ABSTRACT
A central venous catheter is a flexible catheter that is inserted into a vein and ends close to the superior vena cava. It may be inserted through a vein in the neck, chest, or arm. It's also called a central venous line or central line. Peripherally inserted central venous catheters (PICCs) are usually implanted in arm veins such as the basilic vein, the brachial veins or in some cases in the cephalic vein. PICCs can remain in place for up to six months or more. If properly managed, they last even more than a year. PICCs offer the advantage of greater safety for infusion of vesicants/irritants and hyperosmolar solutions and enable the administration of antibiotics, prolonged parenteral nutrition, and chemotherapy agents. They are however, associated with some adverse events such as spontaneous late migration. The reasons for these complications are not yet fully understood. There are now established causes and in some cases hypotheses to explain these phenomena. We describe two clinical cases in which apparently correctly positioned PICCs migrated spontaneously from their original position. The identification of the migration of the vascular catheter was accidental in the two patients, and they did not developed complications. One of the two patients had a pacemaker. The remote migration of a PICC is an event that can occur, and the causes are not definitively clarified in all cases.
Keywords: peripherally inserted central catheter, spontaneous migration, superior vena cava, complications, central catheter correct position
INTRODUCTION
Peripherally inserted central venous catheters (PICCs) are used for infusions of irritant/vesicant drugs such as chemotherapy agents, parenteral nutrition, drugs with extreme pH or high osmolarity. They are vascular catheters that can remain in place for months and have a low degree of complications both during and post insertion [1]. In most cases, the complications are occlusion or malfunction, thrombosis, dislocation, and spontaneous migration [2].
The causes of remote migration are unclear in some cases. Phenomena such as a persistent coughing, vomiting, or other conditions that increase intrathoracic pressure, and affect central venous pressure, were taken into consideration. Large arm movements can also cause the tip of the PICC to move [3]. In this article, we describe two clinical cases of distant spontaneous migration of PICCs, whilst trying to provide possible explanations.
CASE 1
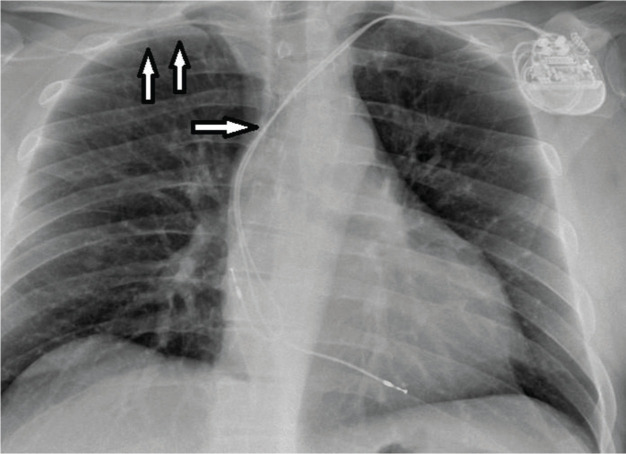
A 58-year-old man received a PICC (Delta Med® PICC power, 4 FR single lumen, polyurethane) insertion to perform a course of chemotherapy after the removal of a colorectal tumour. The PICC was inserted in the right basilic vein, and the total length was 41 cm. The patient had previously had a pacemaker implanted, for symptomatic bradyarrhythmia via the left brachiocephalic vein. Not being able to use the intracavitary ECG technique, we used intraprocedural fluoroscopy and post-implantation chest x-ray was performed [4]. This showed correct positioning in the superior vena cava (SVC), even though it was difficult to establish the exact position of the tip (Figure 1).
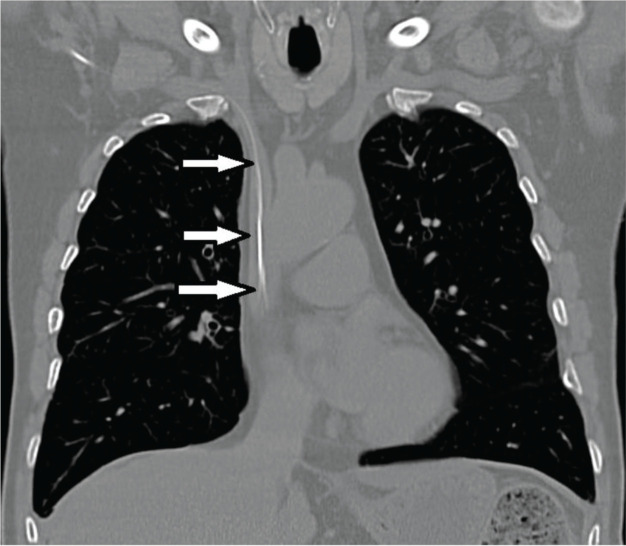
Fig. 1.
PICC with entry from the right arm into the superior vena cava (arrows), in a patient with pacemaker.
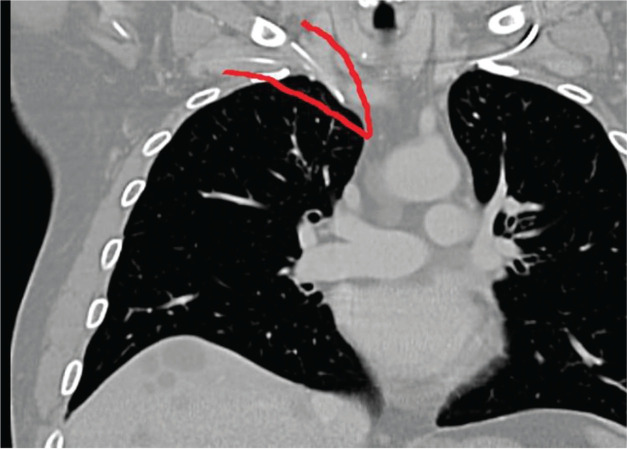
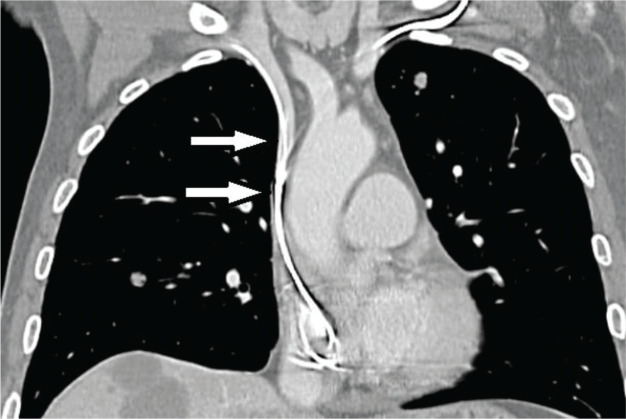
Three months later, the patient underwent a chest CT scan, which showed a loop of the PICC, with the tip ascending in the right internal jugular vein (Figure 2). The PICC was not removed for the communication failure. After another 3 months, a new chest CT scan was performed on the patient as a follow-up to check the progress of the disease and the tip of the PICC had amazingly returned to its original position in the SVC (Figure 3). The patient had not presented any symptoms. There was only a reduction in flow through the vascular catheter. However, the PICC was removed because it was no longer needed. One factor to note is that the patient was an amateur trumpet player.
Fig. 2.
The PICC loops and is in the ipsilateral jugular vein.
Fig. 3.
The PICC has returned to its original position in the superior vena cava (arrows).
CASE 2
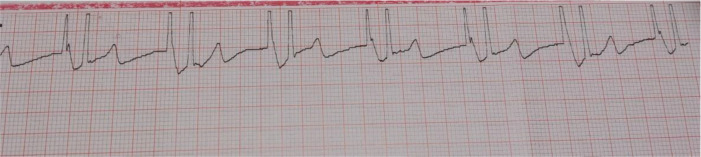
A 64-year-old man had a PICC (Delta Med® PICC power, 4 FR single lumen, polyurethane) inserted for chemotherapy after an intestinal tumour had been removed. The PICC was inserted with an ultrasound technique and the use of the intracavitary ECG to verify the correct position of the tip (Figure 4). The total length was 44 cm.
Fig. 4.
The intracavitary ECG shows the correct positioning of the PICC.
About 2 months after the implant, a chest CT scan was performed as oncological follow-up and this revealed, the correct positioning of the PICC (Figure 5). After 3 months a new chest CT was performed, and this time it showed the migration of the tip of the catheter into the right jugular vein (Figure 6). Again, the patient did not present any symptoms or major problems and had used the vascular catheter without difficulty up to three weeks before the last chest CT scan. The malpositioned PICC was removed and reimplanted in the right brachial vein without any further problems.
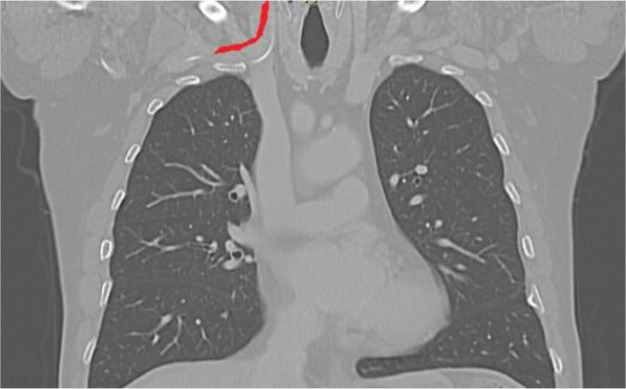
Fig. 5.
A chest CT scan shows the correct positioning of the PICC (arrows).
Fig. 6.
A chest CT scan performed subsequently reveals the migration of the PICC into the ipsilateral internal jugular vein.
DISCUSSION
We have described in this paper two cases of spontaneous migration of PICCs. The determinants that caused the two situations are most likely different. Among these, the non-optimal length of the PICC may have played a role.
Complications related to PICCs can be divided into early or periprocedural and late which occur at a distance. In the first group we can include the hematoma, the arterial or nerve puncture and the primary malposition. In the latter we include infection or catheter related thrombosis, malfunction, and secondary migration. Tip migration of a central venous catheter is a rare complication. The sites most affected by the possible malposition are the opposite brachiocephalic vein, the jugular vein, and the azygous vein [5]. The mechanisms underlying catheter tip migration in some cases are not well understood although some factors are now held responsible for the malposition of the CVC for example, to pressure changes within the thoracic cavity induced by coughing, sneezing, or straining. High infusion pressure has also been correlated with displacement of the tip of a central venous catheter [3]. Two cases of implantable catheter tip migration in SVC in patients with severe cough were also reported [6]. The physical activity of patients is an important factor contributing to the late spontaneous migration of PICCs [7].
In our two clinical cases we cannot be sure of the causes that led to the migration of the catheter.
In the first case, a possible hypothesis may be that the venous catheter was a bit short. In fact, from the chest X-ray it was not clear where the tip of the catheter reached, given the difficulty caused by the simultaneous presence of the pacemaker. In addition, an unexpected, curious, and strange phenomenon occurred. The PICC, which had initially displaced spontaneously, just as spontaneously returned to its original position in the SVC. The patient played the trumpet as a hobby and perhaps the increase in chest pressure caused by this activity may have played a role. Finally, we hypothesize that the return of the catheter tip to its original position may be due to a high-flow procedure, performed by the operator, to overcome a reduction in the infusion rate due to the unknown tip dislocation [8].
In the second case, the PICC measurement was certainly correct, as evidenced by the intraprocedural control with the intracavitary ECG method [9] and by a subsequent chest CT performed for other reasons. The causes that in this case determined its dislocation remain undetermined, given that the patient did not report having coughed or vomited. It could be hypothesized that the movement of the arms of the patient, who in any case led an extremely active life, could have been an important determinant for the dislocation of the PICC tip [7]. An important aspect to underline, remains the fact that in both cases, the patients, fortunately, did not present symptoms or serious complications, and the dislocation of the vascular catheter was discovered by chance.
The question we should ask ourselves is whether it is useful to periodically evaluate the correct position of the tip of the implanted central venous catheters [10] or whether this behaviour is exaggerated in view of the low incidence of dislocation which does not always lead to significant complications.
Obviously, it is mandatory to check the correct position of the tip in case of symptomatic patients or when there is a well-founded suspicion that something has happened and that the tip of the PICC is no longer in a safe position and therefore the vascular catheter must be repositioned correctly [11].
CONCLUSION
PICCs are central venous catheters widely used in clinical practice and have a low incidence of complications. Clinical cases of spontaneous migration of the tip after insertion have been described. In our article we have described two cases of PICC migration and hypothesized possible determinant causes. The cases we have described are particular because in the first case there was a spontaneous migration of the tip which then returned to its original site just as spontaneously. In the second case, the migration of the tip occurred a few months after the implantation since the first control CT scan had not shown any abnormalities in the seat of the PICC tip. A malposition of the central catheter should be suspected if abnormalities are noted in the infusion and appropriate measures should be taken to avoid harm to the patient. Finally, it should be emphasized that central venous catheters are not fixed but follow the dynamics of the host.
Conflicts of interest and funding
No conflicts of interest and no funding to declare.
Ethical considerations
All persons gave their informed consent prior to their inclusion in this article and all ethical principles have been respected. The local ethics committee was notified of the study.
Informed consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
REFERENCES
- 1.Mielke D, Wittig A, Teichgräber U. Peripherally inserted central venous catheter (PICC) in outpatient and inpatient oncological treatment. Support Care Cancer. 2020;28(10):4753–4760. doi: 10.1007/s00520-019-05276-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marsh N, Webster J, Ullman AJ, et al. Peripheral intravenous catheter non-infectious complications in adults: A systematic review and meta-analysis. J Adv Nurs. 2020;76(12):3346–3362. doi: 10.1111/jan.14565. [DOI] [PubMed] [Google Scholar]
- 3.Rasuli P, Hammond DI, Peterkin IR. Spontaneous intrajugular migration of long-term central venous access catheters. Radiology. 1992;182(3):822–824. doi: 10.1148/radiology.182.3.822. Erratum in: Radiology 1992;185(1):286. PMID: 1535901. [DOI] [PubMed] [Google Scholar]
- 4.Erskine B, Bradley P, Joseph T, et al. Comparing the accuracy and complications of peripherally inserted central catheter (PICC) placement using fluoroscopic and the blind pushing technique. J Med Radiat Sci. 2021;68(4):349–355. doi: 10.1002/jmrs.533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Franklin I, Gilmore C. Placement of a peripherally inserted central catheter into the azygous vein. J Med Radiat Sci. 2015;62(2):160–162. doi: 10.1002/jmrs.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu PY, Yeh YC, Huang CH, et al. Spontaneous migration of a Port-a-Cath catheter into ipsilateral jugular vein in two patients with severe cough. Ann Vasc Surg. 2005;19(5):734–736. doi: 10.1007/s10016-005-4638-1. [DOI] [PubMed] [Google Scholar]
- 7.Beccaria P, Silvetti S, Mucci M, et al. Contributing factors for a late spontaneous peripherally inserted central catheter migration: a case report and review of literature. J Vasc Access. 2015;16(3):178–182. doi: 10.5301/jva.5000337. [DOI] [PubMed] [Google Scholar]
- 8.Weber MD, Himebauch AS, Conlon T. Repositioning of malpositioned peripherally inserted central catheter lines with the use of intracavitary electrocardiogram: A pediatric case series. J Vasc Access. 2020;21(2):259–264. doi: 10.1177/1129729819865812. [DOI] [PubMed] [Google Scholar]
- 9.Yu C, Shulan L, Juan W, et al. The accuracy and safety of using the electrocardiogram positioning technique in localizing the peripherally inserted central catheter tip position: A systematic review and meta-analysis. Nurs Open. 2022;9(3):1556–1563. doi: 10.1002/nop2.932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wallace JA, Afonso E, Yu H, et al. Factors that predict increased catheter tip movement in left internal jugular vein implantable venous access ports upon standing. J Vasc Access. 2015;16(3):223–226. doi: 10.5301/jva.5000331. [DOI] [PubMed] [Google Scholar]
- 11.Yu Y, Yuan L. The electrocardiographic method for positioning the tip of central venous access device. J Vasc Access. 2020;21(5):589–595. doi: 10.1177/1129729819874986. [DOI] [PubMed] [Google Scholar]