Abstract
OBJECTIVE:
To conduct a systematic review of the published literature regarding healthcare-based interventions addressing food insecurity during pregnancy and their effects on patient-reported, pregnancy, or nutritional outcomes.
DATA SOURCES:
We performed a systematic search in February 2022 (subsequently updated in August 2022) using Embase, Medline, Cochrane Library, and Scopus using terms related to food insecurity interventions during pregnancy.
STUDY ELIGIBILITY CRITERIA:
Studies examining healthcare-based interventions addressing food insecurity during pregnancy with patient-reported outcomes (e.g., program satisfaction), adverse pregnancy outcomes (e.g., preterm birth), or nutritional outcomes (e.g., dietary intake) were included. Studies using data prior to 1995, conducted outside the United States, or focused solely on dietary content or on WIC/SNAP as the intervention of interest were excluded.
STUDY APPRAISAL AND SYNTHESIS METHODS:
Three authors screened abstracts and full articles for inclusion. The final cohort included five studies. Three authors independently extracted data from each article and assessed study quality using GRADE, and risk of bias using NIH Study Quality Assessment tools.
RESULTS:
Five studies describing interventions addressing food insecurity during pregnancy were included. Study designs included prospective (n=1) and retrospective cohort (n=4) studies. There was heterogeneity in type of intervention, with three utilizing food vouchers, one focusing on a group prenatal service with nutrition and food management education, and one using a food connection program. Most studies (n=4; 80%) shared patient-reported outcomes (e.g., food security levels, program utilization rates), with 2 studies examining pregnancy-related outcomes (i.e., glucose, blood pressure, preterm birth) and 2 studies examining nutritional outcomes. Interventions were associated with improved levels of food insecurity, reduced odds of preterm birth, and improved blood pressure trends; findings demonstrated a 56–81% program utilization rate. All studies exhibited moderate to low study quality, with fair to good internal validity.
CONCLUSION:
Although data on healthcare-based interventions targeted at food insecurity during pregnancy are limited, the few studies identified suggest such interventions may affect pregnancy outcomes. Better understanding of the local scope and context of food insecurity as well as community-based organizations’ efforts not captured by the literature in this area can help inform the development of interventions targeting food access during pregnancy.
Keywords: food insecurity, healthcare intervention, adverse pregnancy outcomes, healthcare utilization, systematic review, social determinants of health
INTRODUCTION
Food insecurity, defined as “[being] uncertain of having, or unable to acquire, enough food to meet the needs of all family members,” is a key public health issue affecting close to 11% of U.S. households in 2019 alone.1,2 This issue has only been exacerbated by the COVID-19 pandemic, with close to 40% of U.S. households impacted.2–4 Pregnant people are particularly at risk of being adversely affected, given that consistent, high-quality nutrition is essential to perinatal health.5 However, fewer than 30% of pregnant people have nutrition intake that is guideline-adherent, commonly due to issues with food access, underscoring food as one of the key social determinants of health (SDoH) for this population.4, 6–7
In addition, disparities in food access are significant. Food insecurity disproportionately burdens female-headed households, low-income people, and people who are Black, Indigenous, and people of color.1,5,8–10 In turn, inadequate food access, given its link with undernourishment, results in adverse health outcomes, including iron deficiency anemia and inappropriate gestational weight gain/loss, among other issues.6,11–14 Addressing SDoH such as food insecurity in an equity-focused manner is essential to improving health in marginalized populations. Yet, interventions to combat food insecurity during pregnancy, with a long-term goal of improving maternal and child health outcomes, are relatively understudied.
OBJECTIVE
Although many studies have focused on improving food access for non-pregnant individuals (e.g., via prescriptions, vouchers, or direct provision of food)15,16 and demonstrated enhanced health and engagement in care in a general population, few studies have focused on such interventions in the unique setting of pregnancy. Yet interventions developed for non-pregnant individuals are not always directly applicable to pregnancy, which is a period of frequent healthcare access, enhanced learning and health behavior change requirements, amplified nutrition challenges, and changes in social dynamics. In particular, pregnancy is a period in which healthcare-based programs focused on health behaviors and SDoH may be particularly efficacious, given the frequency of contact pregnant individuals have with healthcare systems.
Thus, improved understanding of healthcare-based programs and their impact, particularly on low-income pregnant individuals who may have the greatest barriers to full access to food, can help fill current knowledge gaps. We therefore performed a systematic review to assess literature describing healthcare-based interventions addressing food insecurity and/or food access during pregnancy.
METHODS
Eligibility Criteria, Information Sources, and Search Strategy
The review protocol was prospectively registered with PROSPERO, registration number CRD42022306744, and designed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 checklist.17
The primary objective of the search strategy was to identify hospital or clinic-based interventions that address food insecurity during pregnancy. A medical librarian and a maternal-fetal medicine clinician created search strategies for the concepts of food insecurity interventions and pregnant individuals (Appendix A). The search strategies were launched in PubMed (MEDLINE) 1946-, Embase (Elsevier) 1947-, Scopus (Elsevier) 1823-, and the Cochrane Library (Wiley). The search strategies for the Embase, Cochrane, and Scopus, databases were adapted from the PubMed (MEDLINE) search strategy. All databases were searched back to their inception. Initial searches were completed in February 2022.
Duplicates were identified and removed in EndNote (Clarivate, Philadelphia, PA), resulting in 11,200 unique citations. All results were exported to Rayyan (Qatar Computing Research Institute, Doha, Qatar), a software designed to support researchers in conducting systematic reviews.
A secondary search was performed with the same methods in August 2022 to capture studies that had been published in the interim. The search, and subsequent screen, data abstraction, bias assessment, and data synthesis (described below), were performed with the same protocol as outlined above. An additional 536 articles were screened and one additional article was added to the final group (Figure 1).
Figure 1:
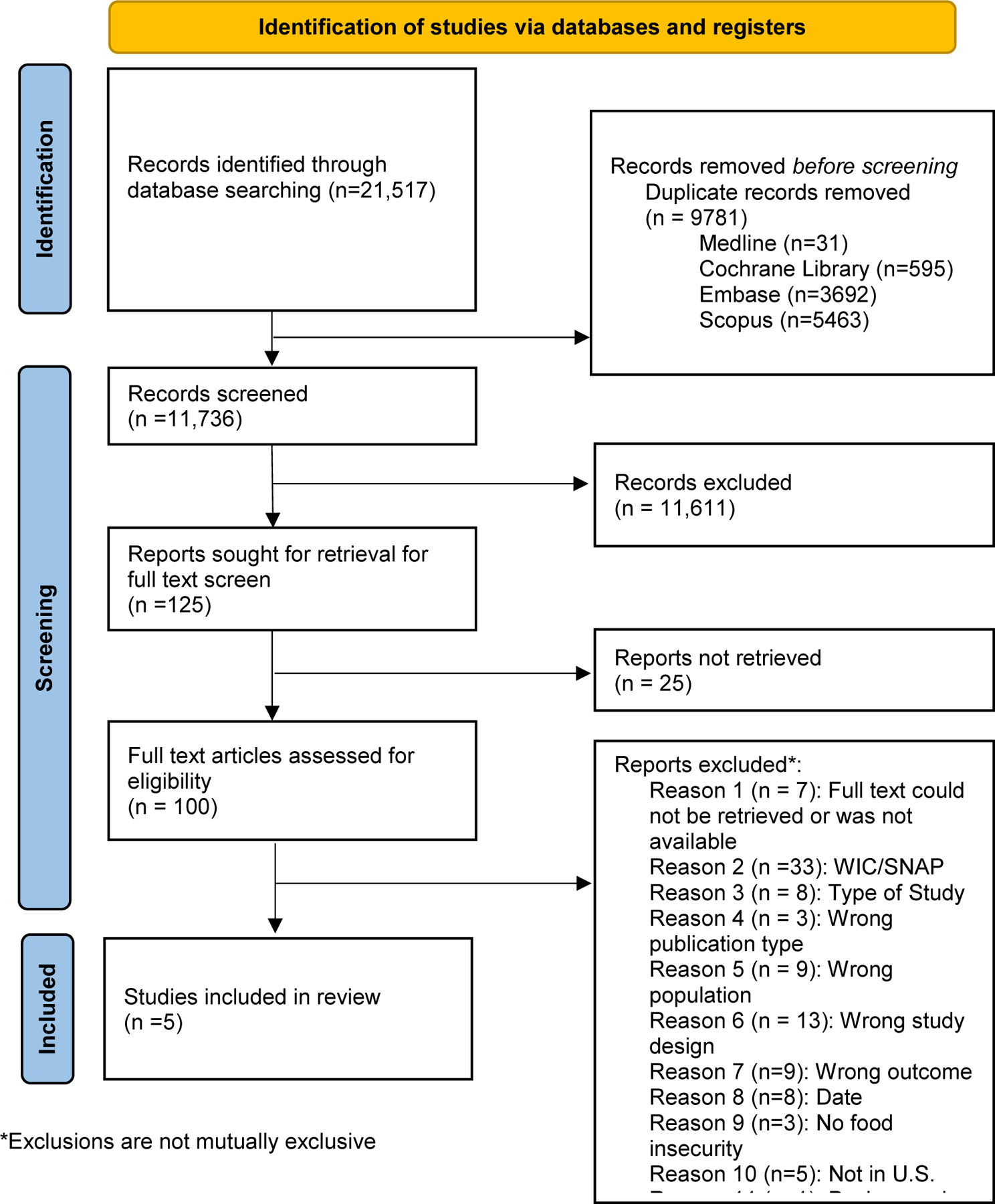
PRISMA Flow Diagram
The PRISMA flow diagram exhibits the systematic review process utilized in this study.
Study Selection
The research team developed inclusion and exclusion criteria to determine eligible studies during the screening process (Appendix B). Studies were eligible for inclusion if full texts were available (through public or institutional access) in English, included pregnant or postpartum (<6 weeks) individuals, included an intervention targeting food access/food insecurity, and measured outcomes related to food access, patient-reported outcomes, adverse pregnancy outcomes, or nutritional outcomes. For the purpose of this review, food insecurity was defined as having limited access or ability to access food at any time. Food insecurity may also include limited access to healthy food or relative food insecurity, such as temporality of food access or favoring of some household members over the pregnant individual.
Notably, interventions had to be focused on improving food access as a social determinant of health, not focused solely on dietary content (i.e., iron deficiency, supplements, medical nutrition therapy), to be included. Given the goal of evaluating healthcare-based programs, the research team excluded studies examining the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) in order to focus exclusively on interventions directly implemented in hospital or clinic-based settings, and because of ample existing literature on WIC. Although the included studies may be related to WIC (e.g., studies of participants in WIC), the intervention under study had to occur outside of the WIC program for the study to be included in this analysis. Outcomes of interest included but were not limited to: changes in household food security, intervention utilization rate, participant satisfaction with intervention, preterm birth, gestational weight gain, and dietary intake. Outcomes could be reported as percentages, odds ratios, risk ratios, or mean differences.
The search was limited to studies in the United States (US), because the type of healthcare system and pregnant individuals’ resources within and outside of it vary based on country. Studies utilizing data prior to 1995, regardless of publication date, were excluded post-screening, due to the shifts in the healthcare landscape over the past 20 years, including changing health policy and the objective of including interventions that reflect closer to present-day needs of the target population. Study designs of randomized controlled trials (RCT), non-RCTs, retrospective or prospective cohort studies, and implementation studies were included.
Study selection was performed using Rayyan.18 To ensure consistency, three authors conducted a preliminary review of 100 randomly selected abstracts. After resolving any disagreements, the same authors reviewed all abstracts and titles for inclusion. A fourth author settled any disagreements. Once relevant abstracts were agreed upon, full-text analysis of included abstracts was performed by two authors, again with a third author settling any disagreements.
Data Extraction
The full text of studies meeting the final inclusion criteria was independently abstracted for first author, publication year, study design, population, sample size, intervention, results, and study quality evaluated using the Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) framework.19 Study quality was categorized as high, moderate, low, or very low.
Assessment of risk of bias
Two authors (BLINDED) separately assessed risk of bias for each included study using the National Institutes of Health Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies and the National Institutes of Health Quality Assessment Tool for Controlled Intervention Studies.20 These tools are specifically designed to assist reviewers in critically appraising the internal validity of studies. Studies were deemed “good,” “fair,” or “poor.” In the case when the authors disagreed on a rating, a third author resolved any disagreements. A detailed list of these questions can appear in Table 2.
Table 2:
Risk of bias for included studies using the National Institute of Health Study Quality Assessment Tools
Data Synthesis
Once the final cohort of studies was identified, each study’s design and findings were qualitatively described. These results preclude the advent of a meta-analysis as a result of heterogeneity in study designs and intervention types. Authors were not contacted, and additional data from included studies were not obtained beyond what was available in the published manuscripts.
RESULTS
Study selection
The search strategy yielded a total of 11,736 abstracts for screening. After removing studies that did not meet the inclusion criteria (n=11,611, 98.9%), (n=125, 1%) studies remained for full-text review including WIC studies (Figure 1). Out of the 125 studies, 5 studies (0.04%) qualified for inclusion by meeting the requirements of studying the effects of non-WIC, healthcare-based interventions aiming to alleviate food insecurity among pregnant individuals. Study designs, as defined by the NIH quality assessment tool,20 included prospective cohort studies (n=1, 20%) and retrospective cohort studies (n=4, 80%, which included 3 pre-post test analyses) (Table 1).
Table 1:
Overview of included studies with interventions to address food insecurity
| Study No. | Title | Author, Year | Study design | Population | Sample size | Intervention | Outcomes | Results | Quality Of Evidence (GRADE) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Fruit and Vegetable Vouchers in Pregnancy: Preliminary Impact on Diet & Food Security | Ridberg et al, 2020 * | Non-randomized, prospective intervention for primary analysis; pre-post study design for exploratory analysis | Pregnant WIC individuals in San Francisco, California from 2–8/2017; inclusion of historical cohort of WIC participant for exploratory analysis from 1/2016–1/2017 | N=592 intervention; N=2299 historical cohort | $40 worth of food vouchers redeemable for fruits and vegetables monthly (in addition to standard WIC package) | Primary outcome: Food insecurity measured by the USDA 6 item survey Secondary outcome: dietary intake measured by validated YRBS fruit and vegetable dietary screener with modified response options Exploratory outcome: preterm birth (compared to historical cohort) |
• Improvement in food security (23% vs. 14%, intervention vs. comparison, p=0.04) • Improvement in mean daily frequency of total vegetables, combined fruits and vegetables, salad, and non-fried potatoes (p<0.05) • Odds of preterm delivery were 37% lower in intervention group compared to the historical cohort (OR 0.63, 95%CI 0.43–0.93) |
Low |
|
| |||||||||
| 2 | Additional Fruit and Vegetable Vouchers for Pregnant WIC Clients: An Equity-Focused Strategy to Improve Food Security and Diet Quality | Ridberg et al, 2022 | Controlled (pre-post) intervention Study | Low-income pregnant individuals enrolled in WIC in San Francisco, California (intervention); comparison was low-income pregnant individuals enrolled in WIC in San Francisco’s neighboring counties of Alameda and San Mateo (2020–2021) | n=609 (total); n=304 (intervention); n = 466 (comparison) | $40/month supplement for fruits & vegetables at participating grocery stores, farmers markets, and corner stores in low-income neighborhoods | Primary outcome: Food insecurity measured by USDA 6-item survey Secondary outcome: Dietary intake of fruits and vegetables (measured by 10-item dietary screener questionnaire |
• Mean ± SD food insecurity at baseline was 3.67 ± 2.79 and 3.47 ± 2.73 in the intervention and comparison groups, respectively, and the adjusted between-group change from baseline to follow-up in food insecurity was 0.05 [95% CI: −0.35, 0.44] (p > 0.05). • Fruit and vegetable intake (in cup equivalents) was 2.56 ± 0.95 and 2.51 ± 0.89 at baseline in the two groups, and the adjusted mean between-group difference in changes from baseline was −0.06 [−0.23, 0.11] (p > 0.05). |
Low to moderate |
|
| |||||||||
| 3 | Mixed Methods Evaluation of a Produce Prescription Program for Pregnant Women | Trapl et al, 2016 | Before-After (pre-post) study with no control group | Pregnant individuals less than 24 weeks’ gestation with limited access to fruits and vegetables in Ohio from 7–10/2013 | N=75 program participants; N=10 health care providers | $40 produce vouchers prescribed monthly by health care providers along with individually-tailored counseling to support local food market usage and fresh fruit and vegetable intake | Participant satisfaction with food markets and produce prescription intervention voucher redemption, impact on participants to visit, shop, and introduce children to farmer’s markets, and patient-provider relationship |
• 95% reported program materials were useful • Mean number of PRx prenatal visits was 2.70 (out of a possible 4 program visits total) • 73% attended more than half of their scheduled visits • More than half of the participants (56.0%) redeemed at least one voucher at a farmer’s market • Providers shared intervention created opportunities to talk about diet with participants, increased awareness about farmer markets, and new shopping habits |
Low |
|
| |||||||||
| 4 | Effects of Group Prenatal Care on Food Insecurity during Late Pregnancy and Early Postpartum | Heberlein et al, 2015 | Prospective cohort study | Racially diverse, low-income pregnant individuals receiving CenteringPregnancy group prenatal care or individual prenatal care in the southeastern US from 2012–2013 | N=124 receiving CenteringPregnancy group prenatal care N=124 receiving individual prenatal care | CenteringPregnancy, a group prenatal care service that provides education regarding nutrition and health eating and the opportunity for women to share experiences and knowledge surrounding food (e.g. strategies for finding lower-cost foods, managing food budgets, preparing meals, etc.) | Food security measured by US Household Food Security Survey Module—Short Form, perception on ability to afford health foods and need to stretch food resources, psychosocial outcomes (measured by validated survey tools – e.g. perceived stress scale) among food-insecure women including maternal-infant attachment scores |
• Among initially food-insecure individuals, intervention participants were more likely to become food-secure in late pregnancy (average predicted probability, 0.67 vs. 0.35, p<0.001) and postpartum (adjusted predicted probability, 0.76 vs. 0.57, p = 0.052) compared to usual care • Intervention group was more likely to perceive a change in their ability to afford healthy foods and stretch food resources compared to usual care • Intervention participants with food insecurity early in pregnancy demonstrated higher maternal-infant attachment scale scores (89.8 vs. 86.2 points, p = 0.03) compared to usual care |
Low |
|
| |||||||||
| 5 | Food Insecurity and Cardiovascular Health in Pregnant Women: Results From the Food for Families Program, Chelsea, Massachusetts, 2013–2015 | Morales et al, 2016 | Retrospective cohort study | Pregnant adult individuals who visited the obstetric clinic at the Chelsea Healthcare Center in Massachusetts from 2013–2015 | N=145 referred to Food for Families program (FFP); N=97 referred to and enrolled; N= 48 referred to but not enrolled; N= 1150 not referred to FFP | FFP identifies food-insecure individuals and connects them to food resources (SNAP, WIC, food Pantries) | Primary outcome: blood pressure (systolic and diastolic) trend during pregnancy Secondary outcome: Trend in blood glucose |
• Individuals referred to and enrolled in FFP had a better SBP (0.20 mm Hg/week lower, p = .01) and DBP (0.10 mm Hg/week lower, p = .02) trend than those who were not referred • No differences in blood glucose trend, either at baseline or over the course of the pregnancy among groups |
Low |
OR, Odds ratio; USDA, United States Department of Agriculture; SD, Standard Deviation; PRx, produce prescription program; SBP, systolic blood pressure; DBP, diastolic blood pressure; SNAP, Supplemental Nutrition Assistance Program; WIC, Special Supplemental Nutrition Program for Women, Infants and Children, FFP: Food for Families program
This study also compared the intervention participants to non-pregnant (breastfeeding or those with children < age 5) WIC participants who did not receive the intervention. However, for the purpose of this systematic review, we are only examining changes that occurred among pregnant participants.
Study characteristics
The types of interventions included the provision of food vouchers (n=3),21–23 a group prenatal service in which food-related education was included (n=1),24 and a food connection program (n=1).25 The majority (n=3) of interventions focused on directly connecting participants to food sources.
Outcomes observed varied across all studies. The majority of studies (n=4) observed patient-reported outcomes, as three focused on food security levels21,22,24 (one of the three also examined healthy food perception)24 and one evaluated several additional outcomes, including program satisfaction, healthcare utilization, impact on patient-provider relationship, and usability rates.23 Two studies evaluated pregnancy-related outcomes, including changes in blood pressure and glucose trends25 and preterm birth.21 Nutritional outcomes (dietary intake and fruit and vegetable intake) were measured in two studies.21,22
Studies represented a broad range of geography, spanning across the United States (US): two studies took place in California, one in Ohio, one in Massachusetts and one in the Southeast region of the US. All studies were started during 2012 (n=1) or later (n=4), and all studies were published between 2015 to 2022. No studies included interventions that were pandemic-focused in their aims or design, although one study occurred during the pandemic.22
Risk of bias and study quality
All (n=5) studies received a GRADE score of low or low-to-moderate. In terms of risk of bias, majority (n=4) of studies proved to be fair21–23,25 with one study being good (Table 2).24 Low GRADE designations were made because of the limitations of study design such as lack of blinding (typically not possible with this type of intervention), lack of control group, or inconsistency or heterogeneity within the results.
Synthesis of results
Several patient-reported outcomes were reported, although no studies included in-depth qualitative data regarding program feasibility, acceptability, or other implementation metrics. Interventions helped improve levels of food security (23% vs. 14%, intervention vs. control, Ridberg et al.)21 with one demonstrating such effects during late pregnancy (adjusted predicted probability of food security, 0.67 group care vs. 0.35 individual care, p< 0.001) and early postpartum (0.76 group care vs. 0.57 individual care, p = 0.05).24 Notably, one intervention showed a decrease in food insecurity between control and intervention groups at 3-month follow up, but with no significant difference between the two groups.22
Program utilization rates were observed in some studies. One voucher program recorded an 81% redemption rate21 and another recorded at least 56% of participants redeeming one voucher for food.23 Healthcare utilization of participants in one study examining a produce prescription program was analyzed. Results showed 73% of participants attended more than half their scheduled visits, although Trapl and colleagues found no significant difference between those who redeemed vouchers and those who did not.23
In terms of pregnancy outcomes, there were lower odds of preterm birth (<37 weeks’ gestational age) among individuals provided food vouchers (10.0% vs 6.5%, p = .018; unadjusted OR 0.63, 95%CI 0.43–0.93).21 With regard to cardiovascular and metabolic health among pregnant individuals, although the food connection program was not associated with an improvement in blood glucose trends (p=0.40), it was associated with improved systolic blood pressure rate (0.20 mm Hg/week lower, p = .01) and diastolic blood pressure (0.10 mm Hg/week lower, p = .02) rate among those enrolled versus those who were not referred to the program.25
Regarding nutritional outcomes, studies had mixed results. In Ridberg et al. 2020 study, they reported improvement in mean daily frequency of combined fruits and vegetables (p<0.05).21 However, in Ridberg et al. 2022 study, they reported that fruit and vegetable intake decreased in both intervention and control groups, with a differences-in-differences effect size of −0.06 (p>0.05).22
COMMENT
Principal findings
We aimed to analyze the current literature examining existing healthcare-based interventions that addressed food insecurity during pregnancy and their associated patient-reported, pregnancy, and nutritional outcomes. Our systematic review suggests a dearth of literature on this topic, with only 0.04% of studies (n=5) out of 11,736 screened meeting these criteria. Most studies demonstrated that interventions benefited patients clinically, such demonstrating as a lower odds of preterm birth, and effectively targeted food insecurity, with one notable exception,22 which could be attributed to changing resource landscape during COVID-19.
Notably, studies did not significantly take into account patient and other stakeholder (e.g., clinicians, healthcare administrators, payors, or community leaders) perspectives during program development. Although Trapl and colleagues captured these perspectives to some extent as part of outcome measurement,23 the majority of studies did not perform an in-depth exploration of stakeholder viewpoints beyond brief assessments of PROs such as patient satisfaction. However, to develop inclusive and sustainable interventions to address food insecurity in pregnancy (and thereby optimize health outcomes), it is necessary to understand the desires of affected individuals, as well as the preferences of health care team members who may deliver or interact with interventions, and incorporate their views on integration of possible interventions with antenatal care.
Comparisons with existing literature
The majority of studies included in this systematic review used food vouchers, with one study focusing on referral to a food program and another on group prenatal care with provision of food access education. De Marchis and colleagues, in their systematic review of healthcare-based food insecurity interventions for non-pregnant adults, identified 23 studies describing similar intervention categories: education and/or provision of food-related resources (such as referrals or vouchers). De Marchis et al. demonstrated that interventions’ impact on fruit and vegetable intake were also mixed, but health outcomes, where measured, tended to have small, positive effects.15 Although programs designed for pregnant individuals likely require different features and design, the similarity in findings between those programs in our review and in the non-pregnant literature suggest that pregnancy-focused interventions may learn lessons from established programs designed for the general population.
Notably, this study did not include studies where WIC/SNAP was the intervention. Many WIC studies examined pregnancy outcomes, demonstrating that use of WIC lowers risk of preterm birth (consistent with Ridberg et al), small for gestational age, and neonatal intensive care unit admission > 24 hours.21,26–29 One study also discussed WIC impact on maternal health outcomes, in which pregnant people with Medicaid coverage and WIC benefits were less likely to have gestational hypertension.27 This finding is consistent with Morales et al.’ study, in which the Food for Families intervention improved blood pressure trends during pregnancy.25 Studies of WIC also demonstrated reduced food insecurity, consistent with our analysis.30 Nutritional outcomes appeared to be less well studied, and, one study by Rojhani et al, concluded WIC recipients’ diet quality required improvement, as the majority of participants did not consume the recommended servings of whole vegetables.31 These studies highlight the importance of evaluating future interventions from multiple perspectives, to ensure they promote clinical benefit, directly improve food security, and support perinatal nutrition.
Regarding healthcare utilization, Trapl and colleagues found no significant difference in the number of prenatal visits attended between those who redeemed vouchers and those that did not.23 De Marchis and colleagues’ systematic review shared two studies on healthcare utilization, including findings of decreased emergency room visits, inpatient admissions, and cost savings.33,34 Similarly, one WIC-focused study demonstrated that WIC enrollment had a protective association against late or no prenatal care utilization.32 Food-insecure pregnant individuals were shown by Testa and Jackson to have attended fewer prenatal care visits, and were more likely not to have initiated prenatal care during the first trimester.35 Given both the link between food insecurity and inadequate prenatal care, and the dearth of literature specifically on whether healthcare-based food access interventions increase antenatal healthcare utilization, further research is warranted on whether food vouchers or provision of food at the sites of prenatal care can play a role in increasing the regularity of prenatal care attendance. This area for future work is especially important given food insecurity’s link with adverse pregnancy outcomes and the potential for pregnant people to receive acute and chronic medical care to better manage their conditions. 6,11–14,27 Household prenatal food insecurity is also correlated with higher rates missed immunizations and inpatient hospitalization for children.36 Thus, we hypothesize that food access interventions may improve perinatal health outcomes both through improved nutrition as well as through improved healthcare utilization, and recommend future work further address these questions.
Strengths and limitations
This systematic review evaluated healthcare-based interventions targeting food insecurity during pregnancy. Our search strategy was extensive; it went through multiple iterations under the guidance of a medical librarian and maternal-fetal medicine physician to ensure we captured all related articles and extracted articles from multiple databases. We performed a preliminary title and abstract screen to ensure all authors took a similar approach to screening articles. Authors independently screened and examined quality of evidence via the NIH Quality Assessment Tool and GRADE.
However, there is a possibility, as with any systematic review, that few studies were missed, although this limitation was mitigated via the extensive screening process. Additionally, the metrics, study population, and study design of each intervention were slightly different, precluding meta-analysis. For instance, one study utilized clinical metrics such as assessment of blood pressure and glucose, while others reported patient-reported metrics such as patient satisfaction. All studies were small and suggest need for further work.
In addition, although we conducted an exhaustive search of the existing academic literature, there are limitations associated with taking an approach focused on interventions detailed in this medium. Community and nonprofit organizations also focus on the delivery of food resources, including some that may exist in the healthcare setting, yet may not study and publish health outcomes associated with their programs. As such, this systematic review likely underestimates the quantity of food security interventions that may be reflected in communities but are not documented in the scientific literature. Notably, these local efforts tend to focus on more broad populations (e.g., low-income individuals) that may include pregnant individuals, but do not target them specifically. A partnership with academic institutions can be leveraged to ensure existing programming can be tailored to the needs of specific populations such as low-income pregnant people.
Conclusions and implications
There are several conclusions and implications that can be drawn from this work. First, academic literature likely underestimates the work of community organizations, who may be key partners in developing healthcare-based programming for food access in pregnancy. Our findings raise implications for the development of academic-health system-community partnerships aiming to address food access during pregnancy. Community organizations have the ability to and should focus on pregnant people, given the importance of this time period for maternal and fetal health, yet few programs are specifically designed for this population. Health systems and academic institutions have the resources to help community organizations measure impact, especially in the context of evaluating specific clinical outcomes. Our findings underscore the importance of further work in this area that specifically leverages academic-community partnerships to provide a methodologically strong approach to evaluating outcomes. Future work can include analysis of outcomes reports and structure of local, community-based food security interventions. In Chicago, some examples include the Greater Chicago Food Depository, Love Fridge Chicago, and Seventh Generations Ahead,37,38 which focus on food access and resources (Table 3). More nationally, programs such as Meals on Wheels, Nourishing Beginnings at Case Western, among others, are all uniquely positioned to address the needs of pregnant individuals.39,40 Note that these interventions are only a sampling of the significant number of programs that exist in the community, so developing a better understanding of the local landscape of community programs tackling this issue is key.
Table 3:
Selected examples of community interventions to address food insecurity
| Intervention | Description |
|---|---|
| Greater Chicago Food Depository | Existing programs target (1) children/their families, (2) older adults, (3) veterans. Provides market-style food distributions for children in schools, older adult community markets and supplemental food programming, VA food pantry, and produce mobiles. |
| Northern Illinois Food Bank | Existing programs include child nutrition programs (meals after school, backpacks filled with food), SNAP outreach team (helps people apply to SNAP), a food pantry in Rockford, IL, two “traveling food pantry” trucks, monthly boxes of non-perishable food for seniors, and an online food pantry. |
| Urban Growers Collective | Operates 8 urban farms, a produce truck, an emergency food relief squad, community gardens, etc. |
| Love Fridge Chicago | Places community refrigerators around Chicago; neighbors can donate food, and take what they need |
| Seventh Generations Ahead | Sustainable food program educates and trains teachers, food service personnel, and administrators to incorporate local, sustainable food into school meals; responsible for Illinois Harvest of the Month food access program. |
| Nourishing Beginnings at Case Western | Focuses on improving nutritious food access and consumption. Groups will receive either boxed food from the Greater Cleveland Food Bank or cash to be used for groceries every other week, in addition to navigation to health food retail, access to nutrition resources, and community health worker support. Participants have access to recipes and nutrition information. |
| The Doula Part | Partners with organizations for community interventions; partnered with Love Fridge Chicago, Chicago Birthworks Collectives (providing freshly prepared meals to new moms), and others. |
Second, future work must incorporate users and other key stakeholders (e.g. clinicians, nurses) in program design, evaluation, and sustainment. Studies should examine the acceptability and feasibility of multiple types of interventions to stakeholders to promote user-centered design for equitable implementation.
In summary, there are few interventions focused on targeting food insecurity during pregnancy. Those that exist are consistent with models reported in the literature that are used more broadly to support other populations. Findings from this review suggest potential positive benefit of these pregnancy-focused food insecurity interventions. However, interventions to date have not significantly incorporated the perspectives of key stakeholders during development of programs, as part of outcome measurement, or in efforts to promote sustainability. Interventions’ link with clinical outcomes as a function of increased healthcare utilization can also be further explored. Finally, partnering with and leveraging the expertise of community partners can promote successful implementation of a food insecurity-focused intervention for low-income pregnant people.
Supplementary Material
A. Quality assessment of controlled intervention studies
| Study No. | Author (Year) | NIH Assessment Study Type | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | Q14 | Ratinga |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Ridberg et al. (2020) | Non-randomized prospective intervention and pre-post for exploratory analysis | N | N | N | N | N | N | N | N | Y | Y | Y | Y | Y | N | Fair |
| 2 | Ridberg et al. (2022) | Non-randomized prospective intervention and pre-post for exploratory analysis | N | N | N | N | N | N | N | NR | NR | N | Y | Y | Y | Y | Fair |
Q1. Was the study described as randomized, a randomized trial, a randomized clinical trial, or an RCT?
Q2. Was the method of randomization adequate (i.e., use of randomly generated assignment)?
Q3. Was the treatment allocation concealed (so that assignments could not be predicted)?
Q4. Were study participants and providers blinded to treatment group assignment?
Q5. Were the people assessing the outcomes blinded to the participants’ group assignments?
Q6. Were the groups similar at baseline on important characteristics that could affect outcomes (e.g., demographics, risk factors, co-morbid conditions)?
Q7. Was the overall drop-out rate from the study at endpoint 20% or lower of the number allocated to treatment?
Q8. Was the differential drop-out rate (between treatment groups) at endpoint 15 percentage points or lower?
Q9. Was there high adherence to the intervention protocols for each treatment group?
Q10. Were other interventions avoided or similar in the groups (e.g., similar background treatments?
Q11. Were outcomes assessed using valid and reliable measures, implemented consistently across all study participants?
Q12. Did the authors report that the sample size was sufficiently large to be able to detect a difference in the main outcome between groups with at least 80% power?
Q13. Were outcomes reported or subgroups analyzed pre-specified (i.e., identified before analyses were conducted)?
Q14. Were all randomized participants analyzed in the group to which they were originally assigned (i.e. did they use an intention-to-treat analysis)?
Y, yes; N, no; NR, not reported; NA, not applicable
– three ratings were possible: “good,” “fair” or “poor”
B. Quality assessment tool for before-after (pre-post) studies with no control group
| Study No. | Author (Year) | NIH Assessment Study Type | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Ratinga |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 3 | Trapl et al. (2017) | Before-After (pre-post) study with no control group | Y | Y | Y | Y | N | N | N | N | N | Y | Y | NA | Fair |
Q1. Was the study question or objective clearly stated?
Q2. Were eligibility/selection criteria for the study population pre-specified and clearly described?
Q3. Were the participants in the study representative of those who would be eligible for the test/service/intervention in the general or clinical population of interest?
Q4. Were all eligible participants that met the pre-specified entry criteria enrolled?
Q5. Was the sample size sufficiently large to provide confidence in the findings?
Q6. Was the test/service/intervention clearly described and delivered consistently across the study population?
Q7. Were the outcome measures pre-specified, clearly defined, valid, reliable, and assessed consistently across all study participants?
Q8. Were the people assessing the outcomes blinded to the participants’ exposures/interventions?
Q9. Was the loss to follow-up after baseline 20% or less? Were those lost to follow-up accounted for in the analysis?
Q10. Did the statistical methods examine changes in outcome measures from before to after the intervention? Were statistical tests done that provided p values for the pre-to-post changes?
Q11. Were outcome measures of interest taken multiple times before the intervention and multiple times after the intervention (i.e., did they use an interrupted time-series design)?
Q12. If the intervention was conducted at a group level (e.g., a whole hospital, a community, etc.) did the statistical analysis take into account the use of individual-level data to determine effects at the group level?
Y, yes; N, no; NR, not reported; NA, not applicable
– ratings were possible: “good,” “fair” or “poor”
C. Quality assessment tool for observational cohort and cross-sectional studies
| Study No. | Author (Year) | NIH Assessment Study Type | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | Q14 | Ratinga |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 4 | Heberlein et al. (2016) | Prospective cohort | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Good |
| 5 | Morales et al. (2016) | Retrospective cohort | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | N | NR | Y | Fair |
Q1. Was the study question or objective clearly stated?
Q2. Was the study population clearly specified and defined?
Q3. Was the participation rate of eligible persons at least 50%?
Q4. Were all the subjects selected or recruited from the same or similar populations (including the same time period)? Were inclusion and exclusion criteria for being in the study prespecified and applied uniformly to all participants?
Q5. Was a sample size justification, power description, or variance and effect estimates provided?
Q6. For the analyses in this paper, were the exposure(s) of interest measured prior to the outcome(s) being measured?
Q7. Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed?
Q8. For exposures that can vary in amount or level, did the study examine different levels of the exposure as related to the outcome (e.g., categories of exposure, or exposure measured as continuous variable)?
Q9. Were the exposure measures (independent variables) clearly defined, valid, reliable, and implemented consistently across all study participants?
Q10. Was the exposure(s) assessed more than once over time?
Q11. Were the outcome measures (dependent variables) clearly defined, valid, reliable, and implemented consistently across all study participants?
Q12. Were the outcome assessors blinded to the exposure status of participants?
Q13. Was loss to follow-up after baseline 20% or less?
Q14. Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)?
Y, yes; N, no; NR, not reported; NA, not applicable
– three ratings were possible: “good,” “fair” or “poor”
1). Condensation:
Given the increased healthcare-system interaction during pregnancy, systematically measuring and reporting healthcare-based interventions that promote food access - a determinant of perinatal health - is key.
3). AJOG at a Glance
A. Why was this study conducted?
Food insecurity is a key social determinant of perinatal health. Many interventions focus on addressing food access in non-pregnant populations, but interventions during pregnancy have not been characterized and are understudied.
B. What are the key findings?
Of 11,736 articles screened, only 5 non-WIC food insecurity interventions addressed food access during pregnancy. These interventions were associated with decreased odds of preterm birth, improved fruit and vegetable intake, decreased food insecurity, and improved blood pressure trends.
Of the interventions that exist, few consider key stakeholders’ perspectives (e.g., patients and providers) to inform program development and sustainability.
C. What does this study add to what is already known?
Evidence-based interventions to address food insecurity during pregnancy are limited.
Stakeholder-driven and community organization led interventions are not well captured in the literature and should be further studied.
FUNDING:
This work was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development R01 HD098178 and R21 HD094271. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
DISCLOSURES: The authors report no conflicts of interest.
Conflict of Interest Statement: The authors report no conflict of interest.
SYSTEMATIC REVIEW REGISTRATION: PROSPERO 2022 CRD42022306744
REFERENCES
- (1).Gomez H, DiTosto JD, Niznik CM, Yee LM. Understanding food security as a social determinant of diabetes-related health during pregnancy. American Journal of Perinatology 2021. doi: 10.1055/s-0041-1740194 [DOI] [PMC free article] [PubMed]
- (2).Coleman-Jensen A, Rabbitt M, Gregory C, Singh A. Household Food Security in the United States in 2019. US Department of Agriculture Economic Research Service 2020;Economic Research Report Number 275
- (3).Schanzenbach D, Tomeh N. State levels of food insecurity during the COVID-19 crisis. Northwestern Institute for Policy Research Rapid Research Report, 2020 (Accessed January 15, 2021, July 14, 2020, at https://www.ipr.northwestern.edu/documents/reports/ipr-rapid-research-reports-app-visualizesfood-insecurity-14-july-2020.pdf.)
- (4).Wolfson JA, Garcia T, Leung CW. Food Insecurity Is Associated with Depression, Anxiety, and Stress: Evidence from the Early Days of the COVID-19 Pandemic in the United States. Health Equity 2021;5:64–71. PMC7929913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- (5).Marshall NE, Abrams B, Barbour LA, et al. The importance of nutrition in pregnancy and lactation: lifelong consequences. Am J Obstet Gynecol 2021. [DOI] [PMC free article] [PubMed]
- (6).Laraia B, Epel E, Siega-Riz A. Food insecurity with past experience of restrained eating is a recipe for increased gestational weight gain. Appetite 2013;65. [DOI] [PMC free article] [PubMed]
- (7).Laraia B, Siega-Riz A, Gunderson C. Household food insecurity is associated with self-reported pregravid weight status, gestational weight gain and pregnancy complications. Journal of the American Dietetic Association 2010;110:692–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (8).Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr 2010;140:304–10. PMC2806885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- (9).Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med 2006;21:71–7. PMC1484604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- (10).Kelli HM, Kim JH, Samman Tahhan A, et al. Living in Food Deserts and Adverse Cardiovascular Outcomes in Patients With Cardiovascular Disease. J Am Heart Assoc 2019;8:e010694. PMC6405658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- (11).Cook JT, Black M, Chilton M, et al. Are food insecurity’s health impacts underestimated in the U.S. population? Marginal food security also predicts adverse health outcomes in young U.S. children and mothers. Adv Nutr 2013;4:51–61. PMC3648739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- (12).Laraia B, Siega-Riz A, Gunderson C. Household food insecurity is associated with self-reported pregravid weight status, gestational weight gain and pregnancy complications. Journal of the American Dietetic Association 2010;110:692–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (13).Laraia B, Epel E, Siega-Riz A. Food insecurity with past experience of restrained eating is a recipe for increased gestational weight gain. Appetite 2013;65. [DOI] [PMC free article] [PubMed]
- (14).Park CY, Eicher-Miller HA. Iron deficiency is associated with food insecurity in pregnant females in the United States: National Health and Nutrition Examination Survey 1999–2010. J Acad Nutr Diet 2014;114:1967–73. [DOI] [PubMed] [Google Scholar]
- (15).De Marchis EH, Torres JM, Benesch T, et al. Interventions addressing food insecurity in health care settings: A systematic review. The Annals of Family Medicine 2019;17(5):436–447. doi: 10.1370/afm.2412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- (16).Screening and interventions for food insecurity in health care settings: State Strategies to increase an underutilized practice in California https://nourishca.org/CalFresh/CFPAPublications/CFPA-FIScreeningsWhitePaper_FINAL.pdf. Published 2016. Accessed December 6, 2022.
- (17).Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. (In eng). DOI: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (18).Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Systematic Reviews 2016;5(1):210. DOI: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (19).Schünemann HBJ, Guyatt G, Oxman A, editors. GRADE handbook for grading quality of evidence and strength of recommendations In: The GRADE Working Group, ed. Updated October 2013. [Google Scholar]
- (20).NIH NH, Lung, and Blood Institute. Study Quality Assessment Tools (https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools).
- (21).Ridberg RA, Marpadga S, Akers MM, Bell JF, Seligman HK. Fruit and vegetable vouchers in pregnancy: Preliminary impact on Diet & Food Security. Journal of Hunger & Environmental Nutrition 2020;16(2):149–163. doi: 10.1080/19320248.2020.1778593 [DOI] [Google Scholar]
- (22).Ridberg RA, Levi R, Marpadga S, Akers M, Tancredi DJ, Seligman HK. Additional fruit and vegetable vouchers for pregnant WIC clients: An equity-focused strategy to improve food security and Diet Quality. Nutrients 2022;14(11):2328. doi: 10.3390/nu14112328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- (23).Trapl ES, Joshi K, Taggart M, Patrick A, Meschkat E, Freedman DA. Mixed Methods Evaluation of a produce prescription program for Pregnant Women. Journal of Hunger & Environmental Nutrition 2016;12(4):529–543. doi: 10.1080/19320248.2016.1227749 [DOI] [Google Scholar]
- (24).Heberlein EC, Frongillo EA, Picklesimer AH, Covington-Kolb S. Effects of group prenatal care on food insecurity during late pregnancy and early postpartum. Maternal and Child Health Journal 2015;20(5):1014–1024. doi: 10.1007/s10995-015-1886-8 [DOI] [PubMed] [Google Scholar]
- (25).Morales ME, Epstein MH, Marable DE, Oo SA, Berkowitz SA. Food insecurity and cardiovascular health in pregnant women: Results from the Food for Families Program, Chelsea, Massachusetts, 2013–2015. Preventing Chronic Disease 2016;13. doi: 10.5888/pcd13.160212 [DOI] [PMC free article] [PubMed]
- (26).Blakeney EL, Herting JR, Zierler BK, Bekemeier B. The effect of women, infant, and children (WIC) services on birth weight before and during the 2007–2009 great recession in Washington State and Florida: A pooled cross-sectional time series analysis. BMC Pregnancy and Childbirth 2020;20(1). doi: 10.1186/s12884-020-02937-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- (27).Currie J, Rajani I. Within-mother estimates of the effects of WIC on birth outcomes in New York City. Economic Inquiry 2015;53(4):1691–1701. doi: 10.1111/ecin.12219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- (28).Fingar KR, Lob SH, Dove MS, Gradziel P, Curtis MP. Reassessing the association between WIC and birth outcomes using a fetuses-at-risk approach. Maternal and Child Health Journal 2016;21(4):825–835. doi: 10.1007/s10995-016-2176-9 [DOI] [PubMed] [Google Scholar]
- (29).Ghafari-Saravi A, Chaiken SR, Packer CH, Garg B, Caughey AB. Impact of WIC benefits on maternal and neonatal outcomes in patients with gestational diabetes. American Journal of Obstetrics and Gynecology 2022;226(1). doi: 10.1016/j.ajog.2021.11.257 [DOI] [Google Scholar]
- (30).Metallinos-Katsaras E, Gorman KS, Wilde P, Kallio J. A longitudinal study of WIC participation on household food insecurity. Maternal and Child Health Journal 2010;15(5):627–633. doi: 10.1007/s10995-010-0616-5 [DOI] [PubMed] [Google Scholar]
- (31).Rojhani A, Ouyang P, Gullon-Rivera A, Dale TM. Dietary quality of pregnant women participating in the Special Supplemental Nutrition Program for Women, infants, and children. International Journal of Environmental Research and Public Health 2021;18(16):8370. doi: 10.3390/ijerph18168370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- (32).Blakeney EL, Herting JR, Bekemeier B, Zierler BK. Social determinants of health and disparities in prenatal care utilization during the Great Recession period 2005–2010. BMC Pregnancy and Childbirth 2019;19(1). doi: 10.1186/s12884-019-2486-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- (33).Beck AF, Henize AW, Kahn RS, Reiber KL, Young JJ, Klein MD. Forging a Pediatric Primary Care–community partnership to support food-insecure families. Pediatrics 2014;134(2). doi: 10.1542/peds.2013-3845 [DOI] [PubMed] [Google Scholar]
- (34).Berkowitz SA, Terranova J, Hill C, et al. Meal delivery programs reduce the use of costly health care in dually eligible Medicare and Medicaid beneficiaries. Health Affairs 2018;37(4):535–542. doi: 10.1377/hlthaff.2017.0999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- (35).Testa A, Jackson DB. Barriers to prenatal care among food-insufficient women: Findings from the Pregnancy Risk Assessment Monitoring System. Journal of Women’s Health 2021;30(9):1268–1277. doi: 10.1089/jwh.2020.8712 [DOI] [PubMed] [Google Scholar]
- (36).Sandoval VS, Jackson A, Saleeby E, Smith L, Schickedanz A. Associations Between Prenatal Food Insecurity and Prematurity, Pediatric Health Care Utilization, and Postnatal Social Needs. Academic Pediatrics 2021;21(3):455–461. doi: 10.1016/j.acap.2020.11.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- (37).The Love Fridge Chicago. https://www.thelovefridge.com/. Accessed November 16, 2022.
- (38).Seven Generations Ahead https://sevengenerationsahead.org/. Published November 7, 2022. Accessed November 16, 2022.
- (39).Nourishing beginnings study aims to improve health, equity of birth outcomes through Nutrition and Social Support. Better Health Partnership https://www.betterhealthpartnership.org/in-the-news/nourishing-beginnings-program. Published June 29, 2022. Accessed November 16, 2022.
- (40).The Doula Part https://thedoulapart.com/. Accessed November 16, 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


