Abstract
Trauma-related hemorrhagic shock is a global problem. This study aimed to analyze the knowledge domain and frontiers of trauma-related hemorrhagic shock research through a bibliometric analysis. Articles on trauma-related hemorrhagic shock published between 2012 and 2022 were retrieved from the Web of Science Core Collection, and a bibliometric analysis was conducted using CiteSpace and VOSviewer. A total of 3116 articles and reviews were analyzed. These publications primarily came from 441 institutions in 80 countries, with the USA having the highest number of publications, followed by China. Among the publications, Ernest E. Moore published the most papers, whereas John B. Holcomb had the most co-citations. The most productive institution was the University of Pittsburgh in the USA. The keyword burst and reference clustering analysis indicated that “reboa,” “whole blood,” “exsome,” “glycocalyx,” “endotheliopathy,” and “predictor” are new trends and developing areas of interest. With the help of CiteSpace and VOSviewer, this study provides a deeper understanding of the research landscape, frontier hotspots, and future trends in trauma-related hemorrhagic shock over the last decade. “Whole blood” instead of “component therapy” shows potential advantage while “REBOA” is increasingly discussed in rapid hemostasis. This study provides important clues for researchers to understand the knowledge domain and frontiers of this study field.
Keywords: bibliometric analysis, CiteSpace, hemorrhagic shock, trauma, visualization, VOSviewer
1. Introduction
Trauma is a major public health crisis, contributing to >4.48 million deaths annually.[1] The most preventable deaths are due to uncontrolled early hemorrhaging.[2] Hemorrhagic shock is an acute hemorrhage or excessive fluid loss resulting in hypovolemia,[3] which may lead to hemodynamic instability, decreased oxygen delivery, cellular hypoxia, organ damage, and ultimately death.[4] Trauma-related hemorrhagic shock causes 1.5 million deaths per year worldwide, representing a substantial global problem.[5]
An increasing number of scholars have devoted themselves to the study of hemorrhagic shock. Consequently, the understanding and management of hemorrhagic shock have evolved significantly[6]; however, there is scant literature depicting published outputs, influential authors, countries/regions, institutions, their collaborations, hotspots, and research trends in trauma-related hemorrhagic shock. Bibliometrics is a multidisciplinary science that applies mathematical and statistical approaches to conduct both qualitative and quantitative analyses of publications in a specific research domain. It can also predict frontiers and research trends based on the literature’s characteristics.[7,8] Additionally, CiteSpace and VOSviewer are 2 popular tools used in bibliometric analysis.[9–11] Accordingly, in this study, we aimed to investigate the knowledge domain and frontiers of trauma-related hemorrhagic shock research using CiteSpace (version 5.8.3) and VOSviewer (version 1.6.18).
2. Materials and methods
2.1. Data source and retrieval strategy
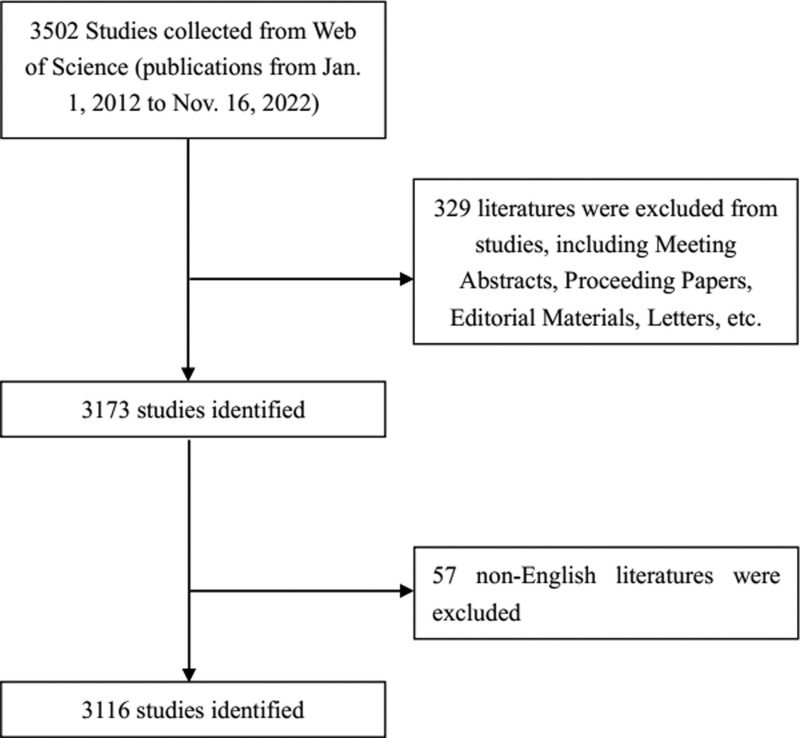
Data were collected from Web of Science Core Collections, and medical subject heading terms were used as retrieval tools. The search strategy was as follows: TS= “hemorrhagic shock” and (“trauma*” or “injur*” or “wound*”). The symbol “*” was used as a wildcard to represent 1 or more letters.[12] The search period was from January 1, 2012, to November 16, 2022. “Article” and “review article” were selected as article types and the language was confined to English. The analysis was conducted on November 16 to avoid data bias due to database updates. In total, 3116 papers were included in this study. The screening process is illustrated in Figure 1.
Figure 1.
Flowchart of the screening process.
2.2. Data analysis and visualization
CiteSpace was used to perform the co-citation analysis (authors, journals, and references), collaboration network analysis (countries/regions, institutions, and authors), citation bursts, and timeline views for keywords and references. The specific parameters were set as follows: time slicing (from January 2012 to November 2022; years per slice = 1), text processing (title, abstract, author keywords, and keywords plus), node type (one option chosen at a time from country, institution, author, co-cited journal, co-cited author, or co-cited reference), link strength (cosine), link scope (within slices), selection criteria (g-index, k = 25), and pruning (none). The other parameters were set to their default values.
VOSviewer was used for map creation, visualization, and exploration based on the network data,[13] and to create keyword co-occurrences and dense maps based on the text data. We also used the visualization to predict future research hotspots based on the network of keywords in color-coded clusters.[14,15]
We obtained the journal citation reports (JCR), 2021 impact factor, and JCR division of the analyzed journals from the Web of Science.
2.3. Ethics and consent
This study involved no animal or human subjects; therefore, no ethical approval was required.
3. Results
3.1. Temporal distribution map of publications and citations
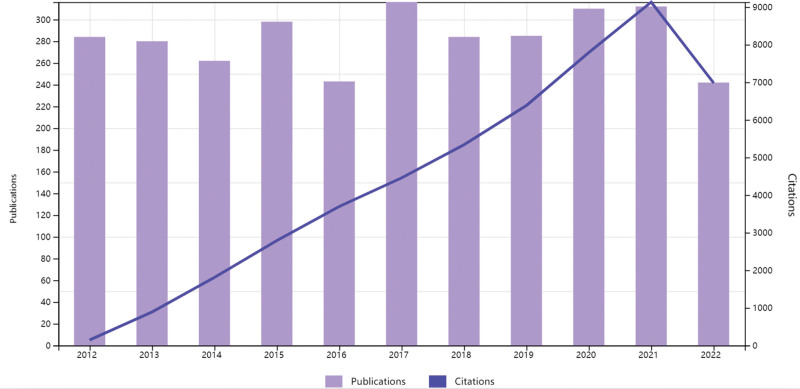
Overall, 3116 papers regarding trauma-related hemorrhagic shock research were published between January 2012 and November 2022. As shown in Figure 2, the output of publications fluctuated, but was stable at >240 annually, with the lowest number in 2022 (242 publications as of November 2022) and the highest in 2017 (316 publications). The results showed a steadily increasing trend in output from 2018 to 2021. Additionally, numbered citations increased steadily from 2012 to 2021.
Figure 2.
Temporal distribution map of publications and citations.
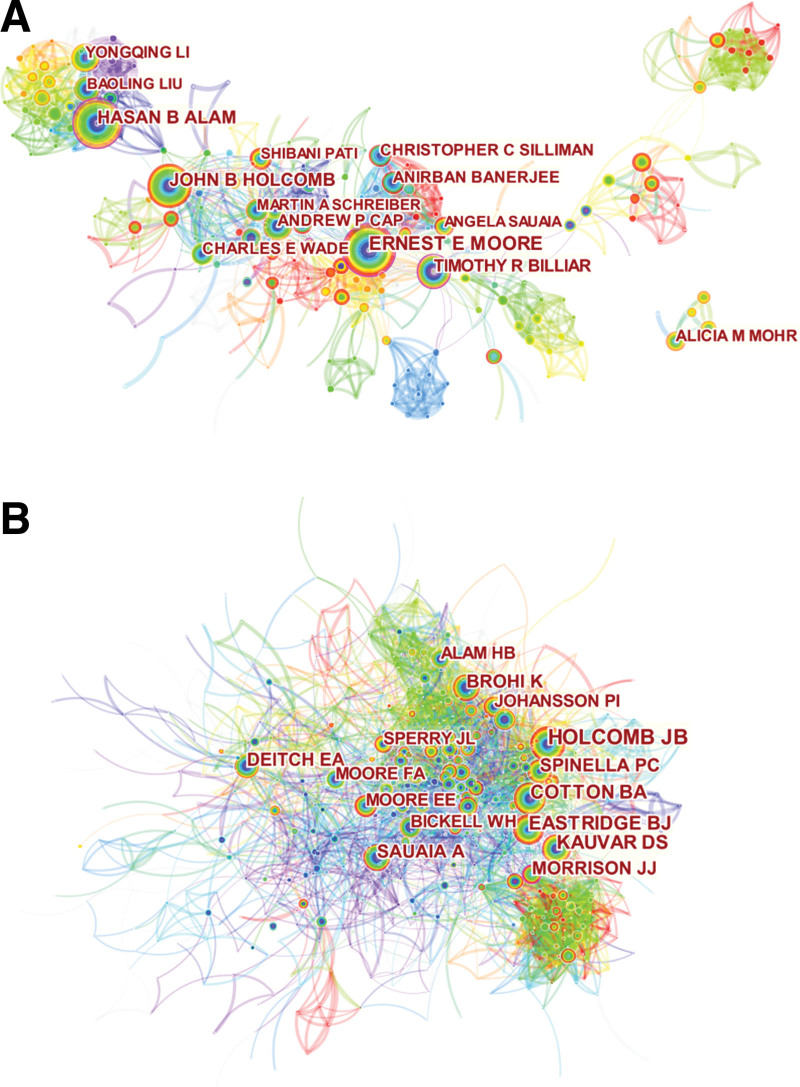
3.2. Visual analysis of authors and co-cited authors
In total, 558 authors and 778 co-cited authors were associated with trauma-related hemorrhagic shock. As shown in Table 1 and Figure 3, the most productive author was Ernest E. Moore from the Denver Health Medical Center, with 75 publications, followed by Hasan B. Alam from Northwestern University, and John B. Holcomb from the University of Alabama Birmingham. Timothy R. Billiar from the University of Pittsburgh had the highest centrality (0.18). Among the top 10 co-cited authors, 8 were cited >200 times. John B. Holcomb (528 citations) was the most frequently cited author, followed by Cotton BA from the University of Texas (278 citations) and Kauvar DS from the Brooke Army Medical Center (276 citations). In addition, Morrison JJ from the University of Maryland had high centrality (0.11).
Table 1.
Top 10 authors and co-cited authors.
| Rank | Authors | Count | Centrality | Co-cited author | Citations | Centrality |
|---|---|---|---|---|---|---|
| 1 | Ernest E. Moore | 75 | 0.13 | Holcomb, J.B. | 528 | 0.03 |
| 2 | Hasan B. Alam | 73 | 0.11 | Cotton, B.A. | 278 | 0.04 |
| 3 | John B. Holcomb | 71 | 0.03 | Kauvar, D.S. | 276 | 0.03 |
| 4 | Timothy R. Billiar | 48 | 0.18 | Eastridge, B.J. | 269 | 0.02 |
| 5 | Andrew P. Cap | 40 | 0.05 | Brohi, K. | 227 | 0.05 |
| 6 | Charles E. Wade | 40 | 0.01 | Deitch, E.A. | 217 | 0.07 |
| 7 | Anirban Banerjee | 39 | 0.01 | Sauaia, A. | 213 | 0.04 |
| 8 | Yongqing Li | 38 | 0 | Spinella, P.C. | 202 | 0.04 |
| 9 | Alicia M. Mohr | 37 | 0 | Morrison, J.J. | 195 | 0.11 |
| 10 | Tao Li | 35 | 0 | Johansson, P.I. | 176 | 0.05 |
Figure 3.
Visual analysis of (A) authors and (B) co-cited authors. The node size represents the number of studies published by the author, with larger nodes representing a higher number of published papers. The closer the collaboration between 2 writers, the shorter the distance between the 2 nodes. The purple nodes represent early publications, while the red nodes represent recent or bursts of published articles.
3.3. Spatial distribution map of countries/regions and institutions
Overall, 441 institutions from 80 countries/regions contributed to the research on trauma-related hemorrhagic shock. As shown in Table 2 and Figure 4, the USA published the most articles (1573 publications), followed by China (590 publications) and Germany (240 publications) (Fig. 4A). In addition, the University of Pittsburgh published the most articles (162 publications), followed by the University of Maryland (103 publications), and the University of Texas Health Science Center, Houston (80 publications). The 10 most productive institutions were from the US, and 4 showed high centrality, namely, the University of Pittsburgh (0.37), the University of Maryland (0.26), the University of Michigan (0.11), and the Uniformed Services University of the Health Sciences (0.1; Fig. 4B, circled in purple). The lines connecting the circles represent international collaboration; dense connections indicate active cooperation among countries and affiliations (Fig. 4).
Table 2.
Top 10 most productive countries/regions and institutions.
| Rank | Country/Regions | Year | Count | Centrality | Institutions | Year | Count | Centrality |
|---|---|---|---|---|---|---|---|---|
| 1 | USA | 2012 | 1573 | 0.36 | Univ Pittsburgh | 2012 | 162 | 0.37 |
| 2 | People’s Republic of China | 2012 | 590 | 0.08 | Univ Maryland | 2012 | 103 | 0.26 |
| 3 | Germany | 2012 | 240 | 0.03 | Univ Texas Hlth Sci Ctr Houston | 2012 | 80 | 0.06 |
| 4 | Japan | 2012 | 158 | 0.01 | Uniformed Serv Univ Hlth Sci | 2012 | 75 | 0.1 |
| 5 | England | 2012 | 120 | 0.1 | Univ Michigan | 2013 | 72 | 0.11 |
| 6 | France | 2012 | 111 | 0.05 | Univ Colorado | 2012 | 67 | 0.04 |
| 7 | Italy | 2012 | 85 | 0.08 | Univ Washington | 2012 | 67 | 0.09 |
| 8 | Canada | 2012 | 84 | 0.14 | Univ Calif San Francisco | 2012 | 66 | 0.07 |
| 9 | Netherlands | 2012 | 69 | 0.04 | Denver Hlth Med Ctr | 2012 | 57 | 0.02 |
| 10 | Brazil | 2012 | 64 | 0.02 | US Army | 2014 | 54 | 0.03 |
Figure 4.
Spatial distribution map of (A) countries/regions and (B) institutions. Each circle in the diagram represents a nation/institution, with the size of the circle indicating the published outputs of the country/institution. The lines that connect the circles represent international collaboration, and the broader the lines, the closer the cooperation. The colors of the nodes and lines represent different years; the warmer the color, the more recent the publication. The purple circle indicates high centrality.
3.4. Visual analysis of journals and co-cited journals
Of the 3116 articles published in 200 academic journals, the Journal of Trauma and Acute Care Surgery (406 publications) published the most articles, followed by Shock (307 publications), and the Journal of Surgical Research (180 publications) (Table 3). Among the 827 co-cited journals, 7 had >1000 citations. As presented in Table 3, the Journal of Trauma had the most co-citations (2115), followed by Shock (1917), and Critical Care Medicine (1540). Six co-cited journals were in the Q1/2 JCR division.
Table 3.
Top 10 journals and co-cited journals.
| Rank | Journal | Count | JCR | IF (2021) | Co-cited journals | Citations | JCR | IF (2021) |
|---|---|---|---|---|---|---|---|---|
| 1 | Journal of Trauma and Acute Care Surgery | 406 | Q2 | 3.697 | Journal of Trauma* | 2115 | - | - |
| 2 | Shock | 307 | Q2 | 3.533 | Shock | 1917 | Q2 | 3.533 |
| 3 | Journal of Surgical Research | 180 | Q4 | 2.417 | Critical Care Medicine | 1540 | Q1 | 9.296 |
| 4 | PLOS One | 92 | Q3 | 3.752 | Journal of Trauma and Acute Care Surgery | 1477 | Q2 | 3.697 |
| 5 | Transfusion | 68 | Q3 | 3.337 | Annals of Surgery | 1284 | Q1 | 13.787 |
| 6 | Critical Care Medicine | 50 | Q1 | 9.296 | Critical Care | 1147 | Q1 | 19.334 |
| 7 | American Journal of Emergency Medicine | 49 | Q4 | 4.093 | Journal of Surgical Research | 1125 | Q4 | 2.417 |
| 8 | Surgery | 46 | Q2 | 4.348 | New England Journal of Medicine | 946 | Q1 | 176.079 |
| 9 | European Journal of Trauma and Emergency Surgery | 42 | Q3 | 2.374 | Injury | 862 | Q3 | 2.687 |
| 10 | Scientific reports | 35 | Q3 | 4.996 | PLOS One | 858 | Q3 | 3.752 |
JCR = journal citation reports.
Continued by the Journal of Trauma and Acute Care Surgery.
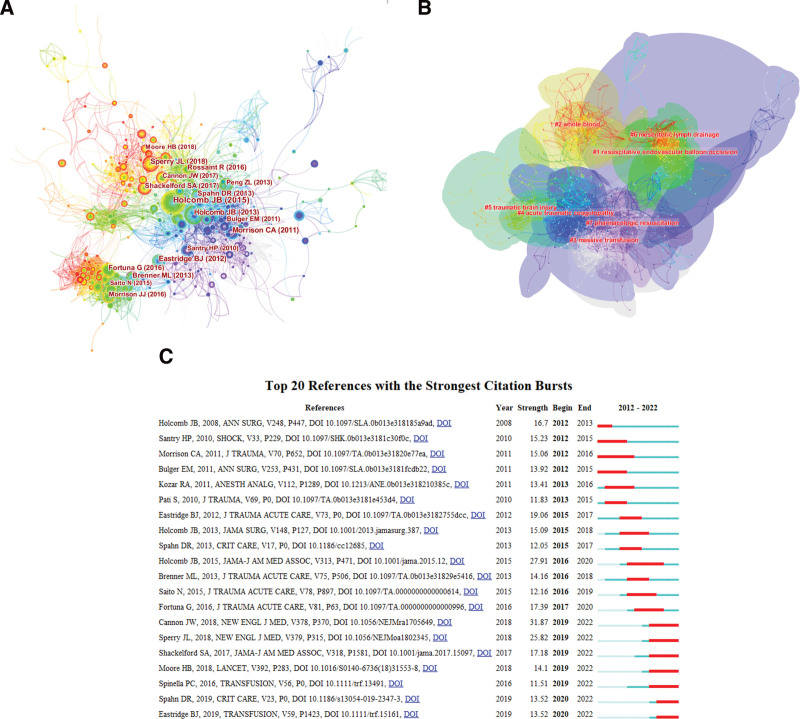
3.5. Visual analysis of co-cited references
Figure 5A displays the co-citations of the 866 citing articles, the first author, and the publication year of the top 10 most cited references, with additional information in Table 4. The most co-cited reference was a clinical trial published in JAMA by Holcomb et al[16] titled, “Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial.” This was followed by a review article by Jeremy W. Cannon[5] titled, “Hemorrhagic Shock” published in the New England Journal of Medicine.
Figure 5.
Visual analysis of (A) co-citations, (B) clustering networks, and (C) reference bursts. Each circle represents a reference. The size of the circle is proportional to the citation’s frequency. The link between the 2 circles represents 2 references cited in the same article among the cited articles. Similarly, line thickness is positively correlated with co-citation frequency.
Table 4.
Top 10 co-cited references.
| Rank | Title | Journal | Co-citation | Centrality |
|---|---|---|---|---|
| 1 | Transfusion of plasma, platelets, and red blood cells in a 1:1:1 versus a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial | JAMA | 146 | 0.4 |
| 2 | Hemorrhagic shock | New England Journal of Medicine | 95 | 0.04 |
| 3 | The prospective, observational, multicenter, major trauma transfusion (PROMMTT) study: comparative effectiveness of a time-varying treatment with competing risks | JAMA Surgery | 78 | 0.12 |
| 4 | Prehospital plasma during air medical transport in trauma patients at risk for hemorrhagic shock | New England Journal of Medicine | 71 | 0.05 |
| 5 | Death on the battlefield (2001–2011): implications for the future of combat casualty care | Journal of Trauma and Acute Care Surgery | 67 | 0.41 |
| 6 | Hypotensive resuscitation strategy reduces transfusion requirements and severe postoperative coagulopathy in trauma patients with hemorrhagic shock: preliminary results of a randomized controlled trial | Journal of Trauma | 61 | 0.09 |
| 7 | Contemporary outcomes of lower extremity vascular repairs extending below the knee: a multicenter retrospective study | Journal of Trauma and Acute Care Surgery | 58 | 0.09 |
| 8 | Association of prehospital blood product transfusion during medical evacuation of combat casualties in Afghanistan with acute and 30-day survival | JAMA | 57 | 0.03 |
| 9 | A clinical series of resuscitative endovascular balloon occlusion of the aorta for hemorrhage control and resuscitation | Journal of Trauma and Acute Care Surgery | 56 | 0.1 |
| 10 | The European guideline on management of major bleeding and coagulopathy following trauma: fourth edition | Critical Care | 50 | 0.04 |
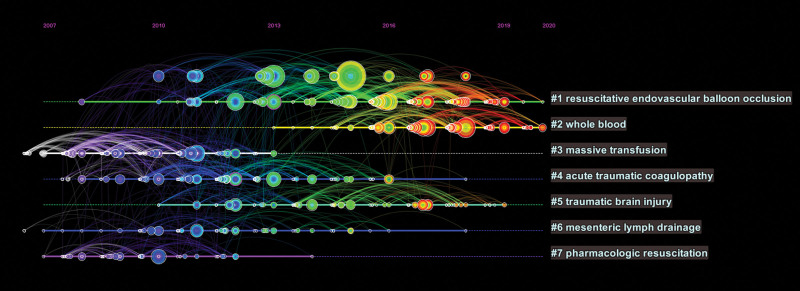
The 7 largest clusters extracted using the logarithmic likelihood ratio algorithm are shown in Figure 5B and include resuscitative endovascular balloon occlusion, whole blood, massive transfusion, acute traumatic coagulopathy, traumatic brain injury, mesenteric lymph drainage, and pharmacologic resuscitation. The total Q-value was 0.703 and each cluster had a weighted mean silhouette of 0.902, suggesting that the cluster quality was reasonable. Yellow clusters (clusters 1 and 2) indicate recently cited references and current hot topics.
The top 20 “burst” references are shown in Figure 5C. The first co-citation burst, titled “Increased plasma and platelet to red blood cell ratios improves outcome in 466 massively transfused civilian trauma patients,” began in 2012. One of the recent burst references, titled “Hemorrhagic Shock” by Jeremy W. Cannon, was published in 2018 and had the highest strength (31.87).[5] In addition, there were 7 co-citation bursts in 2022 regarding prehospital plasma in treating hemorrhagic shock[17–19] and guidelines on the management of major bleeding.[20]
A timeline view can visualize the evolution and progress of research hotspots over time.[21] As indicated in Figure 6, cluster 3 (massive transfusion) started earlier but ceased in 2013; clusters 4 to 7 ceased from 2013 to 2019, while clusters 1 (resuscitative endovascular balloon occlusion) and 2 (whole blood) are still ongoing, and can be considered frontiers.
Figure 6.
Timeline view of co-cited references. Each horizontal line represents a cluster; the smaller the number, the larger the cluster. The node size reflects co-cited frequency, and the links indicate the co-cited relationship; the colors of nodes and lines represent different years.
3.6. Keyword analysis of trending research topic
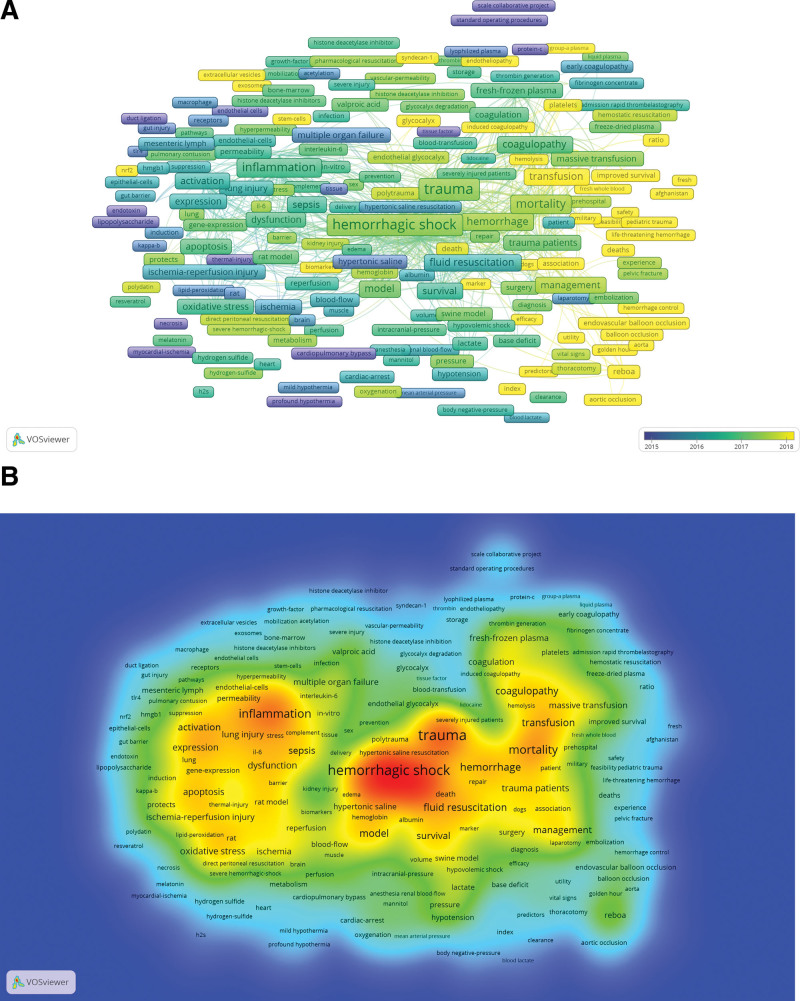
The keywords extracted from the titles and abstracts were analyzed using VOSviewer. A total of 9409 keywords were extracted, of which 557 keywords appeared >10 times, and 90 keywords appeared >50 times. As presented in Figure 7 and Table 5, “trauma” was the most important term with 728 co-occurrences, followed by “hemorrhagic shock,” “resuscitation,” and “injury.” In the keyword co-occurrence and dense visualization diagram, author keywords are marked in different colors according to their average publication years; “reboa,” “fresh whole blood,” “biomarker,” “hemorrhage control,” “exosomes,” “glycocalyx,” and “others” are highlighted in yellow indicating more recent publications.
Figure 7.
The (A) co-occurrence network, density visualization map of the (B) keywords.
Table 5.
Top 20 keywords.
| Rank | Keywords | Occurrences | Total link strength |
|---|---|---|---|
| 1 | Trauma | 728 | 5511 |
| 2 | Hemorrhagic shock | 714 | 5119 |
| 3 | Resuscitation | 613 | 4941 |
| 4 | Injury | 480 | 3481 |
| 5 | Mortality | 424 | 3321 |
| 6 | Inflammation | 381 | 3117 |
| 7 | Shock | 307 | 2545 |
| 8 | Hemorrhage | 304 | 2331 |
| 9 | Coagulopathy | 233 | 2138 |
| 10 | Transfusion | 253 | 2092 |
| 11 | Fluid resuscitation | 241 | 2044 |
| 12 | Model | 232 | 1812 |
| 13 | Activation | 215 | 1729 |
| 14 | Sepsis | 249 | 1846 |
| 15 | Survival | 201 | 1609 |
| 16 | Acute lung injury | 192 | 1487 |
| 17 | Sepsis | 192 | 1487 |
| 18 | Expression | 175 | 1400 |
| 19 | Oxidative stress | 179 | 1374 |
| 20 | Trauma patients | 168 | 1364 |
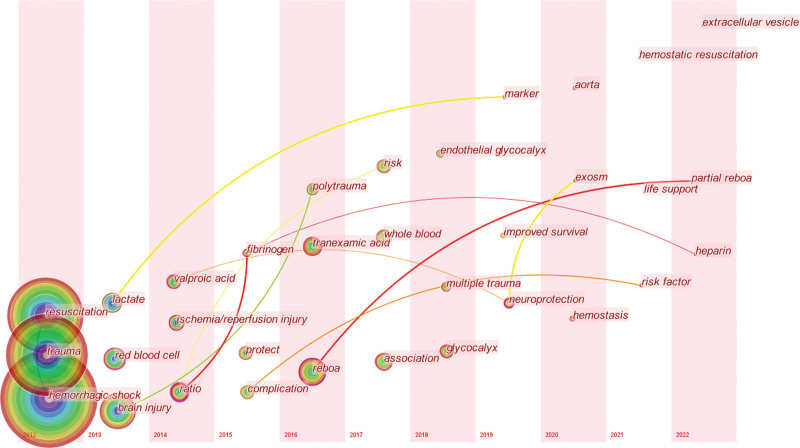
Figure 8 shows the timelines of the keywords and the evolution of the research topic over time. Progress in this field of research can be divided into 2 stages. From 2012 to 2015, studies focused primarily on trauma, lactate, fibrinolysis, and ischemia/reperfusion injury, indicating that researchers paid attention to the mechanisms and related basic research. From 2016 to 2022, the representative burst keywords were “reboa,” “whole blood,” “neuroprotection,” “improved survival,” and “life support,” suggesting a transition from basic to clinical research.
Figure 8.
Timeline view of keywords concerning trauma-related hemorrhagic shock research.
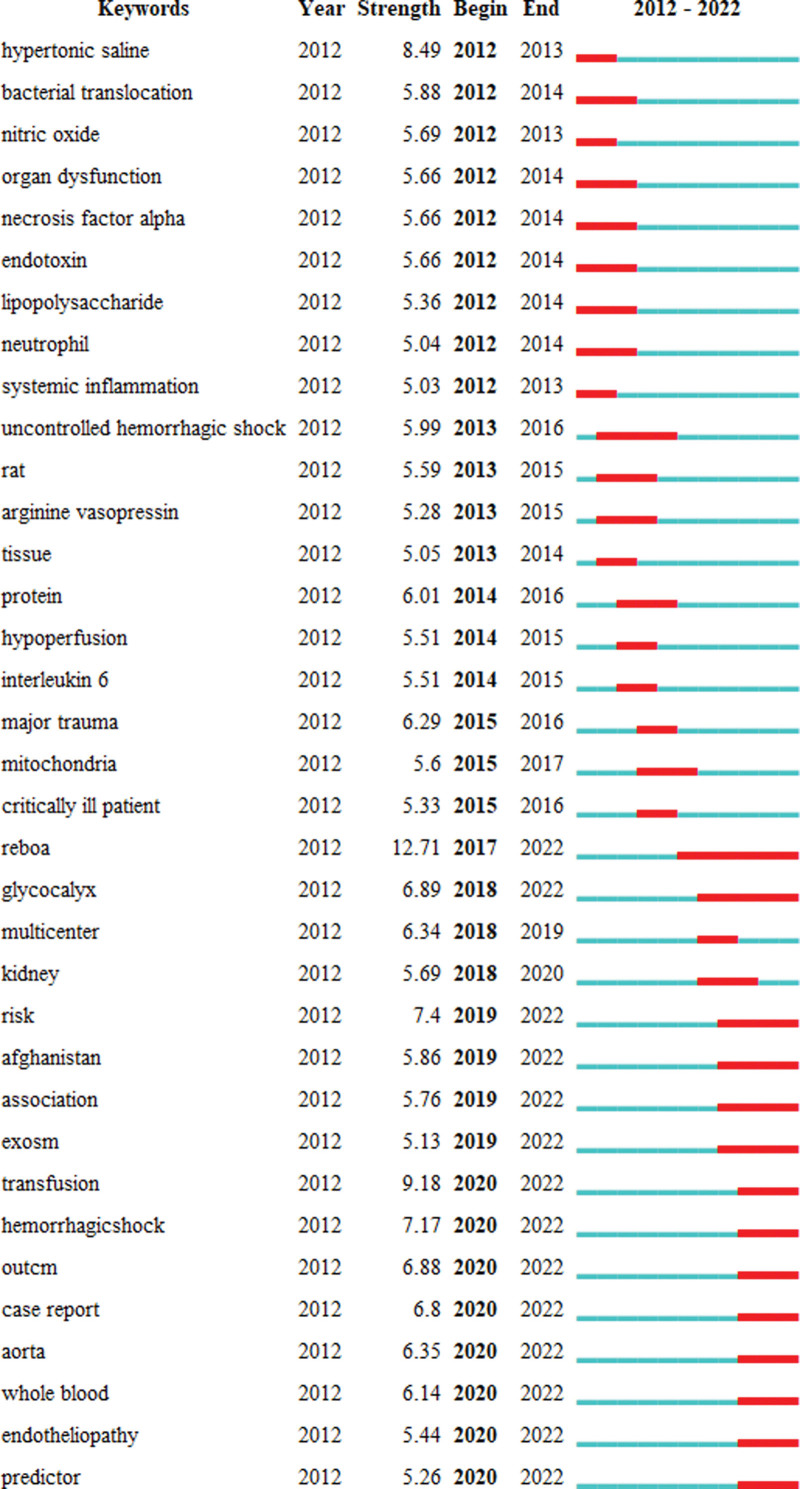
Keyword bursts are frequently cited over a period of time.[21] As shown in Figure 9, “reboa” had the strongest bursts (strength = 12.71), while “exsome,” “glycocalyx,” “endotheliopathy,” “predictor,” and “whole blood” were recently bursting keywords, indicating research trends and hot topics.
Figure 9.
Top 35 keywords with citation burst (sorted by the year in which the burst started).
4. Discussion
4.1. General information
This study was a visual bibliometric analysis of trauma-related hemorrhagic shock. A total of 558 authors from 441 institutions in 80 countries had published 3116 papers in 200 academic journals regarding trauma-related hemorrhagic shock research between 2012 and 2022.
We ranked the 10 most productive authors and co-cited authors in Table 1 and Figure 3. Ernest E. Moore from the Denver Health Medical Center was the most productive author. His research focused on trauma-induced coagulopathy,[22,23] trauma hemostasis,[24] multiple organ failure,[25,26] and prehospital transfusion in hemorrhagic shock.[27] Additionally, he published approximately 10 related articles per year since 2012. John B. Holcomb from the University of Alabama at Birmingham had the most co-citations, with the most cited article being a randomized clinical trial published in JAMA in 2015.[16] Figure 3A shows that the researchers are scattered with relatively few connections, indicating a lack of academic exchange between researchers from different countries.
The spatial distribution map of countries/regions and institutions (Table 2 and Fig. 4) shows that the USA, China, and Germany yielded the most published studies on traumatic hemorrhagic shock. The US has the highest betweenness centrality (0.36), indicating that it plays a key role in international cooperation networks. The University of Pittsburgh published the most papers. Notably, the 10 most productive institutions were all from the US, indicating its leading role in this field of research.
As shown in Table 3, the Journal of Trauma and Acute Care Surgery published >400 articles on trauma-related hemorrhagic shock. Among the top 10 co-cited journals, 6 were in the Q1/2 JCR division, with the highest impact factor of 176.079. The results indicate that this field of research is extremely important and is currently a hotspot.
4.2. Research hotspots and emerging topics
We aimed to objectively summarize the hotspots and emerging trends of research through an analysis of reference clusters and bursts (Fig. 5), timeline views (Fig. 6), keyword co-occurrences (Table 5 and Fig. 7), keyword timeline views, and bursts (Figs. 8 and 9). As indicated in Figures 5 and 6, resuscitative endovascular balloon occlusion of the aorta (REBOA) and whole blood are the primary topics in this field of research.
Over the past decade, REBOA has emerged as a technique to control life-threatening hemorrhaging[28] and has become increasingly common in civilian trauma and acute care settings.[29] It acts as a temporizing measure to reduce noncompressible abdominal and pelvic hemorrhaging and buys time for definitive surgical and/or endovascular management.[30] More recent studies have shown that rapid in-hospital intervention is often insufficient to compensate for severe exsanguination and hypovolemia that occurs before emergency department presentation.[31] Therefore, prehospital REBOA could be a feasible intervention for a significant portion of severely ill patients in a civilian setting; however, the evidence is limited.[28] Partial REBOA is currently discussed in preclinical studies,[29] but has not yet been fully validated.[32]
Whole blood is a desirable fluid for patients with traumatic hemorrhagic shock.[33–35] It has the advantage of providing red blood cells, plasma, and platelets together in a unit, which simplifies and speeds the process of resuscitation, particularly in austere environments.[36] Shea et al[37] have reported that the use of low-titer group O whole blood is independently associated with improved survival compared to component therapy in adults with severe traumatic hemorrhage. Additional studies are underway to define the optimal way to utilize low-titer type O whole blood in both prehospital and trauma center resuscitation of bleeding patients.[38]
As shown in the keyword analysis, besides “reboa” and “whole blood,” “exsome,” “glycocalyx,” “endotheliopathy,” and “predictor,” are also burst keywords, indicating current and future research trends.
Stem cells possess a remarkable potential for developing new cell-based treatments for hemorrhagic shock, and mesenchymal stem cell-derived exosomes are the focus of therapeutic strategies in hemorrhagic shock models.[39] Exosomes have shown protective effects in hemorrhagic shock in swine models.[40,41] Stem cell-related therapeutic strategies represent a potential opportunity for treating hemorrhagic shock-induced second injuries.[39]
The endothelial glycocalyx is a thin sugar-based lining on the apical surface of endothelial cells.[42] Traumatic hemorrhagic shock, sepsis, and other inflammatory processes lead to endotheliopathy through the systemic shedding of the protective glycocalyx barrier.[5,43] Avoiding further damage to the endothelial glycocalyx is an important principle in clinical practice.[42] Early transfusion of plasma and balanced transfusion have been shown to restore the endothelial glycocalyx.[44] Early tranexamic acid administration[45] and restrictive resuscitation[46] have also shown protective effects against glycocalyx degradation in vitro.
Predictors for outcomes in trauma-related hemorrhagic shock have recently been discussed in the research field. For example, Huh et al[47] compared admission lactate and base deficit, which reflect early hemorrhagic shock, as outcome predictors of pediatric trauma. One review reported that hypocalcemia could potentially be used as an independent predictor of multiple transfusions in trauma and hemostatic resuscitation.[48] Jávor et al[49] denied the predictive value of tachycardia for mortality in trauma-related hemorrhagic shock. Other predictors include age,[50] shock index,[51,52] end-tidal CO2.[53]
4.3. Limitations
This study has a few limitations. First, we only extracted articles from the Web of Science database; PubMed, Google Scholar, Scopus, and other databases were not included. Second, the language was restricted to English; a linguistic bias may exist. Third, this study only included articles published between 2012 and 2022. With the recent efforts of researchers and the continuous updating of the literature, the findings of this study may differ from more current studies.
5. Conclusion
With the help of CiteSpace and VOSviewer, this study provides a deeper understanding of the research landscape, frontier hotspots, and future trends in trauma-related hemorrhagic shock based on articles published during the last decade. The results show that “reboa,” “whole blood,” “exsome,” “glycocalyx,” “endotheliopathy,” and “predictor” will be the highlights of future research. This study provides important clues for researchers to understand the knowledge domain and the frontiers of this field of study.
Acknowledgments
We are grateful to the professional editors at Editage, who provided us with excellent assistance in the production of this manuscript.
Author contributions
Conceptualization: Tianbing Wang.
Data curation: Zhe Du, Tianbing Wang.
Investigation: Zhe Du.
Methodology: Zhe Du.
Software: Zhe Du.
Visualization: Zhe Du.
Writing – original draft: Zhe Du.
Writing – review & editing: Tianbing Wang.
Abbreviations:
- JCR
- journal citation reports
- REBOA
- resuscitative endovascular balloon occlusion of the aorta
This study was supported by Peking University People’s Hospital Scientific Research Development Funds (Grant/Award Number: RDJP2022-06).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
How to cite this article: Du Z, Wang T. A bibliometric analysis of publications on trauma-related hemorrhagic shock from 2012 to 2022: Research landscape and future trends. Medicine 2023;102:20(e33814).
References
- [1].Rosenkrantz L, Schuurman N, Hameed M. Trauma registry implementation and operation in low and middle income countries: a scoping review. Glob Public Health. 2019;14:1884–97. [DOI] [PubMed] [Google Scholar]
- [2].Kornblith LZ, Moore HB, Cohen MJ. Trauma-induced coagulopathy: the past, present, and future. J Thromb Haemost. 2019;17:852–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].National Medicine Library. Available at: https://www.ncbi.nlm.nih.gov/mesh/68012771 [accessed December 5, 2022].
- [4].Kuo K, Palmer L. Pathophysiology of hemorrhagic shock. J Vet Emerg Crit Care (San Antonio). 2022;32:22–31. [DOI] [PubMed] [Google Scholar]
- [5].Cannon JW. Hemorrhagic shock. N Engl J Med. 2018;378:370–9. [DOI] [PubMed] [Google Scholar]
- [6].Velez DR. The history of hemorrhagic shock and damage control resuscitation. Am Surg. 2022;88:2656–9. [DOI] [PubMed] [Google Scholar]
- [7].Lu C, Qi H, Xu H, et al. Global research trends of steroid-induced osteonecrosis of the femoral head: a 30-year bibliometric analysis. Front Endocrinol (Lausanne). 2022;13:1027603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Yin H, Yang X, Peng L, et al. Trends of calcium silicate biomaterials in medical research and applications: a bibliometric analysis from 1990 to 2020. Front Pharmacol. 2022;13:991377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Fei X, Wang S, Li J, et al. Bibliometric analysis of research on Alzheimer’s disease and non-coding RNAs: opportunities and challenges. Front Aging Neurosci. 2022;14:1037068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Wang Y, Rao Y, Yin Y, et al. A bibliometric analysis of global trends in the research field of pharmaceutical care over the past 20 years. Front Public Health. 2022;10:980866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Liu D, Chen B, Li T, et al. Research hotspots and trends on acupuncture for neuropathic pain: a bibliometric analysis from 2002 to 2021. J Pain Res. 2022;15:3381–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Du Z, Wang Z, Guo F, et al. Dynamic structures and emerging trends in the management of major trauma: a bibliometric analysis of publications between 2012 and 2021. Front Public Health. 2022;10:1017817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Wang Q, Yang KL, Zhang Z, et al. Characterization of global research trends and prospects on single-cell sequencing technology: bibliometric analysis. J Med Internet Res. 2021;23:e25789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Chen Y, Tang C, Shen Z, et al. Bibliometric analysis of the global research development of bone metastases in prostate cancer: a 22-year study. Front Oncol. 2022;12:947445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Li JY, Yao RQ, Xie MY, et al. Publication trends of research on sepsis and programmed cell death during 2002-2022: a 20-year bibliometric analysis. Front Cell Infect Microbiol. 2022;12:999569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Holcomb JB, Tilley BC, Baraniuk S, et al. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. JAMA. 2015;313:471–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Shackelford SA, Del Junco DJ, Powell-Dunford N, et al. Association of prehospital blood product transfusion during medical evacuation of combat casualties in Afghanistan with acute and 30-day survival. JAMA. 2017;318:1581–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Sperry JL, Guyette FX, Brown JB, et al. Prehospital plasma during air medical transport in trauma patients at risk for hemorrhagic shock. N Engl J Med. 2018;379:315–26. [DOI] [PubMed] [Google Scholar]
- [19].Moore HB, Moore EE, Chapman MP, et al. Plasma-first resuscitation to treat haemorrhagic shock during emergency ground transportation in an urban area: a randomised trial. Lancet. 2018;392:283–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Spahn DR, Bouillon B, Cerny V, et al. The European guideline on management of major bleeding and coagulopathy following trauma: fifth edition. Crit Care. 2019;23:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Zhang J, Song L, Jia J, et al. Knowledge mapping of necroptosis from 2012 to 2021: a bibliometric analysis. Front Immunol. 2022;13:917155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Chapman MP, Moore EE, Moore HB, et al. Overwhelming tPA release, not PAI-1 degradation, is responsible for hyperfibrinolysis in severely injured trauma patients. J Trauma Acute Care Surg. 2016;80:16–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Wohlauer MV, Moore EE, Thomas S, et al. Early platelet dysfunction: an unrecognized role in the acute coagulopathy of trauma. J Am Coll Surg. 2012;214:739–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Jenkins DH, Rappold JF, Badloe JF, et al. Trauma hemostasis and oxygenation research position paper on remote damage control resuscitation: definitions, current practice, and knowledge gaps. Shock. 2014;41:3–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Minei JP, Cuschieri J, Sperry J, et al. The changing pattern and implications of multiple organ failure after blunt injury with hemorrhagic shock. Crit Care Med. 2012;40:1129–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Sauaia A, Moore EE, Johnson JL, et al. Temporal trends of postinjury multiple-organ failure: still resource intensive, morbid, and lethal. J Trauma Acute Care Surg. 2014;76:582–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Pusateri AE, Moore EE, Moore HB, et al. Association of prehospital plasma transfusion with survival in trauma patients with hemorrhagic shock when transport times are longer than 20 minutes: a post hoc analysis of the PAMPer and COMBAT clinical trials. JAMA Surg. 2020;155:e195085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Caicedo Y, Gallego LM, Clavijo HJ, et al. Resuscitative endovascular balloon occlusion of the aorta in civilian pre-hospital care: a systematic review of the literature. Eur J Med Res. 2022;27:202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Van Skike CE, Baer DG, Spalding MC, et al. Complete and partial resuscitative endovascular balloon occlusion of the aorta for hemorrhagic shock. J Vis Exp. 2022:183. [DOI] [PubMed] [Google Scholar]
- [30].Jamal L, Saini A, Quencer K, et al. Emerging approaches to pre-hospital hemorrhage control: a narrative review. Ann Transl Med. 2021;9:1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Broome JM, Ali A, Simpson JT, et al. Impact of time to emergency department resuscitative aortic occlusion after noncompressible torso hemorrhage. Shock. 2022;58:275–9. [DOI] [PubMed] [Google Scholar]
- [32].Heindl SE, Wiltshire DA, Vahora IS, et al. Partial versus complete resuscitative endovascular balloon occlusion of the aorta in exsanguinating trauma patients with non-compressible torso hemorrhage. Cureus. 2020;12:e8999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Naumann DN, Boulton AJ, Sandhu A, et al. Fresh whole blood from walking blood banks for patients with traumatic hemorrhagic shock: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2020;89:792–800. [DOI] [PubMed] [Google Scholar]
- [34].Fisher AD, Carius BM, Corley JB, et al. Conducting fresh whole blood transfusion training. J Trauma Acute Care Surg. 2019;87(1S Suppl 1):S184–90. [DOI] [PubMed] [Google Scholar]
- [35].Kronstedt S, Lee J, Millner D, et al. The role of whole blood transfusions in civilian trauma: a review of literature in military and civilian trauma. Cureus. 2022;14:e24263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Shackelford SA, Gurney JM, Taylor AL, et al. Joint trauma system, defense committee on trauma, and armed services blood program consensus statement on whole blood. Transfusion. 2021;61:S333–5. [DOI] [PubMed] [Google Scholar]
- [37].Shea SM, Staudt AM, Thomas KA, et al. The use of low-titer group O whole blood is independently associated with improved survival compared to component therapy in adults with severe traumatic hemorrhage. Transfusion. 2020;60:S2–9. [DOI] [PubMed] [Google Scholar]
- [38].McCoy CC, Brenner M, Duchesne J, et al. Back to the future: whole blood resuscitation of the severely injured trauma patient. Shock. 2021;56:9–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Huang Q, Gao S, Yao Y, et al. Innate immunity and immunotherapy for hemorrhagic shock. Front Immunol. 2022;13:918380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Williams AM, Dennahy IS, Bhatti UF, et al. Mesenchymal stem cell-derived exosomes provide neuroprotection and improve long-term neurologic outcomes in a swine model of traumatic brain injury and hemorrhagic shock. J Neurotrauma. 2019;36:54–60. [DOI] [PubMed] [Google Scholar]
- [41].Williams AM, Higgins GA, Bhatti UF, et al. Early treatment with exosomes following traumatic brain injury and hemorrhagic shock in a swine model promotes transcriptional changes associated with neuroprotection. J Trauma Acute Care Surg. 2020;89:536–43. [DOI] [PubMed] [Google Scholar]
- [42].Astapenko D, Benes J, Pouska J, et al. Endothelial glycocalyx in acute care surgery – what anaesthesiologists need to know for clinical practice. BMC Anesthesiol. 2019;19:238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Diebel LN, Liberati DM. Effect of tranexamic acid on endothelial von Willebrand Factor/ADAMTS-13 response to in vitro shock conditions. J Trauma Acute Care Surg. 2023;94:273–80. [DOI] [PubMed] [Google Scholar]
- [44].Watson JJ, Pati S, Schreiber MA. Plasma transfusion: history, current realities, and novel improvements. Shock. 2016;46:468–79. [DOI] [PubMed] [Google Scholar]
- [45].Carge M, Diebel LN, Liberati DM. The effect of tranexamic acid dosing regimen on trauma/hemorrhagic shock-related glycocalyx degradation and endothelial barrier permeability: an in vitro model. J Trauma Acute Care Surg. 2022;92:812–20. [DOI] [PubMed] [Google Scholar]
- [46].Chi Y, Jiang X, Chai J, et al. Protective effect of restrictive resuscitation on vascular endothelial glycocalyx in pigs with traumatic hemorrhagic shock. Ann Transl Med. 2022;10:177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Huh Y, Ko Y, Hwang K, et al. Admission lactate and base deficit in predicting outcomes of pediatric trauma. Shock. 2021;55:495–500. [DOI] [PubMed] [Google Scholar]
- [48].Kronstedt S, Roberts N, Ditzel R, et al. Hypocalcemia as a predictor of mortality and transfusion. A scoping review of hypocalcemia in trauma and hemostatic resuscitation. Transfusion. 2022;62:S158–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Javor P, Hanak L, Hegyi P, et al. Predictive value of tachycardia for mortality in trauma-related haemorrhagic shock: a systematic review and meta-regression. BMJ Open. 2022;12:e059271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Hwabejire JO, Nembhard CE, Oyetunji TA, et al. Age-related mortality in blunt traumatic hemorrhagic shock: the killers and the life savers. J Surg Res. 2017;213:199–206. [DOI] [PubMed] [Google Scholar]
- [51].Marenco CW, Lammers DT, Morte KR, et al. Shock index as a predictor of massive transfusion and emergency surgery on the modern battlefield. J Surg Res. 2020;256:112–8. [DOI] [PubMed] [Google Scholar]
- [52].Pariente Juste L, Koo Gomez M, Bonet Burguera A, et al. Prehospital and hospital shock indices as predictors of massive blood transfusion during the initial treatment of polytrauma patients. Emergencias. 2021;33:29–34. [PubMed] [Google Scholar]
- [53].Stone ME, Jr., Kalata S, Liveris A, et al. End-tidal CO2 on admission is associated with hemorrhagic shock and predicts the need for massive transfusion as defined by the critical administration threshold: a pilot study. Injury. 2017;48:51–7. [DOI] [PubMed] [Google Scholar]