Abstract
Study Design:
This was a retrospective study.
Objective:
Since a better understanding of modifiable risk factors for proximal junctional disease (PJD) may lead to improved postoperative outcomes and less need of revision surgery, the aim of the present study is to determine whether sarcopenia and osteopenia are independent risk factors for PJD in patients undergoing lumbar fusion.
Summary of Background Data:
PJD is one of the most frequent complications following posterior instrumented spinal fusion. It is characterized by a spectrum of pathologies ranging from proximal junctional kyphosis (PJK) to proximal junctional failure (PJF). The etiology of PJD is multifactorial and currently not fully understood. Patient-specific factors, such as age, body mass index, osteoporosis, sarcopenia, and the presence of other comorbidities, can represent potential risk factors.
Materials and Methods:
A retrospective review of patients, aging 50–85 years, who underwent a short (≤3 levels) posterior lumbar fusion for degenerative diseases was performed. Through magnetic resonance imaging (MRI), central sarcopenia and osteopenia were evaluated, measuring the psoas-to-lumbar vertebral index (PLVI) and the M-score. A multivariate analysis was performed to determine the independent risk factors for PJD, PJK, and PJF.
Results:
A total of 308 patients (mean age at surgery 63.8 ± 6.2 years) were included. Ten patients (3.2%) developed a PJD and all required revision surgery. Multivariate regression identified PLVI (P = 0.02) and M-score (P = 0.04) as independent risk factors for both PJK (P = 0.02 and P = 0.04, respectively) and PJF (P = 0.04 and P = 0.01, respectively).
Conclusions:
Sarcopenia and osteopenia, as measured by PLVI and M-score, proved to be independent risk factors for PJD in patients who undergo lumbar fusion for degenerative diseases.
Clinical Trial Registration:
The present study was approved by the Institutional Review Board, CE AVEC 208/2022/OSS/IOR.
Keywords: Degenerative disease, osteopenia, proximal junctional disease, sarcopenia
INTRODUCTION
Proximal junctional disease (PJD) is one of the most frequent complications following posterior instrumented spinal fusion,[1] and has a significant impact on a patient's quality of life. It is a spectrum of pathologies ranging from proximal junctional kyphosis (PJK) as a radiologic finding with no clinical relevance to proximal junctional failure (PJF) with instrumentation failure, pain, and neurologic deficit.[2]
A significant challenge in preventing PJD is that its etiology is not fully understood; it is supposed to be multifactorial, and a number of patient-specific (age, body mass index [BMI], preoperative sagittal vertical axis, muscle mass, and bone quality) and surgical (overcorrection, uppermost instrumented vertebra [UIV] in the thoracolumbar spine, sacrum fixation, and rigidity of the construct) risk factors have been reported.[3,4,5,6,7,8]
Central sarcopenia, defined as “syndrome of progressive and generalized loss of muscle mass and strength,” is known to be related to higher morbidity and mortality after spinal and prosthetic surgery.[9,10,11,12] However, its role as a risk factor for PJD is poorly defined. A recent retrospective cohort study on 32 patients reported that sarcopenia is an independent, modifiable predictor for both PJK and PJF, following adult spinal deformity surgery.[13]
Osteopenia, defined as decreased vertebral bone density, alters the biomechanical impact of implants on vertebral bodies and may increase implant-related complications, such as vertebral fractures and implant failure. Because a large proportion of PJK occurs as a result of fracture at the UIV, it is not surprising that osteopenia likely contributes to the development of PJK.[14] In fact, a retrospective comparative study with adult patients has shown that osteopenia is prevalent in patients with PJK.[15]
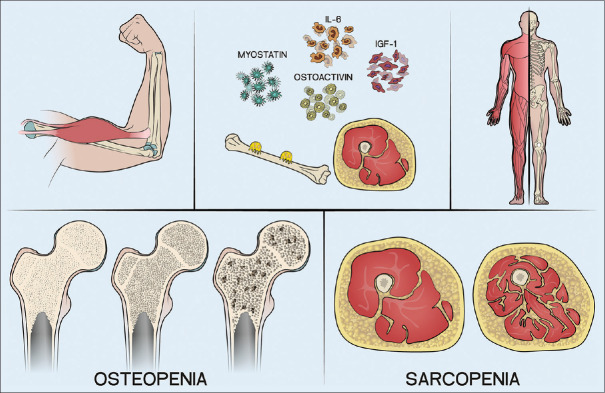
However, it is important to emphasize that osteopenia and sarcopenia are both part of the so-called “fragility syndrome”[16] and are closely related to each other; the presence of reduced muscle mass is directly related with low bone density. This is due to the mutual interaction between the two tissues (bone and muscles) that communicate through paracrine and endocrine molecules that continuously modulate their development and function [Figure 1].[17,18,19]
Figure 1.
Interaction between bone and muscle is mediated by molecules such as myostatin, osteoactivin, IL-6, and IGF-1. IL-6 – Interleukin-6, IGF-1 – Insulin-like growth factor 1
To the best of the authors’ knowledge, no studies investigated the relationship between sarcopenia, osteopenia, and PJD after lumbar fusion. Since a better understanding of modifiable risk factors for PJD may lead to improved postoperative outcomes and less need of revision surgery, the aim of the present study was to determine whether sarcopenia and osteopenia are independent risk factors for PJD in patients undergoing lumbar fusion.[20]
MATERIALS AND METHODS
A retrospective review of patients, aging 50–85 years, who underwent a short (≤3 levels) posterior lumbar fusion for lumbar degenerative diseases between July 2005 and July 2020 (minimum 2 years follow-up) in our institution was performed. Inclusion criteria were the primary degenerative disease of the lumbosacral spine, no history of lumbar vertebral fractures or neoplastic diseases, no previous spinal surgery, available preoperative lumbar spine magnetic resonance image (MRI), minimum 2-year follow-up, and complete medical records of the hospitalization.
The following baseline data were collected: age, gender, smoking history, diabetes, BMI, Charlson Comorbidity Index, and American Society of Anesthesiology classification. Moreover, data about the length of surgery and length of stay were also collected and analyzed.
Then, preoperative MRIs were evaluated. Psoas-to-lumbar vertebral index (PLVI), a validated measure of central sarcopenia,[1] and the M-Score, a validated measure of bone density,[21] were calculated. The PLVI [Figure 2] was calculated by measuring the psoas muscle and the L4 body cross-sectional areas (CSAs) on a single MRI axial cut at the level of L4 pedicles,[1] applying the following formula: (Left psoas CSA + Right psoas CSA)/2/L4 CSA.
Figure 2.
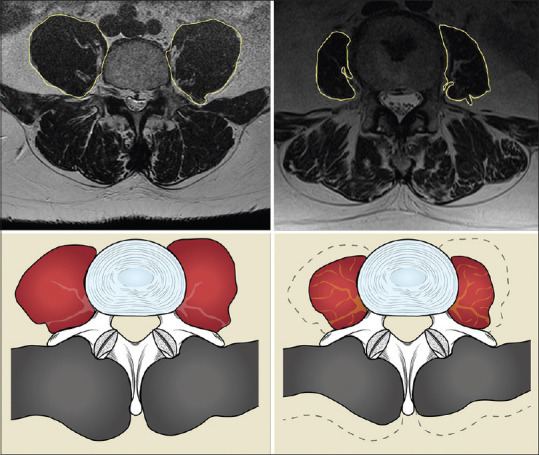
Examples of high (on the left) and low (on the right) PLVI patients. PLVI – Psoas to lumbar vertebral index
The M-score [Figure 3] was calculated on the T1W spin-echo sequence of the preoperative MRI, which is the most accurate for the evaluation of bone marrow. In the sagittal section passing through the spinous process of the lumbar vertebrae, a region of interest (ROI) was placed as a circle in the vertebral body from L1 to L4. Cortical bone, lumbar plexus, focal lesions, and radiological artifacts were avoided. To evaluate the noise, an ROI was also placed outside the patient: signal-to-noise ratio (SNRL1-L4) was calculated by dividing the vertebral body intensity by the standard deviation of the noise. The mean and the standard deviation of the reference population were then used, and the M-score was obtained with the following formula: M-Score = (SNRL1-L4– SNRref)/SDref.[21]
Figure 3.
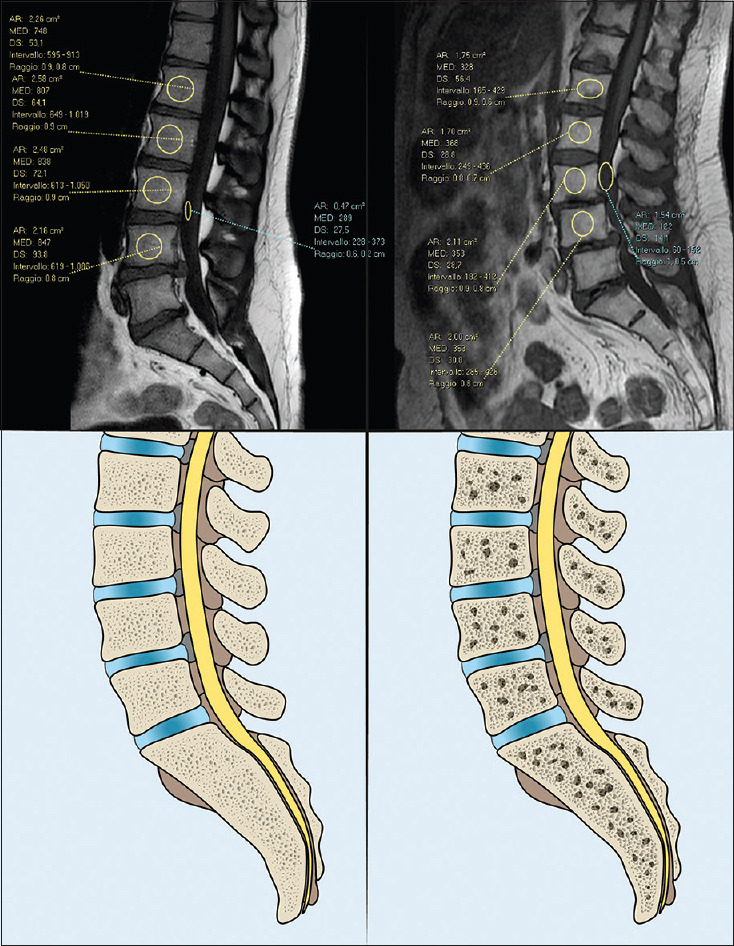
Examples of high (on the left) and low (on the right) M-score patients
Then, the last follow-up full-length standing X-rays were evaluated to identify mechanical complications such as PJK and PJF. PJK was defined as a proximal junctional sagittal Cobb angle between the lower endplate of UIV and the upper endplate of 2 supra-adjacent vertebrae ≥10° or at least 10° greater than the preoperative measurement.[22] PJF is defined as symptomatic PJK requiring revision surgery and includes vertebral fracture of UIV or UIV +1, subluxation between UIV and UIV +1, failure of fixation, implant pull-out or breakage, and/or disruption of the posterior osteoligamentous complex.[23]
All measures were taken by two experienced spine surgeons (TC and MM). They took the measures independently and were blinded to the patients’ names. Mean values were considered.
Statistical analysis
Patients were divided into PJD and non-PJD. Baseline characteristics and incidence of mechanical complications in the two cohorts were calculated and statistically compared.
Parametric test was used to compare samples in the case of continuous variables and normal distribution. The Shapiro–Wilk test was used to verify normal distribution. The Levene test was used to analyze the homogeneity of the variances. For the parametric test, the two-tailed Student's t was used to compare the average of the variables for homoscedastic unpaired groups. For the nonparametric test, the two-tailed Mann–Whitney U for unpaired groups was used. Continuity correction was applied in the case of discrete distribution. Chi-square test was used to quantify the strength of the association between categorical variables. Multivariate linear regression was performed to identify independent risk factors for PJK, PJF, and PJD. P <0.05 was considered significant. All analyses were performed with the Statistical Package for Social Science IBM Corp. (2020). IBM SPSS Statistics for Windows (Version 27.0) [Computer software]. IBM Corp.
RESULTS
Baseline characteristics and demographics
A total of 308 patients (mean age at surgery 63.8 ± 6.2 years) undergoing posterior lumbar fusion for degenerative diseases in our institution met the inclusion criteria, and their records have been reviewed. The mean follow-up was 45.6 (24–124) months. Demographic data and baseline characteristics are summarized in Table 1.
Table 1.
Baseline characteristics of the patients
| Characteristics | Total | Non-PJD | PJD | P |
|---|---|---|---|---|
| n | 308 | 282 | 10 (8 PJF, 2 PJK) | NA |
| Age at surgery (years), mean±SD | 63.8±6.2 | 63.5±6.06 | 67.5±4.04 | 0.002* |
| Gender (female) | 160 | 165 | 8 | 0.04* |
| DM (yes n) | 28 | 26 | 0 | 0.27 |
| CCI (n), mean±SD | 2.57±3.6 | 2.5±1.45 | 3±1.9 | 0.15 |
| ASA score (n), mean±SD | 2.03±0.6 | 2.03±0.58 | 2±0.74 | 0.91 |
| BMI (n), mean±SD | 26.5±6.2 | 26.6±3.7 | 27.1±5.7 | 0.98 |
| Smoking (yes n) | 74 | 66 | 2 | 0.21 |
| Length of stay (day), mean±SD | 11.1±12.7 | 11.2±13.1 | 11.5±4.04 | 0.32 |
| Operative time (min), mean±SD | 193.3±59 | 196±59.1 | 165±52 | 0.30 |
| PLVI, mean±SD | 0.71±0.18 | 0.72±0.19 | 0.6±0.23 | 0.23 |
| PLVI (low n) | 153 | 130 | 4 | 0.03* |
| M-score, mean±SD | 0±128 | −0.91±0.15 | −0.92±0.006 | 0.04* |
| PJD, n (%) | 10 (3.2) |
*Statistically significant, NA - Not applicable, SD - Standard deviation, PJD - Proximal junctional disease, PVLI - Psoas lumbar vertebral index, ASA - American Society of Anesthesiology, CCI - Charlson Comorbidity Index, BMI - Body mass index, DM - Diabetes mellitus, PJK - Proximal junctional kyphosis, PJD - Proximal junctional failure
All patients underwent to posterior lumbar fusion with all-pedicle screws constructs; no patient received proximal augmentation. The overall incidence of PJD was 3.2% [10 cases, Figure 4]: Eight patients (2.6%) had PJF and two (0.6%) had PJK. They all required revision surgery. None of the patients developed distal junctional complications.
Figure 4.
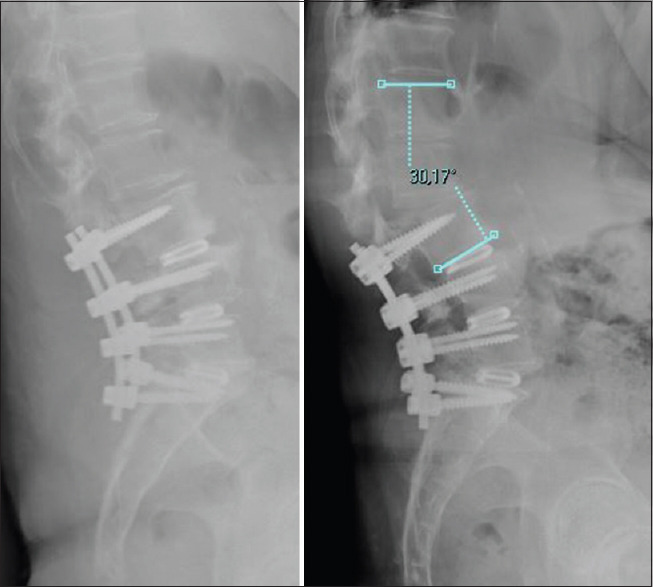
70-year-old female patient, operated for central and foraminal multilevel stenosis. A posterior L3-S1 arthrodesis with intersomatical cages (posterior lumbar interbody fusion) was performed. At 6-month follow-up, the patient developed a PJD. PJD – Proximal junctional disease
Mean M-score and mean PLVI were 0 (range: −1.74– +3.18) and 0.71 (range: 0.18–1.54), respectively. Of the included patients, 155 had high PLVI (>0.71) and 153 had low PLVI (<0.71); low PLVI patients were more likely to have a low M-score (P = 0.03). Ninety-five patients had high M-score (<0), while 213 had low M-score (<0). Low M-score patients did not show a lower PLVI when compared to high M-score patients (P = 0.5).
The relationship between investigated variables and PJD is provided in Table 1. Univariate analysis [Table 1] identified several significant risk factors for PJD, including age at surgery (P = 0.002), female gender (P = 0.04), and PLVI and M-score (P = 0.03 and P = 0.04, respectively). The final multivariable model [Table 2 and Figure 5] confirmed that the four variables identified at the univariate are independent risk factors for PJD: age, gender, PLVI, and M-score.
Table 2.
Multivariate logistic regression analysis of factors associated with proximal junctional disease, kyphosis, and failure risk factors
| Risk factor | Estimate | CI 95% lower | CI 95% upper | P |
|---|---|---|---|---|
| PJD | ||||
| Age at surgery | 0.00617 | 0.00321 | 0.01273 | 0.002 |
| Gender (female) | −0.37632 | −0.62129 | −0.01213 | 0.04 |
| DM (yes) | −0.02908 | −0.14732 | 0.09816 | 0.6 |
| CCI | −0.01906 | −0.04955 | −0.01142 | 0.2 |
| ASA score | 0.00552 | −0.05702 | 0.06806 | 0.8 |
| BMI | 0.11749 | −0.03520 | 0.09311 | 0.8 |
| Smoking (yes) | 0.01937 | −0.3659 | 0.07534 | 0.5 |
| PLVI | 0.11508 | 0.00494 | 0.22523 | 0.03 |
| M-Score | 0.11243 | 0.02030 | 0.30112 | 0.04 |
| PJF | ||||
| Age at surgery | 0.00647 | 0.00131 | 0.01162 | 0.01 |
| Gender (female) | −0.05284 | −0.11485 | 0.00917 | 0.09 |
| DM (yes) | −0.07348 | −0.17839 | 0.013143 | 0.2 |
| CCI | −0.01530 | −0.04109 | 0.01050 | 0.2 |
| ASA score | −0.00833 | −0.06120 | 0.04455 | 0.7 |
| BMI | 0.00308 | −0.00473 | 0.01089 | 0.4 |
| Smoking (yes) | 0.01060 | −0.05000 | 0.07121 | 0.7 |
| PLVI | −0.26592 | −0.52138 | −0.01047 | 0.04 |
| M-Score | 0.11403 | 0.02030 | 0.20776 | 0.01 |
| PJK | ||||
| Age at surgery | 1.5234 | −0.00287 | 0.00337 | 0.8 |
| Gender (female) | −0.00307 | 0.01871 | −0.04000 | 0.2 |
| DM (yes) | −0.01529 | 0.03239 | −0.07920 | 0.9 |
| CCI | −0.00148 | −0.02801 | 0.01353 | 0.8 |
| ASA score | −0.00374 | −0.02801 | 0.03550 | 0.8 |
| BMI | −0.00266 | −00734 | 0.00202 | 0.3 |
| Smoking (yes) | −0.00737 | −0.04372 | 0.02899 | 0.7 |
| PLVI | 0.10042 | 0.00684 | 0.19342 | 0.02 |
| M-Score | −0.26592 | −0.52138 | −0.01047 | 0.04 |
PVLI - Psoas lumbar vertebral index, CI - Confidence interval, PJD - Proximal junctional disease, PJF - Proximal junctional failure, PJK - Proximal junctional kyphosis, ASA - American Society of Anesthesiology, CCI - Charlson Comorbidity Index, BMI - Body mass index, DM - Diabetes mellitus
Figure 5.
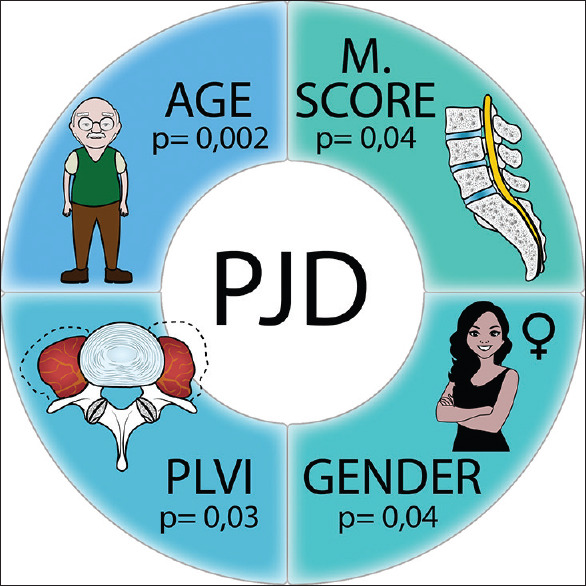
Risk factors for Proximal Junctional Disease
When considering PJF, the multivariable analysis identified age at surgery (P = 0.01), PLVI (P = 0.04), and M-score (P = 0.04) as independent risk factors [Table 2], while only PLVI and M-score were identified as independent risk factors for PJK [P = 0.02 and P = 0.04, respectively, Table 2].
DISCUSSION
The present study evaluating 308 patients who underwent posterior lumbar fusion for degenerative disease, found that low PLVI and low M-Score were significantly associated with the development of PJD (both PJK and PJF) after adjusting for other known risk factors with multivariate analysis.
Results showed that only 3.2% of the patients developed PJD, a very low percentage when compared to the current literature. In fact, the reported incidence of PJD ranges between 17% and 61.7% for PJK and between 1.4% and 31% for PJF.[14] Our data could be explained with the short number of fused levels that have been identified as a protective factor by Hyun et al.[23] Moreover, the majority of studies conducted on the incidence of PJD analyzed patients treated for adult spinal deformities[22,24] and not for lumbar degenerative diseases and it is known that this population is more prone to PJD because of long constructs, corrective maneuvers, often nonphysiological postoperative spinal alignment, and frequent fixation to the pelvis, all common risk factors for PJK and PJF.[14,22,25,26]
The role of sarcopenia as an independent risk factor for PJD has already been studied by two authors,[8,13] whose results are in line with ours. Kim and Iyer, Kim et al.[8,14] found a significant association between the thoracolumbar back muscle volume and the incidence of PJK. However, they did not perform a multivariate analysis and therefore did not adjust their result for other risk factors such as BMI or age. On the other hand, Eleswarapu et al.[13] performed a multivariate analysis, but they included all adult patients (>18 years) without an upper age limit: this could represent a bias due to the inability to distinguish sarcopenia as a pathological entity from the loss of muscle mass due to senescence. Moreover, both studies were conducted on a low number of patients (49 and 32, respectively) who all underwent surgery for spinal deformities.
As for osteopenia, it resulted to be an independent risk factor for PJD in our cohort. This is in line with the results of other authors. Elarjani et al. identified osteopenia as the only risk factor with a statistically significant correlation with PJK in 121 patients requiring revision surgery.[27] Furthermore, Kim et al.[14] found that patients with osteoporosis are twice as likely as others to develop PJD.
Even if our results individually are not new, this is the first study to analyze the relationship of sarcopenia and osteopenia together. Moreover, it confirmed the reliability of PLVI and M-score as a measure of the two clinical entities. These two scores that can be easily and simply measured on the preoperative MRI performed by each patient may help the surgeon and the patient to weigh the risks and benefits of surgery. In case of low scores, preoperative strategies aimed at optimizing bone density and muscle mass (such as perioperative teriparatide, exercise, and adequate nutrition), as well as possible intraoperative vertebral augmentation, may be adopted to mitigate fracture risk.
There are several limitations to this study. First, its retrospective design, thus precluding to the authors’ ability to demonstrate a causative link between sarcopenia, osteopenia, and PJD. Then, PLVI and M-score were the only measurements of sarcopenia and osteopenia. In fact, adding central measurement as muscle strength, physical performance, and dual X-ray absorptiometry was not possible in a retrospective study. Therefore, prospective studies are required for verifying our results. However, this study also has strengths, i.e. a long follow-up, a multivariate analysis, and easily reproducible measures. Finally, the strict inclusion criteria and the low number of fused levels exclude many of the surgery-related risk factors for PJD.
CONCLUSIONS
Sarcopenia and osteopenia, as measured by PLVI and M-score, proved to be independent risk factors for PJD in patients who undergo lumbar fusion for degenerative diseases.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ebbeling L, Grabo DJ, Shashaty M, Dua R, Sonnad SS, Sims CA, et al. Psoas: Lumbar vertebra index: Central sarcopenia independently predicts morbidity in elderly trauma patients. Eur J Trauma Emerg Surg. 2014;40:57–65. doi: 10.1007/s00068-013-0313-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tobert DG, Antoci V, Patel SP, Saadat E, Bono CM. Adjacent segment disease in the cervical and lumbar spine. Clin Spine Surg. 2017;30:94–101. doi: 10.1097/BSD.0000000000000442. [DOI] [PubMed] [Google Scholar]
- 3.Bridwell KH, Lenke LG, Cho SK, Pahys JM, Zebala LP, Dorward IG, et al. Proximal junctional kyphosis in primary adult deformity surgery: Evaluation of 20 degrees as a critical angle. Neurosurgery. 2013;72:899–906. doi: 10.1227/NEU.0b013e31828bacd8. [DOI] [PubMed] [Google Scholar]
- 4.Maruo K, Arizumi F, Kusuyama K, Yoshie N, Tomoyuki K, Tachibana T. Comparison of clinical outcomes after transforaminal interbody fusion using cortical bone trajectory versus percutaneous pedicle screw fixation. World Neurosurg. 2021;151:e821–7. doi: 10.1016/j.wneu.2021.04.130. [DOI] [PubMed] [Google Scholar]
- 5.Cahill PJ, Wang W, Asghar J, Booker R, Betz RR, Ramsey C, et al. The use of a transition rod may prevent proximal junctional kyphosis in the thoracic spine after scoliosis surgery: A finite element analysis. Spine (Phila Pa 1976) 2012;37:E687–95. doi: 10.1097/BRS.0b013e318246d4f2. [DOI] [PubMed] [Google Scholar]
- 6.Hart R, McCarthy I, O’brien M, Bess S, Line B, Adjei OB, et al. Identification of decision criteria for revision surgery among patients with proximal junctional failure after surgical treatment of spinal deformity. Spine (Phila Pa 1976) 2013;38:E1223–7. doi: 10.1097/BRS.0b013e31829fedde. [DOI] [PubMed] [Google Scholar]
- 7.Hart RA, McCarthy I, Ames CP, Shaffrey CI, Hamilton DK, Hostin R. Proximal junctional kyphosis and proximal junctional failure. Neurosurg Clin N Am. 2013;24:213–8. doi: 10.1016/j.nec.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 8.Kim HJ, Iyer S. Proximal junctional kyphosis. J Am Acad Orthop Surg. 2016;24:318–26. doi: 10.5435/JAAOS-D-14-00393. [DOI] [PubMed] [Google Scholar]
- 9.Cruz-Jentoft AJ, Landi F, Schneider SM, Zúñiga C, Arai H, Boirie Y, et al. Prevalence of and interventions for sarcopenia in ageing adults: A systematic review. Report of the international sarcopenia initiative (EWGSOP and IWGS) Age Ageing. 2014;43:748–59. doi: 10.1093/ageing/afu115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Puvanesarajah V, Jain A, Kebaish K, Shaffrey CI, Sciubba DM, De la Garza-Ramos R, et al. Poor nutrition status and lumbar spine fusion surgery in the elderly: Readmissions, complications, and mortality. Spine (Phila Pa 1976) 2017;42:979–83. doi: 10.1097/BRS.0000000000001969. [DOI] [PubMed] [Google Scholar]
- 11.Babu JM, Kalagara S, Durand W, Antoci V, Deren ME, Cohen E. Sarcopenia as a risk factor for prosthetic infection after total hip or knee arthroplasty. J Arthroplasty. 2019;34:116–22. doi: 10.1016/j.arth.2018.09.037. [DOI] [PubMed] [Google Scholar]
- 12.Gibbons D, Ahern DP, Curley AE, Kepler CK, Butler JS. Impact of sarcopenia on degenerative lumbar spondylosis. Clin Spine Surg. 2021;34:43–50. doi: 10.1097/BSD.0000000000001047. [DOI] [PubMed] [Google Scholar]
- 13.Eleswarapu A, O’Connor D, Rowan FA, Van Le H, Wick JB, Javidan Y, et al. Sarcopenia is an independent risk factor for proximal junctional disease following adult spinal deformity surgery. Global Spine J. 2022;12:102–9. doi: 10.1177/2192568220947050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim HJ, Bridwell KH, Lenke LG, Park MS, Ahmad A, Song KS, et al. Proximal junctional kyphosis results in inferior SRS pain subscores in adult deformity patients. Spine (Phila Pa 1976) 2013;38:896–901. doi: 10.1097/BRS.0b013e3182815b42. [DOI] [PubMed] [Google Scholar]
- 15.Dial BL, Hills JM, Smith JS, Sardi JP, Lazaro B, Shaffrey CI, et al. The impact of lumbar alignment targets on mechanical complications after adult lumbar scoliosis surgery? Eur Spine J. 2022;31:1573–82. doi: 10.1007/s00586-022-07200-3. doi: 10.1007/s00586-022-07200-3. [DOI] [PubMed] [Google Scholar]
- 16.Greco EA, Pietschmann P, Migliaccio S. Osteoporosis and sarcopenia increase frailty syndrome in the elderly. Front Endocrinol (Lausanne) 2019;10:255. doi: 10.3389/fendo.2019.00255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reginster JY, Beaudart C, Buckinx F, Bruyère O. Osteoporosis and sarcopenia: Two diseases or one? Curr Opin Clin Nutr Metab Care. 2016;19:31–6. doi: 10.1097/MCO.0000000000000230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tagliaferri C, Wittrant Y, Davicco MJ, Walrand S, Coxam V. Muscle and bone, two interconnected tissues. Ageing Res Rev. 2015;21:55–70. doi: 10.1016/j.arr.2015.03.002. [DOI] [PubMed] [Google Scholar]
- 19.Girgis CM, Mokbel N, Digirolamo DJ. Therapies for musculoskeletal disease: Can we treat two birds with one stone? Curr Osteoporos Rep. 2014;12:142–53. doi: 10.1007/s11914-014-0204-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mikula AL, St Jeor JD, Naylor RM, Bernatz JT, Patel NP, Fogelson JL, et al. Teriparatide treatment increases hounsfield units in the thoracic spine, lumbar spine, sacrum, and ilium out of proportion to the cervical spine. Clin Spine Surg. 2021;34:E370–6. doi: 10.1097/BSD.0000000000001203. [DOI] [PubMed] [Google Scholar]
- 21.Saad MM, Ahmed AT, Mohamed KE, Habba MR. Role of lumbar spine signal intensity measurement by MRI in the diagnosis of osteoporosis in post-menopausal women. Egypt J Radiol Nucl Med. 2019;50:35. https://doi.org/10.1186/s43055-019-0046-3. [Google Scholar]
- 22.Glattes RC, Bridwell KH, Lenke LG, Kim YJ, Rinella A, Edwards C., 2nd Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: Incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976) 2005;30:1643–9. doi: 10.1097/01.brs.0000169451.76359.49. [DOI] [PubMed] [Google Scholar]
- 23.Hyun SJ, Lee BH, Park JH, Kim KJ, Jahng TA, Kim HJ. Proximal junctional kyphosis and proximal junctional failure following adult spinal deformity surgery. Korean J Spine. 2017;14:126–32. doi: 10.14245/kjs.2017.14.4.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mendoza-Lattes S. Proximal junctional kyphosis and proximal junctional failure following spinal deformity surgery. Tech Orthop. 2021;36:1. [Google Scholar]
- 25.Maruo K, Ha Y, Inoue S, Samuel S, Okada E, Hu SS, et al. Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine (Phila Pa 1976) 2013;38:E1469–76. doi: 10.1097/BRS.0b013e3182a51d43. [DOI] [PubMed] [Google Scholar]
- 26.Yolcu YU, Zreik J, Alvi MA, Wanderman NR, Carlson BC, Nassr A, et al. Use of teriparatide prior to lumbar fusion surgery lowers two-year complications for patients with poor bone health. Clin Neurol Neurosurg. 2020;198:106244. doi: 10.1016/j.clineuro.2020.106244. [DOI] [PubMed] [Google Scholar]
- 27.Elarjani T, Basil GW, Kader MZ, Pinilla Escobar V, Urakov T, Wang MY, et al. A single institution experience with proximal junctional kyphosis in the context of existing classification schemes – Systematic review. J Clin Neurosci. 2021;88:150–6. doi: 10.1016/j.jocn.2021.03.031. [DOI] [PubMed] [Google Scholar]