Abstract
Background
Hip fractures are associated with a high risk of death; among those who survive a hip fracture, many experience substantial decreases in quality of life. A comprehensive understanding of the epidemiology and burden of hip fractures by country, age, gender, and sociodemographic factors would provide valuable information for healthcare policymaking and clinical practice. The Global Burden of Disease (GBD) study 2019 was a global-level study estimating the burden of 369 diseases and injuries in 204 countries and territories. An exploration and additional analysis of the GBD 2019 would provide a clearer picture of the incidence and burden of hip fractures.
Questions/purposes
Using data from the GBD 2019, we asked, (1) What are the global, regional, and national incidences of hip fractures, and how did they change over a recent 30-year span? (2) What is the global, regional, and national burden of hip fractures in terms of years lived with disability, and how did it change over that same period? (3) What is the leading cause of hip fractures? (4) How did the incidence and years lived with disability of patients with hip fractures change with age, gender, and sociodemographic factors?
Methods
This was a cross-sectional study. Participant data were obtained from the GBD 2019 (http://ghdx.healthdata.org/gbd-results-tool). The GBD study is managed by the WHO, coordinated by the Institute of Health Metrics and Evaluation, and funded by the Bill and Melinda Gates Foundation. It estimates the burden of disease and injury for 204 countries by age, gender, and sociodemographic factors, and can serve as a valuable reference for health policymaking. All estimates and their 95% uncertainty interval (UI) were produced using DisMod-MR 2.1, a Bayesian meta-regression tool in the GBD 2019. In this study, we directly pulled the age-standardized incidence rate and years lived with disability rate of hip fractures by location, age, gender, and cause from the GBD 2019. Based on these data, we analyzed the association between the incidence rate and latitude of each country. Then, we calculated the estimated annual percentage change to represent trends from 1990 to 2019. We also used the Spearman rank-order correlation analysis to determine the correlation between the incidence or burden of hip fractures and the sociodemographic index, a composite index of the income per capita, average years of educational attainment, and fertility rates in a country.
Results
Globally, hip fracture incidences were estimated to be 14.2 million (95% UI 11.1 to 18.1), and the associated years lived with disability were 2.9 million (95% UI 2.0 to 4.0) in 2019, with an incidence of 182 (95% UI 142 to 231) and 37 (95% UI 25 to 50) per 100,000, respectively. A strong, positive correlation was observed between the incidence rate and the latitude of each country (rho = 0.65; p < 0.001). From 1990 to 2019, the global incidence rate for both genders remained unchanged (estimated annual percentage change 0.01 [95% confidence interval -0.08 to 0.11]), but was slightly increased in men (estimated annual percentage change 0.11 [95% CI 0.01 to 0.2]). The years lived with disability rate decreased slightly (estimated annual percentage change 0.66 [95% CI -0.73 to -0.6]). These rates were standardized by age. Falls were the leading cause of hip fractures, accounting for 66% of all patients and 55% of the total years lived with disability. The incidence of hip fractures was tightly and positively correlated with the sociodemographic index (rho 0.624; p < 0.001), while the years lived with disability rate was slightly negatively correlated (rho -0.247; p < 0.001). Most hip fractures occurred in people older than 70 years, and women had higher incidence rate (189.7 [95% UI 144.2 to 247.2] versus 166.2 [95% UI 133.2 to 205.8] per 100,000) and years lived with disability (38.4 [95% UI 26.9 to 51.6] versus 33.7 [95% UI 23.1 to 45.5] per 100,000) than men.
Conclusion
Hip fractures are common, devastating to patients, and economically burdensome to healthcare systems globally, with falls being the leading cause. The age-standardized incidence rate has slightly increased in men. Many low-latitude countries have lower incidences, possibly because of prolonged sunlight exposure. Policies should be directed to promoting public health education about maintaining bone-protective lifestyles, enhancing the knowledge of osteoporosis management in young resident physicians and those in practice, increasing the awareness of osteoporosis screening and treatment in men, and developing more effective antiosteoporosis drugs for clinical use.
Level of Evidence
Level III, prognostic study.
Introduction
Hip fractures threaten people’s lives and wellbeing, and these injuries impose a major cost on healthcare systems worldwide [22]. The 1-year mortality rate from hip fracture exceeds 30% in some countries and has been estimated to increase by 2% per year [19]. More than 10% of patients are unable to recover to their prefracture functional status, and most will have residual disability or pain. Hip fractures occur in patients with a mean age of more than 80 years, and more than 80% of those patients are women [23]. Despite improvements in surgical treatments, functional outcomes generally have decreased, perhaps because of an aging population [38]. Additionally, 1-year mortality often exceeds 20%, even in high-income countries [30]. This is because the costs of treatment are high, reaching USD 14,000 per patient in the United States, according to one estimate [30]. Therefore, measures are needed to prevent hip fractures. A comprehensive understanding of the up-to-date incidence and burden of hip fractures by country, age, gender, and sociodemographic levels will help to increase public awareness and provide a reference for medical resource allocation and policymaking.
In 1990, the number of hip fractures worldwide was estimated to be 1.3 million [18]. In 2019, the incidence was estimated to be 14.2 million in a recent study using data from the Global Burden of Disease (GBD) Study 2019, and the age-standardized rate has increased by 0.4% each year to 182.5 per 100,000 individuals as of that time [16]. However, there is no detailed depiction of the regional and national incidence to help policymaking and healthcare practice. In addition, the burden of hip fractures has mainly been evaluated by mortality rate in outcome studies [20, 28], but this approach has shortcomings. Because patients with hip fractures may experience long-term loss of health and independence, and some are unable to return to work, simply using the mortality rate does not adequately reflect patients’ actual health and economic burden. A better method is to quantify the years lived with disability to evaluate this burden [1]. Using this method, the GBD 2019 estimated the global burden of hip fractures to be 2.94 million years lived with disability, with an age-standardized rate of 36.8 per 100,000 [16]. However, the years lived with disability and the trends in the past 30 years by country, age, and gender, which are more valuable to guide related efforts, were not detailed in that study. In addition, because the cost to treat hip fractures is much higher than that of other fragility fractures [32], it is more cost-effective to prevent hip fractures than to treat them. Knowing the major causes of hip fractures will contribute to more targeted measures. Finally, the outcome of a fracture is also affected by age, gender, and sociodemographic development levels. Exploring age and gender differences among patients with hip fractures will help to identify individuals who would benefit from additional attention and care. A previous study suggested that the incidence of hip fractures increases with sociodemographic development and reaches a plateau or decreases at a high level of development [2]. Nevertheless, there is still a lack of comprehensive data to analyze the impact of sociodemographic level on the incidence and burden of hip fractures. Revealing this impact will help to guide further policies about sociodemographic factors that are relevant to each country.
We therefore used data from the GBD 2019 and asked, (1) What are the global, regional, and national incidences of hip fractures, and how did they change over a recent 30-year span? (2) What is the global, regional, and national burden of hip fractures in terms of years lived with disability, and how did it change over that same period? (3) What is the leading cause of hip fractures? (4) How did the incidence and years lived with disability of patients with hip fractures change with age, gender, and sociodemographic factors?
Patients and Methods
Data Source
The data used in this cross-sectional secondary analysis were obtained from the GBD 2019 (http://ghdx.healthdata.org/gbd-results-tool). The GBD 2019 is the latest version of the GBD study rounds, which have been conducted since 1990. Funded by the Bill and Melinda Gates Foundation, the GBD studies were run by the WHO and coordinated by the Institute of Health Metrics and Evaluation. In the study, more than 7000 researchers in epidemiology, statistics, and other disciplines from more than 156 countries and territories participated in data collection and analysis. It is one of the most in-depth databases available; it provides timely updates on the global burden of disease. In the GBD 2019 study, the incidence and burden of hip fractures were estimated for 204 countries and territories by age, gender, and sociodemographic index.
Data Processing by the GBD and Additional Analysis in This Study
The GBD 2019 research team collected raw data from civil registration, vital statistics, hospital records, and household surveys in each country [15], providing reliable estimates about the burden of hip fractures. The raw data were then adjusted and smoothened before the final estimation, as described in detail elsewhere [14, 17]; likewise, our methods for estimating injury have been reported elsewhere [11]. Briefly, after data collection, the GBD researchers adjusted inconsistent disease coding with time and different coding methods among countries. Then, the data were split by age, gender, and year. DisMod-MR 2.1, a Bayesian meta-regression tool, was used to produce estimates of the incidence and years lived with disability of hip fractures for each country. The country data were then grouped into 21 GBD regions (Table 1) and were further aggregated to produce global estimates.
Table 1.
The incidence, prevalence, and YLD of hip fractures in 2019 and the estimated annual percentage change from 1990 to 2019 in 21 regionsa
| Region | Incidence number in 1990 (× 1000) | Incidence number in 2019 (× 1000) | ASIR per 100,000 in 2019 | EAPC of ASIR from 1990 to 2019 | YLD number in 1990 (× 1000) | YLD number in 2019 (× 1000) | ASYR per 100,000 in 2019 | EAPC of ASYR from 1990 to 2019 |
| Global | 7393 (5916 to 9261) | 14,244 (11,095 to 18,064) | 182 (142 to 231) | 0.01 (-0.08 to 0.11) | 1817 (1244 to 2484) | 2936 (2030 to 3955) | 37 (25 to 50) | -0.66 (-0.67 to -0.52) |
| Global women | 3923 (3068 to 4952) | 8136 (6184 to 10619) | 190 (144 to 247) | 0.04 (-0.06 to 0.15) | 957 (666 to 1301) | 1291 (885 to 1745) | 38 (27 to 52) | -0.60 (-0.73 to -0.6) |
| Global men | 3470 (2803 to 4300) | 6108 (4916 to 7531) | 166 (133 to 206) | 0.11 (0.01 to 0.2) | 860 (585 to 1197) | 1645 (1150 to 2195) | 34 (23 to 45) | -0.68 (-0.75 to -0.62) |
| East Asia | 644 (469 to 865) | 2087 (1491 to 2831) | 116 (83 to 158) | 0.98 (0.54 to 1.43) | 154 (107 to 208) | 244 (161 to 349) | 13 (8 to 19) | -1.75 (-2.26 to -1.23) |
| Southeast Asia | 341 (271 to 433) | 639 (511 to 792) | 109 (86 to 136) | 0.04 (-0.22 to 0.31) | 120 (80 to 179) | 170 (119 to 230) | 28 (20 to 37) | -1.21 (-1.27 to -1.14) |
| Oceania | 3 (3 to 4) | 9 (7 to 11) | 115 (91 to 144) | 0.54 (0.08 to 1) | 1 (1 to 2) | 3 (2 to 4) | 39 (27 to 52) | 0.45 (0.34 to 0.57) |
| Central Asia | 79 (64 to 97) | 114 (92 to 140) | 132 (107 to 163) | -0.39 (-0.85 to 0.08) | 22 (16 to 30) | 26 (18 to 35) | 30 (21 to 41) | -1.16 (-1.23 to -1.08) |
| Central Europe | 489 (391 to 613) | 556 (439 to 701) | 318 (253 to 400) | -0.84 (-0.96 to -0.71) | 103 (73 to 137) | 77 (53 to 108) | 41 (28 to 58) | -2.31 (-2.49 to -2.13) |
| Eastern Europe | 730 (579 to 910) | 710 (561 to 891) | 259 (205 to 321) | -0.31 (-0.53 to -0.1) | 176 (125 to 234) | 112 (77 to 155) | 37 (26 to 51) | -2.2 (-2.5 to -1.89) |
| High-income Asia Pacific | 337 (266 to 427) | 674 (515 to 873) | 176 (137 to 222) | -0.21 (-0.26 to -0.16) | 48 (33 to 66) | 89 (60 to 127) | 22 (15 to 31) | -0.45 (-0.56 to -0.33) |
| Australia | 76 (60 to 95) | 205 (162 to 254) | 433 (346 to 537) | 0.88 (0.82 to 0.94) | 9 (6 to 12) | 25 (17 to 35) | 51 (35 to 72) | 1.08 (1.03 to 1.14) |
| Western Europe | 1450 (1128 to 1857) | 2441 (1877 to 3148) | 268 (209 to 342) | -0.24 (-0.31 to -0.17) | 186 (126 to 261) | 324 (222 to 458) | 35 (23 to 49) | -0.03 (-0.08 to 0.03) |
| Southern Latin America | 81 (65 to 101) | 138 (111 to 172) | 179 (144 to 224) | -0.05 (-0.1 to 0) | 20 (14 to 26) | 22 (16 to 31) | 28 (20 to 39) | -1.54 (-1.61 to -1.47) |
| High-income North America | 602 (446 to 791) | 1373 (991 to 1849) | 225 (165 to 300) | 0.87 (0.82 to 0.93) | 62 (41 to 91) | 139 (91 to 203) | 23 (15 to 33) | 0.82 (0.78 to 0.87) |
| Caribbean | 38 (31 to 46) | 94 (76 to 116) | 184 (149 to 227) | 1.28 (0.46 to 2.11) | 9 (7 to 12) | 22 (14 to 33) | 43 (28 to 66) | 1.25 (0.77 to 1.73) |
| Andean Latin America | 38 (28 to 56) | 63 (51 to 76) | 106 (87 to 129) | -0.18 (-0.4 to 0.05) | 12 (8 to 18) | 15 (11 to 20) | 26 (18 to 35) | -1.87 (-1.92 to -1.82) |
| Central Latin America | 154 (123 to 196) | 266 (214 to 337) | 111 (89 to 141) | -0.61 (-0.75 to -0.47) | 49 (32 to 77) | 53 (36 to 72) | 22 (15 to 30) | -2.09 (-2.25 to -1.94) |
| Tropical Latin America | 117 (88 to 154) | 252 (183 to 336) | 107 (78 to 144) | -0.06 (-0.14 to 0.02) | 26 (18 to 35) | 39 (27 to 53) | 16 (11 to 22) | -1.34 (-1.56 to -1.13) |
| North Africa and Middle East | 328 (257 to 443) | 752 (577 to 1044) | 148 (113 to 200) | 1.8 (1.33 to 2.27) | 152 (74 to 352) | 203 (114 to 370) | 38 (22 to 66) | -1.49 (-1.63 to -1.35) |
| South Asia | 1316 (1058 to 1637) | 3389 (2648 to 4254) | 242 (188 to 307) | 0.62 (0.52 to 0.72) | 521 (362 to 693) | 1122 (784 to 1486) | 80 (56 to 106) | -0.09 (-0.2 to 0.01) |
| Central Sub-Saharan Africa | 39 (27 to 62) | 69 (55 to 91) | 92 (74 to 113) | -1.53 (-2.89 to -0.15) | 19 (11 to 36) | 43 (24 to 83) | 53 (32 to 92) | -0.07 (-0.52 to 0.38) |
| Eastern Sub-Saharan Africa | 426 (191 to 996) | 198 (159 to 246) | 88 (71 to 107) | -2.14 (-3.11 to -1.16) | 88 (47 to 169) | 122 (69 to 232) | 50 (31 to 86) | -0.93 (-1.2 to -0.67) |
| Southern Sub-Saharan Africa | 21 (16 to 26) | 32 (25 to 40) | 49 (39 to 62) | -0.42 (-0.54 to -0.3) | 9 (6 to 12) | 11 (8 to 14) | 17 (12 to 23) | -1.16 (-1.37 to -0.94) |
| Western Sub-Saharan Africa | 85 (63 to 126) | 183 (140 to 242) | 74 (58 to 94) | 0.13 (-0.17 to 0.43) | 32 (22 to 43) | 74 (50 to 103) | 30 (21 to 40) | 0.1 (-0.03 to 0.22) |
The number of hip fractures and the YLDs in 1990 and 2019 for all regions were directly downloaded from the official website (https://vizhub.healthdata.org/gbd-results/) of the GBD study 2019. The ASIR and ASYR of hip fractures in 2019 for all regions were directly downloaded from the official website (https://vizhub.healthdata.org/gbd-results/) of the GBD study 2019. The EAPC of ASIR and ASYR were additional calculations in this study.
YLD = years lived with disability; ASIR = age-standardized incidence rate; EAPC = estimated annual percentage change; ASYR = age-standardized YLD rate.
Dissimilar to a previous study reporting the aggregated data of all fractures using the same database [16], we focused on hip fractures and pulled data on related global, regional, and national incidence and years lived with disability from the database. Cause-, age-, and gender-related data were also pulled from the database. We then analyzed the association between the age-standardized incidence rate and latitude of the capital of each country to examine the effects of sunlight exposure on hip fractures. We calculated and visualized, in heatmaps, the estimated annual percentage change in the incidence and disability for each country. We also analyzed the correlations between the incidence and years lived with disability and sociodemographic index to explore the impact of sociodemographic factors on the burden of hip fractures, and we calculated the proportion of each cause of hip fractures to determine the leading cause.
Definitions
The GBD 2019 study defined two kinds of injuries to explore causal relationships: the cause and nature of injury. The nature of injury is the consequence to the body, while the cause of injury is the external causes that occur to the body. For example, hip fractures are considered nature of injuries, and can be the result of many causes of injuries, such as falls, road injuries, mechanical forces, and others. One cause might lead to multiple injuries at different anatomic sites. To establish the one-to-one relationship between the two injuries, the GBD study developed a severity hierarchy for the nature of injury (Supplemental Table 1; http://links.lww.com/CORR/A968). Based on this hierarchy, the nature of injury is the one that is responsible for the largest burden and ranks at the top in the hierarchy of injuries. In this study, we directly pulled the cause-specific data of hip fractures from the GBD 2019, and we defined the leading cause of hip fractures as the one that accounted for the largest proportion of incidences and years lived with disability. Years lived with disability are the sum of years patients lived with health loss because of hip fractures. The sociodemographic index developed by the GBD study is a composite indicator reflecting the influence of background social and economic conditions on health outcomes in each location. The sociodemographic index relies on the method used by the United Nations to calculate the Human Development Index [15]. It is calculated from three covariates: the total fertility rate in people younger than 25 years, mean education years for those 15 years or older, and lag-distributed income per capita [10] (Supplemental Digital Content 1; http://links.lww.com/CORR/A969). The sociodemographic index ranges from 0 to 100, with 0 indicating that a location has the theoretical minimum level of sociodemographic development and the outcome for any health problem is expected to be the poorest. On the contrary, a sociodemographic index of 100 indicates that the theoretical level of sociodemographic development is the maximum and the outcome for any health problem is expected to be the best [15].
Primary and Secondary Study Outcomes
Our primary study goal was to delineate the incidence and disease burden of hip fractures at the global, regional, and national level in 2019, as well as the trends from 1990 to 2019. To achieve this, we obtained the numbers and age-standardized rates of incidence and years lived with disability of hip fractures from the GBD 2019. Then, we analyzed their trends from 1990 to 2019 by calculating the estimated annual percentage change.
The secondary outcomes of interest included the leading cause of hip fractures and how the incidence and burden of hip fractures changes with gender, age, and sociodemographic factors. We analyzed cause-specific data and calculated the percentages of each cause for the incidence and years lived with disability of patients with hip fractures. Then, we determined the global incidence and years lived with disability in 2019 and trends from 1990 to 2019 by age and gender. Finally, we used Spearman rank-order correlation analysis to determine associations between the incidence or burden of hip fractures and the sociodemographic index.
Statistical Analysis
In the GBD 2019, the estimates of the disease and injury incidence and burden were produced by DisMod-MR 2.1, a Bayesian meta-regression tool developed by the GBD research team. Each estimate was produced with a 95% uncertainty interval (UI). The 95% UI is different from the commonly used 95% confidence interval (CI) in frequentist estimation. It is analogous to the credible interval produced in Bayesian estimates and refers to an actual probability distribution around a true parameter value, which means that 95% of the probable values of the parameter would fall into the 95% UI [12]. By contrast, the 95% CI is used in testing the significance of the null hypothesis in frequentist analyses. It contains no distribution information and only indicates a range containing all the probable values that would not be rejected with a p value < 0.05. More details and differences between the 95% UI and 95% CI can be learned from a well-recognized article [24].
The absolute numbers of hip fracture incidences and years lived with disability, along with the age-standardized rates for each country and region, were directly pulled from the GBD 2019 study via its official website (https://vizhub.healthdata.org/gbd-results/). Age-, cause-, and gender-specific data and sociodemographic index were also obtained from the database. Based on these data, we first analyzed the association between the age-standardized rate and the latitude of each country to see whether the incidence is correlated to sunlight exposure in different locations. Then, we calculated the estimated annual percentage change and its 95% CI, which has been widely used in studies reporting the burden of other diseases or injuries using the GBD database [10, 26, 33]. The estimated annual percentage change was calculated based on a linear regression model as y = α + βx + ε, in which y indicates log10 (age-standardized rates), x represents the calendar year, and β is the coefficient of the regression model. If the estimated annual percentage change and the upper limit of the 95% CI were below zero, the trend was considered to be downward, and vice versa.
To determine the impact of sociodemographic factors on the incidence and burden of hip fractures, we used Spearman rank order (rho) correlation analysis to determine the correlation between the incidence of hip fractures and the sociodemographic index. In this analysis, we considered the correlation to be week if the absolute value of rho fell within 0.1 to 0.3, medium within 0.3 to 0.5, and strong if the rho was greater than 0.5 [6]. Statistical significance was determined as a p value less than 0.05. All additional data analyses were performed using R software (version 3.6.3).
Results
Incidence of Hip Fractures
There were estimated to be 14.2 million (95% UI 11.1 to 18.1 million) hip fractures worldwide in 2019 (Table 1), which increased by 92.7% compared with the estimate in 1990. The age-standardized incidence rate in 2019 was 182 per 100,000. From 1990 to 2019, the age-standardized incidence rate of both genders remained unchanged (estimated annual percentage change 0.01 [95% CI -0.08 to 0.11]), but slightly increased in men (estimated annual percentage change 0.11 [95% CI 0.01 to 0.2]). Regionally, Australia had the highest incidence rate (433 per 100,000 [95% UI 346 to 537 per 100,000]) in 2019, followed by Central, Western, and Eastern Europe. From 1990 to 2019, the incidence rate increased substantially in North Africa and the Middle East (estimated annual percentage change 1.8 [95% CI 1.33 to 2.27]), followed by the Caribbean and East Asia, while the highest decrease was seen in Eastern Sub-Saharan Africa (estimated annual percentage change -2.14 [95% CI -3.11 to -1.16]).
Nationally, countries in higher latitudes tended to have a higher incidence than those in tropical areas (Fig. 1A), while the trends from 1990 to 2019 were less affected by location (Fig. 1B). Spearman correlation analysis revealed a strong correlation between latitude and the age-standardized incidence rate of hip fractures (rho = 0.65; p < 0.001) (Fig. 2). Croatia (499 [95% UI 389 to 624] per 100,000) led the world in the incidence rate of hip fractures, followed by Slovenia, New Zealand, and Australia (Supplemental Table 2; http://links.lww.com/CORR/A970). The highest increase in age-standardized incidence rates was seen in Syria (estimated annual percentage change 9.2 [95% CI 5.9 to 2.6]). Increased rates were also observed in many countries with high sociodemographic indexes, such as the Netherlands (estimated annual percentage change 1.44 [95% CI 0.76 to 2.11]), Australia (estimated annual percentage change 0.97 [95% CI 0.91 to 1.03]), Canada (estimated annual percentage change 0.82 [95% CI 0.74 to 0.89]), and the United States (estimated annual percentage change 0.83 [95% CI 0.75 to 0.9]).
Fig. 1.
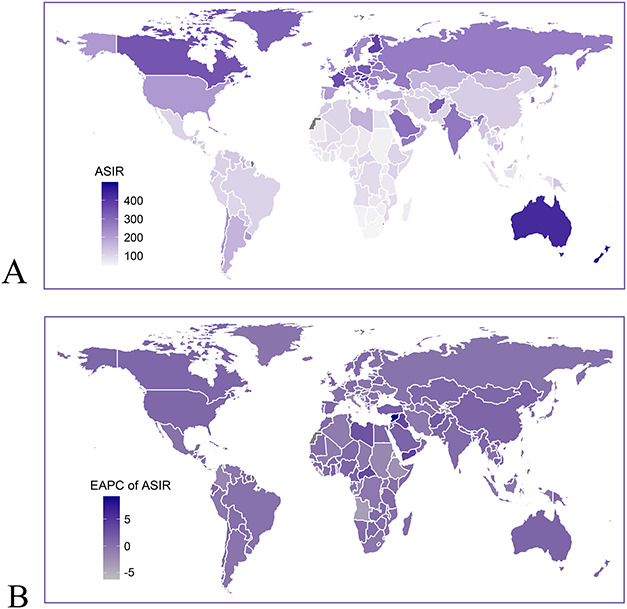
These maps show (A) the ASIR of hip fractures per 100,000 people in 2019 and (B) the EAPC from 1990 to 2019 in 204 countries and territories, for both genders. ASIR = age-standardized incidence rate; EAPC = estimated annual percentage change.
Fig. 2.
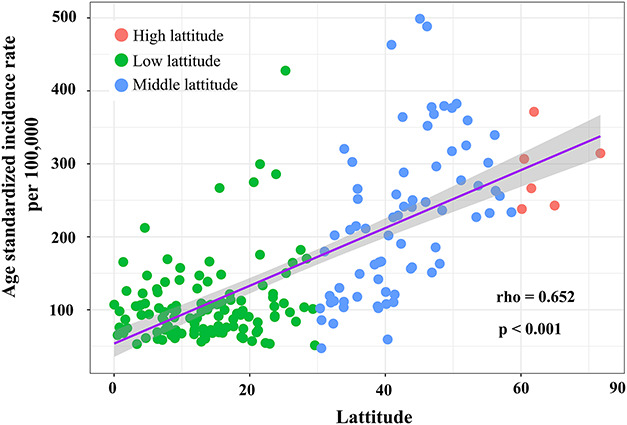
This figure shows the association between the age-standardized incidence rate of hip fractures and the latitudes of each country. We used the latitudes of the capital of each country. The latitudes were divided into three groups: low-latitude region, 0° to 30°; middle-latitude region, 30° to 60°; and high-latitude region, 60°to 90°. We analyzed the association of latitude with the age-standardized rate using Spearman rank-order correlation analysis.
Burden of Disease Attributable to Hip Fractures
Years lived with disability from hip fractures worldwide in 2019 were estimated to be 2.9 million (95% UI 2.0 to 4.0 million), increasing by 61.6% compared with that in 1990 (Table 1). The global age-standardized rate of years lived with disability decreased slightly during this period (estimated annual percentage change -0.66 [95% CI -0.73 to -0.6]). The highest decrease was seen in Central Europe (estimated annual percentage change -2.31 [95% CI -2.49 to -2.13]). Despite decreases in most regions, the Caribbean (estimated annual percentage change 1.25 [95% CI 0.77 to 1.73]), Australia (estimated annual percentage change 1.08 [95% CI 1.03 to 1.14]), and North America and Greenland (estimated annual percentage change 0.82 [95% CI 0.78 to 0.87]) had increased rates.
Nationally, the highest age-standardized rate of years lived with disability from hip fractures in 2019 was 208 per 100,000, observed in Afghanistan (Supplemental Table 2; http://links.lww.com/CORR/A970), followed by Burundi and Rwanda (Fig. 3A). Burundi (estimated annual percentage change 4.48 [95% CI 2.35 to 6.65]) also had higher increases in the years lived with disability rate than other countries (Fig. 3B). Many countries with a high sociodemographic index, including Australia, the United States, Canada, and most countries in Western Europe such as the Netherlands, United Kingdom, Spain, and Germany, also showed increased rates of years lived with disability from 1990 to 2019 (Supplemental Table 2; http://links.lww.com/CORR/A970).
Fig. 3.
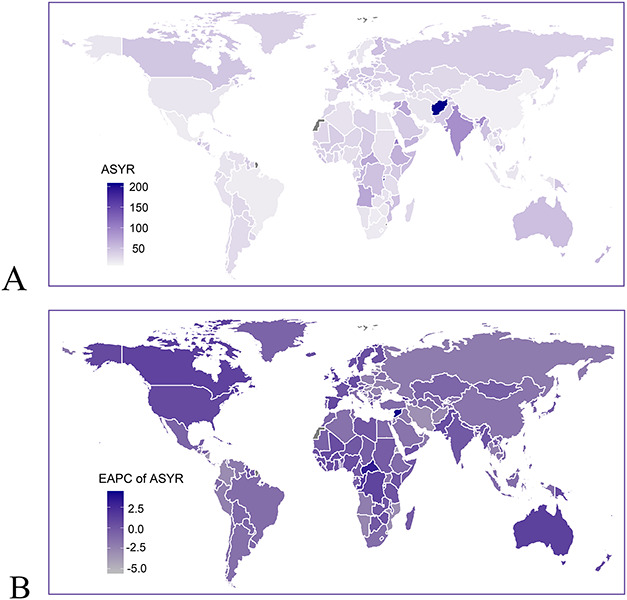
These maps show (A) the ASYR of hip fractures per 100,000 people in 2019 and (B) the EAPC from 1990 to 2019 in 204 countries and territories, for both genders. ASYR = age-standardized YLD rate; EAPC = estimated annual percentage change; YLD = years lived with disability. A color image accompanies the online version of this article.
Leading Causes of Hip Fractures
The leading cause of hip fractures was falls, followed by road injuries (including pedestrian, cyclist, and motor vehicle and other road injuries) and exposure to mechanical forces (Fig. 4A). Conflict and terrorism replaced mechanical forces as the third-leading cause of years lived with disability (Fig. 4B). Fall-related incidences and years lived with disability were estimated to be 9.85 million (95% UI 0.71 to 13.6 million) and 1.62 million (95% UI 1.12 to 2.21 million), respectively, accounting for 66% and 55% of the total incidences and years lived with disability, respectively (Fig. 4, A-B). Road injuries were the second-most common cause of hip fractures, resulting in 13% of total incidences and 24% of the total years lived with disability. Other causes were associated with 16% of the total incidence and 14% of the total years lived with disability. From 1990 to 2019, the incidence of hip fractures caused by falls gradually increased (Fig. 4C), while the years lived with disability decreased from 1990 to 2010 and then increased since 2010 (Fig. 4D).
Fig. 4.
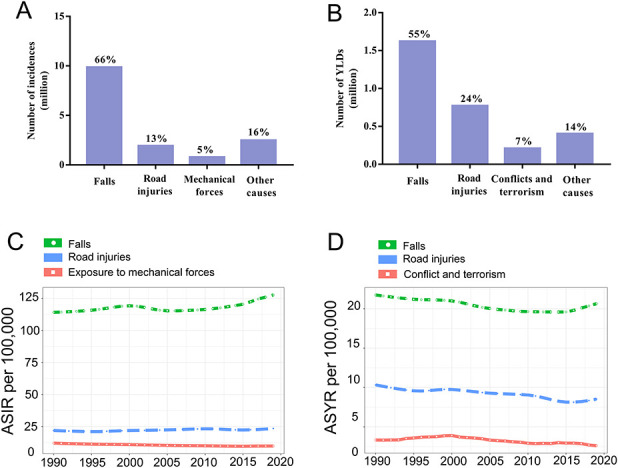
These graphs show the leading causes of the incidence and burden of hip fractures, including (A) the absolute incidence number of hip fractures, (B) the absolute number of years lived with disability of hip fractures, (C) the trends in ASIR associated with the top three causes of hip fractures, and (D) the trends in ASYR associated with the top three causes of hip fractures. ASIR = age-standardized incidence rate; ASYR = age-standardized YLD rate; YLD = years lived with disability. A color image accompanies the online version of this article.
Incidence and Disability of Hip Fractures by Sociodemographic Index, Gender, and Age
In 2019, countries with higher sociodemographic indexes tended to have higher incidence rates than did those with a low sociodemographic index (Fig. 5A). Spearman rank-order analysis revealed a strong, positive correlation between the age-standardized incidence rate (rho = 0.64; p < 0.001) and sociodemographic index (Fig. 5A), but a weak, negative correlation between years lived with disability and sociodemographic index (rho = -0.247; p < 0.001) (Fig. 5B). The estimated annual percentage change from 1990 to 2019 showed no correlation with the sociodemographic index (Fig. 5, C-D).
Fig. 5.
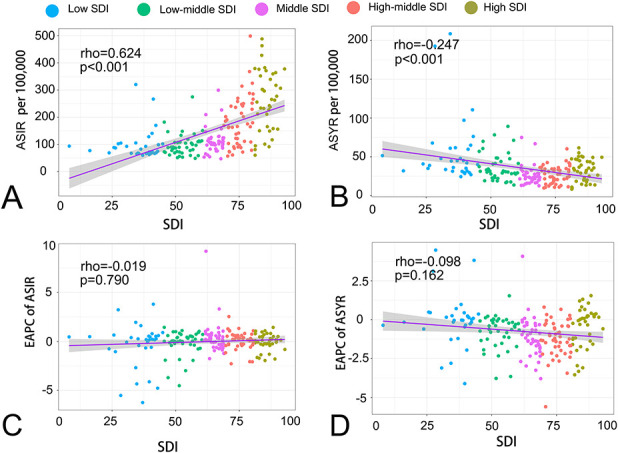
These graphs show the correlations between (A) the ASIR and SDI, (B) age-standardized YLD rate and SDI, (C) EAPC of the age-standardized incidence rate and SDI, and (D) EAPC of the age-standardized YLD rate and SDI. ASIR = age-standardized incidence rate; ASYR = age-standardized YLD rate; YLD = years lived with disability; EAPC = estimated annual percentage change; SDI = sociodemographic index.
Globally, the age-standardized incidence rate and years lived with disability rate in women reached 190 (95% UI 144 to 247) and 38 (95% UI 27 to 52) per 100,000, respectively, and in men reached 166 (95% UI 133 to 206) and 34 (95% UI 23 to 45) per 100,000, respectively. From 1990 to 2019, the age-standardized incidence rate and years lived with disability rate were consistently higher in women than that in men (Fig. 6A and 6B). Men and women worldwide had decreased years lived with disability rates during this time (Fig. 6B).
Fig. 6.
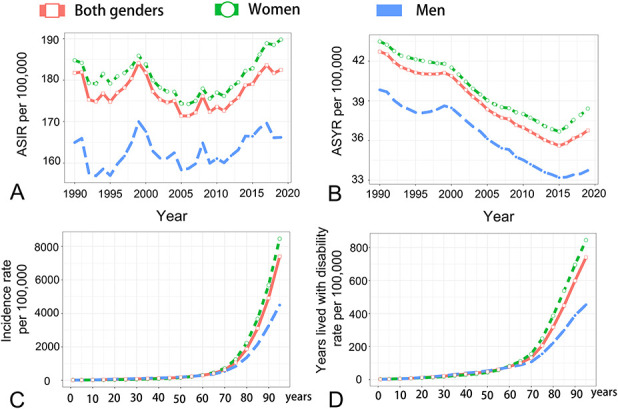
These graphs show the age-standardized incidence and YLD rate of hip fractures by age and gender, including (A) the trends in ASIR of hip fractures from 1990 to 2019 by gender, (B) the trends in ASYR of hip fractures from 1990 to 2019 by gender, (C) the incidence rate of hip fractures by age and gender, and (D) the YLD rate of hip fractures by age and gender. ASIR = age-standardized incidence rate; ASYR = age-standardized YLD rate; YLD = years lived with disability.
Among patients younger than 70 years, the incidence and years lived with disability rates worldwide were similar between women and men, both increasing slightly with age. Nevertheless, in people older than 70 years, the global incidence and years lived with disability rates increased steeply with age (Fig. 6C and 6D), and women showed higher rates of incidence and years lived with disability than men did. The differences between men and women also grew with age, suggesting that women were more likely to experience a disease burden related to hip fractures than men were, and the difference grew larger with advancing age.
Discussion
Hip fractures threaten people’s lives and wellbeing, and they represent a major cost to healthcare systems worldwide. Delineating the temporal and geographic trends in and burden of hip fractures, as well as exploring the leading causes, will help individuals, policymakers, donors, and health program organizers take better actions. Although a previous study reported the global incidence and years lived with disability of hip fractures using data from the GBD 2019 [16], that study did not describe the national and regional epidemiology and burden of hip fractures. It is also important to know the incidence and burden of hip fractures by age, year, gender, and sociodemographic index, which will provide more-valuable information for policymaking and healthcare practice. Using data from that same database, we found the global incidences and years lived with disability of hip fractures were substantial in 2019, with falls being the leading cause. Countries with a higher sociodemographic index tended to have higher incidence rates, but they had lower disability levels associated with hip fractures. Most hip fractures occurred in people older than 70 years, and women were more likely to experience them. Enhanced awareness of osteoporosis treatment and fall prevention, supported by data-driven healthcare policies (using findings from studies like ours), is important to reduce the future burden.
Limitations
The limitations of this work were similar to those in another GBD study [15]. First, because the raw data were obtained from civil registration, vital statistics, and hospital records, the completeness of these systems affects the accuracy of estimates. In some low-income countries or in those with active wars lacking adequate functioning healthcare systems, the raw data were sparse. Thus, the estimates depend largely on the modeling strategies used in the estimating tool, which decreases the accuracy of estimation compared with countries with robust healthcare systems, such as the United States, Canada, and those in Europe. To address this, the research team of the GBD 2019 study made their best efforts to reduce the impact of these issues by including more experts from different countries, updating the raw data for the GBD 2019 from all possible sources, and improving the estimating techniques [15], which make the data in the GBD 2019 more reliable.
Second, because hospital records were used to obtain raw data, the accuracy of estimates was affected by poor access to hospitals in some countries with low sociodemographic indices. In these countries, the high cost of surgical treatment delays or prevents the treatment of hip fractures for patients with limited financial means, which leads to an underestimate of the number and impact of hip fractures. This limitation has been shown to affect data from the most resource-constrained countries, more than it does in more-affluent countries [16], and the results should be interpretated accordingly.
Third, the GBD study covers a wide time period. From 1990 to 2019, the diagnostic and therapeutic methods, as well as a number of social and economic factors, have changed in most countries. Patients in recent years are more likely to seek medical care for hip fractures than those in earlier years. As a result, the incidence of hip fractures was more likely to be underreported in the 1990s than in recent years, which should be considered when interpreting the trends in hip fractures during this time.
Incidence of Hip Fractures
Because of population growth and aging, the estimated number of patients experiencing hip fractures in 2019 was substantial. It was twice as large in 2019 as it was in 1990. The age-standardized incidence rate of hip fractures was positively correlated to the sociodemographic index. High age-standardized incidence rates were seen in countries with a high sociodemographic index, such as Australia and Central, Western, and Eastern Europe. Understanding the reasons for the high incidence rates will help reduce the burden. A previous study on the trends of hip fractures worldwide attributed the high incidence of hip fractures to the process of urbanization [2]. However, that study lacked data from many regions with a low sociodemographic status, such as Asia and South America, and no evidence was provided to explain why urbanization might affect the incidence of hip fractures. In our study, we found the age-standardized incidence rate was strongly and positively correlated with countries’ latitudes. Many countries with low sociodemographic indices in tropical zones have longer sunlight exposure, and the incidence rates in these countries were lower than those with high sociodemographic indices in high latitudes, suggesting that prolonged exposure to sunlight contributes to enhanced bone quality and reduced hip fractures. In addition, countries in regions with high sociodemographic indices tend to have a higher prevalence of tobacco and alcohol consumption [13, 31], which are risk factors for hip fractures [43]. For individuals, health education or programs aimed at improving vitamin D and calcium intake, increasing daily sunlight exposure, and avoiding lifestyle risk factors such as alcohol drinking and smoking would help to reduce the incidence of hip fractures.
Burden of Disease Attributable to Hip Fractures
In terms of the health burden, the global age-standardized rate of years lived with disability in patients with hip fractures decreased between 1990 and 2019. However, the trends differed by country, with many showing increased trends, even in those with a high sociodemographic index. Notably, the age-standardized rate of years lived with disability was negatively correlated with the sociodemographic index, indicating that countries with a low sociodemographic index experienced greater disability because of hip fractures. This association with hip fractures is different from that of vertebral fractures, another typical fragility fracture. There is a positive correlation between the associated burden of disease and the sociodemographic index [11]. Such a difference can be explained by the higher medical cost of hip fractures. Because of the high severity and mortality, more than 95% of hip fractures receive surgical intervention, while for vertebral fractures, the hospitalization rate is only 10% [36]. In the United States, the cost of the overall management of hip fractures has been estimated as approximately USD 14,000 per patient, accounting for more than 70% of the total cost of osteoporotic fractures, which is much higher than that for vertebral fractures (6%) [3, 30]. In countries with a lower sociodemographic index, some patients will not be able to afford the total cost of surgical treatment, which can result in increased and prolonged disability. For example, poverty in Burundi has resulted in a much higher rate of years lived with disability because of hip fractures than in other countries. In these countries, increasing government health spending on hip fracture prevention and treatment will help to ensure adequate medical care for patients with this injury [40]. More importantly, although improved short-term outcomes have been achieved in several places in the past decades [7], hip fractures are associated with high mortality levels, even in many high-income countries [30]. It is essential (and more cost-effective) to focus on the treatment of osteoporosis to prevent hip fractures than to treat them. Policy measures may be taken to develop and promote more effective drugs. For example, denosumab is more effective to treat osteoporosis and prevent fragility fractures than bisphosphonates [27], but its use is limited by its higher cost [9]. Since 2021 in China, the cost of denosumab has been covered by the national medical insurance scheme, and the price has dramatically decreased (from approximately USD 800 to USD 100 per dose) because of policy efforts by the government [29]. The decreased cost has resulted in increased prescribing of the drug by physicians, which helps more patients benefit from it. Anabolic agents such as teriparatide and abaloparatide with antifracture efficacy may also be considered for wider use through policy efforts. Finally, conflict and terrorism ranked as the third-leading cause of the burden of hip fractures. This has resulted in substantial amounts of disability; the highest rate of years lived with disability in Afghanistan was caused by armed conflict.
Leading Causes of Hip Fractures
Falls are the leading cause of hip fractures. The incidence of hip fractures owing to falls has steadily increased year by year during the past 30 years, indicating that the prevention of falls should receive more attention. Many factors are associated with an increased risk of falls, including age, medication use, depression, cognitive impairment, and general frailty [25, 34, 41]. A recent study revealed people with sarcopenia are also at an increased risk of falls and fractures [42]. Measures to prevent falls should be individualized in communities, hospitals, and care facilities to fit the right population. Generally, exercise should be recommended in people without contraindications [5]. Screening for sarcopenia, vision loss, and mental disorders in older people, as well as withdrawal of psychotropic medications (when appropriate) that increase the risk of falls, are also effective measures. These efforts should be made by home caregivers, general practitioners, and staff in care facilities, and enhancing these caregivers’ knowledge about how to prevent falls would help reduce fall-related fractures [4, 5].
Incidence and Disability of Hip Fractures by Sociodemographic Index, Gender, and Age
The incidence and burden of hip fractures are higher in women than in men because there is an increased prevalence of osteoporosis in women after menopause. However, the age-standardized incidence rate of hip fractures has increased in men in the past 30 years. This may result from the general underemphasis of osteoporosis management in men [37]. A previous study revealed that men have higher bone mineral density than women do, but the attributable mortality rates are higher in men than in women once a fracture has occurred [10]. However, the treatment of osteoporosis is inadequate for the entire population (both men and women) in some countries. For example, despite an aging population, the annual prescription rate of antiosteoporotic drugs in the United Kingdom has remained unchanged since 2006 [39]. In the United States, the use of these drugs has even decreased since 2001 [35]. One important reason for the undertreatment of osteoporosis is insufficient knowledge among young resident physicians about screening for and treatment of this disease [8]. These reasons may collectively cause high incidence rates of hip fractures in countries with high sociodemographic indices. Thus, it would be worth taking steps to increase knowledge about osteoporosis among young resident physicians, enhance osteoporosis screening and treatment, and develop and disseminate guidelines for osteoporosis management in men to reduce the burden of hip fractures.
Conclusion
From 1990 to 2019, the absolute number of hip fractures has substantially increased, representing a major threat to people’s health and wellbeing and resulting in great burden to healthcare systems globally. Many countries with low sociodemographic indices in low-latitude regions have lower incidences, perhaps because of prolonged sunlight exposure, but the burden in those countries was still higher than in countries with a high sociodemographic index (likely because of the effects of poverty). Most hip fractures occurred in people older than 70 years, and women were more likely to experience them. To reduce the burden of hip fractures, one needs to begin with the perspective that it is more cost-effective to prevent fractures than to treat them, especially in countries that are more-severely resource-constrained. To achieve a reduced healthcare burden associated with this important injury, a multipronged approach would be needed. Bone-protective lifestyle choices, such as increasing sunlight exposure, supplementing vitamin D, reducing alcohol consumption, and avoiding tobacco use, should be recommended to patients. For young and less-experienced clinicians, increasing the awareness and knowledge of osteoporosis screening and treatment and receiving related clinical training will guarantee better care for patients [8, 21]. For policymakers, increasing budgets for hip fracture treatment, developing more effective antiosteoporosis drugs, and reducing their costs (as was recently done in China [29]) will help us address the future challenges associated with caring for patients with hip fractures.
Acknowledgment
We thank the epidemiologists and scientists who contributed their work to the GBD study.
Footnotes
This study was supported by the Fundamental Research Funds for the Central Universities (HUST: YCJJ202201022).
Each author certifies that there are no funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article related to the author or any immediate family members.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Ethical approval for this study was waived.
This work was performed at Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China.
The first three authors contributed equally to this study.
Contributor Information
Yimin Dong, Email: dongyimin@hust.edu.cn.
Yayun Zhang, Email: zhangyayun@hust.edu.cn.
Kehan Song, Email: kehansong@tjh.tjmu.edu.cn.
Honglei Kang, Email: kanng123@163.com.
Dawei Ye, Email: dy0711@gmail.com.
References
- 1.Ahmadi-Abhari S, Moayyeri A, Abolhassani F. Burden of hip fracture in Iran. Calcif Tissue Int. 2007;80:147-153. [DOI] [PubMed] [Google Scholar]
- 2.Ballane G, Cauley JA, Luckey MM, Fuleihan Gel H. Secular trends in hip fractures worldwide: opposing trends East versus West. J Bone Miner Res. 2014;29:1745-1755. [DOI] [PubMed] [Google Scholar]
- 3.Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465-475. [DOI] [PubMed] [Google Scholar]
- 4.Cheng P, Tan L, Ning P, et al. Comparative effectiveness of published interventions for elderly fall prevention: a systematic review and network meta-analysis. Int J Environ Res Public Health. 2018;15:498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Close JC. How can you prevent falls and subsequent fractures? Best Pract Res Clin Rheumatol. 2013;27:821-834. [DOI] [PubMed] [Google Scholar]
- 6.Cohen J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed. Erlbaum; 1988. [Google Scholar]
- 7.Cram P, Lix LM, Bohm E, et al. Hip fracture care in Manitoba, Canada and New York State, United States: an analysis of administrative data. CMAJ Open. 2019;7:E55-E62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crandall CJ, Chen LY, Rodriguez TD, et al. Knowledge and needs of resident physicians regarding osteoporosis: a nationwide survey of residents. JBMR Plus. 2021;5:e10524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Davis S, Simpson E, Hamilton J, et al. Denosumab, raloxifene, romosozumab and teriparatide to prevent osteoporotic fragility fractures: a systematic review and economic evaluation. Health Technol Assess. 2020;24:1-314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dong Y, Kang H, Peng R, et al. Global, regional, and national burden of low bone mineral density from 1990 to 2019: results from the Global Burden of Disease Study 2019. Front Endocrinol (Lausanne). 2022;13:870905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dong Y, Peng R, Kang H, et al. Global incidence, prevalence, and disability of vertebral fractures: a systematic analysis of the global burden of disease study 2019. Spine J. 2022;22:857-868. [DOI] [PubMed] [Google Scholar]
- 12.Feckler A, Low M, Zubrod JP, Bundschuh M. When significance becomes insignificant: effect sizes and their uncertainties in Bayesian and frequentist frameworks as an alternative approach when analyzing ecotoxicological data. Environ Toxicol Chem. 2018;37:1949-1955. [DOI] [PubMed] [Google Scholar]
- 13.GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2018;392:1015-1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.GBD 2016 Traumatic Brain Injury and Spinal Cord Injury Collaborators. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18:56-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204-1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.GBD 2019 Fracture Collaborators. Global, regional, and national burden of bone fractures in 204 countries and territories, 1990-2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet Healthy Longev. 2021;2:e580-e592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1223-1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int. 1997;7:407-413. [DOI] [PubMed] [Google Scholar]
- 19.Guzon-Illescas O, Perez Fernandez E, Crespi Villarias N, et al. Mortality after osteoporotic hip fracture: incidence, trends, and associated factors. J Orthop Surg Res. 2019;14:203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jennnison T, Yarlagadda R. A case-control study of 30-day mortality in periprosthetic hip fractures and hip fractures. Ann R Coll Surg Engl. 2020;102:229-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kanis JA, Cooper C, Rizzoli R, Reginster JY; Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporisis (ESCEO) and the Committee of Scientific Advistors and National Societies of the International Osteoporosis Foundation (IOF). European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2019;30:3-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Katsoulis M, Benetou V, Karapetyan T, et al. Excess mortality after hip fracture in elderly persons from Europe and the USA: the CHANCES project. J Intern Med. 2017;281:300-310. [DOI] [PubMed] [Google Scholar]
- 23.Keene GS, Parker MJ, Pryor GA. Mortality and morbidity after hip fractures. BMJ. 1993;307:1248-1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kruschke JK, Liddell TM. The Bayesian new statistics: nypothesis testing, estimation, meta-analysis, and power analysis from a Bayesian perspective. Psychon Bull Rev. 2018;25:178-206. [DOI] [PubMed] [Google Scholar]
- 25.Lan X, Li H, Wang Z, Chen Y. Frailty as a predictor of future falls in hospitalized patients: a systematic review and meta-analysis. Geriatr Nurs. 2020;41:69-74. [DOI] [PubMed] [Google Scholar]
- 26.Li X, Cao X, Guo M, Xie M, Liu X. Trends and risk factors of mortality and disability adjusted life years for chronic respiratory diseases from 1990 to 2017: systematic analysis for the Global Burden of Disease Study 2017. BMJ. 2020;368:m234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lyu H, Jundi B, Xu C, et al. Comparison of denosumab and bisphosphonates in patients with osteoporosis: a meta-analysis of randomized controlled trials. J Clin Endocrinol Metab. 2019;104:1753-1765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mattisson L, Bojan A, Enocson A. Epidemiology, treatment and mortality of trochanteric and subtrochanteric hip fractures: data from the Swedish fracture register. BMC Musculoskelet Disord. 2018;19:369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.National Healthcare Security Administration. Policies and regulations. 2020. Available at: http://www.nhsa.gov.cn/art/2020/12/28/art_37_4220.html. Accessed September 2, 2022.
- 30.Papanicolas I, Figueroa JF, Schoenfeld AJ, et al. Differences in health care spending and utilization among older frail adults in high-income countries: ICCONIC hip fracture persona. Health Serv Res. 2021;56:1335-1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Peacock A, Leung J, Larney S, et al. Global statistics on alcohol, tobacco and illicit drug use: 2017 status report. Addiction. 2018;113:1905-1926. [DOI] [PubMed] [Google Scholar]
- 32.Rajabi M, Ostovar A, Sari AA, et al. Direct costs of common osteoporotic fractures (hip, vertebral and forearm) in Iran. BMC Musculoskelet Disord. 2021;22:651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Safiri S, Kolahi AA, Hoy D, et al. Global, regional, and national burden of neck pain in the general population, 1990-2017: systematic analysis of the Global Burden of Disease Study 2017. BMJ. 2020;368:m791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Seppala LJ, Wermelink A, de Vries M, et al. Fall-risk-increasing drugs: a systematic review and meta-analysis: II. psychotropics. J Am Med Dir Assoc. 2018;19:371.e311-371 e317. [DOI] [PubMed] [Google Scholar]
- 35.Solomon DH, Johnston SS, Boytsov NN, McMorrow D, Lane JM, Krohn KD. Osteoporosis medication use after hip fracture in U.S. patients between 2002 and 2011. J Bone Miner Res. 2014;29:1929-1937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tarrant SM, Balogh ZJ. The global burden of surgical management of osteoporotic fractures. World J Surg. 2020;44:1009-1019. [DOI] [PubMed] [Google Scholar]
- 37.The Lancet Diabetes Endocrinology. Osteoporosis: overlooked in men for too long. Lancet Diabetes Endocrinol. 2021;9:1. [DOI] [PubMed] [Google Scholar]
- 38.Turesson E, Ivarsson K, Thorngren KG, Hommel A. Hip fractures - treatment and functional outcome. The development over 25 years. Injury. 2018;49:2209-2215. [DOI] [PubMed] [Google Scholar]
- 39.van der Velde RY, Wyers CE, Teesselink E, et al. Trends in oral anti-osteoporosis drug prescription in the United Kingdom between 1990 and 2012: variation by age, sex, geographic location and ethnicity. Bone. 2017;94:50-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wagstaff A, Neelsen S. A comprehensive assessment of universal health coverage in 111 countries: a retrospective observational study. Lancet Glob Health. 2020;8:e39-e49. [DOI] [PubMed] [Google Scholar]
- 41.Xu T, Clemson L, O'Loughlin K, Lannin NA, Dean C, Koh G. Risk factors for falls in community stroke survivors: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2018;99:563-573 e5. [DOI] [PubMed] [Google Scholar]
- 42.Yeung SSY, Reijnierse EM, Pham VK, et al. Sarcopenia and its association with falls and fractures in older adults: a systematic review and meta-analysis. J Cachexia Sarcopenia Muscle. 2019;10:485-500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang YW, Lu PP, Li YJ, et al. Prevalence, characteristics, and associated risk factors of the elderly with hip fractures: a cross-sectional analysis of NHANES 2005-2010. Clin Interv Aging. 2021;16:177-185. [DOI] [PMC free article] [PubMed] [Google Scholar]


