Abstract
Background
Inter-recti distance (IRD) measurement using musculoskeletal USI has been used in physiotherapy research, in particular, to investigate pregnancy-related diastasis recti abdominis (DRA) and to seek its effective treatment methods. Severe and untreated diastasis may result in the formation of umbilical or epigastric hernias.
Objective
This study aimed to systematically map physiotherapy-related research articles that included descriptions of IRD measurement procedures using USI to present their similarities and differences, and formulate recommendations on the procedure.
Design
A scoping review was conducted according to PRISMA-ScR guidelines, including 49 of 511 publications from three major databases. Publications were selected and screened by two independent reviewers whose decisions were consulted with a third reviewer. The main synthesized data items were: the examinees’ body position, breathing phase, measurement sites, and DRA screening methods. The final conclusions and recommendations were the result of a consensus between seven reviewers from four research centers.
Results
Studies used 1–5 measurement sites that were differently determined. IRD was measured at the umbilicus (n = 3), at its superior (n = 16) and/or inferior border (n = 9), and at different levels: between 2 and 12 cm above the umbilicus, or a third of the distance and halfway between the umbilicus and xiphoid (n = 37); between 2 and 4.5 cm below the umbilicus or halfway between the umbilicus and pubis (n = 27). Different approaches were used to screen subjects for DRA.
Conclusions
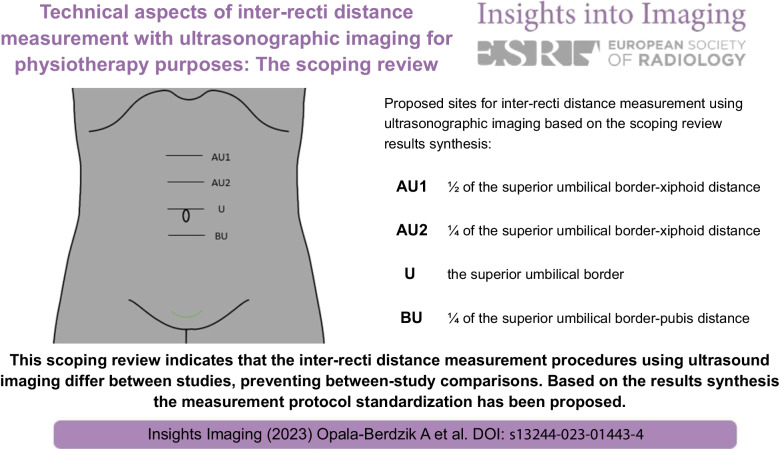
The discrepancies between the measurement procedures prevent between-study comparisons. The DRA screening method should be standardized. IRD measurement protocol standardization has been proposed.
Critical relevance statement
This scoping review indicates that the inter-recti distance measurement procedures using ultrasound imaging differ between studies, preventing between-study comparisons. Based on the results synthesis, the measurement protocol standardization has been proposed.
Key points
The inter-recti distance measurement procedures using USI differ between studies.
Proposed standardization concerns body position, breathing phase, measurements number per location.
Determination of measurement locations considering individual linea alba length is suggested.
Recommended locations: umbilical top, ½ of umbilical top-xiphoid, ¼ of umbilical top-xiphoid/pubis distances.
Diastasis recti abdominis diagnostic criteria are needed for proposed measurement locations.
Graphical Abstract
Supplementary Information
The online version contains supplementary material available at 10.1186/s13244-023-01443-4.
Keywords: Linea alba, Inter-recti distance, Diastasis recti abdominis, Ultrasonographic imaging, Measurement procedure
Introduction
Musculoskeletal ultrasonographic imaging (USI) has become a valuable tool in physiotherapy research and practice [1–5]. Among others, it has been used to measure the width of the fibrous linea alba, also called the inter-recti distance (IRD) [6, 7]. The most common purpose of this measurement is to investigate pregnancy-related diastasis recti abdominis (DRA) or monitor the impact of specific exercises on this condition [8–13]. DRA mostly develops in advanced pregnancy and manifests itself as an overstretched linea alba leading to the excessive separation of the recti abdominis muscles. In approximately 40% of women, the condition persists after pregnancy [14, 15] showing increased linea alba laxity [8, 10] that is accompanied by decreased thickness, strength, and impaired function of the abdominal muscles [16–18]. Due to its appearance, persistent DRA negatively impacts women’s self-esteem and body image [19, 20]. If pronounced, the condition may result in insufficient soft tissue protection of the uterus in successive pregnancies and the formation of umbilical/epigastric hernia that may require surgical intervention [21–24]. Possible pregnancy-related DRA risk factors and the association of post-pregnancy DRA with chronic low back pain or support-related pelvic floor dysfunction are still under investigation [25–30]. According to the systematic reviews, DRA may be associated with impaired abdominal muscle strength [31], health-related quality of life [31, 32], body image satisfaction, abdominal pain [32], low back pain severity [31], and pelvic organ prolapse [32]. No significant association was observed between the DRA and lumbopelvic pain or urinary incontinence [31, 32]. However, further investigation is needed to verify these relationships because of the weak methodological quality of the existing studies and their heterogenicity regarding study design and population [31, 32]. Numerous studies have investigated the impact of specific therapeutic exercises or other physiotherapy methods on pregnancy-related DRA [8, 33–37]. Physiotherapy has been shown to improve the condition [38–40]. However, according to a recent systematic review and meta-analysis, there is currently no high-quality scientific evidence on the most effective exercise programs in the treatment of postpartum DRA [41]. Besides research on pregnancy-related DRA, IRD measurements have also been performed in studies on athletes [42, 43] and individuals with tendinopathy, dysmenorrhea, or lumbopelvic pain [44–46].
In physiotherapy research involving IRD measurement, musculoskeletal USI has been widely used owing to its high reliability [7, 18, 47–50]. However, review studies have indicated that IRD measurement procedure has not been standardized [39, 40]. The main discrepancies between the study protocols concern measurement sites (supraumbilical and infraumbilical) and diagnostic criteria for DRA [14, 38–40]. They also apply to the examinee’s body position, way of abdominal muscle activation, or breathing phase during image capturing. Differences in the measurement procedure may impact study outcomes and make the comparison of findings obtained by different research centers difficult or impossible [40]. Therefore, systematic mapping of physiotherapy-related studies involving IRD measurement with USI and discussions on specific aspects of the measurement procedures in the light of existing knowledge on musculoskeletal USI are warranted. All these should help formulate recommendations on best practices in performing and describing IRD assessment methods. If future studies follow such recommendations and use standardized measurement procedures, reports on DRA incidence or treatment effects could be compared. The recommendations may also help physicians and physiotherapists make more accurate DRA diagnoses and decide what conditions might benefit from physiotherapy. This, in turn, may prevent adverse effects of untreated DRA.
Therefore, this scoping review aimed to collect all peer-reviewed publications related to physiotherapy and physical exercise/training that describe IRD measurement procedures using USI. Based on discussions on similarities and differences of the procedures, and the completeness of their descriptions, it was aimed to formulate recommendations on the IRD measurement protocol standardization, to be considered in designing future physiotherapy studies and used in physiotherapy practice.
Methods
This scoping review was designed and conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses, Extension for Scoping Reviews (PRISMA-ScR) [51, 52]. The PRISMA-ScR checklist is provided in Additional file 1: S1.
Protocol
The study protocol was jointly developed a priori by two review leads (A.O.B. and D.C.). It was registered at the International Platform of Registered Systematic Review and Meta-analysis Protocols (INPLASY). The registration number is 202290116.
Eligibility criteria
The eligibility criteria were developed by two reviewers (A.O.B. and D.C.) with experience in research and practice on women’s health physiotherapy and IRD assessment using USI. Articles published in English starting with the earliest available until the last database entry were considered for review. To assure high-standard measurement procedure descriptions, the included publications were peer-reviewed research papers or registered study protocols. Table 1 presents detailed inclusion and exclusion criteria.
Table 1.
Inclusion and exclusion criteria used in the two-phase selection process to identify publications describing the measurement of inter-recti distance (IRD)/diastasis recti abdominis (DRA) with ultrasonographic imaging (USI)
| Inclusion | Exclusion | |
|---|---|---|
| Publication type | Full-text of a peer-reviewed original research article or registered study protocol | Only abstract form, conference proceeding, letter, review |
| Phase I—title and abstract | ||
| Population | Human adults | Non-humans and human infants, children, and adolescents |
| Concept |
IRD/linea alba width/DRA measurement procedure with USI (detailed procedure description) |
USI or other procedures not related to IRD/linea alba width/DRA measurement; IRD/linea alba width/DRA measurement with other tools, e.g., manual caliper, tape measure, ruler, magnetic resonance, computer tomography, palpation, and intraoperatively |
| Phase II—full text | ||
| Context* | Field of physiotherapy or physical exercise/training | Field of surgery (plastic, general) or other medical fields not related to physiotherapy or physical exercise/training |
*Selection based on the authors’ affiliation, study aims, and information provided in the main text of the publication
Information sources
To identify potentially relevant publications, the PubMed, Embase (Elsevier), and Ovid (Medline) bibliographic databases were searched by two independent reviewers (D.C. and A.O.B.). The most recent electronic literature search was conducted on August 31, 2022. The search was supplemented by hand searching and scanning the reference lists of the included or relevant sources of evidence.
Search strategy
The search strategy was developed by two reviewers (D.C. and A.O.B.) who gained their knowledge through video tutorials and closely cooperated with an experienced librarian from the Medical University Library. For PubMed, the final search strategy used was as follows: ((interrect*[tiab]) OR (inter-rect*[tiab]) OR (linea alba[tw]) OR (recti abdominis[tiab]) OR (recti muscle*[tiab]) OR (rectus muscle[tw]) OR (rectus abdom*[tiab]) OR (recti[tiab]) OR (rectus abdominis[mh])) AND ((diastasis[tiab]) OR (separation[tw]) OR (width[tw]) OR (distance[tiab]) OR (widening[tw])) AND ((USI[tw]) OR (ultrasound imaging[tiab]) OR (ultrasonography[tiab]) OR (ultrasonography[mh]) OR (US[tw]) OR (ultrasound[tiab])); filter: English.
All search results were saved, and duplicate publications were removed manually. To reduce the risk of error, two researchers (D.C. and M.R.Z.) independently removed duplicates and compared the outcomes of their selection.
Selection of sources of evidence
Two standardized forms were developed (using the Microsoft Forms software, Office 365) to guide the screening of the articles identified through the search strategy. Forms I and II concerned title and abstract, and full-text screening, respectively (Additional file 1: S2 and S3). These forms, along with the explanation and elaboration documents (Additional file 1: S4), were developed and refined by two review leads (D.C. and A.O.B.) during the prescreening of 50 random publications. The prescreening was a continuous interactive process of refining the questions to improve their appropriateness, accuracy, and comprehensiveness and ensure that filling out the forms will enable capturing all relevant publications. After both forms had been prepared, four reviewers (D.C., A.O.B., M.R.Z, and J.N.) performed calibration exercises, independently screening a sample of 30 titles and abstracts and filling out Forms I. The Kappa coefficient showed an interrater agreement of 0.80–0.93. The discrepancies between the reviewers’ answers and any unclear issues were discussed until a consensus was reached. Minor refinements were then made to Form I and to the explanation and elaboration document. As the interrater agreements were satisfactory [52], the screening of the titles and abstracts of all remaining publications was continued independently by two reviewers (D.C./J.N. and M.R.Z.). After completing Forms I for all publications, the reviewers compared the answers, discussed and resolved any disagreements by consensus. In cases of uncertainty, an additional reviewer (A.O.B.) was consulted to make the final decision.
The same steps were followed for full-text screening and filling out Forms II. In this phase, the calibration exercises concerned screening a sample of 20 full texts. The interrater agreements were excellent (Kappa coefficient = 1).
Data charting process
A Data-charting Form was jointly developed by two review leads (A.O.B. and D.C.) to extract relevant information on the IRD measurement procedure from the included sources of evidence (Additional file 1: S5). Two reviewers (M.R.Z./J.N. and A.O.B./D.C.) independently copied appropriate extracts from full texts and pasted them into separate forms. To facilitate comparisons, extracts by both reviewers were pasted in two adjacent columns of the final version of the Data-charting Form.
Data items
The following data items on the IRD measurement procedure using USI were sought: publication characteristics (first author, publication year, country/countries of the research center, main study objective); population characteristics (sex, age, body mass index [BMI; mean ± standard deviation], DRA presence, and for females, the number of pregnancies/deliveries, mode of delivery); specific aspects of the measurement procedure (examinee’s body position during the assessment at rest, muscle activation/task during the examination, the respiratory phase/pattern during image capturing (Table 2), the examiner’s profession and experience (hours of training and years of practice), ultrasonographic scanner (brand, type, mode, and field of view) and transducer (type and frequency), measurement site/sites; cutoff values for “normal” IRD or DRA (i.e., IRD considered normal or indicative of a pathological condition), number of images taken at each measurement site and whether measurements were averaged, image processing and measurement methods (online or offline); Table 3).
Table 2.
Study objectives, participants, and conditions for performing the inter-recti distance (IRD) measurement using ultrasonographic imaging (USI) in 49 study protocols
| Study objectives | Participants | Body position during assessment at rest* | Assessment during specific muscle activity/task | Breathing | |
|---|---|---|---|---|---|
|
Abuín-Porras 2019 (Spain) [42] |
To compare abdominal muscle thickness and IRD between female rugby players and non-athletes | 32 nulliparas: 16 rugby players, mean age: 24.7 ± 4.9 yr, BMI: 23.4 (21.9–24.7); 16 non-athletes, mean age: 27.9 ± 6.1 yr, BMI: 22.8 (20.5–25.7) | Supine | Not applicable | At the end of expiration |
| Arranz-Martín 2022 (Spain/Canada) [74] | To determine the acute effect of an abdominal hypopressive exercise (AHE) on IRD, linea alba distortion, and abdominal muscle thickness among primiparous women and to compare this effect with that of other abdominal exercises |
46 primiparas at 3mo after singleton vaginal delivery, mean age: 35 ± 4 yr; median BMI: 22.7 (interquartile range: 21.1–25.8) |
Hook lying |
- AHE: trunk axially extended, wrists, ankles dorsiflexed, shoulders medially rotated; after one breathing cycle, in apnea, ribs expanded laterally, abdominal wall moved inward and cranially - ADIM: after one breathing cycle, navel drawn in toward the spine - Semi curl-up: after breathing cycle, head and shoulders off the table, arms at sides, inferior scapular angles in contact with the table - ADIM + semi curl-up |
Pattern/phase related to specific exercise |
| Balasch-Bernat 2021 (Spain) [56] | To evaluate the differences in IRD and abdominopelvic function between nulliparous, primiparous and multiparous women | 75 women: 25 primiparas and 25 multiparas at 6mo after vaginal delivery, and 25 nulliparas; mean age: 34.2 ± 2.6, 35.0 ± 4.0, 33.2 ± 4.6 yr, respectively; BMI: 23.4 ± 4.2, 22.3 ± 3.0, 22.3 ± 2.9, respectively | Supine, slight knee and hip flexion, a pillow under the knees, arms along the body |
- ADIM: after inhaling and exhaling, navel drawn in toward the spine - Curl-up: head and shoulders lifted, lower scapular angles off the examination table |
Not specified |
|
Barbosa 2013 (Brazil) [60] |
To investigate the accuracy of IRD measurement using a caliper compared with USI | 106 paras 72 h after delivery (62.2% cesarean, 37.8% vaginal), parity: 2.2 ± 1.4, mean age: 27.1 ± 6 yr, BMI: 25.9 ± 6.8 | Supine, lower limbs flexed, and feet on a bed | - Trunk flexed, scapulae off the support, and arms along the body | Not specified |
|
Beamish 2019 (Canada) [8] |
To investigate the impact of the measurement site and task on IRD, linea alba stiffness, and distortion, and to assess the relationships between the linea alba parameters | 20 women (9 nulliparas and 11 paras ≥ 1 yr after vaginal delivery: 1 primipara, 10 multiparas) with and without DRA, mean age: 31 ± 8 yr, BMI: 25.3 ± 3.9 | Supine, thin pillow under the head, and arms along the body |
- Head lift: head gently lifted off the pillow - semi curl-up: head and shoulders lifted and inferior angles (not the spines) of the scapulae in contact with the examination table |
At the end of expiration (breathing paused for image capture) |
|
Belo 2020 (Brazil) [61] |
To determine the reliability and accuracy of IRD measurement using a caliper compared with USI | 54 pregnant women at 28–41wk gestation, mean age: 24.6 ± 5.6 yr, BMI: 29.3 ± 5.1 | Supine, hips and knees flexed, feet on a bed, and arms by the side | - Trunk flexed and lower borders of scapulae off the bed | During expiration |
|
Benjamin 2020 (Australia) [67] |
To determine the criterion validity of the use of a caliper, tape measure, and finger width to evaluate IRD compared with USI | 50 paras ≥ 6wk postpartum (26 primiparas, 24 multiparas, delivery: 21 vaginal, 19 cesarean, and 10 vaginal with instrumentation, age: 32.8 ± 4.8 yr, BMI not reported | Supine, knees flexed to 90°, arms by the side | - Modified abdominal sit-up: arms crossed over the chest, head raised, and inferior angles of the scapulae off the surface | At the end of expiration |
| Castellanos-López 2022 (Spain) [57] | To compare anteroposterior diameter of the levator ani hiatus, abdominal muscle thickness, and IRD between women with and without dyspareunia | 32 non-pregnant, non-postpartum women: 16 with dyspareunia (mean age: 25.4 ± 3.4 yr, BMI: 21.7 ± 2.9), 16 without dyspareunia (mean age: 26.7 ± 4 yr, BMI: 22.8 ± 1.7) | Supine, pillow under the head, hips and knees flexed | - Abdominal contraction: arms crossed over the chest, upper trunk raised, spines of the scapulae off the examination table | Breathing phase considered irrelevant |
|
Chiarello 2013 (USA) [62] |
To assess the concurrent validity of the use of digital calipers and USI for the measurement of IRD | 56 subjects (11 men, mean age: 37.5 ± 9.8 yr, BMI: 30 ± 3.9; 22 nulliparas, mean age: 28.5 ± 6 yr, BMI: 23.4 ± 4; 23 paras, mean age: 39.6 ± 9.8 yr, BMI: 22.6 ± 1.8 | Hook lying, pillow under the head, arms by the side | - Partial curl-up: arms crossed over the chest, head and spine of the scapulae off the examination table | Not specified |
|
Chiarello 2016 (USA) [9] |
To determine whether IRD decreases with active abdominal contraction in men and nulliparous and parous women | 56 subjects (11 men, mean age: 37 ± 10 yr, BMI: 30 ± 3.9; 22 nulliparas, mean age: 27.9 ± 5.9 yr, BMI: 23.4 ± 4; 23 paras, mean age: 39.2 ± 9.7 yr, BMI: 22.6 ± 1.8 | Same as Chiarello (2013) [62] | Same as Chiarello (2013) [62] | Not specified |
|
Coldron 2008 (UK) [16] |
To compare the RA size and shape and IRD between day 1 and month 2, 6, and 12 postpartum, and between paras and nulliparas | 72 primiparas, 43 multiparas at day 1 and month 2, 6, and 12 postpartum, mean age: 32 yr (19–46 yr, and 69 nulliparas, mean age: 27 yr (18–45 yr), BMI not reported | Crook lying, knees flexed over two pillows | Not applicable | Not specified |
|
Corvino 2019 (Italy) [10] |
To categorize the anatomical variations of DRA | 92 women: 10 without DRA and 82 with DRA (5 nulliparas; 77 paras, parity: 1–4, last delivery: 48 vaginal, 29 cesarean), mean age: 35 yr (30–51 yr), BMI not reported | Supine, pillow under head, knees slightly flexed, and arms along the trunk | Not applicable | In a neutral moment immediately after expiration |
|
Crommert 2021 (Sweden) [68] |
To investigate how physical and psychological factors are linked to disability attributed to symptoms from an increased IRD in paras | 139 paras at 1–8 yr since last delivery with IRD ≥ 2 finger widths (38% with at least one cesarean section), mean age: 37 ± 4.9 yr, BMI: 23.9 ± 3.5 | Supine, knees flexed to 90° | Not applicable | At the end of expiration |
|
Da Cuña-Carrera 2021 (Spain) [11] |
To assess the IRD at rest and during abdominal crunch, abdominal crunch with TrA preactivation, and abdominal hypopressive exercise (AHE) | 98 healthy subjects: (64 non-pregnant nulliparas and 32 men), mean age: 22.4 ± 3.6 yr, BMI: 22.8 ± 2.7 |
Supine, knees flexed to 90° , feet supported, and arms along the body |
- Abdominal crunch: arms crossed over the chest, head and scapulae off the surface - Abdominal crunch + TrA preactivation - AHE: arms above the shoulders; after deep exhalation, breath-holding with rib expansion |
At the end of expiration |
| Depledge 2021 (New Zealand) [64] | To determine the (immediate) effect of four abdominal exercises, Tubigrip and taping in reducing DRA at 3 wk postpartum | 29 paras with DRA after vaginal delivery (mean age: 32 ± 4.6 yr, days postpartum: 21 ± 4, body height: 166 ± 5.9 cm, body mass: 65 ± 7.9 kg) | Crook lying, hips, and knees flexed to 90° |
- ADIM + PFM activation - Curl-up: head, scapulae off the examination table, hands along thighs directed toward the knees - Sahrmann early level single leg raise with ADIM; supine, one leg flexed (90° hip flexion) - modified McGill side-lying plank: hip off the examination table to align trunk and thigh - ADIM, curl-up + Tubigrip, taping |
Immediately after relaxed expiration (in a stable position held for 3–4 s) |
|
Eisenberg 2021 (Israel) [27] |
To investigate the clinical and morphological relationships between DRA and pelvic floor trauma in primiparas | 36 primiparas (vaginal delivery), with birth-related pelvic floor trauma: 18 with DRA, mean age: 27.8 ± 4.7 yr, BMI: 23.7 ± 4.1, and 18 without DRA, mean age: 26.8 ± 4.2 yr, BMI: 23.7 ± 3.5 | Supine, knees and pelvis flexed to 90° | - Abdominal curl: head and shoulders lifted, spines of the scapulae off the examination table, hands reaching the knees | At the end of expiration |
|
Fan 2020 (Italy and Canada) [12] |
To investigate differences between abdominal muscles and fasciae in women, depending on delivery mode and in comparison with nulliparas | 36 women: 23 primiparas ≥ 2 yr after delivery (13 cesarean, mean age: 41.7 ± 6.1 yr, BMI: 23.7 ± 2.5 and 10 vaginal, mean age: 47 ± 15.2 yr, BMI: 21.5 ± 2.8 and 13 nulliparas, mean age: 27.1 ± 14.2 yr, BMI: 21.6 ± 1.4 | Supine | Not applicable | At the end of expiration |
|
Fernandes da Mota 2015 (Portugal and Norway) [15] |
To assess the prevalence and risk factors of DRA in pregnant/postpartum women and their relationships with lumbopelvic pain | 84 primiparas (at 35wk gestation, 6–8, 12–14, and 24–26wk postpartum; delivery: 52 vaginal, 32 cesarean); at 6mo postpartum: 33 with DRA, mean age: 31.6 ± 2.2 yr, BMI: 22.3 ± 3.7, and 51 without DRA, mean age: 32.5 ± 2.9 yr, BMI: 22.5 ± 3.2 | Same as Mota (2012) [49] | Not applicable | At the end of expiration |
|
Gillard 2018 (UK) [63] |
To assess the effect of posture and the measurement site on IRD, and to assess the reliability of the measurement in paras |
41 women (12 primiparas and 29 multiparas) between 2mo and 28 yr (mean, 9.8 ± 8.9 yr) after vaginal delivery, mean age: 43 ± 9 yr, BMI: 25.2 ± 4 |
Crook lying, pillow under the head, legs hip-width apart, knees flexed to 90°, feet facing forward, and mid-pelvic alignment |
Postural muscle tone: - Sitting position: feet flat on the floor, arms resting on the thighs, and mid-pelvic alignment - standing position: legs hip-width apart, arms along the body, and mid-pelvic alignment |
At the end of expiration |
|
Gluppe 2020 (Norway) [13] |
To investigate the immediate effects of abdominal and PFM exercises on IRD in paras with DRA | 38 paras > 6wk postpartum with DRA [4 primiparas and 34 multiparas (parity: 2–4), after vaginal and cesarean deliveries], mean age: 36.2 ± 5.2 yr, BMI: 23.2 ± 3.6 | Supine, hips and knees flexed, and feet on a table | Head lift, curl-up, PFM contraction, PFM contraction + curl-up, maximal ADIM, PFM contraction + maximal ADIM, pelvic tilt, and twisted curl-up (to the left and the right) | At the end of expiration |
| He 2021 (China) [65] | To determine the utility of shear wave elastography in assessing abdominal muscles in women with and without DRA | 36 postpartum women with DRA (32 cesarean, 4 vaginal delivery), mean age: 28.6 ± 3.7 yr, pre-pregnancy BMI: 20.2 ± 2.0, parity, days postpartum not specified; 24 nulliparas, mean age: 26.8 ± 4.7 yr, BMI: 20.6 ± 2.1) | Supine, arms across the chest | Not applicable | Not specified |
|
Hills 2018a (Canada) [53] |
To determine the influence of the transducer tilt in cranial and caudal directions on IRD measurement | 15 paras (5 primiparas, 10 multiparas, delivery: 9 vaginal, 6 cesarean; 7/15 with DRA), mean age: 39.4 ± 8 yr, BMI: 29.2 | Supine and legs extended | - Head lift: head lifted with the neck in line with the spine, and the scapula in contact with the examination table | Not specified |
|
Hills 2018b (Canada) [17] |
To compare the trunk muscle function between women with and without DRA at 1 yr postpartum | 40 primiparas at 1 yr postpartum (delivery: 31 vaginal, 9 cesarean): 18 with DRA, mean age: 31.9 ± 3.6 yr, BMI: 25.1 ± 5.6, and 22 without DRA, mean age: 31.2 ± 4.5 yr, BMI: 24.1 ± 3.9 | Supine, knees and hips flexed, and arms by the side | Not applicable | At the end of tidal expiration |
|
Iwan 2014 (New Zealand) [47] |
To assess the reliability of IRD measurement using high- and low-resolution USI, and to compare measurements by novice and experienced sonographers | 30 subjects: 14 men, mean age: 24.2 ± 8.3 yr, BMI: 24.4 ± 2.5, and 16 women (13 nulliparas, mean age: 21.8 ± 1.9 yr, BMI: 23.9 ± 2.8, and 3 postpartum, mean age: 36 ± 6.7 yr, BMI: 21.5 ± 2.4 | Supine, pillow under head, knees flexed to 90°, feet on a table, and arms along the body | - Partial curl-up: arms crossed over the chest and head and scapulae off the examination table | At the end of expiration |
|
Keshwani 2015a (Canada) [48] |
To investigate the intrarater between-session reliability of IRD measurement | 20 primiparas, multiparas with DRA at 3mo to 17 yr (mean: 3 yr) since last delivery (9 cesarean), mean age: 36 ± 6 yr, BMI: 26.1 ± 7 | Supine and pillow under the head | - Head lift: with the neck in line with the spine, head gently lifted off the pillow (head touching the pillow but not supported) | Not specified |
|
Keshwani 2015b (Canada) [54] |
To investigate the criterion-related validity and reliability of IRD measurement using extended field of view (standoff pad and panoramic mode) in paras | 21 non-pregnant primiparas and multiparas with IRD ≤ 3 finger widths (to visualize the entire IRD with conventional USI), mean age: 40 ± 6 yr, BMI: 22.8 ± 1.9 | Supine, pillow under the head, and arms by the side | Not applicable | During expiration |
|
Keshwani 2016 (Canada) [55] |
To investigate the interrater reliability of IRD measured at rest and during head lift in paras | 17 primiparas and multiparas at 6mo to 25 yr (mean: 7 yr) since last delivery; mean age: 38 ± 8 yr, BMI: 26.4 ± 7.3 | Supine, pillow under the head, neck in line with the spine | Same as Keshwani (2015a) [48] | Not specified |
|
Keshwani 2018 (Canada) [20] |
To investigate the relationship between IRD and symptom severity in the early postpartum period | 32 postpartum primiparas with DRA detected at 3–4wk after vaginal delivery; mean age: 32 ± 2 yr, BMI: 25 ± 3.7 | Supine, pillow under the head, and arms by the side | Not applicable | Not specified |
|
Keshwani 2019 (Canada) [33] |
To explore the feasibility of abdominal binding and trunk exercises for the management of DRA | 29 primiparas with DRA (first assessment at 3–4wk postpartum); mean age: 31.5 yr, BMI: 24.7 | Supine | Not applicable | Not specified |
| Kim 2022 (Korea) [69] | To investigate the efficacy of 6-wk core stabilization exercise program conducted in person and through real-time video conferencing on IRD and abdominal muscle thickness in women with DRA at 6-12mo postpartum | 37 DRA women 6-12mo postpartum [online group (9 vaginal, 10 cesarean delivery), mean age: 31.7 ± 3.9 yr, BMI: 22 ± 1.9; direct contact group (6 vaginal, 12 cesarean delivery), mean age: 32.7 ± 2.5 yr, BMI: 22.8 ± 1.9]; parity not specified | Supine | Not applicable | During normal respiration |
|
Lee 2016 (Australia and Canada) [34] |
To investigate IRD and linea alba distortion during curl-ups performed naturally and with TrA preactivation | 26 DRA subjects: 25 paras and 1 nullipara; mean age: 34 ± 4 yr, BMI: 20.6, and 17 non-DRA subjects: 11 nulliparas, mean age: 25 ± 2 yr, BMI: 20.4, and 6 males, mean age: 28 ± 3 yr, BMI: 23.5 | Supine, pillow under the head, hips and knees flexed, feet on a table, and arms by the side |
- Curl-up: head and neck lifted, top of the scapulae off the bed, and arms along the body - Curl-up + preactivated TrA by gentle PFM contraction |
Not specified |
| Li 2022 (China) [66] | To investigate the effects of progressive yoga exercise program on IRD among women in the early postpartum period | 116 primiparas, vaginal delivery [63 yoga exercisers (mean age: 31, BMI: 21.4 ± 2); 53 controls (mean age: 30, BMI: 21.7 ± 2.1)], IRD assessed at postpartum wk 6 and 12 | Supine, relaxed abdominal muscles | Not applicable | Not specified |
|
Liaw 2011 (Taiwan) [18] |
To investigate IRD natural recovery and abdominal muscle strength in women postpartum and to examine the relationship between IRD and abdominal muscle function | 30 paras (17 primiparas, 13 multiparas) at 7wk (4–8 wk) and 6mo (6–8mo) after vaginal delivery, mean age: 32.1 ± 3 yr, BMI: 21.5 ± 2.8; 20 nulliparas, mean age: 31.9 ± 4.1 yr, BMI: 20.7 ± 2.7 | Supine and 2 pillows under the knees | Not applicable | At the end of expiration |
|
Mota 2012 (Portugal and Norway) [49] |
To evaluate the test–retest and intrarater reliability of IRD measurement (during rest and a specific task), and to investigate IRD in postpartum women | 24 women: 12 postpartum (< 6mo), mean age: 31.2 yr (26–36 yr), BMI: 24 (20.8–28.5); 12 with parity 0–2, mean age: 29.9 yr (16–55 yr), BMI: 21.5 (18.9–24.6) | Supine, knees flexed to 90°, feet on a table, and arms along the body |
- Abdominal crunch: head and shoulders raised upward, scapulae off the examination table - ADIM: after inhalation, abdominal muscles drawn in toward the spine with exhalation |
At the end of expiration |
|
Mota 2013 (Portugal and Norway) [71] |
To evaluate the reliability of IRD examination with abdominal palpation and compare palpation with USI | 20 paras, mean parity: 0.7 (0–2), age: 29.3 yr (16–49 yr), BMI: 23 (18.9–28.5); 12/20 in the postpartum period | Same as Mota (2012) [49] | - Abdominal crunch: head and shoulders raised upward, scapulae off the examination table | At the end of expiration |
|
Mota 2015 (Portugal and Norway) [35] |
To evaluate the immediate effect of drawing-in and abdominal crunch exercises on IRD in pregnancy and postpartum | 84 primiparas (at 35–41wk gestation and 6–8, 12–14, and 24–26wk postpartum; delivery: 52 vaginal and 32 cesarean), mean age: 32 yr (25–37 yr), BMI not reported | Same as Mota (2012) [49] |
- Abdominal crunch: head and shoulders raised upward (while exhaling), scapulae off the table - ADIM: after inhalation and exhalation, and the navel drawn in toward the spine |
Immediately at the End of expiration |
|
Mota 2018 (Portugal and Norway) [72] |
To establish “normal” IRD values in primiparas during pregnancy and postpartum | 84 primiparas (at 35–41wk gestation and 6–8, 12–14, 24–26 wk postpartum; delivery: 52 vaginal and 32: cesarean), mean age: 32.1 ± 2.7 yr; BMI not reported | Same as Mota (2012) [49] | Not applicable | At the end of expiration |
|
Morales 2018a (Spain) [43] |
To compare the perimuscular connective tissue and IRD between elite and amateur basketball players | 22 men (11 elite and 11 amateur basketball players), mean age: 21 ± 6 yr, BMI: 22.6 ± 2.6 | Supine | Not applicable | At the end of expiration |
|
Morales 2018b (Spain) [58] |
To assess abdominal muscle thickness and IRD during the drawing-in maneuver with a proprioceptive Stabilizer | 41 healthy subjects, mean age: 31.9 ± 4.5 yr, BMI: 22.9 ± 2.7 | Supine | - ADIM (with the use of Stabilizer) | At the end of expiration |
|
Nanikawa 2021 (Japan) [50] |
To assess the reliability of abdominal wall perimuscular connective tissue measurement | 38 healthy men, mean age: 21.6 ± 0.5 yr, BMI not reported | Supine and arms relaxed | Not applicable | At the end of expiration |
|
Pascoal 2014 (Portugal) [36] |
To determine the effect of abdominal muscle isometric contraction on IRD in postpartum women | 10 primiparas (1–5mo postpartum, delivery: 9 vaginal and 1 cesarean), mean age: 30 ± 4 yr, BMI: 24.1 ± 7.0, and 10 nulliparas, mean age: 28 ± 2 yr, BMI: 21.7 ± 5.3 | Supine, knees flexed to 90° (crook lying), feet on a table, and arms along the trunk | - Abdominal crunch: head and shoulders raised upward, scapulae off the examination table, and fingertips touching knees | At the end of expiration |
|
Romero-Morales 2018 (Spain) [59] |
To compare RA thickness and IRD between patients with Achilles tendinopathy (AT) who underwent an eccentric exercise (EE) program with vibration and EE program with cryotherapy | 61 subjects with AT randomly divided; grade I: 4 men, 26 women receiving EE + vibration, mean age: 41.1 ± 8.2 yr, BMI: 25.2 ± 2.5, gr II: 5 men, 26 women receiving EE + cryotherapy, mean age: 42.1 ± 9.2 yr, BMI: 24.8 ± 2.4 | Supine | - Calf muscle maximal isometric contraction | At the end of expiration |
|
Romero-Morales 2019 (Spain) [44] |
To compare and quantify IRD and abdominal muscle measures between subjects with and without Achilles tendinopathy (AT) | 143 subjects (71 with AT, mean age: 45.1 ± 12.7 yr, BMI: 24.8 ± 2.1, and 72 without AT, mean age: 37.6 ± 11.9 yr, BMI: 23.9 ± 3.7 | Supine | Not applicable | Not specified |
|
Romero-Morales 2020 (Spain) [45] |
To compare abdominal muscles thickness and IRD in women with and without primary dysmenorrhea (PD) | 39 women (19 with PD, mean age: 20 ± 4 yr, BMI: 21.6 ± 3.3 and 20 without PD, mean age: 22.5 ± 7 yr, BMI: 21.5 ± 3.7 | Supine, hips and knees flexed, and arms along the body | Not applicable | At the end of expiration |
|
Sancho 2015 (Portugal and Norway) [73] |
To compare IRD at rest between women who delivered vaginally and by C-section; to describe the effect of different abdominal exercises on IRD | 38 postpartum primiparas after singleton gestation (23 after vaginal delivery, mean age: 31.2 ± 3.6 yr, BMI 22.9 ± 2.7, and 15 after cesarean section, mean age: 32.3 ± 4.4 yr, BMI: 22.8 ± 2.8) | Supine, knees flexed to 90°, feet on a table, and arms along the body |
- Abdominal crunch: head, shoulders raised upward, scapulae off the table, fingertips touching the knees - ADIM: after inhalation, abdominal muscles drawn in toward the spine with exhalation - ADIM + abdominal crunch |
Immediately at the end of expiration |
| Starzec-Proserpio 2022 (Poland) [70] | To evaluate the differences between early postpartum women with and without pelvic girdle pain (PGP) regarding pubic symphysis separation, IRD, and pain catastrophizing | 105 women 24-72 h after vaginal delivery, 35 with PGP (mean age: 32.9 ± 4.5 yr, pre-pregnancy BMI: 24.5 ± 4.5) and 70 without PGP (mean age: 33.0 ± 4.2 yr, pre-pregnancy BMI: 22.5 ± 3.2), each group parity: 1.8 ± 0.9) | Supine | - Curl-up: head and upper torso raised, scapulae off the table | Not specified |
|
Theodorsen 2019 (Norway) [37] |
To assess the effect of the PFM and TrA muscles contraction on IRD in postpartum women with DRA | 38 women 0–26wk postpartum (parity: 1–3) with DRA (delivery: 31 vaginal, 4 vaginal/forceps, 3 cesarean; 4 multiple births), mean age: 34.6 ± 4.0 yr, BMI: 24.2 ± 3.3 | Supine, pillow under head, knees hip-width apart, flexed to 90°, feet on a table, and arms along the body |
- PFM contraction - ADIM - PFM contraction + ADIM |
At the end of expiration |
| Theodorsen 2022** (Norway) [75] | To investigate the effect of a specific exercise program during pregnancy on DRA after the 12-wk intervention and postpartum | Of 100 gravidas with DRA at gestational wk 24 (primigravidas and multigravidas), 50 will be assigned to exercise group and 50 to non-intervention group; IRD to be measured at 24 and 37wk gestation, and at 6wk, 6 and 12mo postpartum | Supine, head on a pillow, arms alongside the body, knees hip-width apart, bent to 90°, feet on a table | Not applicable | Immediately at the end of expiration |
|
Whittaker 2013 (UK and Canada) [46] |
To compare the resting thickness of the abdominal muscles, perimuscular connective tissue, and IRD in persons with and without lumbopelvic pain (LPP) | 50 male and female subjects: 25 with LPP, mean age: 46.6 ± 8 yr, BMI: 24.0 ± 3.5, and 25 without LPP, mean age: 36.3 ± 9.4 yr, BMI: 23.5 ± 2.5 | Supine | Not applicable | At the end of expiration |
*Body position during an assessment at rest and/or the basic starting position for the assessment during specific muscle activity/task (except assessment in the sitting and standing positions [63])
**Study protocol (presenting research project). DRA: diastasis recti abdominis; RA: rectus abdominis; TrA: transversus abdominis; PFM: pelvic floor muscles; and ADIM: abdominal draw-in maneuver
Table 3.
Characteristics of the examiners, ultrasonographic imaging (USI) systems, and inter-recti distance (IRD) measurement methods in 49 study protocols
| Examiner’s profession and experience | Ultrasonographic scanner and transducer | IRD measurement site | Use of cutoff values for “normal” IRD or DRA | Number of images per site | Methods of image processing and measurement | |
|---|---|---|---|---|---|---|
|
Abuín-Porras 2019 (Spain) [42] |
PT with USI experience | LOGIQ S7, XDclear, GE Healthcare; Little Chalfont, UK; 10- to 13-MHz linear probe, 55 mm; B-mode | just under the navel | Not applicable | Mean IRD of 3 images |
Offline measurement with ImageJ software (Research Services Branch, National Institute of Health, Bethesda, MD, USA) |
| Arranz-Martín 2022 (Spain/ Canada) [74] | A women’s health PT with > 5 yr of experience in abdominal and perineal USI |
Mindray 7; 12-MHz 30-mm linear probe (Mindray L14-6NS, Shenzhen, China); B- mode |
2 cm below and above the navel center, the midpoint between the navel center and xiphoid | Not applicable; LA distortion assessment | Mean IRD of 2 images per site and task | measurement with digital caliper |
| Balasch-Bernat 2021 (Spain) [56] | Two PTs with 10 yr of clinical experience in women’s health and rehabilitative USI | Samsung HS30, (Samsung Medison co., LTD, Gangwon-do, Korea); linear probe LN 5–12; B-mode; panoramic mode* | 2 cm above the superior navel border and 2 cm below the inferior navel border | Not applicable | Mean IRD of 3 images per site and task | Not specified |
|
Barbosa 2013 (Brazil) [60] |
Not specified | Medison SonoAce 8000, Korea; 5- to 7-MHz linear probe | 3, 6, 9, 12 cm above the navel | Not applicable | Not specified | Not specified |
|
Beamish 2019 (Canada) [8] |
PT with postgraduate training, > 400-h experience in B-mode USI of the abdominal muscles (two PT students after 10-h training and 10-h practice made offline measurements, intrarater reliability: ICC = 0.96–0.98, interrater reliability: ICC = 0.94–0.95 | SuperSonic Aixplorer UltraFast (SuperSonic Imagine, Aix-en-Provence, France); 10-MHz linear probe (SL15-4); B-mode; shearwave elastography | 3 and 5 cm above and at the superior navel border | DRA = IRD > 22 mm at 3 cm above the umbilicus, DRA = mean IRD > 22 mm across 3 sites; LA stiffness and distortion assessment | Mean IRD of 3 images per site and task | Video and image capturing; image processing with the SuperSonic Aixplorer software |
|
Belo 2020 (Brazil) [61] |
Examiner who was previously trained | Philips HD3xe; 5- to 9-MHz linear probe | 3 cm above, 2 cm below, and at the navel | DRA = IRD > 22 mm at 3 cm above, > 16 mm at 2 cm below, and > 20 mm at the navel | mean IRD of 3 images | Not specified |
|
Benjamin 2020 (Australia) [67] |
PT after a 2-h ultrasonography training session by an experienced sonographer; 16 h of practice in USI of IRD | GE Voluson I; 3- to 8-MHz linear probe, 38.1 mm (9 L) |
4.5 cm above and at the upper border of the navel, 4.5 cm below and at the lower border of the navel |
DRA = IRD > 22 mm; ≥ 2 fingers width | 2 images | Offline measurement |
| Castellanos-López 2022 (Spain) [57] | An expert in USI with several specialization courses and 5 yr of experience |
LOGIC F6, GE Healthcare, Chicago, IL, USA); 6- to 13-MHz linear probe, B-mode |
Same as Chiarello (2013) [62] | Not applicable | Not specified | Not specified |
|
Chiarello 2013 (USA) [62] |
Examiner with advanced training and 7 yr of clinical USI use; intrarater within-session reliability: ICC = 0.90–0.98 | LOGIQ Book XP, GE Healthcare, Waukesha, WI; 5- MHz curvilinear probe; B-mode | 4.5 cm above and below the navel midpoint | Not applicable | Not specified | On-screen measurement |
|
Chiarello 2016 (USA) [9] |
same as Chiarello (2013) [59] | same as Chiarello (2013) [62] | Same as Chiarello (2013) [62] | Not applicable | Not specified | Same as Chiarello (2013) [62] |
|
Coldron 2008 (UK) [16] |
Not specified | SSD, Aloka Co. Ltd., Mitaka-shi, Tokyo, Japan; 5-MHz linear probe (11-cm footprint) | Bottom transducer edge placed just cephalad to the navel | Not applicable | Mean IRD of 2 images | Offline measurement with on-screen calipers using USICA software, Dept. of Medical Physics, St. George’s Hospital, London |
|
Corvino 2019 (Italy) [10] |
Two operators with 33 and 13 yr of experience with USI, respectively. The operators had specific training in evaluating DRA |
Voluson E8, GE Healthcare, and RS85 Samsung Healthcare; broadband probes, typically 10-MHz; for DRA > 4 cm: trapezoid, DRA > 5 cm: extended field of view* |
3 cm above and below the navel (entire midline checked to identify the DRA pattern) |
DRA = IRD > 20 mm at rest; DRA patterns: only above or below the navel, at the navel level, along the entire midline but wider above or below the navel |
Mean IRD of 3 images per site | not specified |
|
Crommert 2021 (Sweden) [68] |
Not specified | LOGIQ-e R7, GE, Boston, MA; 12-MHz linear probe, 47 mm; B-mode; panoramic function* | 4.5 cm above the navel center | increased IRD = IRD ≥ 2 fingers width | Mean IRD of 3 images | Offline analysis with custom-written script in MATLAB (MATLAB R2019a, MathWorks, Natick, MA, USA) |
|
Da Cuña-Carrera 2021 (Spain) [11] |
PT with knowledge of USI and experience in IRD measurement |
SonoSite M-Turbo; 5- to 10-Mz linear probe; B-mode |
Just above the navel (U point), halfway between the U point and xiphoid | Not applicable | Not specified | Frozen image on-screen measurement with transversal caliper |
| Depledge 2021 (New Zealand) [64] | PT experienced in USI, participated in a reliability study on IRD measurement with USI, ICC > 0.91 (Iwan, 2014 [44]) | Philips iU22; 4- to 12-MHz linear or 4- to 9-MHz curvilinear probe (Philips Med. Syst. Co., Eindhoven, NL); B-mode | Same as Mota (2012) [49] | DRA = IRD > 2 fingers width | Mean IRD of 2 images | Not specified |
|
Eisenberg 2021 (Israel) [27] |
A physician specializing in gynecological USI | Voluson 730, GE Medical Systems, Zipf, Austria; probe not specified | Upper margin of the navel, 3 cm above, and 2 cm below the navel | DRA = IRD ≥ 22 mm at 3 cm above the navel, ≥ 20 mm at the upper margin of the navel, and/or ≥ 16 mm at 2 cm below the navel | Not specified |
ARCHIVED data sets were analyzed using the proprietary software 4-D VIEW (GE Medical Systems) |
|
Fan 2020 (Italy and Canada) [12] |
PT with 5-yr experience in musculoskeletal USI | Esaote MyLab Seven (Esaote SpA, Genova, Italy); 6- to 18-MHz linear probe, 37 mm | 2 cm above the navel | Not applicable | Not specified | Not specified |
| Q | PT with specific training in image capturing and measuring IRD | LOGIQ-e, GE; 4- to 12-MHz linear probe, 39 mm; B-mode | 2 cm below the navel center | DRA = IRD > 16 mm at 2 cm below the navel center | Not specified | Images exported in DICOM format, processing as by Mota (2012) |
|
Gillard 2018 (UK) [63] |
PT, > 12mo of experience in USI, training on a national medical US society program; within- and between-session intrarater reliability: ICC = 0.90–0.99 | Mindray DP50; 5-MHz linear probe, 53 mm (75L53 EA); B-mode | One-third of the xiphoid-navel distance, just superior to the navel, half of the navel-pubis distance | Not applicable | Mean IRD of 2 images per site and postural position | Offline measurement on JPEG images with bespoke MATLAB image processing software (ver. 7.1) |
|
Gluppe 2020 (Norway) [13] |
PT after specific training in USI of the pelvic floor and abdomen | LOGIQ-e R7, GE Healthcare; 5- to 13-MHz wideband linear probe, (GE > 12L-RS); panoramic mode* | 2 cm above and below the navel center | DRA = IRD ≥ 2 fingers width, protrusion during curl-up; IRD ˃ 25 mm at 2 cm above/below navel | 1 image per site and condition | Offline analysis with software program (MicroDicom) |
| He 2021 (China) [65] | A senior radiologist with 10 yr of experience in abdominal and musculoskeletal USI | Aixplorer; linear probe (SL10-2), Supersonic Imagine, FR); B-mode | Subxiphoidal, epigastric, umbilical, infraumbilical, suprapubic (International Endohernia Society, Reinpold, 2019 [24]) | DRA = IRD ≥ 2 fingers width (in crook lying, arms crossed over the chest); DRA patterns: same as Corvino (2019) [10] | Not specified | Measurements with an on-screen caliper |
|
Hills 2018a (Canada) [53] |
PT with postgraduate training in musculoskeletal USI and > 50 h of experience in USI of the abdominal muscles | Voluson-i (GE Healthcare, Mississauga, Ontario, Canada); 10-MHz linear probe, 53 mm (9L-RS); B-mode; trapezoid mode* | 3 and 5 cm above the navel | DRA = IRD > 20 mm | 2 images per probe position and task | Offline measurement using Image J, version 1.46r (National Institutes of Health, Bethesda, MD, USA) |
|
Hills 2018b (Canada) [17] |
PT with postgraduate training in musculoskeletal USI, > 100 h of experience in USI of the abdominal muscles | Same as Hills (2018a) [53] | Superior navel border; 3 and 5 cm above the navel | DRA = IRD > 22 mm at 3 cm above navel and at least one other site; mean IRD of 3 sites > 20 mm | Mean IRD of 3 images per site | As by Hills (2018a) [53] |
|
Iwan 2014 (New Zealand) [47] |
PT, 8-yr practice in USI and 4th-yr PT student after 2- × 2-h training in USI of the abdominal anatomy and IRD measurement; intrarater reliability: within-session: ICC = 0.91–0.98 for PT, ICC = 0.89–0.98 for PT student; between-session: ICC = 0.79–0.98 for PT, ICC = − 0.51 to 0.88 for PT students | Low resolution: Chison 8300 Deluxe (Chison Medical Imaging Co. Ltd., China), 7.5-MHz linear probe; high-resolution: Phillips iU22 (Royal Philips Electronics, the Netherlands), 12.5-MHz linear probe | 2 cm above and below the navel | Not applicable | 2 images per condition per researcher | Measurement using the digital caliper setting on the USI unit |
|
Keshwani 2015a (Canada) [48] |
PT after 16 h of formal training on musculoskeletal USI; > 100 h of clinical USI experience; trained on IRD measurement by a USI expert; intrarater between-session reliability: ICC = 0.95–0.99 |
Voluson i (GE Healthcare, Waukesha, WI), 3- to 10-MHz linear probe; MyLab Five (Esaote SpA, Genoa, IT), 4- to 13-MHz linear probe; acoustic standoff pad 2 × 4 cm (ATS Lab., Inc., Bridgeport, CT)* |
5 and 3 cm above and at the superior border of the navel, 3 cm below the inferior border of the navel |
DRA = IRD ≥ 2 fingers width at the navel (in hook lying, neck flexed) | Mean IRD of 5 images per site and condition | Offline measurement using ImageJ (National Institutes of Health, Bethesda, MD) and software with the MyLab Five system (Esaote SpA) |
|
Keshwani 2015b (Canada) [54] |
Investigator after 16 h of formal training in USI of the abdominal muscles and > 200 h of experience in IRD evaluation with USI; 20 h of experience in extended field-of-view use; between-trial reliability for conventional, standoff pad, and panoramic techniques: ICC = 0.98–0.99 |
LOGIQ-e, GE Healthcare, Waukesha, WI; 4- to 13-MHz linear probe, 12.7 × 47.1 mm; B-mode; acoustic standoff pad (15 × 10 × 2 cm), ATS Lab., Bridgeport, CT; panoramic mode |
Superior umbilical border | Not applicable | Mean IRD of 5 images per each method | Offline measurement using ImageJ Version 1.48, National Institutes of Health, Bethesda, MD |
|
Keshwani 2016 (Canada) [55] |
Two PTs after a 16-h course in USI. Rater 1: > 100 USI evaluations of IRD; Rater 2: 10 h of training from Rater 1; interrater reliability: ICC = 0.63–0.96 | Voluson i, GE Healthcare, Chalfont St. Giles, UK; 3- to 10-MHz linear probe; B-mode; acoustic standoff pad 2 × 4 cm, ATS Lab., Bridgeport, CT* | Same as Keshwani (2015a) [48] | Not applicable | Mean IRD of 5 images per site, task, and rater (mean of at least 2 images in case of poor image quality) |
Offline measurement using ImageJ, National Institutes of Health, Bethesda, MD, USA |
|
Keshwani 2018 (Canada) [20] |
Registered sonographer with specific training in the measurement approach | LOGIQ-e, GE, Buckinghamshire, UK; 5- to 13-MHz linear probe; B-mode; panoramic mode* | Same as Keshwani (2015a) [48] | DRA = IRD ≥ 2 fingers width at all sites (in crook lying, head lifted off pillow) | Mean IRD of 5 images in each site | Not specified |
|
Keshwani 2019 (Canada) [33] |
Registered sonographer with > 15 yr of experience in gynecological, obstetrical, and musculoskeletal USI; > 30 h of training on the USI protocol | LOGIQ-e, GE; 4- to 13-MHz linear probe, 12.7 × 47.1 mm; B-mode; panoramic imaging* | Same as Keshwani (2015a) [48] | DRA = IRD ≥ 2 fingers width at all sites (in crook lying, head lifted off pillow) | Mean IRD of 5 images per site | Not specified |
| Kim 2022 (Korea) [69] | Not specified | MySono U5, Samsung Medison, Seoul, Korea, 2010; elliptical probe, B-mode, 47–63 Hz |
2.5 cm above the top of the navel |
DRA = IRD ≥ 2 fingers width—self-examination, verified by USI | Not specified | Measurements made with the caliper of the ultrasound apparatus |
|
Lee 2016 (Australia and Canada) [34] |
Not specified |
MyLab 25, Esaote SpA, Genoa, Italy; 12-MHz linear probe; B-mode |
Just above the navel (U point), halfway between the U point and xiphoid |
DRA = IRD > 22 mm at 3 cm above the navel, DRA = IRD > 15 mm inferior to xiphoid; LA distortion index: the average amount of deviation of the LA path from the shortest path between its attachments |
3 images per site and condition |
Images captured from videos, exported to JPEG format; analyzed using ImageJ (National Institutes of Health, Bethesda, MD, USA) |
| Li 2022 (China) [66] | Three physicians, each with 12 yr of clinical experience | Voluson E10 (GE Healthcare, Milwaukee, WI, USA); 5- to14-MHz linear probe (ML6-15-D) | 3 cm above, below, and at the navel | Not applicable | Not specified | Not specified |
|
Liaw 2011 (Taiwan) [18] |
PT with 13 yr of experience, 5 yr of assessing abdominal muscles using USI; interimage reliability: ICC = 0.91–0.97 | SSD-550, Aloka Co, Tokyo, Japan; 7.5-MHz linear probe, 38 mm; B-mode |
Probe lower edge: 2.5 cm above and at the upper margin of the navel, probe upper edge: 2.5 cm below and at the lower margin of the navel |
Not applicable | Mean IRD of 3 images per site | Measurement with an on-screen caliper |
|
Mota 2012 (Portugal and Norway) [49] |
PT trained in IRD evaluation with USI; discussed the USI protocol and analysis, and practiced with an experienced radiologist. Intra-image reliability: ICC > 0.90, intrarater between-day reliability: ICC = 0.50–0.90 |
LOGIQ-e, GE Healthcare, Waukesha, WI, USA; 4- to12-MHz linear probe, 39 mm; B-mode |
The bottom edge of the probe at 2 cm above and below the navel center | Not applicable | 1 image per site and condition | Offline processing using a customized program, MATLAB image processing software (MathWorks, Inc., Natick, MA); images assumed as a pixel-based coordinate system |
|
Mota 2013 (Portugal and Norway) [71] |
PT trained by an experienced radiologist |
GE LOGIQ-e; 4- to 12-MHz linear probe, 39 mm; B-mode |
Same as Mota (2012) [49] | Not applicable | Not specified | JPG images, processing as by Mota (2012) [49] |
|
Mota 2015 (Portugal and Norway) [35] |
PT with specific training in USI, including 3 yr of experience assessing IRD | LOGIQ-e; GE Healthcare, Waukesha, WI; 4- to 12-MHz linear probe, 39 mm (fixed frequency of 12 MHz); B-mode | The bottom edge of the probe at 2 and 5 cm above and 2 cm below the navel center | Not applicable | 1 image per site and condition | DICOM images, offline analysis using a customized program (MATLAB Image Processing Toolbox) as by Mota (2012) [49] |
|
Mota 2018 (Portugal and Norway) [72] |
PT with specific training in USI, including experience in assessing IRD; discussed and practiced the USI protocol and analysis with an experienced radiologist | LOGIQ-e, GE Healthcare, Waukesha, WI, USA; 12-MHz linear probe, 39 mm; B-mode | Same as Mota (2015) [35] | Determined “normal” IRD values at 5 and 2 cm above, 2 cm below the navel: at 35–41wk gestation: up to 79, 86, and 79 mm, respectively; at 24–26wk postpartum: up to 24, 28, and 21 mm, respectively | 1 image per site | DICOM images, processing as by Mota (2012) [49] |
|
Morales 2018a (Spain) [43] |
PT with 3 yr of rehabilitative USI experience |
Toshiba Aplio 500 Platinum, Toshiba American Medical Systems; CA, USA; 7- to 14-MHz linear probe, 40 mm (18L7PLT-1204BT); B-mode |
Just under the navel | Not applicable | Mean IRD of 3 images | Offline measurement using ImageJ software (version 2.0; US National Institutes of Health, Bethesda, MD, USA) |
|
Morales 2018b (Spain) [58] |
PT with 3 yr of USI experience | LOGIQ S7, GE Healthcare, UK; 3.1- to 10-MHz linear probe, 44 mm (9L-D); B-mode | Same as Morales (2018a) [43] | Not applicable | Same as Morales (2018a) [43] | Offline measurement as by Morales (2018a) [43] |
|
Nanikawa 2021 (Japan) [50] |
PT accustomed to USI, after sufficient practice; intrarater reliability: within-day, ICC = 0.99; between-day, ICC = 0.98 | Noblus, Hitachi, Ltd., Tokyo, Japan; linear L64 probe (5- to 18-MHz); B-mode | Below the navel | Not applicable | Mean IRD of 2 images | Not specified |
|
Pascoal 2014 (Portugal) [36] |
not specified | Sonoline Prime SLC, Siemens, Erlangen, Germany; 7.5-MHz linear probe, 60 mm; B-mode | lower border of the probe: just cephalad to the navel (approximately 2 cm above the navel center) | Not applicable | Not specified | Images recorded on mini DV tape, converted to JPG; semi-automated offline analysis as by Mota (2012) [49] |
|
Romero-Morales 2018 (Spain) [59] |
Not specified | LOGIQ P7, GE Healthcare; UK; 4- to 13-MHz linear probe, 38 mm (L6-12-RS) | same as Morales (2018a) [43] | Not applicable | SAME as Morales (2018a) [43] | ImageJ software (version 2.0) used for offline analysis |
|
Romero-Morales 2019 (Spain) [44] |
PT with 3 yr of experience in USI of the musculoskeletal field | LOGIQ, GE, Healthcare, UK; 4- to 13-MHz linear probe, 38 mm | Same as Morales (2018a) [43] | Not applicable | same as Morales (2018a) [43] | ImageJ software (Bethesda, MD, USA) used for offline measurement |
|
Romero- Morales 2020 (Spain) [45] |
PT with 5 yr of USI experience |
LOGIQ R S7 R3 XDclear, GE Healthcare, Milwaukee, WS, USA; 5- to 15-MHz linear probe, 44 mm (GE ML6–15); B-mode |
Just above the navel (according to the photo and its legend) | Not applicable | Same as Morales (2018a) [43] | Measurement using ImageJ software (version 2.0; US National Institutes of Health, Bethesda, MD, USA) |
|
Sancho 2015 (Portugal and Norway) [73] |
PT trained in image capturing and IRD measurement | LOGIQ-e; GE Healthcare, Hatfield, UK; 4- to 12-MHz linear probe, 30 mm; B-mode | 2 cm above and below the navel center | Not applicable | The best of 3 images (per condition and site) |
images imported in JPG format; offline semi-automated analysis as by Mota (2012) [49] |
| Starzec-Proserpio 2022 (Poland) [70] | Two experienced women’s health PTs trained in the musculoskeletal USI; attended a half-day training together to promote consistency and avoid bias throughout the data collection process | Voluson P6 (GE Healthcare Syst.; Chicago, IL, USA); 4- to 12-MHz, 37-mm linear probe; palpation + caliper used to measure IRD wider than the probe | 2 cm above the navel | Not applicable | Not specified | The measuring feature was used: after capturing the image, an on-screen cursor was used to mark the IRD |
|
Theodorsen 2019 (Norway) [37] |
PT after specific training in USI of the pelvic floor and abdomen | Mindray M7; 5- to 10-MHz linear probe | Lower edge of the probe at 2 cm above and below the navel center | DRA = IRD ≥ 2 finger widths at or 2 cm above/below the navel; protrusion | 1 image per site and condition |
Image in digital format processing; use of ultrasound’s integrated measurement tool |
| Theodorsen 2022** (Norway) [75] | Women’s health PT with 21 yr of clinical experience; with specific training and clinical experience in USI of the pelvic floor and abdomen | Alpinion EC8 Diamond; 8-17 MHz linear probe, B-mode | Lower edge of the probe 2 cm above and below the navel | DRA = IRD ≥ 28 mm at the navel level and/or 2 cm above and below the navel (at rest) and/or abdominal protrusion | Not specified | JPG images will be transferred to a server and the measurements will be performed using MicroDicom software |
|
Whittaker 2013 (UK and Canada) [46] |
PT with 10 yr of USI experience; within- and between-day intrarater reliability of IRD measurement: ICC = 0.99 | MyLab 25, Esaote North America, Inc., Indianapolis, IN; 5.0-MHz curvilinear probe, 40 mm, resolution: 1.0 mm (lateral), 0.93 mm (axial); B-mode | Just inferior to the navel | Not applicable | Mean IRD of 3 images | Offline measurement using MATLAB Ver. 7.1 software, MathWorks, Inc., Natick, MA; in consultation with a video clip of IRD |
*This procedure/mode was used when IRD was too large to be visualized on conventional USI. **Registered study protocol (presenting research project). PT: physiotherapist; DRA: diastasis recti abdominis; LA: linea alba; DICOM: Digital Imaging and Communications in Medicine
Synthesis of results
To present descriptions of specific aspects of the IRD measurement procedure using USI from individual publications, three reviewers (A.O.B., D.C., and M.C.) compared charted extracts, discussed uncertain issues, resolved disagreements, and jointly made summaries of the extracts. If the studies followed the measurement procedure described in previous publications, “same as….” was stated. The citations are presented in Tables 2 and 3 in alphabetical order.
Results
Selection of sources of evidence
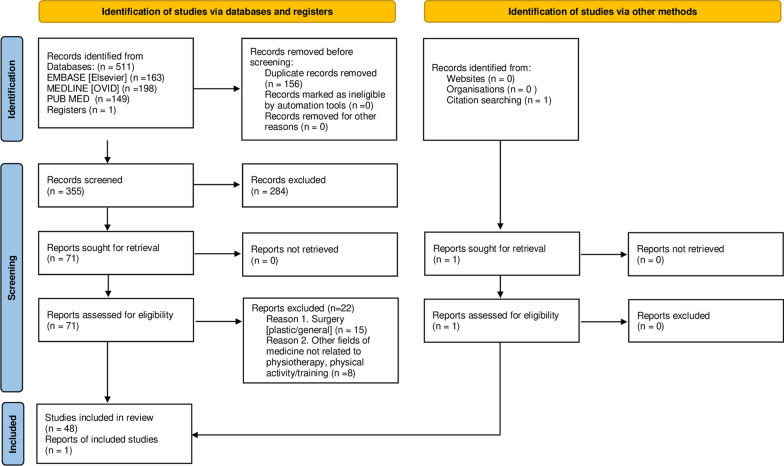
Details on the selection are presented in the PRISMA flow diagram (Fig. 1).
Fig. 1.
PRISMA-ScR flow diagram
Characteristics of sources of evidence
All 49 included publications (published between 2008 and August 2022) were related to physiotherapy or physical exercise/training and described IRD measurements using USI.
Eight studies were from Canada [8, 17, 20, 33, 48, 53–55] and nine from Spain [11, 42–45, 56–59]. Countries with two studies were Brazil [60, 61], the USA [9, 62], the UK [16, 63], Norway [13, 37], New Zealand [47, 64], and China [65, 66]. Countries with one study were Israel [27], Australia [67], Japan [50], Italy [10], Sweden [68], Taiwan [18], Portugal [36], Korea [69], and Poland [70]. Six 2-center studies were from Portugal and Norway [15, 35, 49, 71–73], and one from Italy and Canada [12], Australia and Canada [34], the UK and Canada [46], and Spain and Canada [74]. One registered study protocol was from Norway [75].
Results of the individual sources of evidence
Table 2 presents study objectives, populations, and IRD measurement conditions; Table 3 shows the examiners’ experience, USI systems, and IRD measurement methods.
Synthesis of the results
The main objectives of the 49 studies are presented in Additional file 1: S6—Objectives of the Studies.
Population
Of the 49 publications, 36 (73.5%) concerned women in their perinatal periods: In 31, the assessment was scheduled after pregnancy/pregnancies in [8, 10, 12, 13, 16–18, 20, 27, 33, 34, 36, 37, 48, 49, 53–56, 60, 63–71, 73, 74], in four during and after pregnancy [15, 35, 72, 75], and in one during pregnancy (2.8%) [61]; 17 publications concerned women with increased IRD/DRA [8, 10, 13, 15, 17, 20, 27, 33, 34, 37, 48, 53, 64, 65, 68, 69, 75]. In 13 of the 49 studies (26.5%), the study populations comprised of men and/or women (nulliparas and/or paras): Three were validity/reliability studies [47, 50, 62], three investigated the impact of specific tasks on IRD [9, 11, 58], five assessed the IRD in medical conditions not related to pregnancy [44–46, 57, 59], and two investigated the IRD in athletes [42, 43] (Table 2).
Body position, muscle activity, and breathing during the IRD examination
In all 49 studies, the IRD was measured in the supine position: in 26 (53.1%), at rest and during muscle activity/task [8, 9, 11, 13, 27, 34–37, 47–49, 53, 55–60, 62, 64, 67, 70, 71, 73, 74], in 21 (42.9%), only at rest [10, 12, 15–18, 20, 33, 42–46, 50, 54, 65, 66, 68, 69, 72, 75], in one (2%), only during muscle activity/task [61], and in one (2%), in supine (at rest), and in sitting and standing [63]. One of the studies also performed measurements in side plank position [64].
Of the 27 studies that examined IRD during specific muscle activity/task in supine, some used more than one task. The tasks were head lift [8, 13, 48, 53, 55], trunk flexion with scapulae raised fully or partially off the coach (referred to as trunk flexion [60, 61], partial curl-up [9, 47, 62], semi curl-up [8, 74], curl-up [13, 27, 34, 56, 64, 70], abdominal crunch [11, 35, 36, 49, 71, 73], modified abdominal sit-up [67], and abdominal contraction [56]), transversus abdominis contraction/abdominal drawing-in maneuver (ADIM) [13, 35, 37, 49, 56, 58, 73, 74], curl-up/abdominal crunch with preactivated transversus abdominis (by ADIM [11, 73, 74] or pelvic floor muscles (PFM) contraction [34]), exclusive PFM contraction [13, 37], combined PFM contraction and curl-up [13], combined PFM contraction and ADIM [13, 37, 64], abdominal hypopressive exercise (AHE) [11, 74], pelvic tilt [13], twisted curl-up (to the left and right) [13], calf muscle maximal isometric contraction [59], Sahrmann early level single leg raise combined with ADIM, ADIM with Tubigrip and ADIM with taping, curl-up with Tubigrip, and curl-up with taping [64].
Of the 49 study protocols, 14 (28.6%) mentioned supporting the examinee’s head on a pillow during IRD measurement in the supine position [8–10, 20, 34, 37, 47, 48, 54, 55, 57, 62, 63, 75]. Thirty-one (63.3%) of the 49 protocols specified the examinees’ lower extremity position in supine: In 30, the lower extremities were flexed (for the measurements at rest [10, 15–18, 45, 63, 68, 72, 75], at rest and during specific task/tasks [9, 11, 13, 27, 34–37, 47, 49, 56, 57, 60, 62, 64, 67, 71, 73, 74], and during specific tasks only [61]), and in one they were extended (for the measurements at rest and during head lift) [53].
Of the 30 protocols using flexed lower extremities, in 26 examinees’ feet were supported on the examination table [9–11, 13, 15, 17, 27, 34–37, 45, 47, 49, 60–64, 67, 68, 71–75] (16 specified that knee flexion angle was 90° [11, 15, 27, 35–37, 47, 49, 63, 64, 67, 68, 71–73, 75]), in 3, one [56] or two pillows [16, 18] were placed under the examinees’ knees, and in one the method of obtaining lower extremity flexion was not specified [57] (Table 2).
Of the 49 studies, in 32 (65.3%), IRD images were captured during a specific moment of the breathing phase: in 27 at the end of normal expiration [8, 11–13, 15, 17, 18, 27, 35–37, 42, 43, 45–47, 49, 50, 59, 63, 67, 68, 71–73, 75], in two in a neutral moment immediately after expiration [10, 64], in two during expiration [54, 61], and in one the breathing pattern/phase was related to a specific exercise [74] (Table 2).
Examiners and examination tools
Of the 49 protocols, 36 (73.5%) specified the examiner’s profession: In 31 protocols, it was a physiotherapist [1, 8, 11, 12, 15, 17, 18, 35, 37, 42–50, 53, 55, 56, 58, 63, 64, 67, 70–75], in two registered sonographers [20, 33], in one physicians [66], in one a physician specializing in gynecological USI [27], and in one a radiologist [65]. Of the 49 protocols, 41 (83.7%) included information on the examiner’s training and/or experience in USI [8–13, 15, 17, 18, 20, 27, 33, 35, 37, 42–50, 53–58, 61–65, 67, 70–75] (34 described type of examiner’s training/expertise [8–13, 15, 17, 18, 20, 27, 33, 35, 37, 43, 44, 47–49, 53–56, 58, 62, 63, 65, 67, 70–75] and 25 training and/or experience duration [8–10, 12, 17, 18, 33, 35, 43–48, 53–56, 58, 62, 65, 67, 70, 74, 75]). Twelve studies reported the reliability of the IRD measurements using USI [8, 18, 46–50, 54, 55, 62–64]. (Six of them were reliability studies [47–50, 55, 63].)
Forty-eight (97.9%) of 49 protocols described ultrasound transducer type: 43 chose linear probe [8, 10–13, 15–18, 20, 33–37, 42–45, 47–50, 53–61, 63, 65–68, 70–75], three curvilinear [9, 46, 62], one both types [64], and one provided unclear information [69]. Forty-six protocols specified probe frequency (3–18 MHz); 27 provided probe size (3–11 cm) [12, 15–18, 33, 35, 36, 42–46, 49, 53, 54, 58, 59, 63, 66–68, 70–74]. Eleven studies used additional features, settings, or products (panoramic imaging [13, 20, 33, 54, 56, 68], trapezoid mode [10, 17, 53], and acoustic standoff pad [48, 54, 55]) that enabled field of view extension, one compared IRD measurements using low and high ultrasound resolutions [47] (Table 3).
Measurement sites
Of the 49 protocols, 16 (32.6%) used one measurement site [12, 15, 16, 36, 42–46, 50, 54, 58, 59, 68–70]; another 16 (32.6%) two sites [9–11, 13, 34, 37, 47, 49, 53, 56, 57, 62, 64, 71, 73, 75]; nine (18.4%) three sites [8, 17, 27, 35, 61, 63, 66, 72, 74]; seven (14.3%) four sites [18, 20, 33, 48, 55, 60, 67]; and one (2%) five sites [65]. However, of the 39 studies on pregnancy-related IRD, only seven (17.9%) used one measurement site [12, 15, 16, 36, 54, 68, 69], while of the 10 studies on non-pregnancy-related IRD, one measurement site was used in nine (90%) protocols [42–46, 50, 58, 59, 70].
In 26 (53.1%) of the 49 study protocols, the IRD measurements were made at the superior umbilical border (16/26, 61.5%) [8, 11, 16–18, 20, 27, 33, 34, 36, 45, 48, 54, 55, 63, 67] and/or at the inferior umbilical border (9/26, 34.6%) [18, 42–44, 46, 50, 58, 59, 67] (two studies used both sites [18, 67]), and directly at the umbilicus (3/26, 11.5%) [61, 65, 66].
In 38 (77.5%) of the 49 study protocols, more distant measurement sites were chosen: supraumbilical in 37 (97.4%) [8–13, 17, 18, 20, 27, 33–35, 37, 47–49, 53, 55–57, 60–75] and/or infraumbilical in 27 (71%) [9, 10, 13, 15, 18, 20, 27, 33, 35, 37, 47–49, 55–57, 61–65, 67, 71–75]. (26 of these protocols used both locations [9, 10, 13, 18, 20, 27, 33, 35, 37, 47–49, 55–57, 61–65, 67, 71–75].) Supraumbilical measurements were made at 2 cm [12, 13, 35, 37, 47, 49, 56, 64, 70–75], 2.5 cm [18, 69], 3 cm [8, 10, 17, 20, 27, 33, 48, 53, 55, 60, 61, 66], 4.5 cm [9, 57, 62, 67, 68], 5 cm [8, 17, 20, 33, 35, 48, 53, 55, 72], and 6, 9, and 12 cm [60] above the umbilicus; a third of the distance [63] and halfway [11, 34, 74] between the umbilicus and xiphoid, and at subxiphoid and epigastric sites [65].
Infraumbilical measurements were taken at 2 cm [13, 15, 27, 35, 37, 47, 49, 56, 61, 64, 71–75], 2.5 cm [18], 3 cm [10, 20, 33, 48, 55, 66], and 4.5 cm [9, 57, 62, 67] below the umbilicus, halfway between the umbilicus and pubis [63], and at infraumbilical and suprapubic sites [65].
Of the 38 protocols describing supra- and infraumbilical measurement sites, 37 indicated starting points to identify them: 25 precisely indicated these points [8, 9, 11, 13, 15, 18, 20, 33–35, 37, 48, 49, 55–57, 62, 64, 67–69, 71–74] (14 indicated umbilical midpoint [9, 13, 15, 35, 37, 49, 57, 62, 64, 68, 71–74], and 11 superior and/or inferior umbilical borders [8, 11, 18, 20, 33, 34, 48, 55, 56, 67, 69]); 12 less precisely indicated that the sites were measured from the umbilicus [10, 12, 17, 27, 47, 53, 60, 61, 63, 66, 70, 75] (Table 3).
Screening subjects for DRA
Of the 49 study designs, 19 required screening subjects for DRA/increased IRD: 12 studies chose USI for screening [8, 10, 13, 15, 17, 27, 34, 53, 61, 67, 69, 75]; however, only nine of them referred to normative values (eight [8, 15, 17, 27, 34, 53, 61, 67] referred to “normal” linea alba width values for nulliparas [76] and one [75], to “normal” IRD for postpartum primiparas [72]); nine studies used a palpatory clinical test [77, 78] for screening [13, 20, 33, 37, 48, 64, 65, 68, 69]. (Two performed screening using both USI and palpation [13, 69].) In one study, tape measurement DRA classification [79] was used for screening [13], and in three study protocols, abdominal wall protrusion [80] was an additional inclusion criterion for DRA [13, 37, 75]. Studies used different measurement conditions (i.e., body position, muscle activity, measurement sites) for screening and differently interpreted the palpatory examination outcomes. One study determined “normal” IRD values for primiparas in pregnancy and postpartum [72]. Another study proposed DRA pattern classification [10] (Table 3).
Number of images per measurement site. In 25 (51%) of the 49 studies, more than one image was captured at each measurement site to calculate the mean values of IRD: The mean IRD of three, five, and two images was used in 15 [8, 10, 17, 18, 42–46, 56, 58, 59, 61, 68, 73], five [20, 33, 48, 54, 55], and five [16, 50, 63, 64, 74] studies, respectively. One study used the best of three images at each measurement site [73]. Three studies just mentioned that two [53, 67] or three [34] images were taken per measurement site; five used single images [13, 35, 37, 49, 72]; and 15 did not specify the number of images per sites [9, 11, 12, 15, 27, 36, 57, 60, 62, 65, 66, 69–71, 75] (Table 3).
Image processing and measurement methods
In 38 (77.5%) of the 49 studies, the methods of frozen image processing and IRD measurement were described: 27 indicated offline processing (26 specified software type [13, 15–17, 27, 34–36, 42–46, 48, 49, 53–55, 58, 59, 63, 68, 71–73, 75]), three indicated the measurement tool/software integrated into the ultrasonographic scanner [8, 37, 47], and eight on-screen measurement [9, 11, 18, 62, 65, 69, 70, 74]. In four studies, the procedure included video capturing [8, 34, 36, 46] (Table 3).
Discussion
Summary of evidence
This scoping review aimed to present IRD measurement procedures using USI that have been used in physiotherapy-related research. Using the IRD measurement method descriptions from the 49 systematically mapped original peer-reviewed publications, the data were synthesized. The review indicates that the studies used different approaches regarding specific aspects of the IRD measurement procedure which, to a great extent, restrict or prevent cross-study comparisons. Based on the synthesis of the results, practical conclusions and recommendations on the standardization of the procedure for future physiotherapy research and clinical use have been made.
The first synthesized aspects of the IRD measurement procedure were the examinee’s body position, specific muscle activity/task, and breathing phase during image capturing. In all 49 publications, the supine position was the basic body position for IRD examination. Depending on the study aim, this position was used to measure the IRD at rest, and/or as a starting position to perform a specific task for IRD measurement during muscle activity. Several protocols included information that in the supine position, the examinee’s head was rested on a pillow. Slight head elevation improves the examinee’s comfort and should not interfere with IRD measurements. However, pillows of unspecified sizes do not allow a uniform angle of neck flexion. To standardize the head position, an examination table with adjustable headrest that can be elevated to the desired angle (i.e., 15°) might be considered.
The majority of protocols specified the examinees’ lower extremity position during the IRD examination, and in almost all of them, it was hip and knee flexion. For the examinations at rest and/or during specific tasks, lower extremity flexion was attained by supporting feet on the examination table. The knee flexion angle of 90° was the most frequent. However, in a few studies lower extremity flexion was obtained by placing one or two pillows under the examinees’ knees. To ensure reproducibility, the lower extremity position during the IRD measurement in the supine position should be described in detail. The pillow of unspecified size placed under the examinees’ knees does not allow for reproducing the lower extremity position. Instead of pillows, the examiners may consider a foam roller. For instance, a foam roller of 15 cm in diameter ensures slight hip and knee flexion and enhances the examinee’s comfort in the supine position. The position involving slight lower extremity flexion may be useful, especially if the IRD is measured only at rest.
If the IRD is measured in supine with greater hip and knee flexion angles, this position may be accompanied by reduced anterior pelvic inclination/tilt angle [81]. It should be accounted for that as a result of the increased posterior pelvic tilt, the linea alba insertion at the pubic symphysis and its origin at the xiphoid come closer, and the anterior abdominal wall structures relax. Theoretically, this position may alter the linea alba length, tension, and width; however, to the authors’ knowledge, this has not been investigated. Considering pelvifemoral motion during hip flexion [81], we recommend that researchers provide at least the magnitude of the examinee’s knee flexion angle when using the crook-lying position with feet supported on the examination table. In one study, the authors attempted to standardize the pelvic inclination and examined the IRD after teaching the examinee to maintain a neutral pelvic position [63]. The study was also the only one that used sitting and standing positions in addition to supine for IRD measurement [63]. The measurement in vertical positions is an interesting approach from the perspective of physiotherapy. It may allow to, for example, determine the effects of specific treatments in DRA subjects on their linea alba parameters during postural abdominal muscle tone and increased load on the anterior abdominal wall structures compared to relaxed supine position.
Most protocols included information that IRD images were captured during a specific moment in the breathing phase and most commonly, it was at the end of normal expiration. During resting ventilation, the abdominal cavity volume and intra-abdominal pressure are modulated depending on the respiratory phase; therefore, the tension of the anterior abdominal wall soft tissues, including linea alba, fluctuates. It has been also suggested that normal expiration is accompanied by some engagement and increased thickness of the abdominal muscles [82, 83]. As the linea alba is formed by interlacing abdominal muscle aponeuroses [6], it can be assumed that its tension and width may also change during the respiratory cycle. Ultrasound images should therefore be captured at the same phase of the breathing cycle (specified in the description of the measurement procedure). The approach to capture images at the end of normal expiration is consistent with previous recommendations on the evaluation of the abdominal muscle parameters and IRD with USI [84, 85].
In this review, the characteristics of the examination tools, selection of IRD measurement sites, and methods of DRA screening were also synthesized. Most studies used linear transducers (a few curvilinear) with frequencies ranging from 3 to 18 MHz. In over half of the protocols, transducer’s size was provided, ranging from 3 to 11 cm (most often, 4 cm). Some protocols specified additional features, settings, or products used, such as panoramic imaging, trapezoid mode, and acoustic standoff pad to extend the field of view to measure wider DRA. Acoustic standoff pad and panoramic mode have been suggested to be valid methods to measure the IRD of up to three finger widths. However, further research is needed on the validity and reliability of the extended field-of-view methods for greater IRD [54]. Sufficient training and experience in the use of panoramic USI are also of importance [86].
This scoping review indicates researchers used 1 to 5 measurement sites during their IRD assessments. Most studies that investigated pregnancy-related IRD/DRA used more than one measurement site, while the great majority of studies on individuals with other medical conditions and athletes performed measurements only at one site. As linea alba width changes along its course [6, 10, 72, 76, 87, 88], examining more than one location is important. This review confirms its relevance in research on pregnancy-related IRD/DRA.
Concomitantly, the comparison of findings across studies is only possible if IRD measurements are made at the same anatomical location. This scoping review indicates there is no consistency between study protocols regarding this aspect. The IRD was examined at the superior and/or inferior umbilical borders and at various levels (between 2 and 12 cm) above and (between 2 and 4.5 cm) below the umbilicus. A few protocols presented a valuable approach to supra- and infraumbilical site selection by taking into account the inter-individual variability in the linea alba length (i.e., the distances from the umbilicus to the linea alba origin and insertion). The measurements were performed at a third of the distance [63] or halfway [11, 34, 74] between the umbilicus and xiphoid, and halfway between the umbilicus and pubis [63].
This review also indicates the IRD was more frequently examined at the superior than at the inferior umbilical border, and above than below the umbilicus. In addition, most infraumbilical measurement sites were relatively close to the umbilicus. When choosing the measurement sites along the linea alba, the current knowledge on the measurement reliability at specific locations should be considered [47–50, 55, 63]. According to a systematic review and meta-analytical reliability generalization [7] and subsequent reliability studies [48, 63], the reliability of IRD measurements using USI is high; however, it is slightly lower for infraumbilical than for supraumbilical measurements. Infraumbilical measurements are more challenging because, at this anatomical location, the posterior rectus sheath is hardly visible [48, 89]. In women with DRA and history of cesarean section, the infraumbilical measurements using USI have been reported inaccurate compared to intraoperative surgical compass measurements. The researchers suggested that their difficulty in measuring the IRD at that location was due to the cesarean section-related fibrosis and loss of definition of the posterior layer of the recti muscles [89]. This is consistent with the cadaver study that indicated the posterior rectus sheath below the umbilicus consisted of much thinner collagen fibers than the fibers of the posterior rectus sheath above the umbilicus [6]. It is therefore possible that less frequent use of infraumbilical measurement sites indicated by this scoping review was due to the greater difficulty to measure the IRD at this location. Considering this, it is important to determine measurement reliability at specific sites before the primary investigation, as performed in several studies [8, 18, 46, 54, 62]. It should be noted that measurement reliability may also depend on the examiner’s experience [7, 47].
Most protocols that included IRD measurements away from the umbilicus specified the starting points from which the anatomical locations were measured. These starting points were the umbilical midpoint, and the superior and/or inferior umbilical borders (for locations above and/or below the umbilicus, respectively). To enable cross-study comparisons, we propose the superior umbilical border as the standard starting point to determine supra- and infraumbilical measurement sites. This would reduce possible discrepancies in determining these locations caused by inter-individual variability in the size of the umbilical ring.
Considering the need to standardize the measurement protocol to facilitate cross-study comparisons [7, 39, 40] and the synthesis of results in this scoping review, we propose four basic measurement sites:
half of the superior umbilical border-xiphoid distance;
a quarter of the superior umbilical border-xiphoid distance (most proximal to the umbilicus);
the superior umbilical border;
a quarter of the superior umbilical border-pubis distance (most proximal to the umbilicus; Fig. 2).
Fig. 2.
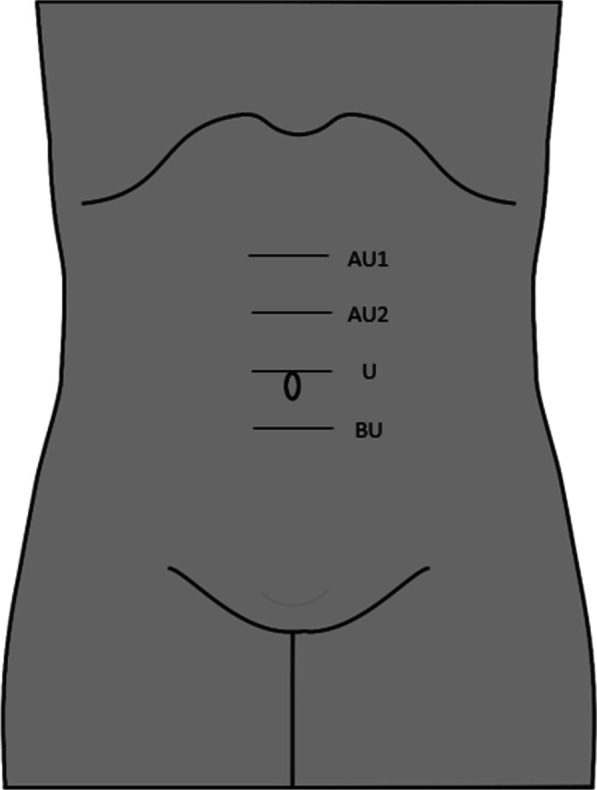
Proposed sites for inter-recti distance measurement using ultrasonographic imaging based on the scoping review results synthesis. AU1: ½ of the superior umbilical border-xiphoid distance; AU2: ¼ of the superior umbilical border-xiphoid distance; U: the superior umbilical border; and BU: ¼ of the superior umbilical border-pubis distance
We recommend the locations of a quarter of the superior umbilical border-xiphoid/pubis distances as they roughly correspond to locations 4.5/5 cm above/below the umbilicus, which have been frequently applied. When choosing measurement sites in women with pregnancy-related DRA, it should be remembered that supraumbilical DRA patterns are the most common, and in the case of complete opening, the diastasis is usually wider above the umbilicus [10].
More than half of the protocols included information that 2–5 images were taken per site to calculate measurement means (most often the mean IRD of three images). In one study, the best of three images per site was used for the measurement [73]. Higher intrarater and interrater reliability and lower intrarater measurement error were demonstrated when using means of 2 or 3 consecutive measurements in determining specific abdominal muscle parameters with musculoskeletal USI [1, 90]. Therefore, to enhance measurement precision, we propose to use the mean value of three measurements taken at each anatomical location. This may be of particular importance when the assessment is performed by a less experienced examiner.
Our synthesis revealed researchers used different selection methods and criteria to identify subjects with or without DRA. Most researchers used ultrasound screening with cutoff values for “normal” linea alba width that had been determined by Beer et al. [76]. In that study, the examinees were in the supine resting position with the lower extremities extended; the measurement sites were at the xiphoid, 3 cm above and 2 cm below the umbilicus [76]. For consistency, these measurement conditions and sites should be followed during screening for DRA. However, some of the studies modified the procedure.
It is still unclear what IRD values (obtained by USI) should be considered physiological and pathological from the perspective of proper functioning of the abdominal wall structures [14, 38–40]. Normative IRD values of up to 15 mm at the xiphoid, up to 22 mm at 3 cm above the umbilicus, and up to 16 mm at 2 cm below the umbilicus were designated using the 90th percentile. The investigators suggested that DRA could be anticipated beyond these values with an error rate of 10%. The study also presented the population’s extreme linea alba widths, which were 31 mm at the xiphoid, 35 mm at 3 cm above the umbilicus, and 31 mm at 2 cm below the umbilicus. They concluded that the DRA could be anticipated beyond these values without doubt [76]. Another study proposed the cutoff values for “normal” IRD in primiparas using the 80th percentile of the values obtained in 84 females in their perinatal period. At six months postpartum, these values were 24 mm at 5 cm above the umbilicus, 28 mm at 2 cm above the umbilicus, and 21 mm at 2 cm below the umbilicus. The authors suggested that, in primiparas, the IRD might be considered “normal” up to values wider than for nulliparas [72]. Further investigation is warranted to clarify the DRA diagnostic criteria based on USI. Also, systematic mapping and verification of the quality of the existing studies that determined “normal” IRD cutoff values using different methods may provide additional information on what is already known and in what direction future research should proceed. Regarding physiotherapy research and practice, we suggest establishing normative values for measurement sites specified in Fig. 2. It is worth mentioning that musculoskeletal USI can also be used to inspect the entire linea alba from its origin to insertion to determine the DRA pattern and identify the location of the greatest IRD [10].
Several reviewed studies used a palpatory clinical test to screen subjects for DRA. This test is performed during abdominal muscle activation to facilitate palpation. The examinee lies in a supine position with the knees bent (at 90°) and feet resting on the examination table. The examinee is asked to raise the head and shoulders upward (until the spines of the scapulae leave the examination table). To palpate the IRD, the examiner places fingers horizontally across the midline of the examinee’s abdomen at the umbilicus. The same procedure is then repeated above and below the umbilicus [67, 71, 77, 78]. This clinical test has shown good [71] and very good [67] intrarater reliability, and moderate [71] or moderate-to-good [67] interrater reliability. The test result is considered negative when a maximum of two-finger widths can be placed between the medial parts of the right and left recti muscle bellies and/or when the fingers do not sink into the gap between the muscles, and/or no linea alba bulging or slumping is present [77–79]. This review revealed that some modifications to the test execution have been introduced by researchers, e.g., the IRD palpation during head lift instead of head and shoulder lift [20, 33, 48]. Such an approach may influence test results because abdominal muscle engagement is different between the two tasks [13, 77, 78]. Another modification concerns the interpretation of the test outcome; some studies classified two- and not more than two-finger widths as DRA [13, 20, 33, 37, 48].
Although the palpatory clinical test [77, 78] is the easiest and fastest screening procedure for DRA, the limits of agreement between this assessment method and USI are wide [67]. We believe palpatory test results of DRA = IRD > two-finger width [77, 78] should be used as indicative only. The two-finger width equals approximately 3 cm; however, it may differ especially between male and female examiners. The original interpretation of the test result as positive or negative also fails to consider the fact that normal linea alba is narrower above and below the umbilicus compared to its width at the umbilicus [6]. Therefore, IRD palpation should be combined with caliper measurement, which is a reliable and valid method [62, 67]. It would be necessary though to determine “normal” IRD values during abdominal muscle activity under standardized conditions using a caliper. Notwithstanding, the strength of the palpatory method is that it enables identifying linea alba slumping or bulging during abdominal muscle activation [79]. It also enables examination of the entire linea alba for the DRA pattern.
Limitations
The limitation of this scoping review is that the publications were searched for in three major databases. Therefore, some studies might have been omitted. Also, only research papers published in English have been included.
Conclusions
This scoping review indicates that most studies provided a detailed description of IRD measurement using USI. IRD examination was typically made with the subject in the supine position. A majority of the examinees had their hips and knees flexed. Most studies captured images at the end of normal expiration. Different measurement sites and starting points to determine supra- and infraumbilical sites were used. Most studies used linear transducers of widths and frequencies 3–11 cm and 3–18 MHz, respectively. To enhance the IRD measurement precision, most studies captured more than one image at each measurement site, and calculated the mean values of the measurements. Different approaches were used to screen subjects for DRA. Further investigation on USI-based measurements (following the protocol proposed in this review) is warranted to clarify the DRA diagnostic criteria. Determining “normal” IRD values using a caliper during abdominal muscle activity (following protocol for palpatory clinical test [67, 71, 77, 78]) should be also considered.
To facilitate the IRD measurement procedure reproducibility and cross-study comparisons, the following protocol standardization for the examination in supine is proposed based on result synthesis:
the headrest of the examination table elevated by 15°; a foam roller (15 cm in diameter) under the knees or the knees flexed to 90° with the feet on the examination table;
image acquisition at the end of normal expiration;
measurement sites: (1) half of the superior umbilical border-xiphoid distance, (2) a quarter of the superior umbilical border-xiphoid distance (most proximal to the umbilicus), (3) the superior umbilical border, and (4) a quarter of the superior umbilical border-pubis distance (most proximal to the umbilicus; Fig. 2);
use of mean IRD value of three images per measurement site as measurement outcome.
Supplementary Information
Additional file 1. Supplementary documents: PRISMA-ScR Checklist, Publication Relevance Screening Form I, Publication Relevance Screening Form II, Explanation and Elaboration Document, Data Charting Form, and Objectives of the Studies.
Abbreviations
- ADIM
Abdominal draw-in maneuver
- AHE
Abdominal hypopressive exercise
- BMI
Body mass index
- DICOM
Digital Imaging and Communications in Medicine
- DRA
Diastasis recti abdominis
- IRD
Inter-recti distance
- LA
Linea alba
- PFM
Pelvic floor muscles
- PRISMA-ScR
Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews
- PT
Physiotherapist
- RA
Rectus abdominis
- TrA
Transversus abdominis
- USI
Ultrasound imaging
Author contributions
AOB and DC contributed equally to this work. AOB, DC, and MC substantially contributed to the conception and design of the work. DC coordinated the study. AOB, DC, MRZ, and JN were involved in data collection. AOB, DC, MRZ, JN, and MC were involved in data management. AOB, DC, and MC synthesized the results. AOB, DC, MC, JB, KG, AGP, and PM interpreted the data. AOB drafted the work. DC, MC, JB, KG, AGP, and PM substantively revised the manuscript for important intellectual content. All authors reviewed the manuscript and approved the submitted version.
Funding
The Jerzy Kukuczka Academy of Physical Education has funded the article’s editorial expenses.
Availability of data and materials
The data sets supporting the conclusions of this article are included within the article (Fig. 1, Tables 2 and 3).
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Agnieszka Opala-Berdzik and Daria Chmielewska have contributed equally to this work.
References
- 1.Gnat R, Saulicz E, Miądowicz B. Reliability of real-time ultrasound measurement of transversus abdominis thickness in healthy trained subjects. Eur Spine J. 2012;21:1508–1515. doi: 10.1007/s00586-012-2184-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Linek P, Wolny T, Sikora D, Klepek A. Intrarater reliability of shear wave elastography for the quantification of lateral abdominal muscle elasticity in idiopathic scoliosis patients. J Manipulative Physiol Ther. 2020;43:303–310. doi: 10.1016/j.jmpt.2018.11.034. [DOI] [PubMed] [Google Scholar]
- 3.Richardson CA, Snijders CJ, Hides JA, Damen L, Pas MS, Storm J. The relation between the transversus abdominis muscles, sacroiliac joint mechanics, and low back pain. Spine (Phila Pa 1976) 2002;27:399–405. doi: 10.1097/00007632-200202150-00015. [DOI] [PubMed] [Google Scholar]
- 4.Scott JM, Martin DS, Ploutz-Snyder R, Caine T, Matz T, Arzeno NM, Buxton R, Ploutz-Snyder L. Reliability and validity of panoramic ultrasound for muscle quantification. Ultrasound Med Biol. 2012;38:1656–1661. doi: 10.1016/j.ultrasmedbio.2012.04.018. [DOI] [PubMed] [Google Scholar]
- 5.Whittaker JL, Teyhen DS, Elliott JM, Cook K, Langevin HM, Dahl HH, Stokes M. Rehabilitative ultrasound imaging: understanding the technology and its applications. J Orthop Sports Phys Ther. 2007;37:434–449. doi: 10.2519/jospt.2007.2350. [DOI] [PubMed] [Google Scholar]
- 6.Axer H, Keyserlingk DG, Prescher A. Collagen fibers in linea alba and rectus sheaths. I. General scheme and morphological aspects. J Surg Res. 2001;96:127–134. doi: 10.1006/jsre.2000.6070. [DOI] [PubMed] [Google Scholar]
- 7.van de Water ATM, Benjamin DR. Measurement methods to assess diastasis of the rectus abdominis muscle (DRAM): a systematic review of their measurement properties and meta-analytic reliability generalization. Man Ther. 2016;21:41–53. doi: 10.1016/j.math.2015.09.013. [DOI] [PubMed] [Google Scholar]
- 8.Beamish N, Green N, Nieuwold E, McLean L. Differences in linea alba stiffness and linea alba distortion between women with and without diastasis recti abdominis: the impact of measurement site and task. Orthop Sports Phys Ther. 2019;49:656–665. doi: 10.2519/jospt.2019.8543. [DOI] [PubMed] [Google Scholar]
- 9.Chiarello CM, McAuley JA, Hartigan EH. Immediate effect of active abdominal contraction on inter-recti distance. J Orthop Sports Phys Ther. 2016;46:177–183. doi: 10.2519/jospt.2016.6102. [DOI] [PubMed] [Google Scholar]
- 10.Corvino A, Rosa D, Sbordone C, Nunziata A, Corvino F, Varelli C, Catalano O. Diastasis of rectus abdominis muscles: patterns of anatomical variation as demonstrated by ultrasound. Pol J Radiol. 2019;84:e542–e548. doi: 10.5114/pjr.2019.91303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Da Cunã-Carrera I, Soto-Gonzalez M, Alonso-Calvete A, Gonzalez-Gonzalez Y, Lantaron-Caeiro EM. Immediate effects of different types of abdominal exercises on the inter-rectus distance. Isokinet Exerc Sci. 2021;29:31–37. doi: 10.3233/IES-203161. [DOI] [Google Scholar]
- 12.Fan C, Guidolin D, Ragazzo S, Fede C, Pirri C, Gaudreault N, Porzionato A, Macchi V, De Caro R, Stecco C. Effects of cesarean section and vaginal delivery on abdominal muscles and fasciae. Medicina (Kaunas) 2020;56:260. doi: 10.3390/medicina56060260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gluppe SB, Engh ME, Bø K. Immediate effect of abdominal and pelvic floor muscle exercises on interrecti distance in women with diastasis recti abdominis who were parous. Phys Ther. 2020;100:1372–1383. doi: 10.1093/ptj/pzaa070. [DOI] [PubMed] [Google Scholar]
- 14.Mota P, Pascoal AG, Bø K. Diastasis recti abdominis in pregnancy and postpartum period. Risk factors, functional implications and resolution. Curr Womens Health Rev. 2015;11:59–67. doi: 10.2174/157340481101150914201735. [DOI] [Google Scholar]
- 15.Fernandes da Mota PG, Pascoal AG, Carita AI, Bø K. Prevalence and risk factors of diastasis recti abdominis from late pregnancy to 6 months postpartum, and relationship with lumbo-pelvic pain. Man Ther. 2015;20:200–205. doi: 10.1016/j.math.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 16.Coldron Y, Stokes MJ, Newham DJ, Cook K. Postpartum characteristics of rectus abdominis on ultrasound imaging. Man Ther. 2008;13:112–121. doi: 10.1016/j.math.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 17.Hills NF, Graham RB, McLean L. Comparison of trunk muscle function between women with and without diastasis recti abdominis at 1 year postpartum. Phys Ther. 2018;98:891–901. doi: 10.1093/ptj/pzy083. [DOI] [PubMed] [Google Scholar]
- 18.Liaw LJ, Hsu MJ, Liao CF, Liu MF, Hsu AT. The relationships between inter-recti distance measured by ultrasound imaging and abdominal muscle function in postpartum women: a 6-month follow-up study. J Orthop Sports Phys Ther. 2011;41:435–443. doi: 10.2519/jospt.2011.3507. [DOI] [PubMed] [Google Scholar]
- 19.de Brito MJ, Nahas FX, Barbosa MV, Dini GM, Kimura AK, Farah AB, Ferreira LM. Abdominoplasty and its effect on body image, self-esteem, and mental health. Ann Plast Surg. 2010;65:5–10. doi: 10.1097/sap.0b013e3181bc30f7. [DOI] [PubMed] [Google Scholar]
- 20.Keshwani N, Mathur S, McLean L. Relationship between interrectus distance and symptom severity in women with diastasis recti abdominis in the early postpartum period. Phys Ther. 2018;98:182–190. doi: 10.1093/ptj/pzx117. [DOI] [PubMed] [Google Scholar]
- 21.Akram J, Matzen SH. Rectus abdominis diastasis. J Plast Surg Hand Surg. 2014;48:163–169. doi: 10.3109/2000656X.2013.859145. [DOI] [PubMed] [Google Scholar]
- 22.Claus CMP, Malcher F, Cavazzola LT, Furtado M, Morrell A, Azevedo M, Meirelles LG, Santos H, Garcia R. Subcutaneous onlay laparoscopic approach (SCOLA) for ventral hernia and rectus abdominis diastasis repair: technical description and initial results. Arq Bras Cir Dig. 2018;31:e1399. doi: 10.1590/0102-672020180001e1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Olsson A, Kiwanuka O, Wilhelmsson S, Sandblom G, Stackelberg O. Cohort study of the effect of surgical repair of symptomatic diastasis recti abdominis on abdominal trunk function and quality of life. BJS Open. 2019;3:750–758. doi: 10.1002/bjs5.50213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reinpold W, Köckerling F, Bittner R, Conze J, Fortelny R, Koch A, Kukleta J, Kuthe A, Lorenz R, Stechemesser B. Classification of rectus diastasis-a proposal by the German Hernia Society (DHG) and the International Endohernia Society (IEHS) Front Surg. 2019;6:1–6. doi: 10.3389/fsurg.2019.00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bø K, Hilde G, Tennfjord MK, Sperstad JB, Engh ME. Pelvic floor muscle function, pelvic floor dysfunction and diastasis recti abdominis: prospective cohort study. Neurourol Urodyn. 2017;36:716–721. doi: 10.1002/nau.23005. [DOI] [PubMed] [Google Scholar]
- 26.Dalal K, Kaur A, Mitra M. Correlation between diastasis rectus abdominis and lumbopelvic pain and dysfunction. Indian J Physiother Occup Ther. 2014;8:210–214. doi: 10.5958/J.0973-5674.8.1.040. [DOI] [Google Scholar]
- 27.Eisenberg VH, Sela L, Weisman A, Masharawi Y. The relationship between diastasis rectus abdominus, pelvic floor trauma and function in primiparous women postpartum. Int Urogynecol J. 2021;32:2367–2375. doi: 10.1007/s00192-020-04619-4. [DOI] [PubMed] [Google Scholar]
- 28.Parker MA, Millar AL, Dugan SA. Diastasis rectus abdominis and lumbopelvic pain and dysfunction: are they related? J Womens Health Phys Ther. 2009;33:15–22. doi: 10.1097/01274882-200933020-00003. [DOI] [Google Scholar]
- 29.Sperstad JB, Tennfjord MK, Hilde G, Ellström-Engh M, Bø K. Diastasis recti abdominis during pregnancy and 12 months after childbirth: prevalence, risk factors and report of lumbopelvic pain. Br J Sports Med. 2016;50:1092–1096. doi: 10.1136/bjsports-2016-096065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Spitznagle TM, Leong FC, Van Dillen LR. Prevalence of diastasis recti abdominis in a urogynecological patient population. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:321–328. doi: 10.1007/s00192-006-0143-5. [DOI] [PubMed] [Google Scholar]
- 31.Benjamin DR, Frawley HC, Shields N, van de Water ATM, Taylor NF. Relationship between diastasis of the rectus abdominis muscle (DRAM) and musculoskeletal dysfunctions, pain and quality of life: a systematic review. Physiotherapy. 2019;105:24–34. doi: 10.1016/j.physio.2018.07.002. [DOI] [PubMed] [Google Scholar]
- 32.Fuentes Aparicio L, Rejano-Campo M, Donnelly GM, Vicente-Campos V. Self-reported symptoms in women with diastasis rectus abdominis: a systematic review. J Gynecol Obstet Hum Reprod. 2021;50:101995. doi: 10.1016/j.jogoh.2020.101995. [DOI] [PubMed] [Google Scholar]
- 33.Keshwani N, Mathur S, McLean L. The impact of exercise therapy and abdominal binding in the management of diastasis recti abdominis in the early post-partum period: a pilot randomized controlled trial. Physiother Theory Pract. 2019;37:1018–1033. doi: 10.1080/09593985.2019.1675207. [DOI] [PubMed] [Google Scholar]
- 34.Lee D, Hodges PW. Behavior of the linea alba during a curl-up task in diastasis rectus abdominis: an observational study. J Orthop Sports Phys Ther. 2016;46:580–589. doi: 10.2519/jospt.2016.6536. [DOI] [PubMed] [Google Scholar]
- 35.Mota P, Pascoal AG, Carita AI, Bø K. The immediate effects on inter-rectus distance of abdominal crunch and drawing-in exercises during pregnancy and the postpartum period. J Orthop Sports Phys Ther. 2015;45:781–788. doi: 10.2519/jospt.2015.5459. [DOI] [PubMed] [Google Scholar]
- 36.Pascoal AG, Dionisio S, Cordeiro F, Mota P. Inter-rectus distance in postpartum women can be reduced by isometric contraction of the abdominal muscles: a preliminary case-control study. Physiotherapy. 2014;100:344–348. doi: 10.1016/j.physio.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 37.Theodorsen NM, Strand LI, Bø K. Effect of pelvic floor and transversus abdominis muscle contraction on inter-rectus distance in postpartum women: a cross-sectional experimental study. Physiotherapy. 2019;105:315–320. doi: 10.1016/j.physio.2018.08.009. [DOI] [PubMed] [Google Scholar]
- 38.Benjamin DR, van Water ATM, Peiris CL. Effects of exercise on diastasis of the rectus abdominis muscle in the antenatal and postnatal periods: a systematic review. Physiotherapy. 2014;100:1–8. doi: 10.1016/j.physio.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 39.Dufour S, Bernard S, Murray-Davis B, Graham N. Establishing expert-based recommendations for the conservative management of pregnancy-related diastasis rectus abdominis: a Delphi consensus study. J Women Health Phys Ther. 2019;43:73–81. doi: 10.1097/JWH.0000000000000130. [DOI] [Google Scholar]
- 40.Werner LA, Dayan M. Diastasis recti abdominis - diagnosis, risk factors, effect on musculoskeletal function, framework for treatment and implications for the pelvic floor. Curr Womens Health Rev. 2019;15:86–101. doi: 10.2174/1573404814666180222152952. [DOI] [Google Scholar]
- 41.Gluppe S, Engh ME, Bø K. What is the evidence for abdominal and pelvic floor muscle training to treat diastasis recti abdominis postpartum? A systematic review with meta-analysis. Braz J Phys Ther. 2021;25:664–675. doi: 10.1016/j.bjpt.2021.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Abuín-Porras V, de la Cueva-Reguera M, Benavides-Morales P, Ávila-Pérez R, Cruz-Torres B, Pareja-Galeano H, Blanco-Morales M, Romero-Morales C. Comparison of the abdominal wall muscle thickness in female rugby players versus non-athletic women: a cross-sectional study. Medicina (Kaunas) 2020;56:8. doi: 10.3390/medicina56010008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Morales CR, Polo JA, Sanz DR, López DL, González SV, Buría JLA. Lobo CC (2018a) Ultrasonography features of abdominal perimuscular connective tissue in elite and amateur basketball players: an observational study. Rev Assoc Med Bras (1992) 1992;64:936–941. doi: 10.1590/1806-9282.64.10.936. [DOI] [PubMed] [Google Scholar]
- 44.Romero-Morales C, Martín-Llantino P, Calvo-Lobo C, San-Antolín M, López-López D, Blanco-Morales M, Rodríguez-Sanz D. Ultrasound imaging of the abdominal wall and trunk muscles in patients with Achilles tendinopathy versus healthy participants. Diagnostics (Basel) 2019;10:17. doi: 10.3390/diagnostics10010017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Romero-Morales C, de la Cueva-Reguera M, Miñambres-Vallejo B, Ruiz-Ruiz B, Calvo-Lobo C, Casado-Hernández I, López-López D, Abuín-Porras V. Ultrasound assessment of the abdominal wall muscles in women with and without primary dysmenorrhea: a cross-sectional study. Diagnostics (Basel) 2020;10:166. doi: 10.3390/diagnostics10030166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Whittaker JL, Warner MB, Stokes M. Comparison of the sonographic features of the abdominal wall muscles and connective tissues in individuals with and without lumbopelvic pain. J Orthop Sports Phys Ther. 2013;43:11–19. doi: 10.2519/jospt.2013.4450. [DOI] [PubMed] [Google Scholar]
- 47.Iwan T, Garton B, Ellis R. The reliability of measuring the inter-recti distance using high-resolution and low-resolution ultrasound imaging comparing a novice to an experienced sonographer. NZ J Physiother. 2014;3:154–162. doi: 10.15619/NZJP/42.3.07. [DOI] [Google Scholar]
- 48.Keshwani N, McLean L. Ultrasound imaging in postpartum women with diastasis recti: intrarater between-session reliability. J Orthop Sports Phys Ther. 2015;45:713–718. doi: 10.2519/jospt.2015.5879. [DOI] [PubMed] [Google Scholar]
- 49.Mota P, Pascoal AG, Sancho F, Bø K. Test-retest and intrarater reliability of 2-dimensional ultrasound measurements of distance between rectus abdominis in women. J Orthop Sports Phys Ther. 2012;42:940–946. doi: 10.2519/jospt.2012.4115. [DOI] [PubMed] [Google Scholar]
- 50.Nanikawa W, Miyazaki J. Intra-rater reliability of measurement of abdominal perimuscular connective tissue thickness on ultrasound images. J Phys Ther Sci. 2021;33:32–36. doi: 10.1589/jpts.33.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, McInerney P, Godfrey CM, Khalil H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. 2020;18:2119–2126. doi: 10.11124/JBIES-20-00167. [DOI] [PubMed] [Google Scholar]
- 52.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 53.Hills NF, Keshwani N, McLean L. Influence of ultrasound transducer tilt in the cranial and caudal directions on measurements of inter-rectus distance in parous women. Physiother Can. 2018;70:6–10. doi: 10.3138/ptc.2016-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Keshwani N, Mathur S, McLean L. Validity of inter-rectus distance measurement in postpartum women using extended field-of-view ultrasound imaging techniques. J Orthop Sports Phys Ther. 2015;45:808–813. doi: 10.2519/jospt.2015.6143. [DOI] [PubMed] [Google Scholar]
- 55.Keshwani N, Hills N, McLean L. Inter-rectus distance measurement using ultrasound imaging: does the rater matter? Physiother Can. 2016;68:223–229. doi: 10.3138/ptc.2015-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Balasch-Bernat M, Pérez-Alenda S, Carrasco JJ, Valls-Donderis B, Dueñas L, Fuentes-Aparicio L. Differences in inter-rectus distance and abdominopelvic function between nulliparous primiparous and multiparous women. Int J Environ Res Public Health. 2021 doi: 10.3390/ijerph182312396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Castellanos-López E, Castillo-Merino C, Abuín-Porras V, López-López D, Romero-Morales C. Ultrasonography comparison of pelvic floor and abdominal wall muscles in women with and without dyspareunia: a cross-sectional study. Diagnostics (Basel) 2022;12(8):1827. doi: 10.3390/diagnostics12081827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Morales CR, Sanz DR, Reguera MC, Martínez SF, González PT, Pascual BM. Proprioceptive Stabilizer™ training of the abdominal wall muscles in healthy subjects: a quasi-experimental study. Rev Assoc Med Bras (1992) 1992;64:1134–1138. doi: 10.1590/1806-9282.64.12.1134. [DOI] [PubMed] [Google Scholar]
- 59.Romero-Morales C, Martín-Llantino PJ, Calvo-Lobo C, Beltran-Alacreu H, López-López D, Sánchez-Gómez R, Rodríguez-Sanz D. Effectiveness of eccentric exercise and a vibration or cryotherapy program in enhancing rectus abdominis muscle thickness and inter-rectus distance in patients with chronic mid-portion achilles tendinopathy: a randomized clinical trial. Int J Med Sci. 2018;15:1764–1770. doi: 10.7150/ijms.28656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Barbosa S, de Sá RA, Coca Velarde LG. Diastasis of rectus abdominis in the immediate puerperium: correlation between imaging diagnosis and clinical examination. Arch Gynecol Obstet. 2013;288:299–303. doi: 10.1007/s00404-013-2725-z. [DOI] [PubMed] [Google Scholar]
- 61.Belo M, Melo A, Delgado A, Costa A, Anísio V, Lemos A. The digital caliper's interrater reliability in measuring the interrecti distance and its accuracy in diagnosing the diastasis of rectus abdominis muscle in the third trimester of pregnancy. J Chiropr Med. 2020;19:136–144. doi: 10.1016/j.jcm.2020.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chiarello CM, McAuley JA. Concurrent validity of calipers and ultrasound imaging to measure interrecti distance. J Orthop Sports Phys Ther. 2013;3:495–503. doi: 10.2519/jospt.2013.4449. [DOI] [PubMed] [Google Scholar]
- 63.Gillard S, Ryan CG, Stokes M, Warner M, Dixon J. Effects of posture and anatomical location on inter-recti distance measured using ultrasound imaging in parous women. Musculoskelet Sci Pract. 2018;34:1–7. doi: 10.1016/j.msksp.2017.11.010. [DOI] [PubMed] [Google Scholar]
- 64.Depledge J, McNair P, Ellis R (2021) Exercises, Tubigrip and taping: can they reduce rectus abdominis diastasis measured three weeks post-partum? Musculoskelet Sci Pract 53:102381. doi: 10.1016/j.msksp.2021.102381. [DOI] [PubMed]
- 65.He K, Zhou X, Zhu Y, Wang B, Fu X, Yao Q, Chen H, Wang X. Muscle elasticity is different in individuals with diastasis recti abdominis than healthy volunteers. Insights Imaging. 2021;12(1):87. doi: 10.1186/s13244-021-01021-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Li Q, Lei S, Liu Y, Liu Q, Chen Y, Lin X, Zhang X. Effectiveness of yoga on the interrectus distance in early postpartum women: a high-frequency ultrasound study. Biomed Res Int. 2022;2022:8908095. doi: 10.1155/2022/8908095. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 67.Benjamin DR, Frawley HC, Shields N, Georgiou C, Taylor NF. Establishing measurement properties in the assessment of inter-recti distance of the abdominal muscles in a postnatal women. Musculoskelet Sci Pract. 2020;49:102202. doi: 10.1016/j.msksp.2020.102202. [DOI] [PubMed] [Google Scholar]
- 68.Crommert ME, Flink I, Gustavsson C. Predictors of disability attributed to symptoms of increased interrecti distance in women after childbirth: an observational study. Phys Ther. 2021;101:1–6. doi: 10.1093/ptj/pzab064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kim S, Yi D, Yim J. The effect of core exercise using online videoconferencing platform and offline-based intervention in postpartum woman with diastasis recti abdominis. Int J Environ Res Public Health. 2022;19(12):7031. doi: 10.3390/ijerph19127031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Starzec-Proserpio M, Lipa D, Szymański J, Szymańska A, Kajdy A, Baranowska B. Association among pelvic girdle pain, diastasis recti abdominis, pubic symphysis width, and pain catastrophizing: a matched case-control study. Phys Ther. 2022;102(4):pza311. doi: 10.1093/ptj/pzab311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mota P, Pascoal AG, Sancho F, Carita AI, Bø K. Reliability of the inter-rectus distance measured by palpation. Comparison of palpation and ultrasound measurements. Man Ther. 2013;18:294–298. doi: 10.1016/j.math.2012.10.013. [DOI] [PubMed] [Google Scholar]
- 72.Mota P, Pascoal AG, Carita AI, Bø K. Normal width of the inter-recti distance in pregnant and postpartum primiparous women. Musculoskelet Sci Pract. 2018;35:34–37. doi: 10.1016/j.msksp.2018.02.004. [DOI] [PubMed] [Google Scholar]
- 73.Sancho MF, Pascoal AG, Mota P, Bø K. Abdominal exercises affect inter-rectus.distance in postpartum women: a two-dimensional ultrasound study. Physiotherapy. 2015;101:286–291. doi: 10.1016/j.physio.2015.04.004. [DOI] [PubMed] [Google Scholar]
- 74.Arranz-Martín B, Navarro-Brazález B, Sánchez-Sánchez B, McLean L, Carazo-Díaz C, Torres-Lacomba M. The impact of hypopressive abdominal exercise on linea alba morphology in women who are postpartum: a short-term cross-sectional study. Phys Ther. 2022;102(8):pzac086. doi: 10.1093/ptj/pzac086. [DOI] [PubMed] [Google Scholar]
- 75.Theodorsen NM, Fersum KV, Moe-Nilssen R, Bo K, Haukenes I. Effect of a specific exercise programme during pregnancy on diastasis recti abdominis: study protocol for a randomised controlled trial. BMJ Open. 2022;12(2):e056558. doi: 10.1136/bmjopen-2021-056558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Beer GM, Schuster A, Seifert B, Manestar M, Mihic-Probst D, Weber SA. The normal width of the linea alba in nulliparous women. Clin Anat. 2009;22:706–711. doi: 10.1002/ca.20836. [DOI] [PubMed] [Google Scholar]
- 77.Huge B, Kisner C. Women's health: obstetrics and pelvic floor. In: Kisner C, Colby L, Borstad J, editors. Therapeutic exercise: foundations and techniques, 7e. New York: McGraw Hill; 2018. [Google Scholar]
- 78.Noble E. The abdominal muscles. In: Noble E, editor. Essential exercises for the childbearing year. A guide to health and comfort before and after your baby is born 4e. Union City: New Life Images; 2003. [Google Scholar]
- 79.Candido G, Lo T, Janssen PA. Risk factors for diastasis of the recti abdominis. J Assoc Chart Physiother Women's Health. 2005;97:49–54. [Google Scholar]
- 80.Brauman D. Diastasis recti: clinical anatomy. Plast Reconstr Surg. 2008;122:1564–1569. doi: 10.1097/PRS.0b013e3181882493. [DOI] [PubMed] [Google Scholar]
- 81.Bohannon RW, Bass A. Research describing pelvifemoral rhythm: a systematic review. J Phys Ther Sci. 2017;29:2039–2043. doi: 10.1589/jpts.29.2039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Abe T, Kusuhara N, Yoshimura N, Tomita T, Easton PA. Differential respiratory activity of four abdominal muscles in humans. J Appl Physiol (1985) 1996;80:1379–1389. doi: 10.1152/jappl.1996.80.4.1379. [DOI] [PubMed] [Google Scholar]
- 83.Ainscough-Potts AM, Morrissey MC, Critchley D. The response of the transverse abdominis and internal oblique muscles to different postures. Man Ther. 2006;11:54–60. doi: 10.1016/j.math.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 84.Hodges PW, Pengel LH, Herbert RD, Gandevia SC. Measurement of muscle contraction with ultrasound imaging. Muscle Nerve. 2003;27:682–692. doi: 10.1002/mus.10375. [DOI] [PubMed] [Google Scholar]
- 85.Teyhen DS, Gill NW, Whittaker JL, Henry SM, Hides JA, Hodges P. Rehabilitative ultrasound imaging of the abdominal muscles. J Orthop Sports Phys Ther. 2007;37:450–466. doi: 10.2519/jospt.2007.2558. [DOI] [PubMed] [Google Scholar]
- 86.Hernández-Belmonte A, Martínez-Cava A, Pallarés JG. Panoramic ultrasound requires a trained operator and specific evaluation sites to maximize its sensitivity: a comprehensive analysis of the measurement errors. Physiol Behav. 2022;248:113737. doi: 10.1016/j.physbeh.2022.113737. [DOI] [PubMed] [Google Scholar]
- 87.Kaufmann RL, Reiner CS, Dietz UA, Clavien PA, Vonlanthen R, Käser SA. Normal width of the linea alba, prevalence, and risk factors for diastasis recti abdominis in adults, a cross-sectional study. Hernia. 2021;26:609–618. doi: 10.1007/s10029-021-02493-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Qu E, Wu J, Zhang M, Wu L, Zhang T, Xu J, Zhang X. The ultrasound diagnostic criteria for diastasis recti and its correlation with pelvic floor dysfunction in early postpartum women. Quant Imaging Med Surg. 2021;11:706–713. doi: 10.21037/qims-20-596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Mendes DA, Nahas FX, Veiga DF, Mendes FV, Figueiras RG, Gomes HC, Ely PB, Novo NF, Ferreira LM. Ultrasonography for measuring rectus abdominis muscles diastasis. Acta Cir Bras. 2007;22:182–186. doi: 10.1590/s0102-86502007000300005. [DOI] [PubMed] [Google Scholar]
- 90.Koppenhaver SL, Parent EC, Teyhen DS, Hebert JJ, Fritz JM. The effect of averaging multiple trials on measurement error during ultrasound imaging of transversus abdominis and lumbar multifidus muscles in individuals with low back pain. J Orthop Sports Phys Ther. 2009;39:604–611. doi: 10.2519/jospt.2009.3088. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Supplementary documents: PRISMA-ScR Checklist, Publication Relevance Screening Form I, Publication Relevance Screening Form II, Explanation and Elaboration Document, Data Charting Form, and Objectives of the Studies.
Data Availability Statement
The data sets supporting the conclusions of this article are included within the article (Fig. 1, Tables 2 and 3).