Abstract
Introduction
Routine diabetes care changed during the COVID-19 pandemic due to precautionary measures such as lockdowns, cancellation of in-person visits, and patients’ fear of being infected when attending clinics. Because of the pandemic, virtual clinics were implemented to provide diabetes care. Therefore, we conducted this study to assess the impact of these virtual clinics on glycaemic control among high-risk patients with type 2 diabetes mellitus (DM).
Methods
A prospective single-cohort pre-/post telemedicine care intervention study was conducted on 130 patients with type 2 DM attending a virtual integrated care clinic at a chronic Illness center in a family and community medicine department in Riyadh, Saudi Arabia during the COVID-19 pandemic.
Results
The mean age of the participants was 57 years (standard deviation (SD) = 12) and the mean (SD) duration of diabetes was 14 (7) years. Over a period of 4 months, the HbA1c decreased significantly from 9.98 ± 1.33 pre-intervention to 8.32 ± 1.31 post-intervention (mean difference 1.66 ± 1.29; CI = 1.43–1.88; P <0.001). In addition, most in-person care visits were successfully replaced, as most patients (64%) needed only one or two in-person visits during the 4-month period, compared with typically one visit every 1–2 weeks in the integrated care programme before the pandemic for this group of high-risk patients.
Discussion
The current study found a significant positive impact of telemedicine care on glycaemic control among high-risk patients with DM during the COVID-19 pandemic. Moreover, it showed that telemedicine could be integrated into diabetic care to successfully replace many of the usual in-person care visits. Consequently, health policy makers need to consider developing comprehensive guidelines in Saudi Arabia for telemedicine care to, ensure the quality of care and address issues such as financial reimbursement and patient information privacy.
Keywords: Telemedicine, uncontrolled diabetes mellitus, COVID-19, Saudi Arabia
Introduction
Coronavirus disease-2019 (COVID-19) has spread quickly across the globe,1–3 with more than 33 million confirmed cases as of 1 October 2020. 3 COVID-19 can lead to severe acute respiratory tract infection among infected individuals, especially patients with comorbidities. It can be transmitted from person to person through direct transmission (e.g. cough, sneeze, respiratory droplets), contact spread (i.e. contact with patients’ materials or human fluids) and contaminated surfaces (e.g. metal or glass surfaces contaminated with the virus). 4 , 5 Since December 2019, the rapid and exponential spread of this newly identified and highly contagious virus throughout the world has caused substantial morbidity and mortality, 3 , 6 , 7 with more than 1 million deaths as of October 2020. 3 The highly contagious nature of the virus and its propensity to disperse from person to person via respiratory droplets mean that the only option to curb its swift spread was to impose containment measures such as enforcing nationwide or local lockdowns, travel restrictions, social distancing, school shutdowns and the cancellation of in-person outpatient visits and reduced hospital/clinic schedules.8–11 These necessary and tough decisions to contain the virus, coupled with the high rate of infections, have inevitably affected healthcare systems and led to negative economic consequences. Patients with severe comorbidities such as diabetes have experienced a myriad of challenges due to the pandemic.12–14
The current evidence suggests that individuals with comorbidities such as diabetes mellitus (DM), hypertension, respiratory system diseases and severe obesity are at a higher risk of developing complications and fatalities in conjunction with COVID-19.15–17 For instance, a study conducted in Wuhan, China that analysed 26 fatal cases demonstrated that DM was found in 42.3% of fatalities due to COVID-19, and was the second most common disease found in COVID-19 patients after hypertension. 18 In addition, the Chinese Centre for Disease Control and Prevention published a report on 72,314 cases of COVID-19 that revealed an increased rate of fatality in patients with DM (7.3%) when compared with the overall mortality of 2.3%. 19 Likewise, a prospective cohort study conducted on COVID-19 patients from New York City reported that diabetes was prevalent among patients admitted to the hospital, with 34% of them having DM. 20
These findings from the literature indicate the need to provide comprehensive and holistic care to patients with DM, which might be challenging during the COVID-19 pandemic due to limited in-person care at outpatient clinics and patients’ fear of exposure risk. 21 Furthermore, care of patients with DM might be compromised because of the diversion of financial, material and human resources towards COVID-19. Some of the primary challenges for diabetes care during the pandemic could be limited access to health care, health education, routine laboratory investigations and medications; this could have worsened due to the COVID-19 lockdown. 12 These restriction measures have also affected the routine care of patients with DM, which, in turn, might result in uncontrolled glycaemia or worsening status of comorbid diseases in patients with DM, mainly among those with uncontrolled diabetes. 14 , 22
Like many countries, in Saudi Arabia, after detecting cases of COVID-19, total and partial lockdowns and other precautionary measures were implemented to prevent the spread of the virus and ensure the safety of the public. 10 As result of the COVID-19 pandemic, the routine management of patients with DM was affected, especially during the lockdown period. However, most of the health sectors in different countries have implemented alternative and effective strategies to overcome this challenge and to provide timely and effective care to such patients. 23 One of such strategy is the provision of health care using digital health or telemedicine platforms. 23 , 24 In Saudi Arabia, manyhospitals and health centres advocated the use of telemedicine to ensure that patients with DM receive the necessary health care in a timely and effective manner. However, the impact of such efforts has not been evaluated on the glycaemic control of patients with DM in Saudi Arabia. Hence, we undertook this study to determine the effect of a virtual integrated care clinic on glycaemic control among high-risk patients with type 2 DM at a chronic illness center in a family and community medicine department in Riyadh, Saudi Arabia.
Methods
Study design and setting
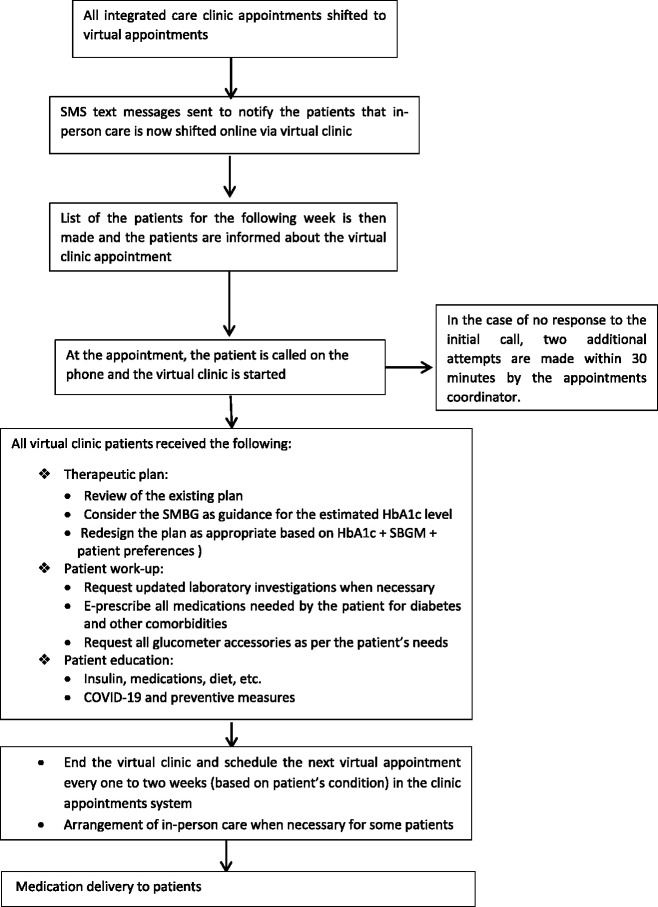
A prospective single-cohort pre-/post-intervention study was conducted on patients with type 2 DM attending a virtual integrated care clinic at a chronic illness center in a family and community medicine department at Prince Sultan Military Medical City in Riyadh, Saudi Arabia from March to June 2020. As the schedules of outpatient clinics including in-person care were largely reduced to a minimum during the pandemic, and because of the lockdown during the early phase of COVID-19, we shifted our integrated care clinic to be a virtual clinic to ensure the continuation of care to the patients with DM. Therefore, all appointments shifted to virtual clinical appointments. SMS text messages were sent informing all patients registered at the clinic that in-person visits to the clinic were cancelled and that the care would be provided as scheduled via the virtual clinic. The workflow of virtual integrated care clinic was discussed among the clinical team of the clinic and the department administration and then agreed upon to ensure smooth running of the clinic and smooth flow of patients (Figure 1). In addition, a guideline for type 2 diabetes management during the COVID-19 pandemic was established and distributed among the clinical team to unify the processes and management. Similar to the in-person integrated care clinic before the pandemic, the virtual clinic had the same clinical team including a senior family physician, clinical pharmacist, diabetic educator and other healthcare professionals. The patient’s medical record was thoroughly reviewed by the physician including medical history and recent laboratory investigations. Then, the patient was referred to the clinical pharmacist for appropriate medication counselling and therapeutic interventions based on the collaborative management plan (the clinical pharmacist is the case manager for the integrated care clinic). Additionally, during the virtual clinic on the same day, the patient was referred to the diabetic educator when needed (e.g. educating new patients about injection sites and technique, and to improve health literacy). Frequent virtual appointments every 1–2 weeks for reviewing the agreed plan and insulin titration was conducted by the case manager of the virtual clinic. The frequency of virtual appointments in integrated care for high-risk patients was scheduled to be similar to in-person visits before the pandemic, i.e. one appointment every 1–2 weeks in the first 3 months was arranged by the case manager. 25 , 26 In fact, this integrated care clinic was established several years before the pandemic to provide comprehensive in-person care with more frequent visits than standard care for high-risk patients with type 2 DM. Consequently, all patients with uncontrolled diabetes (i.e. HbA1c >9) were referred to this integrated clinic from the other chronic illness clinics at our medical centre to receive more specialized and more intensive care. Once their condition is controlled, the patients are referred back to the chronic illness clinics for standard care. 25 , 26
Figure 1.
Flow of the virtual integrated care clinic during COVID-19 pandemic.
At the date and time of appointments, the patients or their caregivers were called on the phone and provided with the appropriate care/consultation (Figure 1). This included a review of the therapeutic plan (i.e. reviewing the existing plan, redesigning the plan when needed based on HbA1c, self-monitoring of blood glucose (SMBG), patient preferences). In addition, the patients were e-prescribed all medications needed for their diabetes and other comorbidities, and all glucometer accessories needed by the patients were requested. Moreover, when necessary, laboratory investigations (e.g. HbA1c) were requested electronically and submitted to the laboratory department. During the virtual clinic, in addition to patient counselling on their medications and dose adjustments, patients were educated about the risk of COVID-19 to patients with DM, and about the importance of precautionary measures such as wearing masks, frequent hand washing, social distancing and avoiding crowded places where the risk of infection is high. Furthermore, to ensure understanding, before ending the virtual appointment, patients or their caregivers were asked to read back the key messages such as medications, doses, frequency, type of insulin, etc. Moreover, when needed, the patient or their caregiver was sent a message via WhatsApp with new dosage instructions, dose modifications, added or stopped medications for further confirmation to ensure patient safety. Then, the prescribed medications and other items (e.g. test strips) were shipped by the medication delivery service at the clinic to the patient’s postal address. During the virtual clinic, all patient interventions and results were recorded in the clinic’s electronic system. In addition, virtual appointments every 1–2 weeks were scheduled based on the patient’s condition and entered in the clinic appointments system.
In this model of the virtual clinic, we used phone calls to communicate with the patients. In addition, WhatsApp was used for providing written instructions, educational materials, audio-visual aids, etc. SMS text messages were also used. During the virtual clinic, for example, the patients or their caregivers were asked to read the SMBG readings (e.g. SMBG readings before breakfast, after 2 hours of each meal). If there is any difficulty in reviewing virtually the SMBG readings, the patients were asked to send them through WhatsApp. This was helped by the fact that the patients at our integrated care clinic were provided with a SMBG booklet to record their SMBG readings as part of our programme before the pandemic. One of the challenges was the patients who would start taking insulin injections. In this case, the educational materials including audio-visual aids were sent by WhatsApp to the patient or the caregiver, with frequent follow-ups to ensure all things are done in an appropriate way. Otherwise, when it was not possible for some cases or virtual education was not effective, an in-person appointment to the clinic was arranged. Moreover, it should be noted that patients with a deteriorating condition that required further investigation (e.g. updated HbA1c) or further essential interventions, were provided with permission to visit the clinic for further care. In addition, for specific groups of patients (e.g. those with mental illness, dementia, illiteracy, etc.), the engagement of family members was arranged during the virtual clinic. A summary of the virtual clinic workflow is summarized in Figure 1.
Population and inclusion and exclusion criteria
We included all adult patients with type 2 DM having an HbA1c value >9 before the pandemic began and with a valid HbA1c value after attending the virtual integrated care clinic for about 3–4 months during the COVID-19 pandemic. We excluded all patients aged <18 years and those with HbA1c values <9 at baseline. We also excluded all patients with no HbA1c values after attending the virtual integrated care clinic. Consequently, based on these criteria, we included 130 patients in this study. The duration of type 2 DM, comorbidities, medication history and any change in medication after attending the virtual integrated care clinic were all recorded.
Ethical approval
The study received ethical approval from the Central Research Ethics Committee of Medical Services General Directorate (CREC-MSD). All information was taken from patient records after obtaining verbal and written consent from the patients.
Statistical analysis
Descriptive analyses are reported using mean and standard deviation (SD) for continuous variables and frequency and percentage for categorical variables. A paired t-test was used to report the changes in pre- and post-intervention HbA1c. A p-value less than 0.05 was considered statistically significant.
Results
Patient characteristics
The mean age (SD) of participants was 57 ± 12.0 years, and the mean (SD) time since the original diagnosis of diabetes was 14 ± 7 years. The HbA1c value pre-enrolment in the virtual clinic was 9.98 ± 1.33. Moreover, the most common comorbidities were dyslipidemia (89%), hypertension (70%), cardiovascular diseases (15%), hypothyroidism (15%), chronic kidney diseases (5%) and cerebrovascular diseases (2%).
Therapeutic interventions and dose adjustment during the virtual clinic
With respect to medications, pre-enrolment in the virtual integrated care clinic, 13.8% of patients were on 30% soluble insulin aspart/protamine–crystallized insulin aspart 70%, 43.8% were using insulin glargine, 43.8% were on aspart insulin and 8.5% were using insulin glargine only. The majority of the participants (84.6%) were taking metformin. Furthermore, 30% of participants were using gliclazide, 46% of patients were using vildagliptin, 11.5% were taking liraglutide, and 1.5% of patients were taking pioglitazone. Upon follow-up during the virtual clinic, insulin doses were increased among a considerable portion of patients to manage their uncontrolled diabetes as part of the integrated care programme protocol. In addition, several dosage adjustments and medication interventions were made based on the clinical condition of the patients (Table 1).
Table 1.
Therapeutic Interventions and medication dose adjustment during the virtual clinic.
| Medication | Frequency | Percentage |
|---|---|---|
| Metformin | ||
| Intervention and dose adjustment (=111) | ||
| No change | 97 | 87.4% |
| Decrease | 3 | 2.7% |
| Increase | 9 | 8.18% |
| Add on | 1 | 1% |
| Stop | 1 | 1% |
| Gliclazide | ||
| Intervention and dose adjustment (=39) | ||
| No change | 29 | 74.4%% |
| Increase | 7 | 17.9% |
| Stop | 3 | 7.7% |
| Liraglutide | ||
| Intervention and dose adjustment (n=17) | ||
| No change | 5 | 29.4% |
| Increase | 9 | 52.9% |
| Add on | 2 | 11.8% |
| Stop | 1 | 5.9% |
| Pioglitazone | ||
| Intervention and dose adjustment (n=3) | ||
| No change | 2 | 66.7% |
| Add on | 1 | 33.3% |
| Vildagliptin | ||
| Intervention and dose adjustment (n=63) | ||
| No change | 47 | 74.6% |
| Increase | 12 | 19 % |
| Add on | 3 | 4.8% |
| Stop | 1 | 0.8% |
| 30% soluble insulin aspart/protamine-crystallized insulin aspart 70% | ||
| Intervention and dose adjustment (n= 18) | ||
| Same | 4 | 22% |
| Increase | 14 | 78 % |
| Insulin NPH/Regular insulin (70/30) | ||
| Intervention and dose adjustment (n=2) | ||
| Increase | 1 | 50 % |
| Add on | 1 | 50 % |
| insulin glargine only | ||
| Intervention and dose adjustment (n=14) | ||
| Increase | 11 | 78.6% |
| Add on | 3 | 21.4% |
| insulin glargine | ||
| Intervention and dose adjustment (n=58) | ||
| No change | 3 | 5.2% |
| Decrease | 2 | 1.5% |
| Increase | 52 | 40% |
| Add on | 1 | 1.7% |
| Aspart insulin | ||
| Intervention and dose adjustment ((n=60) | ||
| No change | 1 | 1.7% |
| Decrease | 3 | 5% |
| Increase | 52 | 86.7% |
| Add on | 3 | 5% |
| Stop | 1 | 1.7% |
Impact of the virtual clinic on glycaemic control
The impact of the virtual clinic on glycaemic control (i.e. HbA1c levels) was assessed before and after telemedicine care. The HbA1c significantly decreased from 9.98 ± 1.33 pre-intervention to 8.32 ± 1.31 post-intervention (mean difference 1.66 ± 1.29 (CI = 1.43–1.88), p < 0.001).
Impact of the virtual clinic on the number of in-person care visits
The need for in-person care visits was assessed during telemedicine care. Typically, before the pandemic, one visit every 1–2 weeks was needed for this high-risk group of patients with DM in the integrated care programme. The frequency of in-person care visits that were necessary to complement virtual clinic appointments were greatly decreased (Figure 2). For most patients (64%), only one or two visits were needed during the 4-month study period.
Figure 2.

The number of in-person visits during the 4-month period
Discussion
We undertook the current study in Saudi Arabia to assess the impact of an integrated care virtual clinic on glycaemic control among high-risk patients with type 2 DM having an HbA1c level >9. The enrolled patients in the study had a baseline HbA1c of approximately 10, and the vast majority of patients were suffering from other comorbidities such as dyslipidemia and hypertension. Despite this, the findings of this study demonstrate a significant difference in HbA1c after the virtual clinic, with a reduction in HbA1c by 1.66 points on average. Moreover, telemedicine care successfully decreased the need for in-person care visits. Typically, before the pandemic, one visit every 1–2 weeks was needed for this high-risk group of patients with DM in our intensified integared care program. In this study, most patients (64%) needed only a few in-person visits, and only approximately 20% required more frequent visits (i.e. four or more visits in a period of 4 months), still fewer than the number of visits before the pandemic. Consequently, telemedicine not only helped with glycaemic control, but has managed to reduce the risk of exposure to infection by having a minimal number of visits. This in turn indicates that telemedicine has a role in the clinical care of patients with DM. Moreover, the patient response to telemedicine services was encouraging. In fact, overall, 87.5% of patients answered the calls and attended the virtual clinics at our hospital during the period from March to June 2020, based on the statistics of the appointment department at our institution. 27
Our findings regarding the impact of telemedicine care on improving the outcomes of patients with DM is consistent with other studies reported in the literature. 28 , 29 For instance, one of the largest studies conducted to investigate the effect of telemedicine on DM outcomes is the Informatics for Diabetes Education and Telemedicine project that included 1665 patients. This randomized controlled trial compared the outcomes of DM patients provided with telemedicine care with DM patients not enrolled in telemedicine system. 30 The study participants in this project showed improvements in glycaemic control, blood pressure readings and cholesterol levels after following the participants for 1 year. 30 Moreover, our findings regarding the reduction in HbA1c levels after virtual care are in line with the findings of a systematic review and meta-analysis that included 35 randomized controlled trials on the effect of various telemedicine approaches (e.g. phone calls, text messages, video conferencing, web-based systems) on glycaemic control in patients with type 2 DM. The findings of the meta-analysis showed that telemedicine over 3–60 months had a significant reduction in HbA1c by −0.37% in the telemedicine group as compared with the controls. 31 Moreover, the findings of a Cochrane review by Flodgren and colleagues reported a significantly lower HbA1c levels in patients allocated to telemedicine than in controls (median = –0.31, 95% CI –0.37 to –0.24; p < 0.00001) at a median of 9 months of follow-up. 32 Similarly, a recent umbrella review of systematic reviews and meta-analyses was conducted to assess the effectiveness of telemedicine on clinical outcomes in patients with chronic conditions including DM. 33 This comprehensive review showed that there were clinically significant improvements in HbA1c levels in patients with DM who received telemedicine care. 33
Overall, our study findings along with the published literature before the pandemic provide evidence that telemedicine was a very useful tool for physicians and other healthcare professionals to provide services, follow-up and treatment to their patients with DM during lockdown in the COVID-19 pandemic. We have successfully shifted our in-person integrated care programme to a virtual clinic to ensure continuity of care to our patients with DM, although this was initially thought to be challenging, especially in this type of patient given their uncontrolled diabetes and the level of interventions needed (Table 1) such as the intensification of insulin treatment. 25 , 26
We believe the way forward to further expand telemedicine care in Saudi Arabia includes addressing several issues. For example, the health institution and healthcare professionals need to ensure the privacy of patients during telecommunication with their patients. In addition, it is expected that, after the pandemic is over, as many patients are currently more familiar with these telemedicine services and healthcare professionals are increasingly using telemedicine technologies, there will be a huge demand for telemedicine by both patients and healthcare professionals. 24 , 34 , 35 Hence, we believe that there is currently a need for national comprehensive guidelines for telemedicine care in Saudi Arabia. This will help to provide guidance and better promote telemedicine care for patients, healthcare professionals and healthcare institutions, and to address issues related to patient privacy (i.e. acceptable telecommunication systems and platforms for telemedicine, security features of platforms, etc.) and financial reimbursement. 36
Implications for practice
Telemedicine was effective at providing appropriate care for patients with DM, especially when in-person usual care was not possible during the COVID-19 pandemic. A virtual clinic can be recommended as a practical solution in this time of crisis. However, based on our experience, several factors should be considered for a successful virtual clinic. First, we believe a good arrangement and coordination with the health facility is essential for the success of the virtual clinic. This includes good coordination via a written workflow of the virtual clinic among healthcare professionals (i.e. the physician, the clinical pharmacist, the dietitian, etc.) and the relevant departments (e.g. the appointment department, laboratory department, pharmacy, medications delivery services, etc.). Second, it is important to categorize patients based on the status of their condition (i.e. triage). This is because the condition of some high-risk patients could deteriorate and need urgent intervention, as any further delay could lead to further complications. In addition, some patients, for example new patients with DM or patients that are prescribed new medications that need special training (e.g. insulin injections), need to be trained to ensure safe and appropriate use. Accordingly, via the remote assessment in the virtual clinic, an in-person appointment for this category of patients can be arranged (e.g. to have a lab investigations or essential training, etc.) and their access to immediate care can be granted. Hence, the majority of patients can appropriately receive the required care online, while the rest can be provided with access to in-person care. Third, it is important to note that some patients (e.g. patients with mental disorders or dementia) need additional arrangements, including the engagement of a family member or caregiver.
Strengths and limitations
To our knowledge, this is one of the first studies of its kind to assess the effect of telemedicine on glycaemic control in patients with DM in Saudi Arabia during the COVID-19 pandemic. In addition, we used objective measures such as HbA1c before and after virtual integrated care to assess the impact of telemedicine care. However, this study has some limitations. First, we did not randomize patients to telemedicine; rather we performed a pre–post telemedicine care study that might not have controlled for unknown confounders. In addition, we could not control for other important factors such as health consciousness or health-seeking behaviour of the patients with DM to isolate the effect of integrated care on glycaemic control. Moreover, we followed patients for a relatively short period of time and could not assess the effect of telemedicine in the long term. However, we believe that our findings could provide further guidance to policy makers for the management of patients with DM, especially during pandemics. Moreover, future research could assess the cost-effectiveness of telemedicine to be implemented as a strategy to replace many of the usual in-person care visits and to reach remote areas and in resource-limited settings for patients with chronic diseases such as DM.
Conclusion
The current study found a significant positive effect of telemedicine care on glycaemic control among high-risk patients with DM during the COVID-19 pandemic. Moreover, it showed that telemedicine could be integrated into the diabetic care to successfully replace many of the usual in-person care visits. In addition, health policy makers need to consider developing comprehensive guidelines in Saudi Arabia to promote best practice of telemedicine to ensure the quality of care, and address issues such as financial reimbursement and patient information privacy.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Alian A Alrasheedy https://orcid.org/0000-0003-3617-7425
References
- 1.Chen Y, Liu Q, Guo D.Emerging coronaviruses: Genome structure, replication, and pathogenesis. J Med Virol 2020; 92: 418–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tu H, Tu S, Gao S, et al. The epidemiological and clinical features of COVID-19 and lessons from this global infectious public health event. J Infect2020; 81(1): 1–9. [DOI] [PMC free article] [PubMed]
- 3.WHO. WHO Coronavirus Disease (COVID-19) Dashboard 2020. [cited 2020 20 September 2020]. Available from: https://covid19.who.int/.
- 4.Khurshid Z, Asiri FYI, Al Wadaani H.Human saliva: Non-invasive fluid for detecting novel coronavirus (2019-nCoV). Int J Env Res Public Health 2020; 17: 2225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peng X, Xu X, Li Y, et al. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci 2020; 12: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nishiura H, Jung SM, Linton NM, et al. The extent of transmission of novel coronavirus in Wuhan, China, 2020. J Clin Med 2020; 24: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khachfe HH, Chahrour M, Sammouri J, et al. An epidemiological study on COVID-19: A rapidly spreading disease. Cureus 2020; 12: e7313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peng F, Tu L, Yang Y, et al. Management and treatment of COVID-19: The Chinese experience. Can J Cardiol 2020; 36(6): 915–930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ibrahim RL, Ajide KB, Olatunde JO.Easing of lockdown measures in Nigeria: Implications for the healthcare system. Health Policy Technol 2020; 9: 399–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alumran A.Role of precautionary measures in containing the natural course of novel coronavirus disease. J Multidiscip Healthc 2020; 13: 615–620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Castle JR, Rocha L, Ahmann A.How COVID-19 rapidly transformed clinical practice at the Harold Schnitzer Diabetes Health Center now and for the future. J Diabetes Sci Technol 2020; 14: 721–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gupta R, Hussain A, Misra AJEjocn.Diabetes and COVID-19: Evidence, current status and unanswered research questions. Eur J Clin Nutr 2020; 74: 864–870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bloomgarden ZT. Diabetes and COVID-19. J Diabetes2020; 12: 347–348. [DOI] [PubMed]
- 14.Banerjee M, Chakraborty S, Pal R.Teleconsultation and diabetes care amid COVID-19 pandemic in India: Scopes and challenges. J Diabetes Sci Technol 2020; 14: 714–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Apicella M, Campopiano MC, Mantuano M, et al. COVID-19 in people with diabetes: Understanding the reasons for worse outcomes. Lancet Diabetes Endocrinol 2020; 8: 782–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang J, Zheng Y, Gou X, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: A systematic review and meta-analysis. Int J Infect Dis 2020; 94: 91–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ceriello A, Schnell O.COVID-19: Considerations of diabetes and cardiovascular disease management. J Diabetes Sci Technol 2020; 14: 723–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deng S-Q, Peng H-J.Characteristics of and public health responses to the coronavirus disease 2019 outbreak in China. J Clin Med 2020; 9: 575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu Z, McGoogan JM.Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020; 323: 1239–1242. [DOI] [PubMed] [Google Scholar]
- 20.Cummings MJ, Baldwin MR, Abrams D, et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: A prospective cohort study. Lancet 2020; 395(10239): 1763–1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nachimuthu S, Vijayalakshmi R, Sudha M, et al. Coping with diabetes during the COVID–19 lockdown in India: Results of an online pilot survey. Diabetes Metab Syndr 2020; 14: 579–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bonora BM, Boscari F, Avogaro A, et al. Glycaemic control among people with type 1 diabetes during lockdown for the SARS-CoV-2 outbreak in Italy. Diabetes Ther 2020: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ghosh A, Gupta R, Misra AJD.Telemedicine for diabetes care in India during COVID19 pandemic and national lockdown period: Guidelines for physicians. Diabetes Metab Syndr 2020; 14: 273–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ahn DT.The COVID-19 pandemic: A “tech”-tonic shift toward virtual diabetes care. J Diabetes Sci Technol 2020; 14: 708–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tourkmani AM, Abdelhay O, Alkhashan HI, et al. Impact of an integrated care program on glycemic control and cardiovascular risk factors in patients with type 2 diabetes in Saudi Arabia: An interventional parallel-group controlled study. BMC Family Pract 2018; 19: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Al Asmary SM, Tourkmani AM, Al Khashan HI, et al. Impact of integrated care program on glycemic control and cardiovascular risk in adult patients with type 2 diabetes. J Clin Outcomes Manage 2013; 20: 356–363. [Google Scholar]
- 27.KPIs. The Chronic Illness Center (CIC), Department of Community and Family Medicine, Prince Sultan Medical center , Riyadh, Saudi Arabia. [Google Scholar]
- 28.Krishna S, Boren SAJJods, technology. Diabetes self-management care via cell phone: A systematic review. J Diabetes Sci Technol 2008; 2: 509–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Klonoff DC.Using telemedicine to improve outcomes in diabetes—an emerging technology. J Diabetes Sci Technol 2009; 3: 624–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shea S, Weinstock RS, Starren J, et al. A randomized trial comparing telemedicine case management with usual care in older, ethnically diverse, medically underserved patients with diabetes mellitus. J Am Med Inform Assoc 2006; 13: 40–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhai Y-K, Zhu W-J, Cai Y-L, et al. Clinical-and cost-effectiveness of telemedicine in type 2 diabetes mellitus: A systematic review and meta-analysis. Medicine 2014; 93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Flodgren G, Rachas A, Farmer AJ, et al. Interactive telemedicine: Effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2015; (9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Timpel P, Oswald S, Schwarz PE, et al. Mapping the evidence on the effectiveness of telemedicine interventions in diabetes, dyslipidemia, and hypertension: An umbrella review of systematic reviews and meta-analyses. J Med Internet Res 2020; 22: e16791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Klonoff DC.Telemedicine for diabetes after the COVID-19 pandemic: We can’t put the toothpaste back in the tube or turn back the clock. J Diabetes Sci Technol 2020; 14: 741–742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Klonoff DC.The coronavirus 2019 pandemic and diabetes: An international perspective. J Diabetes Sci Technol 2020; 14: 703–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thomas EE, Haydon HM, Mehrotra A, et al. Building on the momentum: Sustaining telehealth beyond COVID-19. J Telemed Telecare 2020. doi:10.1177/1357633X20960638. [DOI] [PubMed] [Google Scholar]