Abstract
Introduction
Telehealth and its usage strongly depend on regulatory frameworks and user acceptance. During the COVID-19 pandemic, physiotherapists, occupational therapists, speech-language therapists and their patients experienced restrictions regarding the usual face-to-face therapy. Teletherapy has become a highly discussed medium for providing therapy services. This study aimed at assessing Austrian therapists’ attitudes towards teletherapy, including perceived barriers, during and before the COVID-19 lockdown. Further interest referred to therapists’ technical affinity and experiences with the application of teletherapy.
Methods
Therapists (n = 325) completed an online survey amid the COVID-19 lockdown in 2020. Retrospective indications referred to the time prior to the lockdown. Ratings were opposed across the three therapeutic professions. Subgroup analyses investigated the role of gender and age regarding technical affinity. Measures included custom-made attitudinal statements towards teletherapy and the standardized TA-EG survey.
Results
The COVID-19 lockdown caused attitude changes towards teletherapy – for example, in terms of interest (r = 0.57, p > 0.01), perceived skills for performance of teletherapy (r = 0.33, p > 0.01) and perceived need for physical contact with patients (r = 0.35, p > 0.01). Regarding technical affinity, women reported significantly higher values than men did (r = 0.32, p > 0.01). Nearly half of the participants already applied teletherapy, with mainly positive ratings regarding perceived skills and feasibility. Barriers identified were missing or unstable reimbursement policies by insurance companies and therapeutic software with guaranteed data security.
Discussion
Austrian therapists indicate a relatively high level of telehealth positivity, with an improvement in the course of the COVID-19 lockdown. However, therapists outline the need for stable reimbursement policies and secure software solutions.
Keywords: Attitudes, survey, telehealth, teletherapy, pandemic, COVID-19
Introduction
During the first months of the COVID-19 pandemic, lockdown measures were taken in Austria to limit social contacts. Interactions were restricted to essential professional activities and to meeting one’s own basic needs or those of others. While hospitals and most medical practices remained opened, many rehabilitation clinics and private therapy practices merely treated patients with highly acute problems or closed down due to the unpredictable situation and limited capacities of protective equipment. At that time, telehealth had not been implemented as a standardized means of healthcare provision in Austria.
For the successful implementation of telehealth services, a variety of technological, organizational, human and economic requirements need to be met, 1 which are usually established slowly and fragmentally apart from emergency situations. 2 Factors such as low technical affinity of staff, 3 resistance to change of processes, the redefinition of existing roles, the emergence of new professional profiles and the need for new models of reimbursement,2–4 data security confidentiality and protection 4 were shown to hinder its implementation. In addition to the aforementioned barriers, expectations and beliefs of the stakeholders play a profound role in the process of telehealth implementation.1,5 Wade et al. 6 even concluded that clinicians’ acceptance is the key factor for sustainable telehealth services. Therefore, user attitudes towards telehealth are of high importance regarding their scaling as an equal part of healthcare provision.
Attitudes of Finish physicians, nurses and physiotherapists (PTs) were reported to be ranging from negative to enthusiastically positive, depending on time, situation, profession, health centre and telehealth application. 7 Especially in rural regions, the possibility to provide services over great distances positively influences attitudes. 8 Attitudes may change over time, with individual telehealth experience being a potential positive or negative factor of influence.7,9 Besides experience, historical events can provoke attitude change. 10 The COVID-19 pandemic rapidly leveraged diverse multi-disciplinary telehealth implementation globally,11–17 and thus seems to change attitudes towards telehealth implementation.
The present study explored the impact of the COVID-19 pandemic on the perception of telehealth in a selection of therapeutic healthcare professions. The participating PTs, occupational therapists (OTs) and speech language therapists (SLTs) were severely affected. PTs, OTs and SLTs play a crucial role in the healthcare provision for people with physical, cognitive and mental disabilities and diseases, providing therapy services under a common legal regulation in Austria. 18 This study addresses the professionals’ attitudes regarding the use of telehealth in their therapeutical work rather than their overall opinion on telehealth services. Hence, we use the term teletherapy, which – due to a lack of a consistent definition – has been defined as the provision of physio-, occupational and speech and language therapy over distance using information and communication technology. Therefore, it is a subdiscipline of telehealth, which includes preventative, promotive and curative services.
The primary objective of this study was to assess the attitudes towards teletherapy of Austrian PTs, OTs and SLTs, and their changes due to the COVID-19 pandemic. Secondary objectives aimed at giving a broader insight into relevant influential factors such as technical affinity and teletherapy experiences.
Methods
Study design and participants
PTs, OTs and SLTs working in Austria, without limitations regarding age, years of professional experience, specialization, employment setting and geographical region, were included in this cross-sectional survey. They were recruited via social media (Facebook groups “Ergotherapie Österreich” (2645 members), “Physiotherapie Österreich” (5819 members) and “Logopädie-Netzwerk Österreich” (1250 members)), as well as email newsletters of the aforementioned professional organizations (“Ergotherapie Austria” (2680 recipients), “Physio Austria - Phydelio” (7900 recipients), “Logopädie Austria” (823 recipients)). The survey was online from 3 to 28 April 2020, which was within the timeframe when Austria was under lockdown. At the time this research was carried out, the institutional research ethics committee of FH Campus Wien generally exempted surveys addressing healthcare professionals from formal review. Before answering questions, participants were informed about the study objectives, target groups and data processing procedures. All participants electronically consented to completing the survey voluntarily. No person-identifiable data were collected.
Measures
The participants completed an online survey (www.umfrageonline.com) with questions related to their personal and professional demographics, attitude towards teletherapy as well as its change due to the pandemic, experiences with teletherapy and visions for the future of teletherapy in Austria. The technical affinity of the participants – defined as a personality trait that expresses a person’s positive attitude towards, enthusiasm for and trust in technology – was assessed using the TA-EG, 19 a German standardized, valid and reliable instrument with 19 questions using a five-point Likert scale, with the highest technical affinity being a score of 95, and the lowest 19.
As there is no standardized questionnaire on health professionals’ attitudes towards telehealth procedures, custom-made attitudinal statements towards teletherapy were developed by the research team and asked for retrospective ratings of the participants’ attitudes before the COVID-19 lockdown as well for their current ratings. These questions included topics that the authors perceived as being part of the public discussion regarding teletherapy or telerehabilitation, and explicitly addressed possible barriers and limitations for its implementation, as identified in the literature2–4. Each of these questions was presented twice to those participants who stated that their attitude had changed. The first version asked for a retrospective four-point Likert rating ranging from “I would have fully disagreed” (1) to “I would have fully agreed” (4), and the second version asked for the current rating ranging from “I fully disagree” (1) to “I fully agree” (4). Additionally, the option “not specified” was given in both versions. Those participants who stated that they already had at least some experience with teletherapy, were asked for the ratings on statements concerning the performance of teletherapy with a frequency questionnaire, offering the response options “Often”, “Sometimes”, “Seldom”, “Never” or “No answer”. The survey was piloted with four occupational and physical therapists and refined according to their feedback.
Data analysis
Complete data sets of participants meeting the inclusion criteria were included in the data analysis, which was performed with IBM SPSS Statistics. Normality of data was tested with Shapiro–Wilk tests and graphical inspections of Q–Q plots. Descriptive statistics of categorical outcomes were shown as the number of cases (n) and corresponding percentage. Continuous outcomes were shown as mean with standard deviation (SD), or median with interquartile range in case of non-normality. Bivariate comparisons were tested using independent sample t-tests and Wilcoxon tests, respectively. For the Wilcoxon tests, the effect sizes r were calculated as z/sqrt(n), where n represents the number of observations; 0.1, 0.3 and 0.5 were interpreted as small, medium and large effects, respectively. 20 The relationship between continuous outcomes was assessed by means of Pearson’s correlation. Cross-tabulation was used to compare frequencies across the professions. Considering two degrees of freedom, a Cramer’s V of 0.07, 0.21 and 0.35 was interpreted as small, medium and large effect, respectively. 20 No adjustments were made for multiple testing. Alpha was set at 0.05; exact p-values were reported.
Results
In total, 325 participants (61.2% PTs, 25.2% OTs, 13.5% SLTs) were included in the survey (Table 1); 72.6% of the participants responded within the first two days after publishing the survey. The completion rate of the survey was 78.5%; 85.5% of the participants were female, 13.8% male and 0.6% chose a diverse gender. The sample’s proportion of female participants resembled the figures of the first report of the Austrian register of healthcare professionals 21 (PT: 75%; OT: 98%; SLT: 96%). OT and SLT mean ages were slightly higher than those reported in the register (PT: 39.1 years; OT: 41.1 years; SLT: 39.7 years). Overall, 14,615 PTs, 3830 OTs and 1994 SLTs were registered as employed and/or self-employed in the Austrian healthcare professionals registry as by the end of 2019. 21 Consequently, the sample comprises 1.4%, 2.1% and 2.2% of Austria’s registered and actively working PTs, OTs and SLTs, respectively. With a maximum difference of 5%, the geographical distribution of the participants was comparable with the values listed in the Austrian healthcare professionals register, while Vienna – Austria’s most populous province – was overrepresented by 9%. 21 Respondents indicated that they had worked with a variety of patients/clients and in different settings (Table 2).
Table 1.
Participants’ demographics.
| PT | OT | SLT | Total | |
|---|---|---|---|---|
| Recruited sample, n (%) | 199 (61.2) | 82 (25.2) | 44 (13.5) | 325 (100) |
| Work setting | ||||
| Employed, n (%) | 22 (11.1) | 16 (19.5) | 11 (25) | 49 (15.1) |
| Self-employed, n (%) | 142 (71.4) | 34 (41.5) | 22 (50) | 198 (60.9) |
| Employed and self-employed, n (%) | 35 (17.6) | 32 (39) | 11 (25) | 78 (24) |
| Gender | ||||
| Female, n (%) | 156 (78.4) | 78 (95.1%) | 44 (100) | 278 (85.5) |
| Male, n (%) | 41 (20.6) | 4 (4.9) | 0 (0) | 45 (13.8) |
| Diverse gender, n (%) | 2 (1) | 0 (0) | 0 (0) | 2 (0.6) |
| Age and professional experience | ||||
| Age in years, mean (SD) | 40.16 (8.99) | 38.6 (10.32) | 37.2 (12.39) | 39.36 (9.88) |
| Professional experience in years, mean (SD) | 16.38 (9.61) | 14.26 (9.75) | 15.39 (12.22) | 15.72 (10) |
PT: Physiotherapy, OT: occupational therapy, SLT: speech and language therapy; SD: standard deviation.
Table 2.
Age groups of patients/clients and professional specialization. Multiple answers were possible.
| Patients/clients | N (%) |
|---|---|
| Babies < 1 year | 29 (8.9) |
| Toddlers < 3 years | 45 (13.8) |
| Children 3–6 years | 91 (28) |
| Children 6–10 years | 97 (29.8) |
| Children 10–13 years | 75 (23.1) |
| Teenagers 13–17 years | 92 (28.3) |
| Adults 18–40 years | 187 (57.5) |
| Adults 41–60 years | 236 (72.6) |
| Seniors >60 years | 222 (68.3) |
|
Specialization |
N (%) |
| Neurology | 113 (34.8) |
| Orthopaedics | 204 (62.8) |
| Internal medicine | 34 (10.5) |
| Psychiatry | 18 (5.5) |
| Paediatrics | 107 (32.9) |
| Women’s health | 33 (10.2) |
| Health prevention | 61 (18.8) |
| Other | 42 (12.9) |
Mean (SD) technical affinity was similar across the three professions (total: 52.3 (10.5); PT: 52.2 (10.6); OT: 52.2 (10.9); SLT: 52.6 (9.2)), with the highest scores reported by PTs (PT: 28 to 80; OT 24 to 74; SLT: 36 to 69). On average, female participants rated their technical affinity (53.2; SD: 10.2) higher than male participants (46.4; SD: 10.1). This difference (6.8) was statistically significant (95% confidence interval: 3.5, 10.0; p < 0.001), with a medium effect size (r = 0.32). A small (r = 0.14) significant correlation between age and technical affinity was observed (p = 0.014).
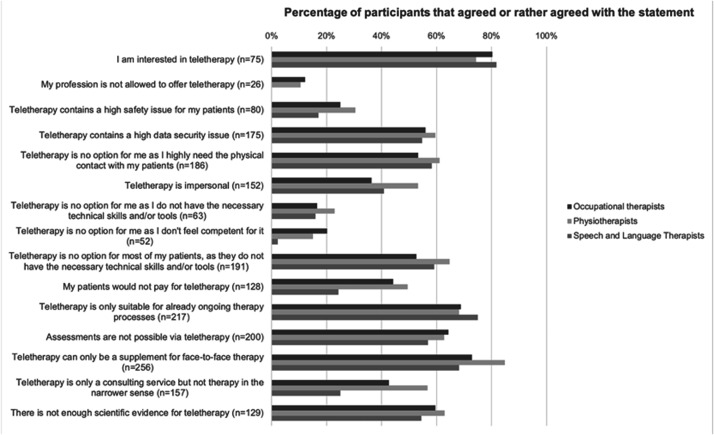
The majority of the participants stated that their attitude towards teletherapy changed due to the COVID-19 pandemic (changed a lot: 36.6%; changed a bit: 38.2%), while 25.3% said that it did not change substantially (did not change at all: 6.8%; hardly changed: 18.5%). The details of attitude changes are depicted in Table 3, taking into account all valid answers per question. Current levels of agreement with attitudes towards teletherapy and its differences between the studied professions are shown in Figure 1. Reasons for not offering teletherapy were lack of refunding from insurance companies (40.3%) or rejection of patients (26.2%), uncertainty of the legal situation (21.8%), lack of desire (19.1%), lack of competence, information and training (18.5%), lack of technical skills (8.9%) and lack of evidence for the effectiveness of teletherapy (7.7%). Other reasons (34.2%) related to workplace issues, patient groups, data security concerns, insufficient time or resources for preparation, absolute need for physical contact with patients or the lack of demand for teletherapy. Amongst the 41.9% who conducted teletherapy sessions (PT: 40.2%; OT: 40.3%; SLT: 52.3%), OTs gave more positive statements related to skills and success (Table 4). SLTs, however, had by far the lowest combined frequency of “sometimes or often” (16.7%) in the statement “teletherapy made my patients know more about their health issues”.
Table 3.
Changes in attitude toward teletherapy before COVID-19 (retrospective) and current ratings.
| Before Median (IQR) | Current Median (IQR) | z | p | r | Effect size interpretation | |
|---|---|---|---|---|---|---|
| I am interested in teletherapy (n = 239) | 2 (3) | 3 (1) | 12.36 | <.001 | .57 | Large |
| My profession is not allowed to offer teletherapy (n = 197) | 2 (1) | 1 (1) | –9.38 | <.001 | –.47 | Medium |
| Teletherapy contains a high safety issue for my patients (n = 212) | 2 (2) | 2 (0) | –0.11 | .916 | –.01 | Negligible |
| Teletherapy contains a high data security issue (n = 221) | 3 (1) | 3 (1) | –4.51 | <.001 | –.21 | Small |
| Teletherapy is no option for me, as I highly need the physical contact with my patients (n = 233) | 3 (1) | 3 (1) | –9.44 | <.001 | –.44 | Medium |
| Teletherapy is impersonal (n = 237) | 3 (1) | 2 (1) | –7.30 | <.001 | –.34 | Medium |
| Teletherapy is not an option for me, as I do not have the necessary technical skills and/or tools (n = 233) | 2 (2) | 2 (1) | –7.20 | <.001 | –.33 | Medium |
| Teletherapy is not an option for me, as I do not feel competent for it (n = 234) | 2 (2) | 2 (1) | –8.66 | <.001 | –.40 | Medium |
| Teletherapy is not an option for most of my patients, as they do not have the necessary technical skills and/or tools (n = 230) | 3 (1) | 3 (1) | –6.53 | <.001 | –.30 | Medium |
| My patients would not pay for teletherapy (n = 204) | 3 (1) | 2 (1) | –8.04 | <.001 | –.40 | Medium |
| Teletherapy is only suitable for already ongoing therapy processes (n = 231) | 3 (1) | 3 (1) | –4.95 | <.001 | –.23 | Small |
| Assessments are not possible via teletherapy (n = 239) | 3 (1) | 3 (1) | –7.41 | <.001 | –.34 | Medium |
| Teletherapy can only be a supplement for face-to-face therapy (n = 238) | 4 (1) | 3 (1) | –7.61 | <.001 | –.35 | Medium |
| Teletherapy is only a consulting service but not therapy in the narrower sense (n = 233) | 3 (2) | 2 (1) | –9.46 | <.001 | –.44 | Medium |
| There is not enough scientific evidence for teletherapy (n = 154) | 3 (1) | 3 (1) | –5.51 | <.001 | –.31 | Medium |
P-values derived from Wilcoxon tests, with test statistic r calculated as z/sqrt(n), where n represents the number of observations.
All statements self-rated on a four-point Likert scale, where higher values express better agreement.
Effect size interpretation: r .1, .3 and .5 represents small, medium and large effects, respectively.
Variation in sample sizes results from differing numbers of valid answers provided by the respondents. Invalid answers resulted from the option “not specified”.
IQR: interquartile range.
Figure 1.
Current attitude towards teletherapy.
Table 4.
Combined frequencies of the answers “sometimes” and “often” in statements related to experiences with teletherapy.
| Valid answers: “sometimes” or “often” (n) | “sometimes” or “often” % (95% CI) | Cramer-V (interpretation) | p-value | ||
|---|---|---|---|---|---|
| I experienced technical difficulties | OT | 33, 12 | 36.4 (20.0, 52.8) | .078 (small) | .701 |
| SLT | 22, 10 | 45.5 (24.6, 66.3) | |||
| PT | 80, 28 | 35.0 (24.5, 45.5) | |||
| Total | 135, 50 | 37.0 (28.9, 45.2) | |||
| I felt competent in what I was doing | OT | 33, 33 | 100.0 (100.0, 100.0) | .184 (small) | .077 |
| SLT | 23, 22 | 95.7 (87.3, 100.0) | |||
| PT | 81, 72 | 88.9 (82.0, 95.7) | |||
| Total | 137, 127 | 92.7 (88.3, 97.1) | |||
| I could realize what I wanted to achieve | OT | 33, 31 | 93.9 (85.8, 100.0) | .058 (negligible) | .914 |
| SLT | 23, 21 | 91.3 (79.8, 100.0) | |||
| PT | 80, 72 | 90.0 (83.4, 96.6) | |||
| Total | 136, 124 | 91.2 (86.4, 95.9) | |||
| I felt that teletherapy works better than I expected | OT | 32, 29 | 90.6 (80.5, 100.0) | .092 (small) | .576 |
| SLT | 22, 19 | 86.4 (72.0, 100.0) | |||
| PT | 76, 63 | 82.9 (74.4, 91.4) | |||
| Total | 130, 111 | 85.4 (79.3, 91.5) | |||
| I felt that teletherapy works better than face-to-face therapy | OT | 33, 5 | 15.2 (2.9, 27.4) | .168 (small) | .184 |
| SLT | 22, 1 | 4.5 (0.0, 13.2) | |||
| PT | 80, 4 | 5.0 (0.2, 9.8) | |||
| Total | 135, 10 | 7.4 (3.0, 11.8) | |||
| My patients were satisfied with teletherapy | OT | 32, 31 | 96.9 (90.8, 100.0) | .069 (negligible) | .867 |
| SLT | 22, 31 | 95.5 (86.8, 104.2) | |||
| PT | 74, 69 | 93.2 (87.5, 99.0) | |||
| Total | 128, 121 | 94.5 (90.6, 98.5) | |||
| Teletherapy made my patients take more responsibility | OT | 27, 26 | 96.3 (89.2, 100.0) | .093 (small) | .083 |
| SLT | 19, 14 | 73.7 (53.9, 93.5) | |||
| PT | 65, 55 | 84.6 (75.8, 93.4) | |||
| Total | 111, 95 | 85.6 (79.1, 92.1) | |||
| Teletherapy made my patients know more about their health issues | OT | 22, 14 | 63.6 (43.5, 83.7) | .371 (large) | <.001 |
| SLT | 18, 3 | 16.7 (0.0, 33.9) | |||
| PT | 69, 46 | 66.7 (55.5, 77.8) | |||
| Total | 109, 63 | 57.8 (48.5, 67.1) |
Effect size interpretation: Cramer-V .07, .21 and .35 represents small, medium and large effects, respectively (degrees of freedom: 2). 8
CI: confidence interval; OT: occupational therapists, PT: physiotherapists, SLT: speech and language therapists.
Question posed to those therapists who indicated at least some experience with teletherapy (n of n participants).
The results indicate that 4.9% (PT: 5.5%; OT: 2.4%; SLT: 6.8%) plan to discontinue teletherapy after the COVID-19 pandemic; 20.9% (PT: 17.6%; OT: 23.2%; SLT: 31.8%) intend to use it in exceptional cases only; 8.3% (PT: 8.5%; OT: 8.5%; SLT: 6.8%) as a supplement to traditional face-to-face therapy; and 2.5% (PT: 2.5%; OT: 3.7%; SLT: 0%) plan to offer pure teletherapy for some of their patients. None of the participants plan to completely switch to teletherapy, while the majority with 63.4% (PT: 65.8%; OT: 62.2%; SLT: 54.5%) stated that they were not able to answer this question as it depends on different factors (e.g. refunding policy of insurance companies). The therapists wished for refunding of teletherapy by the insurance companies in all cases (67.1%) or in specific cases (12.6%). They expressed a need for special software for therapists (64.9%), an explicit legal foundation in the national occupational law (61.2%), software that was certified by a national institution (49.8%), professional training for each health profession and/or for specific health issues (37.8%), more scientific evidence for teletherapy (35.7%), interdisciplinary training (26.5%) or an explicit prohibition of teletherapy in the national occupational law (4.0%).
Discussion
The assumption that the COVID-19 pandemic promoted an attitude change of Austrian PTs, OTs and SLTs regarding teletherapy was clearly confirmed by the results of our survey, as nearly 75% of the participants experienced such an attitude change. The item with the strongest shift was “Interest in teletherapy”. The economic insecurity, which particularly affected freelancers, as well as the lack of alternatives to continuing necessary treatment of patients, most likely influenced the awareness of teletherapy as a valid alternative to established therapy settings. Even though interest in new forms of therapy is necessary, yet not sufficient, the attitudes of stakeholders determine their implementation. Scott Kruse et al., 3 who investigated the adoption of telemedicine worldwide, found that technically challenged staff was one of the most frequent barriers. To our knowledge, our study is the first that explores technical affinity, the individual perception of technical skills regarding the performance of teletherapy and the experience of technical difficulties in teletherapeutical interventions of different health professionals in detail. The technical affinity of the participants had a wide range. Contrary to the common cliché, female participants and older participants showed significantly higher values. Less than 20% believed that teletherapy was no option for them, as they do not have the necessary technical skills and/or tools. The majority of participants, who had already had at least some experience with teletherapy, reported that they never or infrequently experienced technical difficulties. A smaller number of participants were sometimes or often confronted with technical challenges. We conclude that most of the Austrian PTs, OTs and SLTs fulfil the technical prerequisites of performing teletherapy.
Besides the technical conditions, other factors also have an influence on the implementation of teletherapy. Resistance to change is the second biggest barrier for healthcare staff, as the systematic review by Scott Kruse et al. determined. 3 This might relate to costs and reimbursement of the intervention, changes to existing workflows and the influence on the efficiency and effectiveness of care. This was also evident for our survey participants. Nearly 40% of the sample believed that their patients would not pay for teletherapy. Interestingly, this value was comparably low for SLTs (24%). However, the rating was also significantly higher before the pandemic and, therefore, subject to attitude change. We hypothesize that the participating therapists concluded that their patients would be willing to pay for teletherapy in times of the pandemic, as there were no alternative treatment possibilities. Not only the out-of-pocket payments but also the reimbursement situation was found to be a highly influencing factor. Forty percent of the participants who said that they had not implemented teletherapy into their practice confirmed that this was due to missing reimbursement. It should be noted that during the implementation of the survey, several changes in the reimbursement policy of the insurance companies with regard to teletherapy were initiated. More than two-thirds of the participants indicated the wish that teletherapy would be reimbursed in all or at least in special cases. Some mentioned that the continuation of teletherapy would depend on the future reimbursement situation.
Regarding the changes to workflows as well as efficiency and effectiveness of care, we found that the majority of therapists experienced in teletherapy, gave positive ratings in terms of feeling competent in its implementation, being able to perform what they wanted to achieve and obtaining teletherapy performance that exceeded expectations. Aggarwal et al. also reported that SLTs, who started with teletherapy following the COVID-19 pandemic, quickly adapted to the new situation, while still experiencing an increased level of stress due to the new situation. 17 Highlighting the patient side, our participants mostly felt that the patients were satisfied with teletherapy and that they often or sometimes took over more responsibility in the new setting. This is in line with other authors who have described a positive effect of telemedicine services on patient empowerment and autonomy.22–24
Compared to the study by Aggarwal et al., where SLTs had a mixed opinion regarding the question if telepractice could compensate for face-to-face therapy, 17 only a very small percentage of the participants of our survey stated that they often or sometimes felt that teletherapy works better than face-to-face therapy. This is in accordance with only 2.5% planning to continue exclusively with teletherapy and 8.3% planning to use teletherapy merely as a supplement in the future. Notably, the majority was not committing to or against a personal teletherapy service model in the future due to the uncertainty of influencing factors such as reimbursement policies or the further development of the pandemic.
Further, major barriers for the implementation of telehealth according to Scott Kruse et al. 3 were issues concerning legal liability, privacy confidentiality and security of data. Before the COVID-19 pandemic, the legal situation regarding the performance of teletherapy in PTs, OTs and SLTs was unclear and under discussion. This might be reflected by a significant change in the participants’ assessment of the legality of teletherapy in Austria. While the offer of webinars and newsletters dealing with teletherapy increased during the COVID-19 pandemic, this could have had an influence on the awareness of the legality of teletherapy. At the time the survey was conducted, a statement of the government confirmed that teletherapy was allowed under specific circumstances, which might also have shaped the opinion of the participants.
Our participants’ opinion that teletherapy contains a high data security issue only changed slightly and did not seem to be as heavily influenced by the pandemic as other areas. Yet, more than half of the participants found that data security risks are high, which confirms the findings of other authors.25,26 During the increased public and professional discussions, a high demand for education in terms of patient data security became obvious, whereupon several webinars were offered to obtain information about measures that can be used to increase patient data security. The uncertainty of the legal situation and the lack of competence, information and training were co-responsible for the decision of therapists who did not want to offer teletherapy. Additionally, this was reflected in the therapists’ expressed need for professional training, legal foundations and special software that was certified by a national institution. Professional training was shown to have the potential to remove barriers that hinder telehealth implementation. 27
Another barrier to the implementation of Telemedical interventions might be the perception of impersonal care. 3 Nearly half of the surveyed therapists found that teletherapy is impersonal, and more than half agreed that they urgently needed physical contact with their patients. However, both values decreased significantly after the beginning of the pandemic. Lack of hands-on treatment was also addressed as a perceived downside in other publications that focused on telehealth implementation during the pandemic.27,28
Limitations
As this survey was conducted when the lockdown in Austria was in place, it was not possible to assess therapists’ attitudes regarding teletherapy without the presence of a pandemic. Consequently, their attitudes before the COVID-19 pandemic were captured retrospectively and compared with their current ratings. This method has the risk of a recall bias. Hence, results should be interpreted with caution, even though we believe that the recalled period was recent enough to promise valid answers. This survey was designed as a spontaneous reaction to the rapid progression of the pandemic. Therefore, we could not carry out a longitudinal design and include further professions of interest.
Another risk of bias concerns the recruitment strategy for participants. As only digital media were used to distribute the link to the online survey, therapists with lower technical affinity and usage of email or social media might not have been included. This could have affected the representation of the technical affinity scores and attitudes toward teletherapy. In terms of age and gender distribution, the sample is similar to the figures reported in the Austrian register of health professions. Due to aforementioned limitations and the medium sample size, generalized conclusions referring to the population of Austrian PTs, OTs and SLTs should be drawn with care. Nevertheless, this is, to date, the only survey capturing more than 300 therapist attitudes on teletherapy topics. A variety of therapeutical specializations and targeted patient groups of three different therapy professions were present in our sample. Possible differences between the attitudes of this diverse group were not taken into account in the data analysis. Further research should focus on specific research questions to give a more differentiated picture of the attitudes, preferences and needs of PTs, OTs and SLTs.
Conclusion
The COVID-19 pandemic boosted the implementation of teletherapy in Austria and initiated, amongst others, an attitude change of PTs, OTs and SLTs in their interest in and possibilities of teletherapy, as well as skill-assessment of teletherapy performance. Mainly positive findings concerning perceived competence and outcomes were reported, while technical and data security barriers remained. The technical affinity is diverse across all subgroups, with less than half of the participating therapists already having carried out teletherapy. It cannot be ascertained whether the transition to teletherapy influences therapeutical paradigms sustainably. Nonetheless, changes in reimbursement by insurance companies and specific software are regarded as necessary for the substantial integration of teletherapy into existing therapeutic care provision. Further research is required to explore if the effects observed in this study are permanent. Additionally, research exploring the patients’ attitudes toward teletherapy would be beneficial.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Lena Rettinger https://orcid.org/0000-0003-0388-3438
Peter Putz https://orcid.org/0000-0003-2314-3293
References
- 1.Roig F, Saigí F.Barreras para la normalización de la telemedicina en un sistema de salud basado en la concertación de servicios. Gac Sanit 2011; 25: 397–402. [DOI] [PubMed] [Google Scholar]
- 2.Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare 2020; 26: 309–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Scott Kruse C, Karem P, Shifflett K, et al. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare 2018; 24: 4–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scott RE, Mars M.Principles and framework for eHealth strategy development. J Med Internet Res 2013; 15: e155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pan American Health Organization. Framework for the implementation of a telemedicine service. Washington, DC: Pan American Health Organization, 2016. [Google Scholar]
- 6.Wade VA, Eliott JA, Hiller JE.Clinician acceptance is the key factor for sustainable telehealth services. Qual Health Res 2014; 24: 682–694. [DOI] [PubMed] [Google Scholar]
- 7.Vuononvirta T, Timonen M, Keinänen-Kiukaanniemi S, et al. The attitudes of multiprofessional teams to telehealth adoption in northern Finland health centres. J Telemed Telecare 2009; 15(6): 290–296. [DOI] [PubMed] [Google Scholar]
- 8.Mauldon E.The use of and attitudes towards telehealth in rural communities. Aust J Prim Health 2007; 13(3): 6. [Google Scholar]
- 9.Hanson D, Calhoun J, Smith D.Changes in provider attitudes toward telemedicine. Telemed e-Health 2009; 15(1): 39–43. [DOI] [PubMed] [Google Scholar]
- 10.Albarracin D, Shavitt S.Attitudes and attitude change. Annu Rev Psychol 2018; 69: 299–327. [DOI] [PubMed] [Google Scholar]
- 11.Lee AC.COVID-19 and the advancement of digital physical therapist practice and telehealth. Phys Ther 2020; 100: 1054–1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mann DM, Chen J, Chunara R, et al. COVID-19 transforms health care through telemedicine: evidence from the field. J Am Med Inform Assoc 2020; 27: 1132–1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alpalhão V, Alpalhão M.Impact of COVID-19 on physical therapist practice in Portugal. Phys Ther 2020; 100: 1052–1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pedersini P, Corbellini C, Villafañe JH.Italian physical therapists’ response to the novel COVID-19 emergency. Phys Ther 2020; 100: 1049–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fisk M, Livingstone A, Pit SW.Telehealth in the context of COVID-19: changing perspectives in Australia, the United Kingdom, and the United States. J Med Internet Res 2020; 22: e19264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dimer NA, Canto-Soares Nd, Santos-Teixeira LD, et al. Pandemia do COVID-19 e implementação de telefonoaudiologia para pacientes em domicílio: relato de experiência. Codas 2020; 32: e20200144. [DOI] [PubMed] [Google Scholar]
- 17.Aggarwal K, Patel R, Ravi R. Uptake of telepractice among speech-language therapists following COVID-19 pandemic in India. Speech, Lang Hear 2020: 1–7. DOI: 10.1080/2050571X.2020.1812034. [Google Scholar]
- 18. Bundesgesetz über die Regelung der gehobenen medizinisch-technischen Dienste: MTD-Gesetz , 2020, https://www.ris.bka.gv.at/GeltendeFassung.wxe?Abfrage=Bundesnormen&Gesetzesnummer=10010701
- 19.Karrer K, Glaser C, Clemens C, et al. Technikaffinität erfassen - der Fragebogen TA-EG. Der Mensch im Mittelpunkt technischer Systeme. 8. Berliner Werkstatt Mensch-Maschine-Systeme. Düsseldorf: VDI Verlag GmbH; 2009. pp 196–201.
- 20.Cohen J.Statistical power analysis for the behavioral sciences. 2nd ed.United States of America: Lawrence Erlbaum Associates, 1988. [Google Scholar]
- 21.Rappold E, Juraszovich B, Zach M, et al. Jahresbericht Gesundheitsberuferegister 2019. Wien: Gesundheit Österreich GmbH, 2020. [Google Scholar]
- 22.Bradford NK, Caffery LJ, Smith AC.Awareness, experiences and perceptions of telehealth in a rural Queensland community. BMC Health Serv Res 2015; 15: 427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee PA, Greenfield G, Pappas Y.Patients’ perception of using telehealth for type 2 diabetes management: a phenomenological study. BMC Health Serv Res 2018; 18(1): 549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shulver W, Killington M, Crotty M.‘Massive potential’ or ‘safety risk’? Health worker views on telehealth in the care of older people and implications for successful normalization. BMC Med Inform Decis Mak 2016; 16: 131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Savolainen L, Hanson E, Magnusson L, et al. An Internet-based videoconferencing system for supporting frail elderly people and their carers. J Telemed Telecare 2008; 14(2): 79–82. [DOI] [PubMed] [Google Scholar]
- 26.Odole AC, Odunaiya NA, Ojo OD, et al. Tele-physiotherapy in Nigeria: perceived challenges by physiotherapists to its implementation. IJTMCP 2015; 1(2): 186. [Google Scholar]
- 27.Abbott-Gaffney C, Jacobs K.Telehealth in school-based practice: perceived viability to bridge global OT practitioner shortages prior to COVID-19 global health emergency. WOR 2020; 67(1): 29–35. [DOI] [PubMed] [Google Scholar]
- 28.Tenforde AS, Borgstrom H, Polich G, et al. Outpatient physical, occupational, and speech therapy synchronous telemedicine: a survey study of patient satisfaction with virtual visits during the COVID-19 pandemic. Am J Phys Med Rehabil 2020; 99(11): 977–981. [DOI] [PMC free article] [PubMed] [Google Scholar]