Abstract
Family planning researchers have traditionally focused efforts on understanding contraceptive non-use and promoting contraceptive uptake. Recently, however, more scholars have been exploring method dissatisfaction, questioning the assumption that contraceptive users necessarily have their needs met. Here, we introduce the concept of “non-preferred method use”, which we define as the use of one contraceptive method while having the desire to use a different method. Non-preferred method use reflects barriers to contraceptive autonomy and may contribute to method discontinuation. We use survey data collected from 2017 to 2018 to better understand non-preferred contraceptive method use among 1210 reproductive-aged family planning users in Burkina Faso. We operationalise non-preferred method use as both (1) use of a method that was not the user’s original preference and (2) use of a method while reporting preference for another method. Using these two approaches, we describe the prevalence of non-preferred method use, reasons for using non-preferred methods, and patterns in non-preferred method use by current and preferred methods. We find that 7% of respondents reported using a method they did not desire at the time of adoption, 33% would use a different method if they could and 37% report at least one form of non-preferred method use. Many women cite facility-level barriers, such as providers refusing to give them their preferred method, as reasons for non-preferred method use. The high prevalence of non-preferred method use reflects the obstacles that women face when attempting to fulfil their contraceptive desires. Further research on reasons for use of non-preferred methods is necessary to promote contraceptive autonomy.
Keywords: reproductive health, family planning, contraceptive autonomy, method dissatisfaction, non-preferred method use
Résumé
Les chercheurs en matière de planification familiale ont jusqu’à présent centré leurs activités sur la compréhension de la non-utilisation de contraceptifs et la promotion du recours à la contraception. Pourtant, récemment, davantage de spécialistes ont étudié l’insatisfaction quant aux méthodes, en remettant en question le postulat selon lequel les besoins des utilisateurs de contraceptifs sont nécessairement satisfaits. Ici, nous présentons le concept « d’utilisation d’une méthode non préférée », que nous définissons comme l’utilisation d’une méthode contraceptive tout en souhaitant en utiliser une autre. L’utilisation d’une méthode non préférée reflète les obstacles à l’autonomie contraceptive et peut contribuer à l’abandon de la méthode. Nous utilisons des données d’enquête collectionnées de 2017 à 2018 pour mieux comprendre l’utilisation d’une méthode contraceptive non préférée parmi 1210 utilisateurs de planification familiale en âge de procréer au Burkina Faso. Nous opérationnalisons l’utilisation d’une méthode non préférée comme 1) l’utilisation d’une méthode qui n’était pas la préférence initiale de l’utilisation et 2) l’utilisation d’une méthode tout en faisant état de la préférence pour une autre méthode. À l’aide de ces deux approches, nous décrivons la prévalence de l’utilisation d’une méthode non préférée, les raisons de cette utilisation et les modalités dans l’utilisation d’une méthode non préférée par méthode actuelle et préférée. Nous avons observé que 7% des répondants indiquaient utiliser une méthode qu’ils ne souhaitaient pas au moment de l’adoption, 33% utiliseraient une méthode différente s’ils le pouvaient et 37% mentionnent au moins une forme d’utilisation d’une méthode non préférée. Beaucoup de femmes citent les obstacles au niveau des établissements de santé, par exemple le refus par les prestataires de leur donner leur méthode préférée, comme les raisons pour lesquelles elles utilisent une méthode non préférée. La prévalence élevée d’utilisation d’une méthode non préférée reflète les entraves que les femmes rencontrent lorsqu’elles cherchent à réaliser leurs souhaits en matière de contraception. Des recherches supplémentaires sur les raisons de l’utilisation de méthodes non préférées sont nécessaires pour promouvoir l’autonomie contraceptive.
Resumen
Los investigadores en el área de planificación familiar tradicionalmente han centrado sus esfuerzos en entender el no uso de anticonceptivos y promover la aceptación de anticonceptivos. Sin embargo, recientemente más académicos han estado explorando la insatisfacción con métodos, cuestionando la suposición de que las necesidades de las usuarias de anticonceptivos necesariamente son satisfechas. Aquí, presentamos el concepto de “uso de método no preferido”, que definimos como uso de un método anticonceptivo a la vez que se desea usar otro método. El uso de método no preferido refleja las barreras a la autonomía anticonceptiva y podría contribuir a la discontinuación del método. Utilizamos los datos de encuestas de 2017 a 2018 para entender mejor el uso de método anticonceptivo no preferido entre usuarias de planificación familiar en edad reproductiva en Burkina Faso. Operacionalizamos el uso de método no preferido como 1) uso de un método que no fue la preferencia inicial de la usuaria y 2) uso de un método a la vez que se informa la preferencia por otro método. Aplicando estos dos enfoques, describimos la prevalencia de uso de método no preferido, las razones para usar métodos no preferidos y los patrones en el uso de método no preferido por método actual y método preferido. Encontramos que el 7% de las mujeres encuestadas informaron usar un método que no deseaban en el momento de adopción, el 33% usaría otro método si pudiera, y el 37% informó por lo menos una forma de uso de método no preferido. Muchas mujeres citan las barreras en los establecimientos de salud, como la negación de prestadores de servicios a proporcionarles su método preferido, como razones para el uso de método no preferido. La alta prevalencia de uso de método no preferido refleja los obstáculos que enfrentan las mujeres cuando intentan satisfacer sus deseos anticonceptivos. Para promover la autonomía anticonceptiva, se necesitan más investigaciones sobre las razones para usar métodos no preferidos.
Introduction
Concern with contraceptive non-use and barriers to contraceptive uptake has dominated the field of international family planning for decades. Given the field’s goals of expanding access to and promoting the use of contraception, much of the existing research has focused on how to ameliorate obstacles to contraception among those who do not use it, including spotlights on barriers to method initiation, reasons for discontinuation and unmet need for family planning.1–3 Meanwhile, the prevailing assumption in the field has been that people who are currently using a modern method of contraception have their family planning needs met.4 However, in just the past few years, there has been a mounting realisation that this assumption may overlook a substantial group in need of improved family planning services: contraceptive users. A growing body of research is starting to examine the ways that contraceptive users may be ill-served by their method choice and/or the counselling they receive, resulting in method dissatisfaction and other adverse outcomes.5–8
Satisfaction with one’s contraceptive method is an important dimension of person-centred care that provides insights into family planning users’ experiences and opinions regarding their current contraceptive method. Though there is no widespread consensus on the definition of method dissatisfaction, it is generally used to describe contraceptive users who are displeased or unhappy with their current method. An emerging body of empirical research is aiming to develop and apply new measures of contraceptive method dissatisfaction, particularly as it applies to unmet need and contraceptive discontinuation. In 2019, Rominski and Stephenson advocated for an expansion of the concept of contraceptive unmet need to include users dissatisfied with their current method. They argued that the automatic ascription of “met need” to all contraceptive users is unjustified, given that users may experience method dissatisfaction or impactful adverse side effects.4 The authors propose expanding the definition of unmet need to incorporate those using family planning who are not satisfied with their current method.
In 2021, Rothschild et al applied Rominski and Stephenson’s proposed adjustments, estimating that the prevalence of modern contraceptive method dissatisfaction ranged from 7% to 19% in a Kenyan cohort. They operationalised the proposed method satisfaction-adjusted unmet need for family planning, reporting that incorporating method dissatisfaction into calculations would increase unmet need 25–70% from the current national estimate of 12% in Kenya.9 Studies in the United States have found that between 37% and 65% of women who ever used contraception have discontinued due to dissatisfaction.10–12 Importantly, contraceptive discontinuation in and of itself is not an adverse outcome. In cases when, for example, the user would like to get pregnant or otherwise no longer wishes to contracept, the ability to discontinue a method is an important sign of reproductive autonomy.13 However, discontinuation due to method dissatisfaction – especially among those who still desire protection from pregnancy – may indicate a public health concern. Research has found that having less than a college degree11 and using a coitally dependent method10 are both predictors of discontinuation due to dissatisfaction. These studies, in conjunction with some in-depth qualitative research,14,7 have added greatly to our understanding of contraceptive method dissatisfaction by showing the impacts of contraceptive side effects on individuals’ daily lives and highlighting the ways that providers view and respond to side effects as myths rather than realities.
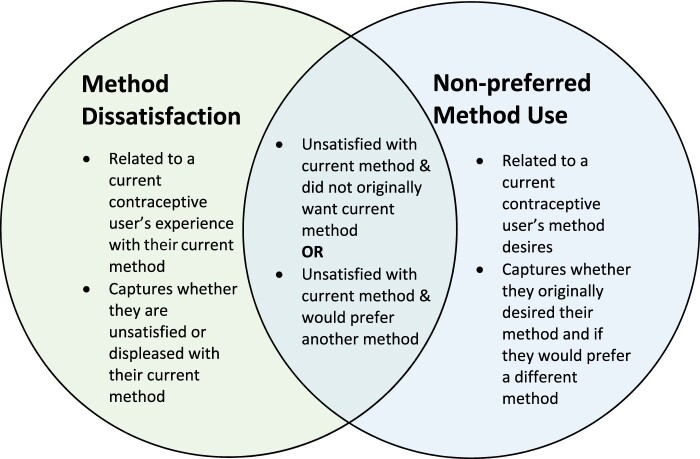
Here, we expand on this growing focus on method dissatisfaction by advancing the conceptualisation and measurement of “non-preferred method use”. Non-preferred method use is a person-centred concept that reflects the method preferences of individuals who are currently using contraception, which often goes unmeasured. A person may be using a non-preferred method if they desire to use a contraceptive method that differs from their current method. The concepts of method dissatisfaction and non-preferred method use may overlap in many cases but may also diverge. For example, a current user of oral contraceptive pills (OCPs) may be both dissatisfied with OCPs and prefer to use the IUD instead. Alternatively, she might be satisfied with OCPs and yet still think the IUD would better meet her needs, in which case concepts of method dissatisfaction and non-preferred method use would not align. As a distinction, non-preferred method use focuses on the method(s) an individual desires to use, whereas method dissatisfaction focuses on experiences with current contraceptive methods (Figure 1).
Figure 1.
Comparison of method dissatisfaction and non-preferred method use
The use of non-preferred family planning methods may be reflective of interpersonal and facility-level barriers to contraceptive autonomy at the time of method provision that prevents women from using the method they desire. Contraceptive autonomy is defined as “the factors that need to be in place for a person to decide for themselves what they want with regard to contraceptive use, and then to realise that decision”.15 Consisting of the sub-domains of informed choice, full choice and free choice, contraceptive autonomy is an important guiding principle for rights-based and person-centred family planning programs.15 Non-preferred method use may be the result of contraventions of all three sub-domains of contraceptive autonomy.
Non-preferred method use may arise from a lack of informed choice, in which an individual does not have sufficient, unbiased information about their method options. At the facility level, a growing body of evidence suggests that women often receive incomplete, inaccurate, biased or directive counselling when seeking contraceptive services, which may prevent them from making informed choices about which method they ultimately use.16–27. Numerous studies have reported that providers promote long-acting contraceptive methods over all others, either through directive or inaccurate counselling tactics22,27 or in more overtly coercive ways.21
Similarly, non-preferred method use may be indicative of a lack of access to a range of methods, representing barriers to full choice. Access and availability of contraceptive methods, including method stock-outs, may influence method selection.28 Medical contraindications to a contraceptive method are one reason that someone may be prevented from using their first choice of method. Legitimate medical contraindications may limit which methods may be safely offered to which people. In a multi-institution US study, less than 5% of women had a contraindication to progestin-only contraceptive pills.29 In another US-based study, 29% of reproductive-aged veterans had at least one contraindication to combined hormonal contraception.30 Data on the prevalence of medical contraindications in in low- and middle-income countries are limited. In addition to legitimate medical contraindications, however, there is evidence that medical criteria may be applied inappropriately in many contexts, unnecessarily limiting contraceptive method choice and contributing to non-preferred method use.31,32
Provider’s counselling may also guide patients away from their preferred method based on individual circumstances; for example, they may suggest a barrier method for an HIV-discordant couple or the discreet use of injectables to a woman whose partner does not support her contraceptive use. In these cases, providers are tailoring their contraceptive counselling to their patient’s individual circumstances, desires or needs by providing them with education on dual protection, contraindications, side effects, discreet use, or other factors that may be important for contraceptive decision-making. This is an important aspect of shared decision-making, in which providers share their expertise on a wide range of contraceptive methods tailored to the patient’s desires. At the same time, under the shared decision-making framework, contraceptive seekers are seen as the experts in their own lives. They, therefore, make the final decision on whether to adopt contraception and which method to choose, even if that decision diverges from provider recommendations.33,34 Shared decision-making is threatened when providers do not honour the desires of their patients or impose their own biases that influence their contraceptive counselling. A large body of evidence demonstrates that providers may violate the tenets of shared decision-making by imposing restrictions on which methods are available to patients based on age, marital status and parity.20,23,8,26 Qualitative data also suggest that providers may refuse to remove long-acting reversible contraception upon request from clients.16,21 Thus, while shared decision-making is a useful framework for counselling, provider biases can violate autonomy and contribute to non-preferred method use.
Non-preferred method use may also be caused by lack of free choice, in which the user faces impediments to their ability to decide about what method to use voluntarily, without barriers, pressure or coercion. Barriers to free choice may occur at the facility or interpersonal level, in which power dynamics may affect family planning decision-making, especially among married women whose husbands decide which method is adopted.35,36 Those using non-preferred methods are unable to make autonomous decisions about their contraceptive use, as they are constrained into using a method they do not desire. This lack of autonomy may in turn contribute to the discontinuation of contraception among those who desire to be using a method, as they are not able to use the method of their choice. Despite the important implications of non-preferred method use for contraceptive autonomy and reproductive health, little is known about the proportion, characteristics or motivations of women using a non-preferred contraceptive method.
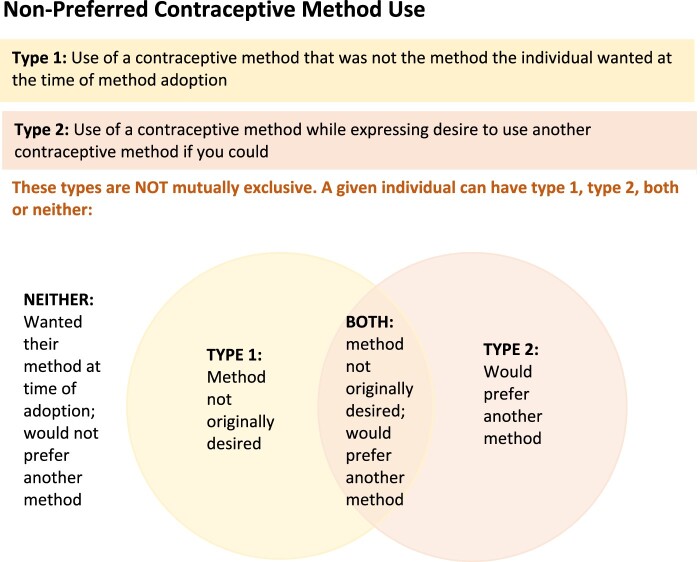
We begin to fill this research gap using population-level data from a novel survey tool to describe the prevalence of non-preferred contraceptive method use among reproductive-age family planning users at two sites in Burkina Faso, a country with a contraceptive discontinuation rate of approximately 36%, according to the Performance Monitoring for Action Project’s 2019 data.37 We explore two different criteria for assessing non-preferred method use: (1) use of a method that was not the user’s original preference and (2) use of a given method while reporting that they would like to use a different method (Figure 2). We describe each type of non-preferred method used by method type and examine the reasoning behind the use of non-preferred methods to provide insights into which methods women in Burkina Faso want to be using and the barriers they face when trying to adopt them.
Figure 2.
Definition of non-preferred method use
Methods
This analysis uses data from the Contraceptive Autonomy Study, a sequential mixed-methods study that took place at two sites in Burkina Faso from 2017 to 2018. The study has been described in detail elsewhere.38 In brief, this analysis uses data from a quantitative survey that included a mix of conventional family planning questions (e.g. those on unmet need for family planning and contraceptive prevalence) adapted from modules in the DHS, and novel questions about each participant’s knowledge and experience with the 14 contraceptive methods.**
Sampling and data collection
The cross-sectional, population-based survey was conducted from April to July of 2018 within the Nouna and the Ouagadougou Health and Demographic Surveillance Systems (HDSS) in Burkina Faso. The Ouagadougou HDSS contains five neighbourhoods, two formal and three informal, in the Northern part of the Burkinabé capital, while the Nouna HDSS consists of the small administrative town of Nouna and 58 surrounding villages. Full profiles of these two HDSSs, as well as details on their periodicity, demographic makeup and methods, can be found elsewhere.39,40 Though these two HDSSs are not nationally representative, they capture considerable diversity in terms of socioeconomic and demographic characteristics, as well as rurality/urbanicity.
Women were eligible for inclusion in the Contraceptive Autonomy Study if they lived within the catchment area of the Nouna or Ouagadougou HDSS, were reproductive-aged (15–49 years, inclusive) and were willing and able to provide informed consent in French, Dioula or Mooré. The full sampling strategy of the Contraceptive Autonomy Study has been described elsewhere.38 Briefly, the study utilised the full Nouna and Ouagadougou HDSSs as sampling frames and drew random samples from both sites. Due to a sampling error in Ouagadougou in which women who no longer resided in the catchment area were initially sampled, inverse probability of sampling weights were created and used in all analyses presented. To conduct interviews, trained research assistants approached women at their homes and orally conducted surveys, with results recorded on Android-based tablets. In total, 3929 women were surveyed.
Analytic approach
This analysis focuses on non-preferred family planning method use; therefore, women who did not report current family planning use at the time of the survey (n = 1719) were excluded from the analytic sample.
We divide the use of a non-preferred family planning method into two distinct types. The first, the use of a method of contraception that was not what the user originally wanted, was measured by asking family planning users, “Was [your current method] the method you wanted?” Respondents who answered “no” were defined as using a non-preferred method, whereas respondents who answered “yes” were using their preferred method. The second type, the use of a method while reporting a preference for a different method, was determined by asking “if you could use [method x] right now, would you want to?” for each of the 14 contraceptive methods that were included on the 2010 Burkina Faso DHS questionnaire: the oral contraceptive pill, injectable, implant, intrauterine device (IUD), external condom, internal condom, calendar method, emergency contraception, lactational amenorrhea method (LAM), standard days method (SDM), spermicide, withdrawal, diaphragm and sterilisation. If a participant had reported that she had never heard of a method before, she was not asked if she would want to use that method (pill n = 31, injectable n = 55, implant n = 23, IUD n = 545, external condom n = 60, internal condom n = 404, calendar method n = 412, emergency contraception n = 870, LAM n = 955, SDM n = 479, spermicide n = 1115, withdrawal n = 982, diaphragm n = 1140, sterilisation n = 440), and thus was classified as not preferring to use that specific method. Participants were not asked if they would want to use their current method, as they were already using it. Participants could indicate a desire to use any of the 14 methods presented, with no restriction on the number of preferred methods they could report. Women who answered that they would want to use at least one of the methods presented were defined as using a non-preferred method. Notably, all included participants were eligible for both types of non-preferred method use. Thus a woman was categorised as having non-preferred method use if she was (i) using a method that she did not originally want, (ii) preferred to be using at least one other method or (iii) both using a method that she did not originally want and preferred to be using another method.
Women who indicated that their current method was not the method they originally wanted were asked for their reason for using their current method. Reasons were categorised by the interviewer into predefined categories. Responses from women who indicated an “other” reason for choosing their current method were translated into English and categorised by the research team. Women who indicated that they would use a different method if they could were asked their reason for not using this different method. Again, “other” responses were translated and categorised. Women who indicated they would rather be using multiple methods other than their current method were asked about their reason for non-use of each of the preferred methods indicated.
We present the sociodemographic characteristics of our analytic sample overall and stratified by site. We estimate the population-level prevalence of non-preferred family planning method use overall, and disaggregated by the two types of non-preferred method use: using a method that was not the user’s first choice and using a method when the user reports they would rather be using a different method. We show reasons for non-preferred method use among women in our sample. We describe non-preferred method use by method type, presenting the proportion of current users of a method who did not want that method at the time of adoption, the proportion of current users of a method who indicate a desire to use another method, and the proportion of non-users of a method who say they would use the method if they could for the 14 different methods. We defined non-users of a given method as women who were currently using contraception who did not report the use of that given method. Finally, we present a heat chart41 in which we disaggregate method preference by the current method used to show patterns and trends in method preference by the current method.
Ethical approval
This research was reviewed and approved by (i) the Institutional Review Board of the Office of Human Research Administration at the Harvard T. H. Chan School of Public Health in Boston, USA (#IRB17-0511, 8th June 2017); (ii) Le Comité d'Ethique pour la recherche en santé du Ministère de la santé du Burkina Faso in Ouagadougou, Burkina Faso (#2017-5-067 – 3rd May 2017) and (iii) Le Comité d’Ethique local du Centre de Recherche en Santé de Nouna, in Nouna Burkina Faso (#2017-01 – 26th May 2017). Written informed consent was obtained for all adult participants. For minors, parental informed consent was obtained in addition to assent from the minor.
Results
Sociodemographic characteristics of family planning users from the Contraceptive Autonomy Study are shown in Table 1. The median age of participants was 29. Most were married (82%) and had at least one child (89%), with more women in Nouna, the rural site, reporting children (93%) compared to women in Ouagadougou, the urban site (82%). Nearly half of participants (49%) reported no education, with women in Nouna more likely to report no formal education compared to women in Ouagadougou (56% vs. 36%). The majority of women in Ouagadougou (69%) reported moped as their primary mode of transport, whereas the majority of women in Nouna (72%) reported bicycle as their primary mode of transport, indicating a higher material standard of living of those from the urban site. Thirty-seven percent of all family planning users indicated that the current method they were using was not their preferred method, either because it was not the method they originally wanted (7%), or because they would rather be using a different method (33%). Just 3% of women reported both that their current method was not the method they originally wanted and that they would prefer to be using another method (Supplementary Table 1). There were no substantial differences in the non-preferred method use by site, so pooled results are presented here.
Table 1.
Demographic characteristics of reproductive-aged family planning users in Burkina Faso
| Ouagadougou n = 424 n (%) or median [Q1, Q3] | Nouna n = 786 n (%) or median [Q1, Q3] | Overall n = 1210 n (%) or median [Q1, Q3] | |
|---|---|---|---|
| Age | 30 [25, 36] | 29 [23, 36] | 29 [24, 36] |
| Married | 331 (78) | 665 (85) | 996 (82) |
| Education | |||
| None | 153 (36) | 444 (56) | 597 (49) |
| At least some primary school | 92 (22) | 204 (26) | 296 (24) |
| At least some secondary school | 162 (38) | 136 (17) | 298 (25) |
| Missing | 16 (4) | 2 (0) | 18 (1) |
| Primary mode of transport | |||
| Foot | 14 (3) | 132 (17) | 146 (12) |
| Bicycle | 54 (13) | 562 (72) | 616 (51) |
| Moped | 292 (69) | 84 (11) | 376 (31) |
| Car | 49 (12) | 0 (0) | 49 (4) |
| Other | 15 (3) | 8 (1) | 23 (2) |
| Number of children | |||
| 0 | 75 (18) | 58 (7) | 133 (11) |
| 1 or more | 348 (82) | 728 (93) | 1,076 (89) |
| Current method is not the method they wanted | 33 (8) | 55 (7) | 88 (7) |
| Would rather be using another method | 142 (34) | 258 (33) | 400 (33) |
| Any indication of non-preferred method use* | 161 (38) | 289 (37) | 450 (37) |
* Includes anyone who indicated that either (a) their current method is not the method they wanted or (b) they would rather be using another method.
Of the 7% of respondents (n = 88) who reported using a different method than the one they originally wanted, 58% cited medical reasons for why they were not using their preferred method, while 23% said that their husband decided on which method they would use (Table 2). Seven percent of women indicated that side effects were too bad with their first-choice method, which is why they were not using their preferred method. A small proportion indicated that their preferred method was not available (3%) or that another family member decided their method (3%).
Table 2.
Reasons for use of method not originally desired
| N | % of people using a method that was not originally desired | % of all current contraceptive users | |
|---|---|---|---|
| N = 88 | N = 1210 | ||
| There was a medical reason I couldn’t use the method | 51 | 58.0% | 4.2% |
| The method I wanted was not available, so the provider told me to use this one | 3 | 3.4% | 0.2% |
| My husband decided the method | 20 | 22.7% | 1.7% |
| Other family member decided the method | 3 | 3.4% | 0.2% |
| Side effects were too bad with method I wanted | 6 | 6.8% | 0.5% |
| Other | 5 | 5.7% | 0.4% |
Over one-third of current contraceptive users (n = 400, 33%) indicated they would prefer to use a different method if they could. These 400 contraceptive users reported a total of 736 methods that they would prefer to be using. Of these, 85% indicated that their reason for not using their preferred method was because a provider would not give it to them if they asked (Table 3). Twelve percent of respondents cited affordability as the primary reason for not using the method they preferred and 8% said they didn’t know where to get their preferred method. Few women noted that they did not adopt their preferred method because health facilities did not offer it (2%) or stigma associated with the method (1%).
Table 3.
Reasons for not using a preferred family planning method
| N people = 400 N methods = 736* | |
|---|---|
| I don’t know where to get it | 58 (7.9) |
| I can’t afford it | 87 (11.8) |
| Health facilities do not offer it | 12 (1.6) |
| Shame/stigma | 6 (0.8) |
| Provider would not give it to me if I asked | 623 (84.6) |
* Some individuals indicated there were multiple methods they would use if they were could. For these people, the reason for each method they indicated they would use is recorded.
The use of non-preferred methods is disaggregated by the method in Table 4. Thirty-one percent of 55 IUD users reported that the IUD was not the method they originally wanted to use (95% confidence interval (CI): 19%, 43%). Fourteen percent of 21 withdrawal users reported that withdrawal was not their originally preferred method (95% CI: 0%, 30%). Eight percent of both external condom users (n = 311; 95% CI: 5%, 12%) and calendar method users (n = 224, 95% CI: 4%, 12%) noted that they did not originally want to use condoms or the calendar method at the time of adoption. Six percent of 205 pill users (95% CI: 3%, 10%) and 4% of both injectable (n = 171, 95% CI: 1%, 6%) and implant (n = 281; 95% CI: 1%, 6%) users indicated that their current method was not preferred. All users of the LAM (n = 6), SDM (n = 4) and sterilisation (n = 9) indicated that their current method was the method they originally preferred.
Table 4.
Use and non-use of preferred methods among family planning users by the method
| Method | Current users of method | Current users who did not want method at time of method adoption | Current users who would rather be using another method | Current users who were non-users of method | Non-users of the method who say they would use the method if they could | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | n | % | 95% CI | n | % | 95% CI | n | n | % | 95% CI | |
| Pill | 205 | 13 | 6.4% | 2.8%, 9.5% | 78 | 38.0% | 31.0%, 45.3% | 1005 | 92 | 9.2% | 7.3%, 11.0% |
| Injectable | 171 | 6 | 3.5% | 0.6%, 5.8% | 45 | 26.3% | 19.8%, 33.2% | 1150 | 60 | 5.2% | 3.9%, 6.6% |
| Implant | 281 | 10 | 3.6% | 1.2%, 5.8% | 83 | 29.5% | 23.8%, 35.3% | 1149 | 61 | 5.3% | 4.0%, 6.7% |
| Intrauterine device (IUD) | 55 | 17 | 30.9% | 19.3%, 43.1% | 13 | 23.6% | 12.1%, 34.0% | 1170 | 40 | 3.4% | 2.4%, 4.5% |
| External condom | 311 | 26 | 8.4% | 5.0%, 11.7% | 162 | 52.1% | 46.1%, 58.1% | 899 | 66 | 7.3% | 5.5%, 9.1% |
| Internal condom | 0 | 0 | NA | – | 0 | NA | – | 1210 | 94 | 7.8% | 6.2%, 9.3% |
| Calendar method | 225 | 18 | 8.0% | 4.0%, 11.7% | 62 | 27.6% | 21.5%, 33.5% | 985 | 89 | 9.0% | 7.2%, 10.9% |
| Emergency Contraception | 4 | 0 | 0.0% | – | 0 | 0.0% | – | 1206 | 90 | 7.5% | 6.1%, 8.8% |
| Lactational Amenorrhea Method (LAM) | 6 | 0 | 0.0% | – | 3 | 50.0% | 0.0%, 99.1% | 1204 | 41 | 3.4% | 2.4%, 4.4% |
| Standard Days Method (SDM) | 4 | 0 | 0.0% | – | 2 | 50.0% | 0.0%, 100% | 1206 | 101 | 8.4% | 6.9%, 9.9% |
| Spermicide | 0 | 0 | NA | – | 0 | NA | – | 1210 | 7 | 0.6% | 0.2%, 1.0% |
| Withdrawal | 21 | 3 | 14.3% | 0.0%, 30.2% | 5 | 23.8% | 6.6%, 45.5% | 1189 | 22 | 1.9% | 1.1%, 2.7% |
| Diaphragm | 0 | 0 | NA | – | 0 | NA | – | 1210 | 2 | 0.2% | 0%, 0.3% |
| Sterilisation | 9 | 0 | 0.0% | – | 0 | 0.0% | – | 1201 | 65 | 5.4% | 4.1%, 6.7% |
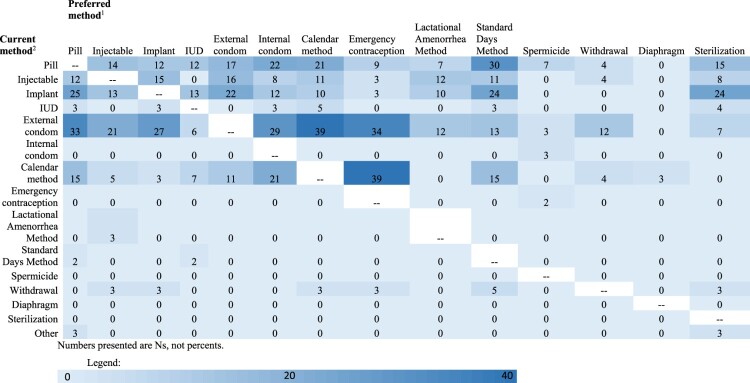
Over half of the 311 current external condom users (52%, n = 162) reported that they would prefer to use another method if they could (95% CI: 46%, 58%). The most commonly preferred method among external condom users was the calendar method (n = 39), followed by emergency contraception (n = 34), pills (n = 33), internal condoms (n = 29) and implants (n = 27, Figure 3). Over a third of the 205 pill users (38%) indicated they would prefer to use another method (95% CI: 31%, 45%), with SDM and internal/external condoms being the most highly preferred methods. About 30% of the 281 implant users noted they would prefer another method (95% CI: 24%, 35%); the pill, SDM and sterilisation were all highly preferred methods among implant users. Just under 30% of users of the calendar method (n = 225) indicated they would prefer other methods (95% CI: 22%, 34%), which included emergency contraception, internal condoms, and pills. Around 25% of the 171 injectable users (95% CI: 20%, 33%), 55 IUD (95% CI: 12% 34%), and 21 withdrawal users (95% CI: 7%, 46%) indicated they would prefer to be using another method. Half of the small number of LAM (n = 6; 95% CI: 0%, 99%) and SDM (n = 4; 95% CI: 0%, 100%) users noted they would use a different method if they could.
Figure 3.
Contraceptive method preferences among current contraceptive users, by current method
Overall, the contraceptive pill, the calendar method, and SDM were the most commonly preferred methods among non-users of those methods, with 9% of the 1005 non-pill users (95% CI: 7%, 11%), 9% of the 985 calendar method non-users (95% CI: 7%, 11%), and 8% of the 1206 non-SDM users (95% CI: 7%, 10%) indicating that they would rather use those methods if they could. Though many non-users of SDM indicated a preference for SDM, only four women (0.3%) in our sample reported currently using SDM. Slightly less than 8% of the 1206 non-emergency contraceptive users (95% CI: 6%, 9%) indicated that they would use emergency contraception if they could, yet again only four women (0.3%) in our sample reported the use of emergency contraception. Approximately 8% of the 1210 internal condom non-users (95% CI: 6%, 9%) and 7% of the 899 external condom non-users (95% CI: 6%, 9%) said they would use internal or external condoms if they could. The use of the external condom was common in our sample (n = 311; 26%), yet no women reported current use of the internal condom despite high preference for that method. About 5% of non-users of the implant (n = 1,149; 95% CI: 4%, 7%) and 3% of non-users of the IUD (n = 1170; 95% CI: 2%, 5%) indicated a preference for these long-acting methods.
Discussion
Using a novel survey tool to estimate the population-level prevalence of non-preferred method use among family planning users in Burkina Faso, we find that just under 40% of women in our study report using a non-preferred family planning method. Given that some women in our sample did not have full information on all available contraceptive methods, this is likely an underestimate of the true proportion of non-preferred method use among these women. The magnitude of these findings has important implications for our understanding of contraceptive autonomy, and for the exercise of informed, full, and free choice in this context. We hypothesise that this level of non-preferred method use may contribute to high rates of contraceptive discontinuation in Burkina Faso, including among women with a desire to prevent pregnancy by using contraception.
When asked why they were not using their preferred contraceptive method, 85% of women who indicated they would rather be using another method said their reason was, “the provider would not give [their preferred method] to [them] if [they] asked”. This demonstrates that most non-preferred method users face barriers at the facility level and perceive providers as limiting their method choice. Other studies exploring facility-level barriers to contraceptive services have reported examples of biased contraceptive counselling, with providers encouraging or discouraging the use of specific methods to certain types of women. In Tanzania, one study found that following a postpartum IUD intervention, providers were less likely to counsel women on methods other than the IUD.22 A study in Kenya reported that providers imposed minimum age restrictions on certain methods and refused to give the injectable to women under age 20.26 Another study in Kenya reported that mystery clients were often denied their preferred method due to provider-imposed requirements for HIV or pregnancy testing or bias based on age, parity or marital status.8 Finally, a study using mystery clients in Nigeria reported that providers were hesitant to give unmarried women hormonal contraceptive methods, citing fear of fertility loss.24 These examples provide insights into how facility-level factors may contribute to non-preferred method use in Burkina Faso.
An additional 12% of women noted that they were not using their preferred contraceptive method due to its cost. At the time this survey took place, contraception was not available free of charge in Burkina Faso.42 However, on 1 June 2019, the government of Burkina Faso committed to offering no-cost family planning services. Future research into how this important reduction in financial barriers to contraceptive access affects the use of non-preferred methods in Burkina Faso is therefore an important next step for this research.43
When asked why they were using a method if it was not their first choice, 58% of non-preferred method users said there was a medical reason why they could not use their preferred method. Some of these cases are likely legitimate medical contraindications; for example, women with breast cancer are contraindicated from using hormonal methods and women with certain cardiovascular diseases are advised to avoid some types of oral contraceptives.31,32 However, some cases of medical contraindication may be incorrectly applied by providers with outdated medical/technical knowledge or may be a means for providers to intentionally encourage the uptake of specific contraceptive methods based on the provider’s personal preferences.44 Previous work has found that providers may use exaggerated or falsified medical information to encourage contraceptive uptake. In one example, a woman was told by a provider that giving birth via caesarean section necessitates the use of injectable contraception and to wait five years before having another child.21 Further research into both legitimate and illegitimate contraceptive counselling on medical contraindications in low- and middle-income countries (LMICs) is warranted and would provide further insights into reasons for the adoption of non-preferred methods from both user and provider perspectives. Additionally, research into potential interventions that promote better clinical practice that follows appropriate medical protocols without violating reproductive autonomy is vital.
An especially high proportion of IUD users (31%) indicated that the IUD was not the method they originally wanted. This could be because contraceptive counselling was successful; a woman may enter counselling with a specific preferred method in mind, but ultimately choose another method that better fits her needs after gathering information about side effects, duration of use and other contraceptive attributes. It also could be because of pressure from a provider to adopt a more effective, long-acting method. Of note, we observe a far lower proportion of implant users who did not originally desire the implant (4%). Provider encouragement or overemphasis of long-acting methods like the IUD can be particularly problematic given that IUDs require skilled providers for removal. Studies in LMICs show that women face barriers to the removal of long-acting methods, including a lack of trained providers, provider unwillingness to remove methods, or unaffordable fees for removal.45,46 Thus, emphasis on informed and free choice is particularly important for women adopting long-acting, provider-dependent methods such as the IUD.
Unlike existing notions of contraceptive dissatisfaction, our indicators of non-preferred method use allow us to explore which methods women are interested in using instead of their current method, which has previously gone unmeasured. In our study, the highest proportion of women reported they would rather be using the pill (9%), followed by the calendar method (9%), SDM (8%), the internal condom (8%), and the external condom (7%). Additionally, though there has been a push from international family planning organisations and researchers to promote highly effective long-acting methods like the implant and IUD, smaller proportions of non-users of these methods in our study noted that they would prefer to use them (5% for the implant and 3% for the IUD).
Our indicators of non-preferred method use also allow us to examine patterns in method preference by the current method. We find that many users of common hormonal methods, like the pill, the implant and the injectable, express a preference for coitally dependent methods like internal or external condoms or fertility awareness-based methods, like the calendar method and SDM. Current users of external condoms and the calendar method were more divided in their desired preferred methods; many expressed preferences for hormonal methods, particularly the pill, implant and injectable, but condoms and fertility awareness-based methods were also highly preferred. Emergency contraception was the most highly preferred method among both calendar method and external condom users. These individuals may not want to continuously use a hormonal method or may not be exposed to the risk of pregnancy often; therefore a barrier or fertility awareness-based method may work best for them, with emergency contraception as a potential backup option.
The misalignment between the preferences of women in our sample and programmatic prioritisation of the most effective, long-acting methods highlights the importance of re-centring contraceptive care on people’s choices. Every contraceptive user has different priorities when it comes to contraception and often effectiveness is not the only contraceptive attribute considered.47 Scholars have warned about the potential pitfalls of promoting only the most effective and longest-acting methods of contraception, cautioning against potential inhibition of contraceptive autonomy.48,49
As operationalised in the present study, non-preferred method use may be a result of a wide range of contraceptive counselling experiences, both positive and negative, or other interpersonal factors that impact decision-making. We classified women who reported using a different method from the method they originally desired as using a non-preferred method. This approach is limited by an inability to distinguish those who were inappropriately denied the method they truly wanted from those who simply changed their mind about which method to use after receiving contraceptive counselling. Indeed, the latter may very well be a reflection of high-quality counselling that helps people achieve their contraceptive desires. Though we have further information about why women ultimately adopted a different method than they originally desired, we still lack contextual details about how and why decisions were made. Thus, we are unable to quantify the extent to which positive counselling experiences may have impacted our measure of non-preferred method use, though we do note that only 7% of women in our sample reported using a method that was not originally desired. Further, we are unable to evaluate if medical contraindications noted or other information given during contraceptive counselling were appropriate, accurate and unbiased.
This study is the first, to our knowledge, to operationalise measures of non-preferred method use, including an indicator of the use of a method not originally desired and an indicator of the use of a method when another method is preferred. While these indicators allow for insights into contraceptive method choice, they also have limitations. First, we did not directly ask women if they wanted to be using their current method of contraception; therefore, we were unable to determine whether women with non-preferred method use desired to discontinue their method. We were also unable to measure ambivalence toward contraceptive use. Women who reported that they would prefer to use other contraceptive methods may not have had strong, unambiguous method preferences; exploring this is an important next step in the measurement of non-preferred method use. Given the limitations of our data, we assumed that women who had never heard of a contraceptive method did not desire to use that method, which likely led to underestimates in the prevalence of non-preferred method use. Additionally, though our study is very much related to method dissatisfaction literature, method dissatisfaction was not directly measured in our data. Future work exploring the ways method dissatisfaction and non-preferred method use overlap and differ would generate fruitful insights into the needs of contraceptive users. Finally, data were collected through a cross-sectional, population-based survey. Though we drew random samples of the Nouna and Ouagadougou HDSSs, our sample of women is not representative of all reproductive-aged women in Burkina Faso, though a wide range of Burkina Faso’s ethno-linguistic and religious diversity is captured between these two research platforms.
Our finding that over one-third of method users report using a non-preferred family planning method indicates an important new priority area for family planning research. Though it is often assumed that women using a contraceptive method have their needs met, this finding – in combination with previous work understanding method dissatisfaction – highlights the necessity of exploring the needs of current family planning users and non-users alike. Future work further delving into the nuances of non-preferred method use using in-depth interviews to inform further iterations of a non-preferred method use indicator is an important next step. Additionally, studies should explore the extent to which non-preferred method use overlaps with method dissatisfaction and contributes to contraceptive discontinuation. To further prioritise the needs and desires of contraceptive users, questions about method dissatisfaction and method preferences should be added to large, population-based surveys so that researchers and policy-makers can further understand the extent of these issues in a wide range of settings. This information can be used to design programmes that seek to help all people, regardless of their contraceptive use status, to fulfil their contraceptive desires. The high prevalence of non-preferred method use in this study demonstrates the need for person-centred family planning care that promotes contraceptive autonomy and values people’s personal preferences.
Supplementary Material
Funding Statement
This study was funded by the following funders/grants: The David and Lucile Packard Foundation #2106-64774 and The Society for Family Planning Research Fund #11-13. BB’s contribution was supported by a National Research Service Award (T32HD052468). BB and KT’s contribution was supported by an infrastructure grant for population research (P2CHD050924) to the Carolina Population Center at the University of North Carolina at Chapel Hill. LS’s contribution was supported by a Ruth L Kirschstein National Research Service Award (T32 HD049302) and Population Research Infrastructure grant (P2C HD047873). The Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) of the National Institutes of Health (NIH) awarded these grants. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the NIH/NICHD. The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Footnotes
These include the oral contraceptive pill, injectable, implant, intrauterine device (IUD), external condom, internal condom, calendar method, emergency contraception, lactational amenorrhea method (LAM), standard days method (SDM), spermicide, withdrawal, diaphragm and sterilization. included in the 2010 Burkina Faso DHS.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Ethics
This research was reviewed and approved by (i) The Institutional Review Board of the Office of Human Research Administration at the Harvard T. H. Chan School of Public Health in Boston, USA (#IRB17-0511); (ii) Le Comité d'Ethique pour la recherche en santé du Ministère de la santé du Burkina Faso in Ouagadougou, Burkina Faso(#2017-5-067) and (iii) Le Comité d’Ethique local du Centre de Recherche en Santé de Nouna, in Nouna Burkina Faso(#2017-01). Written informed consent was obtained for all adult participants. For minors, parental informed consent was obtained in addition to assent from the minor.
Supplemental data
Supplemental data for this article can be accessed online at https://doi.org/10.1080/26410397.2023.2174244.
References
- 1.Rattan J, Noznesky E, Curry DW, et al. Rapid contraceptive uptake and changing method mix with high use of long-acting reversible contraceptives in crisis-affected populations in Chad and the democratic republic of the Congo. Glob Health Sci Pract. 2016;4:S5–S20. doi: 10.9745/GHSP-D-15-00315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sedgh G, Hussain R.. Reasons for contraceptive nonuse among women having unmet need for contraception in developing countries. Stud Fam Plann. 2014;45:151–169. doi: 10.1111/j.1728-4465.2014.00382.x. [DOI] [PubMed] [Google Scholar]
- 3.Speizer IS. Using strength of fertility motivations to identify family planning program strategies. Int Fam Plan Perspect. 2006;32:185–191. doi: 10.1363/ifpp.32.185.06. [DOI] [PubMed] [Google Scholar]
- 4.Rominski SD, Stephenson R.. Toward a new definition of unmet need for contraception. Stud Fam Plann. 2019;50:195–198. doi: 10.1111/SIFP.12084. [DOI] [PubMed] [Google Scholar]
- 5.Brandi K, Fuentes L.. The history of tiered-effectiveness contraceptive counseling and the importance of patient-centered family planning care. Am J Obstet Gynecol. 2020;222:S873–S877. doi: 10.1016/J.AJOG.2019.11.1271. [DOI] [PubMed] [Google Scholar]
- 6.le Guen M, Schantz C, Régnier-Loilier A, et al. Reasons for rejecting hormonal contraception in western countries: a systematic review. Soc Sci Med. 2021;284:114247; doi: 10.1016/J.SOCSCIMED.2021.114247. [DOI] [PubMed] [Google Scholar]
- 7.Stevens LM. “We have to be mythbusters”: clinician attitudes about the legitimacy of patient concerns and dissatisfaction with contraception. Soc Sci Med. 2018;212:145–152. doi: 10.1016/J.SOCSCIMED.2018.07.020. [DOI] [PubMed] [Google Scholar]
- 8.Tumlinson K, Britton LE, Williams CR, et al. Contraceptive method denial as downward contraceptive coercion: a mixed-methods mystery client study in Western Kenya. Contraception. 2022;115:53–58. doi: 10.1016/J.CONTRACEPTION.2022.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rothschild CW, Brown W, Drake AL.. Incorporating method dissatisfaction into unmet need for contraception: implications for measurement and impact. Stud Fam Plann. 2021;52:95–102. doi: 10.1111/SIFP.12146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ersek JL, Huber LRB, Thompson ME, et al. Satisfaction and discontinuation of contraception by contraceptive method among university women. Matern Child Health J. 2011;15:497–506. doi: 10.1007/S10995-010-0610-Y. [DOI] [PubMed] [Google Scholar]
- 11.Littlejohn KE. Hormonal contraceptive use and discontinuation because of dissatisfaction: differences by race and education. Demography. 2012;49:1433–1452. doi: 10.1007/S13524-012-0127-7. [DOI] [PubMed] [Google Scholar]
- 12.Moreau C, Cleland K, Trussell J.. Contraceptive discontinuation attributed to method dissatisfaction in the United States. Contraception. 2007;76:267–272. doi: 10.1016/J.CONTRACEPTION.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 13.Curtis S, Evens E, Sambisa W.. Contraceptive discontinuation and unintended pregnancy: an imperfect relationship. Int Perspect Sex Reprod Health. 2011;37:58–66. doi: 10.1363/3705811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schwarz J, Dumbaugh M, Bapolisi W, et al. “So that’s why I’m scared of these methods”: locating contraceptive side effects in embodied life circumstances in Burundi and eastern democratic republic of the Congo. Soc Sci Med. 2019;220:264–272. doi: 10.1016/J.SOCSCIMED.2018.09.030. [DOI] [PubMed] [Google Scholar]
- 15.Senderowicz L. Contraceptive autonomy: conceptions and measurement of a novel family planning indicator. Stud Fam Plann. 2020;51:161–176. doi: 10.1111/sifp.12114. [DOI] [PubMed] [Google Scholar]
- 16.Britton L, Williams C, Onyango D, et al. “When it comes to time of removal, nothing is straightforward”: A qualitative study of experiences with barriers to removal of long-acting reversible contraception in western Kenya. Contracept X. 2021;3:100063. doi: 10.1016/J.CONX.2021.100063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Calhoun LM, Speizer IS, Rimal R, et al. Provider imposed restrictions to clients’ access to family planning in urban Uttar Pradesh, India: a mixed methods study. BMC Health Serv Res. 2013;13:1–13. doi: 10.1186/1472-6963-13-532/TABLES/6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Manzer J, Bell A.. “We’re a little biased”: medicine and the management of bias through the case of contraception. J Health Soc Behav. 2021;62:120–135. doi: 10.1177/00221465211003232. [DOI] [PubMed] [Google Scholar]
- 19.PMA Burkina Faso . PMA Burkina Faso: Results from Phase 3 cross-sectional survey; 2022.
- 20.Schwandt HM, Speizer IS, Corroon M.. Contraceptive service provider imposed restrictions to contraceptive access in urban Nigeria. BMC Health Serv Res. 2017;17(1): 268. doi: 10.1186/S12913-017-2233-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Senderowicz L. “I was obligated to accept”: A qualitative exploration of contraceptive coercion. Soc Sci Med. 2019a;239:112531; doi: 10.1016/j.socscimed.2019.112531. [DOI] [PubMed] [Google Scholar]
- 22.Senderowicz L, Pearson E, Hackett K, et al. I haven’t heard much about other methods”: quality of care and person-centredness in a programme to promote the postpartum intrauterine device in Tanzania. BMJ Glob Health. 2021;6:e005775; doi: 10.1136/BMJGH-2021-005775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sidze EM, Lardoux S, Speizer IS, et al. Young women’s access to and use of contraceptives: the role of providers’ restrictions in urban Senegal. Int Perspect Sex Reprod Health. 2014;40:176–183. doi: 10.1363/4017614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sieverding M, Schatzkin E, Shen J, et al. Bias in contraceptive provision to young women Among private health care providers in south west Nigeria. Int Perspect Sex Reprod Health. 2018;44:19–29. doi: 10.1363/44E5418. [DOI] [PubMed] [Google Scholar]
- 25.Towriss CA, Phillips TK, Brittain K, et al. The injection or the injection? Restricted contraceptive choices among women living with HIV. Sex Reprod Health Matters. 2019;27:215–227. doi: 10.1080/26410397.2019.1628593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tumlinson K, Okigbo CC, Speizer IS.. Provider barriers to family planning access in urban Kenya. Contraception. 2015;92:143–151. doi: 10.1016/J.CONTRACEPTION.2015.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yirgu R, Wood SN, Karp C, et al. “You better use the safer one … leave this one”: The role of health providers in women’s pursuit of their preferred family planning methods. BMC Womens Health. 2020;20:1–9. doi: 10.1186/S12905-020-01034-1/TABLES/1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zuniga C, Wollum A, Grindlay K, et al. The impacts of contraceptive stock-outs on users, providers, and facilities: A systematic literature review. Glob Public Health. 2022;17:83–99. doi: 10.1080/17441692.2020.1850829. [DOI] [PubMed] [Google Scholar]
- 29.Dutton C, Kim R, Janiak E.. Prevalence of contraindications to progestin-only contraceptive pills in a multi-institution patient database. Contraception. 2021;103:367–370. doi: 10.1016/J.CONTRACEPTION.2021.01.010. [DOI] [PubMed] [Google Scholar]
- 30.Judge CP, Zhao X, Sileanu FE, et al. Medical contraindications to estrogen and contraceptive use among women veterans. Am J Obstet Gynecol. 2018;218:234.e1–234.e9; doi: 10.1016/j.ajog.2017.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chung S. “She told me no, that with my weight it is better to use the IUD:” A Mixed-Methods Study of Non-Preferred Contraceptive Method Use for Medical Reasons [master's thesis]. The University of North Carolina at Chapel Hill; 2022.
- 32.World Health Organization. Reproductive Health and Research, World Health Organization . Medical eligibility criteria for contraceptive use; n.d.. p. 268 [Google Scholar]
- 33.Bullington BW, Sata A, Arora KS.. Shared decision-making: The way forward for postpartum contraceptive counseling. Open Access J Contracept. 2022;13:121–129. doi: 10.2147/OAJC.S360833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dehlendorf C, Grumbach K, Schmittdiel JA, et al. Shared decision making in contraceptive counseling. Contraception. 2017;95:452–455. doi: 10.1016/j.contraception.2016.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Edossa ZK, Debela TF, Mizana BA.. Women’s decision on contraceptive Use in Ethiopia: multinomial analysis of evidence from Ethiopian demographic and health survey. Health Serv Res Manag Epidemiol. 2020;7:233339282092456. doi: 10.1177/2333392820924565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mare KU, Aychiluhm SB, Tadesse AW, et al. Married women’s decision-making autonomy on contraceptive use and its associated factors in Ethiopia: A multilevel analysis of 2016 demographic and health survey. SAGE Open Med. 2022;10:205031212110687. doi: 10.1177/20503121211068719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.PMA Burkina Faso . Performance Monitoring for Action Burkina Faso Results from Phase 1 Baseline Survey; 2019.
- 38.Senderowicz L. Conceptions and measurement of contraceptive autonomy. Cambridge: Harvard T.H. Chan School of Public Health; 2019b. [Google Scholar]
- 39.Rossier C, Soura A, Baya B, et al. Profile: the Ouagadougou health and demographic surveillance system. Int J Epidemiol. 2012;41:658–666. doi: 10.1093/IJE/DYS090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sié A, Louis VR, Gbangou A, et al. The health and demographic surveillance system (HDSS) in Nouna, Burkina Faso, 1993-2007. Glob Health Action. 2010;3:5284. doi: 10.3402/GHA.V3I0.5284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mph RO, Bénet T, Argaud L, et al. Heat map for data visualization in infection control epidemiology: An application describing the relationship between hospital-acquired infections, simplified acute physiological score II, and length of stay in adult intensive care units. Am J Infect Control. 2017;45:746–755. doi: 10.1016/j.ajic.2017.02.012. [DOI] [PubMed] [Google Scholar]
- 42.Browne L, Cooper S, Tiendrebeogo C, et al. Using experience to create evidence: a mixed methods process evaluation of the new free family planning policy in Burkina Faso. Reprod Health. 2022;19:1–16. doi: 10.1186/S12978-022-01375-0/TABLES/3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Burkina Faso: Historic day for advancing sexual and reproductive health rights [ WWW Document] . https://www.amnesty.org/en/latest/campaigns/2019/06/burkina-faso-historic-day-for-advancing-sexual-and-reproductive-health-rights/ (accessed 7.10.22); n.d.
- 44.Shelton JD, Jacobstein RA, Angle MA.. Medical barriers to access to family planning. Lancet. 1992;340:1334–1335. doi: 10.1016/0140-6736(92)92505-A. [DOI] [PubMed] [Google Scholar]
- 45.Romero L, Mendoza Z, Hurst S, et al. Strategies and safeguards to ensure access to long-acting reversible contraception removal after the Zika contraception access network ended: A prospective analysis of patient reported complaints. Contraception. 2020;102:356–360. doi: 10.1016/J.CONTRACEPTION.2020.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tumlinson K, Britton L, Williams C, et al. Provider verbal disrespect in the provision of family planning in public-sector facilities in Western Kenya. Qualitative Research in Health. 2022;2:100178. doi: 10.1016/j.ssmqr.2022.100178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Littlejohn KE. Just get on the pill : the uneven burden of reproductive politics. Oakland, CA: University of California Press; n.d. [Google Scholar]
- 48.Gomez AM, Fuentes L, Allina A.. Women or LARC first? reproductive autonomy and the promotion of long-acting reversible contraceptive methods. Perspect Sex Reprod Health. 2014;46:171–175, doi: 10.1363/46E1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Higgins JA. Celebration meets caution: long acting reversible contraception (LARC)’s boons, potential busts, and the benefits of a reproductive justice approach. Contraception. 2014;89:237–241. doi: 10.1016/J.CONTRACEPTION.2014.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.