Abstract
Background
Fatty liver disease in the absence of excessive alcohol consumption is an increasingly common condition with a global prevalence of ~ 25–30% and is also associated with cardiovascular disease (CVD). Since systemic metabolic dysfunction underlies its pathogenesis, the term metabolic (dysfunction)-associated fatty liver disease (MAFLD) has been proposed for this condition. MAFLD is closely intertwined with obesity, type 2 diabetes mellitus and atherogenic dyslipidemia, which are established cardiovascular risk factors. Unlike CVD, which has received attention in the literature on fatty liver disease, the CVD risk associated with MAFLD is often underestimated, especially among Cardiologists.
Methods and results
A multidisciplinary panel of fifty-two international experts comprising Hepatologists, Endocrinologists, Diabetologists, Cardiologists and Family Physicians from six continents (Asia, Europe, North America, South America, Africa and Oceania) participated in a formal Delphi survey and developed consensus statements on the association between MAFLD and the risk of CVD. Statements were developed on different aspects of CVD risk, ranging from epidemiology to mechanisms, screening, and management.
Conculsions
The expert panel identified important clinical associations between MAFLD and the risk of CVD that could serve to increase awareness of the adverse metabolic and cardiovascular outcomes of MAFLD. Finally, the expert panel also suggests potential areas for future research.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12072-023-10543-8.
Keywords: Metabolic (dysfunction)-associated fatty liver disease, MAFLD, Non-alcoholic fatty liver disease, Cardiovascular disease, Consensus, Delphi survey
Introduction
Nonalcoholic fatty liver disease (NAFLD) is the most common chronic liver condition worldwide, with an estimated global prevalence of 25–30% [1]. Although it is recognized that NAFLD is linked to insulin resistance, overweight/obesity and type 2 diabetes mellitus (T2DM), NAFLD remains a diagnosis of exclusion that exists when all other competing causes of chronic liver disease have been tested for and excluded [2]. Moreover, the lack of any positive diagnostic criteria for NAFLD has not helped with disease characterization, public awareness or agreement on relevant clinical endpoints. In 2020, an international expert consensus recommended that the term “NAFLD” should be changed to the new term “metabolic (dysfunction)-associated fatty liver disease” (MAFLD), proposing a set of specific diagnostic criteria [3, 4]. In particular, the diagnosis of MAFLD is based on the presence of excess liver fat in combination with any of the following: overweight/obesity, T2DM, or evidence of at least two metabolic risk abnormalities (typically featuring the metabolic syndrome) [5]. This proposed change of terminology and definition aligns with the pathophysiology of MAFLD and emphasizes the key role of metabolic dysregulation in disease pathogenesis [6–9].
Although MAFLD and traditional risk factors for cardiovascular disease (CVD) can have a significant overlap, recent studies have shown that MAFLD is a predictor of adverse CVD outcomes, independent of traditional risk factors [10]. Increasing evidence now supports a link between MAFLD and CVD, and the importance of this association is well recognized among Hepatologists [11–14]. However, MAFLD as a novel CVD risk factor remains underappreciated and underdiagnosed, unlike many other traditional CVD risk factors [10]. Given that nearly three-quarters of global deaths are now caused by chronic, lifestyle-associated diseases (such as obesity, hypertension and diabetes), collaboration between medical specialties is essential to improve patient outcomes [15]. In this regard, increasing awareness of the adverse metabolic and cardiovascular effects of MAFLD among Cardiologists might help to decrease the global burden of chronic, lifestyle-associated diseases.
We have developed consensus statements using a two-round Delphi survey methodology among a large multidisciplinary group of international experts to shed light on the current opinion on the link between MAFLD and the risk of CVD. The consensus statements explore issues ranging from epidemiological data and clinical features to pathophysiological mechanisms, surveillance and management of this common and burdensome liver disease.
Methods
Study design
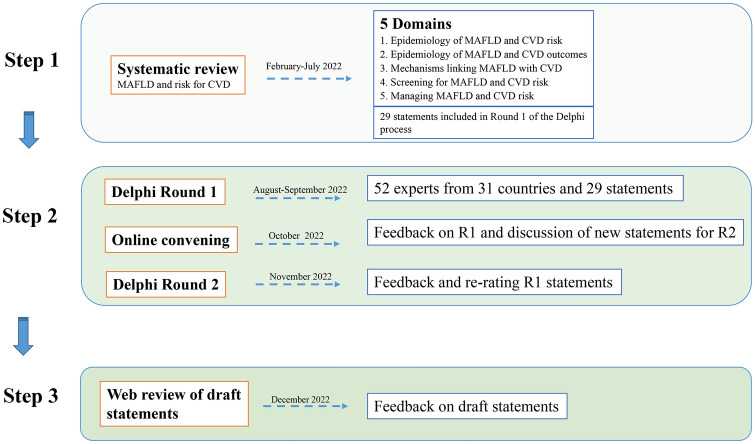
The consensus process used a Delphi procedure via two rounds of online surveys to obtain responses to questions about MAFLD and its association with CVD risk that require more unanimity (Fig. 1).
Fig. 1.
Flowchart of the Delphi procedure adopted for developing a consensus statement on MAFLD and risk of CVD
We (Xiao-Dong Zhou, Giovanni Targher, Christopher D. Byrne, Jacob George and Ming-Hua Zheng) selected expert panelists by identifying representative members from scientific societies of Cardiology, Hepatology, Diabetes/Endocrinology and Family Medicine, as well as core members of MAIDEN (Metabolic fAtty lIver DiseasE coNsortium) or corresponding authors of published articles on the association between MAFLD and CVD. To achieve global representation, we selected expert panelists from six continents: Asia, Europe, North America, South America, Africa and Oceania (Table 1). We created an email template outlining the research project and explaining the requirements of prospective panelists. Experts were included if they replied citing interest in involvement.
Table 1.
Demographic composition of the expert panel
| Characteristics | Round 1 | Round 2 |
|---|---|---|
| Surveys sent, n | 65 | 52 |
| Total respondents, % | 80% (52/65) | 100% (52/52) |
| Participant type, % | ||
| Cardiologist | 27% | |
| Hepatologist | 54% | |
| Endocrinologist | 10% | |
| Other | 10% | |
| Age group, % | ||
| < 40 yrs | 8% | |
| 40–65 yrs | 87% | |
| > 65 yrs | 6% | |
| Gender, % | ||
| Women | 17% | |
| Men | 83% | |
| Region of practice, % | ||
| Asia | 42% | |
| North America | 13% | |
| South America | 2% | |
| Europe | 35% | |
| Africa | 2% | |
| Oceania | 6% | |
In the first phase, we systematically reviewed the relevant literature published up to July 2022 and developed a set of statements for a structured first-round questionnaire. The systematic review took six months. Finally, five domains and 29 draft statements were included in the Round 1 (R1) survey, which was conducted using Google forms (link for R1: https://forms.gle/r2EVVntJkr1eJ1iq6). Experts were asked to score each statement across a four-scale range (‘Agree’/ ‘Somewhat agree’/ ‘Somewhat disagree’/ ‘Disagree’), with each question having a free text comment section.
The second phase, completed by 30th October 2022, included the Round 2 (R2) survey, containing a structured questionnaire in which the experts evaluated and re-evaluated statements until consensus was achieved. The R2 survey questions focused on controversial items identified by analyzing the R1 survey results and opinions (link for R2: https://forms.gle/mTjJvqhAmbvTUgRbA). Statements with agreement more than or equal to 80% were accepted. For questions for which consensus was not achieved in the R1 survey (< 80%), re-voting was carried out in the R2 survey after presenting the available evidence. Experts viewed the group results and changed their responses as they deemed appropriate.
In the last phase, consensus statements were developed. Each statement and recommendation was assigned a grade to indicate the level of agreement, using the grading system recorded in other Delphi studies [16, 17]: ‘U’ was unanimous (100%) agreement, ‘A’ was 90–99% agreement, ‘B’ 78–89% was agreement, and ‘C’ was 67–77% agreement. The statements were presented, discussed, and submitted for approval at the final stage. Any disagreements were resolved through discussion until a consensus was reached. The findings from this discussion and the surveys were used to prepare the consensus report.
Findings
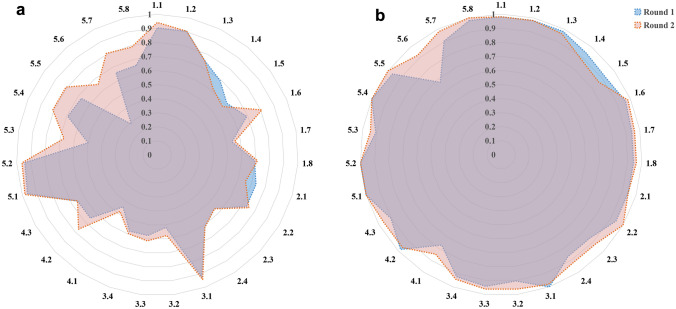
In this Consensus Statement, we report the final statements and recommendations along with a summary of the broader literature relating to the association between MAFLD and the risk of CVD. The consensus for all proposed statements increased across the two-round Delphi surveys. The mean percentage of responses selecting ‘agree’ increased from 67.1% in the R1 survey to 72.4% in the R2 survey (p = 0.002) and ‘agree or somewhat agree’ responses increased from 92.8% to 95.7% (p < 0.001) (Fig. 2). A grade of ‘U’ was given for 6/27 statements, ‘A’ for 18/27 statements, and ‘B’ on 3/27 statements (Table 2).
Fig. 2.
Proportion of experts replying "agree" by experts in Round 1 and Round 2 (a); and total proportion of experts replying "agree or somewhat agree" by experts in Round 1 and Round 2 (b)
Table 2.
Consensus statements on MAFLD and risk of CKD (using a Delphi procedure)
| Domain and statements | Gradea |
|---|---|
| 1. Epidemiology of MAFLD and risk of CVD | |
| 1.1 MAFLD is associated with an increased prevalence of CVD events compared with the non-MAFLD population | A |
| 1.2 MAFLD is associated with an increased incidence of nonfatal CVD events compared with the non-MAFLD population | A |
| 1.3 MAFLD is associated with an increased incidence of CVD mortality compared with the non-MAFLD population | A |
| 1.4 The incidence of fatal and/or nonfatal CVD events in individuals with MAFLD is higher compared to that in the NAFLD population | B |
| 1.5 MAFLD predicts better the risk of CVD events than NAFLD | B |
| 1.6 Increasing severity of liver fibrosis is associated with higher CVD risk | A |
| 1.7 Hepatic steatosis is associated with an increase in CVD risk | A |
| 1.8 MAFLD is a risk factor for CVD events even after adjustment for traditional cardiovascular risk factors | A |
| 2. Epidemiology of MAFLD and CVD outcomes | |
| 2.1 MAFLD is associated with greater carotid-artery intima-media thickness and increased risk of carotid atherosclerotic plaques | A |
| 2.2 MAFLD is associated with atherosclerotic CVD events such as acute coronary syndromes | U |
| 2.3 MAFLD is associated with increased risk of cardiac arrhythmias (mainly permanent atrial fibrillation) | A |
| 2.4 MAFLD is associated with abnormal myocardial function and structure | A |
| 3. Pathophysiological mechanisms linking MAFLD and CVD | |
| 3.1 MAFLD and CVD share multiple cardiometabolic risk factors, such as systemic low-grade inflammation, endothelial dysfunction, increased oxidative stress, insulin resistance and an atherogenic lipoprotein profile | A |
| 3.2 Activation of the renin-angiotensin system is one of the mechanistic links between MAFLD and CVD risk | A |
| 3.3 Some shared genetic polymorphisms (e.g., PNPLA3 I148M, and TM6SF2 E167K) may affect the risk of both MAFLD and CVD | A |
| 3.4 Gut microbiota may play a role in both MAFLD and CVD | A |
| 4. MAFLD and primary prevention of CVD | |
| 4.1 Carotid ultrasonography should be considered in most patients with MAFLD to improve CVD risk assessment | B |
| 4.2 In CVD risk assessment, MAFLD may be considered a CVD risk factor | A |
| 4.3 Screening for MAFLD should be considered in most patients with CVD | A |
| 5. Managing MAFLD and the risk of CVD | |
| 5.1 Clinicians who manage patients with MAFLD should target cardiometabolic risk factors (overweight/obesity, diabetes, dyslipidemia and hypertension) | U |
| 5.2 Lifestyle intervention (including a healthy dietary pattern, weight loss and regular physical exercise) is associated with improvement in both MAFLD and CVD | U |
| 5.3 Alcohol avoidance of any type or amount is advisable in patients with MAFLD and CVD | A |
| 5.4 Treatment with GLP-1RAs is beneficial in MAFLD patients with coexisting T2DM and may reduce CVD outcomes | U |
| 5.5 Treatment with SGLT-2 inhibitors is beneficial in MAFLD patients with coexisting T2DM and may reduce CVD outcomes | U |
| 5.6 Treatment with pioglitazone is beneficial in MAFLD patients and may reduce CVD outcomes, but potential adverse effects (e.g. weight gain, edema and worsening of pre-existing congestive heart failure) should be kept in mind | A |
| 5.7 Statins (if required for the treatment of dyslipidemia or CVD risk reduction) should be prescribed for patients with MAFLD even with modestly elevated serum liver enzyme levels (< 3 ULN) | A |
| 5.8 Bariatric surgery (if required in severely obese patients with MAFLD) improves liver histology features and reduces CVD risk | U |
CVD cardiovascular disease; GLP-1RAs glucagon-like peptide-1 receptor agonists; MAFLD metabolic (dysfunction) associated fatty liver disease; PNPLA3 patatin-like phospholipase domain-containing protein 3; SGLT-2 sodium-glucose cotransporter-2; T2DM type 2 diabetes mellitus; TM6SF2 trans-membrane 6 superfamily 2; ULN upper limit of normal
aGrade: U = unanimous (100%) agreement; A = 90–99% agreement; B = 78–89% agreement, and C = 67–77% agreement
Consensus statements and recommendations
Epidemiology of MAFLD and risk of CVD
Consensus statements 1.1–1.8 (Grade A in 1.1 to 1.3 and 1.6 to 1.8; Grade B in 1.4 and 1.5) (Table 2).
Consensus statement 1.1: MAFLD is associated with an increased prevalence of CVD events compared with the non-MAFLD population (Grade A).
Consensus statement 1.2: MAFLD is associated with an increased incidence of nonfatal CVD events compared with the non-MAFLD population (Grade A).
CVD is the leading cause of mortality in patients with NAFLD [1, 18, 19] and NAFLD is associated with a higher prevalence and incidence of fatal and nonfatal CVD events [20–23]. By definition, MAFLD is tightly linked to obesity, T2DM and atherogenic dyslipidemia, which are established cardiometabolic risk factors [24–27]. It is, therefore, not surprising that MAFLD is associated with a greater prevalence and incidence of adverse cardiovascular events compared to that observed in the non-MAFLD population. In a cohort of 12,183 participants from East China, investigators reported that the CVD burden (defined by Framingham risk score [FRS] or previous CVD) was greater in those with MAFLD than in the non-MAFLD population [28]. In a nationwide cohort of ~ 4.5 million Japanese individuals, Yoneda et al. [29] reported that the incidence rates of CVD were 2.69 (95% CI 2.55–2.83) and 1.01 (95% CI 0.98–1.03) per 1000 person-years in the MAFLD and non-MAFLD groups, respectively. Similar results were reported in other Asian cohort studies [30, 31]. Finally, a global meta-analysis by Wen et al. [32] confirmed that the incidence rates of CVD in patients with MAFLD were more than twice compared to those observed in subjects without MAFLD.
Consensus statement 1.3: MAFLD is associated with an increased incidence of CVD mortality compared with the non-MAFLD population (Grade A).
To date, conflicting data exist on CVD mortality in patients with NAFLD [21, 33, 34]. However, the contemporary largest meta-analysis by Mantovani et al. [23] clearly demonstrated that NAFLD was associated with a higher risk of nonfatal CVD events (pooled random-effects hazard ratio [HR] 1.40; 95% CI 1.20–1.64) and CVD mortality (pooled random-effects HR 1.30; 95% CI 1.08–1.56). Interestingly, the meta-regression analysis showed that pre-existing T2DM was a modifying factor and was associated with increased risk of CVD events. Notably, recent epidemiological data using the MAFLD definition reported that MAFLD was associated with a higher risk of CVD mortality [26, 30]. For instance, Kim et al. [35] analyzed data from 7761 participants from the Third National Health and Nutrition Examination Survey (NHANES III) and demonstrated that individuals with MAFLD had a nearly 25% higher risk of CVD mortality than those without MAFLD (HR 1.24; 95% CI 1.01–1.51). In a nationwide cohort study from South Korea (9.5 million participants), Lee et al. [30] reported that patients with MAFLD were at higher risk of CVD mortality (HR 1.46; 95% CI 1.41–1.52) compared to individuals without either MAFLD or NAFLD, whereas patients with NAFLD were not (HR 1.12; 95% CI 0.96–1.30). The aforementioned meta-analysis by Wen et al. [32] confirmed that CVD mortality was ~ 1.6 times higher in patients with MAFLD than in the control group. Collectively, therefore, accumulating evidence now indicates that MAFLD can identify subjects with poorer “metabolic health status” and higher risk of developing CVD events and mortality.
Consensus statement 1.4: The incidence of fatal and/or nonfatal CVD events in individuals with MAFLD is higher compared to that in the NAFLD population (Grade B).
Since there is considerable overlap (estimated around 80–90%) between the NAFLD and MAFLD populations, it is expected that those with MAFLD have essentially similar CVD risks to those with NAFLD [13, 14]. In line with this, investigators comparing the MAFLD-only and NAFLD-only populations reported that individuals with the MAFLD-only status (i.e. subjects with hepatic steatosis and metabolic risk factors) were at higher risk of CVD events compared with both individuals without MAFLD and those with the NAFLD-only status (i.e. subjects with hepatic steatosis without metabolic risk factors). Indeed, in these cohort studies the association between the NAFLD-only status and risk of CVD events was modest or absent [30, 36]. In the cohort study by Lee et al. [30], individuals with the MAFLD-only status were at higher risk of incident CVD outcomes (HR 1.43; 95% CI 1.41–1.45) compared with those without MAFLD or NAFLD, whereas the association between the NAFLD-only status and risk of CVD events was modest (HR 1.09; 95% CI 1.03–1.15). Similarly, in a retrospective cohort of 2,985 participants followed for 7 years, Niriella et al. [36] showed that the MAFLD-only status was associated with a higher risk of CVD events compared to the control group (HR 7.2; 95% CI 2.4–21.5), whilst the NAFLD-only status was not associated with CVD events compared to the non-steatotic control group (HR 1.90; 95% CI 0.25–14.8). Using data from the NHANES III database, Huang and colleagues [26] were among the first to show that MAFLD was associated with a higher risk of CVD mortality compared to NAFLD (HR 2.01; 95% CI 1.66–2.44 vs. HR 1.53; 95% CI 1.26–1.86, respectively), thus suggesting that the MAFLD definition may better identify subjects with a high-risk of adverse cardiovascular outcomes. In a recent meta-analysis of 7 observational cohort studies (including about 13 million individuals), Mantovani et al. [37] examined the differential risk of NAFLD and MAFLD definitions on fatal and nonfatal CVD events. These authors reported that each of the two definitions were associated with a higher risk of incident CVD events (pooled random-effects HR 1.50, 95% CI 1.30–1.72 for MAFLD vs. no-MAFLD; and pooled random-effects HR 1.27, 95% CI 1.12–1.45 for NAFLD vs. no-NAFLD, respectively). Although MAFLD identified a greater number of CVD events than NAFLD, the risk for fatal and nonfatal CVD events associated with either definition was not significantly different. [37]
Consensus statement 1.5: MAFLD predicts better the risk of CVD events than NAFLD (Grade B).
Predicting CVD risk is not a trivial task and different risk prediction tools have been used in people with MAFLD. Several studies from different countries showed that patients with MAFLD had a higher 10-year CVD risk (as estimated by the FRS or other CVD risk prediction tools) compared to those with NAFLD, thus confirming that MAFLD may identify a greater CVD risk burden [25, 27, 38, 39]. For instance, Zhang et al. [38] analyzed the NHANES 1999–2016 database and reported that patients with MAFLD had higher FRS compared to those with NAFLD, thus confirming that MAFLD may have a greater CVD risk burden. Kim et al. [25] analyzed data from 2,144 subjects without pre-existing CVD and showed that patients with MAFLD had a remarkably higher risk of intermediate to high 10-year CVD risk compared to those with NAFLD-only, with adjusted odds ratio (OR) of 8.17 (95% CI 2.40–36.1). It is known that the Suita CVD risk model is a risk prediction tool that can improve CVD risk prediction, relative to the FRS, among Japanese individuals [39]. Using the Suita CVD model, Tsutsumi et al. [27] reported that the MAFLD definition better identified patients at a high risk of developing CVD events than NAFLD definition.
Consensus statement 1.6: Increasing severity of liver fibrosis is associated with higher CVD risk (Grade A).
The assessment of liver fibrosis is particularly important for prognosis amongst patients with MAFLD because the severity of fibrosis is the strongest predictor of liver disease progression and the risk of CVD events. However, liver fibrosis assessment is often overlooked in relation to risk estimates for CVD events [23, 40]. A historical cohort using data from 8,511 health providers reported that patients with advanced liver fibrosis (estimated by Fibrosis-4 (FIB-4) index ≥ 2.67) had higher risk of CVD events after adjustment for sociodemographic variables, the European Systematic Coronary Risk Evaluation calculator (SCORE) score and use of statins or aspirin (HR 1.63; 95% CI 1.29–2.06), though not for age [41]. In a prospective study of nearly 900 patients with the metabolic syndrome who were followed for a median of 3.4 years, Baratta et al. [42] reported a nearly fourfold increase in fatal and non-fatal CVD events in those with NAFLD and FIB-4 ≥ 2.67 (HR 4.02; 95% CI 1.06–5.74). In the ongoing PLINIO study in Italy, an independent association was also observed between advanced liver fibrosis (as estimated by NAFLD Fibrosis score [NFS], which is primarily driven by metabolic factors) and the risk of CVD (ClinicalTrials.gov no: NCT04036357) [40]. Again, in a prospective study, involving 3,512 Japanese individuals, the presence of advanced liver fibrosis (as non-invasively assessed by FIB-4 ≥ 2.67 and other scores) was associated with higher CVD risk, independent of pre-existing T2DM, hypertension, and dyslipidemia [43]. Han et al. [44] analyzed the Korea NHANES 2008–2011 database and showed that individuals with MAFLD and advanced liver fibrosis (defined as FIB-4 ≥ 2.67) had a greater chance of high probability atherosclerotic CVD risk (OR 2.40; 95% CI 1.75–3.29) compared to those without MAFLD. Collectively, the evidence from these and other studies suggests that the development of hepatic fibrosis in MAFLD is, at least in part, an epiphenomenon of long-term exposure to common cardiometabolic risk factors, such as T2DM, obesity, and hypertension. These cardiometabolic risk factors closely align to systemic insulin resistance, low-grade inflammation, and increased oxidative stress. This, in turn, can exacerbate hepatocyte damage and results in activation of hepatic stellate and Kupffer cells, thereby driving hepatic fibrosis [45]. Thus, the severity of hepatic fibrosis could be considered as a non-lipid marker of CVD risk, while non-invasive fibrosis biomarkers, such as the widely used FIB4 and NFS scores or other newer non-invasive fibrosis biomarkers, such as the Enhanced Liver Fibrosis (ELF) and the PRO-C3 based fibrosis algorithm that included age, pre-existing diabetes, platelet count and serum PRO-C3 concentration (i.e., a marker of type III collagen formation) should be considered in CVD risk assessment. [46, 47]
Consensus statement 1.7: Hepatic steatosis is associated with an increase in CVD risk (Grade A).
Emerging evidence suggests that hepatic steatosis is also associated with increased CVD risk. For example, in a nested cohort study of 3,756 patients from the United States who underwent coronary computerized tomographic angiography, Meyersohn et al. [48] showed that hepatic steatosis on ultrasonography was associated with higher risk of developing major adverse CVD events, irrespective of atherosclerotic CVD risk scores, significant coronary stenosis, and metabolic syndrome features (adjusted HR 1.72; 95% CI 1.16–2.54). The PREVEND cohort involving 6,340 participants without pre-existing CVD also reported that hepatic steatosis (defined as fatty liver index [FLI] ≥ 60) was associated with higher CVD risk even after adjustment for traditional CVD risk factors [49]. Similarly, in a population-based cohort study using the UK Biobank database (196,128 participants), a FLI increase was associated with higher incidence of CVD events [50]. Using the Korean National Health Insurance dataset (involving 139,633 patients diagnosed with new-onset T2DM), Park et al. [51] reported that hepatic steatosis was associated with higher risk of CVD events and mortality. An updated meta-analysis of 38 observational studies reported that the prevalence of clinical and subclinical CVD was higher in patients with moderate to severe steatosis on liver ultrasound than those with mild steatosis. [20]
Consensus statement 1.8: MAFLD is a risk factor for CVD events even after adjustment for traditional cardiovascular risk factors (Grade A).
While evidence for the existence of an association between MAFLD and the risk of developing fatal and nonfatal CVD events is robust, the existence of an independent association between MAFLD and CVD is seemingly conflicting [29, 30, 52]. In the cohort study by Yoneda et al. [29], the risk of CVD events was higher in patients with MAFLD than in those without MAFLD, even after adjusting for common cardiometabolic risk factors. However, a prospective community-based cohort of South Korean individuals followed for 16 years, Moon et al. [52] showed that the association between MAFLD and risk of CVD events disappeared after adjustment for known CVD risk factors. However, it should be noted that this study was conceptually flawed as components of the metabolic syndrome should not be included in a statistical adjustment model for MAFLD, as they are also used to diagnose MAFLD. Removing these metabolic syndrome components invalidates the diagnosis of MAFLD and the resulting estimation only assesses the effect of hepatic steatosis alone on risk of CVD.
Although most of published cohort studies investigating associations between fatty liver disease and CVD, adjust for common CVD risk factors (such as T2DM, obesity, dyslipidemia, and hypertension), these CVD risk factors are often collinear in practice and are also part of the diagnostic criteria used for MAFLD. Probably, a more appropriate analysis would be to stratify patients and undertake a comparison between patients with MAFLD only (i.e., a condition always characterized by hepatic steatosis and coexisting metabolic dysregulation) versus patients with hepatic steatosis but without MAFLD (i.e. subjects with the NAFLD-only status who are characterized by the absence of metabolic dysregulation) or healthy controls.
Epidemiology of MAFLD and CVD outcomes
Consensus statements 2.1–2.4 (Grade U in 2.2; Grade A in 2.1, 2.3 and 2.4) (Table 2).
Consensus statement 2.1: MAFLD is associated with greater carotid-artery intima-media thickness and increased risk of carotid atherosclerotic plaques (Grade A).
NAFLD is closely associated with several markers of subclinical atherosclerosis [20, 24, 53]. There is also accumulating evidence to support an association between MAFLD and subclinical atherosclerosis markers, including higher carotid intima-media thickness (IMT), greater coronary artery calcification (CAC), as well as greater high-risk obstructive plaques and non-calcified plaques of coronary arteries. For instance, in a cross-sectional study of 890 Japanese subjects who underwent health check-ups, Rieko Bessho et al. [54] showed that patients with MAFLD (especially if T2DM was present) had higher odds for CAC compared to both patients with NAFLD and those without hepatic steatosis. In a prospective cohort study of 4,507 participants with normal brachial-ankle pulse wave velocity (baPWV) followed for 4.3 years, Wang et al. [55] reported that MAFLD was associated with higher risk of developing elevated baPWV (> 1773 cm/s). In another prospective community-based cohort of 6,232 participants, who were followed for a median of 4.3 years, Liu et al. [56] reported that MAFLD was associated with a greater risk of developing subclinical atherosclerosis. In addition, in a subsequent study, the same authors also reported that regression of MAFLD was associated with a lower risk of developing subclinical atherosclerosis, especially among those with a low probability of liver fibrosis or fewer metabolic risk factors [56]. Using the Kanbguk Samsung Health Study cohort database, Sung et al. reported that both NAFLD and MAFLD were associated with higher risk of developing incident CAC, even after adjusting for age, sex, educational level, smoking, physical activity, pre-existing coronary artery disease, plasma low-density lipoprtoein (LDL)-cholesterol concentrations, or use of lipid-lowering agents. However, these associations were stronger for MAFLD [57].
Consensus statement 2.2: MAFLD is associated with atherosclerotic CVD events such as acute coronary syndromes (Grade U).
Recent evidence also indicates that MAFLD may be associated with acute or chronic coronary syndromes. In a cohort study of 3,306 patients with chronic coronary syndrome, Liu et al. [58] reported that patients with MAFLD had a higher risk of adverse CVD outcomes compared to their counterparts without MAFLD. In a prospective analysis of nearly 500 hospitalized patients with acute coronary syndrome and hepatic steatosis, Noda et al. [59] found that the coexistence of MAFLD and impaired physical function tests independently predicted the risk of adverse CVD outcomes. Finally, some cohort studies found that the MAFLD-only status was more strongly associated with risk of nonfatal CVD events than the NAFLD-only status [10, 35, 36, 60]. These findings suggest that the MAFLD definition is better than the NAFLD definition for identifying patients who are at high risk of developing major CVD events.
Consensus statement 2.3: MAFLD is associated with increased risk of cardiac arrhythmias (mainly permanent atrial fibrillation) (Grade A).
Growing evidence also suggests that MAFLD is associated with an increased risk of cardiac arrhythmias, mainly permanent atrial fibrillation (AF) and certain ventricular tachyarrhythmias. A meta-analysis of 19 observational studies (involving about 7 million individuals) showed that MAFLD was closely associated with increased prevalence and incidence of permanent AF, QTc interval prolongation and some cardiac conduction defects [61]. In a nationwide health check-up population in China (including more than 2 million individuals), Lei et al. found that MAFLD was associated with a higher risk of having and developing permanent AF [62]. Decoin et al. [63] analyzed a cohort of United States patients after AF ablation and found that advanced liver fibrosis (estimated by non-invasive fibrosis biomarkers) in those with MAFLD was associated with adverse atrial remodeling and AF recurrence following catheter ablation.
Consensus statement 2.4: MAFLD is associated with abnormal myocardial function and structure (Grade A).
MAFLD is also associated with abnormal cardiac function and structure. The magnitude of this risk increases with the severity of liver disease in MAFLD. A meta-analysis by Leite-Moreira et al. [64] reported that MAFLD was associated with adverse structural alterations and cardiac dysfunction (mainly left ventricular diastolic dysfunction). Another updated meta-analysis [65] of observational studies confirmed that MAFLD was associated with impaired systolic and diastolic functions associated with cardiac structural changes. This meta-analysis also found that concomitant metabolic risk factors and liver disease severity were independently associated with abnormalities in cardiac function. Finally, Peng et al [66]. found that MAFLD was associated with left ventricular diastolic dysfunction and cardiac remodeling (including greater inter-ventricular septum thickness and left ventricular posterior wall thickness, as well as larger left atrial diameter and greater left ventricular hypertrophy), especially in patients with coexisting T2DM or obesity and in those with moderate-to-severe hepatic steatosis.
As discussed below in more detail, there are multiple potential pathophysiological mechanisms by which MAFLD may increase the risk of cardiac remodeling and hypertrophy and arrhythmic complications (mostly permanent AF) [67, 68].
Pathophysiological mechanisms linking MAFLD with CVD
Consensus statements 3.1–3.4 (Grade A in 3.1 to 3.4) (Table 2).
Consensus statement 3.1: MAFLD and CVD share multiple cardiometabolic risk factors, such as systemic low-grade inflammation, endothelial dysfunction, increased oxidative stress, insulin resistance and an atherogenic lipoprotein profile (Grade A).
Multiple shared cardiometabolic risk factors linked to MAFLD may synergistically promote the development of CVD [10]. Abnormal glucose and lipid metabolism and increased oxidative stress play key roles in the pathogenesis of metabolic dysregulation in both MAFLD and CVD. First, increased oxidative stress, low-grade inflammation and endothelial dysfunction have been shown to promote a pro-atherogenic milieu that induces the development of CVD [69]. Increased oxidative stress may contribute to low-grade inflammation by inducing endothelial dysfunction that in turn increases platelet activation and vascular plaque formation, thus promoting CVD development in patients with MAFLD [70]. Second, MAFLD predisposes to atherogenic dyslipidemia, which is typically characterized by high levels of triglycerides and very low density lipoprotein (VLDL) remnant lipoproteins, and low levels of high-density lipoprotein (HDL)-cholesterol [71]. Patients with obesity, T2DM or metabolic syndrome have high levels of remnant lipoproteins due to activation of hormone sensitive lipase, which in turns causes increased hydrolysis of triglycerides from adipose tissue, thus inducing elevated plasma free fatty acid levels and hepatic fat accumulation [72]. This altered serum lipoprotein profile associated with MAFLD is typical of the atherogenic dyslipidemia that is characterized by high LDL particle concentration (with normal to modestly elevated LDL-cholesterol levels) and a greater abundance of small dense low density lipoprotein (sd-LDL), as well as increased remnant lipoproteins and decreased HDL particle concentration [73]. This lipid phenotype likely may contribute to the increased CVD risk observed in MAFLD. Lastly, MAFLD is strongly associated with greater insulin resistance which is also involved in CVD development [74]. Insulin resistance increases hyperglycemia, triggers oxidative stress, increases low-grade inflammation, and causes endothelial dysfunction, possibly through the release of several pro-atherogenic, pro-coagulant, and pro-inflammatory mediators [75].
Consensus statement 3.2: Activation of the renin-angiotensin system is one of the mechanistic links between MAFLD and CVD risk (Grade A).
Additional mechanisms contributing to CVD in patients with MAFLD may also include activation of the renin-angiotensin system (RAAS), intestinal dysbiosis and presence of certain genetic polymorphisms. RAAS activation is implicated in the pathophysiology of both MAFLD and CVD [76]. RAAS activation in metabolically active tissues can exert pro-inflammatory effects, mainly via angiotensin II, and is associated with multiple dysfunctional cellular processes, leading to hepatic necro-inflammation and fibrosis [76–78]. In a retrospective, territory-wide cohort study of 12,327 patients with NAFLD, the authors found that treatment with RAAS inhibitors was associated with a lower risk of liver-related events, liver cancer and cirrhotic complications, though the indication for use of RAAS inhibitors was for vascular and not liver disease [79]. Given the current evidence, it could be speculated that RAAS inhibitors may exert some beneficial effects on hepatic fibrosis and its related complications in MAFLD, but larger prospectively designed intervention studies are needed to provide high quality data on this topic [80].
Consensus statement 3.3: Some shared genetic polymorphisms (e.g., PNPLA3 I148M, and TM6SF2 E167K) may affect the risk of both MAFLD and CVD (Grade A).
Some shared genetic polymorphisms associated with MAFLD may contribute to CVD development [81]. Patatin-like phospholipase domain-containing protein 3 (PNPLA3) and trans-membrane 6 superfamily 2 (TM6SF2) are two susceptibility genes for MAFLD that have been shown to be associated with all histologic stages of MAFLD. [82, 83] Interestingly, both of these genes have shown opposite effects on the risk of MAFLD and CVD. Some studies reported that PNPLA3 and TM6SF2 genetic variants are associated with higher risk of fatty liver and steatohepatitis, but with a lower risk of CVD [84, 85]. The current concept is that genetic variants in PNPLA3 and TM6SF2 can regulate the production of VLDL particles by reducing hydrolytic activity and the breakdown of triglycerides in the liver, thereby resulting in intra-hepatic triglyceride accumulation, but reducing circulating levels of VLDL, and by extension, plasma triglycerides and LDL-cholesterol levels, thereby preventing CVD [84, 86]. Some studies showed that carriers of the p.I148M variant in PNPLA3 and p.E167K in TM6SF2 have a lower incidence of CVD [84]. Future prospective studies are required to better understand whether the knowledge on these genetic risk factors can be also translated into CVD risk reduction [87].
Consensus statement 3.4: Gut microbiota may play a role in both MAFLD and CVD (Grade A).
MAFLD may also contribute to CVD development because this liver disease is associated with dysregulated gut microbiota, leading to intestinal bacterial dysfunction and altered microbial-derived metabolites [88–92]. However, it is also likely that dietary factors are the primary cause of dysregulated gut microbiota in MAFLD. A meta-analysis reported abnormalities in gut microbiota composition in patients with MAFLD compared to healthy controls [93]. Studies have also shown that specific intestinal microbiome signatures in MAFLD, liver fibrosis, and cirrhosis could be used as non-invasive diagnostic biomarkers for liver disease diagnosis [94]. Intestinal bacterial dysfunction and metabolic product alterations may contribute to the production of pathogen-associated molecular patterns, increased mucosal barrier permeability and impaired mucosal barrier permeability that lead to increased systemic low-grade inflammation, insulin resistance and obesity, thus promoting MAFLD progression and CVD development [92, 95]. Gut microbiota independent of MAFLD can also influence the development and progression of CVD [96].
MAFLD and primary prevention of CVD
Consensus statements 4.1–4.3 (Grade A in 4.2 and 4.3; Grade B in 4.1) (Table 2).
Consensus statement 4.1: Carotid ultrasonography should be considered in most patients with MAFLD to improve CVD risk assessment (Grade B).
Current guidelines highlight the importance of CVD risk assessment in MAFLD [97, 98]. However, two key questions still remain: 1) which patients with MAFLD should be screened for CVD, and 2) what screening tests should be used for CVD risk assessment. The advantages of screening and thus prevention of a disease depend on baseline risk. As discussed above, MAFLD is associated with several markers of subclinical atherosclerosis (for example, increased carotid IMT, CAC, and atherosclerotic carotid plaques) which are associated with a higher risk of developing major CVD events [20]. Thus, since patients with MAFLD are at higher risk for CVD morbidity and mortality, monitoring subclinical atherosclerosis markers may be of benefit for CVD risk prediction and reduction [99]. Markers of subclinical atherosclerosis should be considered in high-risk individuals, such as computed tomography scanning to assess CAC, or carotid IMT and carotid atherosclerotic plaques. Assessment of carotid artery ultrasound is a widely used, reliable and cost-effective screening tool that can be routinely employed in the clinic with incremental prognostic value over traditional CVD risk factors in patients with MAFLD, who are typically asymptomatic [100]. A recent meta-analysis suggested that the pooled prevalence of subclinical and clinical CVD in NAFLD was 38.7% and 55.4%, respectively. [20]
To date, there are insufficient prospective data to support routine use of carotid artery ultrasound for CVD screening in patients with MAFLD. Also, it is uncertain whether carotid IMT measurement may improve CVD risk stratification over current risk stratification scores such as FRS [101]. In our two-round Delphi survey, 16% of experts somewhat disagreed or disagreed with this statement in the R2 survey. Thus, we need to consider that assessment of carotid artery ultrasound may pose medical resource challenges in some areas (such as over-referral, increased resource use, costs and over-medication). Future studies should specifically evaluate the cost-effectiveness and feasibility of routine carotid ultrasound performance as part of the MAFLD workup.
Consensus statement 4.2: In CVD risk assessment, MAFLD may be considered a CVD risk factor (Grade A).
Since MAFLD may (independently) increase the risk of CVD it could contribute to CVD prediction risk scores, such as FRS or other scores. However, it remains uncertain if the current CVD risk scores could be improved by adding MAFLD. In a setting of clinical suspicion of CVD, MAFLD might be considered as a potential risk-enhancing factor. For example, a multicenter retrospective cohort study of 10,453 individuals by Wu et al. [102] reported that the combination of steatosis imaging information and non-invasive serum fibrosis biomarkers (e.g. FIB-4, NFS) with lipid and apolipoprotein profiles improved the prognostic value of CVD risk scores in patients with MAFLD. In this retrospective cohort study, FRS alone did not provide the best prediction of CVD, particularly when differentiating the risk of CVD with mild steatosis from that without MAFLD. FRS could predict people at low risk, but its predictive performance decreased for people at high risk of severe MAFLD. However, individuals with FRS < 10% and mild steatosis had a cumulative risk of double to almost triple compared to that predicted by FRS [102]. Therefore, current CVD risk scores may underestimate the true CVD risk in patients with advanced MAFLD. Further research is needed to examine the extent to which MAFLD may confer an additional CVD risk compared to traditional cardiovascular risk factors.
Consensus statement 4.3: Screening for MAFLD should be considered in most patients with CVD (Grade A).
Currently, with a lack of uniform MAFLD screening guidelines, screening for MAFLD is not routinely undertaken in patients with CVD [103]. As for screening for MAFLD in patients with CVD, this depends on the most appropriate diagnostic test to evaluate patients with non-invasive versus invasive techniques. Non-invasive tests have lower accuracy while invasive tests although they are more accurate, are associated with higher risks of complications and costs. In clinical practice, most primary care clinicians begin screening for liver disease based on increased levels of serum transaminase liver enzymes. However, most patients diagnosed with MAFLD have normal serum liver enzyme levels and early MAFLD might be missed due to the low sensitivity of this test. Thus, we also need to consider whether screening for MAFLD poses medical resource challenges in some regions. The costs involved in undertaking abdominal ultrasound or other imaging modalities, may not be cost-effective without approved pharmacological therapies. Early screening using non-invasive tests in patients with CVD can be considered for evaluating of hepatic fibrosis when multiple CVD risk factors are present, particularly in the context of T2DM [104]. The independent role of MAFLD-related fibrosis in CVD provides an additional option for CVD primary prevention and may facilitate engagement with advised treatments and lifestyle change. This would enable early detection of advanced liver fibrosis, referral to a liver specialist, and CVD risk assessment [40, 105].
Managing MAFLD and the risk of CVD
Consensus statements 5.1–5.8 (Grade U in 5.1, 5.2, 5.4, 5.5 and 5.8; Grade A in 5.3, 5.6 and 5.7) (Table 2).
Consensus statement 5.1: Clinicians who manage patients with MAFLD should target cardiometabolic risk factors (overweight/obesity, diabetes, dyslipidemia and hypertension) (Grade U).
Consensus statement 5.2: Lifestyle intervention (including a healthy dietary pattern, weight loss and regular physical exercise) is associated with improvement in both MAFLD and CVD (Grade U).
Clinicians managing MAFLD patients should target cardiometabolic risk factors and take into account the recommended behavioral and pharmacotherapy approaches that may have potential benefits (Table 3). MAFLD is a therapeutic area for which many clinical trials are underway; these are summarized in recent reviews [106, 107]. Lifestyle intervention (including a healthy dietary pattern, weight loss and regular physical exercise) is associated with MAFLD improvement [108, 109]. Intensive lifestyle intervention plays an important role in the primary/secondary prevention of CVD and it is specifically mentioned in guidelines for management of MAFLD [110, 111]. A plant-based, Mediterranean type diet is the best cardioprotective approach, with benefits on insulin resistance and oxidative stress and it was also shown to be beneficial in small patient cohorts with MAFLD [112, 113]. Physical activity, independent of weight loss, could be a promising strategy to reduce the incidence of CVD and hepatic steatosis, mainly through positive modulation of insulin signaling [114]. However, weight loss is still strongly recommended in most patients as it has shown benefits on liver histology, systemic insulin resistance, and low-grade inflammation [97].
Table 3.
Recommended behavioral and pharmacotherapy approaches for patients with MAFLD and CVD
| Target population | CVD | Metabolic steatohepatitis (MeSH) | Liver fibrosis | |
|---|---|---|---|---|
| Healthy dietary pattern | Most | + + | + + | + + |
| Weight loss | Most | + + | + + | + + |
| Regular physical exercise | Most | + + | + + | + + |
| Alcohol avoidance | Most | + + | + + | + + |
| GLP-1RAs | T2DM | + + | + + a | + a |
| SGLT-2 inhibitors | T2DM | + + | + + a | ± a |
| Pioglitazone | T2DM | + + | + + a | + a |
| Statins | In the context of dyslipidaemia | + + | ± a | ± a |
| Bariatric surgery | Appropriately selected patients | + + | + + a | + + a |
CVD cardiovascular disease; GLP-1Ras glucagon-like peptide-1 receptor agonists; MAFLD metabolic (dysfunction) associated fatty liver disease; SGLT-2 sodium-glucose cotransporter-2; T2DM type 2 diabetes mellitus; “ + + ” = benefit; “ + ” = potential benefit; “ ± ” = limited data
aNo phase III clinical trials data in this population
Consensus statement 5.3: Alcohol avoidance of any type or amount is advisable in patients with MAFLD and CVD (Grade A).
Heavy alcohol consumption is a risk factor for both progressive MAFLD and CVD. There is debate regarding the effect of moderate drinking on MAFLD and CVD risk [115]. First, there is emerging evidence that even small alcohol amounts are harmful in MAFLD [116, 117]. Modest alcohol consumption has also been associated with decreased improvement in histologic steatosis and steatohepatitis [118]. A systematic review suggested that any level of alcohol consumption is associated with a doubling of incident liver disease outcomes in MAFLD, even when drinking within recommended limits [119]. The 2022 AHA scientific statement on NAFLD and CVD risk reported that alcohol avoidance is strongly encouraged. Second, it remains uncertain whether any benefit to CVD risk outweighs any harm to the liver [120]. Controversy has surrounded the association between alcohol intake and CVD, in part because alcohol use is difficult to measure and changes over time. Numerous studies have demonstrated an association between moderate alcohol use and lower CVD risk in the general population [121]. However, some or all of the apparent cardiac protective benefits of alcohol intake may be due to the product of residual confounding from favorable lifestyle, socio-economic, and behavioral factors that tend to coincide with modest alcohol intake [122, 123]. A cohort study of nearly 370,000 persons from the general population found that after adjustment for healthy lifestyle effects, the apparent cardiovascular benefits of light drinking were substantially reduced. This suggests that any amount of daily alcohol intake is associated with increased CVD risk [124]. A cohort study prospectively assessing the CVD risk of alcohol use in patients with MAFLD also suggested the same. In contrast to general population, alcohol use may not reduce the risk of CVD in patients with MAFLD [125].For example, moderate drinking might be associated with progression of hepatic fibrosis and little or no cardiovascular benefit [126]. Overall, there remains a need for additional high-quality prospective studies that evaluate both liver-related and CVD outcomes at different stages of fibrosis amongst MAFLD patients with moderate or lower amounts of alcohol intake, including the measurement of phosphatidylethanol (PEth). Currently, based on the synthesis of the most up to date longitudinal evidence, we believe that clinicians seeing patients with MAFLD should advise abstinence from alcohol.
Consensus statement 5.4: Treatment with GLP-1RAs is beneficial in MAFLD patients with coexisting T2DM and may reduce CVD outcomes (Grade U).
Glucose-lowering agents may be suitable for mitigating progression of histological features of MAFLD and preventing CVD events if their benefit is mainly derived through reductions in body weight in addition to improving long-term glycemic control [127]. Glucagon-like peptide-1 receptor agonists (GLP-1RAs) are a class of glucose-lowering agents approved for T2DM treatment (they improve glycemic control, induce weight loss, decrease cholesterol levels and liver fat content) which has gained the attention of guidelines as a therapeutic option for T2DM patients with MAFLD to improve CVD outcomes [2, 128]. GLP-1RAs have well-accepted efficacy on improving CVD outcomes [129]. Cardiovascular safety across all GLP-1RAs on CVD outcome trials has demonstrated that these drugs reduce major adverse CVD events, CVD mortality, and all-cause mortality risk with no significant safety concerns [130]. GLP-1RAs also improve some non-invasive markers of MAFLD and have proven effective for reductions in hepatic steatosis and inflammation scores [131, 132]. An updated meta-analysis of eleven phase-2 randomized clinical trials found that using GLP-1RAs to specifically treat MAFLD or nonalcoholic steatohepatitis for a median of 26 weeks was associated with a reduction in absolute percentage of liver fat content on magnetic resonance imaging, as well as greater histological resolution of steatohepatitis without worsening of liver fibrosis (pooled random-effects odds ratio 4.06, 95% CI 2.52–6.55; for liraglutide and semaglutide only) [133]. Global phase III clinical trials to test histological endpoints of steatohepatitis are ongoing. There is no indication yet to use this class as a treatment for steatohepatitis and associated liver fibrosis. Thus, further studies on histological benefits are needed to evaluate the potential for improving liver fibrosis in MAFLD.
Consensus statement 5.5: Treatment with SGLT-2 inhibitors is beneficial in MAFLD patients with coexisting T2DM and may reduce CVD outcomes (Grade U).
Sodium-glucose cotransporter-2 (SGLT-2) inhibitors are another class of glucose-lowering agents that have been approved for treatment of T2DM, reducing the renal capacity to reabsorb filtered glucose, increasing renal glycosuria and osmotic diuresis, thereby improving glucose control. These agents also lead to some weight loss and a lowering of blood pressure [134]. SGLT-2 inhibitors are approved for their favorable long-term effects on risk of major CVD events and currently widely used in T2DM patients at high risk of CVD [135–137]. SGLT2 inhibitors also show improvements in liver fat content and fibrosis markers among T2DM patients with MAFLD [138–140]. In a small biopsy-proven steatohepatitis trial with nine patients who had T2DM but no contemporaneous control subjects, empagliflozin showed improvements in the histological scores of steatosis, hepatocytes ballooning, and fibrosis [139]. However, reports from larger prospective studies are warranted. In this regard, a phase 3 trial of dapagliflozin (DEAN study) based on histological endpoints is now ongoing (NCT03723252). In sum, meta-analyses of recent studies have not reached consensus and the effects of SGLT2 inhibitors on liver fibrosis, especially beyond weight loss, remain to be confirmed [140].
Consensus statement 5.6: Treatment with pioglitazone is beneficial in MAFLD patients and may reduce CVD outcomes, but potential adverse effects (e.g. weight gain, edema and worsening of pre-existing congestive heart failure) should be kept in mind (Grade A).
Pioglitazone was proven to improve hepatic histology in steatohepatitis patients with and without T2DM and recommended for patients with T2DM and biopsy-proven steatohepatitis [141]. The benefits of pioglitazone on CVD outcomes in patients with and without T2DM are promising [142, 143]. The major limitation of pioglitazone in clinical practice as an off-label use for metabolic steatohepatitis is its adverse long-term effects, including moderate weight gain, risk of fracture, and fluid retention [144, 145]. The development of PXL065 (a novel, proprietary deuterium-stabilized r-stereoisomer of pioglitazone) for metabolic steatohepatitis represents a unique opportunity to enhance the therapeutic benefits of pioglitazone whilst reducing or eliminating PPARγ-related side effects [146]. Interestingly, PXL065 at a dose less than 22.5 mg/day for metabolic steatohepatitis is equal to or greater than 45-mg pioglitazone, but without any detrimental weight gain and oedema [146].
Consensus statement 5.7: Statins (if required for the treatment of dyslipidemia or CVD risk reduction) should be prescribed for patients with MAFLD even with modestly elevated serum liver enzyme levels (< 3 ULN) (Grade A).
All patients with MAFLD should be considered for statin treatment due to their increased CVD risk. Statins are the first-line to prevent CVD events in patients at risk for atherosclerotic CVD [147]. Statin treatment in MAFLD patients with mild-to-moderate abnormal serum liver enzymes is safe and may improve liver enzyme levels and reduce CVD morbidity and mortality [148]. Importantly, clinicians are commonly concerned about drug-induced liver injury, but statin use is not associated with abnormal serum liver enzyme levels in patients with hepatic steatosis [149–151]. Based on this, statins are thought to reduce the risk of CVD in MAFLD patients with dyslipidemia even without a beneficial effect on liver histology [110, 152].
Consensus statement 5.8: Bariatric surgery (if required in severely obese patients with MAFLD) improves liver histology features and reduces CVD risk (Grade U).
Lifestyle interventions require long-term adherence, though sustained weight loss is difficult to achieve in patients with long-standing obesity. It has been reported that only 50% of patients can reach 7% weight loss following a 1-year lifestyle intervention [153]. Bariatric surgery has been shown to achieve significant weight loss of 20% to 30% and improves liver histology including fibrosis [154, 155]. Bariatric surgery is also associated with significant reduction in CVD risk in individuals with morbid obesity and MAFLD with the risk of primary and secondary composite CVD outcomes reduced by 47% and 50%, respectively [156]. Hence, bariatric surgery should remain a consideration for selected patients, particularly those without evidence of portal hypertension, with a body mass index (BMI) > 35 kg/m2 (BMI > 30 kg/m2 in Asian people) and MAFLD or metabolic steatohepatitis. For morbidly obese patients with MAFLD, especially those who have not responded to lifestyle intervention, bariatric surgery is arguably an attractive and appropriate treatment option that offers promising liver-related outcomes. However, there are not enough data to support the use of bariatric surgery in all patients with MAFLD. Rather it could be an option for those needing it for obesity reduction and MAFLD; early cirrhosis without significant portal hypertension should not be a contraindication for bariatric surgery.
Strengths and limitations
Although the Delphi method is a robust consensus-building approach to assess the levels of agreement on specific issues and for exploring whether a consensus can be reached, it has strengths and limitations. As an important strength, our Delphi survey demonstrated increased consistency in each subsequent round, allowing us to determine whether the feedback improved statements, increased the degree of consensus, and helped reach an agreement. In the two rounds of surveys, the experts’ ability to include detailed comments on each draft statement and the integration of feedback into the new statement resulted in a growing level of agreement on the consensus statements, from 92.8% in the R1 survey to 95.7% in the R2 survey. The consistently increasing (mean) levels of agreement with the consensus statements together with the high levels of participation [80.0% (52/65) in the R1 survey and 100% (52/52) in the R2 survey] strengthen our confidence in the observed results. Another important strength of the present study is that the resultant consensus statements have been endorsed by representative scientists from 31 countries from six continents globally (involving Hepatologists, Cardiologists, Endocrinologists, Diabetologists and other specialists with extensive research and clinical expertise). This international and multi-disciplinary approach further testifies to its global relevance.
We incorporated the risk factors into the preliminary results of our review and translated them into the Delphi survey report. We received and included many open comments in all five data collection components. This feedback provides a mechanism for reconciling differing opinions. However, Delphi studies usually include face-to-face in-depth discussions and poll surveys. Given the wide geographic distribution of the panel members and COVID-19 travel restrictions, one limitation of this Delphi study is that we conducted the survey rounds online rather than in person. We acknowledge that combining in-person and written feedback might have resulted in more comprehensive contributions. This may have affected the consensus reached. Although there is an overlap between NAFLD and MAFLD populations, we are now beginning to acquire the relevant data about MAFLD and CVD to set a baseline for ongoing improvements in knowledge. Future research will also help in clarifying the most appropriate screening and management of patients currently defined as “lean NAFLD”, who do not meet criteria for MAFLD.
Conclusions
MAFLD and CVD are two highly prevalent global public health challenges. While the proposed change in nomenclature from NAFLD to MAFLD is new, the available evidence provides support for the recommendations of this Delphi-based consensus. The panel of experts has developed and endorsed a set of statements on the link between MAFLD and CVD risk that can provide a framework for developing appropriate guidelines and indicate directions for future research on MAFLD and its associated CVD risk.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors thank two Delphi study methodologists Prof. Joey S.W. Kwong (St. Luke's International University, Japan) and Prof. Zubing Mei (Shuguang Hospital, Shanghai University of Traditional Chinese Medicine, Shanghai, China) for methodological assistance. Seung Up Kim, Vincent Wai-Sun Wong, Mohammed Eslam, Yusuf Yilmaz, Wah Kheong Chan, Sombat Treeprasertsuk, Hasmik Ghazinyan, Jian-Gao Fan, George Boon-Bee Goh, Saeed Hamid, Jacob George and Ming-Hua Zheng are members of the APASL MAIDEN.
Author contributions
Design the study, Participate the Delphi study, Review the data and draft the statement, Review the full draft: X-DZ, GT, CDB. Participate the Delphi study: X-DZ, GT, CDB, MDS, SUK, CAAC, JC, VKS, MH, PGS, K-CS, AM, VW-SW, J-JL, J-GF, CB, YH, GVP, AS, YY, WKC, HH, NM-S, SAA, HC-P, GYHL, RJK, PO, MR-G, ST, GS, JWS, JDR, II, MF, DP, ML-P, HT, HG, JB, ME, MHN, GB-BG, MAM, SH, NP, JG, M-HZ. Review the data and draft the statement: X-DZ, GT, JG, M-HZ. Review the full draft: X-DZ, GT, CDB, MDS, SUK, C. AAC, JC, VKS, MH, PGS, Ki-Chul Sung, AM, VW-SW, J-JL, J-GF, CB, YH, GVP, AS, YY, WKC, HH, NM-S, SAA, HC-P, GYHL, RJK, PO, MR-G, ST, GS, JWS, JDR, II, MF, DP, ML-P, HT, HG, JB. ME, MHN, GB-BG, MAM, SH, NP, JG, M-HZ.
Funding
The authors have not disclosed any funding.
Data availability
All data included in this study are available upon request by contact with the corresponding author (zhengmh@wmu.edu.cn).
Declarations
Conflict of interest
George V Papatheodoridis: Advisor: Abbvie, Albireo, Amgen, Dicerna, Gilead, GlaxoSmithKline, Ipsen, Janssen, Novo Nordisk, Roche and Takeda; Lectures: Abbvie, Gilead, GlaxoSmithKline, Ipsen, Novo Nordisk, Sobi; Research grants: Abbvie, Gilead; Investigator in clinical trials: Abbvie, Astellas, Bayer, Eiger, Gilead, GlaxoSmithKline, Janssen, Merck Sharp & Dohme, Noorik, Novartis, Novo Nordisk, Regulus, Roche, Takeda. Giada Sebastiani: Speaker: Merck, Gilead, Abbvie, Novonordisk, Novartis and Pfizer; Advisory board member: Pfizer, Merck, Novonordisk, Gilead and Intercept; Unrestricted research funding: Theratecnologies Inc. Gregory Y. H. Lip: Consultant and speaker for BMS/Pfizer, Boehringer Ingelheim, Daiichi-Sankyo, Anthem. No fees are received personally. GYHL is co-principal investigator of the AFFIRMO project on multimorbidity in AF, which has received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement No 899871. Jian-Gao Fan: Speaker, a consultant and an advisory for Sanofi, Abbott, EchoSens, Novartis, Hisky, Gilead, Allergan, Terns and MADAUS GMBH. John D. Ryan: None related to MAFLD. Consulting: Bond Biosciences, Pfizer, Gilead; Lectures: Kyowa kirin, Falk. Marat Fudim: Dr Fudim was supported by Bayer. He receives consulting fees from Bayer, Merck, NovoNordisk. Michael D. Shapiro: Research Grants (paid to my institution): AHA, NIH, Amgen, Novartis, Ionis, Esperion; Consultant: Ionis, Novartis, Regeneron; Scientific Advisory Boards: Amgen, Novartis, Precision Bioscience. Mindie H. Nguyen: Last 36 months: Research support: Pfizer, Enanta, Astra Zeneca, Innogen, Exact Science, CurveBio, Delfi Biotech, Gilead, Exact Sciences, Vir Biotech, Helio Health, National Cancer Institute, Glycotest, B.K. Kee Foundation. Consulting and/or Advisory Board: Intercept, Exact Science, Gilead, GSK, Eli Lilly, Laboratory of Advanced Medicine, Exelixis Research grants. Ming-Hua Zheng: Lectures: Hisky Medical. Philippe Gabriel Steg: Research grants: Amarin, Bayer, Sanofi, and Servier; Clinical Trials (Steering committee, CEC, DSMB): Amarin, AstraZeneca, Bayer, Bristol-Myers Squibb, Idorsia, Novartis, PhaseBio, Pfizer, Sanofi, Servier; Consulting or speaking: Amarin, Amgen, BMS/Myokardia, Merck, Novo-Nordisk, Regeneron; Senior Associate Editor at Circulation. Seung Up Kim: He has served as an advisory committee member Gilead Sciences, Bayer, Eisai, and Novo Nordisk. He is a speaker for Gilead Sciences, GSK, Bayer, Eisai, Abbvie, EchoSens, MSD, Eisai, Otsuka, and Bristol-Myers Squibb. He has also received a research grant from Abbvie and Bristol-Myers Squibb. Vincent Wai-Sun Wong: Consultancy: AbbVie, Boehringer Ingelheim, Echosens, Gilead Sciences, Intercept, Inventiva, Novo Nordisk, Pfizer, Sagimet Biosciences, TARGET PharmaSolutions; Lectures: Abbott, AbbVie, Gilead Sciences, Novo Nordisk; Research grants: Gilead Sciences; Stock: Co-founder of Illuminatio Medical Technology Limited. Wah Kheong Chan: Consultant or advisory board member for Roche, Abbvie, Boehringer Ingelheim and Novo Nordisk; speaker for Viatris and Hisky Medical. Yusuf Yilmaz: He has served as consultant to Cymabay, Zydus, Novo Nordisk, and Echosens. The other authors have no conflicts of interest to declare.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xiao-Dong Zhou, Giovanni Targher and Christopher D. Byrne are co-first authors.
Contributor Information
Jacob George, Email: jacob.george@sydney.edu.au.
Ming-Hua Zheng, Email: zhengmh@wmu.edu.cn.
References
- 1.Younossi Z, et al. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology (Baltimore, MD) 2016;64:73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 2.Chalasani N, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology (Baltimore, MD) 2018;67:328–357. doi: 10.1002/hep.29367. [DOI] [PubMed] [Google Scholar]
- 3.Eslam M, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol. 2020;73:202–209. doi: 10.1016/j.jhep.2020.03.039. [DOI] [PubMed] [Google Scholar]
- 4.Zhang XL, Fan JG, Wei L, Shi JP, Zheng MH. Promoting the term MAFLD: China in action. Lancet Gastroenterol Hepatol. 2022;7:598. doi: 10.1016/S2468-1253(22)00127-3. [DOI] [PubMed] [Google Scholar]
- 5.Eslam M, Sanyal AJ, George J. MAFLD: a consensus-driven proposed nomenclature for metabolic associated fatty liver disease. Gastroenterology. 2020;158:1999–2014.e1. doi: 10.1053/j.gastro.2019.11.312. [DOI] [PubMed] [Google Scholar]
- 6.Zheng KI, et al. From NAFLD to MAFLD: a "redefining" moment for fatty liver disease. Chin Med J. 2020;133:2271–2273. doi: 10.1097/CM9.0000000000000981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fouad Y, et al. The NAFLD-MAFLD debate: eminence vs evidence. Liver Int. 2021;41:255–260. doi: 10.1111/liv.14739. [DOI] [PubMed] [Google Scholar]
- 8.Wang TY, George J, Zheng MH. Metabolic (dysfunction) associated fatty liver disease: more evidence and a bright future. Hepatobiliary Surg Nutr. 2021;10:849–852. doi: 10.21037/hbsn-21-352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tilg H, Effenberger M. From NAFLD to MAFLD: when pathophysiology succeeds. Nat Rev Gastroenterol Hepatol. 2020;17:387–388. doi: 10.1038/s41575-020-0316-6. [DOI] [PubMed] [Google Scholar]
- 10.Zhou XD, et al. Metabolic dysfunction-associated fatty liver disease and implications for cardiovascular risk and disease prevention. Cardiovasc Diabetol. 2022;21:270. doi: 10.1186/s12933-022-01697-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chan W, Wong V. Meaning of non-overlapping patients between the MAFLD and NAFLD definitions. Liver Int. 2022;42:271–273. doi: 10.1111/liv.15142. [DOI] [PubMed] [Google Scholar]
- 12.Wong VW, et al. Impact of the new definition of metabolic associated fatty liver disease on the epidemiology of the disease. Clin Gastroenterol Hepatol. 2021;19:2161–2171.e5. doi: 10.1016/j.cgh.2020.10.046. [DOI] [PubMed] [Google Scholar]
- 13.Sun DQ, et al. MAFLD and risk of CKD. Metabolism. 2021;115:154433. doi: 10.1016/j.metabol.2020.154433. [DOI] [PubMed] [Google Scholar]
- 14.Zheng KI, Sun DQ, Jin Y, Zhu PW, Zheng MH. Clinical utility of the MAFLD definition. J Hepatol. 2021;74:989–991. doi: 10.1016/j.jhep.2020.12.016. [DOI] [PubMed] [Google Scholar]
- 15.Das M. WHO urges immediate action to tackle non-communicable diseases. Lancet Oncol. 2022;23:1361. doi: 10.1016/S1470-2045(22)00606-4. [DOI] [PubMed] [Google Scholar]
- 16.Lazarus J, et al. Advancing the global public health agenda for NAFLD: a consensus statement. Nat Rev Gastroenterol Hepatol. 2022;19:60–78. doi: 10.1038/s41575-021-00523-4. [DOI] [PubMed] [Google Scholar]
- 17.Rubino F, et al. Joint international consensus statement for ending stigma of obesity. Nat Med. 2020;26:485–497. doi: 10.1038/s41591-020-0803-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Targher G, Day CP, Bonora E. Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N Engl J Med. 2010;363:1341–1350. doi: 10.1056/NEJMra0912063. [DOI] [PubMed] [Google Scholar]
- 19.Targher G, Byrne C, Tilg H. NAFLD and increased risk of cardiovascular disease: clinical associations, pathophysiological mechanisms and pharmacological implications. Gut. 2020;69:1691–1705. doi: 10.1136/gutjnl-2020-320622. [DOI] [PubMed] [Google Scholar]
- 20.Toh J, et al. A meta-analysis on the global prevalence, risk factors and screening of coronary heart disease in nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2022;20:2462–2473.e10. doi: 10.1016/j.cgh.2021.09.021. [DOI] [PubMed] [Google Scholar]
- 21.Wu S, et al. Association of non-alcoholic fatty liver disease with major adverse cardiovascular events: a systematic review and meta-analysis. Sci Rep. 2016;6:33386. doi: 10.1038/srep33386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Targher G, Tilg H, Byrne CD. Non-alcoholic fatty liver disease: a multisystem disease requiring a multidisciplinary and holistic approach. Lancet Gastroenterol Hepatol. 2021;6:578–588. doi: 10.1016/S2468-1253(21)00020-0. [DOI] [PubMed] [Google Scholar]
- 23.Mantovani A, et al. Non-alcoholic fatty liver disease and risk of fatal and non-fatal cardiovascular events: an updated systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2021;6:903–913. doi: 10.1016/S2468-1253(21)00308-3. [DOI] [PubMed] [Google Scholar]
- 24.Zhou Y, et al. Nonalcoholic fatty liver disease contributes to subclinical atherosclerosis: a systematic review and meta-analysis. Hepatol Commun. 2018;2:376–392. doi: 10.1002/hep4.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim H, et al. MAFLD predicts the risk of cardiovascular disease better than NAFLD in asymptomatic subjects with health check-ups. Dig Dis Sci. 2022;67:4919. doi: 10.1007/s10620-022-07508-6. [DOI] [PubMed] [Google Scholar]
- 26.Huang Q, Zou X, Wen X, Zhou X, Ji L. NAFLD or MAFLD: which has closer association with all-cause and cause-specific mortality? Results from NHANES III. Front Med. 2021;8:693507. doi: 10.3389/fmed.2021.693507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tsutsumi T, et al. MAFLD better predicts the progression of atherosclerotic cardiovascular risk than NAFLD: Generalized estimating equation approach. Hepatol Res. 2021;51:1115–1128. doi: 10.1111/hepr.13685. [DOI] [PubMed] [Google Scholar]
- 28.Wang Y, et al. Cardiovascular and renal burdens among patients with MAFLD and NAFLD in China. Front Endocrinol (Lausanne) 2022;13:968766. doi: 10.3389/fendo.2022.968766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yoneda M, et al. Risk of cardiovascular disease in patients with fatty liver disease as defined from the metabolic dysfunction associated fatty liver disease or nonalcoholic fatty liver disease point of view: a retrospective nationwide claims database study in Japan. J Gastroenterol. 2021;56:1022–1032. doi: 10.1007/s00535-021-01828-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee H, Lee YH, Kim SU, Kim HC. Metabolic dysfunction-associated fatty liver disease and incident cardiovascular disease risk: a nationwide cohort study. Clin Gastroenterol Hepatol. 2021;19:2138–2147.e10. doi: 10.1016/j.cgh.2020.12.022. [DOI] [PubMed] [Google Scholar]
- 31.Liang Y, et al. Association of MAFLD With diabetes, chronic kidney disease, and cardiovascular disease: a 4.6-year cohort study in China. J Clin Endocrinol Metab. 2022;107:88–97. doi: 10.1210/clinem/dgab641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wen W, et al. Metabolic dysfunction-associated fatty liver disease and cardiovascular disease: a meta-analysis. Front Endocrinol (Lausanne) 2022;13:934225. doi: 10.3389/fendo.2022.934225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Targher G, Byrne CD, Lonardo A, Zoppini G, Barbui C. Non-alcoholic fatty liver disease and risk of incident cardiovascular disease: a meta-analysis. J Hepatol. 2016;65:589–600. doi: 10.1016/j.jhep.2016.05.013. [DOI] [PubMed] [Google Scholar]
- 34.Liu Y, Zhong GC, Tan HY, Hao FB, Hu JJ. Nonalcoholic fatty liver disease and mortality from all causes, cardiovascular disease, and cancer: a meta-analysis. Sci Rep. 2019;9:11124. doi: 10.1038/s41598-019-47687-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim D, et al. Metabolic dysfunction-associated fatty liver disease is associated with increased all-cause mortality in the United States. J Hepatol. 2021;75:1284–1291. doi: 10.1016/j.jhep.2021.07.035. [DOI] [PubMed] [Google Scholar]
- 36.Niriella M, et al. Outcomes of NAFLD and MAFLD: results from a community-based, prospective cohort study. PLoS ONE. 2021;16:e0245762. doi: 10.1371/journal.pone.0245762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mantovani A, Csermely A, Tilg H, Byrne C, Targher G. Comparative effects of non-alcoholic fatty liver disease and metabolic dysfunction-associated fatty liver disease on risk of incident cardiovascular events: a meta-analysis of about 13 million individuals. Gut. 2022 doi: 10.1136/gutjnl-2022-328224. [DOI] [PubMed] [Google Scholar]
- 38.Zhang H, Wang Y, Chen C, Lu Y, Wang N. Cardiovascular and renal burdens of metabolic associated fatty liver disease from serial US national surveys, 1999–2016. Chin Med J. 2021;134:1593–1601. doi: 10.1097/CM9.0000000000001513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nishimura K, et al. Predicting coronary heart disease using risk factor categories for a japanese urban population, and comparison with the Framingham risk score: the suita study. J Atheroscler Thromb. 2016;23:1138–1139. doi: 10.5551/jat.Er19356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Angelico F, Baratta F, Pastori D, Ben MD. Assessment of hepatic fibrosis in MAFLD: A new player in the evaluation of residual cardiovascular risk? Dig Liver Dis. 2021;53:383–384. doi: 10.1016/j.dld.2020.12.123. [DOI] [PubMed] [Google Scholar]
- 41.Schonmann Y, Yeshua H, Bentov I, Zelber-Sagi S. Liver fibrosis marker is an independent predictor of cardiovascular morbidity and mortality in the general population. Dig Liver Dis. 2021;53:79–85. doi: 10.1016/j.dld.2020.10.014. [DOI] [PubMed] [Google Scholar]
- 42.Baratta F, et al. Nonalcoholic fatty liver disease and fibrosis associated with increased risk of cardiovascular events in a prospective study. Clin Gastroenterol Hepatol. 2020;18:2324–2331.e4. doi: 10.1016/j.cgh.2019.12.026. [DOI] [PubMed] [Google Scholar]
- 43.Tamaki N, et al. Liver fibrosis and fatty liver as independent risk factors for cardiovascular disease. J Gastroenterol Hepatol. 2021;36:2960–2966. doi: 10.1111/jgh.15589. [DOI] [PubMed] [Google Scholar]
- 44.Han E, et al. Fibrotic burden determines cardiovascular risk among subjects with metabolic dysfunction-associated fatty liver disease. Gut Liver. 2022;16:786–797. doi: 10.5009/gnl210290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ferro D, et al. New insights into the pathogenesis of non-alcoholic fatty liver disease: gut-derived lipopolysaccharides and oxidative stress. Nutrients. 2020;12:2762. doi: 10.3390/nu12092762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Daniels SJ, et al. ADAPT: an algorithm incorporating PRO-C3 accurately identifies patients with NAFLD and advanced fibrosis. Hepatology. 2019;69:1075–1086. doi: 10.1002/hep.30163. [DOI] [PubMed] [Google Scholar]
- 47.Parkes J, et al. Enhanced liver fibrosis test can predict clinical outcomes in patients with chronic liver disease. Gut. 2010;59:1245–1251. doi: 10.1136/gut.2009.203166. [DOI] [PubMed] [Google Scholar]
- 48.Meyersohn NM, et al. Association of hepatic steatosis with major adverse cardiovascular events, independent of coronary artery disease. Clin Gastroenterol Hepatol. 2021;19:1480–1488.e14. doi: 10.1016/j.cgh.2020.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kunutsor SK, Bakker SJL, Blokzijl H, Dullaart RPF. Associations of the fatty liver and hepatic steatosis indices with risk of cardiovascular disease: interrelationship with age. Clin Chim Acta. 2017;466:54–60. doi: 10.1016/j.cca.2017.01.008. [DOI] [PubMed] [Google Scholar]
- 50.Zou B, Yeo Y, Cheung R, Ingelsson E, Nguyen M. Fatty liver index and development of cardiovascular disease: findings from the UK biobank. Dig Dis Sci. 2021;66:2092–2100. doi: 10.1007/s10620-021-06954-y. [DOI] [PubMed] [Google Scholar]
- 51.Park J, et al. The associations of hepatic steatosis and fibrosis using fatty liver index and BARD score with cardiovascular outcomes and mortality in patients with new-onset type 2 diabetes: a nationwide cohort study. Cardiovasc Diabetol. 2022;21:53. doi: 10.1186/s12933-022-01483-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Moon JH, Kim W. Metabolic dysfunction-associated fatty liver disease predicts long-term mortality and cardiovascular disease. Gut Liver. 2022;16:433–442. doi: 10.5009/gnl210167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tang ASP, et al. Non-alcoholic fatty liver disease increases risk of carotid atherosclerosis and ischemic stroke: an updated meta-analysis with 135,602 individuals. Clin Mol Hepatol. 2022;28:483–496. doi: 10.3350/cmh.2021.0406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bessho R, et al. A significant risk of metabolic dysfunction-associated fatty liver disease plus diabetes on subclinical atherosclerosis. PLoS ONE. 2022;17:e0269265. doi: 10.1371/journal.pone.0269265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wang J, et al. New definition of metabolic dysfunction-associated fatty liver disease with elevated brachial-ankle pulse wave velocity and albuminuria: a prospective cohort study. Front Med. 2022;16:714–722. doi: 10.1007/s11684-021-0888-8. [DOI] [PubMed] [Google Scholar]
- 56.Liu S, et al. The progression and regression of metabolic dysfunction-associated fatty liver disease are associated with the development of subclinical atherosclerosis: a prospective analysis. Metabolism. 2021;120:154779. doi: 10.1016/j.metabol.2021.154779. [DOI] [PubMed] [Google Scholar]
- 57.Sung K, et al. Comparative associations of nonalcoholic fatty liver disease and metabolic dysfunction-associated fatty liver disease with coronary artery calcification: a cross-sectional and longitudinal cohort study. Arterioscler Thromb Vasc Biol. 2023;43:482. doi: 10.1161/ATVBAHA.122.318661. [DOI] [PubMed] [Google Scholar]
- 58.Liu H, et al. Metabolic-associated fatty liver disease and major adverse cardiac events in patients with chronic coronary syndrome: a matched case-control study. Hep Int. 2021;15:1337–1346. doi: 10.1007/s12072-021-10252-0. [DOI] [PubMed] [Google Scholar]
- 59.Noda T, et al. The prevalence of metabolic dysfunction-associated fatty liver disease and its association with physical function and prognosis in patients with acute coronary syndrome. J Clin Med. 2022;11:1847. doi: 10.3390/jcm11071847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Nguyen VH, Le MH, Cheung RC, Nguyen MH. Differential clinical characteristics and mortality outcomes in persons with NAFLD and/or MAFLD. Clin Gastroenterol Hepatol. 2021;19:2172–2181.e6. doi: 10.1016/j.cgh.2021.05.029. [DOI] [PubMed] [Google Scholar]
- 61.Gong H, Liu X, Cheng F. Relationship between non-alcoholic fatty liver disease and cardiac arrhythmia: a systematic review and meta-analysis. J Int Med Res. 2021;49:3000605211047074. doi: 10.1177/03000605211047074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lei F, et al. The prevalence of MAFLD and its association with atrial fibrillation in a nationwide health check-up population in China. Front Endocrinol (Lausanne) 2022;13:1007171. doi: 10.3389/fendo.2022.1007171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Decoin R, et al. High liver fibrosis scores in metabolic dysfunction-associated fatty liver disease patients are associated with adverse atrial remodeling and atrial fibrillation recurrence following catheter ablation. Front Endocrinol (Lausanne) 2022;13:957245. doi: 10.3389/fendo.2022.957245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Borges-Canha M, et al. Association between nonalcoholic fatty liver disease and cardiac function and structure-a meta-analysis. Endocrine. 2019;66:467–476. doi: 10.1007/s12020-019-02070-0. [DOI] [PubMed] [Google Scholar]
- 65.Yong J, et al. Non-alcoholic fatty liver disease association with structural heart, systolic and diastolic dysfunction: a meta-analysis. Hep Int. 2022;16:269–281. doi: 10.1007/s12072-022-10319-6. [DOI] [PubMed] [Google Scholar]
- 66.Peng D, et al. Association of metabolic dysfunction-associated fatty liver disease with left ventricular diastolic function and cardiac morphology. Front Endocrinol (Lausanne) 2022;13:935390. doi: 10.3389/fendo.2022.935390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Anstee Q, Mantovani A, Tilg H, Targher G. Risk of cardiomyopathy and cardiac arrhythmias in patients with nonalcoholic fatty liver disease. Nat Rev Gastroenterol Hepatol. 2018;15:425–439. doi: 10.1038/s41575-018-0010-0. [DOI] [PubMed] [Google Scholar]
- 68.Mantovani A, et al. Risk of heart failure in patients with nonalcoholic fatty liver disease: JACC review topic of the week. J Am Coll Cardiol. 2022;79:180–191. doi: 10.1016/j.jacc.2021.11.007. [DOI] [PubMed] [Google Scholar]
- 69.Stahl EP, et al. Nonalcoholic fatty liver disease and the heart: JACC state-of-the-art review. J Am Coll Cardiol. 2019;73:948–963. doi: 10.1016/j.jacc.2018.11.050. [DOI] [PubMed] [Google Scholar]
- 70.Niederseer D, Wernly B, Aigner E, Stickel F, Datz C. NAFLD and cardiovascular diseases: epidemiological, mechanistic and therapeutic considerations. J Clin Med. 2021;10:467. doi: 10.3390/jcm10030467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Siddiqui M, et al. Severity of nonalcoholic fatty liver disease and progression to cirrhosis are associated with atherogenic lipoprotein profile. Clin Gastroenterol Hepatol. 2015;13:1000–8.e3. doi: 10.1016/j.cgh.2014.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cusi K. Role of obesity and lipotoxicity in the development of nonalcoholic steatohepatitis: pathophysiology and clinical implications. Gastroenterology. 2012;142:711–725.e6. doi: 10.1053/j.gastro.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 73.Austin MA, King MC, Vranizan KM, Krauss RM. Atherogenic lipoprotein phenotype. A proposed genetic marker for coronary heart disease risk. Circulation. 1990;82:495–506. doi: 10.1161/01.CIR.82.2.495. [DOI] [PubMed] [Google Scholar]
- 74.Gutiérrez-Cuevas J, Santos A, Armendariz-Borunda J. Pathophysiological molecular mechanisms of obesity: a link between MAFLD and NASH with cardiovascular diseases. Int J Mol Sci. 2021;22:11629. doi: 10.3390/ijms222111629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ormazabal V, et al. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc Diabetol. 2018;17:122. doi: 10.1186/s12933-018-0762-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Goh G, et al. Renin-angiotensin system and fibrosis in non-alcoholic fatty liver disease. Liver Int. 2015;35:979–985. doi: 10.1111/liv.12611. [DOI] [PubMed] [Google Scholar]
- 77.Paschos P, Tziomalos K. Nonalcoholic fatty liver disease and the renin-angiotensin system: implications for treatment. World J Hepatol. 2012;4:327–331. doi: 10.4254/wjh.v4.i12.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Attia H, et al. Chrysin attenuates fructose-induced nonalcoholic fatty liver in rats via antioxidant and anti-inflammatory effects: the role of angiotensin-converting enzyme 2/angiotensin (1–7)/mas receptor axis. Oxid Med Cell Longev. 2022;2022:9479456. doi: 10.1155/2022/9479456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zhang X, et al. Angiotensin-converting enzyme inhibitors prevent liver-related events in nonalcoholic fatty liver disease. Hepatology (Baltimore, MD) 2022;76:469–482. doi: 10.1002/hep.32294. [DOI] [PubMed] [Google Scholar]
- 80.Mantovani A, Dalbeni A. Treatments for NAFLD: state of art. Int J Mol Sci. 2021;22:2350. doi: 10.3390/ijms22052350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Chew NWS, et al. The genetic interactions between non-alcoholic fatty liver disease and cardiovascular diseases. Front Genet. 2022;13:971484. doi: 10.3389/fgene.2022.971484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Anstee QM, Day CP. The genetics of nonalcoholic fatty liver disease: spotlight on PNPLA3 and TM6SF2. Semin Liver Dis. 2015;35:270–290. doi: 10.1055/s-0035-1562947. [DOI] [PubMed] [Google Scholar]
- 83.Sookoian S, Pirola CJ. Meta-analysis of the influence of I148M variant of patatin-like phospholipase domain containing 3 gene (PNPLA3) on the susceptibility and histological severity of nonalcoholic fatty liver disease. Hepatology. 2011;53:1883–1894. doi: 10.1002/hep.24283. [DOI] [PubMed] [Google Scholar]
- 84.Simons N, et al. PNPLA3, TM6SF2, and MBOAT7 genotypes and coronary artery disease. Gastroenterology. 2017;152:912–913. doi: 10.1053/j.gastro.2016.12.020. [DOI] [PubMed] [Google Scholar]
- 85.Rüschenbaum S, et al. Patatin-like phospholipase domain containing 3 variants differentially impact metabolic traits in individuals at high risk for cardiovascular events. Hepatol Commun. 2018;2:798–806. doi: 10.1002/hep4.1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Liu D, et al. Exome-wide association study of plasma lipids in >300,000 individuals. Nat Genet. 2017;49:1758–1766. doi: 10.1038/ng.3977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kessler T, Schunkert H. Coronary artery disease genetics enlightened by genome-wide association studies. JACC Basic Transl Sci. 2021;6:610–623. doi: 10.1016/j.jacbts.2021.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cai J, et al. Nonalcoholic fatty liver disease pandemic fuels the upsurge in cardiovascular diseases. Circ Res. 2020;126:679–704. doi: 10.1161/CIRCRESAHA.119.316337. [DOI] [PubMed] [Google Scholar]
- 89.Drożdż K, et al. Metabolic-associated fatty liver disease (MAFLD), diabetes, and cardiovascular disease: associations with fructose metabolism and gut microbiota. Nutrients. 2021;14:103. doi: 10.3390/nu14010103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Tang WHW, Bäckhed F, Landmesser U, Hazen SL. Intestinal microbiota in cardiovascular health and disease: JACC state-of-the-art review. J Am Coll Cardiol. 2019;73:2089–2105. doi: 10.1016/j.jacc.2019.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Reinhardt C. The gut microbiota as an influencing factor of arterial thrombosis. Hamostaseologie. 2019;39:173–179. doi: 10.1055/s-0038-1675357. [DOI] [PubMed] [Google Scholar]
- 92.Albillos A, de Gottardi A, Rescigno M. The gut-liver axis in liver disease: Pathophysiological basis for therapy. J Hepatol. 2020;72:558–577. doi: 10.1016/j.jhep.2019.10.003. [DOI] [PubMed] [Google Scholar]
- 93.Li F, Ye J, Shao C, Zhong B. Compositional alterations of gut microbiota in nonalcoholic fatty liver disease patients: a systematic review and meta-analysis. Lipids Health Dis. 2021;20:22. doi: 10.1186/s12944-021-01440-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Aron-Wisnewsky J, et al. Gut microbiota and human NAFLD: disentangling microbial signatures from metabolic disorders. Nat Rev Gastroenterol Hepatol. 2020;17:279–297. doi: 10.1038/s41575-020-0269-9. [DOI] [PubMed] [Google Scholar]
- 95.Hu H, et al. Intestinal microbiome and NAFLD: molecular insights and therapeutic perspectives. J Gastroenterol. 2020;55:142–158. doi: 10.1007/s00535-019-01649-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Witkowski M, Weeks TL, Hazen SL. Gut microbiota and cardiovascular disease. Circ Res. 2020;127:553–570. doi: 10.1161/CIRCRESAHA.120.316242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.European Association for the Study of the Liver (EASL); European Association for the Study of Diabetes (EASD); European Association for the Study of Obesity (EASO). Clinical practice guidelines for the management of non-alcoholic fatty liver disease. J Hepatol 2016;64:1388–402 [DOI] [PubMed]
- 98.Choudhary NS, Duseja A. Screening of cardiovascular disease in nonalcoholic fatty liver disease: whom and how? J Clin Exp Hepatol. 2019;9:506–514. doi: 10.1016/j.jceh.2019.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hassen G, et al. Nonalcoholic fatty liver disease: an emerging modern-day risk factor for cardiovascular disease. Cureus. 2022;14:e25495. doi: 10.7759/cureus.25495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Zaidi NR, Gilani SA, Mehboob R, Waseem H, Hassan A. Diagnostic accuracy of carotid intima media thickness by B-mode ultrasonography in coronary artery disease patients. Arch Med Sci Atheroscler Dis. 2020;5:e79–e84. doi: 10.5114/amsad.2020.95651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.den Ruijter HM, et al. Common carotid intima-media thickness does not add to Framingham risk score in individuals with diabetes mellitus: the USE-IMT initiative. Diabetologia. 2013;56:1494–1502. doi: 10.1007/s00125-013-2898-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Wu T, et al. Apolipoproteins and liver parameters optimize cardiovascular disease risk-stratification in nonalcoholic fatty liver disease. Dig Liver Dis. 2021;53:1610–1619. doi: 10.1016/j.dld.2021.02.003. [DOI] [PubMed] [Google Scholar]
- 103.Pandyarajan V, Gish RG, Alkhouri N, Noureddin M. Screening for nonalcoholic fatty liver disease in the primary care clinic. Gastroenterol Hepatol (N Y) 2019;15:357–365. [PMC free article] [PubMed] [Google Scholar]
- 104.Zelber-Sagi S, Schonmann Y, Yeshua H, Bentov I. Reply to: "Assessment of hepatic fibrosis in MAFLD: a new player in the evaluation of residual cardiovascular risk?". Dig Liver Dis. 2021;53:385–386. doi: 10.1016/j.dld.2021.01.014. [DOI] [PubMed] [Google Scholar]
- 105.Srivastava A, et al. Prospective evaluation of a primary care referral pathway for patients with non-alcoholic fatty liver disease. J Hepatol. 2019;71:371–378. doi: 10.1016/j.jhep.2019.03.033. [DOI] [PubMed] [Google Scholar]
- 106.Harrison S, Allen A, Dubourg J, Noureddin M, Alkhouri N. Challenges and opportunities in NASH drug development. Nat Med. 2023;29:562–573. doi: 10.1038/s41591-023-02242-6. [DOI] [PubMed] [Google Scholar]
- 107.Rivera-Esteban J, Armandi A, Augustin S, Bugianesi E. Outcomes and potential surrogate markers for future clinical trials of non-alcoholic steatohepatitis cirrhosis. Liver Int. 2021;41:1999–2008. doi: 10.1111/liv.15013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Zhang XL, Wang TY, Targher G, Byrne CD, Zheng MH. Lifestyle interventions for non-obese patients both with, and at risk, of non-alcoholic fatty liver disease. Diabetes Metab J. 2022;46:391–401. doi: 10.4093/dmj.2022.0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Zou TT, et al. Lifestyle interventions for patients with nonalcoholic fatty liver disease: a network meta-analysis. Eur J Gastroenterol Hepatol. 2018;30:747–755. doi: 10.1097/MEG.0000000000001135. [DOI] [PubMed] [Google Scholar]
- 110.Eslam M, et al. The Asian Pacific Association for the Study of the Liver clinical practice guidelines for the diagnosis and management of metabolic associated fatty liver disease. Hepatol Int. 2020;14:889–919. doi: 10.1007/s12072-020-10094-2. [DOI] [PubMed] [Google Scholar]
- 111.Petroni ML, Brodosi L, Bugianesi E, Marchesini G. Management of non-alcoholic fatty liver disease. BMJ. 2021;372:m4747. doi: 10.1136/bmj.m4747. [DOI] [PubMed] [Google Scholar]
- 112.Baratta F, et al. Adherence to mediterranean diet and non-alcoholic fatty liver disease: effect on insulin resistance. Am J Gastroenterol. 2017;112:1832–1839. doi: 10.1038/ajg.2017.371. [DOI] [PubMed] [Google Scholar]
- 113.Baratta F, et al. Poor adherence to Mediterranean Diet and serum lipopolysaccharide are associated with oxidative stress in patients with non-alcoholic fatty liver disease. Nutrients. 2020;12:1732. doi: 10.3390/nu12061732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.von Loeffelholz C, Roth J, Coldewey SM, Birkenfeld AL. The role of physical activity in nonalcoholic and metabolic dysfunction associated fatty liver disease. Biomedicines. 2021;9:1853. doi: 10.3390/biomedicines9121853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Ajmera VH, Terrault NA, Harrison SA. Is moderate alcohol use in nonalcoholic fatty liver disease good or bad? A critical review. Hepatology. 2017;65:2090–2099. doi: 10.1002/hep.29055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Chang Y, et al. Nonheavy drinking and worsening of noninvasive fibrosis markers in nonalcoholic fatty liver disease: a cohort study. Hepatology (Baltimore, MD) 2019;69:64–75. doi: 10.1002/hep.30170. [DOI] [PubMed] [Google Scholar]
- 117.Rice BA, Naimi TS, Long MT. Nonheavy alcohol use associates with liver fibrosis and nonalcoholic steatohepatitis in the Framingham heart study. Clin Gastroenterol Hepatol. 2022 doi: 10.1016/j.cgh.2022.10.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ajmera V, et al. Among patients with nonalcoholic fatty liver disease, modest alcohol use is associated with less improvement in histologic steatosis and steatohepatitis. Clin Gastroenterol Hepatol. 2018;16:1511–1520.e5. doi: 10.1016/j.cgh.2018.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Jarvis H, et al. Does moderate alcohol consumption accelerate the progression of liver disease in NAFLD? A systematic review and narrative synthesis. BMJ Open. 2022;12:e049767. doi: 10.1136/bmjopen-2021-049767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Costanzo S, Di Castelnuovo A, Donati MB, Iacoviello L, de Gaetano G. Alcohol consumption and mortality in patients with cardiovascular disease: a meta-analysis. J Am Coll Cardiol. 2010;55:1339–1347. doi: 10.1016/j.jacc.2010.01.006. [DOI] [PubMed] [Google Scholar]
- 121.Wood AM, et al. Risk thresholds for alcohol consumption: combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. Lancet. 2018;391:1513–1523. doi: 10.1016/S0140-6736(18)30134-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Hansel B, et al. Relationship between alcohol intake, health and social status and cardiovascular risk factors in the Urban Paris-Ile-de-France Cohort: is the cardioprotective action of alcohol a myth? Eur J Clin Nutr. 2010;64:561–568. doi: 10.1038/ejcn.2010.61. [DOI] [PubMed] [Google Scholar]
- 123.Naimi TS, et al. Cardiovascular risk factors and confounders among nondrinking and moderate-drinking US adults. Am J Prev Med. 2005;28:369–373. doi: 10.1016/j.amepre.2005.01.011. [DOI] [PubMed] [Google Scholar]
- 124.Biddinger KJ, et al. Association of habitual alcohol intake with risk of cardiovascular disease. JAMA Netw Open. 2022;5:e223849. doi: 10.1001/jamanetworkopen.2022.3849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.VanWagner LB, et al. Alcohol use and cardiovascular disease risk in patients with nonalcoholic fatty liver disease. Gastroenterology. 2017;153:1260–1272.e3. doi: 10.1053/j.gastro.2017.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Kashiwagi K, et al. Moderate alcohol consumption is not associated with subclinical cardiovascular damage but with hepatic fibrosis in non-alcoholic fatty liver disease. Alcohol. 2020;89:1–7. doi: 10.1016/j.alcohol.2020.07.010. [DOI] [PubMed] [Google Scholar]
- 127.Moon J, et al. SGLT-2 inhibitors and GLP-1 receptor agonists in metabolic dysfunction-associated fatty liver disease. Trends Endocrinol Metab. 2022;33:424–442. doi: 10.1016/j.tem.2022.03.005. [DOI] [PubMed] [Google Scholar]
- 128.Yan J, et al. Liraglutide, sitagliptin, and insulin glargine added to metformin: the effect on body weight and intrahepatic lipid in patients with type 2 diabetes mellitus and nonalcoholic fatty liver disease. Hepatology (Baltimore, MD) 2019;69:2414–2426. doi: 10.1002/hep.30320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Kristensen SL, et al. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet Diabetes Endocrinol. 2019;7:776–785. doi: 10.1016/S2213-8587(19)30249-9. [DOI] [PubMed] [Google Scholar]
- 130.Bethel MA, et al. Cardiovascular outcomes with glucagon-like peptide-1 receptor agonists in patients with type 2 diabetes: a meta-analysis. Lancet Diabetes Endocrinol. 2018;6:105–113. doi: 10.1016/S2213-8587(17)30412-6. [DOI] [PubMed] [Google Scholar]
- 131.Armstrong MJ, et al. Liraglutide safety and efficacy in patients with non-alcoholic steatohepatitis (LEAN): a multicentre, double-blind, randomised, placebo-controlled phase 2 study. Lancet. 2016;387:679–690. doi: 10.1016/S0140-6736(15)00803-X. [DOI] [PubMed] [Google Scholar]
- 132.Newsome PN, et al. A placebo-controlled trial of subcutaneous semaglutide in nonalcoholic steatohepatitis. N Engl J Med. 2021;384:1113–1124. doi: 10.1056/NEJMoa2028395. [DOI] [PubMed] [Google Scholar]
- 133.Mantovani A, et al. Glucagon-like peptide-1 receptor agonists for treatment of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis: an updated meta-analysis of randomized controlled trials. Metabolites. 2021;11:73. doi: 10.3390/metabo11020073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Scheen AJ. Sodium-glucose cotransporter type 2 inhibitors for the treatment of type 2 diabetes mellitus. Nat Rev Endocrinol. 2020;16:556–577. doi: 10.1038/s41574-020-0392-2. [DOI] [PubMed] [Google Scholar]
- 135.Zelniker TA, Braunwald E. Clinical benefit of cardiorenal effects of sodium-glucose cotransporter 2 inhibitors: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75:435–447. doi: 10.1016/j.jacc.2019.11.036. [DOI] [PubMed] [Google Scholar]
- 136.Zelniker TA, et al. Comparison of the effects of glucagon-like peptide receptor agonists and sodium-glucose cotransporter 2 inhibitors for prevention of major adverse cardiovascular and renal outcomes in type 2 diabetes mellitus. Circulation. 2019;139:2022–2031. doi: 10.1161/CIRCULATIONAHA.118.038868. [DOI] [PubMed] [Google Scholar]
- 137.Zelniker TA, Braunwald E. Mechanisms of cardiorenal effects of sodium-glucose cotransporter 2 inhibitors: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75:422–434. doi: 10.1016/j.jacc.2019.11.031. [DOI] [PubMed] [Google Scholar]
- 138.Bolinder J, et al. Effects of dapagliflozin on body weight, total fat mass, and regional adipose tissue distribution in patients with type 2 diabetes mellitus with inadequate glycemic control on metformin. J Clin Endocrinol Metab. 2012;97:1020–1031. doi: 10.1210/jc.2011-2260. [DOI] [PubMed] [Google Scholar]
- 139.Lai LL, Vethakkan SR, Nik Mustapha NR, Mahadeva S, Chan WK. Empagliflozin for the treatment of nonalcoholic steatohepatitis in patients with type 2 diabetes mellitus. Dig Dis Sci. 2020;65:623–631. doi: 10.1007/s10620-019-5477-1. [DOI] [PubMed] [Google Scholar]
- 140.Mantovani A, Petracca G, Csermely A, Beatrice G, Targher G. Sodium-glucose cotransporter-2 inhibitors for treatment of nonalcoholic fatty liver disease: a meta-analysis of randomized controlled trials. Metabolites. 2020;11:22. doi: 10.3390/metabo11010022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Belfort R, et al. A placebo-controlled trial of pioglitazone in subjects with nonalcoholic steatohepatitis. N Engl J Med. 2006;355:2297–2307. doi: 10.1056/NEJMoa060326. [DOI] [PubMed] [Google Scholar]
- 142.Young LH, et al. Cardiac outcomes after ischemic stroke or transient ischemic attack: effects of pioglitazone in patients with insulin resistance without diabetes mellitus. Circulation. 2017;135:1882–1893. doi: 10.1161/CIRCULATIONAHA.116.024863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Young LH, et al. Heart failure after ischemic stroke or transient ischemic attack in insulin-resistant patients without diabetes mellitus treated with pioglitazone. Circulation. 2018;138:1210–1220. doi: 10.1161/CIRCULATIONAHA.118.034763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Mehtälä J, et al. Pioglitazone use and risk of bladder cancer: a systematic literature review and meta-analysis of observational studies. Diabetol Int. 2019;10:24–36. doi: 10.1007/s13340-018-0360-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Portillo-Sanchez P, et al. Effect of pioglitazone on bone mineral density in patients with nonalcoholic steatohepatitis: a 36-month clinical trial. J Diabetes. 2019;11:223–231. doi: 10.1111/1753-0407.12833. [DOI] [PubMed] [Google Scholar]
- 146.Jacques V, et al. Deuterium-stabilized (R)-pioglitazone (PXL065) Is responsible for pioglitazone efficacy in NASH yet exhibits little to no PPARγ activity. Hepatol Commun. 2021;5:1412–1425. doi: 10.1002/hep4.1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Grundy SM, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e1082–e1143. doi: 10.1161/CIR.0000000000000625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Pastori D, et al. Statin liver safety in non-alcoholic fatty liver disease: a systematic review and metanalysis. Br J Clin Pharmacol. 2022;88:441–451. doi: 10.1111/bcp.14943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Athyros VG, et al. Safety and efficacy of long-term statin treatment for cardiovascular events in patients with coronary heart disease and abnormal liver tests in the Greek Atorvastatin and Coronary Heart Disease Evaluation (GREACE) Study: a post-hoc analysis. Lancet. 2010;376:1916–1922. doi: 10.1016/S0140-6736(10)61272-X. [DOI] [PubMed] [Google Scholar]
- 150.Fatima K, et al. Efficacy of statins in treatment and development of non-alcoholic fatty liver disease and steatohepatitis: a systematic review and meta-analysis. Clin Res Hepatol Gastroenterol. 2021;46:101816. doi: 10.1016/j.clinre.2021.101816. [DOI] [PubMed] [Google Scholar]
- 151.Khoo S, et al. Suboptimal treatment of dyslipidemia in patients with nonalcoholic fatty liver disease. J Gastroenterol Hepatol. 2020;35:320–325. doi: 10.1111/jgh.14794. [DOI] [PubMed] [Google Scholar]
- 152.Du J, Ma YY, Yu CH, Li YM. Effects of pentoxifylline on nonalcoholic fatty liver disease: a meta-analysis. World J Gastroenterol. 2014;20:569–577. doi: 10.3748/wjg.v20.i2.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Vilar-Gomez E, et al. Weight loss through lifestyle modification significantly reduces features of nonalcoholic steatohepatitis. Gastroenterology. 2015;149:367–378. doi: 10.1053/j.gastro.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 154.Arterburn DE, Telem DA, Kushner RF, Courcoulas AP. Benefits and risks of bariatric surgery in adults: a review. JAMA. 2020;324:879–887. doi: 10.1001/jama.2020.12567. [DOI] [PubMed] [Google Scholar]
- 155.Aminian A, et al. Association of bariatric surgery with major adverse liver and cardiovascular outcomes in patients with biopsy-proven nonalcoholic steatohepatitis. JAMA. 2021;326:2031–2042. doi: 10.1001/jama.2021.19569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Elsaid M, et al. Association of bariatric surgery with cardiovascular outcomes in adults with severe obesity and nonalcoholic fatty liver disease. JAMA Netw Open. 2022;5:e2235003. doi: 10.1001/jamanetworkopen.2022.35003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data included in this study are available upon request by contact with the corresponding author (zhengmh@wmu.edu.cn).