Abstract
Rationale
Nurses working in the intensive care unit (ICU) are constantly bombarded with stressful events and traumatic situations that may have deleterious effects on their health. The implications and the outcomes of exposure to these constant stressors by this workforce, on their mental health, are largely unknown.
Objective
To determine and measure if critical care nurses are having more work-related mental disturbances compared to their counterparts who are working in less stressful environments such as wards.
Materials and methods
We collected data from three large tertiary care hospitals in south India spanning over two states (n = 383 and 220 respectively) using various validated tools.
Relevant data and results
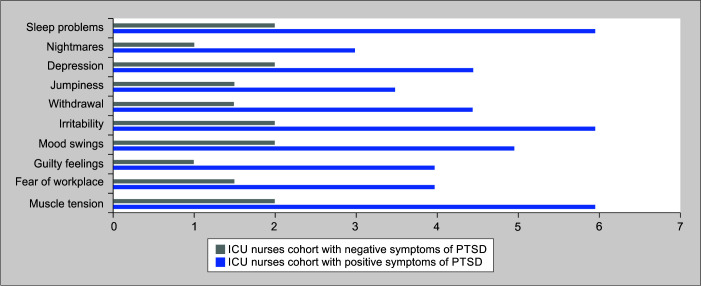
In both cohorts of nurses, we determined the prevalence of symptoms of post-traumatic stress disorder (PTSD), depression, and anxiety using various validated tools such as PTSS-10 and hospital anxiety and depression scale (HADS). About 29% (CI 95%,18–37) of the ICU nurses were found to have symptoms PTSD, in comparison to 15% (95% CI,10–21) of the ward nurses (p = 0.04). The stress levels apart from the workplace reported by both groups were statistically similar. In the sub-domains of depression and anxiety, both groups faired equal probabilities.
Conclusion
From this multicenter study, we have found that the staff nurses working in critical care areas of the hospital suffering from PTSD to a greater extent compared to their counterparts working in calmer ward conditions. This study will shower vital information to hospital administration and nursing leadership in improving the workplace mental health and satisfaction at jobs of ICU nurses working in tedious working conditions.
How to cite this article
Mathew C, Mathew C. The Prevalence of Post-traumatic Stress Disorder Symptoms in Critical Care Nurses of Tertiary Care Hospitals in South India: A Multicenter Cross-Sectional Cohort Study. Indian J Crit Care Med 2023;27(5):330–334.
Keywords: Critical care, Ethics, Indian intensive care unit, Intensive care unit, Nurses, Post-traumatic stress disorder, Quality improvement
Highlights
Nurses working in the ICU are constantly bombarded with work-related stressors compared to their counterparts working in calmer environments such as wards. This has direct implications for their mental health
Mitigation of mental health issues of ICU nurses leads to retention of the workforce and thus greater productivity.
Stress is an integral part of every work-life. The stress levels in the intensive care units (ICUs) are enormous due to the presence of critically ill patients with higher rates of adverse patient events, frequent confrontation of ethical dilemmas, and an adrenaline-rushed atmospheres.1 The psychological effects of the intense working environment in the ICU on critical care nurses are relatively unexplored.2 An estimate in 2019 showed 95 thousand of ICU beds across India.3 The pandemic of COVID-19 and its sequelae causes an increased demand for ICU beds and thus the critical care nursing workforce. The ICU force is frequently bombarded with work-based stressors in the high-dependency environment and the failure to adapt to the field condition has the consequence of developing psychomotor symptoms like post-traumatic stress disorders (PTSD) or depression.4 Various surveys in developed countries found that the reason for the loss of the workforce is to have a peaceful work-life pattern.5,6
According to a famous psychiatry association, PTSD can happen to people who have encountered traumatic events in any domain of their lifetime. They have disturbing and periodic thoughts regarding their harsh experiences through nightmares and flashbacks. They find it difficult to connect with their society. They lag behind their peer in various domains of their life and find it difficult to return back to healthy living.7
We begin our study by hypothesizing that staff nurses working in ICU may be having a higher level of stress-related disorders compared to their co-group managing the non-critical areas like a ward. We have collected, compared, and analyzed data from staff nurses working in critical areas and non-critical areas serving the adult patient population of three tertiary care medical hospitals of South India in the month of June 2022 – DMMC Medical College and Hospital, Wayanad (H1), IQRAA Hospital Sulthanbathery (H2) and the Government Medical College and Hospital, Kozhikode (H3), which are run by a private trust, private management and state government respectively.
Materials and Methods
The survey questionnaire consists of a biography of the respondent and the impressions regarding the place of work. The survey questionnaire was completely voluntary and required a few minutes for its completion. The post-traumatic stress syndrome 10 questions (PTSS-10) inventory, which is a subject-reported scale based on the diagnostic and statistical manual (DSM) for post-traumatic stress disorder was used to measure the symptoms. The diagnosis of PTSD is favored by a score greater than or equal to 35 points in PTSS-10.8,9 The statistical significance on the domains of sensitivity and specificity for PTSS-10 is well validated and is used extensively.10 Post-traumatic stress syndrome 10 questions has high stability (reliability in test-retest conditions, r-value of 0.89) and good internal consistency and reliability (Cronbach's alpha score = 0.92).11 The survey questionnaire also included the hospital anxiety and depression scale (HADS). It has subdomains that measure anxiety and depression levels in the subjects tested.12–14 A score of more than 8 is significant.15
We administered the questionnaires (PTSS-10 and HADS) to full-time employed critical care nurses of three tertiary care hospitals (H1, H2, H3) in South India. The data collection was in the month of June 2022 (mid-year). DMMC Medical College Hospital, Wayanad (H1) also known as Dr. Moopen's Medical College is a 700 bedded tertiary care teaching hospital with 35 adult ICU beds. IQRAA Hospital Sulthan Bathery (H2) is a 100 bedded tertiary care teaching hospital with 13 adult ICU beds. Government Medical College and Hospital, Kozhikode (H3) is a 3025 bedded tertiary care teaching hospital with 184 adult ICU beds. We also administered the questionnaire to full-time employed general ward nurses of these three hospitals. About 383 ICU nurses (H1-82, H2-30, H3-271) and 220 ward nurses (H1-50, H2-20, H3-150) completed the survey. Participants were informed in detail regarding the study and consent was taken. The taboo terms such as “post-traumatic stress disorder, depression, anxiety, etc.” were not used during answering questions regarding the questionnaire. The voluntary survey was completed anonymously. All relevant permissions were taken.
Statistical Analysis
The t-test and Chi-squared test were used for normally distributed data. Non-normal data warranted various non-parametric analyses. In the examination of parameters having positive predictive value towards causation of PTSD, a backward elimination modeling strategy for all multivariable logistic regression analyses was used (JMP; SAS Institute, Inc; Cary, NC). To assess for effect modification, interaction terms between the groups of staff assessed, viz surgical/medical general ward vs ICU, and a group of other independent parameters were entered into the parent model. If the odds ratio is unaffected, individual confounding factors are untouched for analysis which increases the meaningful data volume. In all multivariable logistic regression analyses for each independent variable, 95% confidence intervals (CIs) were determined by us. In all our statistical tests, a significance value of 0.05(α) was used.
Result From the Data
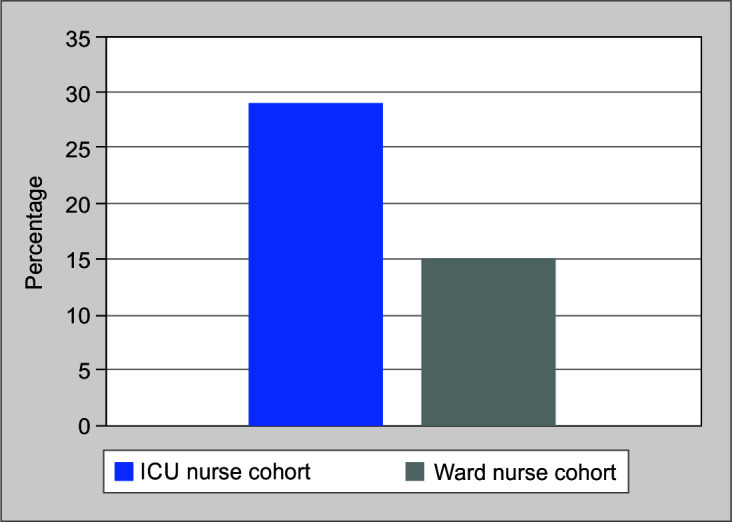
The multicenter cross-sectional cohort study was conducted in the month of June 2022. About six hundred three (603) full-time nursing staff (383 critical nurses and 220 non-critical) from the three hospitals completed the questionnaire. The particulars of the staff participated from each group are shown (Table 1). Averagely critical nurses worked longer shifts and lesser days in a week compared to ward nurses. The average patient-nurse ratio for ward nurses was higher in comparison with their ICU counterparts [7:1(range, 7:1–8:1) vs 3:1 (range, 3:1–3:1); p < 0.001]. Overall, 47% of critical care nurses feel that they helped each other during their duty hours, in comparison with 30% of non-critical nurses (p = 0.03). Both groups showed similar trends in non-job related stressors apart from the hospital environment (3.6 ± 1.4 vs 3.8 ± 1.4 on a scale of 1–7; p = 0.6). Significantly more critical care nurses felt signs and symptoms consistent with post-traumatic stress disorder (29% (95% CI, 18–37)) according to criteria laid down, compared with 15% (95% CI, 10–21) of the ward nurses (p = 0.04); Figure 1. Analysis of the ICU nurse group showed that many had a symptom of a nightmare (23%), and others had panic attacks and anxiety disorders (18%) due to the ICU working environment. Equalizing most of the biographical parameters, the significant factor that stands out to be in direct implication on the PTSD symptom occurrence was being an ICU nurse (Odds ratio, 1.41; 95% CI, 1.20–1.82; p = 0.03). The positive symptoms of PTSD were significantly pronounced in all its domains compared to the negative symptoms of PTSD shown (Table 3) in the group of ICU nurses tested, which was distributed over 10 domains of PTSS-10 scale (p < 0.001 in every domain); Figure 2.
Table 1.
Personal parameters of ICU and ward nurses in the three tertiary care hospitals (H1, H2, H3)
| Group of ICU nurses (n = 383) | Group of Ward nurses (n = 220) | p-value | |
|---|---|---|---|
| Sex, (% F) | 84 | 97 | 0.009 |
| Age, year (mean ± SD) | 33.8 ± 11.5 | 32.5 ± 12.6 | <0.001 |
| Marital status, % Single Married Divorced Other |
35 (134/383) 51 (196/383) 4 (14/383) 10 (39/383) |
46 (103/220) 48 (105/220) 4 (8/220) 2 (4/220) |
0.0032 |
| Children living in household, %positive | 59 | 64 | 0.012 |
| Responsible for primary household income, % | 49 | 46 | 0.06 |
| Experience in nursing field, year (mean ± SD) | 10.4 ± 9.2 | 9.6 ± 9.1 | <0.001 |
| Primary working shift, % day shift | 65 | 71 | 0.11 |
| Patient-to-nurse ratio at primary position, median (25–75% quartiles) | 3:1 (3–3:1) | 7:1 (7–8:1) | <0.001 |
| Hours of work in a day, n (mean ± SD) | 10.9 ± 2.1 | 9.2 ± 1.6 | <0.001 |
| Days of work in a week, n (mean ± SD) | 4.1 ± 0.8 | 4.9 ± 0.7 | <0.001 |
Fig. 1.
Prevalence of positive symptoms for PTSD
Table 3.
Stressors listed by intensive care unit nurses (% reported) at workplace
| Care of the expired patient (63) Witnessing the death of patients (57) Dealing with aggressive patients (57) Hospice care involvement of the dying patient (52) Berating from family members of the patient (46) Beratement from Consultants (44) Beratement from co-workers (43) Gross and disintegrated surgical wound (41) Large hemorrhage (38) Trauma wounds and injuries (37) Doing “futile” patient interventions (32) Doing CPCR-cardio-pulmonary cerebral resuscitation (22) Inadequacy of nurses per patient (21) Bereavement in the loss of a particular patient (11) |
Fig. 2.
Distribution of PTSS-10 scores stratified by ICU nurses for symptoms of PTSD
Table 2.
Data pertaining to ICU nurses pertaining to PTSD: Positive vs negative symptoms
| PTSD positive symptoms(n = 111) | PTSD negative symptoms(n = 272) | p-value | |
|---|---|---|---|
| Age, years (mean ± SD) | 35.9 ± 9.1 | 37.9 ± 8.6 | 0.06 |
| Status of marriage (% married) | 41 | 57 | 0.05 |
| Having children, (% yes) | 45 | 63 | |
| Main bread winner of the family, (%) | 52 | 49 | 0.46 |
| Experience in nursing field, year Median (25–75% quartiles) |
7 (3–11) | 9 (4–18) | 0.21 |
| Work shift pattern, % | |||
| Early day shift Night or late day shift |
18 36 |
82 64 |
0.03 |
| Patients assigned to single nurse, median quartiles (25–75%) | 3:1 (3–3:1) | 3:1 (3–3:1) | 0.32 |
| Hours of work in a day, n (mean ± SD) | 10.8 ± 2.0 | 10.4 ± 1.6 | 0.21 |
| Days of work in a week, n (mean ± SD) | 4.0 ± 0.8 | 3.8 ± 1.0 | 0.05 |
| Overtime working nurses or taking multiple jobs, % | 55 | 63 | 0.57 |
| In the role of head nurse/lead nurse, % | 40 | 65 | 0.03 |
| Working in units where the head/lead nurse has more roles than assigned to them at the time of enrolment, % | 94 | 80 | 0.08 |
The probability of acquiring anxiety due to work environment was essentially similar in the ICU and ward workforce (20 vs 21%; p = 0.34), depression (28 vs 25%; p = 0.41), or anxiety or depression (38 vs 37%, p = 0.76) on the HADS survey. In the domains of anxiety and depression, statistics revealed not much difference between the groups, (12 vs 15%; p = 0.76).
The most frequently occurring PTSD-positive symptoms in ICU nurses were easy irritability, sleep disturbances, easily getting angry and being annoyed, and increased muscle turgor (Supplementary Tables). Evening and night shifts were preferred by the majority of the ICU nurses who showed signs of PTSD and were hesitant to take up the role of leading nurse roles. Surprisingly, the rate of mortality associated with a particular ICU was not found to be correlated with the incidence of PTSD in the nurses working in those units. Evening and night shift working pattern was the only variable found to be of significance in the incidence of PTSD symptoms, from a multivariable analysis (Odds ratio, 1.36; 95% CI, 1.21–1.82; p = 0.03). Table 3 lists the category of events that appeared traumatic related to the working environment of critical care staff.
Discussion
From this multicenter study, we have found that the staff nurses working in critical care areas of the hospital suffering from PTSD to a greater extent compared to their counterparts working in calmer ward conditions. Also, the difference was similar to some trials which suffered during times of war.16,17 Seniority plays a greater role in PTSD symptom occurrence as evidenced by our study.18 This study will shower vital information to hospital administration and nursing leadership in improving the workplace mental health and satisfaction at jobs of ICU nurses working in tedious working conditions.
A national survey conducted in India in 2016 found that women suffer from PTSD more than men.19 PTSD may be the tip of an iceberg of psychiatric symptoms. People who directly witness an unfortunate traumatic event have more recurrence than those who don't have a severe stimulus.20,21
Many of the ICU nurses may not fulfil the diagnostic criteria laid down by DSM-V. Even though all the criteria of PTSD according to DSM-V were not fulfilled by most of the nurses, the perception of significant PTSD-related symptoms was shown by those individuals. Thus, the differentiation between relevant normal and abnormal symptoms of PTSD has to be emphasized more, currently being controversial.20 Thus for our study of PTSD prevalence in critical care nurses, the concept of defining a subthreshold PTSD seems very relevant.20–22
Even though PTSS-10 and HADS we used in this study have excellent statistical value, the downside of it is that they may not diagnose PTSD based on the diagnostic criteria laid. But both tests clearly delineate the individuals having the work-life balance affected by the ICU stressors. A few of the other backsides of this study was that we didn't collect data regarding the permutations and combinations of various background stressors encountered by the critical care nurses of various ICUs and their variable penetration in their life and attitude towards work satisfaction. Again, end-of-life care is an important domain that needs to be taken of care with utmost precision as it may have a greater impact on the causation of PTSD in the staff. Various data collection methods placed as exit surveys, are used to find the causation of work dissatisfaction and the resignation of such staff, which may have deleterious effects in a developing country like India. They help in data collection, the rectification of problems, and retention of maximum staff imparting job satisfaction.
In conclusion, ICU nurses suffer from more PTSD compared to non-ICU nurses in the South Indian subset. The data can be extrapolated to another population subset also. Again, anxiety and depression are also greater in staff working under pressure environments. These findings can show greater light on the incidence and prevalence of stressors in various ICU environments and direct their solution. This can be an essential milestone the hospital administration and healthcare fraternity need to achieve for the collective good in the field of effective and sustainable patient care.
Many validated studies have found useful interventions to reduce stress levels in critical care units. The concept of finding the ‘locus of control’ is the most proven strategy. The individual him/herself will find what/who causes psychological turmoil, whether it occurs by chance or by powerful others; as depicted by a work of 1973.23 A few of the interventions that can be taken to improve the quality, the techniques that can be practiced by the individuals working in demanding environments is that viz, knowing and taking control of own challenging situations and get over the same or trying to modify the situation (control of internal locus). Always troubleshooting the causation and working towards the solution is the key.
Thus, in summary from our multicenter study, we have found that a greater proportion of the critical staff perceives work culture to have immense pressure which causes mental trauma. This overflow of tension from the workplace causes a reduction in their quality of life. This causes direct implications on the productivity of health care and retention of the workforce in the institutes of care. This multicenter study from South India could be extrapolated to bigger horizons for finding and improving the quality of life of those critical care staff who are the backbone of our healthcare establishments.
Orcid
Christopher Mathew https://orcid.org/0000-0002-4565-760X
Christina Mathew https://orcid.org/0000-0001-7434-1228
Supplementary Material
All the supplementary tables are available online on the website of www.IJCCM.org.
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Acker KH. Do critical care nurses face burnout, PTSD, or is it something else? Getting help for the helpers. AACN Clin Issues Crit Care Nurs. 1993;4(3):558–565. 8136229 [PubMed] [Google Scholar]
- 2.Kerasiotis B, Motta RW. Assessment of PTSD symptoms in emergency room, intensive care unit, and general floor nurses. Int J Emerg Ment Health. 2004;6(3):121–133. 15481474 [PubMed] [Google Scholar]
- 3.Sanyukta Kanwal. Estimated number of public and private hospital beds in India 2019. Statista survey. 2022. [Google Scholar]
- 4.Li P, Kuang H, Tan H. The occurrence of post-traumatic stress disorder (PTSD), job burnout and its influencing factors among ICU nurses. Am J Transl Res. 2021;13(7):8302–8308. 34377320 [PMC free article] [PubMed] [Google Scholar]
- 5.Stechmiller JK. The nursing shortage in acute and critical care settings. AACN Clin Issues. 2002;13(4):577–584. doi: 10.1097/00044067-200211000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Steinbrook R. Nursing in the crossfire. N Engl J Med. 2002;346(22):1757–1766. doi: 10.1056/NEJM200205303462225. [DOI] [PubMed] [Google Scholar]
- 7.Diagnostic and Statistical Manual of Mental Disorders (DSM-5), Fifth edition. American Psychiatric Association. 2013 [Google Scholar]
- 8.Schelling G, Stoll C, Haller M, Briegel J, Manert W, Hummel T, et al. Health-related quality of life and posttraumatic stress disorder in survivors of the acute respiratory distress syndrome. Crit Care Med. 1998;26(4):651–659. doi: 10.1097/00003246-199804000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Jonsson A, Segesten K, Mattsson B. Post-traumatic stress among Swedish ambulance personnel. Emerg Med J. 2003;20(1):79–84. doi: 10.1136/emj.20.1.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weisaeth L. Torture of a Norwegian ship's crew: The torture, stress reactions and psychiatric after-effects. Acta Psychiatr Scand Suppl. 1989;355:63–72. 2624136 [PubMed] [Google Scholar]
- 11.Thulesius H, Hakansson A. Screening for posttraumatic stress disorder symptoms among Bosnian refugees. J Trauma Stress. 1999;12(1):167–174. doi: 10.1023/A:1024758718971. [DOI] [PubMed] [Google Scholar]
- 12.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 13.Dahl AA, Haaland CF, Mykletun A, Bremnes R, Dahl O, Klepp O, et al. Study of anxiety disorder and depression in longterm survivors of testicular cancer. J Clin Oncol. 2005;23(10):2389–2395. doi: 10.1200/JCO.2005.05.061. [DOI] [PubMed] [Google Scholar]
- 14.Thompson DR, Meddis R. Wives’ responses to counselling early after myocardial infarction. J Psychosom Res. 1990;34(3):249–258. doi: 10.1016/0022-3999(90)90081-e. [DOI] [PubMed] [Google Scholar]
- 15.Herrmann C. International experiences with the hospital anxiety and depression scale: A review of validation data and clinical results. J Psychosom Res. 1997;42(1):17–41. doi: 10.1016/s0022-3999(96)00216-4. [DOI] [PubMed] [Google Scholar]
- 16.Dobson M, Marshall RP, Grayson DA. Subclinical stress responses in noncombatants. J Nerv Ment Dis. 1996;184(7):437–439. doi: 10.1097/00005053-199607000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Ursano RJ, McCarroll JE. The nature of a traumatic stressor: Handling dead bodies. J Nerv Ment Dis. 1990;178(6):396–398. doi: 10.1097/00005053-199006000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Caplan RP. Stress, anxiety, and depression in hospital consultants, general practitioners, and senior health service managers. BMJ. 1994;309(6964):1261–1263. doi: 10.1136/bmj.309.6964.1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.India state-level disease burden initiative mental disorders collaborators. The burden of mental disorders across the states of India: The global burden of disease study 1990–2017; Lancet Psychiatry. 2020;7(2):148–161. doi: 10.1016/S2215-0366(19)30475-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ruscio AM, Ruscio J, Keane TM. The latent structure of posttraumatic stress disorder: A taxometric investigation of reactions to extreme stress. J Abnorm Psychol. 2002;111(2):290–301. 12003450 [PubMed] [Google Scholar]
- 21.Grubaugh AL, Magruder KM, Waldrop AE, Elhai JD, Knapp RG, Frueh BC. Subthreshold PTSD in primary care: Prevalence, psychiatric disorders, healthcare use, and functional status. J Nerv Ment Dis. 2005;193(10):658–664. doi: 10.1097/01.nmd.0000180740.02644.ab. [DOI] [PubMed] [Google Scholar]
- 22.Blanchard EB, Hickling EJ, Taylor AE, Loos WR, Gerardi RJ. Psychological morbidity associated with motor vehicle accidents. Behav Res Ther. 1994;32(3):283–290. doi: 10.1016/0005-7967(94)90123-6. [DOI] [PubMed] [Google Scholar]
- 23.Levenson, H. Multidimensional locus of control in psychiatric patients. J Consult Clin Psychol. 1973;41(3):397–404. doi: 10.1037/h0035357. [DOI] [PubMed] [Google Scholar]