Abstract
Objectives:
The COVID-19 pandemic greatly impacted the social lives of older adults across several areas, leading to concern about an increase in loneliness. This study examines the associations of structural, functional, and quality aspects of social connection with increased loneliness during COVID-19 and how these associations vary by sociodemographic factors.
Design:
Secondary data analyses on a nationally representative survey of older U.S. adults.
Setting:
The 2020 Health and Retirement Study (HRS) COVID-19 module.
Participants:
The study sample includes 3,804 adults aged 54 or older.
Measurements:
Increased loneliness was based on respondents’ self-report on whether they felt lonelier than before the COVID-19 outbreak.
Results:
While 29% felt lonelier after COVID-19, middle-aged adults, women, non-Hispanic Whites, and the most educated were more likely to report increased loneliness. Not having enough in-person contact with people outside the household was associated with increased loneliness (OR=10.07, p < .001). Receiving emotional support less frequently (OR=2.28, p < .05) or more frequently (OR=2.00, p < .001) than before was associated with increased loneliness. Worse quality of family relationships (OR=1.85, p < .05) and worse friend/neighbor relationships (OR=1.77, p < .01) were related to feeling lonelier. Significant interactions indicated stronger effects on loneliness of poor-quality family relationships for women and insufficient in-person contact with non-household people for the middle-aged group and non-Hispanic Whites.
Conclusions:
Our findings show an increase in loneliness during COVID-19 that was partly due to social mitigation efforts, and also uncover how sociodemographic groups were impacted differently, providing implications for recovery and support.
Keywords: social isolation, psychosocial, diversity, pandemic
Introduction
In the early stage of the COVID-19 pandemic, health experts and governments across the world encouraged social distancing measures to control the spread of the virus and minimize infection risk by reducing close contact among people. These policies have included limits on large social gatherings, stay-at-home orders, and travel restrictions (Gostin and Wiley, 2020), substantially restricting in-person social activities (Okabe-Miyamoto and Lyubomirsky, 2021). While designed to protect individuals, particularly those at increased risk of severe COVID-19 symptoms (e.g., older adults), side effects of social distancing may have disproportionally affected those who were not readily prepared to maintain social connections while being physically distant. Professional communities have raised concerns that the practice of social distancing can contribute to social isolation and loneliness, and older people may be more susceptible to its unintended consequences (Hwang et al., 2020; Miller, 2020). Social distancing remains as the primary strategy for mitigating the transmission of COVID-19 as we confront new surges. This study uses nationally representative survey data of older Americans that were collected during the severe period of COVID-19. The findings inform questions about which aspects of social lives contribute to feelings of loneliness and for which groups. This will help us to make informed public health decisions in the future to protect older adults from new COVID-19 waves and other highly transmissible diseases while minimizing the burdens of social restriction on loneliness risk.
Social isolation and loneliness in older adults are serious public health concerns because of their link to adverse health outcomes such as cardiovascular health, physical morbidity, depression, cognitive impairment, and mortality (Holt-Lunstad et al., 2015; National Academies of Sciences, Engineering, and Medicine [NASEM], 2020). The changes in social life, as evidenced by the changes in social distancing and norms, may have magnified the already existing problem of social disconnection and loneliness among the older population (Thayer and Anderson, 2018; Kasar and Karaman, 2021). A growing number of reports have documented that older adults have experienced worsened loneliness, loss of social support, and social disconnection during the COVID-19 pandemic (van Tilburg et al., 2020; Kotwal et al., 2021; Krendl and Perry, 2021; Stolz, Mayerl and Freidl, 2021). For example, about 73% of U.S. adults aged 50+ reported that the pandemic made it more challenging to connect with friends, and 61% felt socially isolated (AARP Foundation, 2020).
Importantly, this experience of social disconnection and loneliness may be uneven across subpopulations within older adults. Studies have suggested that women, those with low socioeconomic resources, and those who live alone are more likely to experience greater social disconnection and loneliness during the pandemic (Wong et al., 2020; Kasar and Karaman, 2021). This is partly because disadvantaged groups face more challenges in accessing various resources/services (Douglas and Subica, 2020) and technological solutions to help with social distancing requirements (Donovan and Blazer, 2020). Therefore, continued efforts should be made to identify the subgroups at high risk as well as to evaluate the general impacts of COVID-19 on older adults’ social lives.
Our study strengthens the understanding of COVID-related loneliness among older adults by addressing the following research gaps. First, we are among the first studies to focus on multidimensional aspects of social connection (structural, functional, and quality) in relation to changes in COVID-related loneliness, which helps us identify which aspects of older adults’ social lives have been most impacted. Second, most previous studies used convenience sampling, limiting the generalizability of the findings to the U.S. older population (Dahlberg, 2021). Our study uses data from a nationally representative sample of older adults in the U.S., which is important for determining if the association of social connection with increased loneliness was experienced across the population. Third, most research assessed loneliness with questions not specific to the pandemic, which makes it difficult to differentiate whether a high or increased level of loneliness can be attributed to factors related to the COVID-19 pandemic or reflects one’s general state prior. Our study used a question designed to directly measure changes in loneliness due to COVID-19. Last, our research hypotheses are guided by the Social Psychology Theory and resource perspective on loneliness, which can help us connect the study findings to the established literature or inform interventions.
Theoretical Backgrounds and Hypotheses
Social connection has been identified as a multidimensional construct encompassing different aspects of social relationships that include structural, functional, and quality categories. These components provide a holistic understanding of how individuals are socially connected to others (Holt-Lunstad et al., 2017). Structural aspects relate to the existence of and interconnections among social relationships and roles (e.g., social network size, frequency of contact, and marital status). Functional aspects encompass the extent to which others can be relied on (e.g., instrumental and emotional social support). Quality aspects address a sense of connection arising from positive and negative qualities of relationships (e.g., marital quality and sense of belonging) (Carlson et al., 2017). Each component has been found to be correlated but independent from one another, providing evidence of different underlying pathways to health outcomes (Cohen, Gottlieb and Underwood, 2000; Holt-Lunstad, 2017).
Drawing on a cognitive attributional perspective, the Social Psychology Theory of Loneliness posits that loneliness occurs when one’s actual social relationships are perceived as being insufficient, either quantitatively or qualitatively, than what is desired, which is largely dependent on subjective experience (Perlman and Peplau, 1982). The COVID-19 pandemic may have created this discrepancy and increased loneliness by affecting different aspects of social connection: (1) limiting individuals’ social contact (structural), (2) affecting the social support that they receive (functional), and (3) disrupting the quality of relationships with others (quality). Studies have provided supporting evidence for this argument. For example, Spanish adults who had less contact with relatives during COVID-19 reported greater loneliness (Losada-Baltar et al., 2021). Similarly, a loss of social contact and an unfulfilled need for support increased the loneliness of Dutch older adults (van Tilburg et al., 2020). To this end, we hypothesize that changes in different aspects of social connection due to COVID-19 (i.e., limited social contact, impaired relationship quality, and support needs) will lead to increased loneliness (Hypothesis 1).
It is important to note that the subjective experience of loneliness, regardless of actual social contact, varies across individuals’ circumstances and expectations (Perissinotto and Covinsky, 2014). The resource perspective on loneliness argues that one’s access to resources affects loneliness level, either directly or indirectly, through its effects on social relationships (Tesch-Roemer and Huxhold, 2019). The resource here may be both material (e.g., economic status) and interpersonal (e.g., socially responsive environments). According to this perspective, older adults with limited access to resources may be more challenged by the COVID-19 social restrictions and, thus, more prone to increased loneliness. For example, while staying at home, those who do not have other people around or technological access to virtual connection are more susceptible to feeling lonelier. The current study hypothesizes that older adults, men, racial/ethnic minorities, and people with low education will be more likely to experience increased loneliness due to their more limited social resources to counter the impact social distancing measures had on their ways of connecting with others (Hypothesis 2). We also explore sociodemographic differences in the association between three aspects of social connection and increased loneliness. Here, we expect that groups with fewer social or material resources will be strongly impacted by adverse changes in social connection (Hypothesis 3). The overall theoretical framework of this study is presented in Figure 1.
Figure 1.
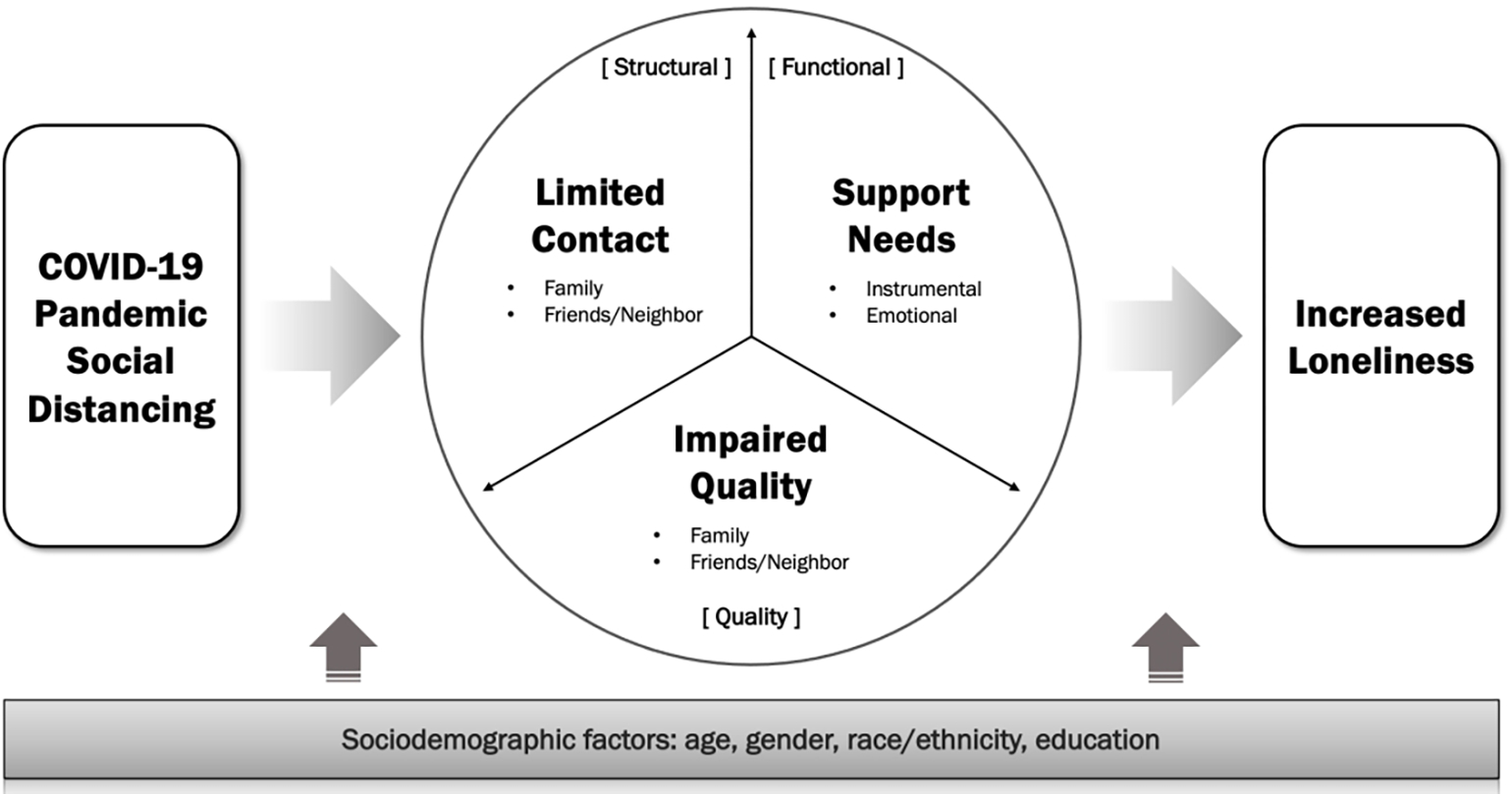
Theoretical Framework on How COVID-19 Pandemic May Have Led to Changes in Three Aspects of Social Connections and Loneliness
Methods
Data and Sample
This study uses data from the Health and Retirement Study (HRS). The HRS is a longitudinal survey of a U.S. nationally representative sample aged 50 years and older, and it has been conducted biannually since 1992. In response to the COVID-19 pandemic, HRS included COVID-19-related questions in the 2020 core interview and collected data between March 2020 through June 2021. The COVID-19 module of the 2020 HRS was administered to the random half of the HRS households, which was further split into two subgroups: the first one starting in June and the remaining other in September of 2020. The participants also received a self-administered leave behind questionnaire (SAQ) by mail, following their core interview. The SAQ included questions on psychosocial changes arising from the COVID-19 pandemic. A total of 4,200 community-dwelling individuals aged 50 or older completed the SAQ survey. We limited to the community-dwelling, HRS cohort members who were 54 and older at the time of the COVID-19 interview (n=3,961). After excluding an additional 157 respondents with missing information on study variables (3.9%), the final analytic sample consisted of 3,804 adults aged 54 or above.
Measures
Loneliness.
Respondents were asked to report whether they felt lonely about the same, more, or less often compared to before the COVID-19 outbreak. As our focus was on examining the increased loneliness due to the pandemic, the responses were coded 0 for about the same or less so and 1 for more so.
Social connection.
The survey included a wide range of questions on changes in social connection since the COVID-19 pandemic. We used items relevant to the structural, functional, and quality aspects of social connection. The structural aspect of social connection was further divided into 1) limited family social gatherings and 2) not enough in-person contact with people outside the household. Limited family social gatherings were assessed by whether the respondent experienced changes in the following activities due to the pandemic: (a) unable to visit a family member in a care facility, nursing home, or group home; (b) family celebrations canceled or restricted; (c) unable to visit a close family member who was in the hospital; (d) unable to attend the in-person funeral or religious services for a family member who died; (e) unable to visit family after the birth of a new baby. The response was coded 1 for yes and 0 for no or not relevant. A summary score was calculated by adding each item, with a total score ranging from 0 to 5. Not enough in-person contact with non-household people was measured with a single question asking how often the respondent has felt that they do not get enough in-person contact with people outside one’s household since the pandemic. The response was coded 0 for hardly ever or never and 1 for sometimes or often. As two measures of the functional aspect of social connection, the respondents were asked how often they had received 1) instrumental support (i.e., help for obtaining necessities or arranging emergency household repairs) or 2) emotional support (i.e., advice, encouragement, or emotional support) from others since the pandemic. Two categorical variables were created with responses grouped into (a) less often; and (b) about the same; (c) more often; and (d) not needed or not relevant. Finally, two indicators of the quality aspect were included: 1) worse quality of relationships with family members (i.e., children, grandchildren, and other family members) and 2) worse quality of relationships with friends or neighbors. Each indicator was coded as 1 if the respondent reported that their relationships had been worse since the pandemic.
Socio-demographic characteristics.
Age was measured in years, and it was further categorized into two groups in analyses: ages 54–74 and ages 75 or older to facilitate subgroup comparisons. Gender was coded 0 for men and 1 for women. Race/ethnic groups consisted of non-Hispanic White, non-Hispanic Black, Hispanic, and others (American Indian, Alaskan Native, Asian, and Pacific Islander). Due to the small number of respondents from minority race/ethnic backgrounds, they were grouped together to create a Minority category for multivariate analyses. Marital status was grouped into (a) married or partnered; (b) separated or divorced; (c) widowed; or (d) never married. Educational attainment was classified as high school graduation or lower and some college or above.
Analytical Strategy
After reviewing the descriptive characteristics of study variables, we compared loneliness changes by socio-demographic groups using chi-square tests. Next, to examine the associations of social connection on increased loneliness during COVID-19, we fitted logistic regression models. The findings remained similar between the models where each indicator of social connection was entered separately and the model with all indicators included simultaneously. We present models with all indicators as the main results and include the results from models with each indicator entered separately in the supplementary materials. Finally, interactions between each significant indicator of social connection and socio-demographic characteristics were examined to test whether the role of social connection in the increase of loneliness would differ across socio-demographic subgroups. A total number of 16 interaction terms were examined (4 significant indicators and 4 sociodemographic factors). While this study set the statistical significance level at p < .05, we also report the Bonferroni-corrected significance threshold of p < .003 to reduce Type I error. Comprehensive information on the exact p values, the nominal significance threshold, and the Bonferroni-corrected threshold would allow more careful interpretation of the findings in light of various biases tied to each of the thresholds - high Type II error rates from the Bonferroni-corrected threshold and inflated Type I error rates from the conventional nominal threshold (VanderWeele and Mathur, 2019). Significant interactions were further examined by post-hoc pairwise comparisons of marginal predictions, which allows estimating group differences in increased loneliness for each response (i.e., yes or no) to a social connection indicator (MacKinnon, 2012). Differences were tested using Wald chi-squared tests. The Bonferroni-corrected significance level for the group differences in the effects of each indicator on increased loneliness was p < .025 as two groups were compared (e.g., women vs. men). All analyses are weighted to correct for differential selection probabilities and non-response and to make the estimates population-representative. All analyses were performed using STATA version 17.0.
Supplementary Analyses
Individuals’ reports on changes in loneliness during COVID-19 may differ depending on one’s usual levels of loneliness before the pandemic. Thus, we conducted supplementary analyses using the previous wave (2016) data to examine whether there are any differences in the factors associated with increased loneliness due to COVID-19 between the pre-lonely and the not pre-lonely groups. Loneliness was measured with the shortened 3-item scale of loneliness (Hughes et al., 2004) from the 20-item Revised UCLA Loneliness Scale (Russell, 1996). Respondents were asked how often they feel (1) lack companionship, (2) left out, and (3) isolated from others. Responses were coded on a three-point Likert scale (1 = often, 2 = some of the time, 3 = hardly ever or never). A summary index of loneliness was created by summing the scores after reverse-coding (Range: 3–9), with higher values indicating greater levels of loneliness. The summary scale was pro-rated for those with at least two of the three items by dividing the non-missing summed scores by the number of non-missing items and multiplying them by 3. The internal consistency for the loneliness scale (Cronbach’s α) was 0.79. Adopting the widely used cut-off score of 6 (Victor and Pikhartova, 2020), those with scores of 3–5 were categorized as ‘not lonely,’ and those with 6 or higher were considered ‘lonely.’ Logistic regressions predicting increased loneliness were performed for each group.
Results
Descriptive Statistics
Table 1 shows the descriptive statistics of the study variables. The mean age of participants was 69.6 years (SD = 9.7), about 77% were aged 54–74 and the remaining 23% were aged 75–95. About 55% were women. Non-Hispanic White was the largest group (79.9%) and racial/ethnic minority consisted of 7.9% non-Hispanic Blacks, 7.1% Hispanics, and 5.1% others (i.e., American Indian, Alaskan Native, Asian, and Pacific Islander). More than half of the sample (65.3%) had some college or above education and 64.1% were married or partnered.
Table 1.
Descriptive Characteristics of Study Variables (N = 3,804)
| Variables | % | ||
|---|---|---|---|
|
| |||
| Socio-demographics | |||
| Age (M±SD) | (69.6±9.7) | ||
| Aged 54–74 | 76.6 | ||
| Aged 75–95 | 23.4 | ||
| Women | 55.2 | ||
| Race/ethnicity | |||
| Non-Hispanic White | 79.9 | ||
| Non-Hispanic Black | 7.9 | ||
| Hispanic | 7.1 | ||
| Other | 5.1 | ||
| Some college or above | 65.3 | ||
| Marital status | |||
| Married/partnered | 64.1 | ||
| Separated/divorced | 15.4 | ||
| Widowed | 13.2 | ||
| Never married | 7.3 | ||
| Social connection during the COVID-19 | |||
| Structural aspect | |||
| Number of limited family social gatherings due to COVID-19 (M±SD) | (2.0±1.5) | ||
| Unable to visit a family member in a care facility | 28.2 | ||
| Family celebrations cancelled or restricted | 75.8 | ||
| Unable to visit a close family member in hospital | 29.1 | ||
| Unable to attend in-person funeral for a family member who died. | 42.3 | ||
| Unable to visit family after the birth of a new baby | 17.9 | ||
| Not enough in-person contact with people outside household since COVID-19 | |||
| Hardly ever or never | 30.9 | ||
| Sometimes or often | 69.1 | ||
| Functional aspect | |||
| Received instrumental support from others | |||
| Not needed | 67.9 | ||
| About the same | 13.9 | ||
| Less often | 2.0 | ||
| More often | 16.1 | ||
| Received emotional support from others | |||
| Not needed | 43.0 | ||
| About the same | 31.0 | ||
| Less often | 1.4 | ||
| More often | 24.6 | ||
| Quality aspect | |||
| Worse quality of relationships with family members | 10.8 | ||
| Worse quality of relationships with friends/neighbors | 14.1 | ||
| Loneliness compared to before COVID-19 | |||
| About the same | 66.7 | ||
| Less so | 4.7 | ||
| More so | 28.6 | ||
Note. Mean (M) and standard deviation (SD) are unweighted, while percentages (%) are weighted. Race/ethnicity of other included American Indian, Alaskan Native, Asian, and Pacific Islander.
As for limited family social gatherings due to COVID-19, the respondents reported that about two social activities were restricted on average (M=2.0, SD=1.5): 76% canceled family celebrations, 42% were unable to attend in-person funeral for a deceased family member, and 29% were unable to visit a close family member in the hospital. About two-thirds of the sample (69%) reported not having enough in-person contact with people outside the household. Regarding the functional aspects of the social connection, 16% and 25% said that they had received instrumental and emotional support more often compared to before COVID-19, respectively. There were a few people who reported receiving support from others less frequently. About 11% of the sample reported their quality of relationships with family members was worse since the pandemic, and 14% reported worse quality of relationships with friends or neighbors. In this sample, 67% felt lonely about the same compared to before COVID-19, while 29% experienced increased loneliness, and the remaining 5% reported feeling less lonely.
Loneliness Changes Compared to Before COVID-19 by Sociodemographic Groups
Figure 2 shows the percent of older adults who reported feeling more or less lonely during Covid (bars represent 95% confidence intervals) across sociodemographic groups. About 29% of the middle-aged group aged 54–74 reported increased loneliness, which is slightly higher than 27% in the older group aged 75 or above. Women were more likely to report increased loneliness than men (34% vs. 22%). Among the race/ethnic groups, 30% of non-Hispanic Whites experienced increased loneliness, which was significantly higher than 22% in the minority group. At the same time, more adults from the racial/ethnic minority group reported feeling less lonely than their non-Hispanic White counterparts (10% vs. 3%). A greater proportion of those with education of some college or above reported increased loneliness than those with a high school education or less (31% vs. 24%). Supplemental Figure 1 shows sociodemographic differences in changes in social connection, which may provide some of the potential explanations for why each sociodemographic group reported different levels of changes in loneliness.
Figure 2.
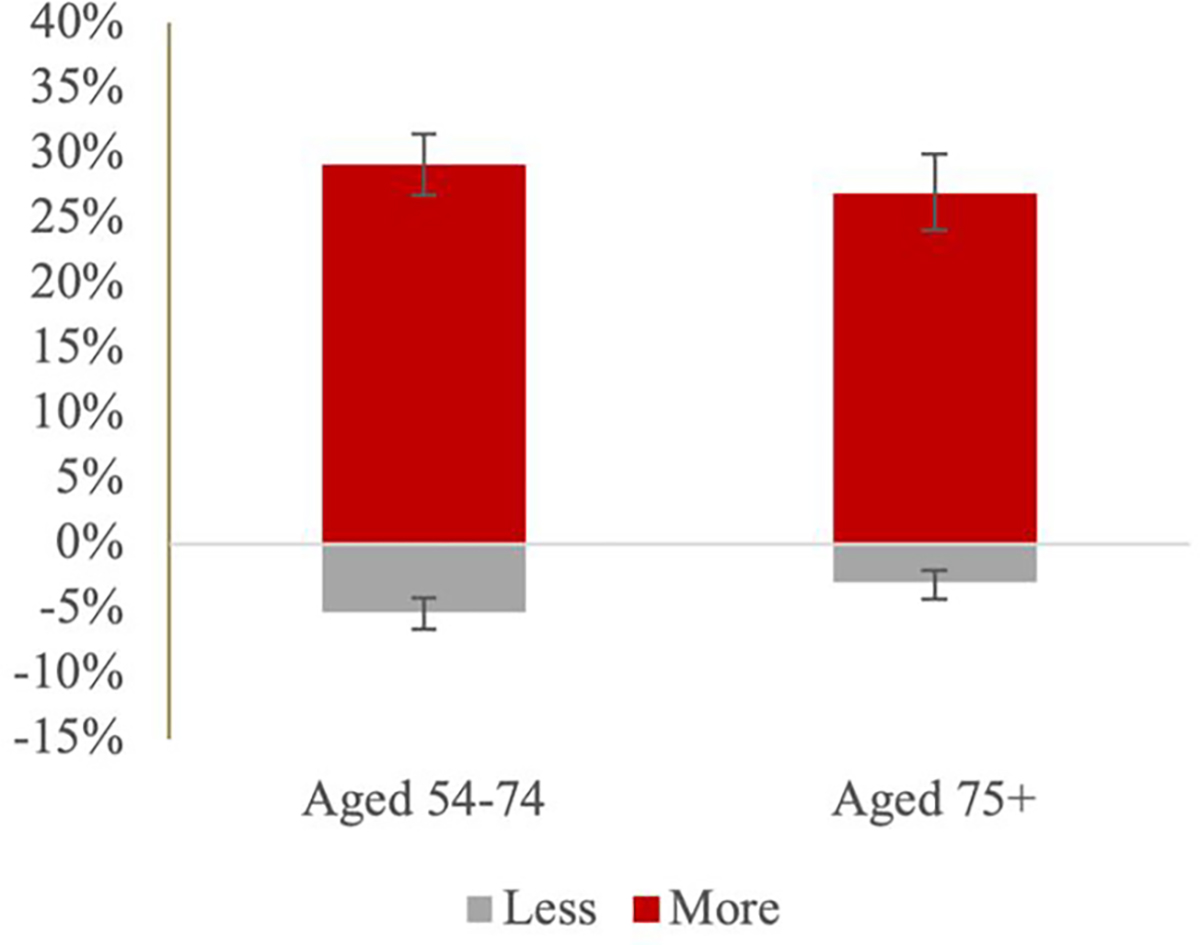
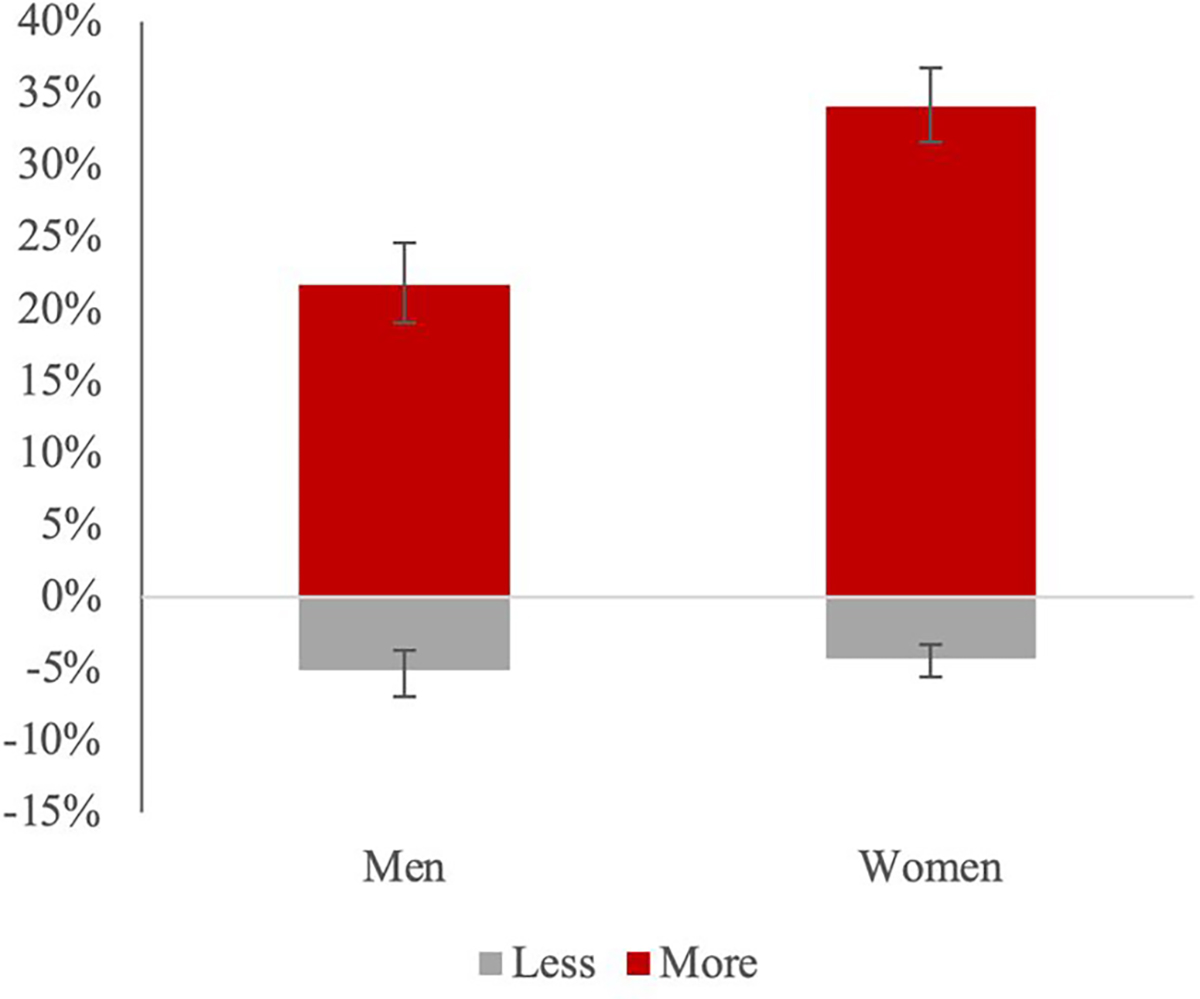
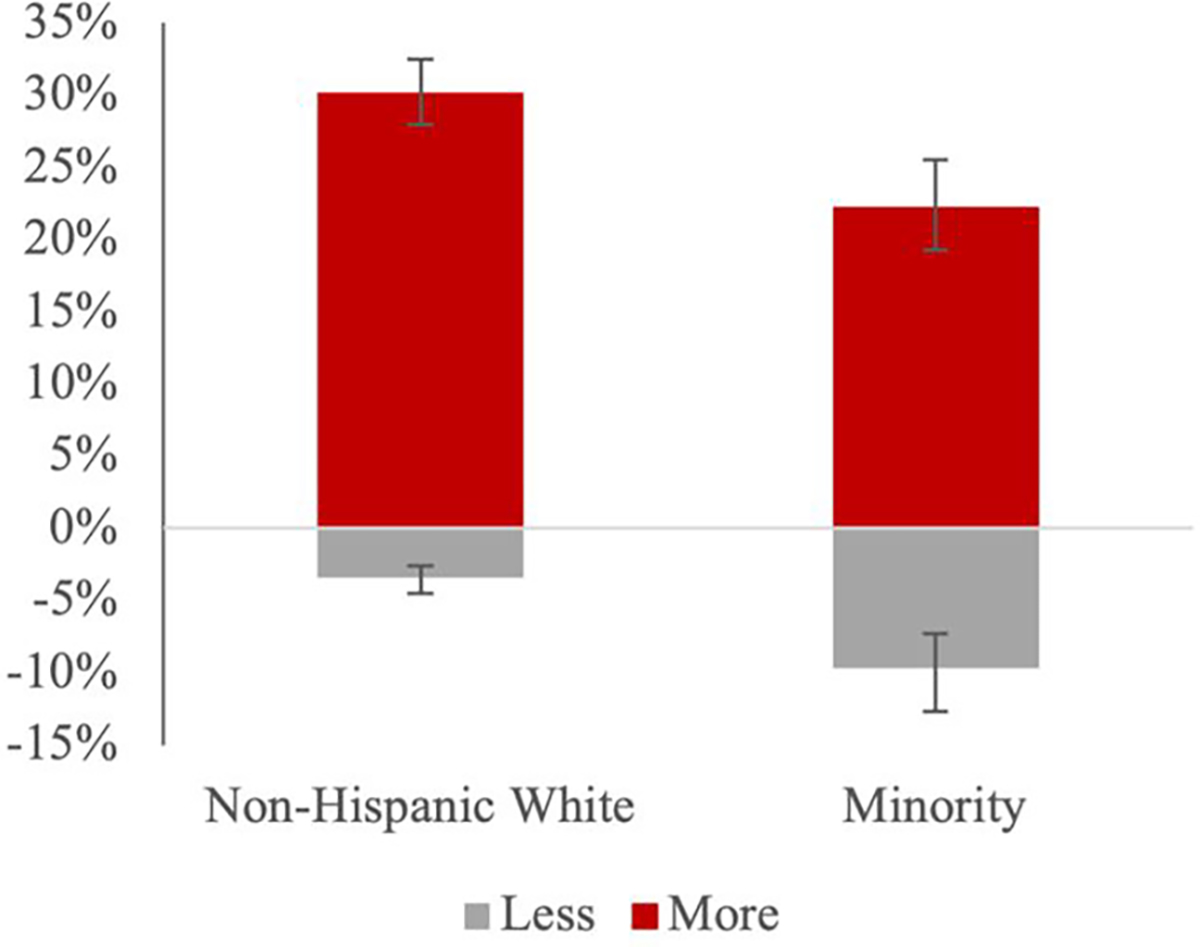
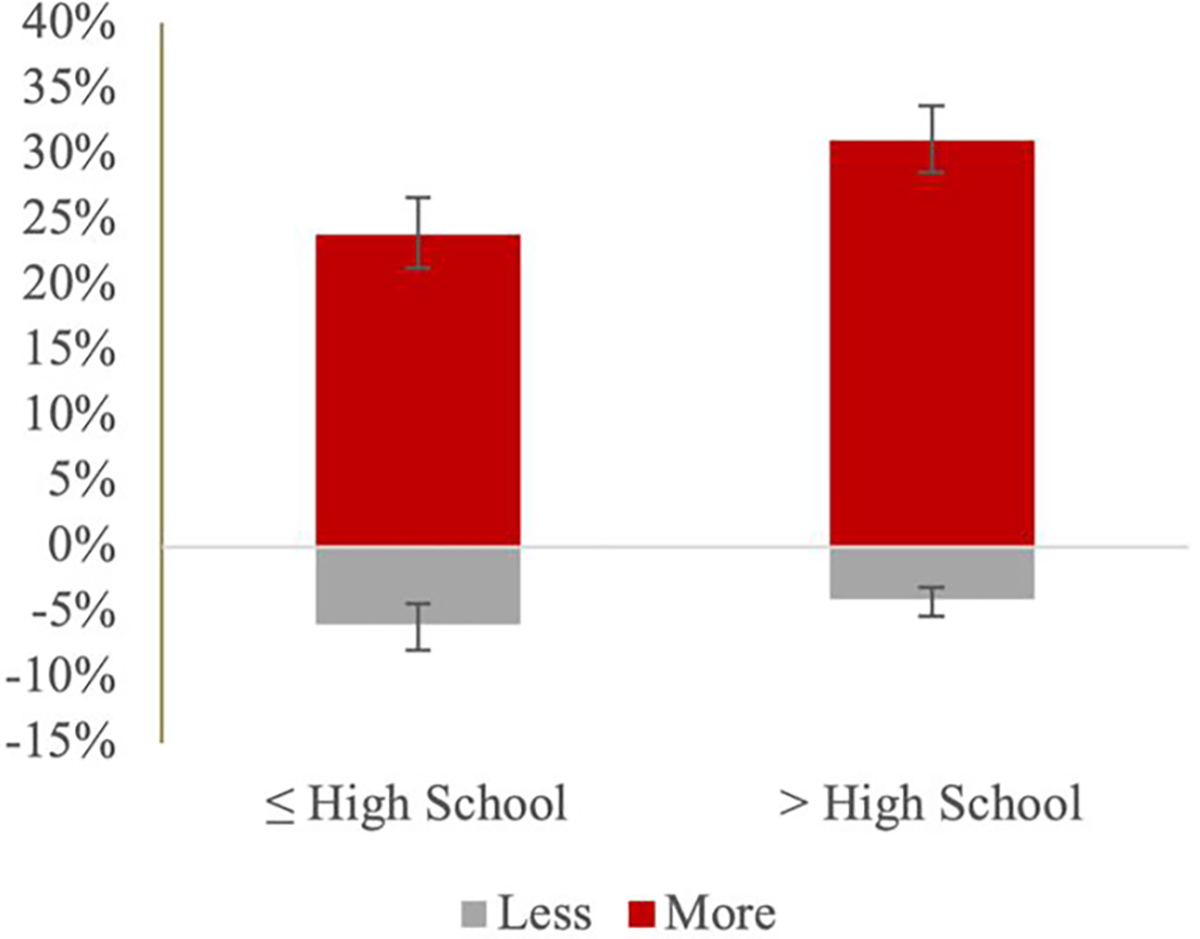
a - Lonely Compared to Before COVID-19
b - Lonely Compared to Before COVID-19
c - Lonely Compared to Before COVID-19
d - Lonely Compared to Before COVID-19
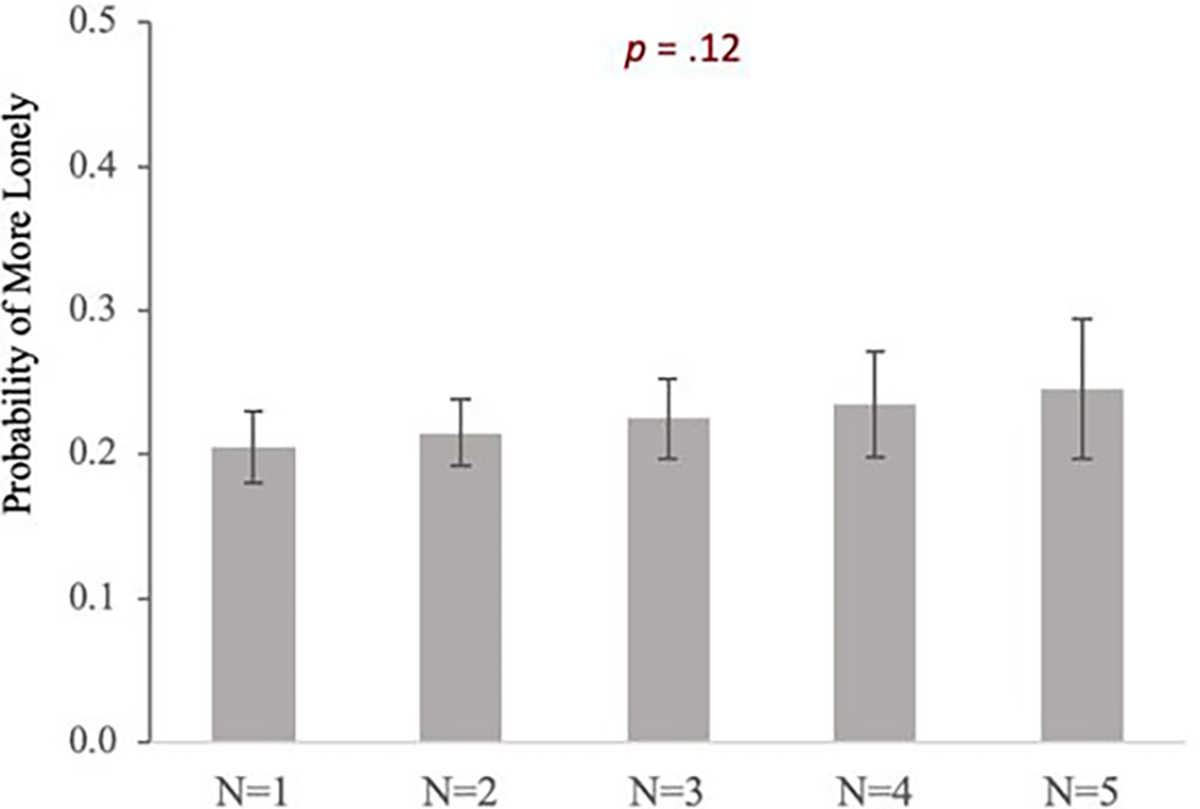
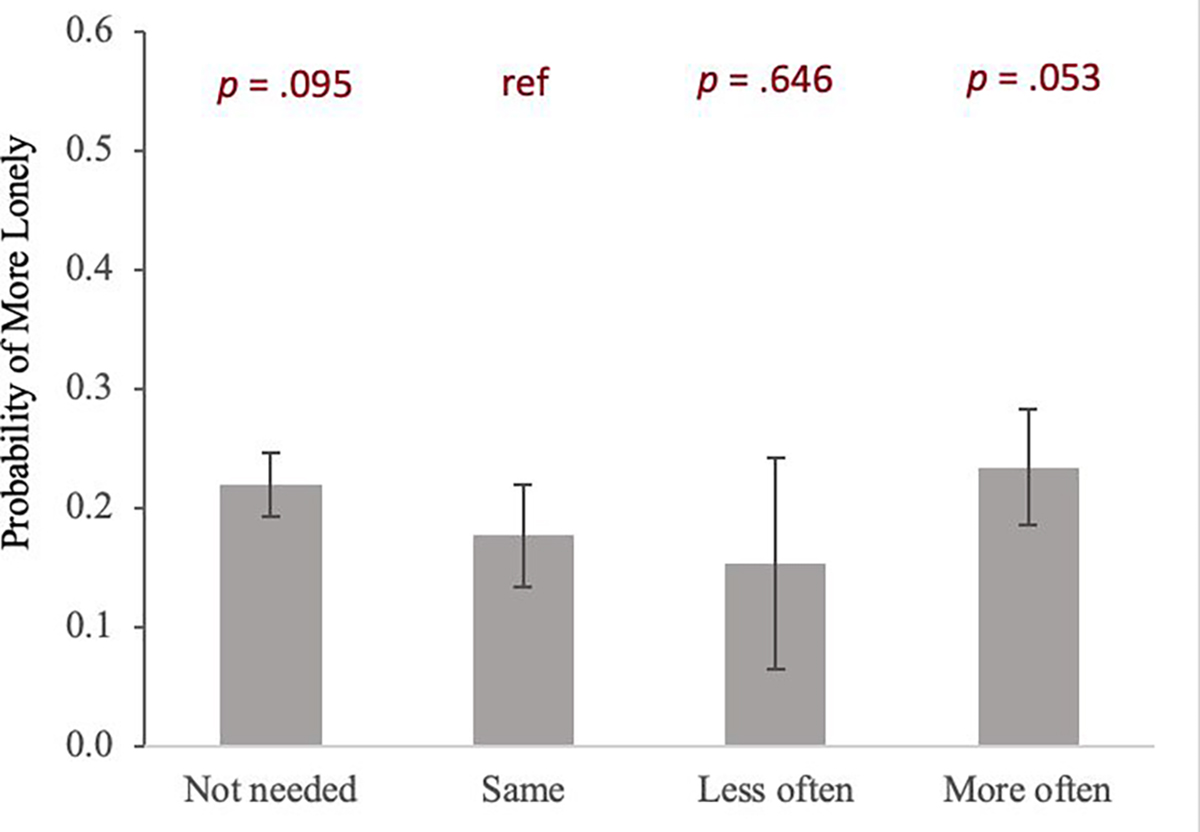
Logistic Regression Models of Increased Loneliness
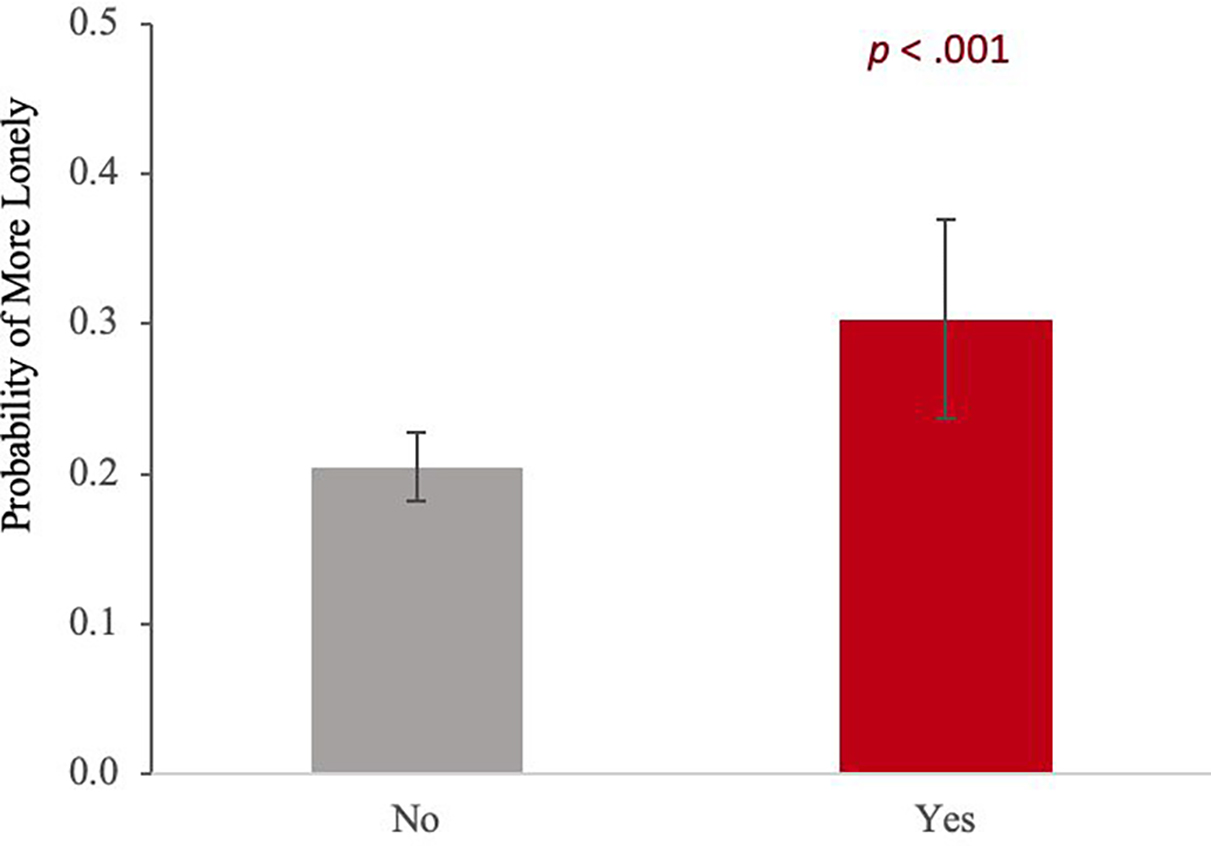
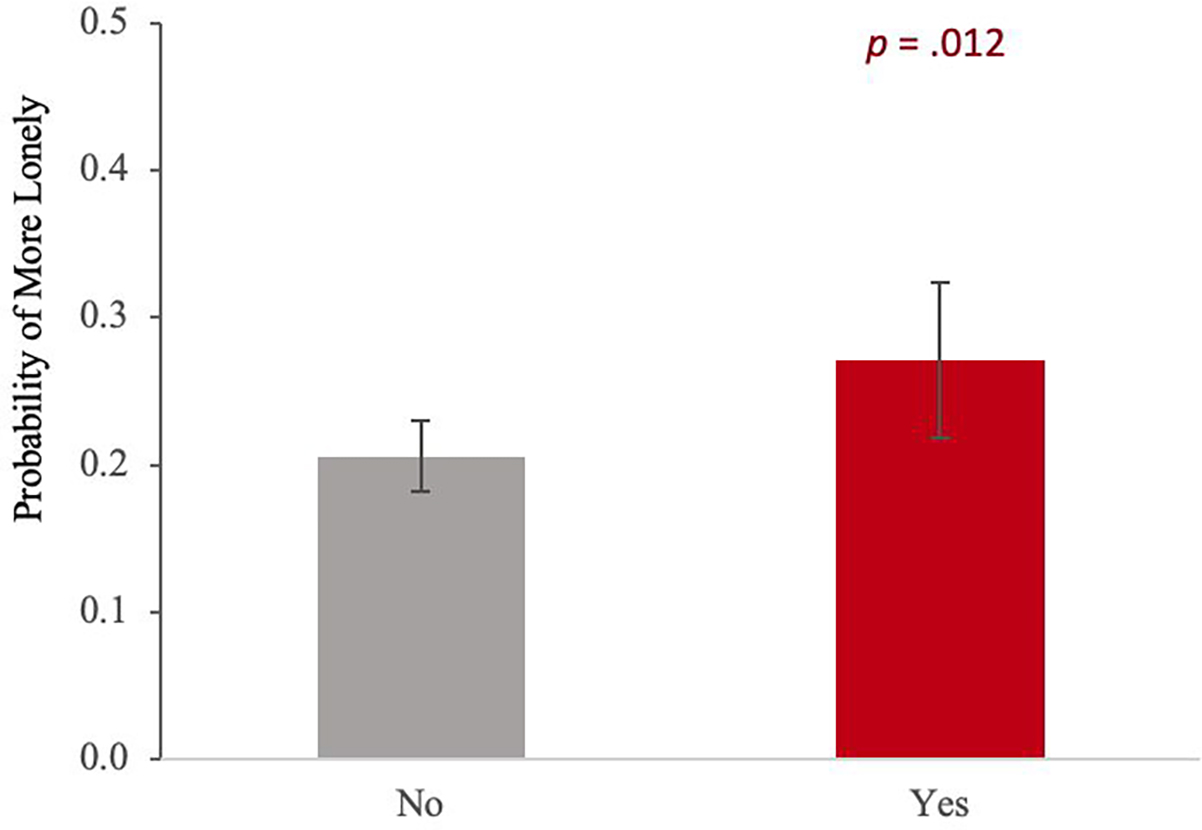
Figure 3 presents the predicted probabilities of increased loneliness by social connection indicators, which was estimated from the logistic regression model of increased loneliness compared to before the pandemic. Full regression results are available in Supplemental Table 1. In terms of structural aspects of social connection, not enough in-person contact with people outside the household was associated with 36% of increased loneliness, which was significantly higher than 5% when having enough contact (OR=10.1; 95% CI=6.88–14.74, p < .001). In addition, Among the functional measures, those who received emotional support more frequently (32%) (OR=2.00, 95% CI=1.53–2.61, p < .001), as well as those who received it less frequently (35%) (OR=2.28, 95% CI=1.13–4.59, p = .021), were more likely to report increased loneliness than those with the same levels of support (19%). Finally, both worse quality of family (30%) (OR=1.69, 95% CI=1.23–2.32, p = .001) and friend/neighbor relationships (27%) (OR=1.44, 95% CI=1.09–1.91, p = .012) were associated with a higher probability of increased loneliness (20% and 21% in their counterparts, respectively). When entered independently into the models adjusting for socio-demographic covariates only, the directions of the associations of each indicator with increased loneliness were similar, but all reached statistically significant levels (see Supplemental Table 2 and Supplemental Figure 2). These findings suggest the correlation shared among the social connection indicators.
Figure 3.
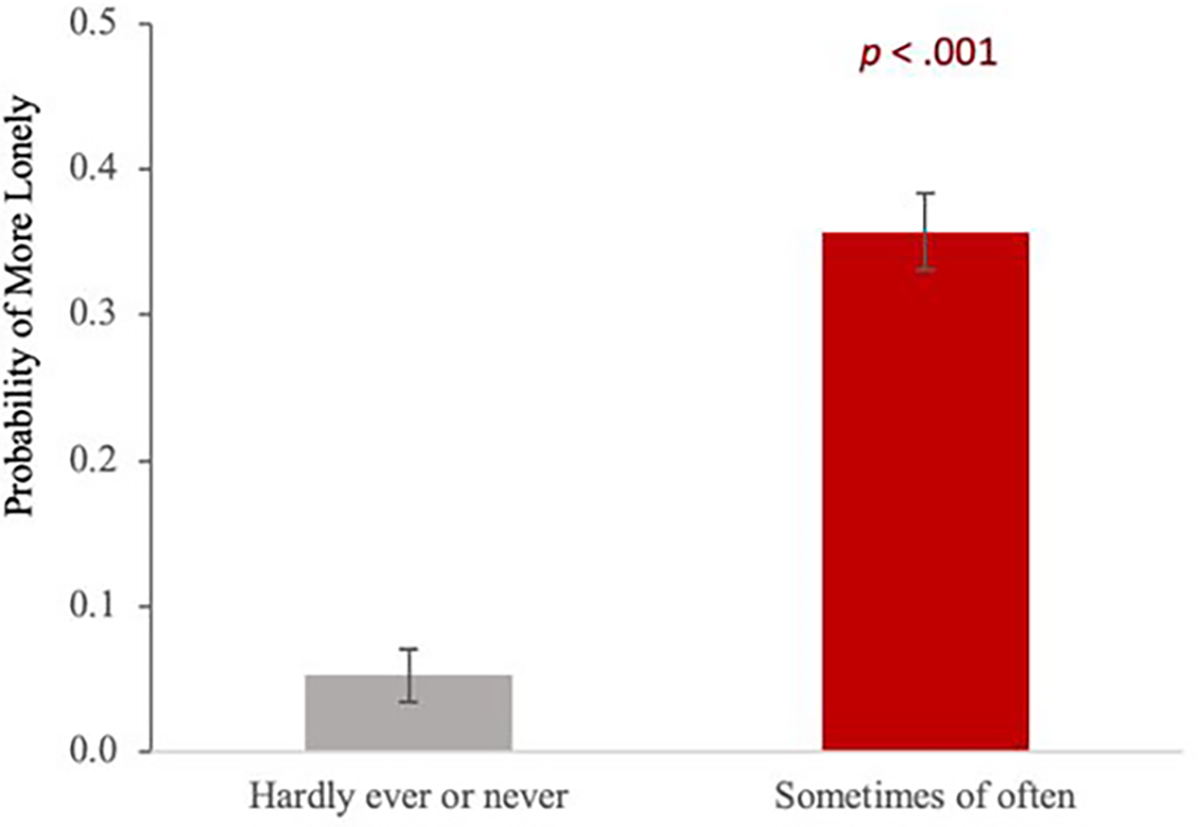
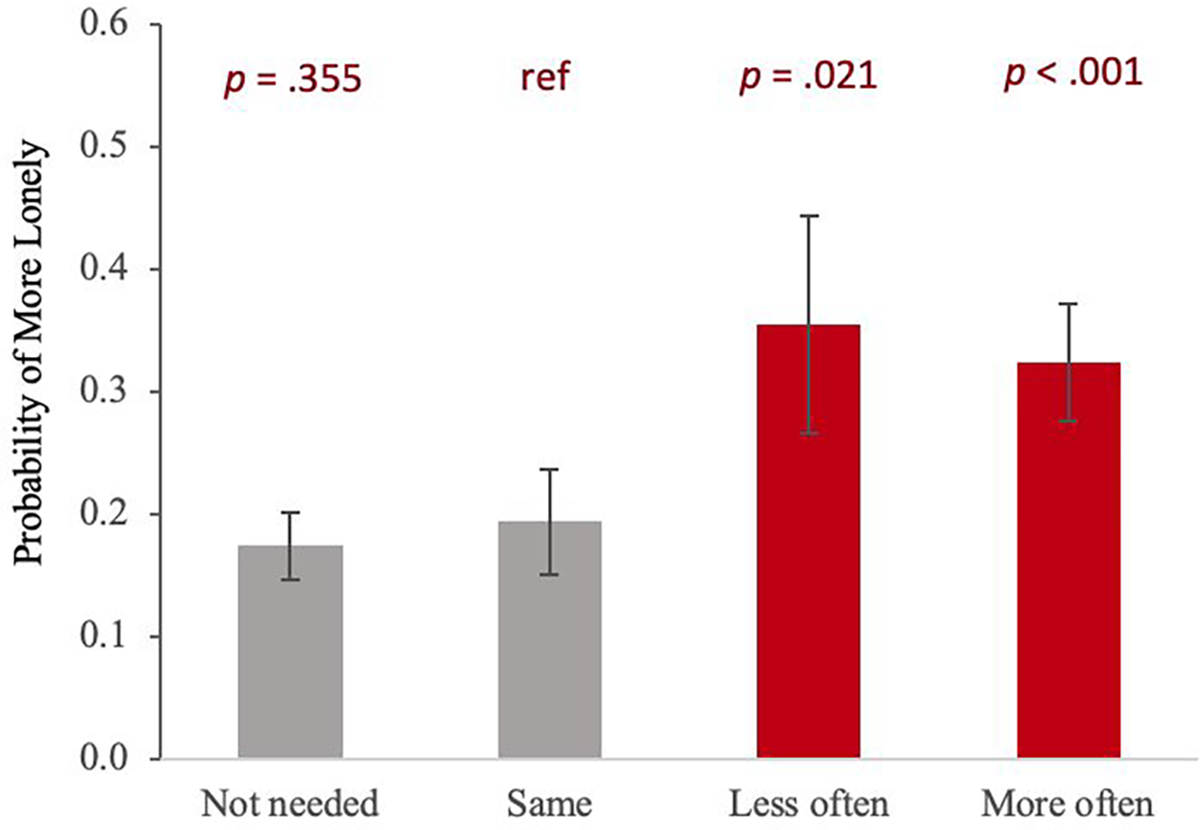
A- a - In-person Contact with People Outside Household
A – b -Limited Family Social Gatherings
Ba - Instrumental Social Support
Bb – Emotional Social Support
Ca – Worse Family Relationships
Cb- Worse Friends/Neighbour Relationships
We also examined differences in the association between social connections and increased loneliness due to COVID-19 by the pre-pandemic loneliness level. As shown in Supplementary Table 3, insufficient in-person contact with non-household people was associated with increased loneliness for both groups and more strongly for the previously lonely group (OR = 20.14, CI = 6.26–64.86). Worse quality of family relationships was significantly associated with increased loneliness for the previously not lonely group (OR = 1.88, CI = 1.22–2.90), while the worse quality of relationships with friends/neighbors was associated with increased loneliness only for the previously lonely group (OR = 2.70, CI = 1.43–5.10).
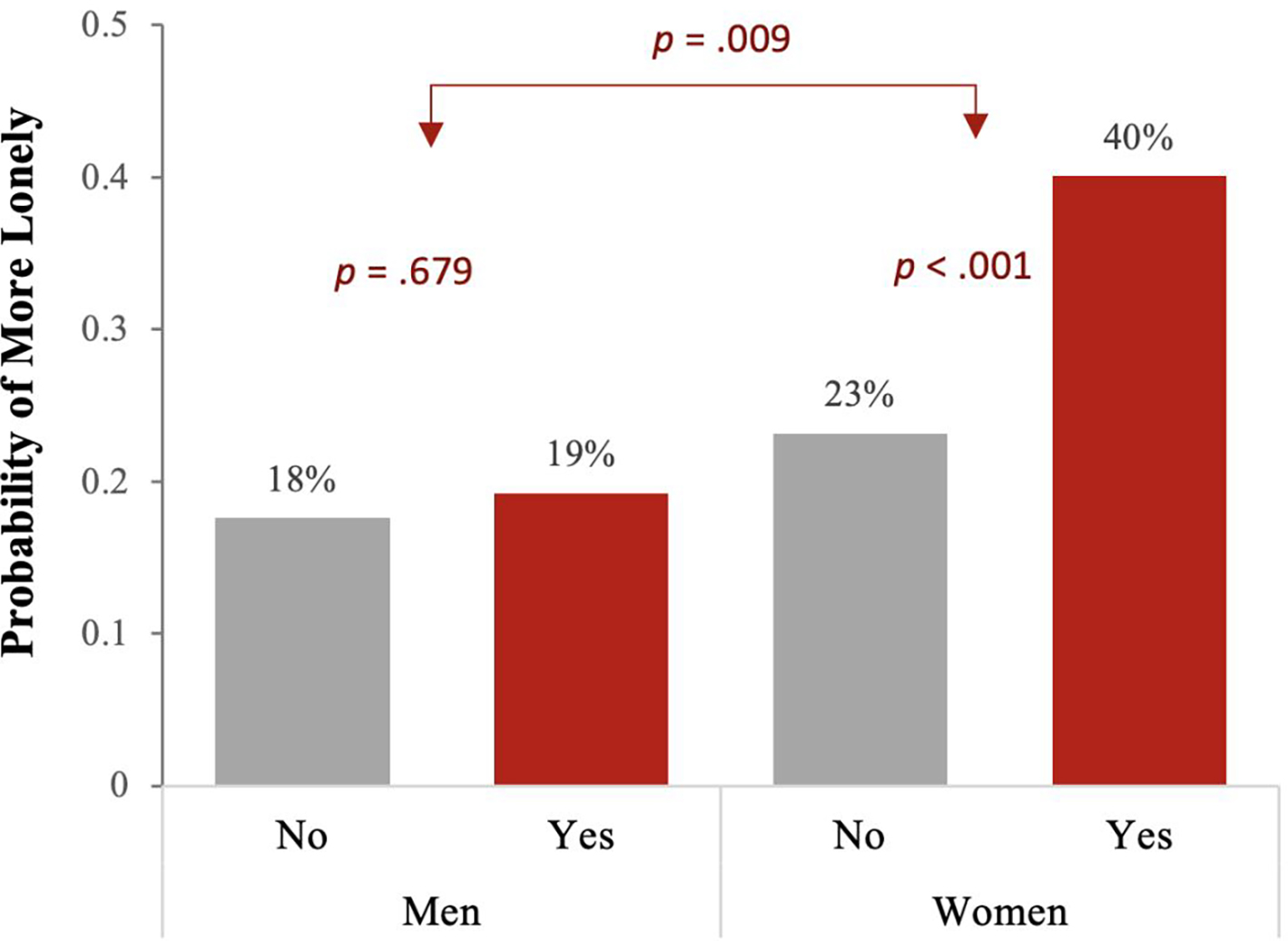
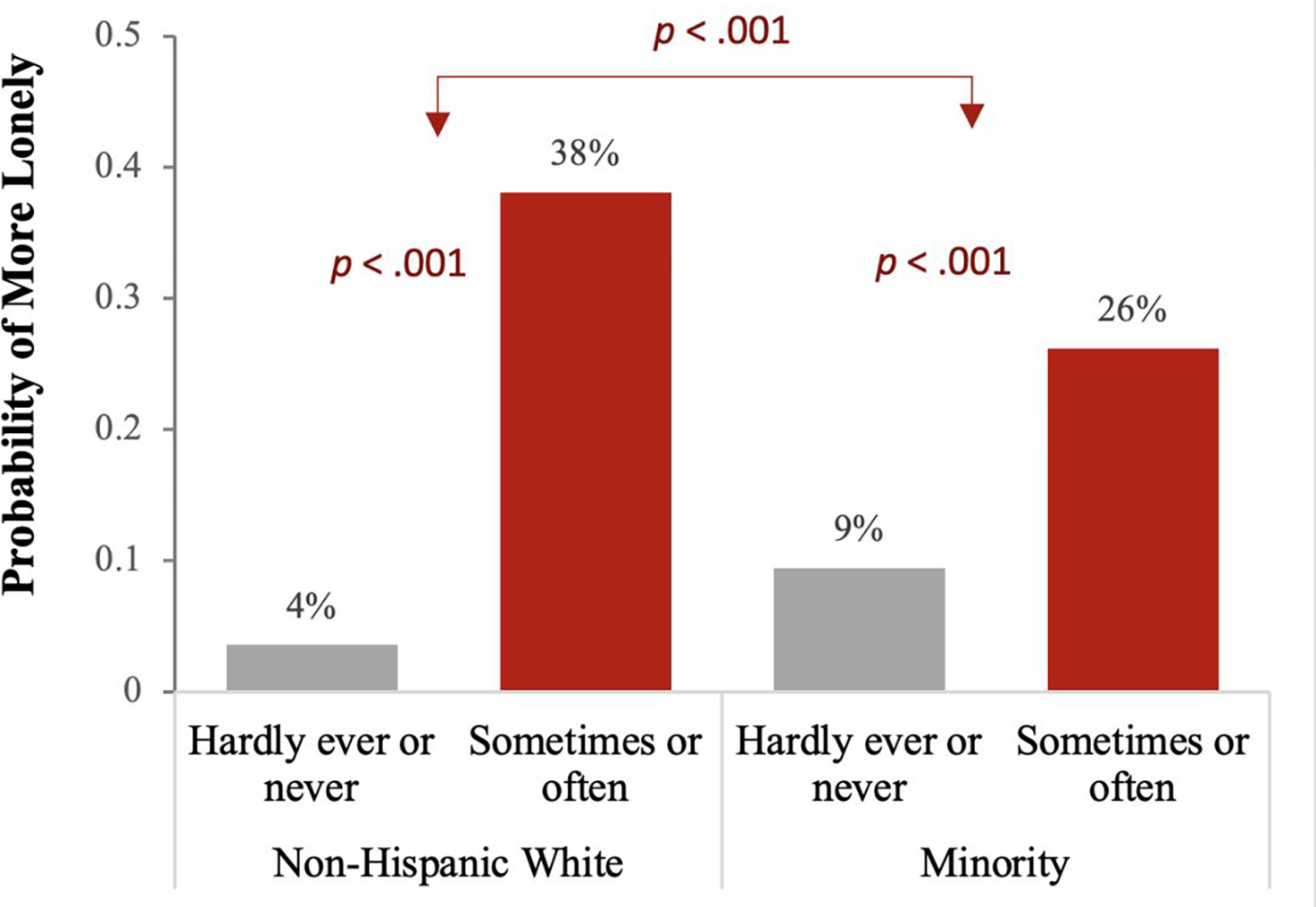
Interaction Effects by Sociodemographic Characteristics
With the same modeling approach, we examined interactions between each significant indicator of social connection and sociodemographic factors to test for differential effects of its effects across sociodemographic groups. A few significant interaction effects were observed as the following: Age groups × not enough in-person contact with people outside the household (OR=0.40, 95% CI=0.19–0.83, p = .014); women × worse quality of relationships with family members (OR=1.99, 95% CI=1.07–3.71, p = .03); racial/ethnic minority × not enough in-person contact with people outside the household (OR=0.21, 95% CI=0.10–0.44, p < .001). Based on the Bonferroni-corrected threshold set at 0.003, only the interactions with race/ethnicity exceeded the significance threshold. To further examine the significant interaction terms, we plotted the predicted probabilities of increased loneliness and performed post-hoc comparisons using contrasts. As presented in Figure 4, not having enough in-person contact with non-household people was more strongly associated with increased loneliness in the middle-aged group and non-Hispanic Whites compared to their older and minority counterparts. The negative effects of worse quality family relationships were stronger among women than men.
Figure 4.
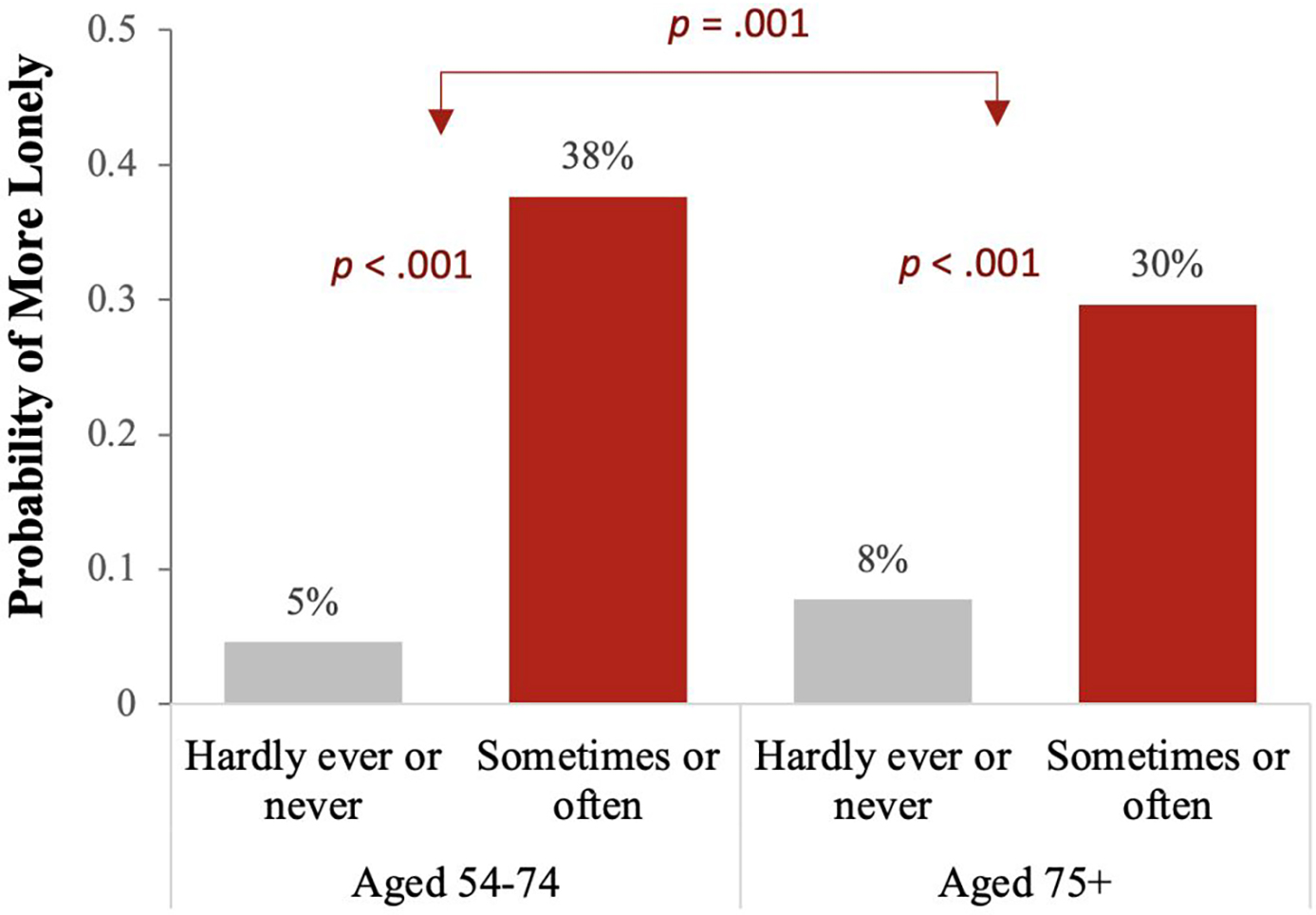
a – Not enough in-person contact with people outside household
b – Worse quality of relationships with family members
c – Not enough in-person contact with people outside household
Discussion
Using data from a nationally representative sample of older U.S. adults aged 50 and above, the present study examined the associations between structural, functional, and quality aspects of social connection and loneliness among older adults in the context of COVID-19, as well as sociodemographic variation in these associations. Our results showed that changes in each aspect of social connection due to COVID-19 were associated with the risk of feeling lonelier. Specifically, those who reported not having enough in-person social contact during COVID-19 had a higher risk of increased loneliness (36% vs. 5%). As expected, people that experienced worse quality of relationships with family members or friends/neighbors since the pandemic more likely to have increased loneliness compared to those that did not have such experiences (30% vs. 20% and 27% vs. 21%, respectively). Interestingly, lack of in-person contact shows a stronger association with increased loneliness in comparison to the quality of relationships. Though it is generally believed that the quality of social connections is equally important as quantity regarding loneliness (Kuczynski et al., 2022), this observation provides an interesting insight that people may feel most isolated when faced with a sudden social shrink in the availability of social resources and support from everyday interactions. Overall, these findings align with the Social Psychology Theory of Loneliness, which argues that an unfulfilled need for social connection leads to loneliness.
It was notable that those receiving emotional support more often as well as less often during COVID-19 were more likely to report increased loneliness than those who reported no changes since the pandemic (32% vs. 19%). This finding was unexpected, as earlier research showed that greater emotional support was associated with less loneliness (van Tilburg et al., 2020; Hu and Gutman, 2021). Unlike these studies, where the respondents reported how much support they received, we focused on whether the respondents had any changes in support since the pandemic. Thus, we cannot rule out the possibility of bi-directionality, such that receiving emotional support more often than before may reflect one’s high vulnerability to social isolation and disconnection.
Furthermore, we found sociodemographic differences in changes in loneliness and social connection. While 29% of the total sample felt lonelier after COVID-19, middle-aged adults, women, non-Hispanic Whites, and the higher education group were more likely to report increased loneliness than their counterparts. Similarly, a handful of previous studies on older adults’ experience of the COVID-19 pandemic reported that middle-aged older adults, men, and non-Hispanic Whites were more vulnerable to social isolation and loneliness than their counterparts (van Tilburg et al., 2020; Whitehead and Torossian, 2021). These findings are counter to our hypothesis based on the resource perspective on loneliness, assuming more vulnerability to loneliness among older adults, men, racial/ethnic minorities, and the lower education group who generally have more limited interpersonal or material resources. Rather, our findings can be understood through a cognitive attributional perspective which emphasizes that loneliness is a consequence of a discrepancy between one’s desired and achieved social relationships (Perlman and Peplau, 1982). Given middle-aged adults, women, and those with higher education have more robust social networks (Davidson, Daly and Arber, 2003; Cornwell, Laumann and Schumm, 2008; DiJulio et al., 2018), they may hold higher expectations of social connections and, thus, be at an elevated risk of experiencing a mismatch between ideal and achieved social relationships during COVID-19. It also should be noted that each sociodemographic group may have a different focus on how they feel connected to others. Increased loneliness for Whites may be due to their greater reliance on friendship-based social networks than Blacks and Hispanics, which are more family-oriented (Ajrouch, Antonucci and Janevic, 2001; Becker et al., 2003; Cudjoe et al., 2020). COVID-19 social mitigation efforts have centered on reducing in-person contact with people outside one’s household (friends and neighbors), which may have affected friendship networks more than family networks.
The supplemental analyses found varying sociodemographic patterns across structural, functional, and quality aspects of social connection. For example, more women reported limited in-person contact with others and family gatherings than men, whereas men received less instrumental and emotional social support. Non-Hispanic Whites were more likely to report not enough in-person contact and worse social relationships with friends or neighbors. More racial/ethnic minorities reported limited family social gatherings but receiving more emotional support. More respondents in the higher education group reported not enough in-person contact, worse friends/neighbor relationships, and receiving instrumental support less frequently than those with high school or less education. These differences may, in part, explain why the COVID-19 pandemic has resulted in increased loneliness more for the groups that were not commonly identified as at-risk. Overall, our findings resonate with the concerns raised early in the pandemic that older adults without previous experience of social isolation may be affected by the social distancing measures due to their lack of coping strategies in the face of the removal of social contacts (Brooke and Jackson, 2020). As older adulthood is characterized by great heterogeneity of health and well-being among individuals, the unintended side-effects of social distancing measures may manifest differently and thus, should be remedied by taking careful consideration of one’s unique characteristics and situation. The current findings add to this discussion and call attention to tailored interventions for each demographic group’s needs as well as further investigations to identify underlying mechanisms.
In interaction analysis, we found sociodemographic differences in the association between each aspect of social connection and increased loneliness. For example, mid-aged adults were more likely to feel lonelier than their older counterparts when not having enough contact with people outside the household (38% vs. 30%). This sizable difference can be interpreted through the lens of the Socioemotional Selectivity Theory (Carstensen, Isaacowitz and Charles, 1999). According to the theory, as our future time perspective becomes shorter, as it typically does with age, people tend to be increasingly selective and invest more effort in emotionally meaningful goals and activities than knowledge acquisition. This means that at older ages, our focus is put more on interactions with family than with connections to people in less intimate relationships. In contrast, distal social networks such as neighbors may have had more powerful impacts in the middle ages, affecting feelings of loneliness. In addition, women are nearly twice as likely to feel lonelier than men when they had worse quality family relationships during COVID-19 (40% vs. 19%). This is in line with prior studies conducted in pre-pandemic (Rossi and Rossi, 2018), and suggests that maintaining a good family relationship may matter more to women’s feelings of loneliness. Further, our findings add to the literature by providing some of the first evidence that women might be more susceptible to the impairment of relationship quality and subsequently increased loneliness triggered by an unexpected event such as the pandemic. In addition, non-Hispanic Whites who reported not enough in-person contact with non-household people were a 1.5 times higher probability to report increased loneliness than other race/ethnic groups (38% vs. 26%). As discussed earlier, COVID-19 and its unintended consequences may have increased loneliness more for older White adults than other groups, partly due to the primary focus of social distancing policies’ on restricting non-household networks (e.g., friendship) than family networks. While further study is required for a better understanding of the observed sociodemographic differences, these findings emphasized the heterogeneous experience of social isolation and loneliness across subgroups of older adults. Our findings also point out the importance of considering different social motives and primary focus on social connections by sociodemographic factors in relation to one’s subjective feelings of social isolation. There is a need to identify how and what specific areas of social connections are influenced by the COVID-19 restrictions for diverse demographic subpopulations, rather than treating older adults as a homogenous group.
Limitations
There are several limitations to be noted when interpreting the study findings. First, our use of the cross-sectional data does not allow for drawing any causal conclusion, though respondents were specifically asked to report how their feelings of loneliness had changed since the start of the pandemic. Second, we could not differentiate between people who answered “no” to questions on limited family social gatherings because they were not able to attend or because they did not have any social gatherings to attend. Third, though we suspect the associations we observed differ by race/ethnicity, we could not conduct subgroup analyses due to small sample sizes of some racial/ethnic minority subgroups (i.e., non-Hispanic Blacks, Hispanics, American Indian, Alaskan Native, Asian, and Pacific Islander). Future research with a larger sample is needed to understand more nuanced associations between social connections during COVID-19 and increased loneliness depending on one’s racial/ethnic background.
Conclusion
The COVID-19 pandemic has amplified the long-standing problems of social isolation and loneliness among the older population. However, this unprecedented situation offers a unique opportunity to observe how people’s feelings of isolation and loneliness may change following an abrupt change in their social connectedness. Our study showed that changes in structural, functional, and quality aspects of social connection during the pandemic substantially increased the risk of feeling lonelier among older adults. Group differences by age, gender, race/ethnicity, and education were found not only for the prevalence of reporting increased loneliness but also for which aspects of social connection are more affected due to COVID-19. We further found that each aspect of social connection was associated with increased loneliness differently across sociodemographic groups. These findings are based on the data collected in the early phase of COVID-19 when the social distancing measures were heavily implemented, so the associations we found may not hold as COVID-19 moves towards endemic. However, individuals continue to practice social distancing measures for new surges and will likely do so for contagious viruses in the future. Our findings, thus, are informative in rethinking the public health policies to allow older adults to be together safely, protecting them from such viruses but also from social isolation.
Supplementary Material
Acknowledgments:
This study was supported by funding from the National Institutes of Health; National Institute on Aging [grant numbers T32-AG000037 and P30-AG017265]. Data used in this study are publicly available from the Health and Retirement Study website: https://hrs.isr.umich.edu/. Study materials and program codes to create analytic data sets shall be made available upon request through the first author’s email. The current research was not preregistered in an independent, institutional registry.
Footnotes
Conflict of interest: The authors have no conflicts of interest to disclose.
References
- AARP Foundation (2020) The Pandemic Effect: A Social Isolation Report. Available at: https://connect2affect.org/wp-content/uploads/2020/10/The-Pandemic-Effect-A-Social-Isolation-Report-AARP-Foundation.pdf.
- Ajrouch KJ, Antonucci TC and Janevic MR (2001) ‘Social Networks Among Blacks and Whites: The Interaction Between Race and Age’, The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 56(2), pp. S112–S118. Available at: 10.1093/geronb/56.2.S112. [DOI] [PubMed] [Google Scholar]
- Becker G et al. (2003) ‘Creating Continuity Through Mutual Assistance: Intergenerational Reciprocity in Four Ethnic Groups’, The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 58(3), pp. S151–S159. Available at: 10.1093/geronb/58.3.S151. [DOI] [PubMed] [Google Scholar]
- Brooke J and Jackson D (2020) ‘Older people and COVID-19: Isolation, risk and ageism’, Journal of Clinical Nursing, 29(13–14), pp. 2044–2046. Available at: 10.1111/jocn.15274. [DOI] [PubMed] [Google Scholar]
- Carlson M et al. (2017) ‘The Brain and Social Connectedness: GCBH Recommendations on Social Engagement and Brain Health’, in. Available at: 10.26419/pia.00015.001. [DOI]
- Carstensen LL, Isaacowitz DM and Charles ST (1999) ‘Taking time seriously: A theory of socioemotional selectivity.’, American Psychologist, 54(3), pp. 165–181. Available at: 10.1037/0003-066X.54.3.165. [DOI] [PubMed] [Google Scholar]
- Cohen S, Gottlieb BH and Underwood LG (2000) ‘Social Relationships and Health’, in Cohen S, Underwood LG, and Gottlieb BH (eds) Social Support Measurement and Intervention. Oxford University Press, pp. 3–26. Available at: 10.1093/med:psych/9780195126709.003.0001. [DOI] [Google Scholar]
- Cornwell B, Laumann EO and Schumm LP (2008) ‘The Social Connectedness of Older Adults: A National Profile’, American Sociological Review, 73(2), pp. 185–203. Available at: 10.1177/000312240807300201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cudjoe TKM et al. (2020) ‘The Epidemiology of Social Isolation: National Health and Aging Trends Study’, The Journals of Gerontology: Series B. Edited by Carr D, 75(1), pp. 107–113. Available at: 10.1093/geronb/gby037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahlberg L (2021) ‘Loneliness during the COVID-19 pandemic’, Aging & Mental Health, 0(0), pp. 1–4. Available at: 10.1080/13607863.2021.1875195. [DOI] [PubMed] [Google Scholar]
- Davidson K, Daly T and Arber S (2003) ‘Older Men, Social Integration and Organisational Activities’, Social Policy and Society, 2(2), pp. 81–89. Available at: 10.1017/S1474746403001118. [DOI] [Google Scholar]
- DiJulio B et al. (2018) ‘Loneliness and Social Isolation in the United States, the United Kingdom, and Japan: An International Survey’, Kaiser Family Foundation; [Preprint]. Available at: http://files.kff.org/attachment/Report-Loneliness-and-Social-Isolation-in-the-United-Statesthe-United-Kingdom-and-Japan-An-International-Survey. [Google Scholar]
- Donovan NJ and Blazer D (2020) ‘Social Isolation and Loneliness in Older Adults: Review and Commentary of a National Academies Report’, The American Journal of Geriatric Psychiatry, 28(12), pp. 1233–1244. Available at: 10.1016/j.jagp.2020.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douglas JA and Subica AM (2020) ‘COVID-19 treatment resource disparities and social disadvantage in New York City’, Preventive Medicine, 141, p. 106282. Available at: 10.1016/j.ypmed.2020.106282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gostin LO and Wiley LF (2020) ‘Governmental Public Health Powers During the COVID-19 Pandemic: Stay-at-home Orders, Business Closures, and Travel Restrictions’, JAMA, 323(21), pp. 2137–2138. Available at: 10.1001/jama.2020.5460. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J et al. (2015) ‘Loneliness and Social Isolation as Risk Factors for Mortality: A Meta-Analytic Review’, Perspectives on Psychological Science, 10(2), pp. 227–237. Available at: 10.1177/1745691614568352. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J et al. (2017) ‘Advancing social connection as a public health priority in the United States’, American Psychologist, 72(6), pp. 517–530. Available at: 10.1037/amp0000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J (2017) ‘The Potential Public Health Relevance of Social Isolation and Loneliness: Prevalence, Epidemiology, and Risk Factors’, Public Policy & Aging Report, 27(4), pp. 127–130. Available at: 10.1093/ppar/prx030. [DOI] [Google Scholar]
- Hu Y and Gutman LM (2021) ‘The trajectory of loneliness in UK young adults during the summer to winter months of COVID-19’, Psychiatry Research, 303, p. 114064. Available at: 10.1016/j.psychres.2021.114064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes ME et al. (2004) ‘A Short Scale for Measuring Loneliness in Large Surveys: Results From Two Population-Based Studies’, Research on Aging, 26(6), pp. 655–672. Available at: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang T-J et al. (2020) ‘Loneliness and social isolation during the COVID-19 pandemic’, International Psychogeriatrics, pp. 1–4. Available at: 10.1017/S1041610220000988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasar KS and Karaman E (2021) ‘Life in lockdown: Social Isolation, Loneliness and Quality of Life in the Elderly During the COVİD-19 Pandemic: A Scoping Review’, Geriatric Nursing [Preprint]. Available at: 10.1016/j.gerinurse.2021.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotwal AA et al. (2021) ‘Social Isolation and Loneliness Among San Francisco Bay Area Older Adults During the COVID -19 Shelter-in-Place Orders’, Journal of the American Geriatrics Society, 69(1), pp. 20–29. Available at: 10.1111/jgs.16865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krendl AC and Perry BL (2021) ‘The Impact of Sheltering in Place During the COVID-19 Pandemic on Older Adults’ Social and Mental Well-Being’, The Journals of Gerontology: Series B. Edited by Isaacowitz DM, 76(2), pp. e53–e58. Available at: 10.1093/geronb/gbaa110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuczynski AM et al. (2022) ‘The effect of social interaction quantity and quality on depressed mood and loneliness: A daily diary study’, Journal of Social and Personal Relationships, 39(3), pp. 734–756. Available at: 10.1177/02654075211045717. [DOI] [Google Scholar]
- Losada-Baltar A et al. (2021) ‘“We Are Staying at Home.” Association of Self-perceptions of Aging, Personal and Family Resources, and Loneliness With Psychological Distress During the Lock-Down Period of COVID-19’, The Journals of Gerontology: Series B. Edited by Issacowitz D, 76(2), pp. e10–e16. Available at: 10.1093/geronb/gbaa048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP (2012) Introduction to Statistical Mediation Analysis. 1st edn. Routledge. Available at: 10.4324/9780203809556. [DOI] [Google Scholar]
- Miller G (2020) Social distancing prevents infections, but it can have unintended consequences, Science | AAAS. Available at: https://www.sciencemag.org/news/2020/03/we-are-social-species-how-will-social-distancing-affect-us (Accessed: 26 July 2020). [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine [NASEM] (2020) Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System. Washington, D.C.: National Academies Press, p. 25663. Available at: 10.17226/25663. [DOI] [PubMed] [Google Scholar]
- Okabe-Miyamoto K and Lyubomirsky S (2021) ‘Social Connection and Well-Being during COVID-19’, in Helliwell JF et al. (eds) World Happiness Report 2021. New York: Sustainable Development Solutions Network, pp. 132–152. Available at: https://worldhappiness.report/ed/2021/social-connection-and-well-being-during-covid-19/#fn3. [Google Scholar]
- Perissinotto CM and Covinsky KE (2014) ‘Living Alone, Socially Isolated or Lonely—What are We Measuring?’, Journal of General Internal Medicine, 29(11), pp. 1429–1431. Available at: 10.1007/s11606-014-2977-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perlman D and Peplau LA (1982) ‘Theoretical approaches to loneliness’, in Letitia Anne P and P. D (eds) Loneliness: A sourcebook of current theory, research and therapy. New York: Wiley. [Google Scholar]
- Rossi AS and Rossi PH (2018) Of Human Bonding: Parent-Child Relations Across the Life Course. 1st edn. Routledge. Available at: 10.4324/9781351328920. [DOI] [Google Scholar]
- Russell DW (1996) ‘UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure’, Journal of Personality Assessment, 66(1), pp. 20–40. Available at: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- Stolz E, Mayerl H and Freidl W (2021) ‘The impact of COVID-19 restriction measures on loneliness among older adults in Austria’, European Journal of Public Health, 31(1), pp. 44–49. Available at: 10.1093/eurpub/ckaa238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tesch-Roemer C and Huxhold O (2019) Social Isolation and Loneliness in Old Age, Oxford Research Encyclopedia of Psychology. Available at: 10.1093/acrefore/9780190236557.013.393. [DOI] [Google Scholar]
- Thayer C and Anderson GO (2018) Loneliness and Social Connections: A National Survey of Adults 45 and Older. AARP Research. Available at: 10.26419/res.00246.001. [DOI] [Google Scholar]
- van Tilburg TG et al. (2020) ‘Loneliness and Mental Health During the COVID-19 Pandemic: A Study Among Dutch Older Adults’, The Journals of Gerontology: Series B. Edited by Carr D, p. gbaa111. Available at: 10.1093/geronb/gbaa111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderWeele TJ and Mathur MB (2019) ‘SOME DESIRABLE PROPERTIES OF THE BONFERRONI CORRECTION: IS THE BONFERRONI CORRECTION REALLY SO BAD?’, American Journal of Epidemiology, 188(3), pp. 617–618. Available at: 10.1093/aje/kwy250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victor CR and Pikhartova J (2020) ‘Lonely places or lonely people? Investigating the relationship between loneliness and place of residence’, BMC Public Health, 20(1), p. 778. Available at: 10.1186/s12889-020-08703-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitehead BR and Torossian E (2021) ‘Older Adults’ Experience of the COVID-19 Pandemic: A Mixed-Methods Analysis of Stresses and Joys’, The Gerontologist, 61(1), pp. 36–47. Available at: 10.1093/geront/gnaa126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong SYS et al. (2020) ‘Impact of COVID-19 on loneliness, mental health, and health service utilisation: a prospective cohort study of older adults with multimorbidity in primary care’, British Journal of General Practice, 70(700), pp. e817–e824. Available at: 10.3399/bjgp20X713021. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


