Abstract
Objective
The annual American College of Medical Informatics (ACMI) symposium focused discussion on the national public health information systems (PHIS) infrastructure to support public health goals. The objective of this article is to present the strengths, weaknesses, threats, and opportunities (SWOT) identified by public health and informatics leaders in attendance.
Materials and Methods
The Symposium provided a venue for experts in biomedical informatics and public health to brainstorm, identify, and discuss top PHIS challenges. Two conceptual frameworks, SWOT and the Informatics Stack, guided discussion and were used to organize factors and themes identified through a qualitative approach.
Results
A total of 57 unique factors related to the current PHIS were identified, including 9 strengths, 22 weaknesses, 14 opportunities, and 14 threats, which were consolidated into 22 themes according to the Stack. Most themes (68%) clustered at the top of the Stack. Three overarching opportunities were especially prominent: (1) addressing the needs for sustainable funding, (2) leveraging existing infrastructure and processes for information exchange and system development that meets public health goals, and (3) preparing the public health workforce to benefit from available resources.
Discussion
The PHIS is unarguably overdue for a strategically designed, technology-enabled, information infrastructure for delivering day-to-day essential public health services and to respond effectively to public health emergencies.
Conclusion
Most of the themes identified concerned context, people, and processes rather than technical elements. We recommend that public health leadership consider the possible actions and leverage informatics expertise as we collectively prepare for the future.
Keywords: public health informatics, information systems, population health, sociological factors, public policy, information technology
BACKGROUND AND SIGNIFICANCE
Public health information systems (PHIS), defined as systems designed to manage public health data,1,2 are critical for appropriate response to emerging health threats. PHIS also include those systems that handle data related to the activities of public health programs and health departments. As an integrated effort, PHIS may be leveraged to improve health outcomes, inform public health interventions, and influence policymaking and decision-making. While the 2009 Health Information Technology for Economic and Clinical Health (HITECH) Act advanced digital health technologies and interoperability across clinical data systems, the nation’s PHIS did not receive similar support nor benefit from the digital modernization efforts despite being invoked in Meaningful Use standards.3 Limitations in the nation’s PHIS were known and documented prior to the COVID-19 pandemic3–7 and existed throughout.8 In 2020, the Centers for Disease Control and Prevention (CDC) launched a Data Modernization Initiative (DMI) with the intent to create a connected, sustainable, and response-ready system capable of supporting ongoing public health surveillance needs.9 Despite this knowledge and the DMI efforts, the COVID-19 pandemic further exposed fragilities in the nation’s PHIS and gaps in digital connectivity and information required for decision-making, all of which can endanger population health and promote health inequities.10,11 The events of COVID-19 have been surprising but not novel to public health. Now is the time to develop a nationwide strategy based on a diagnosis of the challenges faced during this global crisis.12–15
A robust infrastructure is required to provision “information for action.”4 To prepare for the next acute health crisis, and manage ongoing threats from chronic conditions (eg, cardiovascular disease and diabetes), deficits must be addressed. Designing and building an effective PHIS infrastructure requires diverse expertise. Public health domain experts have extensive knowledge and experience in the science and essential services of carrying out the mission of public health “to protect and promote the health of all people in all communities” but often have limited informatics expertise.16 Conversely, clinical informatics domain experts often have limited public health experience but extensive knowledge and experience in the theory and pragmatics of building clinical information systems. Leveraging the experience and lessons learned among the biomedical informatics community may save time and effort, avoiding mistakes made in the clinical environment and waste of public health resources.
Recognizing this need and opportunity, the American College of Medical Informatics (ACMI) chose to focus its 2022 Annual Symposium on enhancing the national PHIS infrastructure to support public health goals. The objective of this article is to present the strengths, weaknesses, threats, and opportunities identified by leaders in public health and informatics attending the Symposium held in April 2022. The findings provide an organized perspective of the forces at work, a critical strategic planning element, to guide a cohesive response that meets local to national public health infrastructure goals.
MATERIALS AND METHODS
The 2022 ACMI Annual Symposium was planned by a committee of 6 ACMI members with expertise in public health informatics, who defined the meeting goals, identified experts from national, state/local, and nonprofit public health organizations, and facilitated the meeting. An overarching goal of the meeting was to summarize key questions and issues related to the nation’s PHIS, from various stakeholder perspectives, to imagine a future, modern infrastructure that meets public health needs.
Conceptual frameworks
A Strengths, Weaknesses, Opportunities, and Threats (SWOT) framework was used to describe the current ability of the nation’s PHIS to meet public health goals.17 These domains were used to guide breakout sessions and to classify findings. The presence of weaknesses and threats represent gaps to be addressed in planning, while the absence of strengths or opportunities clarify needs before action can be taken. “Internal capabilities” may be “strengths” or “weaknesses” and are within the control of the organization towards the end goal (eg, governance, resources, funding, culture). The organization, or internal stakeholders, was defined as public health agencies and partner organizations. “External capabilities” may be “opportunities” or “threats” and are those that the organization does not directly control (eg, political environment, technology development, competing organizations, quality of partnerships). We considered health information exchange (HIE) networks both internal and external entities with respect to the SWOT analysis because PHIS vary by jurisdiction as does the role of HIE. The level of integration and functionality of HIE networks ranges from an integral partner within public health organizations, to an adjacent organization that manages components of health information for public health goals, to limited collaboration with one another.18
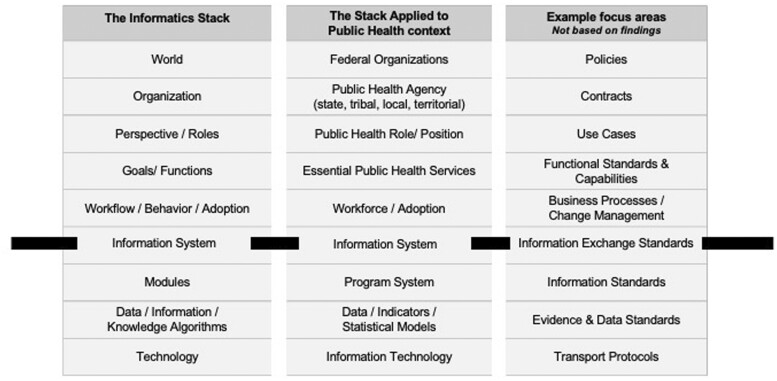
The Informatics Stack (Stack) framework was used to organize the SWOT findings.19 The Stack provides a heuristic framework that embodies a systems perspective where one level communicates to other levels only through intermediary levels (Figure 1).20 One organizing principle of the Stack is the socio-technical perspective, referring to the interrelatedness of social and technical aspects of an organization.21,22 In short, human and organizational factors are as important as technical issues with regards to system effectiveness. Human, organizational, and technical elements should have a mutual alignment or “fit” to ensure successful PHIS implementation.23 The top of the Stack concerns context, people, and processes, critical components of the information infrastructure that exist above the Information System level. The bottom of the Stack concerns technical functionalities for PHIS that exist below the Information System level. The “line” separating the top and the bottom of the Stack is within the Information Systems level. It is useful to further classify the identified SWOT factors as Above or Below the line to understand where to direct resources.
Figure 1.
The Informatics Stack applied to the public health context with example focus areas not based on findings.
Pre-Symposium activities
Before the Symposium, 4 major activities occurred. First, the program committee presented a webinar to share history and known challenges with the nation’s PHIS. The goal was to level-set prior to the meeting so attendees would come prepared with a shared understanding of historical and current challenges to PHIS in the wake of the COVID-19 pandemic. Second, 4 types of attendees were invited to participate in the Symposium. All ACMI members were invited, representing a college of peer-elected fellows who have made significant and sustained contributions to the field of biomedical informatics. ACMI members could invite a guest with expertise in the Symposium topic. Three doctoral students with expertise in public health and informatics were invited by the program committee. Finally, the program committee invited public health and informatics leaders representing key national public health organizations. No explicit effort was made to ensure balanced representation from academia, industry, and governmental/nonprofit organizations. The settings represented by the attendees were assigned using self-reported information in ACMI profiles and meeting registration files. Three “industry” entries were ignored because they always co-occurred with “health system or hospital.”
Third, invited speakers were asked to consider meeting participants as a think tank and to formulate their presentation to generate discussion. They were asked to share the perspectives of their constituents across specific subject areas, including their greatest pain points, future modernization plans, barriers to accomplishing next steps, and successful collaborations between partners and information technology experts.
Fourth, the Program Committee and doctoral students met weekly to develop the data collection and organization strategy in preparation for postsymposium qualitative analysis. One student (JA) led the team with a goal to ensure all data was collected and managed as planned. Data collection involved 3 primary artifacts: a SWOT breakout session facilitation guide and documentation template, a structured notetaking template, and an electronic shared meeting repository for presentations and other meeting artifacts. To reduce potential bias in data collection, the notetaking template was designed to capture all works and perspectives rather than summarize discussion. The notetaking template was organized by sections for each day. The template included: (1) the day’s agenda, (2) instructions about what to document and reminders to tag content by SWOT domain during the meeting, (3) link to an attendee list for reference, (4) links to presentation materials, (5) space to document presentation key points, and (6) space to document discussion, questions, answers, and any follow-up actions as verbatim as possible.
Symposium
The 3-day in-person Symposium provided a highly focused venue for experts to convene in a casual environment for robust discussion of PHIS challenges and solutions as the nation navigates a postpandemic world. The meeting was intentionally not recorded to encourage participants to speak freely and openly about their perspectives. There was no voting or effort to achieve consensus during any part of the meeting.
The Symposium included 8 presentations over the course of 2 days with ample time for group discussion. Day 1 content focused on the national and jurisdictional perspective, including presentations and discussion, and a SWOT-focused breakout session held at the end of Day 1 with a goal to identify internal and external factors that impact rebuilding of the nation’s PHIS infrastructure. Prior to group work, attendees were provided with a working definition of the SWOT analysis framework and were randomly assigned to 1 of the 4 breakout groups targeting an individual SWOT domain based on a tag under their chair. Each group was moderated by a program committee member using the SWOT analysis framework as a facilitation guide and included no more than 10 individuals and a notetaker. Day 2 content focused on HIE and the community organization perspective. Day 3 focused on meeting reflections and recommendations for next steps.
Information from the presentations and discussions were captured by 3 authors (JA, KA, JH), as designated notetakers, using the structured notetaking template to standardize data collection throughout the Symposium. Information from the Day 1 SWOT breakout session was captured in the SWOT-specific documentation template and included the raw discussion by session participants and the summary of SWOT factors presented to the larger group.
Post-Symposium synthesis
After the symposium, authors communicated regularly using synchronous and asynchronous communication, including email and weekly virtual meetings to review and discuss results via cloud-based video conferencing services. All files were managed using a shared electronic repository.
Notetakers prepared information for thematic analysis, including data cleaning steps to correct or delete irrelevant comments and prepare the files for synthesis. Each notetaker’s documents were kept separate during this process. The structured notetaking templates were analyzed by each notetaker independently and manually coded to identify content specific to their assigned SWOT domain. For example, the notetaker assigned to “opportunity” reviewed notes from each day, tagged keywords appropriate for the “opportunity” domain17 and assigned a reference number if there were follow-up questions. One notetaker (JA) covered 2 SWOT domains (Opportunities and Threats).
To classify factors by SWOT domain, the team initially used factors generated from the SWOT-based breakout session documentation. Then, each notetaker supplemented the factors for their assigned domain based on their structured notes, including content from the full meeting agenda. One notetaker (JA) reviewed all documentation materials to generate the final summary of factors for each SWOT domain. As appropriate, factors were merged within SWOT domains. The SWOT-classified factors were then reviewed and reconciled by all authors, requiring only minor modifications.
To characterize SWOT-specific factors along levels of the Stack, authors loosely adapted thematic analysis methods.24 First, we assigned each factor to a level of the Stack. Then, we grouped factors into relevant themes. Draft results were shared with all authors and enhanced through an iterative process until no further edits were recommended. Through this process, factors were merged within SWOT domains, themes were enhanced, and conflicts were resolved by further discussion with all authors.
The Indiana University Institutional Review Board determined this effort is not human subjects research and did not require approval (Protocol No. 15218).
RESULTS
Participants
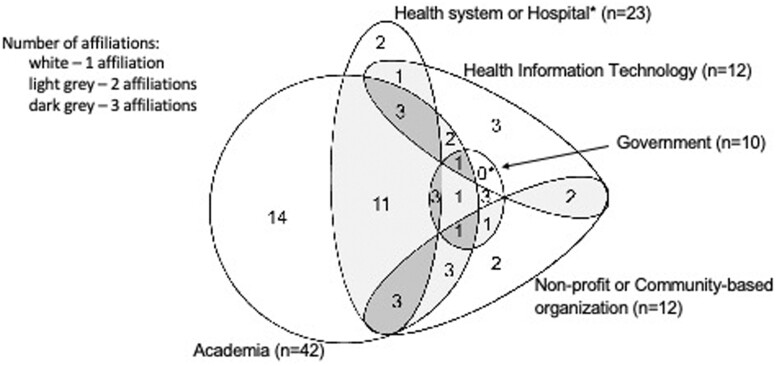
The Symposium was attended by 56 participants, including 41 elected ACMI fellows, 8 invited guests of an ACMI member (including the 3 notetakers), and 7 invited public health and informatics domain experts. Attendees represented a range of public health and clinical informatics experience with a baseline of no less than 10 years of expertise in their reported affiliations, including academia (75%), health system or hospital (41%), health information technology (21%), nonprofit or community-based organization (21%), or government (18%). Over half (57%) of the attendees reported more than one relevant affiliation (Figure 2). The 8 experts invited to present (which included one ACMI member) were all leaders in their organization or field of expertise, including leaders from the CDC, the Office of the National Coordinator for Health Information Technology (ONC), Council of State and Territorial Epidemiologists (CSTE), Association of State and Territorial Health Officials (ASTHO), Public Health Informatics Institute (PHII), Illinois Public health Institute, Contexture, and the Indiana Health Information Exchange.
Figure 2.
Distribution of the professional settings reported by ACMI Symposium attendees (n = 56).
Summary of findings
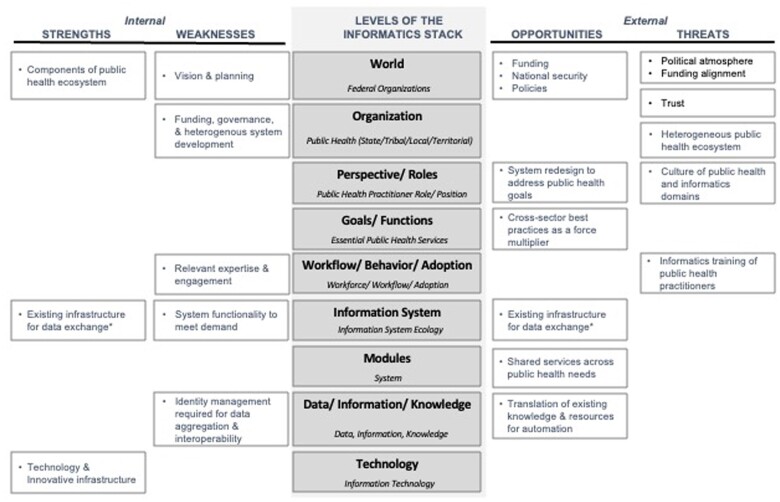
A total of 57 unique SWOT factors related to the current PHIS were identified by Symposium attendees (Table 1), including 9 strengths, 22 weaknesses, 14 opportunities, and 14 threats. The 57 SWOT factors were consolidated into 22 overarching themes according to levels of the Stack (Figure 3). For example, 3 out of 9 strengths were grouped into one theme and level of the Stack—World. Almost 4 times as many themes are clustered at the top of the Stack—concerning context, people, and processes—as opposed to the bottom of the Stack concerning technical issues (n = 15 vs 4). Three themes are on the line at the level of the Information System (Table 2).
Table 1.
Summary of the strengths, weaknesses, opportunities, and threats, organized by Informatics Stack level and themes of the nation’s public health information systemsa, as expressed by ACMI Symposium participants in April 2022
| Domain | Stack level | Theme | SWOT factors |
|---|---|---|---|
| Strengths |
|
Components of the public health ecosystem |
|
|
Existing infrastructures for data exchange |
|
|
|
Technology and innovative infrastructure |
|
|
| Weaknesses |
|
Vision and planning |
|
|
Funding, governance, and heterogenous system development |
|
|
|
Relevant expertise and engagement |
|
|
|
System functionality to meet demand |
|
|
|
Identity management for data aggregation and interoperability |
|
|
| Opportunities |
|
Funding | 30.Influx of historic-level funding |
| National security | 31.A robust infrastructure around health information exchange and public health has implications for national security | ||
| Policies | 32.Explore federal policies that support state-designated health information exchange/health data utility partnerships to create public health assurances as well as policies that compel healthcare/providers to contribute their data where appropriate (eg, Prescription Drug Monitoring Program federal prescription hub, All payer database with public health agency accessibility to the data) | ||
|
System redesign to address public health goals | 33.Paradigm shift for how to collect, use, and share data for the purposes of bidirectional exchange as opposed to government mandates | |
|
Cross-sector best practices as a force multiplier |
|
|
|
Existing infrastructure for data exchange |
|
|
|
Shared services across public health needs | 41.Tools built for COVID-19 can be leveraged for future emerging threats and public health functions | |
|
Translation of existing knowledge and resources for automation |
|
|
| Threats |
|
Political atmosphere |
|
| Funding alignment |
|
||
| World and Organizationb | Trust |
|
|
|
Heterogenous public health ecosystem |
|
|
|
Culture of public health and informatics domains |
|
|
|
Informatics training of public health practitioners |
|
Assuming the public health information systems infrastructure includes functionality for clinical data exchange given that health information exchanges are part of the public health information ecosystem in some jurisdictions.
Trust spans 2 levels of the Stack: World and Organization.
Figure 3.
Summary of themes concerning the nation’s public health information systems, organized by levels of the informatics Stack and identified strengths, weaknesses, opportunities, and threats.
Table 2.
Distribution of themes by SWOT factor and Informatics Stack level
| Informatics Stack level | SWOT domain |
Total | |||
|---|---|---|---|---|---|
| Strength | Weakness | Opportunity | Threat | ||
| Theme count | |||||
| World | 1 | 1 | 3 | 3a | 8 |
| Organization | 0 | 1 | 0 | 1 | 2 |
| Perspective/Roles | 0 | 0 | 0 | 1 | 1 |
| Goals/Functions | 0 | 0 | 1 | 0 | 1 |
| Workflow/Behavior/Adoption | 0 | 1 | 1 | 1 | 3 |
| Information Systems | 1 | 1 | 1 | 0 | 3 |
| Modules | 0 | 0 | 1 | 0 | 1 |
| Data/Information/Knowledge Algorithms | 0 | 1 | 1 | 0 | 2 |
| Technology | 1 | 0 | 0 | 0 | 1 |
| Total | 3 | 5 | 8 | 6 | 22 |
One theme, Trust, spans 2 levels of the Stack: World and Organization. For the purpose of this table, the count for Trust is included in the level of the World.
Strengths
The 3 internal strengths identified were distributed above, on, and below the line. Regarding World, attendees noted strengths within the larger public health ecosystem, including the CDC’s robust and centralized national presence, a highly dedicated workforce, and increased national awareness and dialogue surrounding the need for expanded data for public health purposes (eg, social determinants of health) to be a strength of the current public health environment. Regarding Information Systems, attendees frequently mentioned that established public-private partnerships and HIE networks serve as a potential model for the future national infrastructure and provide a source of cross-industry collaboration. Finally, regarding Technology, there are capable and robust technologies being used in the public health marketplace. However, the pathways through which these innovative technology solutions are scaled up are not well characterized to be implemented widely across the nation.
Weaknesses
The 5 internal weaknesses identified were distributed across 5 levels of the Stack, including 3 above, one on, and one below the line. Regarding World, the lack of shared vision and planning across public health and healthcare ecosystems was an area of concern. For example, clinical and public health functions are often viewed as distinct rather than complementary—each function interacting only when necessary. As data collected in the healthcare setting are captured primarily for clinical purposes, those data do not always fully meet the needs of public health. Regarding Organization, despite the centralized presence of the CDC being named as a strength, the siloed and decentralized structure, funding, and authority models of public health agencies reoccurred during discussions around weaknesses. Participants perceived that this fragmentation leads to financial and infrastructural inefficiencies through the forced re-creation of systems specific to one of many statutory public health programs. Regarding Workflow/Behavior/Adoption, participants discussed the varying jurisdictional informatics capacities, inadequate stakeholder engagement, and inaccessible informatics resources as an additional challenge as the nation looks toward interjurisdictional interoperability and reporting.
Regarding Information Systems, a presentation given on the anticipated North Star architecture, a joint ONC-CDC public health data infrastructure effort for state, territorial, local, and tribal (STLT) public health agencies to share data with each other and the CDC, described an integrated block architecture, with flexible but standardized support levels for STLT partners, a secure cloud environment, and governance policies to promote collaboration and transparency.25,26 Several stakeholders expressed worry that this architecture would reduce public health capacity to the “least common denominator,” rather than increase capacity. The group voiced concerns about the limitations of the planned architecture, including the lack of bidirectional exchange with healthcare and a master person index, an electronic database that maintains a unique index identifier for individuals across separate clinical, financial, and administrative services.27 Additionally, participants felt the active disbursement of funds and aggressive timeline for the data modernization initiative and North Star architecture was likely a weakness to the success of its implementation.9 Participants also discussed the forced secondary data use of clinical data for public health purposes, which often requires additional investigation to capture relevant context outside the healthcare setting. Further, continued investment in development of real-time data and bidirectional communication infrastructure and methods was discussed as necessary to enable public health agencies to participate in delivering up-to-date, actionable decision support for timely day-to-day practice, public health intervention, and enhanced clinical care.28
Finally, regarding Data, Information, and Knowledge, the lack of effective patient identity management in an ecosystem of siloed infrastructures has led to the loss of the longitudinal perspective necessary for public health to understand and respond effectively to evolving threats within a community, especially in real time.
Opportunities
The 8 external opportunities identified were distributed across 6 levels of the Stack, including 5 above, 1 on, and 2 below the line. Three overarching opportunities were especially prominent: (1) addressing the needs for sustainable funding, (2) leveraging existing infrastructure and processes for information exchange and system development that meets public health goals, and (3) preparing the public health workforce to benefit from available resources.
Opportunities for sustainable funding concerned the World. Discussion focused around the historic-level influx of funding in the wake of COVID-19 pandemic and that it should be leveraged to facilitate national strategy and made sustainable to address many of the aforementioned SWOT factors. Participants discussed the opportunity to reframe the need to strengthen the nation’s public health infrastructure as a national security issue—which would enable coordination of funding and effort across the federal government beyond health agencies.
Opportunities to leverage existing expertise and infrastructure for information exchange spanned the Stack. Participants discussed the emergence of a paradigm shift in the public health environment for system redesign to meet public health goals (at the level of Goals/Functions). Participants discussed the opportunity to leverage processes, tools, data models, and data which are more advanced in the clinical and clinical research environments. For example, public health colleagues can leverage automated knowledge management strategies, standardized knowledge used for clinical quality, performance measurement, and clinical research, and data standards lifecycle practices. Participants noted that tools built for COVID-19 should be leveraged for future emerging threats and public health functions (at the level of Modules). In addition, participants noted the power of an HIE and/or health data utility (HDU) as proven mechanisms already in place across many jurisdictions to function as state designated enterprises in which certain levels of connectivity may be set forth in policy29,30 (at the level of Information Systems). While some exchanges have been successful without state designation, many have not, leading to piecemeal capabilities and fragmented interoperability. Designation of a specific organization by the state creates clarity, eliminates fragmentations, and enhances the ability to work with public health.18
For the public health domain to leverage these opportunities, there is a need for public health workforce development. Opportunities exist for education, training, and implementation of new best practices which may require new policies and standards related to accreditation and core competencies for all public health practitioners (at the level of Workflow/Behavior/Adoption).
Threats
The 6 external threats identified were distributed across 4 levels of the Stack, all above the line—the only SWOT domain for which this distribution occurred. Half of the themes (n = 3) concerned World. For example, throughout the symposium, participants discussed threats such as the political atmosphere of the United States, funding alignment problems, and a lack of trust in science and government among the public as a result of COVID-19 response. “Trust” was the only theme to span 2 levels of the Stack within a domain, World and Organization. The perceived lack of trust surrounding data-sharing practices among public health agencies could inhibit the pursuit of a national framework.31,32 Participants feared this threat has the potential to be compounded by political polarization. Regarding Organization, participants mentioned the heterogeneous reporting and privacy policies across jurisdictions as a potential threat. Heterogenous reporting was discussed as adding to the complexity of implementing a national PHIS infrastructure without increased understanding of the different legal approaches states apply to protect sensitive information and clear legal governance on allowable data disclosures.33 Regarding Perspective/Roles, attendees called out the cultural gaps between biomedical informatics and public health practice as a threat to PHIS, eg, historically the 2 domains diverged in mission to serve individual health needs versus population-level issues and interventions.34,35 Finally, regarding Workflow/Behavior/Adoption, the group pointed out limited venues for public health and informatics interaction, resulting in reduced opportunity for expertise cross-pollination.
DISCUSSION
The 2022 ACMI Symposium achieved its main goal to focus discussion on the nation’s PHIS ecosystem needed to support essential public health services. The US PHIS is unarguably overdue for a strategically designed, technology-driven, information infrastructure for delivering day-to-day essential public health services and to respond effectively to public health emergencies.36–38 Creating such an infrastructure is foundational to the national security. While infrastructure for robust, rapid information collection and exchange is available in some parts of the country, many policy, legal, and social barriers must be overcome before the United States as a nation can realize the full potential of this infrastructure. These opportunities and challenges were discussed throughout the Symposium and were found to mostly concern upper levels of the Stack, suggesting where US public health agencies need to focus critical resources.
The US public health system historically has been characterized as fragmented in both organization and funding sources. Funding was the only recurring theme that crossed multiple domains, including Weaknesses, Opportunities, and Threats. It is generally accepted that state, local, and county public health capabilities vary, and persistent funding gaps remain. Shortfalls highlighted during COVID-19 have led to growing awareness of the essential role of public health, and the nation’s underinvestment in this area.39 While there is an historic influx of funding directed to jurisdictions to boost COVID-19 preparedness, prevention, and response efforts, these funds cannot replace or necessarily improve on long-standing gaps in policy, funding, coordination, and communication needed to strengthen PHIS infrastructure.40 Funds should be leveraged, but they must also be sustained over time, not categorically and only in reaction to acute needs, to create common, shared infrastructure that is disease agnostic and more suited towards all essential services as opposed to individual public health Use Cases. Meeting participants discussed the concept of establishing a central Federal authority to govern shared visioning and public health informatics within the CDC, which may map out the needed overhaul of outdated public health laws and regulations. This central coordinating office could include staff with public health law expertise to review existing regulations and ensure they are relevant and legally sound to protect the health of the public. Further, the establishment of this entity would contribute to the removal of technical and legal barriers to data systems interoperability that have plagued public health while ensuring that sufficient security safeguards are in place to achieve compliance with the Health Insurance Portability and Accountability Act (HIPAA).41,42
Modernized, integrated, real-time public health data systems at every level of government will revolutionize the nation’s response to health threats, both acute and chronic. There is a clear need for a national public health data ecosystem that functions well in the interpandemic phase and can seamlessly adapt and scale for a future pandemic or other public health emergency.3 Realizing this vision will require sustained investment and guidance to state, local, tribal, and territorial health departments, the creation of advanced tools and capabilities at all levels, and the realization of best-in-class innovation with research, the private sector, and public health partners. Meeting participants discussed the opportunity to explore policies that may be used as levers to ensure the nation’s health is protected with the support of PHIS, which requires robust privacy and cybersecurity safeguards. One solution that repeatedly came up was leveraging existing heterogenous infrastructure for data exchange through formal state designation of HIE/HDU partnerships. The discussed outcome would be to simplify cooperation with federal agencies and dramatically lower barriers to exchanges serving as vital components of national interoperability. These partnerships would be regulated by the state or public-private regulatory commissions to compel technical interfaces and coordination with public health departments to enhance connectivity, which will serve the greater public health mission.43 One successful example of formal state policies is when the Maryland legislature charged the Maryland Health Care Commission and the Health Services Cost Review Commission (HSCRC) with designating a statewide HIE, a process that occurs every 3 years. This process ensures performance of the state designated HIE response to build and maintain technical infrastructure and an efficient and effective data management strategy that can support the secure statewide exchange of electronic health information for clinical and public health benefit.44 In addition, participants discussed that by framing HIE/HDU as critical for securing national health, funding, and coordination from across the federal government could be unlocked for PHIS strengthening. One participant suggested that we reframe the policy discussion to equate PHIS with national security in the same way that President Eisenhower successfully argued that interstate highways were critical infrastructure that required the full power of the federal government.
Finally, another core theme discussed throughout the Symposium was the critical need to build and support a public health workforce that is skilled in informatics and data science to establish and maintain advanced data ecosystems. This support can be accomplished by reskilling, upskilling, recruiting, and retaining a workforce with the skills to meet 21st century health threats. However, public health has historically faced notable challenges in finding and recruiting sufficient incoming talent, in educating and training the current workforce, and in weathering the high turnover rates in state and local public health for other, higher paying domains. In a recent survey of the public health workforce, ASTHO found that few health departments employ informatics specialists who can harness the power of advanced computing systems and data science techniques.45 The re-establishment of Centers of Excellence in Public Health Informatics could attract students and produce needed workers. Further, public health practitioners do not have to depend on their workforce alone. The field can leverage best practices from the healthcare community and industry. Specifically, they could require use of existing standards (eg, United States Core Data for Interoperability) when initiating digital public health reporting at all levels, and partner with informatics experts to develop open source and application programming interface-based tools that enable rapid adoption allowing for more efficient access to data for day-to-day public health work and during emergencies.
LIMITATIONS
The strengths, weaknesses, threats, and opportunities identified were generated by experts participating in the Symposium, which may have been influenced by the agenda, and may not represent all potentially available input. While experts were gathered to provide input on the topic, the findings do not represent a formal Delphi panel methodology as there was no voting or effort to achieve consensus during any part of the meeting and discussion was intentionally not recorded to encourage open participation. Results highlight the need for future research to assess the needs of the nation’s PHIS more systematically. Discussion of the “North Star” architecture was limited to what was approved for sharing by ONC and CDC at the time of the meeting. Additionally, data collection, synthesis, and interpretation of participant comments were conducted using templates and common processes among the 3 notetakers; the results were not directly provided by experts via survey or other standard data collection methodology. We attempted to use an online whiteboard to capture commentary directly from participants, but the information provided was limited in this format and not easily digestible for data synthesis. Despite these limitations, the symposium included a diverse set of experts that engaged in robust dialogue and provided descriptive and process-oriented ideas worthy of sharing.
CONCLUSION
Use of a socio-technical framework exposed current strengths and weaknesses and may guide decision-making to leverage opportunities and manage threats. Most of the informatics problems identified by public health and informatics leaders related to issues in the top of the Stack—concerning context, people, and processes—all of which are critical components of the PHIS infrastructure. We recommend that public health leadership consider the possible actions and leverage technology and informatics expertise as we collectively prepare for the future.
ACKNOWLEDGMENTS
The authors thank American College of Medical Informatics (ACMI) members for their time and expertise in developing these resources, Michelle Martin of AMIA for her excellent support throughout the planning and execution of the 2022 Symposium, the ACMI Executive Committee for their support of this viewpoint, anonymous reviewers their expertise and feedback on next steps to include a Delphi panel, and public health agencies for openly sharing their strengths and challenges to develop and implement these resources.
Contributor Information
Jessica C Acharya, Healthy Policy & Management, Informatics, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, USA.
Catherine Staes, College of Nursing, University of Utah, Salt Lake City, Utah, USA; School of Medicine, University of Utah, Salt Lake City, Utah, USA.
Katie S Allen, Department of Health Policy & Management, Richard M. Fairbanks School of Public Health, IUPUI, Indianapolis, Indiana, USA; Center for Biomedical Informatics, Regenstrief Institute, Inc., Indianapolis, Indiana, USA.
Joel Hartsell, School of Medicine, University of Utah, Salt Lake City, Utah, USA; Epi-Vant, LLC., Salt Lake City, Utah, USA.
Theresa A Cullen, Center for Biomedical Informatics, Regenstrief Institute, Inc., Indianapolis, Indiana, USA; Pima County Public Health Department, Tucson, Arizona, USA.
Leslie Lenert, Department of Medicine, Medical University of South Carolina, Charleston, South Carolina, USA; Health Sciences South Carolina, Charleston, South Carolina, USA.
Donald W Rucker, 1upHealth, Boston, Massachusetts, USA; Department of Emergency Medicine, Ohio State University, Columbus, Ohio, USA.
Harold P Lehmann, Department of Medicine, Johns Hopkins School of Medicine, Baltimore, Maryland, USA.
Brian E Dixon, Department of Health Policy & Management, Richard M. Fairbanks School of Public Health, IUPUI, Indianapolis, Indiana, USA; Center for Biomedical Informatics, Regenstrief Institute, Inc., Indianapolis, Indiana, USA.
FUNDING
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
AUTHOR CONTRIBUTIONS
All authors provided substantial contribution to the design and execution of the 2022 ACMI Symposium. JA drafted the manuscript. All authors revised it critically for important intellectual content and approved the final version for publication.
CONFLICT OF INTEREST STATEMENT
None declared.
DATA AVAILABILITY
This manuscript leveraged original data generated from the 2022 ACMI Symposium. Given the nature of the data, it is not available for access.
REFERENCES
- 1. National Institute of Standards and Technology. Glossary: Health Information System. MD, USA: National Institute of Standards and Technology. https://csrc.nist.gov/glossary?index=H. Accessed October 15, 2022.
- 2. Brook C. What is a Health Information System? Data Protection 101. MN, USA: Digital Guardian; 2018. https://digitalguardian.com/blog/what-health-information-system#:~:text=A%20health%20information%20system%20%28HIS%29%20refers%20to%20a,management%20or%20a%20system%20supporting%20healthcare%20policy%20decisions. Accessed October 1, 2022.
- 3. Lee P, Abernethy A, Shaywitz D, et al. ; Microsoft. Digital health COVID-19 impact assessment: lessons learned and compelling needs. NAM Perspect 2022. https://nam.edu/digital-health-covid-19-impact-assessment-lessons-learned-and-compelling-needs/. Accessed September 13, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. DeSalvo K, Hughes B, Bassett M, et al. Public health COVID-19 impact assessment: lessons learned and compelling needs. NAM Perspect 2021. https://nam.edu/public-health-covid-19-impact-assessment-lessons-learned-and-compelling-needs/. Accessed September 13, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hurst D, Sharpe S, Yeager VA.. Administrative preparedness strategies: expediting procurement and contracting cycle times during an emergency. Public Health Rep 2017; 132 (3): 294–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Stoto MA, Nelson C, Higdon MA, Kraemer J, Hites L, Singleton CM.. Lessons about the state and local public health system response to the 2009 H1N1 pandemic: a workshop summary. J Public Health Manag Pract 2013; 19 (5): 428–35. [DOI] [PubMed] [Google Scholar]
- 7. Yeager VA, Hurst D, Menachemi N.. State barriers to appropriating public health emergency response funds during the 2009 H1N1 response. Am J Public Health 2015; 105 (S2): S274–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Walker DM, Yeager VA, Lawrence J, McAlearney AS.. Identifying opportunities to strengthen the public health informatics infrastructure: exploring hospitals’ challenges with data exchange. Milbank Q 2021; 99 (2): 393–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. The Centers for Disease Control and Prevention (CDC). Data Modernization Initiative. Better Data. Better Decisions. Better Health. Atlanta, GA: CDC; 2022. https://www.cdc.gov/surveillance/data-modernization/index.html. Accessed October 15, 2022.
- 10. Dixon BE, Caine VA, Halverson PK.. Deficient response to COVID-19 makes the case for evolving the public health system. Am J Prev Med 2020; 59 (6): 887–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Robert Wood Johnson Foundation. Charting a Course for an Equity-Centered Data System. NJ, USA: RWJF; 2021. https://www.rwjf.org/en/library/research/2021/10/charting-a-course-for-an-equity-centered-data-system.html. Accessed September 13, 2022.
- 12. Mallon WT. Does strategic planning matter? Acad Med 2019; 94 (10): 1408–11. [DOI] [PubMed] [Google Scholar]
- 13. Porter M. The Five Competitive Forces That Shape Strategy. Harvard Business Review. MA, USA: HBR; 2008. https://hbr.org/2008/01/the-five-competitive-forces-that-shape-strategy. Accessed October 15, 2022. [PubMed] [Google Scholar]
- 14. Vining AR. Public agency external analysis using a modified “five forces” framework. Int Public Manag J 2011; 14 (1): 63–105. [Google Scholar]
- 15. Rumelt R. Strategy in a ‘structural break’. McKinsey Q 2009; 1: 1–37. https://www.mckinsey.com/capabilities/strategy-and-corporate-finance/our-insights/strategy-in-a-structural-break#/. [Google Scholar]
- 16. Centers for Disease Control and Prevention. 10 Essential Public Health Services. Public Health Professionals Gateway. Atlanta, GA: CDC; 2022. https://www.cdc.gov/publichealthgateway/publichealthservices/essentialhealthservices.html. Accessed October 1, 2022.
- 17. The Centers for Disease Control and Prevention (CDC). Do a SWOT Analysis. Public Health Professionals Gateway. Atlanta, GA: CDC; 2021. https://www.cdc.gov/publichealthgateway/phcommunities/resourcekit/evaluate/do-a-swot-analysis.html. Accessed September 13, 2022.
- 18. Horrocks D. HIEs are Vital to Public Health, But Need Reshaping. Healthcare Information and Management Systems Society. IL, USA: HIMSS; 2020. https://www.himss.org/resources/hies-are-vital-public-health-need-reshaping. Accessed October 2022.
- 19. Lehmann H. The informatics stack: a heuristic tool for informatics teaching. Methods Inf Med 2017; 56 (S 01): e129–33. [Google Scholar]
- 20. Glaser JP. The role of the chief information officer in the health care organization in the 1990s. Top Health Inf Manage 1993; 13 (3): 62–8. [PubMed] [Google Scholar]
- 21. Whetton S. Health Informatics: A Socio-Technical Perspective. Oxford; New York: Oxford University Press; 2005: 262p. [Google Scholar]
- 22. Novak LL, Holden RJ, Anders SH, Hong JY, Karsh BT.. Using a sociotechnical framework to understand adaptations in health IT implementation. Int J Med Inform 2013; 82 (12): e331–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Yusof M, Kuljis J, Papazafeiropoulou A, Stergioulas LK.. An evaluation framework for Health Information Systems: human, organization and technology-fit factors (HOT-fit). Int J Med Inform 2008; 77 (6): 386–98. [DOI] [PubMed] [Google Scholar]
- 24. Braun V, Clarke V.. Thematic Analysis: A Practical Guide . London; Thousand Oaks, California: SAGE; 2022: 338p. [Google Scholar]
- 25. Miliard M. National Coordinator: TEFCA Will Enable “North Star” Architecture for Public Health. Healthcare Information and Management Systems Society. IL, USA: HIMSS. https://www.healthcareitnews.com/news/national-coordinator-tefca-will-enable-north-star-architecture-public-health. Accessed October 15, 2022.
- 26. Centers for Disease Control and Prevention. Advancing Interoperability for Public Health. North Star Architecture. Atlanta, GA: CDC; 2022. https://www.cdc.gov/surveillance/policy-standards/interoperability.html. Accessed October 15, 2022.
- 27. McFarlane TD, Dixon BE, Grannis SJ. Client registries. In: Health Information Exchange. Indiana: Elsevier; 2016: 163–82. https://linkinghub.elsevier.com/retrieve/pii/B9780128031353000116. Accessed October 2, 2022.
- 28. Dixon BE, Gamache RE, Grannis SJ.. Towards public health decision support: a systematic review of bidirectional communication approaches. J Am Med Inform Assoc 2013; 20 (3): 577–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Adler-Milstein J, Dixon BE. Chapter 16 Future Directions in Health Information Exchange. 2016. https://researcherprofiles.org/profile/225078089.
- 30. HIMSS. Expanding Health Data Utility Models and Advancing Standards for Public Health. HIMSS Interoperability & HIE Community; 2022. https://www.himss.org/resources/expanding-health-data-utility-models-and-advancing-standards-public-health. Accessed October 2, 2022.
- 31. Platt JE, Jacobson PD, Kardia SLR.. Public trust in health information sharing: a measure of system trust. Health Serv Res 2018; 53 (2): 824–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Nwebonyi N, Silva S, de Freitas C.. Public views about involvement in decision-making on health data sharing, access, use and reuse: the importance of trust in science and other institutions. Front Public Health 2022; 10: 852971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. State Data Sharing Initiative. Analyzing Data Confidentiality Laws & Regulations. VA, USA: State Data Sharing Initiativ; e. https://www.statedatasharing.org/better-access/. Accessed October 3, 2022. [Google Scholar]
- 34. Shalala DE. The future of America and health. In: National Congress of the Medicine/Public Health Initiative. Chicago, IL; 1996. [Google Scholar]
- 35. Lurie N, Fremont A.. Building bridges between medical care and public health. JAMA 2009; 302 (1): 84–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Yasnoff WA, Overhage JM, Humphreys BL, LaVenture M.. A national agenda for public health informatics: summarized recommendations from the 2001 AMIA Spring Congress. J Am Med Inform Assoc 2001; 8 (6): 535–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Magnuson JA, Dixon BE.. Public health informatics: the path forward. In: Magnuson J, Dixon B, eds. Public Health Informatics and Information Systems. Health Informatics. Cham: Springer; 2020. 10.1007/978-3-030-41215-9_27. [DOI] [Google Scholar]
- 38. Sittig DF, Singh H.. COVID-19 and the need for a national health information technology infrastructure. JAMA 2020; 323 (23): 2373–4. [DOI] [PubMed] [Google Scholar]
- 39. Maani N, Galea S.. COVID-19 and underinvestment in the public health infrastructure of the United States. Milbank Q 2020; 98 (2): 250–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Devi S. US public health budget cuts in the face of COVID-19. Lancet Infect Dis 2020; 20 (4): 415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Martin LT, Nelson C, Yeung D, et al. The issues of interoperability and data connectedness for public health. Big Data 2022; 10 (S1): S19–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Summary of the HIPAA Privacy Rule. Washington DC: U.S. Department of Health and Human Services; 2022. https://www.hhs.gov/hipaa/for-professionals/privacy/laws-regulations/index.html. Accessed October 15, 2022.
- 43. Dixon B, Staes C, Acharya J, et al. Enhancing the nation’s public health information infrastructure: a report from the ACMI symposium. J Am Med Inform Assoc 2023; 30 (5): 1000–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Maryland Health Care Commission. Health Information Technology and Health Information Exchange. MD, USA: Maryland Health Care Commission. https://mhcc.maryland.gov/mhcc/pages/hit/hit_hie/hit_hie.aspx. Accessed October 15, 2022. [Google Scholar]
- 45. McFarlane TD, Dixon BE, Grannis SJ, Gibson PJ.. Public health informatics in local and state health agencies: an update from the public health workforce interests and needs survey. J Public Health Manag Pract 2019; 25 (2): S67–S77. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This manuscript leveraged original data generated from the 2022 ACMI Symposium. Given the nature of the data, it is not available for access.