Abstract
Purpose
While corneal transplantation is known to have a potential risk of transmission of variant Creutzfeldt-Jacob Disease (vCJD), the magnitude of this risk has not been quantified.
Observations
A case report is presented of a 73 year-old man with a penetrating keratoplasty graft from corneal tissue that was recalled after transplantation due to risk of vCJD because it was later discovered that the donor had traveled to the United Kingdom (UK). Probabilities of vCJD transmission were extrapolated using Creutzfeldt-Jacob Disease (CJD) mortality (incidence) rate, all-cause death rate, and rate of recovery for intended transplantation.
Conclusions
An overestimate of the risk of transplanting a cornea infected with vCJD in 2018 was 1 in 940,000. The true risk of vCJD transmission would be even lower due to an incomplete infectivity rate. We conclude that the risk of transmission of latent vCJD by corneal transplantation from a donor who traveled to the UK from 1980 to 1996 is exceedingly low.
Keywords: Variant Creutzfeldt-Jakob disease, Corneal transplantation, Risk assessment
1. Introduction
Prion disease occurs when the cellular prion protein (PrPc), a cell surface receptor protein, undergoes conformational change to scrapie prion protein (PrPsc). The misfolded PrPsc form aggregates in neural tissue and can propagate causing devastating neurologic damage known as transmission spongiform encephalopathy. The transmission spongiform encephalopathies are most commonly sporadic (sCJD), but 10% of cases are familial (fCJD), and variant disease (vCJD) is rare.1 vCJD refers to prion disease acquired by consumption of beef from cattle infected with bovine spongiform encephalopathy (BSE), a neurodegenerative disease of cattle that emerged in the late 1980s in the UK. This outbreak led the European Union to ban the export of British beef worldwide from 1996 to 2006, but people residing in the UK may have consumed infected beef before this time when the causal relationship between BSE and vCJD was not understood.2
According to the medical standards of the Eye Bank Association of America (EBAA), persons who spent three months or more cumulatively in the United Kingdom from 1980 to 1996 are ineligible to donate eye tissue due to the risk of transmission of variant Creutzfeldt-Jakob Disease (vCJD). This risk exists because vCJD can have a latency period (average of 11–12 years) between the time of infection and the time of presenting symptoms. Last updated in 2014, the Donor Risk Assessment Interview (DRAI) also has addenda to exclude tissue from donors with history of travel to regions with endemic Ebola and Zika virus transmission. The aforementioned exclusion criteria regarding travel to the UK between 1980 and 1996 is the only uniform travel screening criteria on the DRAI still in effect from prior to 2014.3 Only about 1.2–1.6% of the approximately 32,000 corneas in 2018 intended for transplant but not released were rejected due to travel history, and postoperative recalls due to travel history audits are rare.4
2. Case report
A 73 year-old male with blurry vision in his left eye and no significant past medical history had phacoemulsification cataract surgery. The cataract surgery was complicated by posterior capsule rupture with retained lens fragments. He underwent multiple additional surgeries including pars plana vitrectomy and epiretinal membrane peel. The post-operative course was further complicated by cystoid macular edema and corneal edema secondary to pseudophakic bullous keratopathy. He subsequently underwent successful penetrating keratoplasty for his left eye. Three months after the surgery, the eye bank recalled the corneal tissue transplanted in this patient due to eligibility concerns for the donor tissue.
Eligibility screening for corneal donation is performed, in part, through the DRAI questionnaire. This donor's family reported on the DRAI that the donor had visited Scotland for an unknown period of time. A quality-control audit performed subsequent to release of tissue and subsequent to use for transplantation revealed that the donor had lived in Scotland for more than two years during the 1990s. The key question in this case was: What is the risk of this patient developing vCJD due to this corneal transplant tissue?
3. Discussion
Martheswaran et al. described a method of approximating the number of corneas from donors with latent CJD recovered for intended transplant in a given year.5 First they divided the United States (U.S.) population into cohorts by decades of age. Then CJD mortality data (an approximate of incidence) for a given cohort was multiplied by 10 years to approximate the prevalence within that cohort. The prevalence estimate was then multiplied by the all-cause death rate for that age cohort to approximate the number of deceased donors with latent CJD, and that value was doubled (two corneas per donor) to arrive at the number of infected corneas. Finally, that figure was multiplied by a factor specific to each age group representing the probability that a given cornea would be recovered for intended transplant from that age group. Using this methodology, they predicted that there were 3.8 corneas expected to be infected with latent CJD recovered for intended transplant in 2018 for all age groups combined. When these same calculations were aggregated across all age groups and across all years from 1979 to 2018, they estimated that 47 CJD-infected corneas have entered the donor pool. Only five actual documented cases were believed to cause infection in the recipient, suggesting that the infectivity rate may be as low as 10.6%.
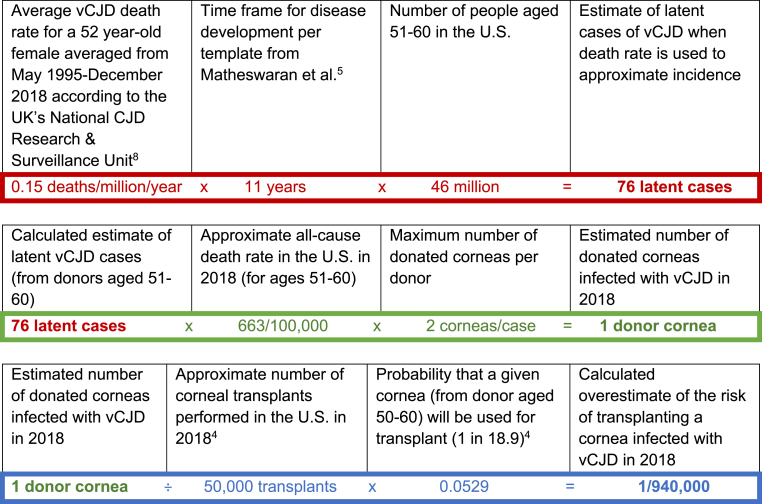
We performed a similar calculation (Fig. 1) for the risk of vCJD transmission by transplant with a cornea from a 52 year-old female donor with history of time spent in the UK as in the case presented in this report. According to the National CJD Research & Surveillance Unit in the UK, the average vCJD death rate for a 52 year-old female has been 0.15 deaths/million/year averaged from May 1995-December 2, 018.6 This incidence would overestimate the risk for U.S. donors because this figure includes a population that resides in the UK (rather than visitation from the U.S.) and present incidence of vCJD is considerably less than it was in the late 1990s and early 2000s. We used this figure to overestimate the number of corneas from donors with latent vCJD that have been recovered for intended transplant in a given year. These calculations suggest that an overestimate of the risk of transplanting a cornea infected with vCJD in 2018 was 1 in 940,000. The true risk of vCJD transmission would be even lower due to the incomplete infectivity rate. Note that these calculations are limited by the use of some population averages (e.g. death rates, number of corneal transplants performed) which can change with time and the use of average disease latency which may have significant variability across individuals.
Fig. 1.
Overestimated Risk of vCJD Transmission via Corneal Transplantation in 2018. Calculations to find the risk of vCJD transmission by transplant with a cornea from a 52 year-old female donor with history of time spent in the UK.
After literature review and analysis as discussed above, the patient was counseled that his probability of contracting vCJD from corneal transplantation was exceedingly low. The decision was made not to explant the corneal graft from this patient. Besides the risk of infection transmission, other variables that we considered included the age of the patient (at age 73, the patient was not concerned about a low risk of a disease with a 10+ year latency), ocular comorbidities that might complicate additional ocular surgery (he had multiple prior ocular surgeries), and the timing of recall following the transplant surgery (his corneal transplant was healing well at 3 months post-surgery when the recall occurred). Because of this exceedingly low probability of transmission of vCJD and because there are no effective treatments for CJD aside from supportive care, the burdens of additional testing for the patient far outweigh any benefits that early diagnosis would provide. These burdens include time and discomfort of testing to the patient, financial costs to the healthcare system, and psychological stresses associated with the testing. However, providers for this patient should have CJD within their differential diagnosis if the patient develops signs/symptoms of CJD in the future, such as altered mental status or hyperreflexia. While definitive diagnosis can only be made with brain biopsy, supplemental testing that may aid in the diagnosis of suspected CJD includes electroencephalogram, lumbar puncture, and magnetic resonance imaging of the brain. As of the publication of this report, the patient has not experienced any neurologic sequelae to raise suspicion for acquired vCJD. Our analysis is limited to a theoretical calculation of risk based on empirical population-based data. Unfortunately (or thankfully), there are no confirmed cases of vCJD transmission via corneal transplantation for evaluation of outcomes analysis.
PrPsc has not been directly detected by biochemical or immunohistochemical means in corneal tissue and penetrating keratoplasty performed in guinea pigs and non-human primates with CJD have not been shown to result in transmission of the disease.7 However, there have been two confirmed cases of CJD transmission resulting in death in humans through corneal transplantation with diagnosis of CJD confirmed by autopsy in both the patient and the donor.5 There have been eight other cases worldwide in which CJD transmission through corneal transplant has been suspected, with an average incubation period of 8–12 months. There have been no reported cases of CJD transmission through corneal transplantation since 2006 and none of the ten cases mentioned prior were suspected to involve vCJD.
Rates of vCJD in the UK and around the world have been declining since about 2000. There have been approximately 180 confirmed cases of vCJD in the UK and an additional 50 cases in the rest of the world. The last known death from vCJD was in the UK in 2016, although a researcher in France died from vCJD in 2019 after accidently inoculating herself with contaminated tissue.8,9 Only four cases of vCJD have ever been identified in the U.S. and only two of those individuals had prior travel to the UK. The other two cases were believed to originate in the Middle East, or possibly Russia.10 There have been more recent confirmed outbreaks of BSE in Wales (2013) and in Scotland (2018). While BSE outbreaks are monitored closely due to their potential to evolve into outbreaks of vCJD, there have been no records of associated human infection in these cases.
4. Conclusions
The risk of transmission of latent vCJD by corneal transplantation from a donor who traveled to the UK from 1980 to 1996 is exceedingly low. While this tissue recall placed a burden on the patient and physicians to understand the risk involved, the data summarized here may guide others encountering or studying this problem.
Patient consent
Written informed consent for publication was obtained from the patient described in this case report.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments & disclosures
No funding was received for the production of this report. The authors declare no conflicts of interest regarding the publication of this article. This material is the result of work supported with resources and the use of facilities at the VA Western New York Healthcare System. The contents do not represent the views of the U.S. Department of Veterans Affairs or the United States Government. All authors attest that they meet the current ICMJE criteria for authorship. Acknowledgements: None.
Contributor Information
Jeffrey Desilets, Email: jdesilet@buffalo.edu.
Abhiniti Mittal, Email: abhiniti@buffalo.edu.
John A. Sellick, Jr., Email: jsellick@buffalo.edu.
Sangita P. Patel, Email: sppatel@buffalo.edu.
References
- 1.Geschwind M.D. Prion diseases. Continuum. 2015;21(6 Neuroinfectious Disease):1612–1638. doi: 10.1212/CON.0000000000000251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beck M., Kewell B., Asenova D. BSE crisis and food safety regulation: a comparison of the UK and Germany. The York Management School Working Papers. 2007;38 [Google Scholar]
- 3.Uniform Donor Risk Assessment Interview Donor greater than 12 Years old [American association of tissue banks]. September 10. 2014. https://www.aatb.org/standards/uniform-drai Available at:
- 4.Eye Banking statistical report [Eye Bank association of American (EBAA)]. 2020. 2019. https://restoresight.org/wp-content/uploads/2020/04/2019-EBAA-Stat-Report-FINAL.pdf Available at:
- 5.Martheswaran T., Desautels J.D., Moshirfar M., et al. A contemporary risk analysis of iatrogenic transmission of creutzfeldt-jakob disease (CJD) via corneal transplantation in the United States. Ophthalmol Ther. 2020;9(3):465–483. doi: 10.1007/s40123-020-00272-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Creutzfeldt-jakob disease surveillance in the UK [the national CJD Research & surveillance unit] 2018. https://www.cjd.ed.ac.uk/sites/default/files/report27.pdf Available at:
- 7.Armitage W.J., Tullo A.B., Ironside J.W. Risk of Creutzfeldt-Jakob disease transmission by ocular surgery and tissue transplantation. Eye. 2009;23(10):1926–1930. doi: 10.1038/eye.2008.381. [DOI] [PubMed] [Google Scholar]
- 8.The National CJD Research & Surveillance Unit (NCJDRSU) Creutzfeldt-jakob disease in the UK. 2020. https://www.cjd.ed.ac.uk/sites/default/files/figs.pdf Available at:
- 9.Brandel J.P., Vlaicu M.B., Culeux A., et al. Variant creutzfeldt-jakob disease diagnosed 7.5 Years after occupational exposure. N Engl J Med. 2020;383(1):83–85. doi: 10.1056/NEJMc2000687. [DOI] [PubMed] [Google Scholar]
- 10.vCJD cases reported in the US [centers for disease control and prevention] Oct. 9, 2018. https://www.cdc.gov/prions/vcjd/vcjd-reported.html Available at: