Abstract
BACKGROUND
Acral persistent papular mucinosis (APPM) is a rare idiopathic subtype of localized lichen myxedematosus. To date, there have been 40 APPM cases reported worldwide; however, only 7 cases have been reported in the Korean literature.
CASE SUMMARY
A 70-year-old man was referred to our hospital with a solitary pinkish nodule on the dorsum of his right hand. Despite the absence of symptoms, the patient wanted to know the exact diagnosis; thus, a biopsy was performed. Histopathological examination of a biopsy specimen obtained from the nodule on the dorsum of his hand revealed orthokeratotic hyperkeratosis with patchy parakeratosis, prominent hypergranulosis, and diffuse dissecting mucinous deposition between collagen bundles, along with some bland-looking spindle cells throughout the dermis. The nodule was histologically diagnosed as an APPM, and an intralesional triamcinolone injection (2.5 mg/mL) was started every 2 wk. After three sessions of treatment, the patient showed marked improvements.
CONCLUSION
To the best of our knowledge, this is the first case of a Korean APPM presenting as a solitary nodule that showed a marked response to triamcinolone intralesional injection. Since it is a rare disease, we report this case to contribute to future research on the pathogenesis and treatment of APPM.
Keywords: Acral persistent papular mucinosis, Localized lichen myxedematosus, Cutaneous mucinosis, Mucin, Case report
Core Tip: Acral persistent papular mucinosis (APPM) is a rare idiopathic subtype of localized lichen myxedematosus. To date, 40 cases have been reported worldwide; however, only seven cases have been reported in the Korean literature. This article reports on a rare case of solitary APPM, which was histologically diagnosed in a 70-year-old Korean man with a pinkish nodule on the dorsum of his hand. The patient showed marked improvement after three sessions of intralesional triamcinolone injection. This is the first reported case of a Korean APPM presenting as a solitary nodule and emphasizes the importance of continued research into the pathogenesis and treatment of this rare disease.
INTRODUCTION
Acral persistent papular mucinosis (APPM) is a rare idiopathic subtype of localized lichen myxedematosus (LM)[1]. It is characterized by white or skin-colored, 2–5 mm papules on the hands, wrists, and extensor aspects of the forearms[1]. The number of papules varies from a few to hundreds and is usually asymptomatic; however, some patients complain of pruritus[1].
Most cases have a favorable prognosis and require no treatment; however, in some cases, tacrolimus ointments or triamcinolone intralesional injections have been administered.
To date, there have been 40 APPM cases reported worldwide[1,2], however, only 7 cases have been reported in the Korean literature. Herein, we present a new case of an older Korean adult with solitary APPM as an atypical manifestation. In addition, we summarized 8 cases of APPM, including ours.
CASE PRESENTATION
Chief complaints
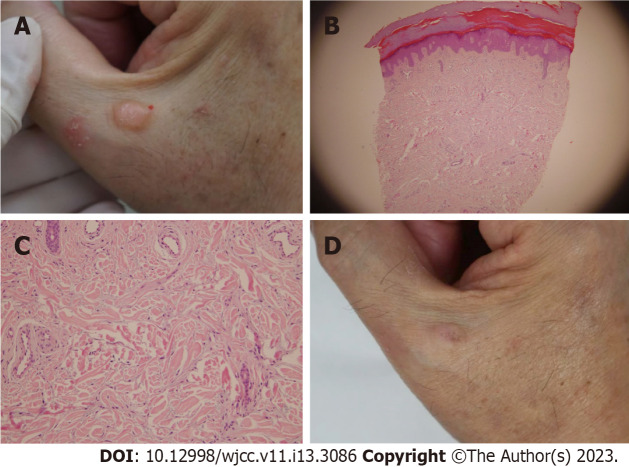
A 70-year-old man was referred to our hospital with a solitary pinkish nodule on the dorsum of his right hand (Figure 1A).
Figure 1.
A pinkish, solitary nodule measuring 1 cm was found on the right dorsum of the hand. A: A clinical image taken before treatment showed the appearance of the nodule; B: Biopsy results showed orthokeratotic hyperkeratosis with patchy parakeratosis, prominent hypergranulosis; C: Diffuse dissecting mucinous deposition between collagen bundles, along with some bland-looking spindle cells throughout the dermis (H&E; B: ×40, C: ×200); and D: Following three sessions of intralesional triamcinolone injection every 2 wk, a marked improvement was observed.
History of present illness
The patient was asymptomatic and did not complain of pruritus or pain.
History of past illness
His medical history showed that he had psoriasis for decades, which was managed using topical agents.
Personal and family history
He denied any other familial history of dermatologic or endocrinologic diseases.
Physical examination
Despite the absence of symptoms, the patient wanted to know the exact diagnosis; thus, biopsy and blood tests were performed.
Laboratory examinations
Blood tests showed no endocrine abnormalities including thyroid function.
Imaging examinations
Histopathological examination of a biopsy specimen obtained from the nodule on the dorsum of his hand revealed orthokeratotic hyperkeratosis with patchy parakeratosis, prominent hypergranulosis, and diffuse dissecting mucinous deposition between collagen bundles, along with some bland-looking spindle cells throughout the dermis (Figure 1B and C).
FINAL DIAGNOSIS
The nodule was histologically diagnosed as an APPM.
TREATMENT
To reduce the size, intralesional triamcinolone injection (2.5 mg/mL) was administered once every 2 wk.
OUTCOME AND FOLLOW-UP
After three sessions of treatment, the patient showed marked improvements (Figure 1D).
DISCUSSION
Cutaneous mucinosis is a medical term used for a diverse group of skin disorders that involve a localized or widespread accumulation of mucin in the skin or within the hair follicle[3,4]. Mucin is composed of mucopolysaccharides acid or hyaluronic acid and is generally present as part of the connective tissue of the dermis[3,4]. Its main function is to maintain the balance of salt and water in the dermis. The excessive deposition of mucin manifests as a clinically specific lesion or a mucinous rash[3,4]. Cutaneous mucinosis can be divided into two main groups: Generalized form (scleromyxedema), which classically presents with systemic abnormalities, such as monoclonal gammopathy or thyroid disease; and localized form (LM), which is a rare form and classically presents with a lack of systemic disease[3,4].
APPM was first described by Rongioletti et al[1] in 1986. It is one of the five subtypes of LM, namely, a discrete form, APPM, self-healing papular mucinosis, papular mucinosis of infancy, and a pure nodular form[3]. APPM is a chronic idiopathic cutaneous mucinosis characterized by lichenoid papules or nodules with mucin deposition and the absence of associated thyroid disease, paraproteinemia, and other systemic abnormalities[3-5]. Patients with this diagnosis are typically women and present with a bilaterally symmetrical distribution on their hands and wrists but not on the trunk and face[6].
The etiology of APPM is still unknown; however, family cases have shown that genetic and environmental factors play an important role[7]. Interleukin-1, interferon gamma, tumor necrosis factor-alpha (TNF-α), and transforming growth factor beta may stimulate glycosaminoglycan synthesis, but the true triggers are unknown, and there is a report of cutaneous mucinosis developing after using a biological agent, such as a TNF-α inhibitor, in patients with psoriasis[8]. Our patient had psoriasis for a long time; however, the direct link between cutaneous mucinosis and psoriasis is not well-known, with no reported literature. Human immunodeficiency virus (HIV) infection can also be linked to primary cutaneous mucinoses, and 18 cases of primary cutaneous mucinoses in HIV-infected patients have been reported, 2 of which are APPM. It has been speculated that direct stimulation of fibroblasts by HIV infection or fibroblast stimulation by activated serum cytokines owing to overactive B-cell function may be associated with mucin deposition, but no definitive mechanism has been elucidated[9].
Since APPM has rarely been reported in Korea, we have summarized the characteristics of APPM cases that have occurred in Korea[6,9-13] (Table 1). To the best of our knowledge, there are eight cases, including the present one, of which five were reported in males and three in females. Their ages ranged from 31 to 70 years, and most were middle-aged. Most had no underlying disease and only two patients had reported underlying medical conditions; one, who was a patient in our case, had psoriasis, while the other had HIV. Only one patient complained of itching, while the rest were asymptomatic. Notably, except for our case, all cases presented symmetrical, multiple papules. To the best of our knowledge, this is the first case of a large solitary nodule. As it is a rare form that has not been previously reported, the possibility of APPM should be considered even with a single nodule. Among the 40 cases reported worldwide, it is interesting that 8 were Korean and 24 were Japanese[1,2], suggesting a racial influence; however, further studies are necessary to confirm this because of the small number of samples.
Table 1.
Summary of the Korean cases of acral persistent popular mucinosis
|
Case
|
Ref.
|
Age/Sex
|
Onset
|
Past medical history
|
Clinical manifestation
|
Treatment
|
Outcome
|
| 1 | Kim et al[11], 1993 | F/56 | 1 mo ago | s/p Rt. Nephrectomy d/t renal cancer | Multiple, flesh-colored papules on both forearms, wrists and hands without symptoms | None | - |
| 2 | Lee et al[12], 2000 | M/43 | 6-7 years ago | None | Multiple discrete white to flesh-colored papules are present on the extensor surface of hand without symptoms | None | - |
| 3 | Lee et al[12], 2000 | M/50 | 7 years ago | None | Multiple whitish papules on dorsum of the hand without symptoms | None | - |
| 4 | Song et al[6], 2002 | F/50 | 3 years ago | None | Pruritic numerous papular eruption on the dorsa of the hands, and the extensor surface of the forearms | Intralesional triamcinolone injection | No improvement |
| 5 | Ryu et al[13], 2003 | M/64 | 15 years ago | s/p Subtotal gastrectomy d/t gastric ulcer | Asymptomatic flesh-colored or translucent papules on wrists, back of the hands, and distal forearms | None | - |
| 6 | Choi et al[9], 2007 | M/31 | 2 mo ago | AIDS | Multiple tiny flesh-colored papules on the extensor surface of the wrist and the distal part of forearm | After 5 wk of starting highly active antiretroviral therapy for AIDS, the skin lesions were also resolved | Resolved |
| 7 | Jun et al[10], 2016 | F/53 | 7-8 years ago | None | Asymptomatic 1-3 mm flesh-colored papules symmetrically located on both dorsum of hands and wrists, and on anterior chest | Tacrolimus ointment 0.1% once a day | After 15 wk, responded partially |
AIDS: Acquired immunodeficiency syndrome.
No effective treatment has been established for APPM. Treatment options range from topical steroids or tacrolimus and intralesional corticosteroids to oral tranilast, which inhibits the release of histamine and prostaglandins from mast cells[2]. However, the effects of these treatments are variable. In the Korean cases, four patients were not treated, and the exact outcome could not be identified owing to loss of follow-up. One patient showed some improvement after 15 wk of topical application of tacrolimus. In another case, an intralesional steroid injection was administered but no improvement was noted, and the exact number and interval of treatment were not known. In one case with acquired immunodeficiency syndrome (AIDS) as an underlying disease, APPM improved with antiviral treatment for AIDS without any specific treatment for APPM[6,9-13]. In our case, intralesional triamcinolone injection was effective; therefore, it can be estimated that intralesional corticosteroids are effective in APPM alone, but additional research is needed. Recently, since the main component of mucin is hyaluronic acid, there have been several case reports in which scleromyxedema and popular dermal mucinosis were treated with hyaluronidase[14,15]. Another therapeutic option is electrocoagulation or erbium-YAG laser[16,17].
CONCLUSION
To the best of our knowledge, this is the first case of a Korean APPM presenting as a solitary nodule that showed a marked response to triamcinolone intralesional injection. Since it is a rare disease, we report this case to contribute to future research on the pathogenesis and treatment of APPM.
ACKNOWLEDGEMENTS
The authors declare that they have no proprietary, commercial, or financial interests that could be construed to have inappropriately influenced this study.
Footnotes
Informed consent statement: The primary version of the consent that has been signed by the patient in the study is attached as a separate file.
Conflict-of-interest statement: All the authors report no relevant conflicts of interest for this article.
CARE Checklist (2016) statement: The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: December 29, 2022
First decision: March 10, 2023
Article in press: March 31, 2023
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Fan L, China S-Editor: Liu XF L-Editor: A P-Editor: Zhang XD
Contributor Information
Yu Jeong Park, Department of Dermatology, Dongguk University Ilsan Hospital, College of Medicine, Dongguk University, Goyang-si, Gyeonggi-do, Korea 10326, South Korea.
Hui Young Shin, Department of Dermatology, Dongguk University Ilsan Hospital, College of Medicine, Dongguk University, Goyang-si, Gyeonggi-do, Korea 10326, South Korea.
Woo Kyoung Choi, Department of Dermatology, Dongguk University Ilsan Hospital, College of Medicine, Dongguk University, Goyang-si, Gyeonggi-do, Korea 10326, South Korea.
Ai-Young Lee, Department of Dermatology, Dongguk University Ilsan Hospital, College of Medicine, Dongguk University, Goyang-si, Gyeonggi-do, Korea 10326, South Korea.
Seung Ho Lee, Department of Dermatology, Dongguk University Ilsan Hospital, College of Medicine, Dongguk University, Goyang-si, Gyeonggi-do, Korea 10326, South Korea.
Jong Soo Hong, Department of Dermatology, Dongguk University Ilsan Hospital, College of Medicine, Dongguk University, Goyang-si, Gyeonggi-do, Korea 10326, South Korea. jsttjstt@hanmail.net.
References
- 1.Rongioletti F, Ferreli C, Atzori L. Acral persistent papular mucinosis. Clin Dermatol. 2021;39:211–214. doi: 10.1016/j.clindermatol.2020.10.001. [DOI] [PubMed] [Google Scholar]
- 2.Mori A, Shinkuma S, Mitsui Y, Ogawa K, Miyagawa F, Asada H. Acral persistent papular mucinosis: A case report and summary of 24 Japanese cases. J Dermatol. 2021;48:1574–1578. doi: 10.1111/1346-8138.16043. [DOI] [PubMed] [Google Scholar]
- 3.Rongioletti F, Rebora A. Updated classification of papular mucinosis, lichen myxedematosus, and scleromyxedema. J Am Acad Dermatol. 2001;44:273–281. doi: 10.1067/mjd.2001.111630. [DOI] [PubMed] [Google Scholar]
- 4.Cárdenas-Gonzalez RE, Ruelas MEH, Candiani JO. Lichen myxedematosus: a rare group of cutaneous mucinosis. An Bras Dermatol. 2019;94:462–469. doi: 10.1590/abd1806-4841.20198478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harris JE, Purcell SM, Griffin TD. Acral persistent papular mucinosis. J Am Acad Dermatol. 2004;51:982–988. doi: 10.1016/j.jaad.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 6.Song JY, Lee SW, Kim CW, Kim HO. A case of acral persistent popular mucinosis. Ann Dermatol. 14:178–180. [Google Scholar]
- 7.Menni S, Cavicchini S, Brezzi A, Gianotti R, Caputo R. Acral persistent papular mucinosis in two sisters. Clin Exp Dermatol. 1995;20:431–433. doi: 10.1111/j.1365-2230.1995.tb01366.x. [DOI] [PubMed] [Google Scholar]
- 8.Zhou X, Mubanga D, Chen Z, Bi X. Secondary Generalized Cutaneous Mucinosis Developed During Etanercept Treatment in a Patient with Psoriasis. Clin Cosmet Investig Dermatol. 2022;15:987–992. doi: 10.2147/CCID.S368390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choi JE, Kim JW, Cho HM, Ahn HH, Kye YC, Kim SN. A case of acral persistent popular mucinosis in patient with HIV infection. Korean J Dermatol. 2007;45:951–955. [Google Scholar]
- 10.Jun JY, Oh SH, Shim JH, Kim JH, Park JH, Lee DY. Acral Persistent Papular Mucinosis with Partial Response to Tacrolimus Ointment. Ann Dermatol. 2016;28:517–519. doi: 10.5021/ad.2016.28.4.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim YH, Yoon JS, Lee JS, Lee JH, Park JK. A case of acral persistent popular mucinosis. Kor J Dermatol. 1993;31:232–235. [Google Scholar]
- 12.Lee MW, Choi JH, Sung KJ, Moon KC, Koh JK. Acral persistent popular mucinosis. Kor J Dermatol. 2000;38:236–239. [Google Scholar]
- 13.Ryu HJ, Son SW, Kim Aeree, Kim IH. A case of acral persistent popular mucinosis. Ann Dermatol. 2003;15:8–11. [Google Scholar]
- 14.Akaslan TÇ, Yıldız P, Onsun N. Clinical and histopathological improvement of scleromyxedema-induced microstomia after hyaluronidase injection. J Cosmet Dermatol. 2022;21:4319–4322. doi: 10.1111/jocd.15007. [DOI] [PubMed] [Google Scholar]
- 15.Ramamurthi A, Bicknell L, McCarty M. Hyaluronidase in the treatment of papular dermal mucinosis: first case reported in North America. J Surg Dermatol. 2016;4:9–13. [Google Scholar]
- 16.André Jorge F, Mimura Cortez T, Guadalini Mendes F, Esther Alencar Marques M, Amante Miot H. Treatment of acral persistent papular mucinosis with electrocoagulation. J Cutan Med Surg. 2011;15:227–229. doi: 10.2310/7750.2011.10030. [DOI] [PubMed] [Google Scholar]
- 17.Graves MS, Lloyd AA, Ross EV. Treatment of acral persistent papular mucinosis using an Erbium-YAG laser. Lasers Surg Med. 2015;47:467–468. doi: 10.1002/lsm.22368. [DOI] [PubMed] [Google Scholar]