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zhang J, et al. The protective effects of human umbilical cord mesenchymal stem cell-derived extracellular vesicles on cisplatin-damaged granulosa cells. Taiwan J Obstet Gynecol. 2020;59(4):527–533. doi: 10.1016/j.tjog.2020.05.010. [DOI] [PubMed] [Google Scholar]
- 83.Sun L, et al. Exosomes derived from human umbilical cord mesenchymal stem cells protect against cisplatin-induced ovarian granulosa cell stress and apoptosis in vitro. Sci Rep. 2017;7(1):2552. doi: 10.1038/s41598-017-02786-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhou Y, et al. Matrigel/umbilical cord-derived mesenchymal stem cells promote granulosa cell proliferation and ovarian vascularization in a mouse model of premature ovarian failure. Stem Cells Dev. 2021;30(15):782–796. doi: 10.1089/scd.2021.0005. [DOI] [PubMed] [Google Scholar]
- 85.Yoon SY, et al. Recovery of ovarian function by human embryonic stem cell-derived mesenchymal stem cells in cisplatin-induced premature ovarian failure in mice. Stem Cell Res Ther. 2020;11(1):255. doi: 10.1186/s13287-020-01769-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Huang B, et al. Fetal liver mesenchymal stem cells restore ovarian function in premature ovarian insufficiency by targeting MT1. Stem Cell Res Ther. 2019;10(1):362. doi: 10.1186/s13287-019-1490-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Xiao GY, et al. Exosomal miR-10a derived from amniotic fluid stem cells preserves ovarian follicles after chemotherapy. Sci Rep. 2016;6:23120. doi: 10.1038/srep23120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Liu R, et al. Human amniotic mesenchymal stem cells improve the follicular microenvironment to recover ovarian function in premature ovarian failure mice. Stem Cell Res Ther. 2019;10(1):299. doi: 10.1186/s13287-019-1315-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Li J, et al. Human chorionic plate-derived mesenchymal stem cells transplantation restores ovarian function in a chemotherapy-induced mouse model of premature ovarian failure. Stem Cell Res Ther. 2018;9(1):81. doi: 10.1186/s13287-018-0819-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ding C, et al. Exosomal miRNA-320a is released from hAMSCs and regulates SIRT4 to prevent reactive oxygen species generation in POI. Mol Ther Nucleic Acids. 2020;21:37–50. doi: 10.1016/j.omtn.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Zhang Q, et al. Human amniotic epithelial cells inhibit granulosa cell apoptosis induced by chemotherapy and restore the fertility. Stem Cell Res Ther. 2015;6:152. doi: 10.1186/s13287-015-0148-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Zhang Q, et al. Paracrine effects of human amniotic epithelial cells protect against chemotherapy-induced ovarian damage. Stem Cell Res Ther. 2017;8(1):270. doi: 10.1186/s13287-017-0721-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Zhang Q, et al. Human amniotic epithelial cell-derived exosomes restore ovarian function by transferring MicroRNAs against apoptosis. Mol Ther Nucleic Acids. 2019;16:407–418. doi: 10.1016/j.omtn.2019.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Atabiekov I, et al. The role of gene therapy in premature ovarian insufficiency management. Biomedicines. 2018 doi: 10.3390/biomedicines6040102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Gao H, et al. Advances in the cellular immunological pathogenesis and related treatment of primary ovarian insufficiency. Am J Reprod Immunol. 2022;88(5):e13622. doi: 10.1111/aji.13622. [DOI] [PubMed] [Google Scholar]
- 96.Liu P, et al. Dysregulated cytokine profile associated with biochemical premature ovarian insufficiency. Am J Reprod Immunol. 2020;84(4):e13292. doi: 10.1111/aji.13292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Iyer SS, et al. Role of interleukin 10 transcriptional regulation in inflammation and autoimmune disease. Crit Rev Immunol. 2012;32(1):23–63. doi: 10.1615/critrevimmunol.v32.i1.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Li J, et al. Treatment of autoimmune ovarian disease by co-administration with mouse zona pellucida protein 3 and DNA vaccine through induction of adaptive regulatory T cells. J Gene Med. 2008;10(7):810–820. doi: 10.1002/jgm.1200. [DOI] [PubMed] [Google Scholar]
- 99.Corenblum B, et al. High-dose, short-term glucocorticoids for the treatment of infertility resulting from premature ovarian failure. Fertil Steril. 1993;59(5):988–991. doi: 10.1016/s0015-0282(16)55915-9. [DOI] [PubMed] [Google Scholar]
- 100.Liu T, et al. MicroRNA-146b-5p overexpression attenuates premature ovarian failure in mice by inhibiting the Dab2ip/Ask1/p38-Mapk pathway and gammaH2A.X phosphorylation. Cell Prolif. 2021;54(1):12954. doi: 10.1111/cpr.12954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Dai A, et al. MicroRNA-133b stimulates ovarian estradiol synthesis by targeting Foxl2. FEBS Lett. 2013;587(15):2474–2482. doi: 10.1016/j.febslet.2013.06.023. [DOI] [PubMed] [Google Scholar]
- 102.Zhang L, et al. Translation regulatory long non-coding RNA 1 (TRERNA1) sponges microRNA-23a to suppress granulosa cell apoptosis in premature ovarian failure. Bioengineered. 2022;13(2):2173–2180. doi: 10.1080/21655979.2021.2023802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Liu YX, et al. LncRNA NEAT1 inhibits apoptosis and autophagy of ovarian granulosa cells through miR-654/STC2-mediated MAPK signaling pathway. Exp Cell Res. 2023;424(1):113473. doi: 10.1016/j.yexcr.2023.113473. [DOI] [PubMed] [Google Scholar]
- 104.Filali-Mouncef Y, et al. The menage a trois of autophagy, lipid droplets and liver disease. Autophagy. 2022;18(1):50–72. doi: 10.1080/15548627.2021.1895658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Zhang Y, et al. MiRNA-190a-5p promotes primordial follicle hyperactivation by targeting PHLPP1 in premature ovarian failure. Front Genet. 2022;13:1034832. doi: 10.3389/fgene.2022.1034832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lewis DI. Animal experimentation: implementation and application of the 3Rs. Emerg Top Life Sci. 2019;3(6):675–679. doi: 10.1042/ETLS20190061. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.