Abstract
Introduction
The aim of this study was to examine whether telehealth is as safe and effective as traditional office visits in assessing and treating patients with symptoms consistent with COVID-19.
Methods
In this retrospective cross-sectional study, the primary outcome was any 14-day related healthcare follow-up event(s). Secondary outcomes were the type of 14-day related follow-up event including hospital admission, emergency department visit, office visit, telehealth visit and/or multiple follow-up visits. Individual visit types were identified due to the significant difference between a hospital admission and an office visit. Logistic regressions were done using the predictors of visit type, age, gender and comorbidities and the primary outcome variable of a related follow-up visit and then by follow-up type: hospital admission, emergency department visit or office visit.
Results
Of 1305 visits, median age was 42.3 years and 65.8% were female. Traditional office visits accounted for 741 (56.8%) of initial visits, while 564 (43.2%) visits occurred via telehealth. One hundred and forty-six (25.9%) of the telehealth visits resulted in a 14-day related healthcare follow-up visit versus 161 (21.7%) of the office visits (adjusted odds ratio (OR) 1.22, 95% CI 0.94–1.58).
Discussion
There was no significant difference in related follow-ups of initial telehealth visits compared to initial office visits including no significant difference in hospital admission or emergency department visits. These findings suggest that based on follow up healthcare utilization, telehealth may be a safe and effective option in assessing and treating patients with respiratory symptoms as the COVID-19 pandemic continues.
Keywords: COVID-19, respiratory assessment, primary care, telehealth
Introduction
The COVID-19 pandemic required adaptation across industries in the United States, and the rest of the countries in the world and their healthcare systems were not exempt from the need for innovation. As healthcare systems faced an influx of patients with respiratory illnesses and concerns for symptoms consistent with COVID-19, the decision regarding how to provide a safe and accurate assessment of patients became extremely important. Healthcare institutions, large and small, developed numerous innovative approaches in the spring of 2020 to deal with the presence of the novel coronavirus. The development of Respiratory Assessment Centres (RACs) to evaluate patients in a separate facility dedicated to complaints concerned with COVID-19 became a preferred option for many health systems.1–3 An RAC allows for the safe separation of patients with no or low concern for a respiratory illness and provides a dedicated staff to address only patients with suspicion of COVID-19.
Telehealth visits became readily available for many different reasons during the pandemic, and this platform offered the opportunity to improve the efficiency of patient evaluation while keeping patients and providers safe.4,5 Clinician assessment of patients by telehealth for COVID-19 symptoms is a viable method to limit exposure considering the contagious spread of this potentially fatal virus. 4 Numerous specialty clinics utilized telehealth during the pandemic to continue to provide care.6,7 Telehealth has been shown in some care settings to be equivalent to in-person care, and patient satisfaction has previously been shown to be high.8–10 Telehealth may decrease barriers to access to primary care services (e.g. transportation and childcare) and can provide access to the health system that has not always been available.11–13 The importance of early assessment of respiratory symptoms along with a detailed history of travel and past medical/social history can efficiently take place by telehealth.2,3 The utilization of telehealth in the midst of the pandemic as part of an RAC was appealing for all of these reasons and offered a unique opportunity to assess this modality in this unprecedented context.
The goal of this study is to determine if telehealth is an acceptable option to evaluate patients with COVID-19 symptoms using 2-week follow-up events as a proxy for effective care delivery when compared to patients evaluated in person. We hypothesize that telehealth will be as effective as face-to-face visits in the assessment of patients with respiratory symptoms potentially related to COVID-19 and will not result in a significant increase in subsequent healthcare utilization.
Methods
Setting and study sample
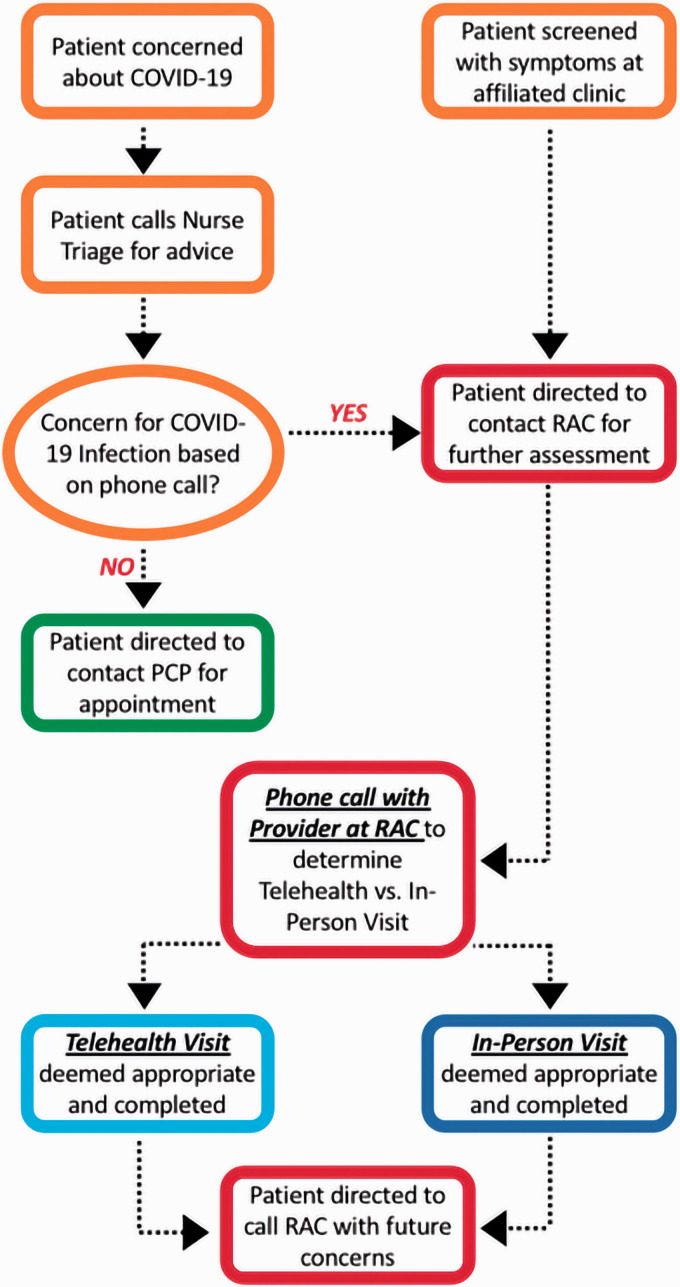
This study is a retrospective, cross-sectional study conducted at a large academic primary-care-run RAC. The Institutional Review Board (IRB) approved the study without requirement for patient consent. All patients evaluated at the RAC during an 8-week time period from 23 March 2020 to 23 May 2020 were eligible for inclusion in the study. The population included patients of all ages from less than 1 to over 90 years old. There were 1368 patient encounters at the RAC during this time period. We excluded any visits that were for asymptomatic screening purposes. Figure 1 depicts patient assessment with respiratory symptoms or COVID-19 concerns triaged by a clinician to an in-person visit at the RAC or a telehealth visit. The initial assessment occurred via telephone with a clinician stationed in the RAC. Physician assistants, nurse practitioners, family medicine residents and faculty conducted the screening via telephone using clinical judgement. Questions for screening patients included fever or cough or vomiting and/or diarrhoea in the last 24 hours, or contact with someone diagnosed with COVID-19, along with temperature screening. Based on the initial triage, the clinician determined whether the patient came to the office or if a telehealth visit was appropriate (Figure 1). Considerations in the decision of visit type include severity of symptoms, comorbidities, age, vital signs and assessment of other pertinent history.
Figure 1.
RAC patient identification workflow and follow-up process.
Data procedures
Data was extracted from the electronic health record (EHR) into an Excel® file to gather patient demographics including medical record number, age, gender and body mass index as well as initial visit type (telehealth or office). The study team then reviewed the EHR manually for each encounter to confirm the demographic data and correct initial visit type before manually adding 14-day follow-up events and coding them according to related or not related to the initial visit type. A visit was considered ‘related’ to the initial encounter if the medical problems or symptoms in the subsequent visit were something that was either identical or very similar to the initial encounter diagnosis. A visit was considered ‘unrelated’ if the diagnosis in the subsequent visit was not at all similar to the initial encounter diagnosis. For example, if a patient was seen for shortness of breath initially and then admitted to the hospital the next day for shortness of breath or similar complaint, that would count as a ‘related’ visit. If a patient was seen for shortness of breath initially and then had a visit for a different problem (e.g. regular follow-up with their primary care provider 10 days later), that was considered an unrelated visit. We set specific criteria for EHR data collection with a random sample of 200 charts recorded separately and checked by two authors (JP and JK) for discrepancies to achieve agreement. We maintained patient confidentiality by de-identifying patient records and storing electronic data in password-protected files. The coding of follow-up events included hospital admission, emergency department visit, office visit, telehealth visit or no visit. Two authors reviewed problem and medication lists in the EHR to document comorbidity status for relevant conditions that could result in more severe COVID-19 disease.14–16 We used a 14-day follow-up period to assess events due to the likelihood of resolution or worsening, based on the natural history of COVID-19 and other respiratory illnesses. 17
Exposures and outcomes
Patient evaluation occurred at the RAC via telehealth or a traditional in-person visit, and follow-up events for each group were tracked and documented. The completed telehealth visits used in this study were done by telephone. The primary study outcome was any related healthcare follow-up within a 14-day period after the initial encounter. Secondary outcomes were related visit types in the 14-day time period including hospital admission, emergency department visit, office visit, telehealth visit and/or multiple related visits. Secondary outcomes were examined because of the large difference in cost and illness severity between types of follow-up events. A hospital admission is considered much more serious than a follow-up phone visit in most cases, and the secondary outcomes were examined to determine the type of follow-up event that patients in each group were having. We documented the primary diagnosis in the event of multiple diagnoses associated with the visit. If there were no visits within the 14-day period after the initial encounter, the documentation indicated the patient had no follow-up. Patient visits occurring in the 14-day window included classification as either related or unrelated to the initial encounter as discussed above.
Statistical analysis
Data from the EHR using Tableau® and Epic Workbench® were aggregated into Excel® and SPSS® (Version 26) for analysis. Descriptive univariate statistics for all variables were done. This was followed by bivariate analysis comparing patient visits by initial visit type, telehealth versus office visit by demographics, comorbidities and primary diagnosis. Logistic regressions were then done using the single predictor of visit type and the primary outcome variables of presence or absence of a related follow-up visit and then by follow-up type: hospital admission, emergency department visit, office visit or telehealth visit. We added covariates including age, gender and comorbidities to the logistic regressions to help remove confounding. Similar logistic regressions predicted who would have multiple follow-up visits. The primary and secondary outcomes were quantified using odds ratios (OR) with 95% confidence interval (CI) for each value. The odds ratios reported are in regard to initial telehealth visits and provide a numerical association of having a follow-up event based on the initial visit type of telehealth or office visit.
Results
There were 1368 patient encounters at the RAC between 23 March and 23 May 2020. We excluded 63 visits because of asymptomatic screening appointments made for employees at local companies. Table 1 contains demographics of the remaining 1305 patients evaluated at the RAC during that time period including age, gender and relevant comorbidities. The groups were similar in each category with the exception of age and average number of comorbidities. The telehealth visit group (564 visits, 43.2% of the total visits) was older with a mean age of 42.7 years (SD 19.5 years) compared to the office visit group (741 visits, 56.8% of the total visits) with a mean age of 40.1 years (SD 21.8 years, P = 0.023). The telehealth group had an average number of 1.50 comorbidities (SD 1.45) compared to 1.33 (SD 1.44) in the office visit group (P = 0.039). The primary diagnoses varied widely among visits with 52 unique diagnoses for all 1305 visits. If all visits are considered, viral upper respiratory infection (URI) and viral URI with cough made up over 33% (431/1305) of all visit diagnoses. Table 1 includes the 10 most frequent diagnoses from all visits.
Table 1.
Demographics of patients at respiratory assessment centre by initial visit type.
| Demographics | Initial telehealth visit (n = 564) | Initial office visit (n = 741) | P-valuea |
|---|---|---|---|
| Age | Median 43.47 (mean 42.7) | Median 42.05 (mean 40.1) | 0.023 |
| Female % | 66.8 | 63.6 | 0.218 |
| Comorbidity | |||
| Hypertension | 148 (26.2%) | 200 (27.0%) | 0.762 |
| Diabetes | 69 (12.2%) | 83 (11.2%) | 0.564 |
| Obesityb | 252 (44.7%) | 295 (39.8%) | 0.077 |
| Chronic obstructive pulmonary disease | 26 (4.6%) | 36 (4.9%) | 0.834 |
| Asthma | 101 (17.9%) | 104 (14.0%) | 0.057 |
| Obstructive sleep apnoea | 66 (11.7%) | 67 (9.0%) | 0.116 |
| CAD/heart failure | 40 (7.1) | 45 (6.1%) | 0.460 |
| HIV | 2 (0.4%) | 8 (1.1%) | 0.137 |
| Chronic kidney disease | 7 (1.2%) | 20 (2.7%) | 0.067 |
| Immunosuppressivesc | 26 (4.6%) | 33 (4.5%) | 0.893 |
| Smokingd | 110 (19.5%) | 98 (13.2%) | 0.002 |
|
Mean comorbidities (SD) |
Mean comorbidities (SD) |
||
| 1.50 (1.45) | 1.33 (1.44) | 0.039 |
aChi-square for individual comorbidities, independent t-test for total comorbidities and age.
bDefined as body mass index (BMI) ≥30.
cIncluded patients on biologic immunosuppression or long-term steroid therapy based on medication list.
dOnly included current smokers of any duration.
CAD: coronary heart disease; HIV: human immunodeficiency virus.
The primary outcome of this study was a related follow-up event within a 14-day period. Table 2 displays 14-day follow-up events separated by visit type. Among the initial telehealth visits, 146 (25.9%) had a related follow-up healthcare visit within 14 days compared to 161 (21.7%) of the initial office visits (P = .079). In this population, there was no significant difference in total number of follow-up events between telehealth and in-office visits.
Table 2.
Follow-up data separated by initial visit type.
| Patient 14-dayFollow-up events | Initial telehealth visit, total (%) (n = 564) | Initial office visit, number (%) (n = 741) | P-valuec |
|---|---|---|---|
| None | 377 (66.8%) | 519 (70.0%) | 0.218 |
| Any healthcare visita | 187 (33.2%) | 222 (30.0%) | |
| Related healthcare visit | 146 (25.9%) | 161 (21.7%) | 0.079 |
|
Related healthcare visits |
|||
| Hospital admission | 11 (2.0%) | 21 (2.8%) | 0.307 |
| ED visit | 28 (5.0%) | 29 (3.9%) | 0.357 |
| Office visit | 69 (12.2%) | 66 (8.9%) | 0.033 |
| Telehealth visit | 62 (11.0%) | 72 (9.7%) | 0.452 |
| Multiple related visitsb | 28 (5.0%) | 32 (4.3%) | 0.581 |
aAny healthcare visit was an encounter regardless of reason within 14-day time period.
bPatients with multiple different visits within 14-day period.
cChi-square.
The primary outcome was the total number of related follow-up visits for each patient, but we also wanted to determine if there were any differences not just in total numbers of visits but also for a specific visit type (i.e. office, hospital admission). In order to examine differences in visit type, we categorized follow-up visits into hospital admission, emergency department (ED) visit, office visit or telehealth visit. No statistical difference was found between telehealth visits and office visits for hospital admission 2.0% (telehealth) versus 2.8% (office) (P = .307), ED visits 5.0% (telehealth) vs 3.9% (office) (P = .357), or telehealth visit 11.0% (telehealth) vs 9.7% (office) (P = .452). The only statistically significant difference found was in the related office visits. Patients who had an initial telehealth visit were slightly more likely to have a follow-up office visit 12.2% (telehealth) versus 8.9% (office) (P = .033) during the 14-day follow-up period. Patients who received an initial telehealth visit were no more likely to have multiple follow-up visits (more than 1) in the 14-day period at 5.0% versus 4.3% in the office visit group (P = .581).
Table 3 shows the results of the logistic regressions using 14-day follow-up as the dependent variable and controlling for initial type of visit, age, gender and the number of comorbidities. The odds ratio and 95% confidence interval are shown for each type of related follow-up visit. When controlling for the potential covariates, we found that age was associated with an increased risk of hospitalization if the initial visit was a telehealth visit (OR 1.04, CI 1.01–1.06). We also found that an increase in the number of comorbidities was associated with an increased risk of a related healthcare visit of any type (hospital admission, ED visit, office visit, etc.) and a related office visit during the 14-day follow-up period.
Table 3.
Logistic regression models predicting overall related follow-up visits and type of follow-up visit by initial visit, demographics and comorbidities.
| 14-Day related follow-up events | Initial visit type | Age | Gender | Comorbidities |
|---|---|---|---|---|
| Related healthcare visit | 1.22 (0.94–1.58) | 1.00 (0.99–1.01) | 0.80 (0.60–1.05) | 1.13 (1.02–1.25) |
| Hospital admission | 0.64 (0.31–1.35) | 1.04 (1.01–1.06) | 0.65 (0.29–1.46) | 1.09 (0.85–1.38) |
| ED visit | 1.24 (0.73–2.11) | 1.00 (0.99–1.02) | 0.61 (0.33–1.13) | 1.09 (0.89–1.33) |
| Office visit | 1.46 (1.02–2.10) | 0.99 (0.98–1.01) | 0.71 (0.48–1.06) | 1.16 (1.00–1.33) |
| Telehealth visit | 1.11 (0.78–1.59) | 1.01 (0.99–1.02) | 0.83 (0.57–1.23) | 1.06 (0.93–1.22) |
| Multiple related visitsc | 1.11 (0.66–1.88) | 1.01 (0.99–1.03) | 0.64 (0.35–1.16) | 1.00 (0.83–1.22) |
aData presented as odds ratio (confidence interval).
bOdds ratio always in reference to initial telehealth visits.
cPatients with two or more different visits within 14-day period.
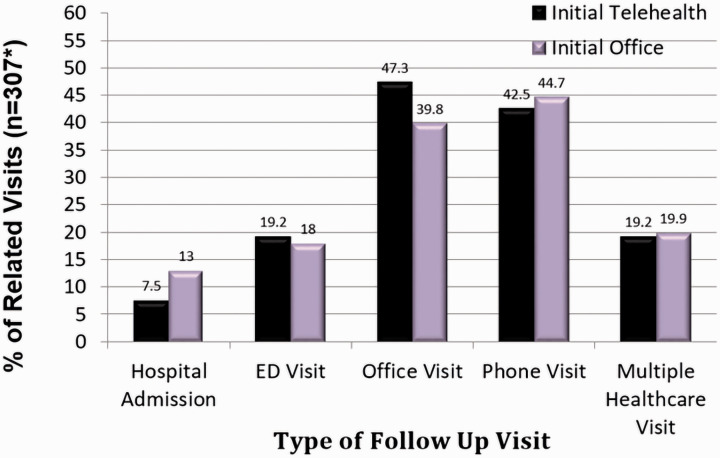
Figure 2 shows the breakdown of follow-up visit type within the 14-day window. Patients with an initial office visit had a higher percentage of related hospital admissions (13.0% vs. 7.5% in the telehealth group, P = 0.307), as well as higher related follow-up telehealth visits (44.7% vs. 42.5% in the telehealth group, P = 0.452). Patients with an initial office visit also had a slightly higher percentage of multiple follow-up visits in the 14-day period (20.5% vs. 19.2% in the telehealth group, P = 0.581).
Figure 2.
Related follow-up visits by type of visit.
Discussion
In this setting of an RAC and in the patient population studied, when initial telehealth visits were compared to initial office visits there was no significant difference in the primary outcome of a related healthcare follow-up within 14 days. This result affirms the hypothesis that overall patients with respiratory complaints can be assessed safely and effectively via telehealth as part of an RAC with proper initial triage. Patients that received care via telehealth were slightly more likely to have a related healthcare follow-up visit, but this result was not statistically significant.
There was a statistically significant difference in the likelihood of a subsequent office visit if the initial visit was done via telehealth compared to initial in-person office visits. When the first encounter was done via telehealth there was an absolute increase of 3.3% in a follow-up office visit compared to when the first visit was done as a face-to-face office visit. Using a number needed to harm methodology, this translates into one extra return office visit for every 30 patients done by telehealth, which is an acceptable outcome.
The logistic regression analysis considers the potential confounders of age, gender and comorbidities. As seen in Table 3, it uses the 14-day follow-up as the dependent variable and controls for initial type of visit, age, gender and the number of comorbidities.18,19 The group with more average comorbidities was the telehealth group. The relative effectiveness of telehealth visits when compared to office visits even with more comorbidities in the former group strongly suggests that telehealth visits can be effective in this population. As expected, older age on its own was associated with more hospital admissions, although this effect was minimal. Even though the telehealth group was on average older, there was a lower hospital admission rate among the patients with an initial telehealth visit demonstrating the small role age difference played in the results and possibly even bolstering the evidence that telehealth visits do not increase hospital admission rates. It is helpful, however, to know that older patients with COVID-19 symptoms may need a different approach to their assessment when compared to younger, healthier individuals with similar symptoms.
Several healthcare systems set up RACs dedicated to handling all respiratory complaints during the pandemic. Models for primary care providers implementing RACs during the COVID-19 pandemic are underway.2,3,20 Combining the technology of telehealth with an RAC offers a unique opportunity and has been used in multiple settings thus far in the pandemic, as well as previously in other crisis settings.21,22 Providers can see patients via telehealth or by traditional office visits based on initial triage. In theory, this increases the ability to handle a higher volume of patients and still provide adequate care while also potentially reducing cost to the system as a whole. 23
Telehealth has previously demonstrated promise in certain care areas, such as stroke, in improving outcomes and reducing cost. 24 There are, however, varying results on the question of cost saving, and it may be more complex and highly dependent on the clinical scenario.25,26 It has previously been pointed out that lack of reimbursement for telehealth has largely limited its advancement. 27 The era of COVID-19 offered a brief look into expanded reimbursement for telehealth services and may serve as a catalyst to more widespread availability in the future. Continued evidence that telehealth does not increase subsequent utilization as we have attempted to show here will hopefully solidify reimbursement models for telehealth services.
This study provides evidence that telehealth visits are comparable to in-person visits for patients with COVID-19 symptoms or concerns with regards to subsequent healthcare utilization. Evidence supporting telehealth use during a pandemic is important because it can provide a way to limit patients’ exposure to potentially infectious individuals and overcomes many barriers that impede access to care in clinic settings. 28 Additionally, patient and provider satisfaction with telehealth visits have previously been documented as positive in the literature. Both access to care and satisfaction are important considerations with the stress of the pandemic on people and systems.9,29,30
While previous literature has examined outcomes related to telehealth for specific disease states (heart failure, etc.) and home healthcare, to our knowledge, there has been little direct study of subsequent utilization after telehealth visits.31–34 Gordon et al. did a similar study in 2017 examining urgent care visits completed via telehealth vs. in-person care and found similar healthcare utilization for each modality after the initial visit, supporting our findings here. 35 This study adds value to the telehealth conversation because it examines subsequent care utilization after telehealth appointments, a key metric in the viability of telehealth in this setting. When thinking about how to organize care in the midst of a pandemic and afterwards, knowing that telehealth does not increase subsequent utilization will be valuable for clinical managers and providers alike. It should bolster confidence in this modality when used properly, and our hope is that it will allow for the continued expansion of this valuable tool.
Limitations
This study has several limitations, the first of which is non-randomization in the form of clinical decision making by phone triage. Real-time clinical decision making by providers determined which visit type patients initially received. Although this makes the groups unequal from a statistical analysis perspective, it does fit more closely with the real world, and thus allows institutions elsewhere to use this model to care for patients with respiratory symptoms as the pandemic continues. Other limitations include not accounting for additional confounders such as insurance status, comfort using a telephone and comorbid disease severity. Additionally, the COVID-19 testing at our institution, especially at the beginning of the study period, was limited and patients were not always tested as readily as they may have been in current times. However, patients were tested when deemed appropriate. This study also does not take into account the difference in cost and reimbursement of telehealth visits but rather focuses on the viability of such a clinic.
Conclusion
There was no significant difference in related healthcare follow-ups of initial telehealth visits compared to initial office visits including no significant difference in hospital admissions or ED visits. These findings suggest telehealth may be a safe and effective option in assessing and treating patients with respiratory symptoms as the COVID-19 pandemic continues.
Acknowledgement
We would like to thank Carol Hildebrandt and Dr Stephanie Daniel for editing this manuscript along with Cathy Jessup for aiding us in coding of visits for this review.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Julienne K Kirk https://orcid.org/0000-0002-5144-7780
References
- 1.Wosik J, Fudim M, Cameron B, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc 2020; 27(6): 957–962. doi.org/10.1093/jamia/ocaa067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harmes MDK, Jenq MDG, Standiford BST, et al. Implementation of primary care pandemic plan: Respiratory clinic model. Ann Fam Med. Epub ahead of print 13 April 2020. https://deepblue.lib.umich.edu/handle/2027.42/154742
- 3.Mehrotra A, Ray K, Brockmeyer DM, et al. Rapidly converting to “virtual practices”: Outpatient care in the era of Covid-19. N Engl J Med 2020; 1: 1(2). [Google Scholar]
- 4.Hollander JE, Carr BG.Virtually perfect? Telemedicine for COVID-19. N Engl J Med 2020; 382: 1679–1681. doi 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 5.Wijesooriya R, Mishra V, Brand P, et al. COVID-19 and telehealth, education, and research adaptations. Pediatric Resp Rev 2020; 35: 38–42. doi.org/10.1016/j.prrv.2020.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Isasti G, Diaz Fernandez J.Comparison of telehealth and traditional face-to-face model during COVID-19 pandemic. Medicina Clinica (English Edition) 2020; 155(8): 361–362. doi: 10.1016/j.medcle.2020.06.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Womack C, Farsin R, Farsad M, et al. Emerging alternatives to conventional clinic visits in the era of COVID-19: Adoption of telehealth at VCU Adult Cystic Fibrosis Center. Int J Gen Med 2020; 13: 1175–1186. doi: 10.2147/IJGM.S274193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shigekawa E, Fix M, Corbett G, et al. The current state of telehealth evidence: a rapid review. Health Affairs 2018; 37: 1975–1982. doi.org/10.1377/hlthaff.2018.05132 [DOI] [PubMed] [Google Scholar]
- 9.Martinez K, Rood M, Jhangiani N, et al. Patterns of use and correlates of patient satisfaction with a large nationwide direct to consumer telemedicine service. J Gen Intern Med 2018; 33: 1768–1773. doi.org.10.1007/s11606-018-4621-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Andrews E, Berghofer K, Long J, et al. Satisfaction with the use of telehealth during COVID-19: An integrative review. Int J Nurs Stud Adv. Epub ahead of print 16 October 2020. doi: 10.1016/j.ijnsa.2020.100008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reed ME, Huang J, Parikh R, et al. Patient–provider video telemedicine integrated with clinical care: Patient experiences. Ann Intern Med 2019; 171(3): 222–224. doi.org/10.7326/M18-3081 [DOI] [PubMed] [Google Scholar]
- 12.Powell RE, Henstenburg JM, Cooper G, et al. Patient perceptions of telehealth primary care video visits. Ann Fam Med 2017; 15(3): 225–229. doi.org/10.1370/afm.2095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bashshur RL, Howell JD, Krupinski EA, et al. The empirical foundations of telemedicine interventions in primary care. Telemed e-Health 2016; 22(5): 342–375. doi.org/10.1089/tmj.2016.0045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sanyaolu A, Okorie C, Marinkovic A, et al. Comorbidity and its impact on patients with COVID-19. SN Comp Clin Med. Epub ahead of print 25 June 2020. doi: 10.1007/s42399-020-00363-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gallo Marin B, Aghagoli G, Lavine K, et al. Predictors of COVID-19 severity: A literature review. Rev Med Virol. Epub ahead of print 30 July 2020. doi: 10.1002/rmv.2146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stefan N, Birkenfeld AL, Schulze MB, et al. Obesity and impaired metabolic health in patients with COVID-19. Nat Rev Endocrin 2020; 23: 1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lauer SA, Grantz KH, Bi Q, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: Estimation and application. Ann Intern Med 2020; 172(9): 577–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lin CH, Tseng WP, Wu JL, et al. A double triage and telemedicine protocol to optimize infection control in an emergency department in Taiwan during the COVID-19 pandemic: Retrospective feasibility study. J Med Internet Res 2020; 22(6): e20586. doi: 10.2196/20586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu Z, McGoogan JM.Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020; 323: 1239–1242. doi:10.1001/jama.2020.2648 [DOI] [PubMed] [Google Scholar]
- 20.Greenhalgh T, Koh GC, Car J.Covid-19: A remote assessment in primary care. BMJ 2020; 368. doi.org/10.1136/bmj.m1182 [DOI] [PubMed] [Google Scholar]
- 21.Smith AC, Thomas . E, Snoswell CL, et al. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare 2020; 20: 1357633X20916567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Uscher-Pines L, Fischer S, Chari R.The promise of direct-to-consumer telehealth for disaster response and recovery. Prehosp Disaster Med 2016; 31(4): 454–456. doi: 10.1017/S1049023X16000558 [DOI] [PubMed] [Google Scholar]
- 23.Chakrabarti O.Telehealth: Emerging evidence on efficiency. Int Rev Econ Finance 2019; 60: 257–264. doi: 10.1016/j.iref.2018.10.021 [Google Scholar]
- 24.Halbert K, Bautista C.Telehealth use to promote quality outcomes and reduce costs in stroke care. Crit Care Nurs Clin North Am 2019; 31(2): 133–139. doi.org/10.1016/j.cnc.2019.02.001 [DOI] [PubMed] [Google Scholar]
- 25.Licurse A, Mehrotra A.The effect of telehealth on spending: Thinking through the numbers. Ann Intern Med 2018; 168(10): 737–738. doi: 10.7326/M17-3070 [DOI] [PubMed] [Google Scholar]
- 26.Ashwood JS, Mehrotra A, Cowling D.Direct-to-consumer telehealth may increase access to care but does not decrease spending. Health Affairs 2017; 36(3): 485–491. doi: 10.1377/hlthaff.2016.1130 [DOI] [PubMed] [Google Scholar]
- 27.Dorsey R, Topol E.State of telehealth. New Engl J Med 2016; 375: 154–161. doi: 10.1056/NEJMra1601705 [DOI] [PubMed] [Google Scholar]
- 28.Pariser P, Pham TN, Brown JB, et al. Connecting people with multimorbidity to interprofessional teams using telemedicine. Ann Fam Med 2019; 17(Suppl 1): S57–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Uscher-Pines L, Mulcahy A, Cowling D, et al. Access and quality of care in direct-to-consumer telemedicine. Telemed E-Health 2016; 22(4) :282–287. doi: 10.1089/tmj.2015.0079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Uscher-Pines L, Mehrotra A.Analysis of Teladoc use seems to indicate expanded access to care for patients without prior connection to a provider. Health Affairs 2014; 33: 258–264. doi.org/10.1377/hlthaff.2013.0989 [DOI] [PubMed] [Google Scholar]
- 31.Finkelstein SM, Speedie SM, Potthoff S.Home telehealth improves clinical outcomes at lower cost for home healthcare. Telemed E-Health 2006; 12(2): 128–136. doi: 10.1089/tmj.2006.12.128 [DOI] [PubMed] [Google Scholar]
- 32.Hopp F, Woodbridge P, Subramanian U, et al. Outcomes associated with a Home Care Telehealth Intervention. Telemed E-Health 2006; 12(3): 297–307. doi: 10.1089/tmj.2006.12.297 [DOI] [PubMed] [Google Scholar]
- 33.Srivastava A, Do J-M, Sales VL, et al. Impact of patient-centered home telehealth programme on outcomes in heart failure. J Telemed Telecare 2019; 25(7): 425–430. doi: 10.1177/1357633X18775852 [DOI] [PubMed] [Google Scholar]
- 34.Dansky KH, Vasey J, Bowles K.Impact of telehealth on clinical outcomes in patients with heart failure. Clin Nurs Res 2008; 17(3): 182–199. doi: 10.1177/1054773808320837 [DOI] [PubMed] [Google Scholar]
- 35.Gordon AS, Adamson WC, DeVries AR.Virtual visits for acute, nonurgent care: A claims analysis of episode-level utilization. J Med Internet Res 2017; 19(2): e35. doi: 10.2196/jmir.6783 [DOI] [PMC free article] [PubMed] [Google Scholar]