Abstract
Objectives
Families in the Neonatal Intensive Care Unit (NICU) experience significant psychological distress. Fellowship training requires education on mental health issues. No standardized program exists. We evaluated the impact of an online course, combining research with family perspectives, on neonatology fellow knowledge and self-efficacy when emotionally supporting NICU families.
Methods
Fellows from 20 programs completed a course covering: (1) Parent Mental Health, (2) Infant Mental Health, (3) Communication, and (4) Comprehensive Mental Health (e.g., discharge, bereavement) with pre- and post-course knowledge and self-efficacy assessments.
Results
Fellows (n=91) completed the course and assessments. Pre-course knowledge was similar by year of training (1st: 66.9%; 2nd: 67.2%; 3rd: 67.4%). Mean knowledge and self-efficacy improved between pre- and post-course assessments regardless of training year or prior education for knowledge (d=1.2) (67.1% vs. 79.4%) and for self-efficacy (d=1.2) (4.7 vs 5.2 on 6-point Likert scale). Fellows who gained more knowledge had higher self-efficacy scores at post-test (r = .37).
Conclusions
Current neonatal fellowship training under-educates on mental health. An online course improved fellow knowledge and self-efficacy. Our course may be an exemplar for others creating similar curricula.
Innovation
An online course enriched by patient perspectives is an effective method of disseminating education around mental health.
Keywords: Medical education, Mental health, Communication, Neonatology, Digital platform
Highlights
-
•
Neonatal Intensive Care Unit families experience high levels of emotional distress
-
•
No national mental health training program exists for neonatology fellows
-
•
An online mental health course improved fellow knowledge and self-efficacy
-
•
This course can be an example for others creating mental health training in medicine
1. Introduction
Approximately 10-15% of US born infants require care in the Neonatal Intensive Care Unit (NICU), making up a sizable fraction of future pediatric clinic and inpatient populations [1]. Both NICU infants and their parents experience high rates of distress, with up to 20-60% of mothers developing postpartum depression, anxiety, or posttraumatic stress disorder [[2], [3], [4], [5], [6], [7], [8]]. Fathers are not immune to mental health issues either [9]. These conditions may adversely impact parent-infant attachment and parenting behaviors, leading to higher risks of worse physical and developmental outcomes in their infants [[10], [11], [12]]. Research suggests that providing psychosocial support to NICU parents can reduce their distress, depression, and anxiety, potentially leading to healthier infant outcomes [[13], [14], [15], [16]]. Infants also experience elevated levels of distress from stressful environments, multiple painful procedures, and separation from parents producing changes in the hypothalamic-pituitary axis, which may be lifelong [[17], [18]]. Adults and adolescents born preterm, for example, experience higher rates of depression and anxiety than the general population [[19], [20]].
While the prevalence of emotional distress and mental health disorders in the U.S. provides a strong rationale for all trainees to receive education around mental health needs of patients, pediatricians in particular are tasked with treating children in the context of the family, necessitating skills at identifying and managing mental health issues in children and their parents. A national survey of pediatricians by the American Academy of Pediatrics (AAP) in 2013 indicated that a majority (65%) felt unprepared to handle mental health issues [21]. In 2014 the American Board of Pediatrics (ABP) Strategic Planning Committee identified the areas of behavioral and mental health as the highest priority for education of pediatric trainees [22]. The Roadmap Project was developed by the ABP in 2018 as a guide for advocacy and education on mental health issues in pediatrics with the stated goal of supporting “the resilience, emotional, and mental health of pediatric patients with chronic conditions and their families.”[23] The AAP updated its policy statement on mental health competencies for pediatric practice in 2019 [24], stressing the need for communication skills, the integration of mental health care into routine clinical care, improvement in core knowledge, and the ability to co-manage with mental health clinicians. An accompanying recommendation outlined guidance for training programs [25]. Finally, in 2019, the Accreditation Council for Graduate Medical Education (ACGME) instituted requirements that all training programs include training in mental health, but each specialty and subspecialty were left to develop their own programming.
Although some neonatology fellowship programs teach communication skills for high stress situations [[26], [27], [28], [29], [30]], no comprehensive program exists in psychosocial care of NICU families. We present the impact of the first such national course to teach recognition and mitigation of mental health issues in neonatology, in alignment with the ABP Roadmap’s Key Drivers.
2. Methods
2.1. Course development
A four-module online course was adapted from a seven-hour course on psychosocial support for NICU families, “Caring for Babies,” designed primarily for nurses, with extensive input from former NICU families. A study of that course among NICU nurses showed it was effective in improving their knowledge and self-efficacy in providing psychosocial support to NICU parents [31]. A team of 2 neonatologists, a maternal-infant psychiatrist, and a NICU psychologist edited and distilled course content to four 30-minute modules: Trauma-informed Communication (“Communication”), Infant Mental Health (“Infant Mental Health”), Parent Mental Health (“Parent Mental Health”), and Comprehensive Mental Health (“Comprehensive Mental Health”), which covered staff support, peer support, palliative care and discharge planning. Content, in alignment with ABP and ACGME guidelines and requirements, included written narrative, audio clips and other quotes representing the experiences of NICU graduate parents, trauma-informed and culturally responsive care scripts, links to relevant internet resources as well as downloads of pertinent articles, and best practice recommendations. (Outline of course content in the appendix and online at www.myperinatalnetword.org.) IRB approval was obtained at study source institution.
2.2. Pre-implementation survey
In May 2019, all ACGME accredited neonatology fellowship program directors (PDs) in the United States were surveyed via email regarding existing training in NICU family mental health and communication, knowledge and plan for new ACGME requirements, and interest in a national curriculum on this topic. Questions were derived by lead study authors to gauge the need for and interest in development of a national curriculum in this area. Data was stored in REDCap. In October 2019, the same PDs were individually contacted regarding the opportunity for enrollment in a multi-center evaluation of the impact of the course on fellow knowledge and self-efficacy in recognizing and mitigating emotional distress in NICU families. Participating programs obtained IRB approval or waiver from their institutions. Rolling recruitment occurred between January 2020 and January 2021 due to variability in IRB process; once enrolled, fellows were emailed a link to the online program which began with study consent. Information on participating program demographics and educational content was obtained by survey via email with link to REDCap.
2.3. Course implementation and measures
The courses, with integrated pre- and post-course fellow assessments and knowledge exams, were offered on the online Prosperity Learning Management System created by Ziiva (www.ziiva.com). All fellow demographic and course data were stored in Rackspace (www.rackspace.com) in a Tier 1 data center which is ISO 27001 compliant. Content and user data were accessible only by administrators with logins and assigned permissions.
After enrolling in the study, fellows were originally given three months to complete it. However, because the COVID-19 pandemic intervened, time was extended until January 2021 for all participants. After consenting, fellows completed a demographics questionnaire and questions on previous mental health and communication training. A knowledge assessment (32 questions; 8 from each content domain) was also administered. Knowledge questions were created by course creators to reflect course content in agreement with the stated educational goals set forth in the ABP Roadmap Project, current neonatology board content and with the input of NICU psychologists, neonatologists and former NICU parents. Knowledge scores were tabulated as mean percent correct overall and within each content domain. Finally, fellows rated themselves on a series of questions (1 = strongly disagree to 6 = strongly agree) assessing their self-efficacy (32 questions, 8 from each domain) in various aspects important to supporting family mental health. For example, confidence in addressing implicit bias was assessed by fellow responses to “I am aware that we all have implicit biases that can impact service delivery” and “It is important to me to keep working to become aware of my own biases to keep them from affecting the care I give to families.” Overall scores and scores per domain were computed as mean ratings across all items. This efficacy survey was adapted from previously validated survey instruments from the “Caring for Babies” study which assessed nurses’ self-efficacy in supporting NICU parent mental health.[31] All surveys were pretested by two neonatology fellows from Stanford University for readability, clarity, and length. Surveys were revised based on this feedback. (See Appendix for exams and surveys).
Upon completion of the course, fellows repeated the knowledge and self-efficacy assessments with scores computed as previously described. To further estimate the change in scores from pre- to post-program, difference scores were computed. Feedback on fellows’ experience of the course was also obtained using a 6-point Likert scale to respond to statements (1=strongly disagree to 6=strongly agree).
Three months after course completion, fellows were contacted to complete assessments of knowledge and self-efficacy. Enrollment in the initial course close to the date of study closure precluded assessment of retention for some fellows.
All statistical analyses were conducted in SPSS Ver. 26.1. Prior to analyses, distributions were inspected for normality, skewness, and kurtosis. Descriptive statistics are provided as the mean (M) and standard deviation (SD), as well as the median values. Pre-program scores on the knowledge and self-efficacy assessments were evaluated by fellowship year using mixed ANOVAs with content domain (4 levels) as the within-subjects factor and fellowship year (3 levels) as the between-subjects factor. Within-subjects contrasts were used to explore differences between scores in the various content domains. To evaluate the effectiveness of the online training, the degree of change in knowledge and efficacy scores from pre- to post-program assessments was evaluated using ANOVAs as a function of fellowship year as the between-subjects factor and assessment point (time) and domain (4 levels) as the within-subjects factors. Changes from pre- to post-test were also analyzed in terms of difference scores (post-test – pre-test) within each domain using ANCOVA, controlling for overall knowledge or efficacy scores at pretest. Differences in knowledge and efficacy scores at 3 months after course completion were also compared to pretest scores (retention – pre-test). F statistics are reported for all ANOVAs with significance levels set at p < .05.
3. Results
3.1. Pre-implementation survey
Survey of neonatology fellowship PDs (n=96) in May 2019 produced 27 responses (28% response rate). While 45% reported they provided no teaching on parent mental health and 35% had no teaching on infant mental health, 75% had a communication course of some kind. Although 80% of PDs were aware of the new ACGME requirements, 50% had no plan for addressing them. Twenty neonatology fellowship programs elected to participate in the study. Table 1 shows program demographics. While approximately half of the programs reported existing communication training and had psychology support in the NICU, very few had current training for fellows in the identification and management of NICU family mental health concerns.
Table 1.
Background information on Fellowship Programs (n=20 programs)
| Program Features | Number of Fellowship Programs |
|---|---|
| How many fellows in the program? | |
| 4-9 | 16 |
| 10-15 | 3 |
| 16-21 | 1 |
| Simulation program for teaching communication? | |
| Yes | 10 |
| No | 10 |
| If yes, hours spent on above | Mean: 5.9 hrs Range: 1-15 hrs |
| Training on parental mental health? | |
| Yes | 2 |
| No | 18 |
| If yes, hours spent on above | Mean: 1 hr Range: 1 hr |
| Training on infant mental health? | |
| Yes | 2 |
| No | 18 |
| If yes, hours spent on above | Mean: 2.5 hrs Range: 1-4 hrs, optional |
| NICU Psychologist? | |
| Yes | 8 |
| No | 12 |
| Psych interacts with patients? | |
| Yes | 9 |
| No | 11 |
| Psych devel support for infants? | |
| Yes | 2 |
| No | 18 |
3.2. Fellow demographics and previous training in communication and mental health
Of the 187 fellows who were registered for the study by their PDs, 119 (16.0% male; 81.5% female; 2.5% prefer not to disclose) consented to participate. Of these, 108 fellows completed both the pre-course assessments and some of the online courses; 91 completed all of the courses and their post-course assessments, and 45 completed the 3-month follow-up survey to assess retention of results. Approximately half were 1st year, with the remaining equally distributed among 2nd and 3rd years. About 50% of fellows reported 6-20 hours of prior training in communication and mental health during medical school and residency. Training during fellowship was most often (> 80%) reported as less than 5 hours, especially in the domain of mental health.
Completion rates for the course tended to be lower among fellows from programs that had NICU-dedicated psychologists (49% of registered fellows and 58% of those consenting) compared with fellows from programs without psychologists (65% of those registered and 82% of those consenting), although these differences failed to reach statistical significance.
3.3. Results of pre-course surveys
Table 2 presents descriptives for fellow knowledge prior to the online program overall and for each of the domains by fellowship year. Analyses indicated that mean pre-test scores differed by content domain (F(1, 105) = 27.1, p < .001). Within-subjects contrasts indicated that fellows scored highest in “Communication” relative to “Parent Mental Health” (F(1, 105) = 7.1, p < .009), and lower in the “Comprehensive Mental Health” domain than both “Infant” and “Parent Mental Health” (F(1, 105) = 14.6, p < .0001). Importantly, overall pre-program knowledge scores did not differ as a function of fellowship year (F(2, 105) = 0.02, p = .98). In addition, the pattern of knowledge scores across domains was not different for fellows at different levels (F(2, 105) = 1.0, p = .36). Thus, fellows from all years of training had similar pre-course knowledge and similar patterns of knowledge gaps. Further, overall scores on the pre-course knowledge surveys were similar in those with or without previous communication (F(2, 105) = 0.24, p = .79) or mental health (F(2, 104) = 1.13, p = .33) training.
Table 2.
Descriptives statistics for knowledge and self-efficacy scores at pre-test by domain and fellowship year (n = 108)
| Fellowship Year |
||||||
|---|---|---|---|---|---|---|
| 1st Year | 2nd Year | 3rd Year | ||||
| M (SD) | Median | M (SD) | Median | M (SD) | Median | |
| Knowledgea | 67.0 (10.6) | 69.0 | 67.2 (8.0) | 69.0 | 67.4 (9.0) | 66.0 |
| Communication | 74.5 (18.8) | 75.0 | 69.6 (16.1) | 75.0 | 73.0 (16.8) | 75.0 |
| Parent Mental Health | 66.9 (14.7) | 62.5 | 67.9 (14.3) | 75.0 | 65.0 (13.0) | 62.5 |
| Infant Mental Health | 65.9 (15.5) | 68.8 | 70.7 (14.5) | 75.0 | 69.5 (16.6) | 75.0 |
| Comprehensive Mental Health | 60.7 (15.3) | 62.5 | 60.7 (11.4) | 62.5 | 62.0 (14.2) | 62.5 |
| Self-Efficacyb | 4.6 (0.4) | 4.6 | 4.8 (0.4) | 4.7 | 4.8 (0.5) | 4.8 |
| Communication | 4.8 (0.4) | 4.9 | 4.9 (0.4) | 5.0 | 5.0 (0.4) | 5.0 |
| Parent Mental Health | 4.4 (0.5) | 4.5 | 4.6 (0.5) | 4.5 | 4.6 (0.7) | 4.6 |
| Infant Mental Health | 4.6 (0.4) | 4.5 | 4.7 (0.4) | 4.9 | 4.8 (0.6) | 4.8 |
| Comprehensive Mental Health | 4.5 (0.4) | 4.5 | 4.8 (0.5) | 4.9 | 4.8 (0.5) | 4.8 |
Mean (SD) and median percent correct on knowledge assessment, overall and for four domains.
Mean (SD) and median ratings of self-efficacy, overall and for four domains, on a 6-point scale from strongly disagree to strongly agree.
Table 2 also shows that pre-program ratings of self-efficacy were generally high, but differed depending on fellowship year (F(2, 105) =3.71, p < .03). Self-efficacy scores for 1st year fellows were significantly lower than those of 3rd year fellows (p < .05), while 2nd and 3rd year fellows had similar self-efficacy scores (p > .11). Moreover, self-efficacy scores were highest in “Communication” and lowest in “Parent Mental Health” (p < .001), regardless of fellowship year (F(6, 315) = 1.07, p = .35). Finally, those fellows who had received the most prior training had higher ratings of self-efficacy (Communication: M = 5.1 (0.3); Mental Health: M = 4.9 (0.4)) than those with only some (Communication: M = 5.0 (0.4); Mental Health: M = 4.7 (0.5)) or little (Communication: M = 4.7 (0.4); Mental Health: M = 4.5 (0.4)) prior training (p < .001).
3.4. Effects of course on knowledge and self-efficacy
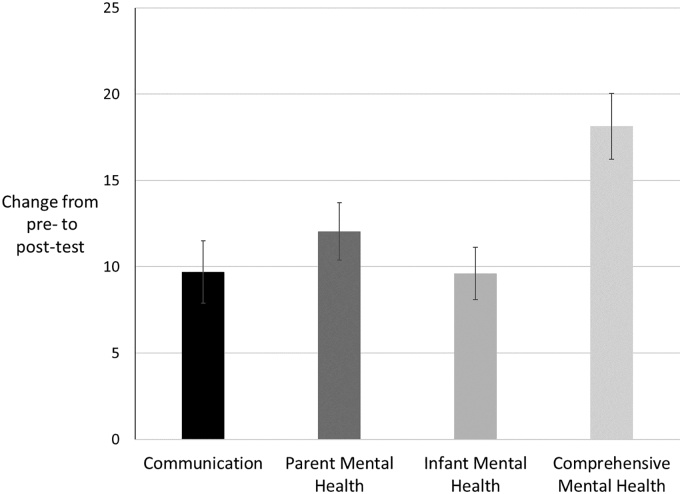
Table 3 presents descriptives for the knowledge assessments both overall and within each of the domains at pre- and post-test. Overall, knowledge scores increased from pre- to post-test (F(1,89) = 28.8, p < .001), with similar increases in knowledge scores across all domains (F(1,87) = 0.96, p = .41). Difference scores also indicated significant increases within each domain, even when controlling for overall initial knowledge scores at pre-test (Figure 1). Knowledge scores increased by 9 to 18 points, representing medium to large effects for all domains (d = .62 to 1.0). Further analyses indicated that increases were of similar extents regardless of fellowship year (F(2, 87) = 0.78, p = .46).
Table 3.
Descriptives for knowledge and self-efficacy assessments at 3 time points
| Pre-test (n = 108) |
Post-test (n = 91) |
3 month follow-up (n = 45) |
||||
|---|---|---|---|---|---|---|
| Knowledgea | 67.2 (9.4) | 69.0 | 79.1 (10.8) | 81.5 | 74.5 (8.3) | 75.0 |
| Communication | 72.6 (17.5) | 75.0 | 82.0 (16.8) | 88.0 | 79.4 (14.9) | 75.0 |
| Parent Mental Health | 66.8 (14.1) | 62.5 | 78.9 (14.3) | 75.0 | 71.1 (16.0) | 75.0 |
| Infant Mental Health | 68.3 (15.4) | 75.0 | 77.3 (13.6) | 75.0 | 80.6 (11.5) | 87.5 |
| Comprehensive Mental Health | 61.0 (13.8) | 62.5 | 78.3 (16.5) | 88.0 | 66.7 (15.5) | 62.5 |
| Self-Efficacyb | 4.7 (0.4) | 4.7 | 5.2 (0.4) | 5.1 | 5.1 (0.4) | 5.0 |
| Communication | 4.9 (0.4) | 5.0 | 5.2 (0.4) | 5.1 | 5.1 (0.4) | 5.1 |
| Parent Mental Health | 4.5 (0.6) | 4.5 | 5.2 (0.5) | 5.0 | 5.0 (0.4) | 5.0 |
| Infant Mental Health | 4.6 (0.5) | 4.8 | 5.3 (0.5) | 5.1 | 5.1 (0.4) | 5.0 |
| Comprehensive Mental Health | 4.7 (0.5) | 4.6 | 5.1 (0.5) | 5.0 | 5.1 (0.4) | 5.0 |
Mean (SD) and median percent correct on knowledge assessment, overall and for four domains.
Mean (SD) and median ratings of self-efficacy, overall and for four domains, on a 6-point scale from strongly disagree to strongly agree.
Fig. 1.
Estimated marginal means in difference scores on knowledge assessments (change from pre- to post-test) by domain, controlling for overall knowledge scores at pre-test (n = 109)
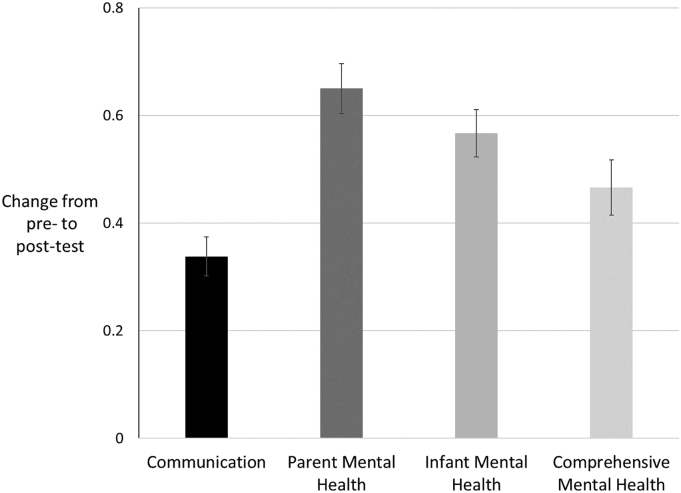
Self-efficacy scores also significantly increased from pre- to post-test assessment (F(1,90) = 165.8, p < .001) (Table 3), in all domains, however, increases were somewhat greater in “Infant Mental Health” and “Parent Mental Health” than in other domains. Analyses using difference scores also showed significant effects of program participation in all domains (Figure 2). Effect sizes were all large (d = .86 to 1.3). Further analyses indicated that self-efficacy scores increased more for fellows in their 1st year than for those in later years of fellowship and reached levels comparable to fellows from later years on post-course assessment. Fellows who made more gains in knowledge scores also showed the strongest increases in self-efficacy (r(90) = .37, p < .001).
Fig. 2.
Estimated marginal means in difference scores on self-efficacy assessments (change from pre- to post-test) by domain, controlling for overall self-efficacy scores at pre-test (n = 109)
Assessments at 3-months post-education (Table 3) revealed that the significant increases from pre-course levels persisted for both knowledge (F(1, 42) = 37.8, p < .001) and self-efficacy (F(1, 42) = 41.0 , p < .001). There was no significant effect of fellowship year on persistence of gains for either knowledge or self-efficacy, meaning all fellows showed similar retention.
3.5. Post-course feedback
Finally, feedback on the post-course survey indicated that 84% of fellows completing the online course agreed or strongly agreed that the course improved their knowledge about how to better provide emotional support to NICU families (Likert score mean 5.15 out of 6), 83% agreed or strongly agreed that taking the course would change their practice (5.0 out of 6), and 84% that they would recommend the course to other colleagues (5.15 out of 6).
4. Discussion and conclusion
4.1. Discussion
In spite of high levels of emotional distress among NICU families, educational deficits in mental health issues during both pediatric and neonatology training persist. A number of educational interventions have been developed for pediatric residents on communication and mental health, described in a 2019 AAP report [25], Most target specific mental health conditions as opposed to general principles. Additionally, the ACGME has noted that subspecialty-bound residents may receive less mental health training than residents entering general practice, because those interested in subspecialties spend more of their 6 months of individualized learning time focused on their future subspecialty [26]. Studies of prior communication training programs for neonatal fellows have focused almost exclusively on end-of-life conversations in small numbers of fellows [[27], [28], [29]]. In contrast, our course focused on general principles of communication and mental health in the NICU involving a larger number of participants.
Although we did not receive responses from all neonatology PDs, our data suggests that a lack of understanding of mental health issues in the NICU may represent a major educational weakness nationally, that could create impairments in care with long lasting impact. Our study found that knowledge scores did not differ among fellows of different years of training—all scores were equally low-- indicating that among programs surveyed, fellowship training is ineffectively covering this content. While knowledge scores did not differ by year of training, self-efficacy did. Exposure to clinical environments and what formal teaching exists may be providing a false sense of confidence in the content area of mental health. Knowledge and self-efficacy were largely unrelated at pre-course measurement indicating that trainees are unaware of what they do not know. Overconfidence in medicine has been linked to an increase in errors and reduction in performance [30,31], meaning some fellows maybe doing a poor job supporting NICU family mental health and inadvertently failing to mitigate or potentially increasing distress in their patients. Higher self-efficacy leads an individual to engage in tasks they believe they have strengths in accomplishing. Fellows in our study with low self-efficacy may be avoiding interacting with families in crisis, believing, for some erroneously, that they lack the required skills [32]. A paucity of education around mental health issues, coupled with lack of feedback, may cause significant deficits in addressing the emotional needs of NICU families, either through poor performance for those overconfident, or through avoidance for those with low self-efficacy but solid knowledge. Strong interest in mental health programming shown in pre-study PDs survey supports overall awareness of gaps in training. As most educational programming is guided by ABP board requirements, expansion of these content areas may motivate creation and adoption of mental health curricula.
Increasingly, modern technology has supported the development of national or international online learning programs with documented success in improving trainee knowledge, confidence and practice behaviors, including in neonatology [[33], [34], [35], [36]]. Members of the Organization of Neonatal Training Program Directors Council are developing a nationally available cache of presentations covering core physiology topics for fellows to support flipped classroom methodology [37]. Sharing of online educational resources and conference presentations were further expanded during the COVID pandemic highlighting the capabilities of digitally available programming [38]. Our course is an effective example of online core educational programming that significantly improved fellow knowledge and self-efficacy in recognizing and managing NICU family mental health issues with lasting retention. In addition, the majority of fellows found the course valuable and would recommend it to others. Most current programs to improve mental health training in pediatrics are occurring at the community and state level [39], making our program unique in its national reach. Our educational course is an example of an accessible, effective, scalable, and valued educational program for fellows, implemented at the national level, and may be an exemplar for others attempting to create similar content in their own subspecialties of pediatrics.
Curricula in mental health, in particular, may be conducive to presentation in an online platform. Although increased recognition of mental health disorders is occurring, available resources to appropriately cover these topics may be lacking at many institutions. A survey of pediatric residency program directors listed a lack of instructional content, instructional methods and resources among the barriers to behavioral health training [40]. Among pediatric resident continuity clinics, only half have access to mental health professionals [16,40] and most pediatricians lack the ability to model effective mental health practices [21,41]. Among the programs which participated in our study, only half had psychology services available in the NICU and even fewer had psychologists supporting infant/family mental health. Even when mental health clinicians are embedded in clinical teams, they are often stretched thin and are tasked with primarily clinical care rather than education [42]. This leaves frontline clinical providers with the responsibility to assess and manage common mental health concerns among patients and families. Availability of an online course to effectively cover mental health topics may be the best way for many programs to provide this information for their trainees.
Although most fellows in our study reported having some mental health education during medical school and/or residency, there was no correlation between the degree of previous training and knowledge on pre-course assessment. Training during medical school and residency may familiarize fellows with mental health issues overall but the specific presentation and mitigation strategies in the NICU may be unique to the particular patient population. The results of our study underscore the need for more targeted subspecialty-specific training. Other specialties should make their own assessments as similar targeted mental health training may be needed.
Our study has several limitations. First, sampling bias exists at both the program and fellow level. Participating programs may not represent the national pool as program directors with greater interest in mental health issues or with no psychology resources may have been more likely to participate. In addition, fellows were not required to participate so that fellows who did engage may have been more interested in the topic with potentially higher knowledge and self-efficacy than the general fellow population. However, enthusiasm for the course may also have been skewed to higher ratings. In addition, observational bias exists as fellows were aware of course participation and serial evaluation. This may have consciously or unconsciously had an effect on their answers.
Although our course produced significant improvements in knowledge and self-efficacy on serial surveys, it is unknown how these results might translate into performance in live simulations or real patient encounters, which is ultimately the key metric by which this and other similar courses should be judged. Several other educational programs have used the combination of online content with simulation to good results[43]. Subsequent evaluation of the course’s impact on fellow interactions with simulated patients experiencing emotional distress might shed more light on whether knowledge and self-efficacy translates into performance improvement. Additionally, future research could include assessments of fellow interactions with families by faculty, nurses and the families themselves.
Online learning programs have both advantages and limitations. Although current learners may be comfortable with electronic devices, a year on digital platforms during the COVID-19 pandemic has shown limitations such as risk of boredom and poor connections with other students [44]. Live interpersonal interactions are important when providing psychosocial support to families. This course might be most effective when coupled with an interactive simulation component, whether in-person or accomplished on a virtual platform, allowing trainees to practice their skills. A flipped classroom model using case or in-person discussions with former NICU parents are other possible avenues to enrich the course.
4.2. Innovation
Although online platforms have been used to disseminate education nationally, to the knowledge of the authors, no national program exists to teach medical trainees how to handle mental health issues either in pediatrics or in any of its subspecialties, leaving each individual PD to create their own. The relative paucity of psychology resources in pediatric care settings and discomfort among pediatricians in addressing psychological issues leave the area of mental health undersupported in individual educational programs. Both the content and style of our course may serve as a template for others developing similar curricula, with the opportunity to standardize and scale content meeting criteria prescribed by accrediting bodies, saving valuable time and resources among faculty already stretched thin with teaching responsibilities. In particular the marriage of evidence-based content covering both parent and infant distress in a structure utilizing family quotes and stories is an innovative and effective method to harness the family experience in mental health training within neonatology.
4.3. Conclusion
Mental health training is vital to pediatric trainees, including neonatal fellows, and represents a national deficit. Our course was effective at improving neonatology fellows’ knowledge and self-efficacy in recognizing and mitigating emotional distress in the NICU with results lasting over 3 months later. Most courses to teach mental health issues in pediatrics have occurred at a local level. To the knowledge of the authors, our program is the first national pediatric course to train fellows in mental health challenges in our patients and their families, and may serve as an exemplar to other specialties creating their own programming. Future research should explore impacts of this course, and others teaching mental health, on trainee clinical behavior and patient outcomes. It should be a goal of every pediatric training program, including fellowships in neonatology and all other subspecialties, to include a formal course offering training in communication and in mental health of patients and their families.
Acknowledgments
Acknowledgments
We would like to thank the following for their support and participation:
Women & Infants Hospital of Rhode Island/Warren Alpert Medical School of Brown University -Beatrice E. Lechner, MD
Duke University-Susan Izatt, MD, MEd
Emory University School of Medicine/Children’s Healthcare of Atlanta-Theresa W. Gauthier, MD
Medstar Georgetown University Hospital-Karen Kamholtz, MD, MPH
Harvard University/Boston Children’s Hospital-Kristen T. Leeman, MD
Oregon Health & Science University-Amanda Kim, MD
Saint Louis University-Rebecca Petersen, MD, MACM
Stanford University/Lucile Packard Children’s Hospital-Melissa Scala, MD
University of Texas Health San Antonio-Margarita M Vasquez, MD
University of California, Davis Medical Center-Kristin R. Hoffman, MD
University of California San Francisco Division of Neonatology-Luke M. Judge, MD, PhD and Katelin P. Kramer, MD
University of Colorado School of Medicine-Jeanne P Zenge, MD
University of California Los Angeles David Geffen School of Medicine-Josephine M Enciso, MD, MACAM
University of Connecticut School of Medicine/Connecticut Children’s Hospital-Jennifer M. Trzaski, MD
University of New Mexico-Jessie R. Maxwell, MD and Dawn Novak, MD
University of Wisconsin-Madison School of Medicine and Public Health-C. Lydia Wraight, MD
Vanderbilt University Medical Center-Maria Gillam-Krakauer, MD, MEd
Weill Cornell Medical College-Ericalyn Kasdorf, MD
University of Tennessee Health Science Center-Jennifer Davidson, DO.
University of Minnesota-Johannah M. Scheurer, MD, Heidi Kamarth, DO, Elizabeth Ramey, MS, CCRC
Funding
Support for this project was provided by a Special Projects Grant from the Association of Pediatric Program Directors.
The authors have no competing interests to declare.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pecinn.2022.100053.
Appendix A. Supplementary data
Supplementary material
References
- 1.March of Dimes March of Dimes. https://www.marchofdimes.org Accessed November 13, 2021.
- 2.Shaw R., Deblois T., Ikuta L., Ginzburg K., Fleisher B., Koopman C. Acute stress disorder among parents of infants in the neonatal intensive care nursery. Psychosomatics. 2006;47:206–212. doi: 10.1176/appi.psy.47.3.206. [DOI] [PubMed] [Google Scholar]
- 3.Kim P., Swain J.E. Review: Sad dads: Paternal postpartum depression. Psychiatry. 2007;4:36–47. [PMC free article] [PubMed] [Google Scholar]
- 4.Hynan M.T., Mounts K.O., Vanderbilt D.L. Screening Parents of High-Risk Infants for Emotional Distress: Rationale and Recommendations. J Perinatol. 2013;33:748–753. doi: 10.1038/jp.2013.72. [DOI] [PubMed] [Google Scholar]
- 5.Holditch-Davis D., Santos H., Levy J., White-Traut R., O’Shea T.M., Geraldo V., et al. Patterns of psychological distress in mothers of preterm infants. Infant Behav Dev. 2015;41:154–163. doi: 10.1016/j.infbeh.2015.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim W.J., Lee E., Kim K.R., Namkoong K., Park E.S., Rha D.W. Progress of PTSD symptoms following birth: a prospective study in mothers of high-risk infants. J Perinatol. 2015;35:575–579. doi: 10.1038/jp.2015.9. [DOI] [PubMed] [Google Scholar]
- 7.Greene M.M., Rossman B., Patra K., Kratovil A.L., Janes J.E., Meier P.P. Depression, anxiety, and perinatal-specific posttraumatic distress in mothers of very low birth weight infants in the neonatal intensive care unit. J Dev Behav Pediatr. 2015;36:362–370. doi: 10.1097/DBP.0000000000000174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lean R.E., Rogers C.E., Paul R.A., Gerstein E.D., Hospitalization N.I.C.U. Long-Term Implications on Parenting and Child Behaviors. Curr Treat Options Pediatr. 2018;4:49–69. [PMC free article] [PubMed] [Google Scholar]
- 9.Garfield C.F., Lee Y.S., Warner-Shifflett L., Christie R., Jackson K.L., Miller E. Maternal and paternal depression symptoms during NICU stay and transition home. Pediatrics. 2021;148:2. doi: 10.1542/peds.2020-042747. [DOI] [PubMed] [Google Scholar]
- 10.Bernard-Bonnin A.C. Canadian paediatric society, mental health and developmental disabilities committee. Maternal depression and child development. Paediatr Child Health. 2004;9:575–583. [Google Scholar]
- 11.Huhtala M., Korja R., Lehtonen L., Haataja L., Lapinleimu H., Rautava P., et al. Parental psychological well-being and behavioral outcome of very low birth weight infants at 3 years. Pediatrics. 2012;129:e937–e944. doi: 10.1542/peds.2011-2411. [DOI] [PubMed] [Google Scholar]
- 12.Surkan P.J., Ettinger A.K., Ahmed S., Minkovitz C.S., Strobino D. Impact of maternal depressive symptoms on growth of preschool- and school-aged children. Pediatrics. 2012;130:e847–e855. doi: 10.1542/peds.2011-2118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Melnyk B.M., Feinstein N.F., Alpert-Gillis L., Fairbanks E., Crean H.F., Sinkin R.A., et al. Reducing premature infants’ length of stay and improving parents’ mental health outcomes with the Creating Opportunities for Parent Empowerment (COPE) neonatal intensive care unit program: a randomized, controlled trial. Pediatrics. 2006;118:e1414–e1427. doi: 10.1542/peds.2005-2580. [DOI] [PubMed] [Google Scholar]
- 14.Brecht C.J., Shaw R.J., St. John N.H., Horwitz S.M. Effectiveness of therapeutic and behavioral interventions for parents of low-birth-weight premature infants: A review. Infant Ment Health J. 2012;33:651–665. doi: 10.1002/imhj.21349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Segre L.S., Chuffo-Siewert R., Brock R.L., O’Hara M.W. Emotional distress in mothers of preterm hospitalized infants: a feasibility trial of nurse-delivered treatment. J Perinatol. 2013;33:924–928. doi: 10.1038/jp.2013.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shaw R.J., John N. St, Lilo E.A., Jo B., Benitz W., Stevenson D.K., et al. Prevention of traumatic stress in mothers with preterm infants: a randomized controlled trial. Pediatrics. 2013;132:e886–e894. doi: 10.1542/peds.2013-1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pickler R.H., McGrath J.M., Reyna B.A., McCain N., Lewis M., Cone S., et al. A model of neurodevelopmental risk and protection for preterm infants. J Perinat Neonatal Nurs. 2010;24:356–365. doi: 10.1097/JPN.0b013e3181fb1e70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pereira F.L., de Góes Fdos S. Nogueira, Fonseca L.M., Scochi C.G., Castral T.C., Leite A.M. A manipulação de prematuros em uma Unidade de Terapia Intensiva Neonatal [Handling of preterm infants in a neonatal intensive care unit] Rev Esc Enferm USP. 2013;47:1272–1278. doi: 10.1590/S0080-623420130000600003. [DOI] [PubMed] [Google Scholar]
- 19.Patton G.C., Coffey C., Carlin J.B., Olsson C.A., Morley R. Prematurity at birth and adolescent depressive disorder. Br J Psychiatry. 2004;184:446–447. doi: 10.1192/bjp.184.5.446. [DOI] [PubMed] [Google Scholar]
- 20.Singh G.K., Kenney M.K., Ghandour R.M., Kogan M.D., Lu M.C. Mental health outcomes in US children and adolescents born prematurely or with low birthweight. Depress Res Treat. 2013;2013:5070743. doi: 10.1155/2013/570743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Horwitz S.M., Storfer-Isser A., Kerker B.D., Szilagyi M., Garner A., O’Connor K.G., et al. Barriers to the identification and management of psychosocial problems: changes from 2004 to 2013. Acad Pediatr. 2015;15:613–620. doi: 10.1016/j.acap.2015.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Behavioral and Mental Health: Gaps and Challenges The American Board of Pediatrics. https://www.abp.org/news/behavioral-and-mental-health-gaps-and-challenges Published March 12, 2018. Accessed November 13, 2021.
- 23.Roadmap Project The American Board of Pediatrics. 2021. https://www.abp.org/foundation/roadmap Accessed November 13, 2021.
- 24.Foy J.M., Green C.M., Earls M.F. Committee on psychosocial aspects of child and family Health MHLWG. Mental health competencies for pediatric practice. Pediatrics. 2019;144:5. doi: 10.1542/peds.2019-2757. [DOI] [PubMed] [Google Scholar]
- 25.Green C.M., Foy J.M., Earls M.F. Committee on psychosocial aspects of child and family health MHLWG. Achieving the pediatric mental health competencies. Pediatrics. 2019;144:5. doi: 10.1542/peds.2019-2758. [DOI] [PubMed] [Google Scholar]
- 26.Accreditation Council on Graduate Medical Education ACGME Core Competencies. https://www.ecfmg.org/echo/acgme-core-competencies.html Available at. Accessed March 9, 2018.
- 27.Harris L.L., Placencia F.X., Arnold J.L., Minard C.G., Harris T.B., Haidet P.M. A structured end-of-life curriculum for neonatal-perinatal postdoctoral fellows. Am J Hosp Palliat Care. 2015;32:253–261. doi: 10.1177/1049909114523825. [DOI] [PubMed] [Google Scholar]
- 28.Lizotte M.H., Barrington K.J., Sultan S., Pennaforte T., Moussa A., Lachance C., et al. Techniques to communicate better with parents during end-of-life scenarios in neonatology. Pediatrics. 2020;145 doi: 10.1542/peds.2019-1925. [DOI] [PubMed] [Google Scholar]
- 29.Boss R., Urban A., Barnett M., Arnold R. Neonatal critical care communication (NC3): training NICU physicians and nurse practitioners. J Perinatol. 2013;33:642–646. doi: 10.1038/jp.2013.22. [DOI] [PubMed] [Google Scholar]
- 30.Saposinik G., Redelmeler D., Ruff C.C., Tobler P.N. Cognitive biases associated with medical decisions: a systematic review. BMC Med Inform Decis Mak. 2016;16:138. doi: 10.1186/s12911-016-0377-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Crowe S., Clarke N., Brugha R., R. ‘You do not cross them’: hierarchy and emotion in doctors’ narratives of power relations in specialist training. Soc Sci Med. 2017;186:70–77. doi: 10.1016/j.socscimed.2017.05.048. [DOI] [PubMed] [Google Scholar]
- 32.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 33.Bundy D.G., Dorawski L.F., Lazorick S., Bradbury S., Kamachi K., Suresh G.K. Education in Quality Improvement for Pediatric Practice: an online program to teach clinicians QI. Acad Pediatr. 2014;14:517–525. doi: 10.1016/j.acap.2014.05.008. [DOI] [PubMed] [Google Scholar]
- 34.Stankovic C., Wolff M., Chang T.P., Macias C. A national patient safety curriculum in pediatric emergency medicine. Pediatr Emerg Care. 2019;35:519–521. doi: 10.1097/PEC.0000000000001533. [DOI] [PubMed] [Google Scholar]
- 35.Pahud B., Williams S. Elizabeth, Lee B.R., Lewis K.O., Middleton D.B., Clark S., et al. A randomized controlled trial of an online immunization curriculum. Vaccine. 2020;38:7299–7307. doi: 10.1016/j.vaccine.2020.09.043. [DOI] [PubMed] [Google Scholar]
- 36.Neonatal Resuscitation Program American Academy of Pediatrics. http://services.aap.org/en/learning/neonatal-resuscitation-program/ Accessed November 13, 2021.
- 37.Izatt S., Gray M., Dadiz R., French H. Development and implementation of a national neonatology flipped classroom curriculum. J Grad Med Educ. 2019;11:335–336. doi: 10.4300/JGME-D-18-00907.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mikuteit M., Steffens S., Grigull L., Kuhnle L., Behrends M., Schmidt R., et al. Rapid development of a digital module during the Covid 19 pandemic in undergraduate medical education of pediatrics by teachers and students. GMS J Med Educ. 2020;37:Doc66. doi: 10.3205/zma001359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mental Health Initiatives | Implementation of the Curriculum American Academy of Pediatrics. http://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Mental-Health/Pages/implementation.aspx Accessed November 13, 2021.
- 40.Shahidullah J.D., Kettlewell P.W., Palejwala M.H., Forman S.G., Billups A., Anismatta S.L., et al. Behavioral health training in pediatric residency programs: a national survey of training directors. J Dev Behav Pediatr. 2018;39:292–302. doi: 10.1097/DBP.0000000000000548. [DOI] [PubMed] [Google Scholar]
- 41.Hampton E., Richardson J.E., Bostwick S., Ward M.J., Green C. The current and ideal state of mental health training: pediatric resident perspectives. Teach Learn Med. 2015;27:147–154. doi: 10.1080/10401334.2015.1011653. [DOI] [PubMed] [Google Scholar]
- 42.Samsel C., Ribeiro M., Ibeziako P., DeMaso D.R. Integrated behavioral health care in pediatric subspecialty clinics. Child Adolesc Psychiatr Clin N Am. 2017;26:785–794. doi: 10.1016/j.chc.2017.06.004. [DOI] [PubMed] [Google Scholar]
- 43.Fallucco E.M., Hanson M.D., Glowinski A.L. Teaching pediatric residents to assess adolescent suicide risk with a standardized patient module. Pediatrics. 2010;125:953–959. doi: 10.1542/peds.2009-2135. [DOI] [PubMed] [Google Scholar]
- 44.Baltà-Salvador R., Olmedo-Torre N., Peña M., Renta-Davids A.I. Academic and emotional effects of online learning during the COVID-19 pandemic on engineering students. Educ Inf Technol (Dordr) 2021:1–28. doi: 10.1007/s10639-021-10593-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material