Abstract
Objective
To investigate subgroups of health-related quality of life (HRQoL) in the Chinese medical staff and identify the demographic factors associated with these profiles.
Methods
574 Chinese medical staff were surveyed online. HRQoL was measured by using the 36-Item Short Form Health Survey, Version 2. Latent profile analysis (LPA) was used to identify the profiles of HRQoL. The associations between HRQoL profiles and covariates were assessed using multinomial logistic regression.
Results
Three HRQoL profiles were developed: low HRQoL at 15.6%, moderate HRQoL at 46.9%, and high HRQoL at 37.6%. Multinomial logistic regression showed night shift times, aerobic exercise conditioning, and personality type significantly predicted the profile membership.
Conclusion
Our findings develop earlier approaches that only used total scores to evaluate this group’s HRQoL and help them with tailored interventions to promote better HRQoL.
Keywords: health-related quality of life, China, medical staff, latent profile analysis, COVID-19
1. Introduction
As defined by the World Health Organization (WHO), the quality of life (QoL) concerns an individual’s current situation and their morals, expectations, beliefs, and concerns—all of which are influenced by the complex relationship between an individual’s physical health, mental health, social relationships, and environmental change (1–3). Health-related quality of life (HRQoL) mainly covers the health-related parts of QoL. In health economics, HRQoL is usually measured using a scale and serves as a barometer of personal, community, and socioeconomic development (4). The interest in HRQoL of medical staff has shown an increasing trend in recent years, along with the recognition of its impact on public health and medical development. The higher scores of HRQoL, the better general health and the fewer disorders or disabilities (5).
The nature of the work of healthcare professionals is both stressful and challenging, which can pose a threat to them and may impact their HRQoL (6, 7). In addition, the specific working environment and interpersonal relationships can impact the HRQoL of medical personnel (8). Studies have proved that medical staff was more likely to be stressed (6, 9), anxious, and depressed (10–12), especially since the outbreak of COVID-19. A meta-analysis also discovered consistent evidence for the widespread and profound impact of large outbreaks on the mental health of frontline medical staff (13). Furthermore, medical staff is more likely to suffer from job burnout due to the enormous workload they experience in the workplace (14–16).
Further research supports the idea that the HRQoL of medical staff maintains and promotes their compassion and empathy for patients and is closely related to the quality of care they provide (17, 18). Consequently, understanding and measuring HRQoL among medical staff has recently emerged as a priority. Prevention of negative emotional and physical problems in health care workers and promotion of overall health is one of the priorities advocated by the state and public health authorities (19). Positive psychology holds that emphasizing a person’s vitality and virtues is crucial. It promotes personal and social development by leveraging inner and constructive strengths. The ultimate goal of positive psychology is to pursue human happiness (20). However, most current studies on this particular group have focused on describing negative emotions such as anxiety, depression, and job burnout rather than overall HRQoL.
Currently, a variety of scales were used to measure human beings’ HRQoL. The appropriate HRQoL measurement metrics, however, lack a standardized definition. The 36-Item Short Form Health Survey, Version 2 (SF-36 v2) has been used to measure this outcome (both mental health and physical health) and has its advantages (21, 22). It has been considered an appropriate tool for measuring HRQoL in different populations and is favored in terms of its psychometric properties and convenience for monitoring HRQoL (23, 24). Moreover, it also helps monitor HRQoL in the healthy population (25). Furthermore, most of the previous literature used composite scores on scales to assess the level of HRQoL of the medical staff, few studies used the SF-36v2 scale to measure (26, 27). Additionally, this approach does not allow for further population classification; it only offers a comprehensive assessment of the population’s HRQoL. In addition, quantitative research on different HRQoL profiles in medical staff has received scant attention in the literature.
A method focused on the individual called latent profile analysis (LPA) uses continuous variables to divide samples into more meaningful subgroups based on similar characteristics (28). LPA is also a statistical method for determining whether heterogeneous subgroups exist within a population of interest. It can determine the underlying characteristics of individuals based on their response patterns to explicit topics to understand the characteristics of people with different profiles (29, 30). It is helpful to learn more about the population characteristics of different potential profiles by using LPA to explore HRQoL in medical staff and identify the sociodemographic correlates to the profiles of QoL. At present, there are few potential profile models of the HRQoL of medical staff. In conclusion, more LAP-based research needs to be investigated.
Therefore, the main goal of this study was to find the distinct profiles of HRQoL in Chinese medical staff using an LPA approach. Then, we studied the sociodemographics associated with profile membership. This study will provide fundamental evidence for public health to create targeted intervention strategies to improve HRQoL in medical staff.
2. Method
2.1. Study design
A multi-center cross-sectional study was carried out. And the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines were followed in this study.
2.2. Participants
An online survey was conducted by enrolling a convenience sample of medical staff mainly from six hospitals (the 1st Affiliated Hospital of Wenzhou Medical University, the 2nd Affiliated Hospital of Wenzhou Medical University, the 2nd Hospital of Dalian Medical University, the 2nd Affiliated Hospital of Zhongguo Medical University, Lishui People’s Hospital, and Chenzhou 3rd People’s Hospital) in China. Medical staff was eligible if they had legal rights and obligations to the hospital. Medical staff was excluded if they were unwilling to participate in the study or had severe mental health problems. Two were disqualified from the total 574 eligible participants who agreed to take part because their responses were not complete—resulting in a 572 (99.7%) valid sample size.
2.3. Data collection
Between May and July 2020, online questionnaires were collected anonymously from medical staff who met the criteria. Every Internet Protocol (IP) address was only permitted to access the survey once in order to avoid double enrollment. Each questionnaire took about 15–20 min to complete. The system would exclude questionnaires that took less than 10 min to complete.
2.4. Measures
2.4.1. Sociodemographic characteristics
The characteristics of medical staff included gender, age, marital status, education level, professional title, department, position, employment status, work time per day, night shift times per week, individual income monthly, exercise condition and self-reported personality.
2.4.2. Health-related quality of life
The SF-36v2 was used to assess self-perceived HRQoL. The eight dimensions of physical functions (PF), role-physical (RP), physical pain (PP), health in general (HG), vitality (VT), social functions (SF), role-emotional (RE), and mental health (MH) accounted for 10 items, 4 items, 2 items, 5 items, 4 items, 2 items, 3 items, and 5 items, respectively, for a total of 36 items. The physical component summary (PCS) and the mental component summary (MCS) are the two subscales among the eight dimensions. The present study showed satisfactory reliability (Cronbach’s α = 0.861).
2.5. Ethical consideration
The study followed the ethical principles of the Helsinki declaration (31). The institution the corresponding author was associated with approved our study through its institutional review board (LCKY2019-288). Before formally starting to fill out the questionnaire, participants will be shown a statement about informed consent, the purpose of the study, and the content of the study. Participants have the right to decide whether or not to continue filling out the questionnaire. All patients gave informed consent.
2.6. Statistical analysis
The following versions of softwares were used to analyze the data: Mplus version 8.3 (Muthen & Muthen, Los Angeles, CA, Unites States), SPSS version 25.0 (IBM, Armonk, NY, Unites States), and Stata version 14.1 (StataCorp LP, 1985–2015). All variables were first subjected to descriptive statistics. Second, different LPA models were developed to explore the profiles of HRQoL among 572 medical staff. The Akaike information criterion (AIC), Bayesian information criterion (BIC), adjusted Bayesian information criterion (aBIC), and the Lo–Mendell–Rubin adjusted likelihood ratio test (LMRT) were used to determine the ideal number of profiles (32). Lower values for the AIC, BIC, and aBIC signify a better-fitting model. Models with different numbers of latent profiles were compared using LMRT. When a k-class model showed a non-significant value, a k-1 class model should be accepted. Entropy was used to evaluate the classification precision of the model, varying between 0 and 1, with larger values being better. When the number exceeds 0.80, the classification accuracy has been determined to be adequate. Item means were examined using Analysis of Variance (ANOVA) to determine if profiles derived from LPA differed significantly. Third, when the best profile model was determined, each profile was named according to its distributions. The Chi-squared test was used to determine how the various profiles differed in terms of sociodemographic traits, and Bonferroni method for multiple comparisons. Multinomial logistic regression was used to adjust confounding factors. All variables with univariate p values <0.05 were chosen as independent variables for the multinomial regression models.
3. Results
3.1. Descriptive statistics
There were 521 female participants (91.1%) and 51 male participants (8.9%). Nurses and doctors accounted for 474 (82.9%) and 59 (10.3%), respectively. The mean age of the medical staff was 34.18 ± 6.36 (range 21–55). The majority of participants said they had a college degree (73.8%, n = 422) or higher in education (11.2%, n = 64), were married (81.8%, n = 464), with primary (44.2%, n = 253) or medium (46.0%, n = 263) professional title, and were officially employed by the hospital (68.2%, n = 390). More than half participants reported working more than 8 h a day (65.2%, n = 373) and one night shift per week (50.0%, n = 286). Individual participants’ monthly incomes were as follows: 237 (41.4%) reported having an income of 6,000 RMB or less, 143 (25.0%) reported having an income between 6,000 RMB and 8,000 RMB, and 192 (33.6%) reported having an income of >8,000 RMB. Most participants never exercised (43.2%, n = 247) or exercised 1–2 h per day (41.8%, n = 239). As for personality, approximately 24.1% (n = 138) participants considered themselves extroverted, 22.9% (n = 131) considered themselves introverted, and 54.5% (n = 303) considered themselves intermediate. Table 1 displayed all of the remaining general data.
Table 1.
Comparison of socio-demographic characteristics among different health-related quality of life (HRQoL) profiles (n = 572).
| Variables | Total sample | Low HRQoL | Moderate HRQoL | High HRQoL | χ 2 | p | |
|---|---|---|---|---|---|---|---|
| Gender | 4.255 | 0.119 | |||||
| Male | 51(8.9) | 4(4.5) | 22(8.2) | 25(11.6) | |||
| Female | 521(91.1) | 85(95.5) | 246(91.8) | 190(88.4) | |||
| Age | 3.486 | 0.480 | |||||
| 20–29 | 142(24.8) | 22(24.7) | 67(25.0) | 53(24.7) | |||
| 30–39 | 324(56.6) | 55(61.8) | 154(57.5) | 115(53.5) | |||
| ≥40 | 106(18.5) | 12(13.5) | 47(17.5) | 47(21.9) | |||
| Marital status | 1.603 | 0.822 | |||||
| Single | 99(17.3) | 19(21.3) | 46(17.2) | 34(15.8) | |||
| Married | 464(81.8) | 69(77.5) | 218(81.3) | 177(82.3) | |||
| Divorce | 9(1.6) | 1(1.1) | 4(1.5) | 4(1.9) | |||
| Education | 2.138 | 0.710 | |||||
| Below college | 86(15.0) | 12(13.5) | 39(14.6) | 35(16.3) | |||
| College degree | 422(73.8) | 70(78.8) | 199(74.3) | 153(71.2) | |||
| Above college | 64(11.2) | 7(7.9) | 30(11.2) | 27(12.6) | |||
| Professional title | 3.304 | 0.508 | |||||
| Primary | 253 (44.2) | 44(49.4) | 120(44.8) | 89(41.4) | |||
| Medium | 263(46.0) | 40(44.9) | 119(44.4) | 104(48.4) | |||
| High | 56(9.8) | 5(5.6) | 29(10.8) | 22(10.2) | |||
| Department | 16.990 | 0.386 | |||||
| Medical | 89(15.6) | 22(24.7) | 41(15.3) | 26(12.1) | |||
| Surgical | 61(10.7) | 7(7.9) | 33(12.3) | 21(9.8) | |||
| Pediatric | 30(5.2) | 4(4.5) | 14(5.2) | 12(5.6) | |||
| Obstetrics and Gynecology | 41(7.2) | 6(6.7) | 15(5.6) | 20(9.3) | |||
| Emergency room | 111(19.4) | 14(15.7) | 47(17.5) | 50(23.3) | |||
| Operating room | 18(3.1) | 2(2.2) | 10(3.7) | 6(2.8) | |||
| ICU | 26(4.5) | 2(2.2) | 16(6.0) | 8 (3.7) | |||
| NICU | 14(2.4) | 3(3.4) | 7(2.6) | 4(1.9) | |||
| Others | 182(31.8) | 29(32.6) | 85(31.7) | 68(31.6) | |||
| Position | 4.063 | 0.397 | |||||
| Doctor | 59(10.3) | 7(7.9) | 29(10.8) | 23(10.7) | |||
| Nurse | 474(82.9) | 79(88.8) | 222(82.8) | 173(80.5) | |||
| Others | 39(6.8) | 3(3.4) | 17(6.3) | 19(8.8) | |||
| Employment status | 0.890 | 0.641 | |||||
| Official | 390(68.2) | 57(64.0) | 186(69.4) | 147(68.4) | |||
| Contract/temporary | 182(31.8) | 32(36.0) | 82(30.6) | 68(31.6) | |||
| Work time per day | 7.012 | 0.030 | |||||
| <8 | 199(34.8) | 25(28.1) | 85(31.7) | 89(41.4) | |||
| ≥8 | 373(65.2) | 64(71.9) | 183(68.3) | 126(58.6) | |||
| Night shift times per week | 11.238 | 0.024 | |||||
| 0 | 147(25.7) | 16(18.0) | 60(22.4) | 71(33.0) | |||
| 1 | 286(50.0) | 46(51.7) | 143(53.4) | 97(45.1) | |||
| ≥2 | 139(24.3) | 27(30.3) | 65(24.3) | 47(21.9) | |||
| Income per month | 7.518 | 0.111 | |||||
| <6,000 | 237(41.4) | 45(50.6) | 113(42.2) | 79(36.7) | |||
| 6,000–8,000 | 143(25.0) | 18(20.2) | 73(27.2) | 52(24.2) | |||
| >8,000 | 192(33.6) | 26(29.2) | 82(30.6) | 84(39.1) | |||
| Exercise | 17.023 | 0.002 | |||||
| Never | 247(43.2) | 49(55.1) | 121(45.1) | 77(35.8) | |||
| 1-2 h/week | 239(41.8) | 34(38.2) | 113(42.2) | 92(42.8) | |||
| ≥3 h/week | 86(15.0) | 6(6.7) | 34(12.7) | 46(21.4) | |||
| Personality | 12.060 | 0.017 | |||||
| Extroverted | 138(24.1) | 18(20.2) | 57(21.3) | 63(29.3) | |||
| Introverted | 131(22.9) | 30(33.7) | 63(23.5) | 38(17.7) | |||
| Intermediate | 303(54.5) | 41(46.1) | 148(55.2) | 114(53.0) | |||
Data presented as frequency (percentage).
Table 2 displayed the descriptive statistics and correlations of the grouping variables used. The highest mean was for BP, and the lowest mean was for VT, with little difference between the means of the eight subgroup variables. High positive correlations between RP and RE, GH and VT, GH and MH, VT and MH, SF and RE, and SF and RH were found in the results of the correlation analysis.
Table 2.
Descriptive statistics and correlations.
| Variables | M | SD | PF | RP | BP | GH | VT | SF | RE |
|---|---|---|---|---|---|---|---|---|---|
| PF | 47.60 | 9.38 | 1 | ||||||
| RP | 47.04 | 10.78 | 0.414*** | 1 | |||||
| BP | 47.79 | 9.25 | 0.372*** | 0.353*** | 1 | ||||
| GH | 44.51 | 9.28 | 0.356*** | 0.269*** | 0.441*** | 1 | |||
| VT | 40.35 | 10.94 | 0.357*** | 0.276*** | 0.418*** | 0.628*** | 1 | ||
| SF | 44.62 | 11.04 | 0.362*** | 0.461*** | 0.482*** | 0.434*** | 0.493*** | 1 | |
| RE | 44.83 | 12.85 | 0.376*** | 0.667*** | 0.332*** | 0.321*** | 0.417*** | 0.544*** | 1 |
| MH | 40.43 | 10.97 | 0.319*** | 0.290*** | 0.422*** | 0.581*** | 0.777*** | 0.589*** | 0.487*** |
M, mean; SD, standard deviation; PF, physical functioning; RP, role-physical; BP, bodily pain; GH, general health; VT, vitality; SF, social functioning; RE, role-emotional; MH, mental health.
P<0.001.
3.2. Latent profile analysis
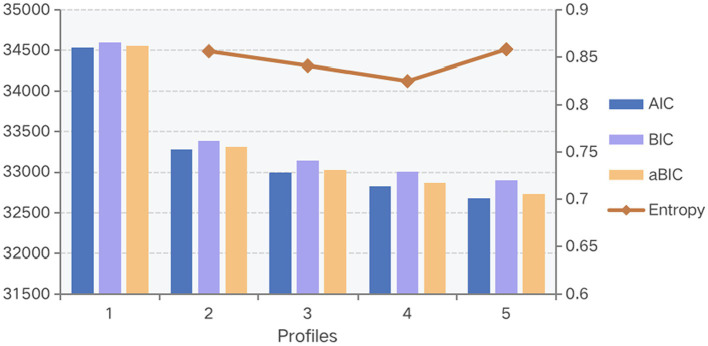
A one-to-five classification was present, according to information-based fit indices (Table 3). Figure 1 showed that AIC, BIC, and aBIC gradually improved (number decreased) as the number of profiles increased, and it displayed the trend of entropy. Considering both LMRT and BLRT showed significance in profiles 2 and 3. Based on the analysis of the available data, the three-profile model was selected for this study (33). It had a suitable entropy value of 0.841, indicating a distinct classification. The mean posterior probabilities that participants pertained to the latent profile where they were assigned were 91.6–95.0%, indicating that the three-profile models were credible (Table 4).
Table 3.
Fit statistics for the latent class model with 1–5 classes.
| AIC | BIC | aBIC | Entropy | LMRT | BLRT | Latent class probability | |
|---|---|---|---|---|---|---|---|
| p value | p value | ||||||
| 1 class | 34530.769 | 34600.355 | 34549.562 | ||||
| 2 class | 33281.312 | 33390.040 | 33310.676 | 0.856 | <0.001 | <0.001 | 0.46329/0.53671 |
| 3 class | 32991.884 | 33139.755 | 33031.820 | 0.841 | 0.0213 | <0.001 | 0.15559/0.46853/0.37587 |
| 4 class | 32821.123 | 33008.136 | 32871.630 | 0.825 | 0.0452 | <0.001 | 0.13811/0.25000/0.24825/0.36364 |
| 5 class | 32673.388 | 32899.543 | 32734.466 | 0.858 | 0.0972 | <0.001 | 0.25175/0.01923/0.26573/0.11014/0.35315 |
AIC, Akaike information criteria; BIC, Bayesian information criteria; aBIC, adjusted Bayesian information criterion.
LMRT, Lo–Mendell–Rubin likelihood ratio test; BLRT, Bootstrapped likelihood ratio test.
Figure 1.
Comparison of the information criteria.
Table 4.
Average latent class probabilities for most likely latent class membership (Row) by latent class (Column).
| C1 | C2 | C3 | |
|---|---|---|---|
| C1 | 0.924 | 0.076 | 0.000 |
| C2 | 0.041 | 0.916 | 0.043 |
| C3 | 0.000 | 0.050 | 0.950 |
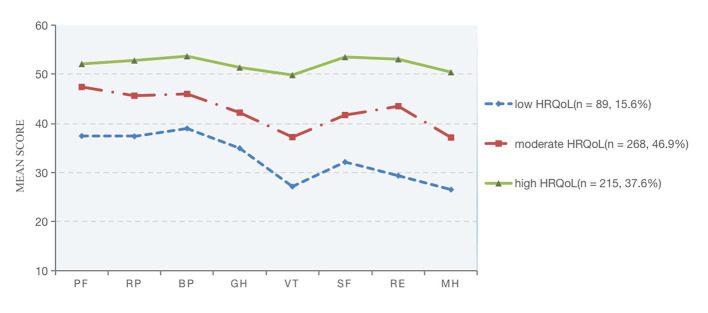
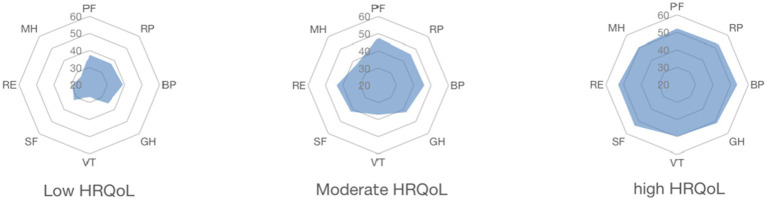
Following that, the names of the three profiles were determined by their characterized patterns of HRQoL. And named C1–C3 as “Low HRQoL,” “Moderate HRQoL,” and “High HRQoL” individually, as seen in Figure 2 and Table 5. Significant mean differences between the manifest indicators for each profile were revealed by the three-profile solution (Table 5). The high HRQoL profile made up the second most common proportion of participants (n = 215, 37.6%). The moderate HRQoL profile was the largest profile (n = 268, 46.9%). The low HRQoL profile was the third most prevalent profile (n = 89, 15.6%). The tendencies of the three HRQoL profiles were illustrated in Figure 3.
Figure 2.
Item means for the three-profile mode of HRQoL. PF, physical functioning; RP, role-physical; BP, bodily pain; GH, general health; VT, vitality; SF, social functioning; RE, role-emotional; MH, mental health.
Table 5.
Descriptive statistics for health-related quality of life (HRQoL) disaggregated by latent profile class.
| Variable | Class 1 Low HRQoL n = 89, 15.6% |
Class 2 Moderate HRQoL n = 268, 46.9% |
Class 3 High HRQoL n = 215, 37.6% |
F | |||
|---|---|---|---|---|---|---|---|
| M | SE | M | SE | M | SE | ||
| PF | 37.483 | 1.802 | 47.506 | 0.818 | 52.095 | 0.387 | 63.608*** |
| RP | 37.404 | 1.627 | 45.717 | 1.146 | 52.806 | 0.649 | 87.574*** |
| BP | 39.015 | 0.990 | 46.083 | 0.921 | 53.672 | 0.507 | 58.409*** |
| GH | 34.973 | 1.601 | 42.255 | 0.582 | 51.374 | 0.657 | 51.051*** |
| VT | 27.146 | 2.592 | 37.251 | 0.621 | 49.827 | 0.712 | 52.697*** |
| SF | 32.162 | 1.243 | 41.763 | 1.049 | 53.502 | 0.604 | 62.869*** |
| RE | 29.354 | 1.671 | 43.566 | 1.466 | 53.059 | 0.633 | 99.544*** |
| MH | 26.517 | 1.936 | 37.170 | 0.793 | 50.409 | 0.626 | 46.226*** |
p < 0.001. PF, physical functioning; RP, role-physical; BP, bodily pain; GH, general health; VT, vitality; SF, social functioning; RE, role-emotional; MH, mental health.
Figure 3.
The tendencies of three distinctive HRQoL. PF, physical functioning; RP, role-physical; BP, bodily pain; GH, general health; VT, vitality; SF, social functioning; RE, role-emotional; MH, mental health.
3.3. Predictor of latent profile membership
The Chi-squared test results revealed significant differences in work time per day (χ2 = 7.012, p = 0.030), night shift times per week (χ2 = 11.238, p = 0.024), exercise (χ2 = 17.023, p = 0.002), and personality (χ2 = 12.060, p < 0.017) between the three profiles (Table 1).
With the low HRQoL group as the reference group, multinomial logistic regression was further used to investigate the sociodemographic predictors of profile membership, and significant influencing factors in the Chi-square test were included (Table 6). In comparison to the low HRQoL group, medical staff with introverted traits (OR: 0.495; CI: 0.268, 0.915) had lower odds of being in the high HRQoL group. Compared to those who exercise more than 3 h per week, medical staff who never exercise (OR: 0.250; CI: 0.098, 0.638) had lower odds of being in the high HRQoL group than the high HRQoL group. Moreover, medical staff with no night shift per week (OR: 2.299; CI: 1.089, 4.855) were more likely to fall into the high HRQoL group than the low HRQoL group.
Table 6.
Odds ratios for the covariates predicting latent profile membership.
| Covariate | Moderate HRQoL vs. Low HRQoL | High HRQoL vs. Low HRQoL | |||||
|---|---|---|---|---|---|---|---|
| OR | 95%CI | P | OR | 95%CI | P | ||
| Worktime | |||||||
| <8 | 0.940 | 0.544–1.625 | 0.824 | 0.651 | 0.371–1.143 | 0.135 | |
| ≥8 | Ref | Ref | Ref | Ref | Ref | Ref | |
| Night shift times per week | |||||||
| 0 | 1.568 | 0.757–3.247 | 0.226 | 2.299 | 1.089–4.855 | 0.029 | |
| 1 | 1.333 | 0.749–2.373 | 0.328 | 1.176 | 0.635–2.179 | 0.606 | |
| ≥2 | Ref | Ref | Ref | Ref | Ref | Ref | |
| Exercise | |||||||
| never | 0.469 | 0.183–1.197 | 0.113 | 0.250 | 0.098–0.638 | 0.004 | |
| 1-2 h/week | 0.610 | 0.235–1.582 | 0.309 | 0.400 | 0.155–1.032 | 0.058 | |
| ≥3 h/week | Ref | Ref | Ref | Ref | Ref | Ref | |
| Personality | |||||||
| Extroverted | 0.854 | 0.452–1.614 | 0.627 | 1.183 | 0.620–2.258 | 0.610 | |
| Introverted | 0.603 | 0.344–1.059 | 0.078 | 0.495 | 0.268–0.915 | 0.025 | |
| Intermediate | Ref | Ref | Ref | Ref | Ref | Ref | |
OR, odds ratio; CI, confidence interval. Low HRQoL as a refer.
4. Discussion
By using LPA analysis, three profiles representing the level of HRQoL of Chinese medical staff were created for the present study. They were low HRQoL, moderate HRQoL, and high HRQoL, which accounted for 15.6, 46.9, and 37.6%, respectively. According to our findings, the majority of participants were in the moderate HRQoL group and exhibited comparatively moderate levels of physical functions, role-physical, physical pain, general health, vitality, social functions, role-emotional, and mental health. Overall, it is important to value and improve the level of HRQoL among medical staff.
Medical staff in the low HRQoL profile represented the smallest percentage of the overall sample in the present study. Focusing on each dimension indicates that the average score for MH was only about 26 in the low HRQoL group, which is a large gap from the scores of the high HRQoL group (higher than 50), showing a bipartition trend. This suggests a potential need to tailor interventions to medical staff’s mental health condition. The study by Liu et al. (34) can support our view that of the 1,090 Chinese medical professionals, 13.3, 18.4, and 23.9% suffered from anxiety, depression, or both, respectively. Since the questionnaire was collected during the COVID-19 epidemic, those who were unprepared for a sudden outbreak are likely to experience mental health issues, especially the special population of medical staff, who dealt with greater challenges and stress (35). In conclusion, our study demonstrates the importance of mental health in improving the HRQoL of medical professionals. So among the various aspects of HRQoL, mental health needs the most attention in the present study.
It is worth noting that the third dimension-BP, had the highest mean score among all three profiles of HRQoL, followed by the second dimension-RP. This could be a result of the fact that, in comparison to other jobs, medical professionals will adopt more healthy behaviors, such as giving up smoking and drinking alcohol, putting more emphasis on eating well, and exercising more as they become more knowledgeable about diseases and health-related issues. Previous studies have also confirmed this view. A study by Liu et al. (36) revealed that healthcare workers are more concerned about food safety following a pandemic outbreak. A meta-analysis also suggested that interventions aimed at lifestyle change are more likely to improve nurses’ HRQoL (37). In other words, healthcare professionals who prioritize their own health will adopt healthier habits and lifestyles, enhancing their physical well-being, lessening physical discomfort, and ultimately enhancing their general HRQoL accordingly.
Multiple regression showed in the current research that factors influencing the HRQoL of medical staff included the work time per day and the nightshifts per week, respectively. The absence of nightshifts was a protective factor for the HRQoL of medical staff. In addition, we found that VT was the second lowest dimension in the three HRQoL profiles. The specific 4 items for this dimension are “Did you feel full of pep?” “Did you have a lot of energy?” “Did you feel worn out?” and “Did you feel tired?” The findings mentioned above imply that a lower VT score may be linked to long working hours, high intensity, stress brought on by frequently working nights, physical overdraft, and burnout. It’s consistent with the study by Silva et al. (38). Among medical staff, the dimensions with the lowest mean scores in the SF-36 were VT. A study from Italy also found that night nurses had lower HRQoL in all dimensions than the general population (39). As a result, by altering scheduling practices, better allocating human resources, and changing management paradigms, healthcare administrators can enhance the HRQoL for healthcare workers. It is important to note that a previous study (40) identified effort-reward imbalance as a significant factor contributing to work stress and fatigue in medical staff. Based on Siegrist’s effort-reward imbalance model (ERI) (41), the subsequent study can further explore the relevant factors influencing the psychological dimensions of this population. By the way, even though the univariate analysis demonstrated that work time per day was statistically significant, it was excluded from the logistic regression model. It probably due to the sample size is not large enough. Future studies could include a larger sample of medical staff for analysis.
This study also noted that the HRQoL of medical staff was related to exercise condition and personality type. As in previous studies (42, 43), medical personnel with exercise habits were more likely to maintain higher levels of mental well-being and physical health. Heidke et al. (44) found that physical inactivity was negatively related to HRQoL. These results support the statement in the present study that a higher frequency of weekly exercise is a protective factor for the HRQoL of medical personnel. Therefore, medical professionals can increase their HRQoL by increasing weekly exercise frequency. In addition, extroverts were more likely absent of depression and had high mental well-being (45). Consistent with previous research, individuals with introverted personalities were more likely to be in the low HRQoL group than those with intermediate personalities in the present study. Hence, introversion may be a risk factor for the HRQoL of medical staff. This suggests a potential need to tailor interventions according to personality differences.
A series of our findings can help provide medical staff with interventions for improving HRQoL. As HRQoL is sometimes used interchangeably with mental well-being. The majority of the interventions available today for healthcare professionals focus on psychological issues like anxiety and depression and how to control them. There are relatively few interventions that specifically address how to improve the quality of life of healthcare professionals. Consequently, it is imperative to develop interventions that take into consideration the relevant characteristics and cultural identity of Chinese medical personnel. Considering the findings of our study, future research might focus on enhancing the physical condition of medical personnel. Despite the fact that most medical professionals are knowledgeable about health issues, the intense work demands and lack of personal time present some challenges for this group in managing their own health. Psychological interventions can be used to alleviate symptoms like fatigue. For instance, mindfulness reduces the emotional burden on the nurse, which in turn reduces the level of burnout (46). And resilience training also showed a positive effect on medical staff’s anxiety and stress (47). However, psychological interventions typically need to be carried out over a longer period of time and by qualified psychologists. Our vision can be placed on the availability of direct and simple physical interventions to alleviate their fatigue and tiredness levels. This has immediate implications for medical professionals.
4.1. Strengths and limitations
Some contributions stem from the present study. The present findings reveal heterogeneity in the healthcare worker sample, implying the need for suitable quality of life improvement programs for various healthcare groups. As far as we are aware, there have not been any studies using LPA to investigate the variables affecting healthcare workers’ HRQoL. We can use the profile membership information provided by LPA to identify groups of healthcare professionals with various HRQoL traits. Integrating medical staff’s HRQoL traits with demographic characteristics in subsequent studies to find more targeted intervention plans. However, certain limitations should be taken into account. On the one hand, we cannot determine how profiles may change or stabilize over time or how profiles would predict the long-term HRQoL of medical staff due to the cross-sectional design of the current study. Further longitudinal studies can be performed to gather information on how medical staff’s HRQoL evolves over time. On the other hand, in the absence of objective assessment criteria, the level of HRQoL is self-reported results. Recall bias may affect study results. A multi-information strategy would be advantageous for upcoming research. What’s more, the extrapolation of the results may be somewhat constrained because the current study only focused on the population of Chinese healthcare workers. Nevertheless, convenience sampling can be unreliable and limit the generalization of research findings to other population groups; we consider to incorporate design-based principles such as randomization or systematic sampling into future survey designs.
5. Conclusion
The current study explored different profiles of HRQoL among Chinese medical staff to analyze the level of HRQoL of this population more specifically and we finally found three different levels of HRQoL traits among Chinese medical staff. The results of our study are important to the development of public health today.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Research Ethics Committee of the Second Affiliated Hospital of Wenzhou Medical University (LCKY2019-288). Informed consent was obtained from all subjects involved in the study.
Author contributions
JH and JZ wrote the main manuscript text. YR, HZ, and WG contributed to the data collection. JH contributed to the data analysis. AD contributed to the study design and had full access to all the data in the study, taking responsibility for the data analysis’s accuracy and the data’s integrity, and contributing to revising the article and final approval. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Medical Science and Technology Project of Zhejiang province, China (2022KY898) and the Science and Technology Plan Project of Wenzhou, China (Y2019038) provided funding for this study, which had no role in the study design, collection, analysis, or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank all patients and staff who cooperated in this study.
References
- 1.WHOQOL Group. Study protocol for the World Health Organization project to develop a quality of life assessment instrument (WHOQOL). Qual Life Res. (1993) 2:153–9. doi: 10.1007/BF00435734, PMID: [DOI] [PubMed] [Google Scholar]
- 2.WHOQOL Group. The World Health Organization quality of life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med. (1995) 41:1403–9. doi: 10.1016/0277-9536(95)00112-K, PMID: [DOI] [PubMed] [Google Scholar]
- 3.Haraldstad K, Wahl A, Andenæs R, Andersen JR, Andersen MH, Beisland E, et al. A systematic review of quality of life research in medicine and health sciences. Qual Life Res. (2019) 28:2641–50. doi: 10.1007/s11136-019-02214-9, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fumincelli L, Mazzo A, Martins JCA, Mendes IAC. Quality of life and ethics: a concept analysis. Nurs Ethics. (2019) 26:61–70. doi: 10.1177/0969733016689815 [DOI] [PubMed] [Google Scholar]
- 5.Fusar-Poli P, Salazar de Pablo G, de Micheli A, Nieman DH, Correll CU, Kessing LV, et al. What is good mental health? A scoping review. Eur Neuropsychopharmacol. (2020) 31:33–46. doi: 10.1016/j.euroneuro.2019.12.105 [DOI] [PubMed] [Google Scholar]
- 6.Mo Y, Deng L, Zhang L, Lang Q, Liao C, Wang N, et al. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J Nurs Manag. (2020) 28:1002–9. doi: 10.1111/jonm.13014, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu Q, Luo D, Haase JE, Guo Q, Wang XQ, Liu S, et al. The experiences of health-care providers during the COVID-19 crisis in China: a qualitative study. Lancet Glob Health. (2020) 8:e790–8. doi: 10.1016/S2214-109X(20)30204-7, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oyama Y, Fukahori H. A literature review of factors related to hospital nurses’ health-related quality of life. J Nurs Manag. (2015) 23:661–73. doi: 10.1111/jonm.12194 [DOI] [PubMed] [Google Scholar]
- 9.Chew NWS, Lee GKH, Tan BYQ, Jing M, Goh Y, Ngiam NJH, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. (2020) 88:559–65. doi: 10.1016/j.bbi.2020.04.049, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhu J, Sun L, Zhang L, Wang H, Fan A, Yang B, et al. Prevalence and influencing factors of anxiety and depression symptoms in the first-line medical staff fighting against COVID-19 in Gansu. Front Psych. (2020) 11:386. doi: 10.3389/fpsyt.2020.00386, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kang L, Ma S, Chen M, Yang J, Wang Y, Li R, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. (2020) 87:11–7. doi: 10.1016/j.bbi.2020.03.028, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Busch IM, Moretti F, Mazzi M, Wu AW, Rimondini M. What we have learned from two decades of epidemics and pandemics: a systematic review and Meta-analysis of the psychological burden of frontline healthcare workers. Psychother Psychosom. (2021) 90:178–90. doi: 10.1159/000513733, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rezaei S, Karami Matin B, Hajizadeh M, Soroush A, Nouri B. Prevalence of burnout among nurses in Iran: a systematic review and meta-analysis. Int Nurs Rev. (2018) 65:361–9. doi: 10.1111/inr.12426, PMID: [DOI] [PubMed] [Google Scholar]
- 15.Roberts DL, Cannon KJ, Wellik KE, Wu Q, Budavari AI. Burnout in inpatient-based versus outpatient-based physicians: a systematic review and meta-analysis. J Hosp Med. (2013) 8:653–64. doi: 10.1002/jhm.2093, PMID: [DOI] [PubMed] [Google Scholar]
- 16.Guo Y, Hu S, Liang F. The prevalence and stressors of job burnout among medical staff in Liaoning, China: a cross-section study. BMC Public Health. (2021) 21:777. doi: 10.1186/s12889-021-10535-z, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cruz JP. Quality of life and its influence on clinical competence among nurses: a self-reported study. J Clin Nurs. (2017) 26:388–99. doi: 10.1111/jocn.13402, PMID: [DOI] [PubMed] [Google Scholar]
- 18.Hall LH, Johnson J, Watt I, Tsipa A, O’Connor DB. Healthcare staff wellbeing, burnout, and patient safety: a systematic review. PLoS One. (2016) 11:e0159015. doi: 10.1371/journal.pone.0159015, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Søvold LE, Naslund JA, Kousoulis AA, Saxena S, Qoronfleh MW, Grobler C, et al. Prioritizing the mental health and well-being of healthcare workers: An urgent global public health priority. Front Public Health. (2021) 9:679397. doi: 10.3389/fpubh.2021.679397, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Seligman MEP. Positive psychology: a personal history. Annu Rev Clin Psychol. (2019) 15:1–23. doi: 10.1146/annurev-clinpsy-050718-095653 [DOI] [PubMed] [Google Scholar]
- 21.Roser K, Mader L, Baenziger J, Sommer G, Kuehni CE, Michel G. Health-related quality of life in Switzerland: normative data for the SF-36v2 questionnaire. Qual Life Res. (2019) 28:1963–77. doi: 10.1007/s11136-019-02161-5, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhou K, Li M, Wang W, An J, Huo L, He X, et al. Reliability, validity, and sensitivity of the Chinese short-form 36 health survey version 2 (SF-36v2) in women with breast cancer. J Eval Clin Pract. (2019) 25:864–72. doi: 10.1111/jep.13088, PMID: [DOI] [PubMed] [Google Scholar]
- 23.AboAbat A, Qannam H, Bjorner JB, Al-Tannir M. Psychometric validation of a Saudi Arabian version of the sf-36v2 health survey and norm data for Saudi Arabia. J Patient Rep Outcomes. (2020) 4:67. doi: 10.1186/s41687-020-00233-6, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alhaji MM, Johan NH, Sharbini S, Abdul Hamid MR, Khalil MAM, Tan J, et al. Psychometric evaluation of the Brunei-Malay SF-36 version 2 health survey. Asian Pac J Cancer Prev. (2018) 19:1859–65. doi: 10.22034/APJCP.2018.19.7.1859, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kangwanrattanakul K, Auamnoy T. Psychometric testing of the health-related quality of life measurement, SF-36v2, in the general population of Thailand. Expert Rev Pharmacoecon Outcomes Res. (2019) 19:313–20. doi: 10.1080/14737167.2019.1530595, PMID: [DOI] [PubMed] [Google Scholar]
- 26.Huang F, Yang Z, Wang Y, Zhang W, Lin Y, Zeng LC, et al. Health-related quality of life and influencing factors of pediatric medical staff during the COVID-19 outbreak. Front Public Health. (2020) 8:565849. doi: 10.3389/fpubh.2020.565849, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Niestrój-Jaworska M, Dębska-Janus M, Polechoński J, Tomik R. Health behaviors and health-related quality of life in female medical staff. Int J Environ Res Public Health. (2022) 19:3896. doi: 10.3390/ijerph19073896, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marsh HW, Lüdtke O, Trautwein U, Morin AJ. Classical latent profile analysis of academic self-concept dimensions: synergy of person-and variable centered approaches to theoretical models of self-concept. Struct Equ Model Multidiscip J. (2009) 16:191–225. doi: 10.1080/10705510902751010 [DOI] [Google Scholar]
- 29.MacLean E, Dendukuri N. Latent class analysis and the need for clear reporting of methods. Clin Infect Dis. (2021) 73:e2285–6. doi: 10.1093/cid/ciaa1131, PMID: [DOI] [PubMed] [Google Scholar]
- 30.Sinha P, Calfee CS, Delucchi KL. Practitioner’s guide to latent class analysis: methodological considerations and common pitfalls. Crit Care Med. (2021) 49:e63–79. doi: 10.1097/CCM.0000000000004710, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.World Medical Association . World medical association declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. (2013) 310:2191–4. doi: 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 32.Kim SY. Determining the number of latent classes in single-and multi-phase growth mixture models. Struct Equ Modeling. (2014) 21:263–79. doi: 10.1080/10705511.2014.882690, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Preacher KJ, Merkle EC. The problem of model selection uncertainty in structural equation modeling. Psychol Methods. (2012) 17:1–14. doi: 10.1037/a0026804, PMID: [DOI] [PubMed] [Google Scholar]
- 34.Liu Y, Chen H, Zhang N, Wang X, Fan Q, Zhang Y, et al. Anxiety and depression symptoms of medical staff under COVID-19 epidemic in China. J Affect Disord. (2021) 278:144–8. doi: 10.1016/j.jad.2020.09.004, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Du J, Mayer G, Hummel S, Oetjen N, Gronewold N, Zafar A, et al. Mental health burden in different professions during the final stage of the COVID-19 lockdown in China: cross-sectional survey study. J Med Internet Res. (2020) 22:e24240. doi: 10.2196/24240, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Luo L, Ni J, Zhou M, Wang C, Wen W, Jiang J, et al. Food safety knowledge, attitudes, and self-reported practices among medical staff in China before, during and after the COVID-19 pandemic. Risk Manag Healthc Policy. (2021) 14:5027–38. doi: 10.2147/RMHP.S339274, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stanulewicz N, Knox E, Narayanasamy M, Shivji N, Khunti K, Blake H. Effectiveness of lifestyle health promotion interventions for nurses: a systematic review. Int J Environ Res Public Health. (2019) 17:17. doi: 10.3390/ijerph17010017, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Silva AA, Souza JM, Borges FN, Fischer FM. Health-related quality of life and working conditions among nursing providers. Rev Saude Publica. (2010) 44:718–25. doi: 10.1590/S0034-89102010000400016 [DOI] [PubMed] [Google Scholar]
- 39.Turchi V, Verzuri A, Nante N, Napolitani M, Bugnoli G, Severi FM, et al. Night work and quality of life. A study on the health of nurses. Ann Ist Super Sanita. (2019) 55:161–9. doi: 10.4415/ANN_19_02_08 [DOI] [PubMed] [Google Scholar]
- 40.Mengyao L, Kanghui H, Yulian H, Yuanyuan Z, Yaqing Z. The exploration of the influencing factors of occupation fatigue of nurses. Chin J Nurs. (2022) 57:853–8. doi: 10.3761/j.issn.0254-1769.2022.07.014 [DOI] [Google Scholar]
- 41.Siegrist J. Adverse health effects of high-effort/low-reward conditions. J Occup Health Psychol. (1996) 1:27–41. doi: 10.1037/1076-8998.1.1.27, PMID: [DOI] [PubMed] [Google Scholar]
- 42.Coyle C, Ghazi H, Georgiou I. The mental health and well-being benefits of exercise during the COVID-19 pandemic: a cross-sectional study of medical students and newly qualified doctors in the UK. Ir J Med Sci. (2021) 190:925–6. doi: 10.1007/s11845-020-02423-z, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ruegsegger GN, Booth FW. Health benefits of exercise. Cold Spring Harb Perspect Med. (2018) 8:a029694. doi: 10.1101/cshperspect.a029694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Heidke P, Vandelanotte C, Irwin C, Williams S, Saluja S, Khalesi S. Associations between health-related quality of life and health behaviors in Australian nursing students. Nurs Health Sci. (2021) 23:477–89. doi: 10.1111/nhs.12832 [DOI] [PubMed] [Google Scholar]
- 45.Spittlehouse JK, Vierck E, Pearson JF, Joyce PR. Temperament and character as determinants of well-being. Compr Psychiatry. (2014) 55:1679–87. doi: 10.1016/j.comppsych.2014.06.011 [DOI] [PubMed] [Google Scholar]
- 46.Suleiman-Martos N, Gomez-Urquiza JL, Aguayo-Estremera R, Cañadas-De La Fuente GA, De La Fuente-Solana EI, Albendín-García L. The effect of mindfulness training on burnout syndrome in nursing: a systematic review and meta-analysis. J Adv Nurs. (2020) 76:1124–40. doi: 10.1111/jan.14318, PMID: [DOI] [PubMed] [Google Scholar]
- 47.Kunzler AM, Helmreich I, König J, Chmitorz A, Wessa M, Binder H, et al. Psychological interventions to foster resilience in healthcare students. Cochrane Database Syst Rev. (2020) 7:Cd013684. doi: 10.1002/14651858.CD013684 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.