Abstract
Objectives:
To determine the rate of erectile dysfunction in male patients who have sustained an acetabular fracture with no previously identified urogenital injury.
Design:
Cross-sectional survey.
Setting:
Level 1 Trauma Center.
Patients/Participants:
All male patients treated for acetabular fracture without urogenital injury.
Intervention:
The International Index of Erectile Function (IIEF), a validated patient-reported outcome measure for male sexual function, was administered to all patients.
Main Outcome Measurements:
Patients were asked to complete the International Index of Erectile Function score for both preinjury and current sexual function, and the erectile function (EF) domain was used to quantify the degree of erectile dysfunction. Fractures were classified according the OTA/AO classification schema, fracture classification, injury severity score, race, and treatment details, including surgical approach were collected from the database.
Results:
Ninety-two men with acetabular fractures without previously diagnosed urogenital injury responded to the survey at a minimum of 12 months and an average of 43 ± 21 months postinjury. The mean age was 53 ± 15 years. 39.8% of patients developed moderate-to-severe erectile dysfunction after injury. The mean EF domain score decreased 5.02 ± 1.73 points, which is greater than the minimum clinically important difference of 4. Increased injury severity score and associated fracture pattern were predictive of decreased EF score.
Conclusion:
Patients with acetabular fractures have an increased rate of erectile dysfunction at intermediate-term follow-up. The orthopaedic trauma surgeon treating these injuries should be aware of this as a potential associated injury, ask their patients about their function, and make appropriate referrals.
Level of Evidence:
III.
Key Words: acetabulum, sexual dysfunction, neurologic dysfunction, erectile dysfunction, acetabular fracture
1. Introduction
The acetabulum anatomically makes up a part of the pelvic ring, though is usually thought of as a distinct structure in the minds of orthopaedic traumatologists. Acetabular fractures are difficult to treat, and they tend to have high rates of complications.1,2 Much of the previously published literature on complications in acetabular fracture surgery has focused on post-traumatic arthritis and the rate of conversion to arthroplasty, nerve injury, deep vein thrombosis, heterotopic ossification, or infection rates.2–4 Both pelvic ring injuries and acetabular fractures require a high amount of energy to disrupt the osseous anatomy in young patients. Sexual dysfunction is a common complication of high-energy pelvic ring injuries (erectile dysfunction).5–8 Although the energy required to sustain an acetabular fracture is similar, and the acetabulum makes up part of the pelvic ring, no study has reported on the incidence of sexual or erectile dysfunction specifically in the setting of acetabular fracture. The aim of this study was to evaluate the incidence of erectile dysfunction with a validated patient-reported outcome measure after acetabular fracture.
2. Materials and Methods
2.1. Study Design
After institutional review board approval, all patients with pelvis and acetabular fractures presenting to our medical center between January 1, 2012, and December 31, 2017, were identified using a prospectively collected trauma database. The data presented here are a subset of a larger study performed by the urology department on patients with injuries to the pelvic ring and acetabulum.9 The study exclusion criteria included spinal cord injured patients, patients diagnosed with lower urogenital tract injuries, patients discharged to jail, and patients with combined pelvic ring fracture and acetabular fracture. All other patients between the ages of 18 and 70 years were considered eligible for inclusion. Data collected from the registry included age at injury, race, primary insurance, injury severity score (ISS), and fracture pattern according to OTA/AO classification.10 Patients with acetabular fractures are typically treated with open reduction and internal fixation at this institution when any joint incongruity exists or instability is present. Positioning does not include the use of a center post in the groin for traction, so direct pressure is not applied to the perineum.
Each patient's chart was reviewed to further classify each fracture according to the Letournel classification for acetabular fractures and whether anterior or posterior (or both) surgical approaches were used to access the fracture for fixation. The Letournel fracture classification was simplified into elementary versus associated patterns.2
A multicomponent online survey was developed11 and sent to all eligible subjects as outlined in the inclusion and exclusion criteria between November and December of 2018. The full International Index of Erectile Function (IIEF) consists of 15 questions and was administered twice to patients both in a recall fashion, that is, asking them what their sexual function was before injury and what their current function was.12,13 The erectile function (EF) domain score was the main outcome instrument used in this study and is useful in determining the level of EF in male patients (Table 1).14,15 Minimum clinically important difference (MCID) value for the EF domain has been determined to be 4.14
TABLE 1.
Erectile Dysfunction Domain of IIEF and the Corresponding Severity of Erectile Dysfunction
| Severity of Erectile Dysfunction | EF Domain Score |
| Normal range, no erectile dysfunction | 26–30 |
| Mild erectile dysfunction | 22–25 |
| Mild-to-moderate erectile dysfunction | 17–21 |
| Moderate erectile dysfunction | 11–16 |
| Severe erectile dysfunction | <10 |
2.2. Statistics
Demographics were analyzed using means, standard deviations, and confidence intervals. T tests were used to compare the means for the EF domain scores for preinjury and postinjury states. Linear regression was used to analyze the effect of being older than 60 years on the postinjury EF domain. Linear regression was used to analyze possible predictors for a postinjury EF score. Age, ISS, OTA/AO fracture pattern type and group, and whether an anterior approach was used were used as predictor variables in the multivariate regression. A P value of 0.05 was used to determine statistical significance.
3. Results
A total of 1912 male patients were identified who sustained OTA/AO 61 and 62 fractures. One thousand five hundred fifty-four (81.3%) of these men met the inclusion criteria, of which 277 (17.8%) returned completed surveys. Of the 277 survey respondents, 93 (33.5%) had isolated acetabular fractures. One patient returned a questionnaire but did not respond to the IIEF questions. This patient was removed from this analysis leaving the total respondents to 92 (33.2%). For those patients who were excluded, 77.1% (n = 276) were for being outside the specified age range, 19.0% (n = 68) were excluded for previously diagnosed urologic injury, 15.6% (n = 56) for penetrating trauma, 3.6% (n = 13) for spinal cord injury, and 2.2% (n = 8) for incarceration. There were 17 patients with combined pelvic ring and acetabular injuries removed from the analysis. Thirty-six patients had an anterior approach to the acetabulum, 27 of which had a middle or medial window of the ilioinguinal approach developed.
The mean age of patients in this cohort was 51.4 ± 14.9 years, and the average ISS was 15 (95% confidence interval [CI], 12 to 17). The average follow-up was 42.3 months with minimum 12.5 months of follow-up from injury.
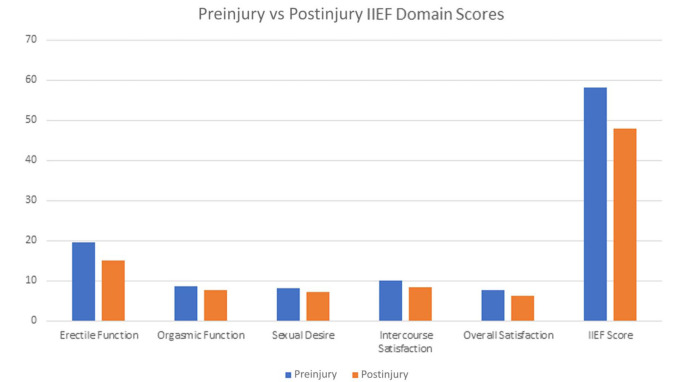
The complete IIEF score was significantly different from preinjury to postinjury (59.5 vs. 49.6; P < 0.001) (Fig. 1). The mean preinjury EF domain score was significantly different from the mean postinjury EF domain score (24.8 vs. 19.3; P < 0.001). The mean preinjury orgasmic function score was significantly different from the mean postinjury orgasmic function score (8.7 vs. 7.8; P = 0.026). The mean preinjury sexual desire score was significantly different from the mean postinjury sexual desire score (8.2 vs. 7.4; P = 0.019). The mean preinjury intercourse satisfaction score was significantly different than the mean postinjury intercourse satisfaction score (10.4 vs. 8.7; P = 0.008). The mean preinjury overall satisfaction score was significantly different than the postinjury overall satisfaction score (7.9 vs. 6.4; P < 0.001).
Figure 1.
Individual domain scores of the IIEF composite score compared for preinjury and postinjury.
The number of patients meeting criteria for mild erectile dysfunction and moderate-to-severe erectile dysfunction on the EF domain score before and after injury is shown in Table 2. Patients are split into younger than 60 years and older than 60 years to attempt to account for age-related differences in EF. Erectile dysfunction severity increased in at least 36 patients based on categories of EF domain (Table 3). The percentage of patients with erectile dysfunction by fracture pattern and the mean postinjury EF domain score are presented in Table 4. The mean EF score changed from 21.3 (95% CI, 19.6 to 22.9) preinjury to 19.2 (95% CI, 17.1 to 20.9) postinjury and was statistically significantly different (P < 0.001). The average magnitude of decrease of the EF score was a decrease of 5.02 points, and 34.1% of the respondents had experienced a decline in their score of at least the MCID of 4 points or greater (Table 5). Patients with associated patterns had a significantly lower postinjury EF score compared with patients who had elementary patterns (17.2 vs. 21.6, P = 0.03). No difference was detected in postinjury EF score between patients who had a middle or medial window of the ilioinguinal approach developed, as compared with a posterior approach (17.2 vs. 19.2, P = 0.459). No relationship was found between the time elapsed since injury to erectile dysfunction nor was a linear relationship between age and postinjury EF score found.
TABLE 2.
Erectile Dysfunction before and after Acetabular Fracture
| Preinjury Erectile Function Domain | Postinjury Erectile Function Domain | |||
| Younger than 60 yrs | ||||
| Average age (yrs) | 42.9 | |||
| n | 55 | 55 | ||
| No erectile dysfunction | 41 | 75% | 28 | 50% |
| Mild erectile dysfunction | 10 | 18% | 10 | 18% |
| Moderate-to-severe erectile dysfunction | 4 | 7% | 17 | 30% |
| Older than 60 yrs | ||||
| Average age (yrs) | 66.9 | |||
| n | 37 | 37 | ||
| No erectile dysfunction | 20 | 54% | 11 | 30% |
| Mild erectile dysfunction | 7 | 19% | 7 | 19% |
| Moderate-to-severe erectile dysfunction | 10 | 27% | 19 | 51% |
TABLE 3.
Cross-tabulation
| Preinjury ED | Postinjury ED | Total | |||||
| <10 | 10–16 | 17–21 | 22–25 | 26–30 | |||
| Severe ED | <10 | 5 | 0 | 0 | 0 | 0 | 5 |
| Moderate ED | 10–16 | 3 | 4 | 1 | 0 | 1 | 9 |
| Mild-to-moderate | 17–21 | 0 | 2 | 1 | 0 | 0 | 3 |
| Mild ED | 22–25 | 1 | 6 | 2 | 4 | 1 | 14 |
| No ED | 26–30 | 9 | 4 | 3 | 6 | 37 | 59 |
| Total | 18 | 16 | 7 | 10 | 39 | 90 | |
Bold numbers represent patients that had worse ED following injury.
TABLE 4.
Postinjury Erectile Function Domain Score in Patients With Acetabular Fractures
| Mean Postinjury Erectile Function Domain Score | % of Patients With Moderate-to-Severe Erectile Dysfunction (EF < 16) | |
| All patterns | 19.2 | 39.8% |
| OTA/AO A | 19.0 | 41.3% |
| OTA/AO B | 20.3 | 33.3% |
| OTA/AO C | 17.2 | 50.0% |
| Elementary patterns | 21.6 | 32.6% |
| Associated patterns | 17.1 | 46.0% |
| Anterior approach used | 16.8 | 50.0% |
TABLE 5.
Erectile Function Change in Patients With Acetabular Fractures
| Average Erectile Function Change* | % of Patients Meeting MCID Change for Erectile Function Score | n | |
| All patterns | −5.02 | 34.1% | 31/91 |
| OTA/AO A | −5.20 | 39.1% | 18/46 |
| OTA/AO B | −4.28 | 25.0% | 8/32 |
| OTA/AO C | −6.15 | 38.5% | 5/13 |
| Elementary patterns | −4.51 | 34.9% | 15/43 |
| Associated patterns | −5.48 | 33.3% | 16/48 |
| Anterior approach used | −6.85 | 41.2% | 14/34 |
Erectile function change is the change in the erectile function domain of the International Index of Erectile Function patient-reported outcome measure. A change of 4 point represents the minimum clinically important difference.
Linear regression was performed to evaluate for predictors of decreased EF domain score. Associated fracture pattern and high ISS adequately predicted a low postinjury EF score, but no other variables were predictive of low EF domain score (Table 6).
TABLE 6.
Regression Coefficients for Variables Included in Linear Regression
| Regression Coefficient | 95% Confidence Interval | P | ||
| Anterior approach used | −1.92 | −4.25 | 0.40 | 0.104 |
| ISS | −0.26 | −0.51 | 0.00 | 0.046 |
| Age | −0.01 | −0.15 | 0.13 | 0.863 |
| Elementary versus associated pattern | −4.34 | −8.48 | −0.19 | 0.042 |
| OTA/AO 62A1 | −6.95 | −27.15 | 13.25 | 0.495 |
| OTA/AO 62A2 | −15.85 | −36.93 | 5.22 | 0.138 |
| OTA/AO 62A3 | −14.22 | −34.47 | 6.03 | 0.166 |
| OTA/AO 62B1 | −6.92 | −27.38 | 13.53 | 0.502 |
| OTA/AO 62B2 | −16.00 | −37.59 | 5.59 | 0.144 |
| OTA/AO 62B3 | −9.43 | −29.83 | 10.98 | 0.360 |
| OTA/AO 62C1 | −14.22 | −35.00 | 6.56 | 0.177 |
| OTA/AO 62C2 | −12.25 | −34.29 | 9.79 | 0.272 |
| OTA/AO 62C3 | −2.00 | −29.88 | 25.88 | 0.886 |
4. Discussion
This study is the first data published to describe erectile dysfunction among a cross-sectional sample of patients who have sustained a fracture of the acetabulum. The acetabulum makes up part of the pelvic ring, and injuries to the acetabulum are often times disruptions of the pelvic ring itself.2 Acetabular fractures in young patients are typically high-energy injuries, similar to pelvic ring injuries. Recovery from pelvic ring injuries can be similar to that of acetabular fractures in that there are often times protracted recovery time, impaired ambulation, and prolonged pain issues.2–4,16–18 Sexual dysfunction in the form of erectile dysfunction in male patients has been shown to be a common occurrence after pelvic ring injury, although no study has reported on the specific complication of erectile dysfunction after acetabular fracture.5,7,9,11,19,20 The exact cause of sexual or erectile dysfunction after pelvic ring injury is likely multifactorial and poorly understood with vascular, corporeal, neurogenic, and psychogenic factors likely playing roles in its development.6
Previous studies on sexual and erectile dysfunction have focused on pelvic ring injuries with displacement or patients presenting with urogenital injuries along with their pelvic ring disruption.21–25 The acetabulum is not anatomically located near the urethra, which when damaged is often cited as a major cause for postinjury sexual dysfunction.21 Perhaps because of this anatomic disconnect, the relationship between acetabular fractures and sexual dysfunction after injury has not been studied. Patients with a combined pelvic ring injury were removed from the analysis because these injuries have been shown to be associated with sexual dysfunction in the past, and we wished to remove confounding variables.6,8,9
There are several studies in the orthopaedic literature examining sexual and erectile dysfunction among patients with pelvic ring injuries. Metze et al8 administered the IIEF questionnaire to patients who had sustained pelvic fracture at a mean of 29 months postinjury. They found that posterior ring disruptions and patients who sustained a distraction type injury in the anterior pelvis were at higher risk for long-term problems. Wright et al queried patients who had sustained a pelvic fracture whether they “experienced sexual dysfunction.” Their patients were identified from the Pennsylvania Trauma Outcomes Study and pelvic ring injuries identified through Abbreviated Injury Scale-90 codes. They found a rate of 21% among patients in their study and were unable to stratify based on the OTA/AO pattern.22 Harvey-Kelly et al examined a cohort of 110 patients, both male patients and female patients, and used sex-specific outcome measures to examine both quality of life and sexual function after pelvic ring injury. They found that urethral injury, pelvic fracture severity, and increased age were shown to be independent risk factors for sexual dysfunction.7 Vallier et al9 studied women who sustained pelvic ring injury and found a high rate of sexual dysfunction after injury. Specifically, dyspareunia was present in 91% of women with APC injuries, and surgical treatment of any pelvic ring injury was associated with dyspareunia at a rate of 74% compared with 35% of nonoperatively treated pelvic ring injuries. Their study was the most recent to look specifically at female sexual dysfunction after pelvic ring injury and had control groups of recruited patients from nonpelvis injury orthopaedic clinics as well as gynecology clinics. There have been reports of sexual and urinary dysfunction in female patients dating back to the 1990s. None of these studies have examined acetabular fractures as a risk factor for sexual dysfunction in either sex.26–28 Several authors in the trauma literature have examined the role of angioembolization in the development of sexual dysfunction and found that angioembolization likely does not play a decisive role in the development of sexual dysfunction.29,30 None of the above studies examined patients with acetabular fractures specifically, so we have to interpret these numbers with caution. Again, no study has examined sexual dysfunction in patients with acetabular fractures.
The IIEF score has several domains, each of which measure separate aspects of male sexual health.12 Fig. 1 breaks down the IIEF score into its constituent domains and what the mean responses preinjury and postinjury were for each. The IIEF score has been shortened for clinical use to the EF domain, and as displayed in our data, the major change in the complete IIEF score comes from the change in the EF domain of the complete score.15 The published MCID for the EF domain of the IIEF score is 4,14 and 34.1% of the patients in this study met this change. Patients can also be split into severity of erectile dysfunction based on their EF domain score (Table 1).15 This study showed that 39.8% of patients had a score of 16 or less in the EF domain of the IIEF score, indicating moderate-to-severe erectile dysfunction. On cross-tabulation examination (Table 3), there were 36 patients of 93 who decreased at least 1 category in the severity of their erectile dysfunction. Twenty-two participants found themselves with new moderate-to-severe erectile dysfunction after an injury to the acetabulum.
Our study shows that associated pattern acetabular fractures according to the Letournel and Judet classification system were more likely to have a lower EF domain score for EF. These patterns are by definition more complex with their osseous disruption, and all involve disruption of the pelvic ring either through the anterior column, posterior column, or both. The baseline rates of moderate-to-severe erectile dysfunction seen in the study population are comparable with baseline rates of erectile dysfunction in the general population,31 namely approximately 7% in male patients aged 45 years and 30% in male patients aged 60 years. Subsequently, the elevated rates of erectile dysfunction in both the younger and the older cohorts in this case can likely be attributed to their injuries (Table 2).
The strengths of the study include the length of follow-up, the use of a previously validated patient-reported outcome metric, and the fact that no study has reported on erectile dysfunction in patients sustaining acetabular fracture. We observed an erectile dysfunction rate of 39.8% as defined by the EF domain score of 16 or less at intermediate-term follow-up. No relationship between erectile dysfunction and time from injury was found. Associated pattern injuries were more likely to experience erectile dysfunction, although anterior approaches specifically were not. This study is likely underpowered to determine a relationship between approach and erectile dysfunction should a relationship exist. We focused specifically on the middle and medial windows of the ilioinguinal approach because these were believed to be most relevant to genitourinary anatomy. Overall, patients sustaining acetabular fractures had a high rate of erectile dysfunction as determined by the EF score outcome metric.
Several limitations are inherent in this article. First is that, these patients were retrospectively identified to be contacted, and our response rate was relatively low indicating an issue with selection bias. The long follow-up and recall bias may preferentially select for patients with problems, although this is unknown. Our study is underpowered to detect differences in erectile dysfunction between different specific fracture patterns or treatment characteristics, although we were able to show a difference between elementary and associated fracture patterns. A power calculation was not able to be performed due to the fact that there is no published rate of sexual dysfunction in patients with acetabular fracture in the literature. The patients were asked about their sexual function before injury, and this introduces recall bias, especially because so much time has elapsed since injury for many of these patients. Finally, sexual dysfunction is a multifactorial process, with many possible influencing factors. Post-traumatic stress disorder, head injury, job loss, depression, comorbidities such as peripheral vascular disease or diabetes, and relationship stress have all been shown to affect sexual function.19,32–35 We are unable to control for most of these factors.
There are treatment options available for these patients, although without discussing erectile dysfunction and sexual dysfunction with their orthopaedic surgeon, many patients may not be aware of these options. None of the patients in this study received a referral to a urologic specialist at the time of the injury or initial follow-up. Some of the patients included in the study did seek urologic care after they had been discharged from orthopaedic care months or years later. The topic of erectile dysfunction is sometimes uncomfortable for orthopaedic surgeons, but it is a necessary topic after pelvic or acetabular trauma. The urologic literature is replete with studies regarding the rate of sexual dysfunction after various orthopaedic injuries, though, how many orthopaedists are aware of these problems?36
In conclusion, erectile dysfunction is potentially a common complication of acetabular fracture in male patients. Orthopaedic surgeons who care for patients with acetabular fractures need to be aware of the potentially associated predilection for sexual dysfunction and make the appropriate referrals to urologists. In addition, this study provides a baseline to inform design of future prospective studies of sexual dysfunction and outcomes of patients with acetabular fracture.
Footnotes
The authors received no financial support for the research, authorship, and/or publication of this article.
The authors have no conflicts of interest to disclose.
Contributor Information
Iain S. Elliott, Email: elliott.iain@gmail.com.
Julie Agel, Email: bagel@uw.edu.
Max Coale, Email: mcoale@uw.edu.
Joseph T. Patterson, Email: Joseph.Patterson@med.usc.edu.
Reza Firoozabadi, Email: rezaf2@uw.edu.
Michael Githens, Email: mfg28@uw.edu.
Niels V. Johnsen, Email: Niels.v.johnsen@vumc.org.
REFERENCES
- 1.Matta JM, Dickson KF, Markovich GD. Surgical treatment of pelvic nonunions and malunions. Clin Orthop. 1996;329:199–206. [DOI] [PubMed] [Google Scholar]
- 2.Letournel E. Acetabulum fractures: classification and management. Clin Orthop. 1980;151:81–106. [PubMed] [Google Scholar]
- 3.Matta JM, Anderson LM, Epstein HC, et al. Fractures of the acetabulum: a retrospective analysis. Clin Orthop. 1986;205:230–240. [PubMed] [Google Scholar]
- 4.Verbeek DO, van der List JP, Tissue CM, et al. Long-term patient reported outcomes following acetabular fracture fixation. Injury. 2018;49:1131–1136. [DOI] [PubMed] [Google Scholar]
- 5.King J. Impotence after fractures of the pelvis. J Bone Joint Surg Am. 1975;57:1107–1109. [PubMed] [Google Scholar]
- 6.Harwood PJ, Grotz M, Eardley I, et al. Erectile dysfunction after fracture of the pelvis. J Bone Joint Surg Br. 2005;87:281–290. [DOI] [PubMed] [Google Scholar]
- 7.Harvey-Kelly KF, Kanakaris NK, Obakponovwe O, et al. Quality of life and sexual function after traumatic pelvic fracture. J Orthop Trauma. 2014;28:28–35. [DOI] [PubMed] [Google Scholar]
- 8.Metze M, Tiemann AH, Josten C. Male sexual dysfunction after pelvic fracture. J Trauma. 2007;63:394–401. [DOI] [PubMed] [Google Scholar]
- 9.Vallier HA, Cureton BA, Schubeck D. Pelvic ring injury is associated with sexual dysfunction in women. J Orthop Trauma. 2012;26:308–313. [DOI] [PubMed] [Google Scholar]
- 10.Meinberg EG, Agel J, Roberts CS, et al. Fracture and dislocation classification compendium—2018. J Orthop Trauma. 2018;32:S1. [DOI] [PubMed] [Google Scholar]
- 11.Johnsen NV, Lang J, Wessells H, et al. Barriers to care of sexual health concerns in men following traumatic pelvic fractures. J Sex Med. 2019;16:1557–1566. [DOI] [PubMed] [Google Scholar]
- 12.Rosen RC, Riley A, Wagner G, et al. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–830. [DOI] [PubMed] [Google Scholar]
- 13.Karakiewicz P, Shariat SF, Naderi A, et al. Reliability of remembered International Index of erectile function domain scores in men with localized prostate cancer. Urology. 2005;65:131–135. [DOI] [PubMed] [Google Scholar]
- 14.Rosen RC, Allen KR, Ni X, et al. Minimal clinically important differences in the erectile function domain of the International Index of Erectile Function Scale. Eur Urol. 2011;60:1010–1016. [DOI] [PubMed] [Google Scholar]
- 15.Cappelleri JC, Rosen RC, Smith MD, et al. Diagnostic evaluation of the erectile function domain of the international index of erectile function. Urology. 1999;54:346–351. [DOI] [PubMed] [Google Scholar]
- 16.Miranda MA, Riemer BL, Butterfield SL, et al. Pelvic ring injuries: a long term functional outcome study. Clin Orthop Relat Res. 1996;329:152–159. [PubMed] [Google Scholar]
- 17.Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78:1632–1645. [PubMed] [Google Scholar]
- 18.Tannast M, Najibi S, Matta JM. Two to twenty-year survivorship of the hip in 810 patients with operatively treated acetabular fractures: J Bone Joint Surg-Am. 2012;94:1559–1567. [DOI] [PubMed] [Google Scholar]
- 19.Sorensen MD, Wessells H, Rivara FP, et al. Prevalence and predictors of sexual dysfunction 12 months after major trauma: a national study. J Trauma. 2008;65:1045–1053. [DOI] [PubMed] [Google Scholar]
- 20.Bellabarba C, Stewart JD, Ricci WM, et al. Midline sagittal sacral fractures in anterior—posterior compression pelvic ring injuries. J Orthop Trauma. 2003;17:32–37. [DOI] [PubMed] [Google Scholar]
- 21.Chung PH, Gehring C, Firoozabadi R, et al. Risk stratification for erectile dysfunction after pelvic fracture urethral injuries. Urology. 2018;115:174–178. [DOI] [PubMed] [Google Scholar]
- 22.Wright JL, Nathens AB, Rivara FP, et al. Specific fracture configurations predict sexual and excretory dysfunction in men and women 1 year after pelvic fracture. J Urol. 2006;176:1540–1545. [DOI] [PubMed] [Google Scholar]
- 23.Koraitim MM. Predictors of erectile dysfunction post pelvic fracture urethral injuries: a multivariate analysis. Urology. 2013;81:1081–1085. [DOI] [PubMed] [Google Scholar]
- 24.Malavaud B, Mouzin M, Tricoire JL, et al. Evaluation of male sexual function after pelvic trauma by the International Index of Erectile Function. Urology. 2000;55:842–846. [DOI] [PubMed] [Google Scholar]
- 25.Copuroglu C, Yilmaz B, Yilmaz S, et al. Sexual dysfunction of male, after pelvic fracture. Eur J Trauma Emerg Surg. 2017;43:59–63. [DOI] [PubMed] [Google Scholar]
- 26.Copeland CE, Bosse MJ, McCarthy ML, et al. Effect of trauma and pelvic fracture on female genitourinary, sexual, and reproductive function. J Orthop Trauma. 1997;11:73–81. [DOI] [PubMed] [Google Scholar]
- 27.Baessler K, Bircher MD, Stanton SL. Pelvic floor dysfunction in women after pelvic trauma. BJOG. 2004;111:499–502. [DOI] [PubMed] [Google Scholar]
- 28.McCarthy ML, MacKenzie EJ, Bosse MJ, et al. Functional status following orthopedic trauma in young women. J Trauma. 1995;39:828–836. [DOI] [PubMed] [Google Scholar]
- 29.Ramirez JI, Velmahos GC, Best CR, et al. Male sexual function after bilateral internal iliac artery embolization for pelvic fracture. J Trauma Acute Care Surg. 2004;56:734–741. [DOI] [PubMed] [Google Scholar]
- 30.Goussous N, Sawyer MD, Wuersmer L-A, et al. Comparison of sexual function and quality of life after pelvic trauma with and without angioembolization. Burns Trauma. 2015;3:s41038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kessler A, Sollie S, Challacombe B, et al. The global prevalence of erectile dysfunction: a review. BJU Int. 2019;124:587–599. [DOI] [PubMed] [Google Scholar]
- 32.Yehuda R, Lehrner A, Rosenbaum TY. PTSD and sexual dysfunction in men and women. J Sex Med. 2015;12:1107–1119. [DOI] [PubMed] [Google Scholar]
- 33.Elliot ML, Biever LS. Head injury and sexual dysfunction. Brain Inj. 2009;10:703–717. [DOI] [PubMed] [Google Scholar]
- 34.Liu Q, Zhang Y, Wang J, et al. Erectile dysfunction and depression: a systematic review and meta-analysis. J Sex Med. 2018;15:1073–1082. [DOI] [PubMed] [Google Scholar]
- 35.Maiorino MI, Bellastella G, Esposito K. Diabetes and sexual dysfunction: current perspectives. Diabetes Metab Syndr Obes. 2014;7:95–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mallet R, Tricoire J-L, Rischmann P, et al. High prevalence of erectile dysfunction in young male patients after intramedullary femoral nailing. Urology. 2005;65:559–563. [DOI] [PubMed] [Google Scholar]