Abstract
Due to the cognitive decline associated with aging, it is necessary to determine the variables involved in this process to implement preventive actions to avoid or help slow the progression of cognitive decline to dementia in older adults. This is a priority in the current pandemic situation, due to the consequences of periods of confinement due to COVID-19.
To address these challenges, this study was conducted through Information and Communication Technologies (ICTs), by adapting an in-person assessment protocol into an online Tele neuropsychological consultation. The correlation between autonomy and cognitive performance variables is analyzed in 47 Mexican subjects over 60 years of age.
The results of the statistical analyses suggest a moderate correlation between the level of autonomy and cognitive performance (with MOCA and Clock Drawing Test), significant correlation values are outlined in some of the variables reviewed, and interesting data were found in the correlation of cognitive reserve with cognitive decline and the educational level from the participants.
Finally, future analysis is proposed of the sensitivity of screening tests (CDT) to find indicators of Mild Cognitive Impairment (MCI) in this population that is not detected in classical tests (MOCA). Developing ICT-based screening protocols for the elderly may be a key tool in these coronavirus times or under any given circumstances.
Keywords: Tele neuropsychological, ICTs, Screening, Older people, Caregivers, Autonomy, Mild cognitive impairment, eHealth, Cognitive reserve
1. Introduction
In recent years, population aging has been considered a process resulting from decreased birth and uprising death rates [1]. The world population has been slowing down its average annual growth rate, which has led to a proportional increase of older adults concerning the total population, with values that reached 32 percentage points for men and 48 points for women, compared to previous periods [2]. It is estimated that this increase in the general population will correlate with the incidence of pathologies typical of old age, in which cognitive function disorders stand out, such as cognitive impairment since it might be an indicator of dementia in the future.
Following the classical line established by Petersen on the Cognitive Reserve (CR) construct, Borrás & Biña in 2016 [3] state that cognitive impairment is considered the loss of cognitive functions, which depend on both physiological and environmental factors and is subject to a wide interindividual variability, the maintenance of cognition in the elderly is related to variables such as the person's pathologies, mood, social support and the presence of certain geriatric syndromes so that it would not be correct to attribute the cognitive alterations presented in the elderly only to the neurological aging aspect.
An example of this is the study by Zamora-Macorra et al. [4], which analyzed the effect of social support on cognitive decline in Mexican adults over 50 years of age, which correlated with the study by Feng, Ji & Xu. [5] conducted with older Chinese adults, observing that social support is essential for cognitive maintenance in older adults over 70 years of age, and the variables that had the greatest impact on cognitive impairment, apart from age, were economic status, social support, educational level, and place of residence.
Regarding the detection of cognitive impairment in older people, memory has historically been considered the most sensitive data to determine when a person has initial cognitive impairment [6]. In the new DSM 5 definition, the criterion that defined the presence of memory impairment as the earliest and most prominent criterion for the diagnosis of dementia has been eliminated. This new edition gives equal weight to other cognitive deficits in other domains, such as complex attention, executive function, learning, language, perceptual motor skills, and social cognition[7]. In this sense, the Clock Drawing Test (CDT) has proven to be very useful to discriminate indicators of this condition, since it addresses aspects of executive functions and visuoconstructional skills [8].
On the other hand, in the systematic review conducted by Mias and Causse [9] on the relationship between Subjective Memory Complaints (SMC) and vulnerability to cognitive impairment, the results of the studies are not consistent. Thus, some studies find a relationship with mild cognitive impairment, others link complaints as a risk factor for impairment, and a third group connects them mainly with psychological distress. With an elderly population, using PRISMA methodology, of 21,445 older adults evaluated, it is relevant to point out that 65% identified a relationship between SMC and changes in the measurement of memory and 56% in executive functions, although only 22% were associated with cognitive impairment. But what should be noted, is that, in almost 4 out of 5 of the studies, they consider SMC as a risk factor, increasing its value in combination with emotional vulnerability variables (anxious or depressive). And, as followed in the approach of our work, it is necessary to complement the objective performance of memory and other executive functions with the assessment of a key informant [10]. This is a deficient aspect in some of the proposals for neuropsychological screening assessment mediated by ICTs, and it detracts from the validity of screening results with contaminated epidemiological rates (false positives or negatives). Hence, rigorous assessment criteria should be maintained regardless of the modality, as advocated by the American Psychological Association [7].
Furthermore, numerous factors aim to halt or delay the presence of possible cognitive decline or the development of healthy aging. For example, the cognitive reserve (CR), is defined by Stern [11] as the capacity of the organism to resist brain deterioration without presenting symptoms. According to this variable, those people with greater CR would present a lower risk or vulnerability of suffering a degenerative pathological process in cognitive deterioration in old age. And, besides CR, multiple variables affect its development, maintenance, and enhancement throughout the life cycle, such as occupation, education, and leisure activities: physical, mental, and social [12].
In the same matter, Wöbbeking-Sánchez et al. [13] have pointed out some variables that influence cognitive decline, defining the line that differentiates normal aging from pathological aging (schooling, reading patterns, etc.). The link between CR and physical activity patterns or motivational reserve is very important, which would focus on the meaning of life, as well as emotional cues [14]. The inclusion of this variable seems necessary to determine patterns of healthy aging from a preventive perspective in large sectors of the population to make them responsible for their well-being at the end of life. Also, in a recent study, functional magnetic resonance imaging was used to evaluate the effect of cognitive training on brain activation as a function of learning stage and level of education; it showed that those with lower education had reduced activation of the right temporal lobe. This work reinforces Stern's model of cognitive reserve in the sense that educational variables are evidenced with fMRI techniques, given that depending on these variables, activation of the right temporal lobe is a differential indicator of the reserve. According to this, older people with a lower cognitive reserve (in terms of educational variables) achieve less generalized brain plasticity in stimulation programs than peers with a higher educational level [15].
Therefore, assessing intellectual functioning should be present in any assessment of older people, but a comprehensive diagnosis should also consider other criteria. Fontán and his team [16] pointed out that the functioning of preserved activities of daily living should also be included, since by observing the patient's level of autonomy, the cognitive mental state of the patient can be inferred. In this sense, Wadley, and his collaborators [17] were able to show the importance of studying cognitive impairment in activities of daily living, which are key to the autonomy and quality of life of older people. Recent studies reveal that functionality may be a prognostic factor in determining the degree of progression of deterioration to dementia in the short or medium term [[18], [19], [20]].
In this sense, it has been observed, that the functionality and autonomy of older adults have been negatively impacted by the confinement they had to maintain during the COVID-19 pandemic, as close contact with infected people increases the likelihood of infection [21]. Mobility restriction measures, although necessary for their health safeness, have significantly reduced the possibilities of social interaction and autonomy for the elderly population, generating situations of unwanted loneliness and greater vulnerability and cognitive deterioration due to lack of stimulation [22]. Hence the importance of enabling care alternatives that range from face-to-face care to a Tele neuropsychological (TeleNP) consultation that allows the necessary care to be provided to the elderly in any situation, especially in the pandemic circumstances that we have experienced lately [23].
Also, the World Alzheimer Report in 2022 estimates that 75% of people with dementia are not diagnosed globally, with that rate believed to rise as high as 90% in some lower-and middle-income countries (such as Mexico). But diagnosis is only the first, albeit arduous, step on the journey. Post-diagnosis support is often a daunting field to navigate, particularly when the systems meant to provide such support are confusing, limited, or outright non-existent depending on where one lives [24]. Hence the importance of early detection is to establish intervention strategies as soon as possible.
Given this scenario, it is a priority to develop early detection strategies that allow early intervention for this sector of the population, as well as to identify the key variables, such as the level of autonomy, that affect normal or pathological aging [25,26]. Furthermore, although old age seems to be associated with an increase in the probability of suffering from certain diseases, as well as experiencing a relative intellectual decline, not all cases evolve similarly, so it is important to explore possible predictors of cognitive decline in the elderly [27,28].
Therefore, this study focuses on the exploration and assessment of vulnerability to cognitive impairment in older adults through ICTS (Information Communication Technology Services) and the implementation of the APA TeleNP Guidelines [29]. The aim is to explore whether there is a relationship between the level of autonomy of older adults and their cognitive performance in screening tests (MOCA, CDT, and Word Accentuation Test [TAP]). Exploring predictors of cognitive impairment in the Mexican population over 60 years of age will allow for early attention that will lead to timely treatment. In addition, the use of an ICTS protocol will significantly broaden the spectrum of the older adult population that can be assessed in the future.
2. Methods
This research was conducted in a group of 47 persons, 34 of them women (72.3%), with an average age of 64.8 years (SD = 4.2, minimum = 60, maximum = 78). Inclusion criteria were that they were Mexican citizens, aged 60 years or older, had a minimum of 6 years of schooling, were not institutionalized, and had Spanish as their native language. Exclusion criteria were the previous diagnosis of cognitive impairment, subjects with depression and a history of psychiatric care, alcoholism or other addictions, and subjects with pharmacological treatment for heart conditions or hypertension.
For the selection of the sample, access was requested to geriatric centers known as day centers, which implies that the elderly people attend on daily bases, but are not institutionalized, they do not stay overnight. Given this sampling procedure, and the fact that no formal impairment assessment was used to accept/reject participants, we left open the possibility that some participants may have had some level of undiagnosed cognitive impairment. The cutoffs of the cognitive instruments described in the next paragraph were used to compare the cases detected by each screening method (MoCA, or CDT). Once contact was established with these institutions, authorization was requested to extend the invitation to participate in the study so that those interested could make an appointment for the online assessment through ICTs.
Before the implementation of the online protocol, a thorough pilot test was conducted with the population of interest to adapt the instruments: Montreal Cognitive Assessment (MOCA), Clock Drawing Test (CDT), Test of Word Accentuation (TAP), Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE) and the Activities of Daily Living Questionnaire (IDDD) to a TeleNP Assessment. Because the research was conducted at the height of the COVID-19 pandemic, all guidelines suggested by the American Psychological Association (APA) were followed in terms of the settings and conditions necessary for patients to feel comfortable and for the sessions to be as similar as possible to a face-to-face appointment [30].
The instruments used included the Montreal Cognitive Assessment (MOCA), Clock Drawing Test (CDT), Test of Word Accentuation (TAP), Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE), and the Activities of Daily Living Questionnaire (IDDD), all adapted into a TeleNP consultation. MoCA has evidence of validity to detect cognitive impairment in the Mexican population using a cutoff score of <26, also showing fair correlation with MMSE (kappa = 0.39), and good internal consistency reliability (Cronbach's alpha = 0.87) [31].
The specific Cacho version of the CDT used in this study has not been validated in the Mexican population, therefore, this is the first study, to our knowledge, that has used the scoring method proposed by Cacho [8], who proposes a cutoff score of <6 from a total of 10 points, in which a score below 6 would be an indicator of MCI. Related to that, another scoring method of the CDT [32] in a Mexican sample has shown good internal reliability (alpha = 0.75), good inter-rater reliability (ICC = 0.993), and good sensitivity (90%) and specificity (95%) for major neurocognitive disorders [33]. The TAP has no previous adaptation to the Mexican population, but it has shown good internal (alpha = 0.841) and test-retest (r = 0.908) reliability while showing convergent validity with WAIS-IV scores (r = 0.827) in a sample in Ecuador [34].
To assess the functionality and cognitive decline of those evaluated, we used the IQCODE a questionnaire that asks an informant (could be a close family member or a caregiver) about changes in an elderly person's everyday cognitive function. Although not validated, it has been used in the Mexican population, to determine the functional status of patients before and after a vascular stroke [35], using the cutoff suggested initially by Jorm which is the same cutoff used in this study (>57 indicates probable cognitive impairment who found it to have high internal reliability in the general population sample (alpha = 0.95) and reasonably high test-retest reliability over one year in the dementing sample (r = 0.75). The total IQCODE score, as well as each of the 26 items, was found to discriminate well between the general population and dementing samples [36].
Regarding the level of autonomy, an IDDD interview was conducted with the informants, previous studies had shown that people with mild dementia are impaired to different degrees in their initiative and performance of instrumental activities of daily living and that impairments relating to social activities particularly relate to well-being [37]. There is a study that presented an adaptation and validation of the IDDD for Spanish-speaking communities, in which the IDDD demonstrated great internal consistency (α = 0.985) and reproducibility (intraclass correlation coefficient = 0.94). Correlations were high (r = 0.81), showing the Spanish-IDDD is a reliable adaptation of the original IDDD scale and may be used successfully in Spanish -speaking populations for staging and follow-up of subjects with dementia, therefore it was used in this study with the same score references ([33–36] Normal, 37–40 MCI Indicators, >40 Cognitive impairment indicators in different degrees of severity) [38].
The application of the protocol was conducted in a 45-min online session via Zoom, of which the first part (30 min) was with the patient and the second (15 min) was with the key informant (family member or caregiver). The older adult was evaluated by implementing the TeleNP adapted versions of MoCA, CDT (Order and Copy), to assess cognitive status, and the TAP to ascertain cognitive reserve. The key informant was asked to answer the IDDD questionnaire to assess the level of autonomy, and the IQCODE to know his or her appreciation of the patient's cognitive decline.
3. Results
The descriptive of the variables (socio-demographic, health, and cognitive), and summary data are presented in Table 1, where it can be inferred that most of this study sample were women (72.3%), with higher education (68.1%), and who don't live alone (89.4%). Regarding health variables, most of the sample did not report cardiovascular risk (87.2%), diabetes (80.9%), or hypertension (68.1%), and most of them take medication (57.4%). Also, most of the participants do not smoke tobacco (95.7%) nor drink alcohol (85.1%).
Table 1.
Descriptive data of sociodemographic variables.
| Variable | Value |
|---|---|
| Gender | |
| Feminine (%) | 34 (72.3) |
| Masculine (%) | 13 (27.7) |
| Average Age (DE) | 64.8 (4.2) |
| Average years of study (DE) | 17.2 (4.7) |
| Educational level | |
| Postgraduate (%) | 19 (40.4) |
| Bachelor's degree (%) | 13 (27.7) |
| Technical Education (%) | 4 (8.51) |
| High School (%) | 3 (6.38) |
| Secondary School(%) | 5 (10.6) |
| Elementary School (%) | 3 (6.38) |
| Whom do they live with | |
| Alone (%) | 5 (10.6) |
| Accompanied (%) | 42 (89.4) |
| Cardiovascular risk | |
| Yes | 6 (12.8) |
| No | 41 (87.2) |
| Diabetes | |
| Yes | 9 (19.1) |
| No | 38 (80.9) |
| High blood pressure | |
| Yes | 15 (31.9) |
| No | 32 (68.1) |
| Medication | |
| Yes | 27 (57.4) |
| No | 20 (42.6) |
| Smoke | |
| Yes | 2 (4.26) |
| No | 45 (95.7) |
| Alcohol | |
| Sí | 7 (14.9) |
| No | 40 (85.1) |
Table 2 shows the descriptive results for the cognitive impairment indicator scores on the MOCA, Clock Drawing Test on command (CDT-CM), and Copied Clock Drawing Test (CDT-CP), as well as the IQCODE, TAP, and IDDD.
Table 2.
Descriptive data of cognitive variables (MoCA, Clock Drawing Test-Command condition (CDT-CM), and Clock Drawing Test-Copy condition (CDT-CP), Improvement pattern (CDT-IP), IQCODE), premorbid level (Word Accentuation Test, TAP), and autonomy (IDDD).
| Instrument | Mean (SD) | Min | Max | Skewness (SD) | Kurtosis (SD) | Shapiro-Wilk's p-value |
|---|---|---|---|---|---|---|
| MoCA | 25.8 (3.2) | 18 | 30 | −0.8 (0.3) | −0.3 (0.7) | 0.003 |
| CDT-CM | 8.9 (1.6) | 4 | 10 | −1.4 (0.3) | 1.2 (0.7) | <0.001 |
| CDT-CP | 9.6 (0.7) | 8 | 10 | −1.5 (0.3) | 1.0 (0.7) | <0.001 |
| CDT-IP | 0.65 (1.2) | 0 | 5.5 | 2.3 (0.3) | 6.1 (0.7) | <0.001 |
| TAP | 25.3 (2.9) | 19 | 30 | −0.2 (0.3) | −0.8 (0.7) | 0.094 |
| IQCODE | 50.7 (8.5) | 25 | 70 | −0.9 (0.3) | 1.9 (0.7) | <0.001 |
| IDDD | 35.1 (3.0) | 33 | 47 | 1.9 (0.3) | 4.4 (0.7) | <0.001 |
The statistical analyses (Pearson's correlation) of the association between autonomy and cognitive variables are presented below, the results show a moderately significant correlation between the level of autonomy and cognitive performance in MOCA and CDT.
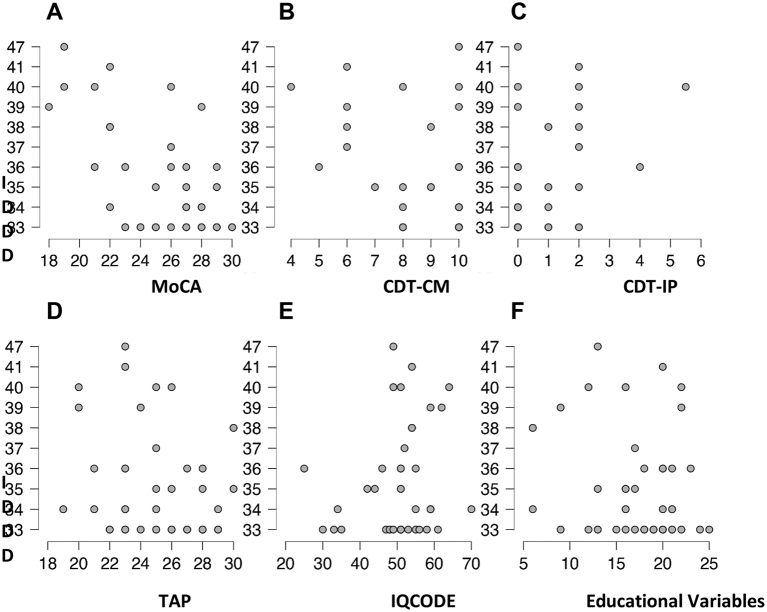
Table 3 presents the correlation between the IDDD Questionnaire and MOCA scores, with a significant negative correlation of −0.793 and a p-value of 0.011. As for the level of autonomy and the CDT, there is a tendency towards a significant correlation. Concerning the level of autonomy and the presence of the CDT-IP Improvement Pattern (IP), a significant correlation of 0.716 and a p-value of 0.046 is obtained, which implies that some of the patients who obtain the IP of the CDT(which is an indicator of mild cognitive impairment) also score low results in their levels of autonomy (Fig. 1C).
Table 3.
Correlation matrix between cognitive variables (MoCA, CDT-CM, CDT-IP, IQCODE), premorbid cognition (TAP), and educational variables.
| Variable | IDDD | MOCA | CDT-CM | CDT-IP | TAP | IQCODE | |
|---|---|---|---|---|---|---|---|
| MoCA | Pearson's r | −0.616*** | |||||
| p-value | <0.001 | ||||||
| CDT-CM | Pearson's r | −0.355* | 0.424** | ||||
| p-value | 0.014 | 0.003 | |||||
| CDT-IP | Pearson's r | 0.366* | −0.423** | −0.902*** | |||
| p-value | 0.011 | 0.003 | <0.001 | ||||
| TAP | Pearson's r | −0.226 | 0.285 | 0.043 | −0.062 | ||
| p-value | 0.127 | 0.052 | 0.773 | 0.680 | |||
| IQCODE | Pearson's r | 0.143 | −0.344* | −0.252 | 0.240 | −0.123 | |
| p-value | 0.337 | 0.018 | 0.087 | 0.104 | 0.411 | ||
| Educational Variables | Pearson's r | −0.231 | 0.450** | 0.312* | −0.270 | 0.141 | −0.212 |
| p-value | 0.117 | 0.002 | 0.033 | 0.067 | 0.343 | 0.152 |
Fig. 1.
Scatterplots of the relation between IDDD and MOCA (A), TRO (B), IP (C), TAP (D), IQCODE (E), and educational variables (F).
Finally, the correlation between the scores obtained in the tests that assess the cognitive status of the participating subjects was analyzed (Table 3), finding a positive correlation between the MOCA and CDT scores of 0.424 (p = .003), which indicates a moderate correlation. As for the association between the MOCA scores and the CDT-IP in the detection of Mild Cognitive Impairment with the results analyzed so far, no significant correlation is observed.
However, in the scattering data of the results, it is observed that some patients who present the IP between CDT-CM and CDT-CP, also present scores that, according to the MOCA cut-off point (Mild Cognitive Impairment Indicator ≤20) could indicate the presence of mild cognitive impairment, it will be closely observed how the correlation between these scores (MOCA-IP) behaves once the sample is enlarged.
Regarding the difference in the relationships between autonomy and cognitive decline we have found that cognitive status (assessed with MoCA) is related to educational variables and IQCODE, but autonomy is not as shown in Table 3. And on the CDT only the score CDT-CM correlates with cognitive reserve (Educational variables), but not with the CDT-IP.
Lastly, it is worth noting a relevant result regarding the greater potential sensitivity of CDT over MoCA in this population. Thus, of the 39 cases classified in the normal range by MoCA, 6 cases (12.8%) were classified as impaired by CDT-IP (see Table 4). For epidemiological studies on such large population sectors, such as the high proportion of the population over 60 years of age (both in Mexico and in other countries), this data provides an extremely useful measure for case-non-case differentiation. If, in addition to that, the fact that it has been explored through a tele neuropsychological application such as the one conducted for this study highlights the importance of using ICTs in near future with older people.
Table 4.
Comparison between MoCA and Improvement Pattern of the Clock Drawing Test (CDT-IP), in the classification of detected cognitive impairment.
| CDT-IP Category |
||||
|---|---|---|---|---|
| MoCA Category | No | Yes | Total | |
| Normal | Count | 33 | 6 | 39 |
| % of total | 70.2% | 12.8% | 83.0% | |
| MCI | Count | 1 | 3 | 4 |
| % of total | 2.1% | 6.4% | 8.5% | |
| Cognitive Impairment | Count | 1 | 3 | 4 |
| % of total | 2.1% | 6.4% | 8.5% | |
| Total | Count | 35.000 | 12.000 | 47.000 |
| % of total | 74.468% | 25.532% | 100.000% | |
4. Discussion and conclusión
In a post-pandemic stage, in which the health programs interrupted in the critical phases of COVID-19 are being recovered, the older adult population must be among the priorities to be addressed. For this reason, the assessment developed using ICTs, with a protocol composed of valid and reliable tests in both face-to-face and telematic environments, is relevant to respond to this challenge. It should be noticed how the Primary Health Care systems have been insufficient, limited, and collapsed because of the coronavirus pandemic, and the first that was left behind because of this were the elderly. We must therefore continue to increase this line of screening of the processes of deterioration with procedures based on Teleneuropsychology.
Regarding the results obtained, we can point out that they indicate the presence of a correlation between the level of autonomy and cognitive impairment, as stated in the hypothesis: The higher the level of autonomy, the lower the cognitive impairment, and conversely, the lower the level of autonomy, the greater the mild cognitive impairment in the older adults participating in the study. This is evidence contrasted with previous studies [8,39].
Significant data is obtained between the variables of autonomy and cognitive impairment, as well as in the resulting values of the IDDD and the CDT, but no such significance is found between autonomy and the CDT-IP. In the statistical analyses, a correlation has also been observed that appears to be significant between the instruments used to assess the general cognitive status and to identify indicators of cognitive impairment, i.e., patients who obtain scores on the MOCA that indicate possible cognitive impairment also obtain indicators of cognitive impairment on the CDT with the presence of IP. This is important because the discrepancy of two points of improvement between the CDT-CM and the CDT-DP could be indicative of cognitive impairment associated with the early stages of Alzheimer's disease, which is consistent with other studies [41].
On the other hand, there are previous studies that suggest that functionality might be a prognostic factor in determining the progression from mild cognitive impairment to dementia in the short or medium term [42], therefore the importance of assessing autonomy as an essential criterion when evaluating older people cognitive status, which should include not only cognitive tests but also address the use of these cognitive skills in daily life activities [43] without leaving aside the cognitive reserve [44], although the results in our study are not entirely consistent, perhaps due to the small sample size.
For the moment, with this study, it can be inferred that the sample needs to be enlarged to consolidate a significant correlation between the variables involved. However, in the dispersion of the scores obtained (Fig. 1), a trend can be observed that may lead us to think that the hypothesis can be accepted with a greater population representation. In this sense, it is important to point out that an international study is being conducted using the same protocol and methodology mediated by ICTs in other countries (Spain and Chile), to alleviate the limitations pointed out in the present study.
In a recent review on the subject in Spanish [45], it is noted that among the most used tests are two used in our work (MoCA and Clock DrawingTest). And as they require visuospatial skills, the adaptations coincide with asking the participant to show the camera the drawings so that once completed they can be corrected by the examiner at that moment. We used screen capture to leave permanent evidence. It was not necessary to control for the learning effect, as in some studies, which used two alternative forms of the tests administered in a counterbalanced manner.
Regarding the place of administration of the tests through TeleNP, the evaluation was carried out in the participants' homes or the senior centers, depending on personal circumstances in terms of technical availability. The authors of the paper point out that a progressive improvement of both the equipment and the videoconferencing systems used for TeleNP is observed since in recent years different platforms have been developed that allow online videoconferencing (Zoom in our case with a non-encrypted network).
What is relevant is that most of the works have assessed the differences in the mean test scores across modalities and/or the correlations between the two modalities, through the Intraclass Correlation Coefficient (ICC). Overall, the results support TeleNP as a viable and acceptable method for assessing cognitive functioning in healthy and neurologically and psychiatrically impaired individuals.
4.1. Innovation
The implementation of active cognitive stimulation strategies is essential for healthy aging and for improving CR [[46], [47], [48]]. Nowadays, older adults are increasingly using ICTs, which is a way to stimulate cognitive processes and facilitate social participation and personal development [49]. Along these lines, the Prototype of intervention and training in cognitive reserve in active aging (RESCOG-TALENT) has been developed [50]. To work on this concept, a “Cognitive Reserve Savings Chart” was developed, consisting of three types of reserve: cognitive, emotional, and physical.
To this end, a website (https://rescogtalent.wordpress.com) was developed containing the three types of savings (cognitive, emotional, and physical), with various activities suggested for completing their own savings booklet in these areas. This project was focused on and designed to improve the quality of life of the elderly, as the literature indicates that the key to optimal aging is to work on prevention with this population.
Illustration 1.
Cognitive reserve innovation project Rescog-Talent website.
We consider this study highly innovative because most of the innovations applying ICTs to caregivers [51] have focused on intervention on dementia awareness or coping skills (behavioral alterations, emotional self-care). Moreover, the protocols for MCI screening through ICTs (online assessment), are based solely on information from the caregiver (professional or family member). In our investigation, we combine an objective assessment of cognitive performance and associated variables with the tests answered by the key informant (caregivers).
Therefore, both types of information sources allow screening with fewer false positives (the problem of unnecessary costs of confirming the diagnosis) and fewer false negatives (with the implications of the consequences of late diagnosis of the disease and its therapeutic possibilities). The following illustration outlines the evaluation model used, showing the strengths highlighted, as well as the innovation provided (Illustration 2).
Illustration 2.
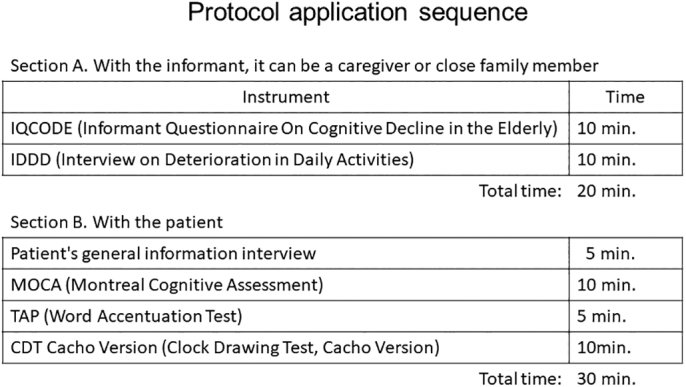
Protocol application sequence.
5. Conclusion
The results of this study allow us to conclude that the screening protocol used for the assessment of vulnerability to cognitive impairment of older adults through ICTs presents optimal levels of usability both for professionals and for the targeted adults and their caregivers. The correlation between the level of autonomy of older adults and their cognitive performance (MOCA and CDT and cognitive reserve (TAP) have been demonstrated, although the CR variable is less consistent in comparison to what is reported in the literature. A Tele neuropsychological assessment implementation to identify predictors of cognitive impairment in the Mexican population over 60 years of age, with the protocol described in this paper, will enable early detection in large sectors of the population of older adults. Moreover, when “suspicious cases” are confirmed with a Cognitive Impairment condition or dementia diagnosis, proper intervention with both pharmacological and non-pharmacological therapies will be possible.
Lastly, despite the limitations (cross-sectional study or non-random sampling), the exploratory nature of this study is consistent with recent lines of research on the controversy concerning the highly discriminatory use of some tests [51], which are precisely those used in our study (MOCA, CDT). The innovative addition is the use of ICTs to face the challenge of the large undiagnosed elderly population (World Alzheimer Report, 2022), along with the added difficulties of using traditional methods of screening.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit organizations.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We thank CETYS Universidad for the support staff, the availability of the laboratories, the administrative permissions, and the positive report from the ethics committee (D-CEI055).
References
- 1.Phillips C. Lifestyle modulators of neuroplasticity: how physical activity, mental engagement, and diet promote cognitive health during aging. Neural Plast. 2017;2017:3589271. doi: 10.1155/2017/3589271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tisnés A., Salazar-Acosta L.M. Envejecimiento poblacional en Argentina:¿ qué es ser un adulto mayor en Argentina? Una aproximación desde el enfoque de la vulnerabilidad social. Papeles de población. 2016;22(88):209–236. [Google Scholar]
- 3.Borrás B.C., Viña R.J. Neurofisiología y envejecimiento. Concepto y bases fisiopatológicas del deterioro cognitivo. Rev Esp Geriatr Gerontol. 2016;51:3–6. doi: 10.1016/S0211-139X(16)30136-6. [DOI] [PubMed] [Google Scholar]
- 4.Zamora-Macorra M., de Castro E.F., Ávila-Funes J.A., Manrique-Espinoza B.S., López-Ridaura R., Sosa-Ortiz A.L., et al. The association between social support and cognitive function in Mexican adults aged 50 and older. Arch. Gerontol. Geriatr. 2017;68:113–118. doi: 10.1016/j.archger.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 5.Feng D., Ji L., Xu L. Mediating effect of social support on the association between functional disability and psychological distress in older adults in rural China: does age make a difference? PLoS One. 2014;9 doi: 10.1371/journal.pone.0100945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clemente Y., García J., Méndez I. Memoria, funciones ejecutivas y deterioro cognitivo en población anciana. EUR. J. Investig. Psicología de la Salud Educ. 2015;5(2):153–163. doi: 10.1989/ejihpe.v5i2.108. [DOI] [Google Scholar]
- 7.American Psychiatric Association (APA) Fifth Edition. American Psychiatric Association; Arlington, VA: 2013. Diagnostic and Statistical Manual of Mental Disorders (DSM-V) [Google Scholar]
- 8.Cacho J., García-García R., Fernández-Calvo B., Gamazo S., Rodríguez-Pérez R., Almeida A., et al. Improvement pattern in the clock drawing test in early Alzheimer’s disease. Eur. Neurol. 2005;53(3):140–145. doi: 10.1159/000085832. [DOI] [PubMed] [Google Scholar]
- 9.Mias C., y Causse, M.B Quejas subjetivas de memoria, desempeño objetivo y funciones neuropsicológicas relacionadas. Una revisión sistemática. Revista Perspectivas Metodológicas. 2021;21(e3440):1. doi: 10.18294/pm.2021.3440. [DOI] [Google Scholar]
- 10.Zuroff L., Wisse L.E., Glenn T., Xie S.X., Nasrallah I.M., Habes M., et al. Self- and Partner-Reported Subjective Memory Complaints: Association with Objective Cognitive Impairment and Risk of Decline. J. Alzheimer’s Dis. Rep. 2022;6(1):411–430. doi: 10.3233/ADR-220013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stern Y. What is cognitive reserve? Theory and research application of the reserve concept. JINS. 2002;8:448–460. [PubMed] [Google Scholar]
- 12.La Barba P. reserva cognitiva como prevención en el deterioro de las funciones neurocognitivas en la vejez. Rev. Invest. Cien Edu. 2021;5(20):1074–1083. doi: 10.33996/revistahorizontes.v5i20.258. [DOI] [Google Scholar]
- 13.Wöbbeking M., Bonete B., Cabaco A.S., Urchaga-Litago J.D., Afonso R.M. Relationship between Cognitive Reserve and Cognitive Impairment in Autonomous and Institutionalized Older Adults. Int. J. Environ. Res. Public Health. 2020;17:5777. doi: 10.3390/ijerph17165777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wöbbeking M., Cabaco A., Bonete B., Urchaga J.D., Loureiro M.J., y Mejía M Physical Activity, and Life satisfaction: An empirical study in a population of senior citizens. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.636914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Belleville S., Mellah S., Boller B., Ouellet E. Activation changes induced by cognitive training are consistent with an improved cognitive reserve in older adults with subjective cognitive decline. Neurobiol. Aging. 2022;121:107–118. doi: 10.1016/j.neurobiolaging.2022.10.010. In this issue. [DOI] [PubMed] [Google Scholar]
- 16.Fontán L.E., Lorenzo J., Silveria A. Perfil de Alteración en el Mini-Mental State Examination en pacientes con deterioro cognitivo leve. Rev. Neurol. 2004;39:316–321. [PubMed] [Google Scholar]
- 17.Wadley V.G., Crowe M., Mariske M., Cook S.E., Unverzagt F.W., Rosenber A.L., et al. Changes in everyday function in individuals with psychometrically defined mild cognitive impairment in the advance cognitive training for independent and vital elderly study. J. Am. Geriatr. Soc. 2007;55:1192–1198. doi: 10.1111/j.1532-5415.2007.01245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harrison J.K., Noel-Storr A.H., Demeyere N., Reynish E.L., Quinn T.J. Outcomes measures in a decade of dementia and mild cognitive impairment trials. Alzheimers Res. Ther. 2016;8(1):1–10. doi: 10.1186/s13195-016-0216-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beishon L., Haunton V.J., Panerai R.B., Robinson T.G. Cerebral hemodynamics in mild cognitive impairment: a systematic review. J. Alzheimers Dis. 2017;59(1):369–385. doi: 10.3233/JAD-170181. [DOI] [PubMed] [Google Scholar]
- 20.Lek-Ahmadi M. Reversion from mild cognitive impairment to normal cognition. J. Alzheimers Dis. 2016;30(4):324–330. doi: 10.1097/WAD.0000000000000145. [DOI] [PubMed] [Google Scholar]
- 21.Rejón A., Rodríguez Y., Lima H., Hernández N., Martínez-G B.M. Deterioro cognitivo leve en ancianos hospitalizados en el servicio de Geriatría. Hospital Clínico Quirúrgico “Comandante Faustino Pérez Hernández” 2016-2017. Dominio de las Ciencias. 2021;7(1):346–363. [Google Scholar]
- 22.Shen H.T., Zhu X., Zhang Z., Wang S.H., Chen Y., Xu X., et al. Heterogeneous data fusion for predicting mild cognitive impairment conversion. In Fusion. 2021;66(3):54–63. doi: 10.1016/j.inffus.2020.08.023. [DOI] [Google Scholar]
- 23.Mera A., Tabares-González E., Montoya-González S., Muñoz-Rodríguez D., Monsalve Vélez F. Recomendaciones prácticas para evitar el desacondicionamiento físico durante el confinamiento por pandemia asociada a COVID-19. Universidad Y Salud. 2020;22(2):166–177. doi: 10.22267/rus.202202.188. [DOI] [Google Scholar]
- 24.World Alzheimer Report 2022. wwwalzintorg [Internet] 2022. https://www.alzint.org/resource/world-alzheimer-report-2022/ Available from:
- 25.Cullen N.C., Leuzy A., Palmqvist S., Janelidze S., Stomrud E., Pesini P., et al. Individualized prognosis of cognitive decline and dementia in mild cognitive impairment based on plasma biomarker combinations. Aging. 2021;1(1):114–123. doi: 10.1038/s43587-020-00003-5. [DOI] [PubMed] [Google Scholar]
- 26.Cancino M., Rehbein L. Factores de riesgo y precursores del Deterioro Cognitivo Leve (DCL): Una mirada sinóptica. Ter. Psicol. 2016;34(3):183–189. doi: 10.4067/S0718-48082016000300002. [DOI] [Google Scholar]
- 27.Cheng Y.W., Chen T.F., Chiu M.J. From mild cognitive impairment to subjective cognitive decline: conceptual and methodological evolution. Clin. Child Psychol. Psychiatry. 2017;13:491. doi: 10.2147/NDT.S123428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fonte T., Santos D.J. Deterioro cognitivo leve en personas mayores de 85 años. Rev. Cubana Med. 2020;59(1):1–13. [Google Scholar]
- 29.Tele-Neuropsychology Guidelines [Internet] Inter Organizational Practice Committee. 2022. https://iopc.online/teleneuropsychology-guidelines Available from:
- 30.Martínez-Ramírez D., Rodríguez-Violante M., González-Latapi P., Cervantes-Arriaga A., Camacho-Ordoñez A., Morales-Briceño H., et al. Comparison of the Montreal Cognitive Assessment and Mini Mental State Examination Performance in Patients with Parkinson’s disease with w Low Educational Background. Res. Neurol. Int. J. 2014;1–7 doi: 10.5171/2014.773162. [DOI] [Google Scholar]
- 31.Parsey C.M., Schmitter-Edgecombe M. Quantitative and qualitative analyses of the clock drawing test in mild cognitive impairment and Alzheimer disease: evaluation of a modified scoring system. J. Geriatr. Psychiatry Neurol. 2011;24(2):108–118. doi: 10.1177/0891988711402349. [DOI] [PubMed] [Google Scholar]
- 32.Aguilar-Navarro S.G., Mimenza-Alvarado A.J., Palacios-García A.A., Samudio-Cruz A., Gutiérrez-Gutiérrez L.A., Ávila-Funes J.A. Validity and Reliability of the Spanish Version of the Montreal Cognitive Assessment (MoCA) for the Detection of Cognitive Impairment in Mexico. Rev. Colomb Psiquiatr (Engl Ed). 2018;47(4):237–243. doi: 10.1016/j.rcp.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 33.Graham Pluck PhD, Almeida Meza P., González-Lorza M., Muñoz-Ycaza R.A., Trueba A. Estimation of Premorbid Cognitive Function With the Word Accentuation Test. Rev. Ecuat. Neurol. 2017:26 (3). [Google Scholar]
- 34.Galos E.G., Petersen R.C. Mild cognitive impairment in geriatrics. Clin. Geriatr. Med. 2018;34(4):563–589. doi: 10.1016/j.cger.2018.06.005. [DOI] [PubMed] [Google Scholar]
- 35.Arauz A., Rodríguez-Agudelo Y., Sosa A.L., Chávez M., Paz F., González M., et al. Vascular cognitive disorders and depression after first-ever stroke: the Fogarty-Mexico Stroke Cohort. Cerebrovasc. Dis. 2014;38(4):284–289. doi: 10.1159/000366471. (Epub 2014 Nov 20. PMID: 25412708) [DOI] [PubMed] [Google Scholar]
- 36.Jorm A.F., Jacomb P.A. The Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE): socio-demographic correlates, reliability, validity and some norms. Psychol. Med. 1989;19(4):1015–1022. doi: 10.1017/s0033291700005742. (PMID: 2594878) [DOI] [PubMed] [Google Scholar]
- 37.Giebel C.M., Challis D.J., Montaldi D. A revised interview for deterioration in daily living activities in dementia reveals the relationship between social activities and well-being. Dementia (London). 2016;15(5):1068–1081. doi: 10.1177/1471301214553614. (Epub 2014 Oct 2. PMID: 25280491) [DOI] [PubMed] [Google Scholar]
- 38.Böhm P., Peña-Casanova J., Aguilar M., Hernández G., Sol J.M., Blesa R. Clinical validity and utility of the interview for deterioration of daily living in dementia for Spanish-speaking communities NORMACODEM Group. Int. Psychogeriatr. 1998;10(3):261–270. doi: 10.1017/s1041610298005377. (PMID: 9785147) [DOI] [PubMed] [Google Scholar]
- 39.Vassilaki M., Aakre J.A., Cha R.H., Kremers W.K., Sauver J.L., Mielke M.M., et al. Multimorbidity and risk of mild cognitive impairment. J American Geriatr Soc. 2015;63(9):1783–1790. doi: 10.1111/jgs.13612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Peres K., Chrysostome V., Fabrigoule C., Orgogozo J.M., Dartigues J.F. Restriction in complex Activities of daily living in MCI: Impact of outcomes. Neurology. 2006;67:461–466. doi: 10.1212/01.wnl.0000228228.70065.f1. [DOI] [PubMed] [Google Scholar]
- 42.De Simone M.S., Perri R., Fadda L., Caltagirone C., Carlesimo G.A. Predicting progression to Alzheimer’s disease in subjects with amnestic mild cognitive impairment using performance on recall and recognition tests. J. Neurol. 2019;266(1):102–111. doi: 10.1007/s00415-018-9108-0. [DOI] [PubMed] [Google Scholar]
- 43.Feldberg C., Tartaglini M.F., Hermida P.D., Moya-García L., Licenciada-Caruso D., Stefani D., et al. El rol de la reserva cognitiva en la progresión del deterioro cognitivo leve a demencia: un estudio de cohorte. Neurol. Argentina. 2021;13(1):14–23. [Google Scholar]
- 44.Pérez P., Ramos D. Teleneuropsicología en países de habla hispana: Una mirada crítica al uso de Tecnologías de Información y Comunicación en la evaluación neuropsicológica. Revista Iberoamericana de Neuropsicología. 2021;4(1):1–27. [Google Scholar]
- 45.Wöbbeking M., Cabaco A.S., Urchaga J.D., Sitges E., Bonete B. Reserva Cognitiva: Un análisis bibliométrico desde su implantación hasta la actualidad. Revista de Psicología de la Salud. 2017;5(1):86–113. [Google Scholar]
- 46.Sánchez N., Cabaco A., Urchaga J.D., Villasan A. Aplicación de técnicas de estimulación cognitiva en envejecimiento utilizando TIC: Estudio de caso. Neurama. 2019;6(1):40–47. [Google Scholar]
- 47.Lázara V., Viteri E., Terranova E., Ordoñez S. Nuevas tecnologías de la comunicación y capacidad cognitiva de los adultos mayores. Universidad, ciencia y tecnología. 2018;22(89):82–87. [Google Scholar]
- 48.Cotten S.R. Examining the Roles of Technology in Aging and Quality of Life. J. Gerontol. B Psychol. Sci. Soc. Sci. 2017;72(5):823–882. doi: 10.1093/geronb/gbx109. [DOI] [PubMed] [Google Scholar]
- 49.Cabaco A., Bonete B., Wobbeking M. Club Universitario de Innovación. Universidad Pontificia de Salamanca; 2017. Prototipo de intervención y formación en reserva cognitiva en envejecimiento activo. (RESCOG-TALENT) [Google Scholar]
- 50.Sitges-Maciá E., Bonete-López B., Sánchez-Cabaco A., Oltra-Cucarella J. Effects of e-Health Training and Social Support Interventions for Informal Caregivers of People with Dementia—A Narrative Review. Int. J. Environ. Res. Public Health. 2021;18:7728. doi: 10.3390/ijerph18157728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Costa S., St George R.J., McDonald J.S., Wang X., Alty J. Diagnostic Accuracy of the Overlapping Infinity Loops, Wire Cube, and Clock Drawing Tests in Subjective Cognitive Decline, Mild Cognitive Impairment, and Dementia. Geriatrics. 2022;7:72. doi: 10.3390/geriatrics7040072. [DOI] [PMC free article] [PubMed] [Google Scholar]