Abstract
Objective:
To draw lessons from Fiji regarding the challenges and opportunities for policy initiatives to restrict (i) food marketing to children and (ii) marketing of breast milk substitutes, to inform policy for the double burden of malnutrition.
Design:
Qualitative political economy analysis of two policy case studies.
Setting:
Fiji.
Participants:
Eleven key informants from relevant sectors, representing public health, economic and consumer interests.
Results:
This study used two policy initiatives as case studies to examine factors influencing decision-making: Marketing Controls (Foods for Infants and Young Children) Regulations 2010, amended in 2016 to remove guidelines and restrictions on marketing in the form of labelling, and the draft Advertising and Promotion of Unhealthy Foods and Non-Alcoholic Beverages to Children Regulation developed in 2014 but awaiting review by the Solicitor General’s Office. Factors identified included: a policy paradigm in which regulation of business activity contradicts economic policy goals; limited perception by key policy actors of links between nutrition and marketing of breast milk substitutes, foods and beverages; and a power imbalance between industry and public health stakeholders in policymaking. Regulation of marketing for health purposes sits within the health sector’s interest but not its legislative remit, while within the economic sector’s remit but not interest. Opportunities to strengthen restrictions on marketing to improve nutrition and health include reframing the policy issue, strategic advocacy and community engagement.
Conclusions:
Restricting marketing should be recognised by public health actors as a public health and an industry policy issue, to support strategic engagement with economic policy actors.
Keywords: Political economy, Food marketing, Malnutrition, Double burden, Fiji
Globally, multiple forms of malnutrition coexist in almost every country(1). Undernutrition, micronutrient deficiencies and diet-related noncommunicable diseases (NCD) are associated with significant personal, social and economic costs(2). Poor nutrition costs the global economy over $US3·5 trillion per year and is identified as a critical development challenge in the United Nations Sustainable Development Goals(3,4). In response to evidence that marketing of breast milk substitutes impacts on rates of breast-feeding(5), the World Health Organization (WHO) has recommended restrictions on marketing of breast milk substitutes since the 1980s to support action on child undernutrition(6). More recently, as evidence for the contribution of marketing to the rising consumption of unhealthy foods has mounted(7,8), the WHO has also recommended restrictions on marketing of foods and beverages to children for prevention of diet-related NCD(9). These initiatives were developed at different times and for different purposes but with new global attention on the ‘double burden of malnutrition’(10,11) – that is, the coexistence of undernutrition along with overweight/obesity and diet-related NCD – they have the shared aim of creating food environments that support good nutrition.
Marketing ‘refers to any form of commercial communication or message that is designed to, or has the effect of, increasing the recognition, appeal and/or consumption of particular products and services. It comprises anything that acts to advertise or otherwise promote a product or service’(9). There is significant evidence that marketing can be powerful and persuasive in influencing family decisions about child feeding, as well as children’s own decisions and their future brand loyalty(5,7,12). However, the majority of foods and beverages marketed to children are energy dense and nutrient poor (i.e. unhealthy)(12). Similarly, the marketing of breast milk substitutes has contributed to lower breast-feeding rates(5,13).
Despite this, there has been limited success globally in implementation of marketing restrictions to address the double burden of malnutrition. Regulation to reduce exposure of children to marketing of unhealthy foods and beverages has tended to be voluntary or led by industry(14,15) and has had little effect(16,17). Industry continues to market breast milk substitutes(18,19) as restrictions on marketing breast milk substitutes have often been weaker than global recommendations and poorly enforced(5,19). This limited success reflects broader challenges faced by low- and middle-income countries in operationalising strong nutrition policy measures, including the influence of powerful food industry interests on policymaking(20), and tension between global agendas for economic liberalisation and efforts to reduce availability of highly processed (often profitable) foods and beverages(21). Recent analysis indicates that these challenges are common across ‘all forms of malnutrition’(22), suggesting that integrated examination of policies to address undernutrition alongside diet-related NCD prevention can provide insights for addressing the complex double burden of malnutrition.
In this paper, we examine challenges faced by the Government of Fiji in seeking to implement strong restrictions on marketing to address the double burden of malnutrition. The Government of Fiji has demonstrated longstanding commitment to addressing nutrition as a policy priority, including taking action to reduce consumption of fatty meats and sugar-sweetened beverages, and developing community-level NCD prevention programmes(23–26). More recently, the Government of Fiji has sought to introduce two policy initiatives to restrict marketing, in order to improve nutrition, both of which reflect strong operationalisation of global best-practice recommendations: the Marketing Controls (Foods for Infants and Young Children) Regulations 2010, components of which were rolled back in 2016 (case study 1), and the draft Advertising and Promotion of Unhealthy Foods and Non-Alcoholic Beverages to Children Regulation (case study 2). However, these policies have faced challenges in implementation, even in a national context of long-term commitment to addressing the double burden of malnutrition. Understanding the opportunities and obstacles faced by the Government of Fiji and implementing partners can shed light on the political economy of restrictions on marketing and inform future policymaking. This paper extends previous research in Fiji that suggests corporate interests have sought to influence nutrition-related policymaking(20,27). In particular, industry in Fiji has been observed to exert corporate political influence through positioning themselves as part of the solution (including through sponsorship of major sporting events), emphasising the importance of their economic contribution and bringing in experts from overseas to consult regarding public health-related policies(20).
Methods
This study aimed to draw lessons from Fiji regarding the challenges and opportunities for policy initiatives that aim to restrict (i) food marketing to children and (ii) marketing of breast milk substitutes, by examining influences on the decision-making process in each case study. Case study and political economy analysis research methods informed our study design(28,29). Case study research methods were used as the basis for the study design; we drew on documentary and interview data to construct narrative cases of agenda setting, and policy development and change in both case studies, informed by policy theory. We drew on theories of political economy and priority setting to analyse the data regarding relevant influences on decision-making, particularly with respect to power, institutions, ideas and interest groups(30,31).
Data collection
Policy-relevant documents were identified through internet searches using the key words ‘marketing’, ‘Fiji’, ‘breast milk substitutes’, ‘children’, ‘health’ and ‘NCD prevention’. We also searched Hansard for the Parliament of the Republic of Fiji (http://www.parliament.gov.fj/hansard/) using the same terms and asked interviewees for relevant documentation. All relevant documents identified are cited below.
We identified initial potential interviewees based on the likelihood of their (professional) familiarity with the issue. We initially invited participation from: (1) Government Ministries with responsibility for the issue area (Ministries of Economy, Health, Communications, Trade and Commerce); (2) industry actors affected by policy decisions regarding marketing (e.g. manufacturers of processed food, advertising agencies) and (3) civil society actors with an interest in children’s nutrition and health (e.g. consumer representative organisations). We recruited initial interviewees through requests to relevant agencies and subsequently recruited additional interviewees through snowball sampling.
Interviews were semi-structured. We developed the interview schedule based on theories of the policy process(32), particularly Kingdon’s theory of agenda setting, which focuses on how problems are conceptualised and understood, policy solutions proposed and the role of politics and actors on a given policy decision (or non-decision)(33). The schedule included questions about: interviewees’ role and perspectives on diet-related NCD; opinions regarding the marketing of foods and breast milk substitutes in Fiji; the processes related to the two case study policies, with a focus on actor influence and politico-economic factors; and opinions regarding how policy action to restrict marketing for nutrition could be strengthened. The interview schedule was piloted with two retired experts in nutrition in Fiji, in December 2017, and the wording of questions and prompts refined for clarity.
We conducted eleven key informant interviews in Suva during 2018. Interviewees were policy actors familiar with the case study policies from within and outside government and represented public health (n 9), economic (n 1) and consumer (n 2) interests (Table 1). Interviews were conducted by three members of the research team and were 45–60 min in duration. Interviews were digitally audiorecorded (with participants’ informed consent) and transcribed verbatim. Ten potentially relevant policy actors declined to participate (or did not respond to the invitation), the largest proportion (n 5) representing industry interests.
Table 1.
Summary description of interviewees and non-participants*
| Type of organisation (n 11) | Main sectoral interest (n 11)† | Non-participants (n 10) |
|---|---|---|
| Multilateral (n 2) | Public health (n 9) | Economic/industry (n 5) |
| NGO (n 2) | Economic/industry (n 1) | Public health (n 3) (from multilateral and NGO) |
| National government (n 7) | Consumer interests (n 2) | Consumer interests (n 1) |
| Media (n 1) |
NGO, non-governmental organisations.
We describe interviewees and non-participants at a high level to avoid potential identification of actors in a small island context.
One respondent had both consumer and public health responsibilities.
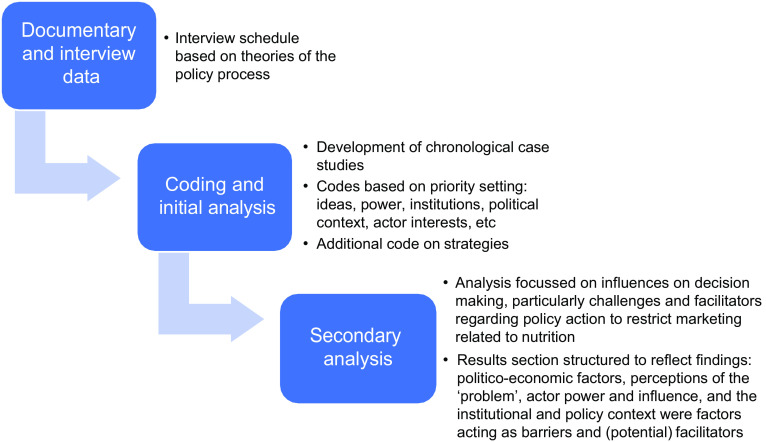
Analysis
Based on the document review, we constructed a case study summary for each policy, which informed the interviews and were subsequently refined using interview data. We used the NVivo software package to manage and organise interview data, to support the coding and thematic content analysis. In line with our primary research question – What influences decisions on restricting marketing of foods to (for) children? – our analysis had an explicit political economy focus, informed by policy theory. Predetermined codes were based on theoretical frameworks related to priority setting and political economy(29,33,34) and included: frames/ideas related to the problem and solution; power of actors and institutions; political context and institutions; role of policy entrepreneurs; issue characteristics and stakeholder interests. We also added a code related to strategies for strengthening policy action, given the project aimed to inform future policy action. Four interview transcripts were coded by five team members to identify a common approach. The lead researcher then coded and analysed the data, and the research team reviewed preliminary findings. We then conducted secondary analysis of these coded data, with an explicit focus on influences on decision-making, and particularly challenges and facilitators regarding policy action to restrict marketing. This secondary analysis indicated that politico-economic factors, perceptions of the ‘problem’, actor power and influence, and the institutional and policy context were critical dimensions of factors acting as barriers and (potential) facilitators, and the Results section is structured in line with these findings (Fig. 1). We do not present a detailed ‘within-case’ analysis for three reasons: the interviews involved discussion of both case studies and often the responses related to both; the nature of Fiji as a Small Island Developing State meant that a within-case analysis might be too identifying; and finally, we found the issues were very similar across both cases so presenting the findings separately for each would have been quite repetitive.
Fig. 1.
Flow chart of analysis
The study was funded through a School of Psychology and Public Health Engagement Income Growth Grant at LaTrobe University. Permission was granted by the College Human Ethics Sub-Committee, University Human Ethics Committee and College Health, Research and Ethics Committee of the Fiji National University and LaTrobe University, and through the Fiji National Health Research and Ethics Review Committee of the Fiji Ministry of Health and Medical Services.
Results
We first present detailed accounts of the two case studies and then address the core influences on decision-making apparent in these efforts to implement strong restrictions on marketing related to the double burden of malnutrition.
Overview of findings
The first case study was the 2016 decision by the Government of Fiji to roll back components of the Marketing Controls (Foods for Infants and Young Children) Regulations 2010 (case study 1). The second case study was the draft Advertising and Promotion of Unhealthy Foods and Non-Alcoholic Beverages to Children Regulation, which was initially developed in 2014 (case study 2). Analysis of these case studies suggests that challenges to the restriction of marketing of breast milk substitutes and of unhealthy foods and beverages to children included: (1) a prevailing policy paradigm in which regulation of business activity contradicts economic policy goals; (2) limited perception by key policy actors of links between nutrition and industry marketing of breast milk substitutes, foods and beverages; (3) power imbalances between industry and public health stakeholders in policymaking and (4) a policy environment in which regulation of marketing for health purposes sits within the health sector’s interest but not responsibility, while within the economic sector’s responsibility but not interest. Interviewees identified several opportunities to strengthen restrictions on marketing to improve nutrition and health, including reframing the policy issue, strategic advocacy and community engagement.
Policy case study 1: efforts to restrict marketing of breast milk substitutes in Fiji
Fiji was an early adopter of the International Code of Marketing of Breastmilk Substitutes and the first Pacific Island country to fully implement the Code in its laws(35). The Marketing Controls (Foods for Infants and Young Children) Regulations 2010 were introduced to ‘ensure safe and adequate nutrition for infants and young children by promoting and protecting breast-feeding and by regulating the marketing of designated products intended for use by infants and young children’(36). The regulations restrict the promotion and marketing of breast milk substitutes via images and text on the label, as well as the use of advertising, special displays, discounts, premiums, rebates, prizes, gifts and donations(36). Labels were required to include the following notice:
IMPORTANT NOTICE: Breastfeeding is best. Breast milk is the ideal food for the healthy growth and development of infants and young children. It protects against diarrhea and other illnesses.
WARNING: Before deciding to supplement or replace breastfeeding with this product, seek the advice of a health professional. It is important for your baby’s health that you follow all preparation instructions carefully. If you use a feeding bottle, your baby may refuse to feed from the breast. It is more hygienic to feed from a cup.
Specifications for the text size of these notices were included. Similar warnings were required for labels on feeding bottles or teats. The regulations applied to infant formula, follow-up formula, complementary foods and relevant feeding accessories. Companies were given a grace period until the end of May 2011 to implement the regulations(36). According to the Consumer Council of Fiji and a local news agency, Fiji Village, companies did not change their labels to comply with the regulations in a timely way or comply with a Health Ministry directive that temporary labels be applied to formula containers stating ‘Breast feeding is best for your baby’, and instead recalled products from the shelves when the grace period expired(37,38).
Fiji’s Marketing Controls (Foods for Infants and Young Children) Regulations 2010 were amended in June 2016 to effectively remove all guidelines and restrictions on marketing in the form of labelling in Part IV of the regulations and replace them with the much weaker Standard on Foods for Infants and Other Vulnerable Populations, which do not apply to follow-up formula, growing up milks, complementary foods and feeding appliances(35,39,40). This was explained in Parliament as a response to ‘unintended negative consequences for women and children … the effect has been to keep some of the best baby formula in the world out of Fiji because the manufacturers were unwilling to pay for special labelling for such a small market’(39). At the time of writing, this weaker regulation remains in place.
Policy case study 2: efforts to restrict marketing of unhealthy foods and non-alcoholic beverages to children in Fiji
In 2014, Fiji became the first Pacific Island country to draft regulations to restrict marketing of food and non-alcoholic beverages to children(41). The draft Advertising and Promotion of Unhealthy Foods and Non-Alcoholic Beverages to Children Regulation was developed under the Food Safety Act 2003(41). The development of the regulation was requested by the then Minister for Health and overseen by the Food Taskforce Technical Advisory Group(41). Food Taskforce Technical Advisory Group members include representatives of the Ministry of Health, Ministry of Agriculture and Ministry of Trade and Finance, as well as representatives from non-governmental organisations (NGO), the food industry and academics. The development process involved drafting by a consultant, peer review by Australian experts, consultation with the food industry, and then the draft regulations were sent to the Solicitor-General’s office for consideration(41).
A health impact assessment funded by WHO was undertaken in late 2015. The draft regulation is not publicly available, but the health impact assessment report indicates that the draft regulation aims to control advertising of unhealthy foods and beverages to children in Fiji in an attempt to halt the rising prevalence of overweight/obesity and obesogenic diets, and it includes in its scope mass media advertising, sponsorship or promotion at children’s activities/events, school-based promotion, rewards and prizes, food labelling and signage(41). At the time of writing, the draft regulation was still awaiting review by the Solicitor General’s office.
Factors identified as influencing decision-making with respect to marketing restrictions, across both case studies
Marketing regulation and the economy
Five interviewees – including the respondent from the economic sector – expressed the view that marketing is an essential business practice, and that restricting marketing would have significant impacts on industry operations and potentially profits. As one interviewee stated, ‘to run a business, they have to do marketing’ (Economic). Industry actors were characterised as strongly opposed to marketing restrictions, given their perceived reactions to the draft legislation restricting marketing of foods and beverages to children and to the policy restricting marketing of breast milk substitutes.
… the industry are opposing it … maybe because the regulation is a bit strict, and a bit harsh on the businesses. (Economic)
…we were able to have that passed, that piece of regulation [on breastmilk substitutes] but even before that we had very tough opposition from the milk companies. (Consumer/public health)
Industry, specifically the food industry, was perceived as core to achieving government economic goals and an important contributor to the economy and trade. As one interviewee explained, ‘food marketing …supports the government in terms of trade’ (Consumer/Public health). Another referred to companies that sell ‘Coke’ as ‘the ones that are driving the economy in Fiji’ (Public health). Public health actors described the active involvement of industry actors by government in the development of marketing regulations: for example, ‘… the Ministry of Health started the conversation with the private sector … around what can we do to try and change the situation’ (Public health). While such multisectoral collaboration and consultation was seen to be potentially valuable, three public health interviewees suggested that industry had made specific efforts to cultivate a positive image with government through community investments and lobbying to highlight their importance to the economy.
Nonetheless, there was concern that regulation of marketing would have adverse impacts on industry – not just the food and breast milk industry but other industries such as tourism – and the economy. This was recognised explicitly by the economic interviewee, as well as the majority of public health interviewees. For example: ‘if you start regulating the market, they might want to exit [the market], or run away. So we don’t want to put too much pressure on them’ (Economic). Indeed, a few interviewees suggested a direct link between the economy and population health, with economic growth positioned as having ‘trickle down’ benefits for health. As one interviewee explained, ‘once you grow your economy, definitely this going to trickle down to the health impacts’ (Consumer/Public health). But the majority of public health interviewees described a tension between fostering industry investment and activity on the one hand and improving nutrition on the other. They suggested that public health goals were obscured by the pursuit of economic growth: ‘…at the end of the day they want the economy growing, they want job creation. So health often falls out of the plate, it’s never on the plate’ (Consumer interest). Indeed, many public health actors said health was treated as less important than economic interests by politicians and industry:
Politicians …are siding with the large transnational food industry corporation because they come in thinking if [the corporations] go away there’s loss of employment… and they don’t put public health to an equal level. (Public health)
Varied perceptions of marketing as a ‘policy problem’ relevant to nutrition
All interviewees recognised poor nutrition and NCD as critical public health problems. Interviewees from across sectors cited local (Fiji) data showing rising health and nutrition problems among children. For example, one interviewee referred to Ministry of Health data ‘which revealed increasing health problems amongst children’ (Economic). There was also recognition that NCD prevention was important, due to the economic cost of acute healthcare. One government official, for example, explained that ‘[the health sector had] a lot of interest in the prevention of NCDs … it was straining a lot of finance from our budget’ (Public health).
However, there was less consensus regarding whether marketing restrictions were an effective or appropriate action to address these problems. Public health respondents identified marketing of breast milk substitutes and unhealthy food and drink as a key contributor to undernutrition and poor diets among children. They suggested that marketing influences childhood nutrition via diverse pathways, including television advertising, social media and school-based marketing: ‘The TV ad is very influential and the second one is the social media. And anything that infiltrates into the school’ (Public health). Further, two public health interviewees expressed concern that industry self-regulation has been ineffective, with widespread non-compliance with voluntary regulation. They promoted a mandatory policy approach to restricting marketing to children in order to promote population health and nutrition:
…the voluntary approach is also either completely or partly ineffective so I think you have to introduce regulations that control how and when and about what products can be marketed to children. (Public health)
Beyond marketing of breast milk substitutes and unhealthy foods and drinks, however, all interviewees identified other key influences on nutrition in Fiji, which shaped their perception of marketing as a relevant ‘policy problem’. These included urbanisation, the changing responsibilities of working parents, the price of healthy foods, taste (salt, sugar and fat), westernisation, low literacy and convenience of processed foods. Changes in the workforce, in particular, were considered a pivotal influence on breast-feeding rates and children’s diets, which had implications for interviewees’ perception of the appropriateness of marketing restrictions as a policy ‘solution’. Three interviewees noted that increased formal employment among parents had resulted in children eating poorer quality food because parents had less time to prepare food (thus identifying poor diets among children as problematic, but not necessarily that it was ‘marketing’ generating the problem). In contrast, use of breast milk substitutes was not viewed as a problem by some interviewees, with access to breast milk substitutes seen as essential for working mothers: ‘We cannot see [infant formula as] a problem… it’s easy for… working mothers’ (Public health). Indeed, three public health interviewees noted that unsupportive workplace environments were more of a barrier to breast-feeding than marketing. And some interviewees also suggested that consumers were not concerned about marketing of breast milk substitutes: for example, ‘…we don’t have anything like that, where the mothers are saying there should be restriction on these formulas that has been sold’ (Consumer interest).
Power imbalance among stakeholders
Interviewees referred to an imbalance in the influence of industry and public health stakeholders in policy. This was seen as a pivotal barrier to effective restriction of marketing. Industry actors were understood to have had substantial opportunity to influence the case study policies for three reasons. First, the dominant economic paradigm in policymaking (i.e. economic goals have primacy and economic actors are engaged in policymaking, discussed above) meant that industry was consulted in decision-making. Their active engagement in policymaking by Government officials was perceived to be a strategy to ensure they kept business, and associated employment opportunities, in the country. Four interviewees mentioned the Government working with breast milk substitute and food companies: for example, ‘they [industry] are just more strategic [than public health]. They are also more involved in the economy and with politics generally’ (Public health).
Second, three public health interviewees indicated that industry actors had significant political influence via lobbying and funding of politicians. One interviewee explained, ‘it’s most of these business people that funds political parties’ (Public health). Industry actors were also seen to have substantial resources available for policy advocacy, lobbying and to influence public opinion. For example, two public health interviewees noted that industry had strategically withdrawn products from market to foster public discontent with the restriction on marketing of breast milk substitutes: ‘[The industry] created a vacuum and then … the people to respond, so that was the strategy they used and they’ve used it previously’ (Public health). Industry was also said to use significant resources to foster goodwill among the public and policy community, for example, Coca-Cola Amatil Fiji providing sponsorship for the Fiji Secondary School Athletics, a schools athletics sports meet known as the ‘Coca-Cola Games’, and other sports events:
They used to only do the Coca Cola Games. Ever since discussions on the marketing bill, they have moved to Kaji rugby I think, they have now moved to wellness. They are trying to improve their image with Government to make sure that Government stays on their side on this. (Public health)
In contrast, civil society actors had relatively limited resources and capacity to sustain advocacy. A few interviewees noted a previous campaign for improving nutrition that was seen as effective but under-resourced and ‘within a short while they were gone, no money’ (Public health). Similarly, public health interviewees noted the limited resources available to Government to promote healthy food in comparison with the marketing resources of the private sector to promote profitable, processed and usually less healthy foods: ‘Ministry might have one ten dollar bill to advertise, the big companies have $500 comparatively’ (Public health).
Third, lack of public and civil society engagement was identified by many public health interviewees as hampering a strong public health voice on marketing restrictions. For example: ‘The public is not saying anything, you need consumer groups… you need people who have vested interest in health speaking up’ (Public health). This was linked to a perception that both consumers and Government were focused more on treatment than prevention of chronic disease:
The priority is to treat the sick patients, the priority is to provide them with beds, and the priority is to give them medication … who cares about marketing… So, you see the emotion that is involved. So that is where the government’s priority will link. (Consumer interest)
Divided governance responsibilities
All interviewees commented on the complex policy environment, in which interest and responsibility for regulation of marketing for health purposes were split across health and economic sectors. For example, one interviewee explained that ‘the trade sector has a very big influence on this. Because we are trying to regulate [industry actors] that are trading junk food but Government is seeing them as a source of revenue’ (Public health). These sectors were seen to be working at cross purposes, with health stakeholders seeking to regulate industry marketing and the economic sector seeking to promote commerce and trade. In this multisectoral context, leadership from only the health sector was considered insufficient to overcome this tension. For example, in the case of restriction of marketing of breast milk substitutes introduced in 2010, senior Ministry of Health support was key in progressing policy, but industry made appeals to the economic sector, which resulted in subsequent changes. Similarly, one interviewee described vocal government lobbying by the beverage industry to the economic sector in response to draft beverage marketing restrictions:
Industry has been quite proactive in lobbying against it. The beverage industry put forward their own MoU, to Ministry of Industry and Trade and said ‘we don’t need this’ multiple times. They have only heard the industry side of the story. They are saying it would be restrictive, would drive them out of business. (Public health)
The governance responsibilities of international institutions, particularly WHO, was also raised by interviewees. WHO was cited as a lead public health actor and critical in operationalising and guiding health sector action. However, actors outside the public health sector questioned the relevance of the ‘international agenda’ for Fiji:
…unfortunately that’s how some policy are made in the government, that it’s the international agenda rather than looking at the country’s statistics and understanding our economic and social conditions so that we can use that information and see which aspect of international policy we can push and which one can be suitable. (Consumer interest)
Opportunities and strategies
Interviewees, particularly from the public health sector, identified three key opportunities for strategic policy engagement to support restrictions on marketing, which broadly align to the factors identified as barriers. First was the potential to reframe the policy issue in a way that speaks to the dominant economic policy paradigm: that is, good population health is good for the economy. As one interviewee stated: ‘It’s an economic issue, it’s not only a health issue. Economy is built on health and education; you improve on these two [and] the economic development will take place’ (Public health).
Second, interviewees saw potential for strategic advocacy and presentation of evidence to a range of relevant stakeholders including politicians, economic actors that influence policymaking, industry actors and the wider community. There was a perception that this could generate stronger multisectoral concern regarding the impacts of marketing.
I think we should call all the politicians, continue to give them evidence…the impact of NCDs in Fiji from the health point of view…That might probably change their mind and the business people, and the industry … the manufacturers of Coke, fizzy drinks and all these snacks … the fast food outlets … Yeah, there’s a need for a lot of consultations and evidence to be produced to them and … make them change their thinking. (Public health)
Finally, almost all interviewees mentioned the need for community engagement in calling for and supporting regulation of marketing of breast milk substitutes and foods and beverages. This was perceived as a way to counter strong industry lobbying. Some highlighted the importance of using media to communicate and raise public awareness around nutrition. Others suggested building on previous community-level successes and initiatives, such as the Fiji Alliance for Healthy Living (a group of health experts, researchers and consumer advocates) to lobby for stronger regulations. They noted the limitations of community engagement and initiatives due to funding and resource constraints, but suggested that community lobbying of politicians could effect change.
…politicians are interested in doing what they believe their community wants them to do partly for altruistic reasons but partly because they want to get re-elected as well. So if they believe that this is truly what their community wants and that their community is demanding it, then they will do it and I don’t think we’re in that situation yet. (Public health)
Discussion
There have been recent calls for public health research to gain ‘a deeper understanding of the complex and changing rationalities of policymaking’ as a crucial step for social determinants of health research, with a focus on the politics and processes of policy change(42). This study contributes to deeper understanding through taking a political economy analysis approach to policy analysis. Specifically, this study explicitly examines the interface between public health nutrition policy and the economic sectors in which it is often enacted; the sectors governing the food environment and broader food system include Commerce, Trade, Agriculture and Finance, all of which tend to have primarily an economic mandate(21,43,44).
The findings of this study in Fiji identify challenges to the adoption of strong restrictions on marketing of both breast milk substitutes and unhealthy foods and beverages to children. Across both case studies, strong resistance to marketing regulation by private sector actors was observed, as well as significant constraints to effective multisectoral action as the health and economic sectors work at cross-purposes to promote their respective priorities. Restrictions on marketing are strongly recommended by global public health bodies as part of comprehensive public health nutrition policy; yet, as this study clearly shows, they are contrary to prevailing economic policy priorities to foster economic growth through private sector activities. In addition, the responsible government sector with regulatory remit for restriction of marketing is the economic sector. In line with this, industry was positioned as a key stakeholder, and marketing as a core business activity that was not an appropriate target of regulation. In the face of this tension between economic and public health nutrition goals, participants identified a critical need for strengthening the participation of civil society actors in policy making, in hand with raising public awareness regarding the potential health benefits of restricting marketing.
These findings are consistent with global reviews of constraints to nutrition-related policy action, specifically that weak regulatory decisions have been influenced by resistance by industry, both local and transnational, as well as by power imbalances between stakeholder groups and ideological factors that preference economic and industry priorities(45). Recent studies in low- and middle-income countries have identified a lack of consensus on the nature and causes of the policy ‘problem’ and conflicts with other policy priorities as barriers to strong nutrition policy(46), and a clear need for engagement with, and mobilisation of the public, for adoption of effective policy across sectors to address all forms of malnutrition(47,48). Previous studies of the political economy of nutrition have also identified similar challenges with diverse framings of nutrition hampering strong policy, sectoral conflicts due to a shared (or divided) policy space and the limited capacity and power of nutritionists (within the health sector) to manage the policy development process(49).
In this study, participants also suggested that marketing regulation could be better enabled through reframing regulation policies to resonate with dominant economic policy paradigms and the remit of powerful government Ministries (e.g. healthy populations enable healthy economies). They recommended that this strategy should be supported by increasing advocacy and presentation of evidence to a diverse range of relevant stakeholders and promoting and enabling community engagement in regulation of marketing. These suggestions align with recent evidence that indicates that approaches to securing policy change should not be based on linear conceptualisations of policy processes but rather engage with the messy reality of policymaking, embracing dialogic approaches, community engagement and philosophical and moral reasoning as well as presentation of evidence and population health rationales(42).
A key strength of this study is that it presents an integrated analysis of two policies relating to marketing of products associated with the double burden of malnutrition. Despite recent global attention to ‘double duty actions’ to address malnutrition in all its forms(10), there has been little examination of the common challenges faced by such action. The study conclusions are limited by the lack of industry participation, which would likely have provided insights into marketing as a business practice, industry interests and opposition to marketing restrictions. Conversely, the high proportion of public health-oriented respondents may have provided an over-representation of concerns regarding marketing. This study was also limited to a single country and to case studies chosen to highlight the challenges rather than success stories. The significance of these ‘challenge’ case studies is that in many situations industry power is not explicitly evident or visible in decision-making regarding the revoking of policy or decisions not to endorse policy(50). Indeed, in non-decision-making in particular, the exercise of power can be nearly invisible to many stakeholders(51). It is likely that in many other cases, policy action is mooted before it is publicly announced.
Conclusion
These policy case studies from Fiji indicate that restrictions on marketing of unhealthy foods and breast milk substitutes, which are globally recommended policy initiatives to address the double burden of malnutrition, face politico-economic challenges. In particular, they face opposition by food industry actors, which represents a key stakeholder for the economic sectors with regulatory remit – and indeed, who explicitly position themselves as pivotal to economic growth. In addition, the policy role of the economic sector in this public health issue, where restricting marketing represents highly sensitive regulation of business practice, also appeared to hamper strong regulatory action. Recognition of the divided priorities of economic and health sectors, and identification of opportunities for multisectoral action, could help to strengthen implementation of global recommendations. At the national level, reframing the policy issue to speak to influential economic paradigms and developing strategic and inclusive approaches to public health advocacy and community engagement may help to gain traction for marketing restrictions across relevant government sectors.
Acknowledgements
Acknowledgements: The authors gratefully acknowledge the time and expertise of the interviewees and the input of the anonymous peer reviewers. We also thank Zoe Fyffe and Penelope Elix for their background reviews. Financial support: The project was funded through a School of Psychology and Public Health Engagement Income Growth Grant 2017, La Trobe University. Conflict of interest: None. Authorship: A.M.T., G.W., T.P., C.M., J.T. and D.G. formulated the research questions; A.M.T., D.G., T.P., C.M., G.W. and J.B. led the study design; A.M.T., G.W., A.R., J.T. and D.G. led the development of tools, piloting and data collection; A.M.T. led the analysis of the data, with initial co-coding by J.B., G.W. and D.G. and then review of the analysis by all authors; A.M.T. led the writing of the article, and all authors contributed. All authors read and approved the final version. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the College Human Ethics Sub-Committee, University Human Ethics Committee and College Health, Research and Ethics Committee of the Fiji National University and LaTrobe University, and through the Fiji National Health Research and Ethics Review Committee of the Fiji Ministry of Health and Medical Services. Written informed consent was obtained from all participants.
References
- 1. Fanzo J, Hawkes C, Udomkesmalee E et al. (2018) 2018 Global Nutrition Report: Shining a Light to Spur Action on Nutrition. Bristol, UK: Development Initiatives. [Google Scholar]
- 2. Global Panel on Agriculture and Food Systems for Nutrition (2016) Cost of Malnutrition. Why Policy Action Is Urgent. London, UK: Global Panel on Agriculture and Food Systems for Nutrition. [Google Scholar]
- 3. Global Panel on Agriculture and Food Systems for Nutrition (2016) Food Systems and Diets: Facing the Challenges of the 21st Century. London: Global Panel on Agriculture and Food Systems for Nutrition. [Google Scholar]
- 4. United Nations (2015) Transforming Our World: The 2030 Agenda for Sustainable Development. New York: United Nations. [Google Scholar]
- 5. Piwoz EG & Huffman SL (2015) The impact of marketing of breast-milk substitutes on WHO-recommended breastfeeding practices. Food Nutr Bull 36, 373–386. [DOI] [PubMed] [Google Scholar]
- 6. WHO (World Health Organization) (1981) International Code of Marketing of Breastmilk Substitutes. Geneva: World Health Organization. [DOI] [PubMed] [Google Scholar]
- 7. Boyland EJ, Nolan S, Kelly B et al. (2016) Advertising as a cue to consume: a systematic review and meta-analysis of the effects of acute exposure to unhealthy food and nonalcoholic beverage advertising on intake in children and adults. Am J Clin Nutr 103, 519–533. [DOI] [PubMed] [Google Scholar]
- 8. Harris JL, Pomeranz JL, Lobstein T et al. (2009) A crisis in the marketplace: how food marketing contributes to childhood obesity and what can be done. Annu Rev Public Health 30, 211–225. [DOI] [PubMed] [Google Scholar]
- 9. WHO (2010) Set of Recommendations on the Marketing of Foods and Non-Alcoholic Beverages to Children. Geneva: World Health Organization. [Google Scholar]
- 10. WHO (2017) Double-Duty Actions for Nutrition: Policy Brief. Geneva: World Health Organization. [Google Scholar]
- 11. WHO (2017) The Double Burden of Malnutrition: Policy Brief. Geneva: World Health Organization. [Google Scholar]
- 12. Boyland EJ & Whalen R (2015) Food advertising to children and its effects on diet: review of recent prevalence and impact data. Pediatr Diabetes 16, 331–337. [DOI] [PubMed] [Google Scholar]
- 13. Barennes H, Slesak G, Goyet S et al. (2016) Enforcing the International Code of Marketing of Breast-milk Substitutes for Better Promotion of Exclusive Breastfeeding: can lessons be learned? J Hum Lact 32, 20–27. [DOI] [PubMed] [Google Scholar]
- 14. CFBAI Children’s Food and Beverage Advertising Initiative. https://bbbprograms.org/programs/CFBAI/ (accessed February 2019).
- 15. Hawkes C (2007) Marketing Food to Children: Changes in the Global Regulatory Environment, 2004–2006. Geneva: World Health Organization. [Google Scholar]
- 16. Kunkel DL, Castonguay JS & Filer CR (2015) Evaluating industry self-regulation of food marketing to children. Am J Prev Med 49, 181–187. [DOI] [PubMed] [Google Scholar]
- 17. Smithers LG, Lynch JW & Merlin T (2014) Industry self-regulation and TV advertising of foods to Australian children. J Paediatr Child Health 50, 386–392. [DOI] [PubMed] [Google Scholar]
- 18. Pries AM, Huffman SL, Mengkheang K et al. (2016) Pervasive promotion of breastmilk substitutes in Phnom Penh, Cambodia, and high usage by mothers for infant and young child feeding. Matern Child Nutr 12, Suppl. 2, 38–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Vinje KH, Phan LTH, Nguyen TT et al. (2017) Media audit reveals inappropriate promotion of products under the scope of the International Code of Marketing of Breast-milk Substitutes in South-East Asia. Public Health Nutr 20, 1333–1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mialon M, Swinburn B, Wate J et al. (2016) Analysis of the corporate political activity of major food industry actors in Fiji. Globalization Health 12, 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Thow AM, Greenberg S, Hara M et al. (2018) Improving policy coherence for food security and nutrition in South Africa: a qualitative policy analysis. Food Secur 10, 1105–1130. [Google Scholar]
- 22. Baker P, Hawkes C, Wingrove K et al. (2018) What drives political commitment for nutrition? A review and framework synthesis to inform the United Nations Decade of Action on Nutrition. BMJ Glob Health 3, e000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ministry of Economy, Republic of Fiji (2017) 5-Year and 20-Year National Development Plan: Transforming Fiji. Suva: Government of Fiji. [Google Scholar]
- 24. Hendriks A-M, Delai MY, Thow A-M et al. (2015) Perspectives of Fijian policymakers on the obesity prevention policy landscape. Biomed Res Int 2015, 926159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Thow AM, Swinburn B, Colagiuri S et al. (2010) Trade and food policy: case studies from three Pacific Island countries. Food Policy 35, 556–564. [Google Scholar]
- 26. Ministry of Health and Medical Services (2014) Non-Communicable Diseases Strategic Plan 2015–2019. Suva: Fiji Health Sector Support Program, Government of Fiji. http://www.health.gov.fj/wp-content/uploads/2018/03/Final-NCD-Strategic-Plan-2015-2019.pdf (accessed January 2020). [Google Scholar]
- 27. Sacks G, Mialon M, Vandevijvere S et al. (2015) Comparison of food industry policies and commitments on marketing to children and product (re) formulation in Australia, New Zealand and Fiji. Crit Public Health 25, 299–319. [Google Scholar]
- 28. Yin RK (2003) Case Study Research: Design and Methods, Applied Social Research Methods Series, Vol. 5. Thousand Oaks: Sage Publications. [Google Scholar]
- 29. Reich MR & Balarajan Y (2014) Political economy analysis for nutrition policy. Lancet Glob Health 2, e681–e682. [DOI] [PubMed] [Google Scholar]
- 30. Moore K, Kleinman DL, Hess D et al. (2011) Science and neoliberal globalization: a political sociological approach. Theory Soc 40, 505–532. [Google Scholar]
- 31. Campbell JL (1998) Institutional analysis and the role of ideas in political economy. Theory Soc 27, 377–409. [Google Scholar]
- 32. Hill M (2005) The Public Policy Process, 4th ed. Harlow: Pearson Education Limited. [Google Scholar]
- 33. Kingdon JW (2003) Agendas, Alternatives and Public Policies. New York: Longman. [Google Scholar]
- 34. Shiffman J & Smith S (2007) Generation of political priority for global health initiatives: a framework and case study of maternal mortality. Lancet 370, 1370–1379. [DOI] [PubMed] [Google Scholar]
- 35. International Baby Food Action Network (n.d.) 24 Jun breaking news – Code regression in Fiji.
- 36. Fijian Government (2011) Marketing Controls of Food for Infants and Young Children. Suva: Fijian Government. [Google Scholar]
- 37. Kumar P (2011) Enough Time Was Given to Infant Formula, Baby Food Distributors. Suva: Consumer Council of Fiji. [Google Scholar]
- 38. Koroitanoa S (2011) Supermarkets not selling SMA/S26 infant milk cans. Fiji Village. https://fijivillage.com/news/Supermarkets-notselling-SMAS26-infant-milk-cans-95k2rs/ (accessed January 2020).
- 39. Parliament of the Republic of Fiji (2016) Official Report of Proceedings (Hansard) Wednesday 22nd June 2016. Suva: Parliament of the Republic of Fiji.
- 40. World Health Organization (2018) Marketing of Breast-Milk Substitutes: National Implementation of the International Code, Status Report 2018. Geneva: WHO. [Google Scholar]
- 41. Harris P, Wate J & Friel S (2016) A Health Impact Assessment (HIA) on the Draft Regulation ‘Advertising and Promotion of Unhealthy Foods and Non-Alcoholic Beverages to Children Regulation’ in Fiji. Sydney: Menzies Centre for Health Policy, University of Sydney. [Google Scholar]
- 42. Carey G & Crammond B (2015) Action on the social determinants of health: views from inside the policy process. Social Sci Med 128, 134–141. [DOI] [PubMed] [Google Scholar]
- 43. Mozaffarian D, Angell SY, Lang T et al. (2018) Role of government policy in nutrition – barriers to and opportunities for healthier eating. BMJ 361, k2426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Gillespie S & van den Bold M (2017) Agriculture, food systems, and nutrition: meeting the challenge. Global Challenges, 1600002-n/a. [DOI] [PMC free article] [PubMed]
- 45. Cullerton K, Donnet T, Lee A et al. (2016) Playing the policy game: a review of the barriers to and enablers of nutrition policy change. Public Health Nutr 19, 2643–2653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Unwin N, Samuels TA, Hassell T et al. (2017) The development of public policies to address non-communicable diseases in the Caribbean Country of Barbados: the importance of problem framing and policy entrepreneurs. Int J Health Policy Manage 6, 71–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Huang TTK, Cawley JH, Ashe M et al. (2016) Mobilisation of public support for policy actions to prevent obesity. Lancet 385, 2422–2431. [DOI] [PubMed] [Google Scholar]
- 48. Harris J, Drimie S, Roopnaraine T et al. (2017) From coherence towards commitment: changes and challenges in Zambia’s nutrition policy environment. Glob Food Secur 13, 49–56. [Google Scholar]
- 49. Balarajan Y & Reich MR (2016) Political economy challenges in nutrition. Glob Health 12, 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Mialon M, Swinburn B & Sacks G (2015) A proposed approach to systematically identify and monitor the corporate political activity of the food industry with respect to public health using publicly available information. Obes Rev 16, 519–530. [DOI] [PubMed] [Google Scholar]
- 51. Bachrach P & Baratz MS (1962) Two faces of power. Am Polit Sci Rev 56, 947–952. [Google Scholar]