Abstract
Objectives:
This study examined the association between loneliness and risk of incident all-cause dementia and whether the association extends to specific causes of dementia.
Design:
Longitudinal
Setting:
Community
Participants:
Participants were from the UK Biobank (N=492,322)
Intervention:
None
Measurements:
Loneliness was measured with a standard item. The diagnosis of dementia was derived from health and death records, which included all-cause dementia and the specific diagnoses of Alzheimer’s disease (AD), vascular dementia (VD), and frontotemporal dementia (FTD), over 15 years of follow-up.
Results:
Feeling lonely was associated with a nearly 60% increased risk of all-cause dementia (HR=1.59, 95% CI=1.51–1.65; n=7,475 incident all-cause). In cause-specific analyses, loneliness was a stronger predictor of VD (HR=1.82, 95% CI=1.62–2.03; n=1,691 incident VD) than AD (HR=1.40, 95% CI=1.28–1.53; n=3135 incident AD), and was, surprisingly, a strong predictor of FTD (HR=1.64, 95% CI=1.22–2.20; n=252 incident FTD). The associations were robust to sensitivity analyses and were attenuated but remained significant accounting for clinical (e.g., diabetes) and behavioral (e.g., physical activity) risk factors, depression, social isolation, and genetic risk. The association between loneliness and all-cause and AD risk was moderated by APOE ε4 risk status such that the increased risk was apparent in both groups but stronger among non-carriers than carriers of the risk allele.
Conclusion:
Loneliness is associated with increased risk of multiple types of dementia.
Keywords: Loneliness, Social disconnection, Alzheimer’s disease, Vascular dementia, Frontotemporal dementia
There is a growing literature that implicates loneliness as a risk factor for Alzheimer’s disease and related dementias: Individuals who feel that they do not have the social connectedness that they desire are at greater risk for developing incident dementia compared to individuals who perceive a match between their desired and actual social connectedness (Sundström et al., 2020; Sutin et al., 2020; Wilson et al., 2007). This association is consistent with the broader literature on loneliness and health that indicates greater perceived feelings of disconnection, independent of objective social isolation, are associated with worse health outcomes (Courtin and Knapp, 2017), including premature mortality (Holt-Lunstad et al., 2015).
Not all studies, however, find an association between loneliness and risk of dementia (e.g., Joyce et al., 2022). Further, most research on loneliness and dementia has focused on all-cause (Sutin et al., 2020) or Alzheimer’s disease (AD; Wilson et al., 2007), and less is known about other causes of dementia. Some work suggests that loneliness is associated with risk of AD but not vascular dementia (VD; Salinas et al., 2022; Sundström et al., 2020). Research on mental health factors related to loneliness, however, suggest a different pattern. Depressive symptoms (related but not equivalent to loneliness; Cacioppo et al., 2010), for example, are associated with an increased risk of both types of dementia, but the risk associated with depressive symptoms is much stronger for VD compared to AD (Barnes et al., 2012). Further, we are unaware of any study that has examined the association between loneliness and risk of frontotemporal dementia (FTD). One study on neuroticism, a psychological trait related to loneliness (Buecker et al., 2020), found that neuroticism was associated with an increased risk of both AD and VD but not FTD (Terracciano et al., 2021). Whether this pattern holds for loneliness is not yet known.
The present study aims to extend previous research on loneliness and incident dementia risk by examining this association in the UK Biobank. Two strengths of the UK Biobank are its large sample and linked hospital and death records. With clinical diagnoses, it is possible to test the relation with specific types of dementia, in addition to all cause, and with the large sample size, it is possible to identify somewhat rarer causes of dementia, such as FTD. The UK Biobank also offers the opportunity to evaluate the robustness of the association with rich data to address whether clinical and behavioral factors related to both loneliness and dementia risk account for the association. Although a previous study using the UK Biobank did not find an association between loneliness and dementia risk (Elovainio et al., 2022), with the longer follow-up used in the present study, we expect loneliness to be associated with increased risk of incident all-cause dementia and AD due to the broader literature on loneliness and dementia risk. We do not make hypotheses for VD and FTD because of the few and inconsistent findings reported in the literature. Finally, we test whether the association between loneliness and dementia risk is moderated by the apolipoprotein (APOE) ε4 risk allele.
Participants and Procedure
The UK Biobank (http://www.ukbiobank.ac.uk) is a large prospective cohort study on the prevention, diagnosis, and treatment of common diseases. Between 2006 and 2010, more than 500,000 individuals registered with the UK National Health Service (NHS) were recruited and tested at 22 assessment centers across the UK. Loneliness and the covariates were measured at this baseline assessment. Linked health records from the NHS were used to identify incident cases of dementia. The present analysis was based on 492,322 participants; Figure 1 shows the study sample flow chart. Ethical approval for the UK Biobank was obtained from the North West Multicenter Research Ethics Committee. All participants gave informed consent. This research was conducted using the UK Biobank Resource (Application Reference Number 57672).
Figure 1.
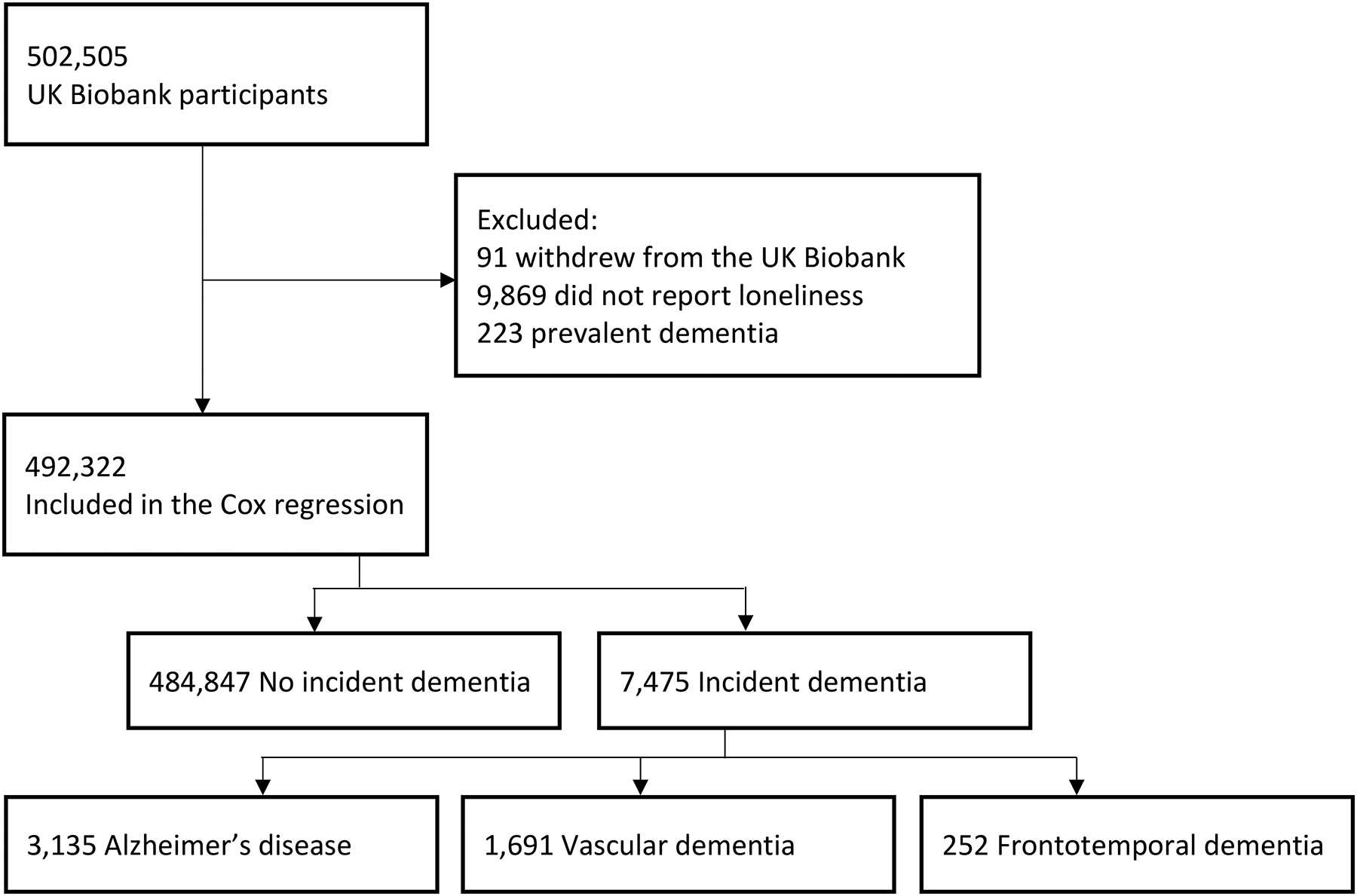
Flow chart of study participants selection and dementia outcome.
Measures
Loneliness.
Loneliness was measured with the item, “Do you often feel lonely?” Responses were coded as 0=no and 1=yes. Previous research has found that this item has a similar association with dementia risk as continuous, multi-item scales (Sutin et al., 2020) and other cognitive outcomes (de Lange et al., 2021; Sundström et al., 2020).
Dementia.
Dementia was derived from NHS hospital (93.4%) or death (6.6%) records. We used dementia adjudication and dates generated by the UK Biobank Outcome Adjudication Group (http://biobank.ctsu.ox.ac.uk/crystal/crystal/docs/alg_outcome_dementia.pdf). All-cause dementia, AD, VD, and FTD were identified from these records; not every case of all-cause dementia had a specific cause identified. Since our focus was on incident cases of dementia, we excluded cases that had a relevant ICD code prior to the baseline assessment or if a diagnosis was self-reported at recruitment.
Sociodemographic covariates.
Age in years and sex (0=male, 1=female) were reported at baseline and included in all models. Education was a university degree or equivalent (0=no, 1=yes). The Townsend deprivation index, based on participants’ postcodes, was included as a neighborhood measure of socioeconomic status. Total household income was the average total income of the household before tax reported on a scale from 1 (<18,000) to 5 (>100,000); prefer not to answer and do not know responses were set to missing.
Depression and social isolation.
Depression was assessed with the Patient Health Questionnaire-2 (PHQ-2; Kroenke et al., 2003), which was the sum of two symptoms rated from 0 (not at all) to 3 (nearly every day) and dichotomized to reflect current depression (0=less than three, 1=three or higher). Social isolation was measured with three items: household size (0=lives with others, 1=lives alone), frequency of visits with family or friends (0=at least once per month, 1=less than once per month), and frequency of leisure/social activities (0=at least weekly participation, 1=no participation at least weekly in any activity). Items were summed, and isolation classified as two or more on this index (0=less than two, 1=two or more).
Vascular and behavioral covariates.
Participants reported doctor-diagnosed diabetes, hypertension, stroke, and heart attack (0=no, 1=yes for each disease). Smoking status was current smoker (1=current) versus not current smoker (0=never/former). The International Physical Activity Questionnaire was used to estimate the sum of minutes walking and moderate and vigorous activity. Staff-assessed height and weight were used to calculate obesity (body mass index≥30). High sensitivity c-reactive protein (CRP; marker of inflammation), low-density lipoprotein (LDL; marker of hyperlipidemia), and hemoglobin A1c (HbA1c; marker of diabetes) were assayed from non-fasting venous blood samples obtained by trained staff (https://biobank.ndph.ox.ac.uk/showcase/showcase/docs/serum_biochemistry.pdf).
APOE ε4 risk status.
Participants with either one or two copies of the ε4 allele in the APOE gene were contrasted against non-carries (0=carries no copies of ε4 allele, 1=carries one or two copies of the ε4 allele).
Statistical Approach
All analyses, except where noted, were run with SPSS version 27. Cox proportional hazard regression was used to evaluate loneliness as a predictor of incident dementia. Time was coded in years from the baseline assessment (2006–2010) to the first dementia report, death, or censoring date (7 November 2021). The date of the first report of dementia was used for both all-cause and cause-specific dementia analyses (a specific diagnosis may have occurred in the health record after the first instance of dementia but the date of the first dementia code was used in the analysis). Multiple models were run to evaluate the associations. Model 1 controlled for age and sex. We tested the proportional hazard assumption based on the scaled Schoenfeld residuals using the function “test.ph” within the “survival” package (Therneau, 2019) run with R software (R Development Core Team, 2020). We then ran four sensitivity analyses for Model 1: excluding participants with more than one cause of dementia (Model 1.1), excluding incident dementia cases within five years of baseline to reduce the likelihood that participants already had dementia at baseline (Model 1.2), excluding dementia cases identified through death records (Model 1.3), and excluding participants younger than 50 years old at baseline because they were less likely to develop dementia over the follow-up (Model 1.4). Models 2–4 evaluated the robustness of the association controlling for relevant covariates. Model 2 was Model 1 with education; Model 2.1 further included household income and the Townsend deprivation index as additional covariates. Model 3 was Model 2 with depression; Model 3.1 further included social isolation. Model 4 was Model 2 with the vascular risk factors (self-reported diabetes, hypertension, stroke, heart attack, ever smoker, obesity) added and Model 4.1 further included HbA1c, CRP, LDL, and physical activity. Model 5 was Model 2 with the APOE ε4 risk status added. Finally, we tested for an interaction between loneliness and APOE ε4 risk status on dementia risk. All analyses were performed on all-cause dementia and each type of dementia.
Results
Table 1 reports the descriptive statistics for all study variables. At baseline, loneliness was reported by 18.5% of participants who remained unimpaired during the study and by about 20% to 24% of those who later developed dementia. Over the nearly 16 years of follow-up (range .03–15.66 years), 7,475 participants developed all-cause dementia, 3,135 developed AD, 1,691 developed VD, and 252 developed FTD. Table 2 reports the results of the Cox regression analyses. In the basic analysis, feeling lonely was associated with a nearly 60% increased risk of all-cause dementia. There was evidence that the assumption of proportionality was violated based on the assessment of Schoenfeld residuals for loneliness (p<.001). We thus performed follow-up analyses that stratified the sample by length of follow-up. This analysis suggested that the association was stronger with shorter (<5 years) or longer (≥10 years) follow-ups (Supplemental Table S1). Supplemental Figure S1 shows the Kaplan Meier curve for loneliness and all-cause dementia. The association between loneliness and dementia risk was robust, with a similar HR found in each sensitivity analysis for Model 1. The association was attenuated somewhat by the inclusion of socioeconomic, depression/social isolation, vascular/behavioral, and genetic risk factors, but remained associated with an about 35% to 50% increased risk of incident all-cause dementia.
Table 1.
Baseline descriptive statistics for the full sample and by dementia outcome at follow-up.
| Total | Not impaired | All-cause dementia | Alzheimer’s disease | Vascular dementia | Frontotemporal dementia | |
|---|---|---|---|---|---|---|
| N | 492,322 | 484,847 | 7,475 | 3,135 | 1,691 | 252 |
| Loneliness | 91,319 (18.5%) | 89,657 (18.5%) | 1,662 (22.2) | 637 (20.3%) | 399 (23.6%) | 60 (23.8%) |
| Age, years | 56.55 (8.09) | 56.43 (8.07) | 64.26 (4.78) | 64.74 (4.21) | 64.88 (4.14) | 61.47 (5.83) |
| Follow-up, years | 12.38 (1.84) | 12.43 (1.78) | 9.19 (2.86) | 9.06 (2.79) | 8.94 (2.88) | 8.06 (2.91) |
| Sex (Women) | 267,792 (54.5%) | 264,245 (54.5%) | 3,547 (52.5%) | 1621 (51.7%) | 699 (41.3%) | 112 (44.4%) |
| College | 158,746 (32.2%) | 157,260 (32.4%) | 1,486 (19.9%) | 582 (18.6%) | 271 (16.0%) | 73 (29.0%) |
| Deprivation | −1.32 (3.08) | −1.32 (3.08) | −0.93 (3.32) | −1.09 (3.23) | −0.67 (3.44) | −1.33 (3.05) |
| Income | 2.61 (1.19) | 2.62 (1.19) | 1.88 (1.01) | 1.86 (0.99) | 1.77 (0.95) | 2.32 (1.19) |
| Diabetes | 25,769 (5.2%) | 24,714 (5.1%) | 1,055 (14.1%) | 389 (12.4%) | 360 (21.3%) | 25 (9.9%) |
| Hypertension | 120,143 (24.4%) | 117,698 (24.3%) | 2,445 (32.7%) | 1,005 (32.1%) | 604 (35.7%) | 72 (28.6%) |
| Stroke | 6,271 (1.3%) | 5,966 (1.2%) | 305 (4.1%) | 87 (2.8%) | 136 (8.0%) | 5 (2.0%) |
| Heart attack | 11,594 (2.4%) | 11,088 (2.3%) | 506 (6.8%) | 183 (5.8%) | 189 (11.2%) | 12 (4.8%) |
| Obesity | 119,704 (24.3%) | 117,670 (24.3%) | 2,034 (27.2%) | 759 (24.2%) | 570 (33.7%) | 66 (26.2%) |
| HbA1c, mmol/mol | 36.11 (6.75) | 36.07 (6.70) | 38.84 (9.28) | 38.44 (8.78) | 40.88 (11.00) | 37.61 (9.82) |
| CRP, mg/L | 2.59 (4.35) | 2.59 (4.34) | 2.92 (5.00) | 2.58 (4.40) | 3.34 (5.32) | 2.94 (4.74) |
| LDL, mmol/L | 3.56 (0.87) | 3.56 (0.87) | 3.42 (0.97) | 3.48 (0.96) | 3.29 (1.01) | 3.56 (0.88) |
| Current smoker | 51,733 (10.5%) | 433,910 (89.5%) | 3,987 (53.3%) | 283 (9.0%) | 209 (12.4%) | 25 (9.9%) |
| Physical activity | 127.18 (101.89) | 127.23 (101.83) | 124.10 (105.98) | 133.30 (108.70) | 117.90 (104.62) | 113.47 (94.34) |
| Depression | 27,150 (5.9%) | 26,602 (5.5%) | 548 (7.3%) | 195 (6.2%) | 145 (8.6%) | 22 (8.7%) |
| Social Isolation | 44,651 (9.1%) | 43,679 (9.0%) | 972 (13.0%) | 356 (11.4%) | 238 (14.1%) | 29 (11.5%) |
| APOE ε4 | 115,472 (28.5%) | 112,293 (28.2%) | 3,179 (52.8%) | 1,571 (62.2%) | 674 (50.1%) | 82 (38.5%) |
Notes. Sample size as indicated in the Table except for Income (n = 418,852), physical activity (n = 396,781), HbA1c (n = 457,536), CRP (n = 458,518), LDL (n = 459,645), Depression (n=29,872), and APOE ε4 (n=404,876). Income is the household average total income before tax on a scale from 1 to 5. Physical activity is the sum of minutes performing walking, moderate and vigorous activity.
Table 2.
Cox regression analysis predicting risk of all-cause, Alzheimer’s disease, vascular dementia, frontotemporal dementia from loneliness.
| All-cause dementia | Alzheimer’s disease | Vascular dementia | Frontotemporal dementia | |
|---|---|---|---|---|
| Model 1, # cases | 7,475/484,847 | 3,135/484,846 | 1,691/484,846 | 252/483,992 |
| Model 1, HR (95% CI) | 1.59 (1.51–1.65) | 1.41 (1.29–1.54) | 1.83 (1.63–2.04) | 1.65 (1.23–2.21) |
| Sensitivity analyses / Robustness check | ||||
| Model 1.1, # cases | - | 2,726/484,844 | 1,301/484,622 | 194/483,992 |
| Model 1.1, HR (95% CI) | - | 1.39 (1.27–1.53) | 1.92 (1.69–2.18) | 1.62 (1.16–2.26) |
| Model 1.2, # cases | 6,740/476,541 | 2,828/476,541 | 1,502/476,533 | 215/476,200 |
| Model 1.2, HR (95% CI) | 1.54 (1.46–1.64) | 1.40 (1.27–1.53) | 1.74 (1.54–1.97) | 1.55 (1.12–2.13) |
| Model 1.3, # cases | 7,056/484,847 | 3,000/484,761 | 1,627/484,622 | 236/483,992 |
| Model 1.3, HR (95% CI) | 1.60 (1.52–1.69) | 1.40 (1.28–1.53) | 1.83 (1.63–2.05) | 1.68 (1.25–2.28) |
| Model 1.4, # cases | 7,342/369,932 | 3,107/369,931 | 1,678/369,931 | 241/369,159 |
| Model 1.4, HR (95% CI) | 1.58 (1.49–1.67) | 1.40 (1.28–1.53) | 1.82 (1.62–2.03) | 1.78 (1.33–2.39) |
| Socioeconomic covariates | ||||
| Model 2, # cases | 7,475/484,847 | 3,135/484,846 | 1,691/484,846 | 252/483,992 |
| Model 2, HR (95% CI) | 1.57 (1.48–1.66) | 1.38 (1.27–1.51) | 1.78 (1.59–1.99) | 1.65 (1.23–2.22) |
| Model 2.1, # cases | 5,588/412,722 | 2,291/412,722 | 1,258/412,722 | 187/411,648 |
| Model 2.1, HR (95% CI) | 1.42 (1.33–1.51) | 1.24 (1.12–1.38) | 1.56 (1.37–1.79) | 1.76 (1.25–2.47) |
| Depression and Social Isolation | ||||
| Model 3, # cases | 6,791/455,659 | 2,856/455,659 | 1,522/455,659 | 230/454,882 |
| Model 3, HR (95% CI) | 1.44 (1.35–1.53) | 1.32 (1.20–1.45) | 1.54 (1.36–1.76) | 1.61 (1.17–2.22) |
| Model 3.1, # cases | 6,791/455,621 | 2,856/455,621 | 1,522/455,621 | 230/454,844 |
| Model 3.1, HR (95% CI) | 1.37 (1.29–1.46) | 1.28 (1.16–1.41) | 1.46 (1.28–1.66) | 1.58 (1.14–2.19) |
| Vascular and Behavioral covariates | ||||
| Model 4, # cases | 7,475/484,847 | 3,135/484,846 | 1,691/484,846 | 252/483,992 |
| Model 4, HR (95% CI) | 1.48 (1.40–1.56) | 1.34 (1.23–1.46) | 1.56 (1.39–1.75) | 1.61 (1.20–2.16) |
| Model 4.1, # cases | 4,874/348,596 | 2,049/348,596 | 1,102/348,596 | 172/348,029 |
| Model 4.1, HR (95% CI) | 1.45 (1.35–1.56) | 1.30 (1.17–1.46) | 1.57 (1.36–1.81) | 1.51 (1.05–2.18) |
| APOE ε4 risk allele covariate | ||||
| Model 5, # cases | 6,017/398,859 | 2,524/398,858 | 1,346/398,696 | 213/398,209 |
| Model 5, HR (95% CI) | 1.56 (1.46–1.66) | 1.34 (1.21–1.48) | 1.78 (1.57–2.02) | 1.77 (1.29–2.42) |
Notes. Model 1 to Model 1.4 include the covariates age and sex; Model 1.1 excludes cases with more than one type of dementia code (e.g., AD and VD); Model 1.2 excludes incident cases of dementia within 5 years of baseline assessment; Model 1.3 excludes dementia ascertained from death records; Model 1.4 excludes participants younger than age 50 at baseline; Model 2 includes the covariates of Model 1 plus education; Model 2.1 further adds household income and the Townsend deprivation index; Model 3 includes the covariates of Model 2 plus depression; Model 3.1 further adds social isolation; Model 4 includes the covariates of Model 2 plus vascular risk factors (self-reported diabetes, hypertension, stroke, heart attack, ever smoker, BMI > 30); Model 4.1 further add HbA1c, CRP, LDL, and the sum of minutes performing walking, moderate and vigorous activity. Model 5 is Model 2 with APOE ε4 risk allele status. HR = Hazard Ratio; CI = Confidence Interval.
The overall pattern of results was similar for the three specific types of dementia (Table 2). Specifically, loneliness was associated with an about 40% increased risk of AD, an about 80% increased risk of VD, and an about 60% increased risk of FTD. There were two patterns worth noting. First, contrary to previous reports on loneliness and cause-specific dementia (Salinas et al., 2022; Sundström et al., 2020), loneliness had a stronger association with VD than AD (i.e., the confidence intervals for VD and AD did not overlap). The hazard ratio was twice as strong for VD as AD, and the confidence intervals did not overlap. Second, loneliness was a strong predictor of FTD, which was surprising and contrary to research on neuroticism and risk of FTD (Terracciano et al., 2021). As with all-cause dementia, the association between loneliness and each cause-specific dementia was robust to the sensitivity analyses as well as the additional covariates.
Finally, APOE ε4 risk status moderated the association between loneliness and risk of all-cause dementia (HRinteraction=.75, 95% CI=.67–.85) and AD (HRinteraction=.77, 95% CI=.63–.94) but not VD (p=.057) or FTD (p=.835). Stratified analysis by APOE ε4 risk status for both all-cause and AD indicated that the association was significant in both groups but stronger among non-carriers (all-cause: HR=1.86, 95% CI=1.70–2.02; AD: HR=1.63, 95% CI=1.40–1.90) than carriers (all-cause: HR=1.36, 95% CI=1.24–1.48; AD: HR=1.22, 95% CI=1.07–1.38). A similar pattern was found for VD (non-carrier: HR=2.08, 95% CI=1.74–2.47; carrier: HR=1.59, 95% CI=1.32–1.92), and this difference approached statistical significance (p=.057). Interestingly, the pattern was in the opposite direction for FTD (non-carrier: HR=1.68, 95% CI=1.13–2.52; carrier: HR=1.91, 95% CI=1.16–3.14), but not statistically different (p=.835) because it was underpowered to detect differences.
Discussion
The present research found a robust association between loneliness and risk of all-cause and cause-specific dementia: Feeling lonely was associated with an about 60% increased risk of incident all-cause dementia over an up to nearly 16 years of follow-up. Most notably, the cause-specific analyses indicated that loneliness was a stronger risk factor for VD compared to AD, and it also emerged as a robust predictor of FTD. These associations were somewhat attenuated by socioeconomic factors, depression and social isolation, and vascular and behavioral risk factors that are associated with both loneliness and dementia risk, as well as genetic risk. The associations, however, persisted after accounting for these factors. Finally, although apparent in both groups, the association between loneliness and all-cause dementia and AD was stronger among non-carriers than carriers of the APOE ε4 risk allele.
The association between loneliness and risk of dementia is consistent with the growing literature on the poor cognitive outcomes associated with loneliness (Lara et al., 2019; Luchetti et al., 2020), and with worse health outcomes more generally (Courtin and Knapp, 2017). Loneliness, for example, has been associated with poor cardiovascular health (Valtorta et al., 2016), disease burden (Christiansen et al., 2021), and premature mortality (Holt-Lunstad et al., 2015). These associations may be due, in part, to health-risk behaviors. That is, individuals who feel lonely are more likely to smoke and are less likely to be physically active (Yang et al., 2022). The depression and the other clinical (body mass index, the diseases, and the biomarkers) and behavioral (smoking, physical activity) risk factors may be on the causal pathway between loneliness and dementia, whereas the sociodemographic factors and APOE are more likely to be true confounders. As such, the reduction in association accounting for depression and the clinical and behavioral risk factors suggests that these factors could be mechanisms underlying the association. These factors also do not account for all the association between loneliness and dementia risk. This pattern suggests other mechanisms are likely to contribute to this association, such as less engagement in cognitively stimulating activities, more sedentary behavior, less social support, and greater stress among individuals who often feel lonely.
The present research allowed for distinguishing between causes of dementia. Most previous research has focused on either all-cause dementia or AD (Shibata et al., 2021; Sutin et al., 2020; Wilson et al., 2007), with less research also including VD and none with FTD. In contrast to two previous studies on cause-specific dementia (Salinas et al., 2022; Sundström et al., 2020), we found loneliness had a stronger association with risk of VD than AD. Our results, however, are consistent with work on depressive symptoms (Barnes et al., 2012) and neuroticism (Terracciano et al., 2021) that found stronger associations with VD than AD. VD is generally diagnosed at relatively younger ages than AD (Goodman et al., 2017), which might contribute to these results in at least two ways. First, participants in the UK Biobank tend to be relatively young compared to the average age of diagnosis for AD, which may contribute to the slightly higher proportion of VD in this sample compared to VD estimated in the population (Rizzi et al., 2014). Second, greater vascular risk factors associated with loneliness may make individuals more susceptible to VD before AD can develop. Loneliness has been associated with many clinical vascular factors that are risk factors for vascular dementia, including diabetes (Hackett et al., 2020), coronary heart disease and stroke (Valtorta et al., 2018), metabolic syndrome (Henriksen et al., 2019), and cardiovascular fitness (Hawkley et al., 2003), as well as behavioral factors for poor vascular outcomes, such as smoking (Yang et al., 2022). As noted, the association between loneliness and VD (as well as AD) remained significant controlling for many of these risk factors. It is possible that other vascular risk factors or constellations of risk factors explain this association.
Of particular note, loneliness was associated with greater risk of FTD. This association was surprising given that previous work in the UK Biobank on a related construct (neuroticism) was unrelated to FTD risk (Terracciano et al., 2021). Further, individuals who develop FTD tend to have an emotional profile that is not sensitive to internal feelings of distress (Bathgate et al., 2001), which presumably could have extended to loneliness. FTD is characterized by socially inappropriate behavior and impairment in emotion recognition (Migliaccio et al., 2020). Interestingly, qualitative studies with loved ones of individuals with FTD find a consistent theme of a loss of closeness and intimacy with the individual (Shiba et al., 2022). These qualitative studies suggest that, in retrospect, loved ones tend to point to this change in intimacy as the first sign of the disease, usually well before diagnosis. It is of note, then, that loneliness of the individual would be a predictor of developing FTD. Although our sensitivity analysis that excluded diagnosis within five years only slightly reduced the HR, suggesting against reverse causality, it may be that there is a long preclinical phase and that feeling lonely may be an early indicator of the disease process. Future work would benefit from examining changes in loneliness prior to onset of cognitive deficits.
The presence of at least one copy of APOE ε4 is a genetic risk factor for Alzheimer’s disease (Verghese et al., 2011). In the present study, the association between loneliness and dementia risk was independent of this genetic risk factor. There is some previous evidence for an interaction between neuroticism and the presence of the risk allele such that higher neuroticism amplified the risk associated for APOE ε4 (Dar-Nimrod et al., 2012), although other studies have not replicated this interaction (Terracciano et al., 2014). The present research found the opposite pattern: Loneliness was a stronger predictor of risk of all-cause dementia and AD among individuals who did not carry any copies of the risk allele. It is possible that the genetic risk associated with the ε4 allele is a strong enough predictor of AD that it overwhelms the risk associated with other factors, such as loneliness. When the genetic risk associated with ε4 is not present, aspects of social health, like loneliness, may be more potent predictors of poor cognitive outcomes.
The present study builds on recent work published in International Psychogeriatrics. A recent review, for example, highlighted the role of loneliness in the development of depressive symptoms and maintenance of depression (Van As et al., 2022). Depression may be one mechanism through which loneliness is associated with increased risk of dementia. In the present study, however, depression did not account for all the association, so there are likely to be other important mechanisms as well. In addition, treatment of loneliness may help to support cognitive function. There is recent evidence, for example, that change in neuroticism after treatment for depression is associated with preserving more cognitive function over time (Steffens et al., 2022). Decreases in loneliness may be similarly protective of cognitive function and help delay the development of dementia. Greater feelings of social integration may also help buffer against negative life events that may pose threats to health and well-being in older adulthood (Switsers et al., 2021), and may extend to cognitive health as well.
Two previous studies that used the UK Biobank did not find an association between loneliness and all-cause dementia risk controlling for social isolation (Elovainio et al., 2022; Shen et al., 2022), whereas the current study did find this association. There are at least two differences between these two studies and the current one that might explain this discrepancy. First, the follow-up interval was longer in the current study (Mfollow-up=12.38 years versus Mfollow-up=8.8 [Elovainio et al., 2022] and Mfollow-up=11.7 years [Shen et al., 2022]) and with more cases of dementia identified over this follow-up (n=7,475 versus n=1444 [Elovainio et al., 2022] and n=4,998 [Shen et al., 2022]), there may have been more power to detect an association. Second, the present study used a measure of loneliness consistent with previous research on loneliness and dementia (e.g., Sundström et al., 2020) that has been found to have the same predictive power as validated scales (Sutin et al., 2020), whereas the other studies used an unusual aggregate of items that classified some people with loneliness as non-lonely (both items had to be endorsed to be classified as lonely; associations with the second item were similar but lower in magnitude in the present study [Supplemental Table S2]). The association between loneliness and dementia was likely diluted because participants who endorsed loneliness on one item but not the other were classified as not lonely. These differences in the length of follow-up, number of cases, and assessment of loneliness may account for the different results.
The present study has several strengths, including the large sample size, clinical diagnosis of dementia, analysis of cause-specific dementia risk, up to nearly 16-years of follow-up, and the inclusion in the analyses of multiple risk factors for dementia. There are some limitations that could be addressed in future research. First, some dementia cases, especially during the early phases, are likely to be missed by medical records. Second, the sample was based entirely on adults living in the UK. Future research could evaluate this association in other cultural and economic contexts, particularly in low- and middle-income countries. Third, we did not identify mechanisms that accounted for all the associations between loneliness and dementia risk. Future research could take a more comprehensive approach to potential mediators, especially across types of dementia. Finally, we considered loneliness measured at a one-time point. Future research could distinguish between transient and persistent loneliness and whether each type is differentially associated with dementia risk. Despite these limitations, the present research supports the literature on loneliness and dementia risk and indicates some differential associations across causes of dementia.
Supplementary Material
Acknowledgement
This research has been conducted using the UK Biobank Resource (Application Reference Number 57672). The study was not pre-registered and the authors do not have permission to distribute the data, but data is available upon application from http://www.ukbiobank.ac.uk.
Funding
This work was supported by the National Institute on Aging of the National Institutes of Health (grant numbers R01AG053297, R01AG068093). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or other funding Institutes.
Footnotes
Conflict of Interest
None.
Author Roles
A. Sutin conceptualized the study, analyzed the data, and wrote the draft article.
M. Luchetti assisted with writing the article.
D. Aschwanden conducted a subset of analyses and assisted with writing the article.
X. Zhu assisted with writing the article.
Y. Stephan assisted with writing the article.
A. Terracciano assisted with conceptualization of the study, secured the data from the UK Biobank, and assisted with writing the article.
References
- Barnes DE, Yaffe K, Byers AL, McCormick M, Schaefer C and Whitmer RA (2012). Midlife vs late-life depressive symptoms and risk of dementia: differential effects for Alzheimer disease and vascular dementia. Archives of General Psychiatry 69, 493–498. doi: 10.1001/archgenpsychiatry.2011.1481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bathgate D, Snowden JS, Varma A, Blackshaw A and Neary D (2001). Behaviour in frontotemporal dementia, Alzheimer’s disease and vascular dementia. Acta Neurologica Scandinavica 103, 367–378. doi: 10.1034/j.1600-0404.2001.2000236.x [DOI] [PubMed] [Google Scholar]
- Buecker S, Maes M, Denissen JJA and Luhmann M (2020). Loneliness and the big five personality traits: A meta-analysis. European Journal of Personality 34, 8–28. doi: 10.1002/per.2229 [DOI] [Google Scholar]
- Cacioppo JT, Hawkley LC and Thisted RA (2010). Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychology and Aging 25, 453–463. doi: 10.1037/a0017216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christiansen J, Lund R, Qualter P, Andersen CM, Pedersen SS and Lasgaard M (2021). Loneliness, social isolation, and chronic disease outcomes. Annals of Behavioral Medicine 55, 203–215. doi: 10.1093/abm/kaaa044 [DOI] [PubMed] [Google Scholar]
- Courtin E and Knapp M (2017). Social isolation, loneliness and health in old age: a scoping review. Health Society and Care Community 25, 799–812. doi: 10.1111/hsc.12311 [DOI] [PubMed] [Google Scholar]
- Dar-Nimrod I et al. (2012). Personality factors moderate the associations between apolipoprotein genotype and cognitive function as well as late onset Alzheimer disease. American Journal of Geriatric Psychiatry 20, 1026–1035. doi: 10.1097/JGP.0b013e318267016b [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Lange AG et al. (2021). Prominent health problems, socioeconomic deprivation, and higher brain age in lonely and isolated individuals: A population-based study. Behavior Brain Research 414, 113510. doi: 10.1016/j.bbr.2021.113510 [DOI] [PubMed] [Google Scholar]
- Elovainio M et al. (2022). Association of social isolation, loneliness and genetic risk with incidence of dementia: UK Biobank Cohort Study. BMJ Open 12, e053936. doi: 10.1136/bmjopen-2021-053936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman RA, Lochner KA, Thambisetty M, Wingo TS, Posner SF and Ling SM (2017). Prevalence of dementia subtypes in United States Medicare fee-for-service beneficiaries, 2011–2013. Alzheimer’s & Dementia 13, 28–37. doi: 10.1016/j.jalz.2016.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hackett RA, Hudson JL and Chilcot J (2020). Loneliness and type 2 diabetes incidence: findings from the English Longitudinal Study of Ageing. Diabetologia 63, 2329–2338. doi: 10.1007/s00125-020-05258-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, Burleson MH, Berntson GG and Cacioppo JT (2003). Loneliness in everyday life: cardiovascular activity, psychosocial context, and health behaviors. Journal of Personality and Social Psychology 85, 105–120. doi: 10.1037/0022-3514.85.1.105 [DOI] [PubMed] [Google Scholar]
- Henriksen RE, Nilsen RM and Strandberg RB (2019). Loneliness as a risk factor for metabolic syndrome: results from the HUNT study. Journal of Epidemiology and Community Health 73, 941–946. doi: 10.1136/jech-2019-212335 [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Baker M, Harris T and Stephenson D (2015). Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspectives in Psychological Science 10, 227–237. doi: 10.1177/1745691614568352 [DOI] [PubMed] [Google Scholar]
- Joyce J et al. (2022). Social isolation, social support, and loneliness and their relationship with cognitive health and dementia. International Journal of Geriatric Psychiatry 37. doi: 10.1002/gps.5644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL and Williams JB (2003). The Patient Health Questionnaire-2: validity of a two-item depression screener. Medical Care 41, 1284–1292. [DOI] [PubMed] [Google Scholar]
- Lara E et al. (2019). Does loneliness contribute to mild cognitive impairment and dementia? A systematic review and meta-analysis of longitudinal studies. Ageing Research Reviews 52, 7–16. doi: 10.1016/j.arr.2019.03.002 [DOI] [PubMed] [Google Scholar]
- Luchetti M, Terracciano A, Aschwanden D, Lee JH, Stephan Y and Sutin AR (2020). Loneliness is associated with risk of cognitive impairment in the Survey of Health, Ageing and Retirement in Europe. International Journal of Geriatric Psychiatry 35, 794–801. doi: 10.1002/gps.5304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Migliaccio R et al. (2020). Cognitive and behavioural inhibition deficits in neurodegenerative dementias. Cortex 131, 265–283. doi: 10.1016/j.cortex.2020.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Development Core Team. (2020). R: A language and environment for statistical computing (Version 3.5.1) [Computer software]. https://www.r-project.org/index.html
- Rizzi L, Rosset I and Roriz-Cruz M (2014). Global epidemiology of dementia: Alzheimer’s and vascular types. Biomedical Research International, 908915. doi: 10.1155/2014/908915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salinas J et al. (2022). Association of loneliness with 10-year dementia risk and early markers of vulnerability for neurocognitive decline. Neurology 98, e1337–e1348. doi: 10.1212/WNL.0000000000200039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen C, Rolls E, Cheng W, Kang J, Dong G, Xie C, … Feng J (2022). Associations of social isolation and loneliness with later dementia. Neurology. doi: 10.1212/WNL.0000000000200583 [DOI] [PubMed] [Google Scholar]
- Shiba T, Yamakawa M, Endo Y, Konno R and Tanimukai S (2022). Experiences of families of people living with frontotemporal dementia: a qualitative systematic review. Psychogeriatrics. doi: 10.1111/psyg.12837 [DOI] [PubMed] [Google Scholar]
- Shibata M et al. (2021). Emotional loneliness is associated with a risk of dementia in a general Japanese older population: The Hisayama Study. Journals of Gerontology Series B Psychological Sciences and Social Sciences 76, 1756–1766. doi: 10.1093/geronb/gbaa196 [DOI] [PubMed] [Google Scholar]
- Steffens DC, Manning KJ, Wu R, & Grady JJ (2022). Association of 1-year change in neuroticism and 3-year change in cognitive performance among older depressed adults. International Psychogeriatrics, 34, 645–650. doi: 10.1017/S1041610222000084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundström A, Adolfsson AN, Nordin M and Adolfsson R (2020). Loneliness increases the risk of all-cause dementia and Alzheimer’s disease. Journals of Gerontology Series B Psychological Sciences and Social Sciences 75, 919–926. doi: 10.1093/geronb/gbz139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutin AR, Stephan Y, Luchetti M and Terracciano A (2020). Loneliness and risk of dementia. Journals of Gerontology Series B Psychological Sciences and Social Sciences 75, 1414–1422. doi: 10.1093/geronb/gby112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Switsers L, Dierckx E, Domènech-Abella J, De Donder L, Dury S, & Consortium D-S (2021). Negative old-age life events and well-being in later life: the moderating and mediating role of loneliness. International Psychogeriatrics, 33, 1265–1276. 10.1017/S1041610220004196 [DOI] [PubMed] [Google Scholar]
- Terracciano A et al. (2021). Is neuroticism differentially associated with risk of Alzheimer’s disease, vascular dementia, and frontotemporal dementia? Journal of Psychiatric Research 138, 34–40. doi: 10.1016/j.jpsychires.2021.03.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A et al. (2014). Personality and risk of Alzheimer’s disease: New data and meta-analysis. Alzheimer’s & Dementia 10, 179–186. doi: 10.1016/j.jalz.2013.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Therneau TM (2019). Package “survival” (Version 2.44–1.1) [Computer software]. https://cran.r-project.org/web/packages/survival/survival.pdf
- Van As BAL, Imbimbo E, Franceschi A, Menesini E, & Nocentini A (2022). The longitudinal association between loneliness and depressive symptoms in the elderly: a systematic review. Int Psychogeriatr, 34, 657–669. doi: 10.1017/S1041610221000399 [DOI] [PubMed] [Google Scholar]
- Valtorta NK, Kanaan M, Gilbody S and Hanratty B (2018). Loneliness, social isolation and risk of cardiovascular disease in the English Longitudinal Study of Ageing. European Journal of PreventiveCardiology 25, 1387–1396. doi: 10.1177/2047487318792696 [DOI] [PubMed] [Google Scholar]
- Valtorta NK, Kanaan M, Gilbody S, Ronzi S and Hanratty B (2016). Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart 102, 1009–1016. doi: 10.1136/heartjnl-2015-308790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verghese PB, Castellano JM and Holtzman DM (2011). Apolipoprotein E in Alzheimer’s disease and other neurological disorders. Lancet Neurology 10, 241–252. doi: 10.1016/S1474-4422(10)70325-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson RS et al. (2007). Loneliness and risk of Alzheimer disease. Archive of General Psychiatry 64, 234–240. doi: 10.1001/archpsyc.64.2.234 [DOI] [PubMed] [Google Scholar]
- Yang J, Yockey RA, Chu Y and Lee JGL (2022). The influence of loneliness on the smoking and physical activity of community-dwelling older adults: Results from the Health and Retirement Study. American Journal of Health Promotion 36, 959–966. doi: 10.1177/08901171221081136. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


