Abstract
Objective
To understand parents' of children with developmental and epileptic encephalopathies needs and preferences for psychological resources.
Methods
Using a person-based approach, a multidisciplinary panel of clinician and researchers (n = 9) hosted a priority-setting workshop to 1) understand parents' needs and preferences for psychological resources and 2) to develop ‘guiding principles’ to inform a future suite of psychological resources. The multidisciplinary panel analysed the parent priority-setting workshop data, using a combination of thematic and lexical analysis.
Results
Thematic analysis identified six key domains wherein parents (n = 8) prioritised a need for psychological resources to support adaptation to their child's genetic DEE diagnosis. Lexical analysis revealed that connection to diagnosis-specific resources provided a pathway to promote enhanced psychological adaptation, by reducing social isolation and reorienting parents towards feelings of hope. Combination of both analyses generated six thematic informed ‘guiding principles’.
Conclusion
Codesigned psychological resources may help parents to cope with the unique and complex interplay of stressors associated with their child's DEE diagnosis and treatment. Our ‘guiding principles’ will be translated to inform a future suite of tailored psychological resources.
Innovation
This study demonstrates an innovative codesign approach to inform tailored psychological resources for families of children with rare genetic conditions.
Keywords: Person-based, Qualitative research, Codesign, Positive psychology, Parent mental health
Highlights
-
•
There is a deficit of research exploring the psychological impacts of parenting children with genetic DEEs.
-
•
Tailored and codesigned psychological resources are essential due to the complexity and uniqueness of genetic DEEs.
-
•
We collaborated with parents to codesign the content and scope of a future suite of person-based psychological resources.
-
•
Thematic and lexical analyses combined identified that person-based resources reduced parent isolation and promoted hope.
-
•
Insights generated from this study will be applied to inform psychological resources tailored for rare disease families.
1. Introduction
Developmental and epileptic encephalopathies (DEEs) represent a group of severe epilepsies of infancy, associated with frequent, treatment-resistant seizures and impact on development [1]. Long-term prognoses are typically poor, with complex co-morbidities, associated with neurocognitive and psychological decline, vastly reduced quality of life and heightened risk of premature death [2]. Advances in genetic testing have revolutionised DEE diagnostics and we now understand that a large proportion of childhood onset DEEs are due to individually rare genetic causes [3,4]. However, despite the promise of ‘precision medicine’, an aetiological diagnosis rarely translates into targeted treatments and children are frequently trialled on multiple antiepileptics, specialist diets and, in some cases, epilepsy surgery.
There is emerging evidence associating poor psychological outcomes among parents, with a paucity of psychological resources tailored to support unique challenges associated with their child's genetic DEE diagnosis [[5], [6], [7], [8], [9]]. Psychological resources comprise psychotherapeutic interventions developed with intent to improve parents emotional or psychological wellbeing by altering their cognitions and behaviour [10]. Engaging parents of children with genetic DEEs to understand their perspectives, needs and preferences for psychological resources is a pivotal first step to codesign tailored psychological resources that are likely to have meaningful and beneficial impact [8,11]. However, despite international research calls to support parents' psychological functioning [12], knowledge to inform the development of psychological resources that support parents facing a complex genetic DEE diagnosis in their child is limited [6,13].
Recognising the limitations of the available literature, this research adopted a person-based framework [14,15], to actively partner with parents, to understand their perspectives, needs and preferences for diagnosis-specific psychological resources. The person-based framework focuses on consulting and working together with relevant stakeholders, including parents and multidisciplinary clinicians providing care for children with genetic DEEs [16,17]. The involvement of multidisciplinary clinicians in the design of tailored resources is also crucial, as they are the interface of the healthcare system to parents [18]. Prior to the current study, the researchers conducted a systematic review of the literature [7] and an in-depth interview study with parents to explore the psychosocial impacts of receiving genetic testing for their child's DEE [6]. Both studies identified a clear need to improve psychosocial resources, highlighting a need for tailored psychological resources to be integrated into healthcare services for families undergoing genetic testing for their child's DEE. However, they did not illuminate how to design psychological resources that offer appropriate support to parents. To better understand how to build psychological resources for parents of children with genetic DEEs, we report here the findings of a priority-setting workshop with parents to:
-
(1)
Understand parents' perspectives, needs and preferences for psychological resources.
-
(2)
Identify ‘guiding principles’ to inform the content, scope and features of future psychological resources, based on key themes derived from the priority-setting workshop.
A priority-setting workshop was used as this offers a research design that 1) facilitates cross-pollination of opinions, enabling participants to build on or negate the ideas of fellow participants [19] and 2) produces transcripts that are appropriate for thematic and lexical analysis [20].
2. Methods
2.1. Design
The first key element of the person-based approach involves qualitative research to gain deep understanding of the psychosocial context of parents and their perspectives and preferences for a future suite of psychological resources [14,15]. Insights from this stage can be iteratively incorporated to modify the design of the resources, to make them more relevant, engaging and meaningful to the intended target users. The second element of the person-based approach is to identify ‘guiding principles’, derived from the qualitative data. Thematically-derived ‘guiding principles’ can inform the development of psychological resources by highlighting pathways through which the resources can address predefined context-specific issues.
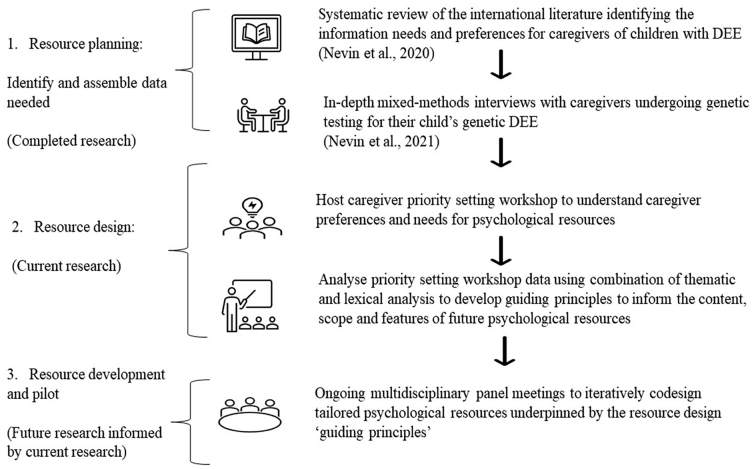
A flow chart of the study is provided in Fig. 1. which summarises our application of a person-based approach to develop a future suite of psychological resources.
Fig. 1.
Stages of person-based approach to inform a suite of psychological resources.
Nine multidisciplinary clinicians, including representatives from neurology, genetics, and psychiatry, and behavioural scientists, who provide healthcare services to children and families with genetic DEEs were invited to participate in a multidisciplinary panel. Guided by the aforementioned systematic literature review [7], and prior in-depth interviews with parents of a child with DEE [6] (Fig. 1), the goal of the multidisciplinary panel was to (1) prepare materials for the priority-setting workshop, (2) to examine the qualitative data that emerged from the parent priority-setting workshop and (3) to develop guiding principles to inform a future suite of psychological resources tailored for parents of children with DEEs. The multidisciplinary panel developed a purpose-designed workshop schedule which comprised open-ended, semi-structured questions to explore parents' needs and preferences regarding the course, scope, and features of psychological resources (Supplementary Appendix A). In addition, the multidisciplinary panel prepared a PowerPoint presentation for display during the parent priority-setting workshop which included an overview of the parent workshop objectives, and a presentation of the results from the in-depth interviews previously conducted with parents of children with genetic DEEs [6].
2.2. Participants
We recruited 13 parents of a child (<18 years old) with a confirmed or suspected genetic DEE, to participate in a parent priority-setting workshop via email. Eight parents (n = 8) of patients from the Sydney Children's Hospital Network accepted our invitation to participate in the priority-setting workshop. Prior to the scheduled workshop, parents were mailed the PowerPoint presentation, prepared by the multidisciplinary panel (described above) and were informed that their contribution during the workshop would guide the development of a suite of psychological resources tailored for parents of children with genetic DEEs. Participation was voluntary and no compensation was provided. Parent confidentiality was maintained and to preserve participant privacy limited demographic details were collected (Table 1). Ethics approval for this study was granted by the hospital human research ethics review board (HREC LNR/18/SCHN/10).
Table 1.
Parent participant and child with genetic DEE demographics.
| Parent participant age (years) | N = 8 |
|---|---|
| Mean (SD) | 40 (3.4) |
| Range | 34–45 |
| Sex | N = 8 |
| Male | 1 |
| Female | 7 |
| Employment status | N = 8 |
| Employed | 6 |
| Full-time caregiver | 2 |
| Marital Status | N = 8 |
| Married / de facto | 7 |
| Separated | 1 |
| Child with genetic DEE age (years) | N = 7 |
| Mean (SD) | 4 |
| Range | 2–10 |
| Child genetic test result | N = 7 |
| Positive | n = 5 |
| Average time to diagnosis | 14 months |
| Genes | CACNB4 |
| KCNQ2 | |
| WWOX | |
| SCN2A | |
| SCN1A | |
| STXBP1 | |
| Undiagnosed | n = 1 |
2.3. Priority-setting workshop
The parent priority-setting workshop was conducted via a secure online platform (Zoom™) and lasted approximately one hour in duration. The workshop commenced with an introductory stage, followed by a questioning stage, and concluded with a debriefing stage [21]. The objective of the workshop was to understand parents' perspectives, needs and preferences for psychological resources. The workshop was conducted by a single moderator with experience conducting interviews and focus groups with parents of children with DEE (SN). An expert epilepsy research coordinator and epilepsy clinical nurse consultant co-facilitated the workshop and took field notes (FLM, EB). Following informed consent, the workshop discussion was digitally recorded and transcribed verbatim by an independent paid transcription company.
2.4. Analysis
In this study, we adopted an innovative qualitative research methodology, incorporating both thematic and lexical analysis to analyse the parent priority-setting workshop data. Combining these two different qualitative research approaches facilitated understanding the data from different vantage points and illuminated potential pathways through which psychological resources can be designed to improve parent wellbeing [22,23]. Thematic analysis [24,25] is a well-established qualitative research technique frequently employed to analyse textual data, to develop understanding of complex phenomena and to elucidate themes [24,26]. Lexical analysis is a novel qualitative research methodology that can be used in combination with thematic analysis to improve relational understanding of health-seeking behaviours, indicating opportunities for innovative resource intervention [23]. Lexical analysis offers a “helicopter” view of textual data, grounding the analysis in the participants' voices and can draw researcher attention to relationships between concepts that may not have been identified through thematic analysis alone [27,28]. Concepts represent ‘collections of words that generally travel together throughout the text’. [20] Lexical analysis has been successfully incorporated to improve healthcare in other settings [28,29], however there have been no studies using this methodology for investigating the psychological support needs of parents of a child with a genetic DEE. We analysed the workshop transcript first using thematic analysis and then analysed the transcript using lexical analysis. The multidisciplinary panel used key themes derived from the priority-setting workshop to develop ‘guiding principles’ to inform the content, scope and features of a future suite of psychological resources.
2.5. Thematic analysis
The first author (SN) analysed the deidentified transcript using thematic analysis [25]. Adopting an inductive approach, SN continued to read the transcript, constructing themes and concepts that clarified parents' perspectives, needs and preferences for psychological resources. The members of the multidisciplinary panel then independently analysed the transcript. Following this, SN constructed a codebook (Supplementary Appendix B) coding the transcript, line-by-line [30]. To improve the rigour of the thematic analysis, the multidisciplinary panel convened on multiple occasions (n = 10) following the parent priority-setting workshop to iteratively discuss, critique, and refine the emerging concepts to ensure the themes were generated rigorously and systematically. The various disciplinary lens' of the multidisciplinary panel (genetics, psychiatry, psychology, neurology, and behavioural sciences) enhanced the fidelity of the results.
2.6. Lexical analysis
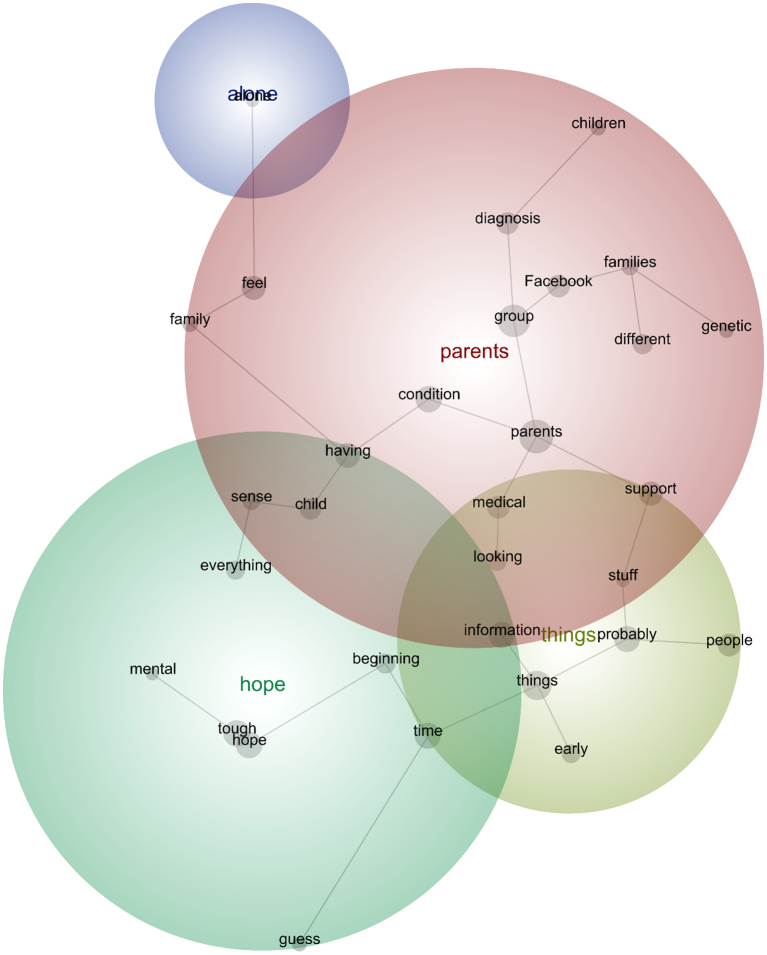
A lexical analysis involving conceptual and relational thematic analysis was conducted, aided by Leximancer [31]. Leximancer is a data-mining software that uses Bayesian reasoning to detect key concepts within a transcript and to reveal their relationships (Fig. 2). Using algorithms, Leximancer identifies frequently occurring and co-occurring words and amalgamates these to visually map concepts that reflect themes within the text [32]. The maps convey three types of information – ‘the main concepts in the text and their relative importance; the strength of links between concepts (how often they co-occur); and similarities in contexts where links occur’. [33] Leximancer was used in two steps. First, after removing the moderator prompts from the transcript and uploading the transcript to the program, we used the ‘discovery’ mode to ‘see what concepts were automatically generated by Leximancer without intervention’. [34] Concepts that were semantically and conceptually similar were merged. Second, Leximancer was used to examine the relative importance of the concepts, as denoted by relevancy weightings. A relevancy weighting denotes ‘the relative strength of a concept's frequency of occurrence’. [35]
Fig. 2.
Discovery Mode Concept Map. The components of these concepts are ordered within a thesaurus and weightings to indicate relative importance. Within the map, connections between concepts are represented by grey lines. Clusters of concepts within a map – known as themes – suggest contextual similarity [36]. For clarity, themes are colour-coded to signify those that are (and are not) important, whereby the ‘most important theme appears in red, and the next hottest in orange, and so on according to the colour wheel’. [20]
3. Results
The results of thematic and lexical analysis of the parent priority-setting workshop are provided here. A summary of six key prioritised themes generated from the data are presented below. Anonymised quotes from the priority-setting workshop group are presented in Table 2 to illustrate the narrative.
4. Thematic analysis
4.1. Access to specialist psychological resources to cope with uncertainty
The need for tailored psychological resources that are sensitive to the fragile emotional states of parents in the acute care setting was consistently emphasised. Due to the chronic uncertainty parents experienced regarding their child's ultra-rare genetic condition, many parents struggled to navigate the healthcare system and searched extensively for resources. Parents stressed the importance of connecting with diagnosis-specific psychological resources in the early periods of their child's initial diagnostic presentation. It was also considered essential that the resources did not give the impression that their caregiving experiences would automatically become easier after they ‘accepted’ their child's diagnosis. Tailored psychological resources to sustain parents' long-term coping throughout the course of their child's lifecycle were widely desired.
“At the beginning, we were scrambling because we knew she had all these different issues with movement and neurology and then gastro issues, and no one quite understood the gene enough to know that they're all actually just part of her issue. It wasn't until we got the right team that everything got a lot better for us. If we had that connection earlier on, I feel dealing with her condition would have been easier to begin with.”
4.2. No-one understands – I'm on my own
Due to the rarity of individual genetic DEE diagnoses, parents were unable to connect with local diagnosis-specific support groups with whom they could identify. Limited opportunity to interact with other parents, combined with challenges communicating their child's diagnosis, caused parents to feel alienated and distressed. Parents reported a need to establish peer-to-peer support groups for parents of children with genetic DEEs and to initiate pathways that promote early peer connectedness to overcome initial isolation and to support their mental health.
“It's very important to know that you're not alone and to feel like you're part of a community. Otherwise you just feel like you are all alone dealing with these things, because you're only one of a handful, like 100 – I think there's 100 children or so in the world who have the same diagnosis as my daughter, which is KCNQ2. It's quite rare, so you do feel alone.”
4.3. Too muchness – I need help
Parents described experiencing ongoing psychological distress associated with their “sustained high-pressure” caregiving role, as they responded to their child's complex and chronic developmental needs. In some cases, parents perceived stressors increased over time. Several parents highlighted the need for psychoeducation about the potential impacts of a genetic DEE diagnosis on the entire family, as well as guidance for seeking professional psychological help when required. This knowledge was crucial to support family relationships, as many parents discussed the additional psychological toll that relationship breakdowns contributed, and the intense difficulty when trying to manage their child's diagnosis alone. Streamlined access to specialised and tailored psychological resources were considered particularly pertinent in circumstances where symptomology might arise from pre-existing or underlying parent mental health symptoms.
“Knowing if you have a partner that has some mild mental health symptoms, that this very well could bring on a nervous breakdown or severe depression or severe anxiety, then you really need some serious psychological help or services for that person, because then you're on your own. You don't have that partner to fall back on or get help from.”
4.4. Putting the pieces together and going forward
A challenge highlighted among parents was accessing the “right style of therapy”, with experts who understood their experiences caring for a child with a genetic DEE. Parents described that their mental health needs often changed over the course of their child's DEE lifecycle. For example, transitioning out of in hospital care to caregiving in the home was reported as extremely challenging, without access to a coordinated care pathway. To cater for the scope of their needs, parents recommended developing psychological resources that provide social-emotional connection, as well as practical psychoeducational coping tools. Parents emphasised that tailored psychological resources hosted on hospital endorsed platforms were necessary to cut down on time spent outsourcing resources that might not be relevant to their needs.
“It's about what does the science say and what's some simple science that we can understand, and what does this mean for my life, and how I need to go about daily activities and all of that sort of stuff.”
4.5. Grieving together and finding strength
Parents relayed that having access to family centred psychological resources and, as well as appropriately funded therapies for their child was essential to sustain their mental health. Several parents relayed that they valued listening to other parents experiences throughout different stages of their child's development and learning that there are other parents experiencing similar challenges. Parents recommended that including a “parent voice” in the psychological resources would increase engagement and appeal. Additionally, parents recommended designing the psychological resources in formats that can be shared (eg. online links) to further support them in building sustained connections with other parents.
“As soon as you have another family that has a similar story to you, you don't feel so alone and then your wellbeing is better. Obviously, it can help in so many different ways. It's great having a psychological talk, but also having links that a family could then access free mental healthcare plans and stuff like that as well”.
4.6. Resilience and hope
Throughout the challenges encountered, parents emphasised the importance of normalising their caregiving journey and never losing hope. Several parents discussed their deliberate decision to “reframe” the diagnosis early in their child's diagnostic journey. Parents explained that choosing to focus on the positive aspects of what their child could achieve helped them to become more accepting of their situation. In achieving this, parents discussed the importance of finding joy through the rewarding experiences of caring for a child who was much more than their medical condition.
“I think it could have gone one of two ways for us. We could have become really despondent and sunk into a deep depression. I'm sure that could have happened for us, but I think quite early on in the journey we shifted our focus and also never lost hope. There's always hope and that keeps us going.”
4.7. Lexical analysis
The discovery mode concept map revealed four thematic nodes – namely: ‘parents’, ‘things’ (closely linked to ‘information’), ‘hope’, and ‘alone’ (see Figure). These highlight key clusters of concepts, represented within the priority-setting workshop discussion. Theme position, as shown in Fig. 2, illustrated the relationships between the concepts.
The largest grouping within the concept map centres on the word ‘parents’ linked to key concepts including ‘group’, ‘condition’, ‘having’, ‘feel’, ‘medical’, ‘Facebook’, ‘diagnosis’, ‘child’, ‘different’, ‘family’, ‘children’, and ‘genetic’. This grouping suggests these concepts were connected within the discourse. For instance, the participants spoke of: feeling different because of their situation, and attempting to find others they could personally relate to. However, given the rarity of their child's diagnosis, this was often difficult. Nevertheless, they exercised agency by harnessing the reach of social media, such as ‘Facebook’ to contact other individuals who also had a child with a rare condition:
“Just a few comments on getting support on Facebook groups. When [my daughter] was first diagnosed, with her condition being so ultra-rare, we really didn't have any resources at all and we actively sought out other parents around the world with the same condition, or children with the same condition.”
The ambiguously labelled theme, ‘things’, was connected closely with ‘information’ and encompassed concepts including ‘probably’, ‘time’, ‘support’, ‘people’, ‘early’ and ‘looking’. Collectively, these concepts spoke to the uncertain nature of genetic DEEs and the plethora of ‘things’ parents' needed to navigate their child's genetic diagnosis. It highlighted the overwhelming and uncertain nature of parents' continued search for tailored information and support relevant to their child's diagnosis:
“It's very, very early that you'll be on there, 2:00 am in the morning, reading information maybe before you have any idea about anything being genetic.”
The value of ‘things’ is suggested by its position within the concept map. In particular, it intersects ‘parents’ with ‘hope’, akin to a steppingstone between them. This suggests a relationship between ‘things’ (information, resources, supports) that parents can do or have that combine to provide a means of hope. The theme ‘hope’ encompassed the concepts: ‘tough’, ‘beginning’, ‘everything’, ‘sense’, ‘guess’, and ‘mental’. These concepts collectively highlight parents' resilience, despite the uncertainty and challenges they experienced.
“I mean of course it's very overwhelming in the beginning and there's a lot of challenge and there's a lot of uncertainty, and you find yourself being the hamster on the wheel trying to understand all the information and put all your services in place, but at the same time you've still got this hope that runs through everything that you do. You've still got this joy of having this child that's also more than their medical condition, if that makes sense.”
In contrast, the theme ‘alone’ is distant from the theme ‘hope’ which suggests that discourse pertaining to ‘alone’ did not travel with that pertaining to ‘hope’ (and vice versa). Similarly, the themes ‘things’ and ‘alone’ do not overlap. The lack of direct overlap with the ‘hope’ and ‘alone’ and ‘alone’ and ‘things’ suggests that these themes are mediated through parents. For example, this raises the notion that parents ‘aloneness’ may need to be addressed through the role in the family, rather than providing information or personal hopefulness alone.
“I'm from a country that doesn't have lots of things to give to people - and every time we receive support from NDIS, [partner's name] and myself always comment positive things about that. I mean the Australian Government is giving us lots of things. We have lots of therapy; we have equipment for [child's name]. I would like to include the positive things that give us hope.”
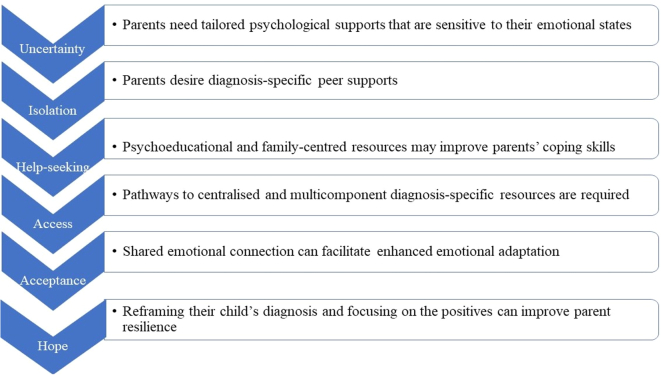
4.8. Thematic-derived ‘guiding principles’ to inform future psychological resources
The most important insights generated through the qualitative analysis of the parent priority-setting workshop are encapsulated through the development of six thematic-informed ‘guiding principles’. The guiding principles consist of two elements: (1) psychological resource design objectives, and (2) a summary of the key features of the psychological resources that can help achieve the objectives [15]. ‘Guiding principles’ are useful to produce following high-quality qualitative research, as they can be consulted throughout the resource planning and development phases to ensure that the psychological resources address relevant context-specific needs (Fig. 3) [14].
Fig. 3.
Guiding principles identified using person-based framework.
5. Discussion and conclusion
Global healthcare policies have prioritised the development of innovative resources to protect the psychological wellbeing of parents following a genetic DEE diagnosis [37]. Yet, psychological resources are an underutilised intervention for parents of children with rare neurogenetic conditions and there is a dearth of evidence regarding parents' preferences for psychological resources [38,39]. This is one of the key issues hampering the field from delivering high-quality resources to improve parent outcomes [40]. To our knowledge, this is the first study to use a person-based approach, to investigate parents' perspectives and preferences for psychological resources and to clarify how their mental health can be supported with novel psychological resources. The person-based approach provides an empirical framework that supports multidisciplinary collaboration [41] to inform the development of resources through iterative qualitative assessment of parents' psychological needs. The combination of both thematic and lexical analyses generated six thematic-derived ‘guiding principles’ that parents perceive are of highest priority to address to support improved psychological adaptation to their child's genetic DEE diagnosis.
Thematic analysis highlighted heightened parent distress and uncertainty following their child's diagnosis. Previous studies have suggested that the emotional impact of a genetic diagnosis is mediated by the extent to which parents have access to diagnosis-specific resources [8,42], and our study emphasised the need for tailored psychological resources for parents offered genetic testing for their child's DEE in the acute care setting. Chronic distress following their child's genetic diagnosis has a substantial impact on parent psychological functioning [43] and individuals with other rare conditions have voiced frustration, and hopelessness navigating fragmented healthcare systems [44]. The combination of thematic and lexical qualitative analyses afforded insight into the co-existing challenges parents face while also illustrating parents' resilience and hope. Emerging studies indicate that strategies including positive reappraisal and support seeking have been successful in lowering distress and enhancing adjustment to genetic diagnoses [45,46]. Our study extends the literature in this field, as both the thematic and lexical analysis suggested that access to diagnosis-specific information and tailored psychological provided a potential pathway to improve parent outcomes by reducing uncertainty and social isolation. Our findings support a clear need for the development of psychological resources that are appropriately tailored to the unique and high-stress experiences of parents, while also ensuring diagnosis-specific information is provided in a time-sensitive manner.
6. Innovation
As genetic testing continues to be integrated into clinical practice, improving parent psychological adaptation to their child's genetic DEE diagnosis is a critical long-term strategy to optimise outcomes for children and families [47]. There are few published examples of engaging multidisciplinary clinician researchers and parents of a child with a rare genetic condition in shaping healthcare services to support parents' psychological wellbeing [48]. This study offers a novel person-based approach, incorporating a priority-setting workshop to understand parents' perspectives and preferences for psychological resources. By establishing a partnership between multidisciplinary clinician researchers and parents in the early stages of the design of the resources, we have leveraged the expertise of both groups to develop ‘guiding principles’. The ‘guiding principles’ developed through this research will be translated to maximise the likelihood that future psychological resources will be engaging and acceptable for parents of children with rare genetic conditions.
7. Conclusion
Understanding parent perspectives and preferences for tailored psychological resources is crucial in the context of rare and complex genetic DEEs. Using a novel, person-based approach, our study indicates that there is substantial potential for developing tailored psychological resources which aim to lower parent distress and to promote enhanced psychological adaptation following a genetic DEE diagnosis in their child. Notably, our analysis revealed that fast-tracked pathways to connect parents with diagnosis-specific peer-supports and tailored psychological resources might fortify parents' personal capacity to support both themselves and their families. The combination of both thematic and lexical analyses generated six thematic-derived ‘guiding principles’, which will inform a future suite of psychological resources. The extent to which tailored psychological resources, underpinned by these ‘guiding principles’ are helpful towards reducing isolation and maximising hope among parents of a child with genetic DEE should be explored via future research studies.
Sources of support
The authors acknowledge the support of the Maridulu Budyari Gumal, The Sydney Partnership for Health, Education, Research & Enterprise (SPHERE) Kids to Adults (K2A) Clinical Academic Group. This work was also supported by Luminesce Alliance – Innovation for Children's Health Luminesce Alliance - Innovation for Children's Health, is a not-for-profit cooperative joint venture between the Sydney Children's Hospitals Network, the Children's Medical Research Institute, and the Children's Cancer Institute. The authors would like to thank Manildra Corporation and NSW Kids and Families for generous funding support. Claire Wakefield is supported by a Career Development Fellowship from the National Health and Medical Research Council of Australia (APP1143767).
Declaration of Competing Interest
None.
Appendix
Table 2.
Anonymised parent quotations from the priority-setting workshop are presented to illustrate the narrative.
| Access to specialist psychological resources to support coping with uncertainty |
| “At the very beginning for us, we were scrambling because we knew she had all these different issues with movement and neurology and then gastro issues, and no one quite understood the gene enough to know that they're all actually just part of her issue. It wasn't until we got the right team that everything got a lot better for us. If we had that connection earlier on, I feel dealing with her condition would have been easier to begin with.” |
| “I guess what I would like to say as well is that it doesn't seem to get easier for me. It changes and things - but the ongoing - I really feel an ongoing sense of trauma and chronic stress with [child's name] because you're constantly being put in these emergency situations with her seizures, it's kind of almost compounding.” |
| No-one understands – I'm on my own: Extreme isolation |
| “it's very important to know that you're not alone and to feel like you're part of a community. Otherwise you just feel like you are all alone dealing with these things, because you're only one of a handful, like 100 – I think there's 100 children or so in the world who have the same diagnosis as my daughter, which is KCNQ2. It's quite rare so you do feel alone.” |
| “When [child's name] was first diagnosed, with her condition being so ultra-rare, we really didn't have any resources at all and we actively sought out other parents around the world with the same condition, or children with the same condition.” |
| Too muchness – I need help |
| “Knowing if you have a partner that has some mild mental health symptoms, that this very well could bring on a nervous breakdown or severe depression or severe anxiety, then you really need some serious psychological help or services for that person, because then you're on your own. You don't have that partner to fall back on or get help from.” |
| “I don't find there's really specific counselling or psychological services to deal with the overall umbrella of parents that have possibly some mild pre-existing mental health, but then it just really crashes once they have a child with any type of disability. It's really hard finding the right services for your partner. We've tried lots of different medications and whatnot, but it hasn't really worked.” |
| Putting the pieces together and going forward |
| “If you receive your child's diagnosis it would be great if your clinician or genetic counsellor - can point you in the direction of a database right at the beginning. You can get on there and just cut down on that initial search where you can spend hours and hours reading through scientific papers trying to make sense of what's going on” |
| “It's about what does the science say and what's some simple science that we can understand, and what does this mean for my life, and how I need to go about daily activities and all of that sort of stuff.” |
| Grieving together and finding strength |
| “I must admit once we transitioned out of early intervention and into the school system, I really felt like I lost pretty much all peer support.. in terms of the models of care and circles of support and all that type of stuff that is more readily available through local-based early intervention services like supported playgroups, where you've got that opportunity to connect.” |
| “as soon as you have another family that has a similar story to you, you don't feel so alone and then your wellbeing is better. Obviously it can help in so many different ways. I think that would be - it's great having a psychological talk, but also having links that a family could then access free mental healthcare plans and stuff like that as well”. |
| Resilience and hope |
| “I think it could have gone one of two ways for us. We could have become really despondent and sunk into a deep depression. I'm sure that could have happened for us, but I think quite early on in the journey we shifted our focus and also never lost hope. There's always hope and that keeps us going.” |
| “I mean of course it's very overwhelming in the beginning and there's a lot of challenge and there's a lot of uncertainty, and you find yourself being the hamster on the wheel trying to understand all the information and put all your services in place, but at the same time you've still got this hope that runs through everything that you do. You've still got this joy of having this child that's also more than their medical condition, if that makes sense (emphasis added).” |
Table 3.
Leximancer ranked concept list for lexical analysis.
| Concept | Count | Relevance |
|---|---|---|
| Name-Like | ||
| 7 | 47% | |
| Word-Like | ||
| Parents | 15 | 100% |
| Things | 13 | 87% |
| Feel | 12 | 80% |
| Time | 11 | 73% |
| Group | 10 | 67% |
| Hope | 10 | 67% |
| Tough | 10 | 67% |
| Probably | 10 | 67% |
| People | 10 | 67% |
| Condition | 9 | 60% |
| Information | 9 | 60% |
| Having | 9 | 60% |
| Diagnosis | 9 | 60% |
| Different | 9 | 60% |
| Guess | 9 | 60% |
| Early | 8 | 53% |
| Support | 7 | 47% |
| Family | 7 | 47% |
| Beginning | 6 | 40% |
| Everything | 6 | 40% |
| Sense | 6 | 40% |
| Families | 6 | 40% |
| Genetic | 6 | 40% |
| Alone | 6 | 40% |
| Medical | 5 | 33% |
| Child | 5 | 33% |
| Looking | 5 | 33% |
| Children | 5 | 33% |
| Stuff | 5 | 33% |
| Mental | 5 | 33% |
For a more granular examination of the concept map, the concepts were considered, as were their relevancy weightings. The thirty concepts with the strongest relevance ranged in textual association from 33% to 100% (see Table). ‘Parents’ (relevance: 100%; count: 15), ‘things’ (relevance: 87%; count: 13), ‘feel’ (relevance: 80%; count: 12), and ‘time’ (relevance: 73%; count: 11) were deemed to be most relevant within the discourse. This suggests that when the participants spoke of ‘parents’, they were likely to speak of ‘things’, ‘feel’, and ‘time’, and unlikely to speak of ‘medical’, ‘stuff’, or ‘mental’, among others.
Table 4.
Ranked concept list for the selected concept – ‘Support’.
| Concept | Count | Relevance |
|---|---|---|
| Name-Like | ||
| 2 | 29% | |
| Word-Like | ||
| Stuff | 2 | 40% |
| Group | 3 | 30% |
| Probably | 3 | 30% |
| People | 3 | 30% |
| Condition | 2 | 22% |
| Different | 2 | 22% |
| Parents | 3 | 20% |
| Medical | 1 | 20% |
| Looking | 1 | 20% |
| Children | 1 | 20% |
| Beginning | 1 | 17% |
| Things | 2 | 15% |
| Family | 1 | 14% |
| Early | 1 | 12% |
| Information | 1 | 11% |
| Time | 1 | 9% |
References
- 1.Keezer M.R., Sisodiya S.M., Sander J.W. Comorbidities of epilepsy: current concepts and future perspectives. The Lancet Neurol. 2016;15:106–115. doi: 10.1016/S1474-4422(15)00225-2. [DOI] [PubMed] [Google Scholar]
- 2.Cockerell O.C., Johnson A.L., Sander J.W., Shorvon S.D. Prognosis of epilepsy: a review and further analysis of the first nine years of the British National General Practice Study of Epilepsy, a prospective population-based study. Epilepsia. 1997;38:31–46. doi: 10.1111/j.1528-1157.1997.tb01075.x. [DOI] [PubMed] [Google Scholar]
- 3.Talwar D., Hammer M.F. SCN8A epilepsy, developmental encephalopathy, and related disorders. Pediatr Neurol. 2021;122:76–83. doi: 10.1016/j.pediatrneurol.2021.06.011. [DOI] [PubMed] [Google Scholar]
- 4.Jeffrey J.S., Leathem J., King C., Mefford H.C., Ross K., Sadleir L.G. Developmental and epileptic encephalopathy: personal utility of a genetic diagnosis for families. Epilepsia Open. 2021;6(1):149. doi: 10.1002/epi4.12458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McKeon G., Palmer E.E., Macintosh R., Nevin S.M., Wheatley L., Rosenbaum S. Feasibility of a mental health informed physical activity intervention for the carers of children with developmental and epileptic encephalopathy. Epilepsy Behav. 2021;121 doi: 10.1016/j.yebeh.2021.108022. [DOI] [PubMed] [Google Scholar]
- 6.Nevin S.M., Wakefield C.E., Barlow-Stewart K., McGill B.C., Bye A., Palmer E.E., et al. Psychosocial impact of genetic testing on parents of children with developmental and epileptic encephalopathy. Dev Med Child Neurol. 2021;64:95–104. [Google Scholar]
- 7.Nevin S.M., Wakefield C.E., Schilstra C.E., McGill B.C., Bye A., Palmer E.E., et al. Epilepsy Behav. 2020;112 doi: 10.1016/j.yebeh.2020.107382. [DOI] [PubMed] [Google Scholar]
- 8.Jakobsen A.V., Møller R.S., Nikanorova M., Elklit A. The impact of severe pediatric epilepsy on experienced stress and psychopathology in parents. Epilepsy Behav. 2020;113 doi: 10.1016/j.yebeh.2020.107538. [DOI] [PubMed] [Google Scholar]
- 9.Gonçalves C., Martins S., Fernandes L. Dravet syndrome: Effects on informal caregivers’ mental health and quality of life–A systematic review. Epilepsy Behav. 2021;122:108206. doi: 10.1016/j.yebeh.2021.108206. [DOI] [PubMed] [Google Scholar]
- 10.Eccleston C., Fisher E., Law E., Bartlett J., Palermo T.M. Psychological interventions for parents of children and adolescents with chronic illness. Cochrane Database Syst Rev. 2015;4:1–21. doi: 10.1002/14651858.CD009660.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Janssens R., Huys I., van Overbeeke E., Whichello C., Harding S., Kübler J., et al. Opportunities and challenges for the inclusion of patient preferences in the medical product life cycle: a systematic review. BMC Med Informat Dec Making. 2019;19:1–16. doi: 10.1186/s12911-019-0875-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.England M.J., Liverman C.T., Schultz A.M., Strawbridge L.M. Summary: a reprint from epilepsy across the spectrum: promoting health and understanding. Epilep Curr. 2012;12:245. doi: 10.5698/1535-7511-12.6.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adama E.A., Adua E., Bayes S., Mörelius E. Support needs of parents in neonatal intensive care unit: An integrative review. J Clin Nurs. 2021:1–16. doi: 10.1111/jocn.15972. [DOI] [PubMed] [Google Scholar]
- 14.Yardley L., Ainsworth B., Arden-Close E., Muller I. The person-based approach to enhancing the acceptability and feasibility of interventions. Pilot Feasib Stud. 2015;1:1–7. doi: 10.1186/s40814-015-0033-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yardley L., Morrison L., Bradbury K., Muller I. The person-based approach to intervention development: application to digital health-related behavior change interventions. J Med Internet Res. 2015;17 doi: 10.2196/jmir.4055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McCann L., Moore M. The importance of co-design in the development of an e-Supportive Care System to support families with children and young people with complex health care needs. BCS Health Informat Scotland. 2016:1–4. [Google Scholar]
- 17.Eyles H., Jull A., Dobson R., Firestone R., Whittaker R., Te Morenga L., et al. Co-design of mHealth delivered interventions: a systematic review to assess key methods and processes. Curr Nutr Rep. 2016;5:160–167. [Google Scholar]
- 18.Elliott E.J., Zurynski Y.A. Rare diseases are a’common’problem for clinicians. Aust Fam Physician. 2015;44:630–633. [PubMed] [Google Scholar]
- 19.Rubin H.J., Rubin I.S. Sage; 2011. Qualitative interviewing: The art of hearing data. [Google Scholar]
- 20.Leximancer . Leximancer Pty Ltd; Brisbane, QLD: 2011. Leximancer manual. [Google Scholar]
- 21.Liamputtong P. Focus group methodology: Introduction and history Focus group methodology. Princ Pract. 2011;224 [Google Scholar]
- 22.Pluye P., Hong Q.N. Combining the power of stories and the power of numbers: mixed methods research and mixed studies reviews. Annu Rev Public Health. 2014;35:29–45. doi: 10.1146/annurev-publhealth-032013-182440. [DOI] [PubMed] [Google Scholar]
- 23.Dadich A., Fulop L., Ditton M., Campbell S., Curry J., Eljiz K., et al. Finding brilliance using positive organizational scholarship in healthcare. J Health Organ Manag. 2015;29(6):750–777. doi: 10.1108/JHOM-11-2013-0256. [DOI] [PubMed] [Google Scholar]
- 24.Vaismoradi M., Jones J., Turunen H., Snelgrove S. 2016. Theme Development in Qualitative Content Analysis and Thematic Analysis. [Google Scholar]
- 25.Braun V., Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. [Google Scholar]
- 26.Brod M., Tesler L.E., Christensen T.L. Qualitative research and content validity: developing best practices based on science and experience. Qual Life Res. 2009;18:1263–1278. doi: 10.1007/s11136-009-9540-9. [DOI] [PubMed] [Google Scholar]
- 27.Leximancer User Guide. 2021 Accessed August 27 2021.
- 28.Dadich A., Jarrett C. Understanding practitioner perspectives of youth healthcare using thematic and lexical analyses. Health Expect. 2019;22:1144–1155. doi: 10.1111/hex.12950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Karimi L., Dadich A., Fulop L., Leggat S.G., Rada J., Hayes K.J., et al. Empirical exploration of brilliance in health care: Perceptions of health professionals. Aust Health Rev. 2016;41:336–343. doi: 10.1071/AH16047. [DOI] [PubMed] [Google Scholar]
- 30.Braun V., Clarke V. Reflecting on reflexive thematic analysis Qualitative Research in Sport. Exer Health. 2019;11:589–597. [Google Scholar]
- 31.Gephart R.P. From the editors: qualitative research and the academy of management. J Acad Manag. 2004;47:454–462. [Google Scholar]
- 32.Young L., Denize S. Competing interests: The challenge to collaboration in the public sector. Int J Sociol Soc Policy. 2008;28:46–58. [Google Scholar]
- 33.Hewett D.G., Watson B.M., Gallois C., Ward M., Leggett B.A. Intergroup communication between hospital doctors. Soc Sci Med. 2009;69:1732–1740. doi: 10.1016/j.socscimed.2009.09.048. [DOI] [PubMed] [Google Scholar]
- 34.Angus-Leppan T., Benn S., Young L. A sensemaking approach to trade-offs and synergies between human and ecological elements of corporate sustainability. Bus Strateg Environ. 2010 May;19:230–244. [Google Scholar]
- 35.Leximancer Understanding Displays and Outputs. https://hypermancer.leximancer.com/faq/display_and_output.html# Available at. Accessed 21st Mar.
- 36.Hepworth N., Paxton S.J. Pathways to help-seeking in bulimia nervosa and binge eating problems: A concept mapping approach. Int J Eat Disord. 2007;40:493–504. doi: 10.1002/eat.20402. [DOI] [PubMed] [Google Scholar]
- 37.Smith G., Wagner J., Andrews J., Austin J., Mueller M., Carter E., et al. Caregiving in pediatric epilepsy: results of focus groups and implications for research and practice. Epilepsy Behav. 2014;34:34–41. doi: 10.1016/j.yebeh.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 38.Baumbusch J., Mayer S., Sloan-Yip I. Alone in a crowd? Parents of children with rare diseases’ experiences of navigating the healthcare system. J Genet Couns. 2018:1–11. doi: 10.1007/s10897-018-0294-9. [DOI] [PubMed] [Google Scholar]
- 39.Pelentsov L.J., Laws T.A., Esterman A. The supportive care needs of parents caring for a child with a rare disease: a scoping review. Disab Health J. 2015;8:475–491. doi: 10.1016/j.dhjo.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 40.Guilfoyle S.M., Wagner J.L., Modi A.C., Junger K.F., Barrett L.E., Riisen A.C., et al. Pediatric epilepsy and behavioral health: The state of the literature and directions for evidence-based interprofessional care, training, and research. Clin Pract Pediatr Psychol. 2017;5:79. [Google Scholar]
- 41.Morrison L., Muller I., Yardley L., Bradbury K. The person-based approach to planning, optimising, evaluating and implementing behavioural health interventions. The Eur Health Psychol. 2018;20:464–469. [Google Scholar]
- 42.McAllister M., Davies L., Payne K., Nicholls S., Donnai D., MacLeod R. The emotional effects of genetic diseases: implications for clinical genetics. Am J Med Genet A. 2007;143:2651–2661. doi: 10.1002/ajmg.a.32013. [DOI] [PubMed] [Google Scholar]
- 43.Webster M. Illness. The cycle of uncertainty: parents’ experiences of childhood epilepsy. Sociol Health & Illness. 2019;41:205–218. doi: 10.1111/1467-9566.12815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Currie G., Szabo J. It is like a jungle gym, and everything is under construction: The parent’s perspective of caring for a child with a rare disease. Child Care Health Dev. 2019;45:96–103. doi: 10.1111/cch.12628. [DOI] [PubMed] [Google Scholar]
- 45.Courtney E., Kiernan G., Guerin S., Ryan K., McQuillan R. Mothers’ perspectives of the experience and impact of caring for their child with a life-limiting neurodevelopmental disability. Child Care Health Dev. 2018;44:704–710. doi: 10.1111/cch.12580. [DOI] [PubMed] [Google Scholar]
- 46.Haw T., Henriques S. Exploring how mothers of a child with a genetic disorder experience their couple relationship in a low socio-economic setting. J Genet Couns. 2021;30(3):885–899. doi: 10.1002/jgc4.1391. [DOI] [PubMed] [Google Scholar]
- 47.Vlaskamp D.R., Rump P., Callenbach P.M., Brilstra E.H., Velthuizen M.E., Brouwer O.F., et al. Changes in empowerment and anxiety of patients and parents during genetic counselling for epilepsy. Eur J Paediatr Neurol. 2021;32:128–135. doi: 10.1016/j.ejpn.2021.03.015. [DOI] [PubMed] [Google Scholar]
- 48.Oulton K., Gibson F., Williams A., Geoghegan S., Aldiss S., Wray J. Supporting families of children with an undiagnosed genetic condition: Using co-design to ensure the right person is in the right post doing the right job. Child Care Health Dev. 2021;47:300–310. doi: 10.1111/cch.12838. [DOI] [PubMed] [Google Scholar]