Abstract
Greater symptom complexity in women, compared with men, could slow ST-elevation AMI (STEMI) recognition and delay door-to-balloon (D2B) times. We sought to determine sex differences in symptom complexity and their relation to D2B times in 1677 young and older patients with STEMI using data from the VIRGO and SILVER-AMI studies. Symptom complexity was defined by the number of symptom patterns or phenotypes and average number of symptoms. The numbers of symptom phenotypes were compared in women and men using Monte Carlo permutation testing. Groups were also compared using generalized linear regression and logistic regression. The number of symptom phenotypes (244 vs. 171, p=0.02), mean number of symptoms (4.7 vs. 4.2, p<0.001), and mean D2B time (114.6 vs 97.8 minutes, p=0.004) were greater in young women as compared with young men but were not significantly different in older women as compared with older men. Regression analysis did not show a relationship between symptom complexity and D2B time overall, although chest pain was a significant predictor of D2B times, and young women were more likely to report symptoms other than chest pain. Of STEMI patients, 36% did not receive PCI, which was associated with presentation delay > 6 hours. In STEMI patients with either D2B time ≥90 minutes or no PCI, women had significantly more symptom phenotypes overall and in VIRGO but not in SILVER-AMI. In conclusion, markers of symptom complexity were not associated with D2B time overall but a greater number of symptom phenotypes in young women was associated with prolonged D2B time or no PCI. In addition, greater frequency of non-chest pain symptoms in young women may have also slowed the recognition of STEMI and D2B times in young women. Further research on symptoms clusters is needed to improve the recognition of STEMIs to improve the D2B times in young women.
Keywords: ST-elevation myocardial infarction, door-to-balloon time, gender disparities, symptom phenotypes, diagnostic reasoning
Introduction
Studies have consistently shown that average door-to-balloon times are longer in women, which has implications for their outcomes.1–6 A possible reason for the longer door-to-balloon times in women may be related to symptom presentation. Women are marginally less likely to have chest pain and more likely to have atypical symptoms,7–10 which may obscure the initial diagnosis, causing delays in the door-to-balloon time. Two recent studies examined sex differences in symptom patterns, or symptom phenotypes, in young and older patients with acute myocardial infarction (AMI),11,12 but these studies did not assess whether greater symptom complexity was associated with longer door-to-balloon times. If symptom complexity makes AMI recognition more difficult,13 it could have a detrimental effect on door-to-balloon times in patients with STEMI. Accordingly, the aim of this study is to examine how symptom complexity affects door-to-balloon times, whether that relationship varies by sex, and whether symptom complexity explains door-to-balloon times sex differences.
Methods
The study population included young patients with AMI from the VIRGO study14 and older patients with AMI from the SILVER-AMI study.15 Patients enrolled in both studies met the criteria for the Third Universal Definition of AMI.16 Patients were enrolled in both studies at the time of hospitalization and underwent comprehensive, structured interviews at baseline by local research coordinators. Further abstraction of medical records was performed by the Yale Coordinating Center for in-depth chart review. The Institutional Review Boards at each institution approved both studies and all participants provided informed consent.
The VIRGO study is the largest prospective observational study of young women and men with AMI in the US.14 The VIRGO study prospectively collected information on 3501 young women and men (18–55 years) hospitalized for AMI in 103 hospitals in the United States and 24 hospitals in Spain between August 2009 and January 2012. The VIRGO study focused on the characteristics of young women with AMI and therefore enrolled patients using a 2:1 female-to-male enrollment ratio.
The SILVER-AMI study is a large prospective study of older patients (≥75 years old) with AMI.15 The SILVER-AMI study prospectively collected information on 3041 participants from 94 hospitals between January 2013 and June 2018.
In the VIRGO and SILVER-AMI studies, each patient was interviewed by a trained local research coordinator who specifically asked and systematically recorded the patient’s presenting symptoms. The symptoms that were recorded for each study are listed in Table 1. Most of the symptoms were identical for the two studies and for symptoms that were different, we matched symptoms by performing additional searches of transcribed symptoms to create the comparable symptoms between the two studies (Table 1). Having matched the symptoms between the two studies, the data from both studies were unified for further analysis.
Table 1.
Symptoms recorded in VIRGO and SILVER-AMI and Matched Symptoms
| VIRGO | SILVER-AMI | Matched Symptoms |
|---|---|---|
| Chest pain | Chest pain | Chest pain |
| Dizziness | Light-headed | Dizziness/Lightheadedness |
| Indigestion | Indigestion/epigastric pain | Indigestion/epigastric pain |
| Nausea | Nausea/vomiting/belching | Nausea/vomiting/belching |
| Other pain/discomfort | Radiation | Radiating or other pain |
| Palpitations | Anxiety/stress/agitation | Anxiety/agitation/palpitations |
| Shortness of breath | Dyspnea | Dyspnea |
| Sweating | Diaphoresis | Diaphoresis |
| Weakness/fatigue | Weakness/fatigue | Weakness/fatigue |
| Confusion | Confusion | Confusion |
Patients who presented with STEMI and received emergency PCI within 12 hours of presentation were defined as the D2B Sample for both study populations.
Symptoms obtained by standardized interviews in both studies were analyzed by combining the symptoms in individual patients into combinations, or symptom phenotypes, as in the two prior studies.11,12 In both the VIRGO and SILVER-AMI studies, trained personnel conducted review of the medical charts during the index AMI admission to record sociodemographic factors and medical history, including cardiac risk factors, co-morbid conditions, AMI type, presentation delay, and door-to-balloon time.
In both the VIRGO and SILVER-AMI studies, there were unequal numbers of women and men, which could bias the comparison of the number of phenotypes in women and men by affecting to ability to detect rare symptom phenotypes in a smaller group of patients. To overcome this source of potential bias, we used Monte Carlo permutation testing as the primary method for analyzing the differences in the number of symptom phenotypes between women and men.
For Monte Carlo permutation analysis, patients’ sexes were randomly permuted to generate 99,999 data sets reflecting the null hypothesis that any difference in the number of phenotypes was due to the unequal sample sizes for women and men rather than the effect of sex. This analysis created an empirical distribution of the differences between women and men in the number of phenotypes for significance testing. The median of the empirical distribution was interpreted as an estimate of the difference in the number of phenotypes between women and men that would have been expected due to differences in the sample sizes alone and the P value was the proportion of the empirical distribution showing differences as large or larger than the differences between sexes observed in the original VIRGO or SILVER-AMI data.
Comparisons of door-to-balloon times were performed between young and older patients from the two study populations and between women and men in each study. Since the observed door-to-balloon times were best described by an inverse Gaussian distribution (rather than normal or gamma), the effects of sex, study, number of symptoms, individual symptoms, and other factors on door-to-balloon time were analyzed via generalized linear regression, using the identity link and an inverse Gaussian distribution. The effects of sex and study on symptom counts were analyzed via negative binominal regression, and the effects of sex and study on the presence of individual symptoms were analyzed via logistic regression. In each of these regression analyses, sex and study were allowed to interact.
Since number of symptom phenotypes is a property of a group rather than an individual, it was not possible to analyze the effect of the number of symptom phenotypes using door-to-balloon time as a patient-level continuous variable, so we divided patients into subgroups according to whether the reported door-to-balloon time was < 90 minutes or ≥ 90 minutes. We arbitrarily chose a 90-minute cutoff given that 90 minutes is a commonly used threshold for door-to-balloon time. We also compared patients with door-to-balloon time < 90 minutes with patients with door-to-balloon time ≥ 90 minutes combined with STEMI patients who did not receive PCI. The resulting groups were compared using the methods described above (but using logistic regression to model door-to-balloon time subgroups rather than a generalized linear model of the door-to-balloon time itself).
As these analyses are exploratory in nature, a two-sided significance threshold of .05 was used throughout, except for the comparisons of frequencies of individual symptoms; here, the Hochberg procedure was used to maintain an overall type 1 error rate of .05 across the 40 comparisons (10 symptoms × [2 comparisons of sex within study + 2 comparisons of study within sex]). Mean values were reported ± standard deviations and median values were reported with interquartile ranges (IQRs). Model comparisons were based on the Akaike information criterion as modified for finite samples (AICC), which balances model fit with parsimony by penalizing models with more parameters.17 All analyses were conducted using SAS/STAT software, version 15.2 (SAS Institute, Inc, Cary, NC).
Results
There were 3501 patients in the VIRGO study (2349 women and 1152 men) and 3041 patients (1346 women and 1645 men) in the SILVER-AMI study, for a total of 6542 AMI patients. STEMI was diagnosed in 1811 (52%) of the VIRGO patients and 797 (26%) of the SILVER-AMI patients. The D2B Sample (STEMI patients receiving emergency PCI within 12 hours of arrival) consisted of 1167 VIRGO patients (717 women and 450 men) and 510 SILVER-AMI patients (228 women and 282 men) for a total of 1677 patients (Figure 1).
Figure 1.
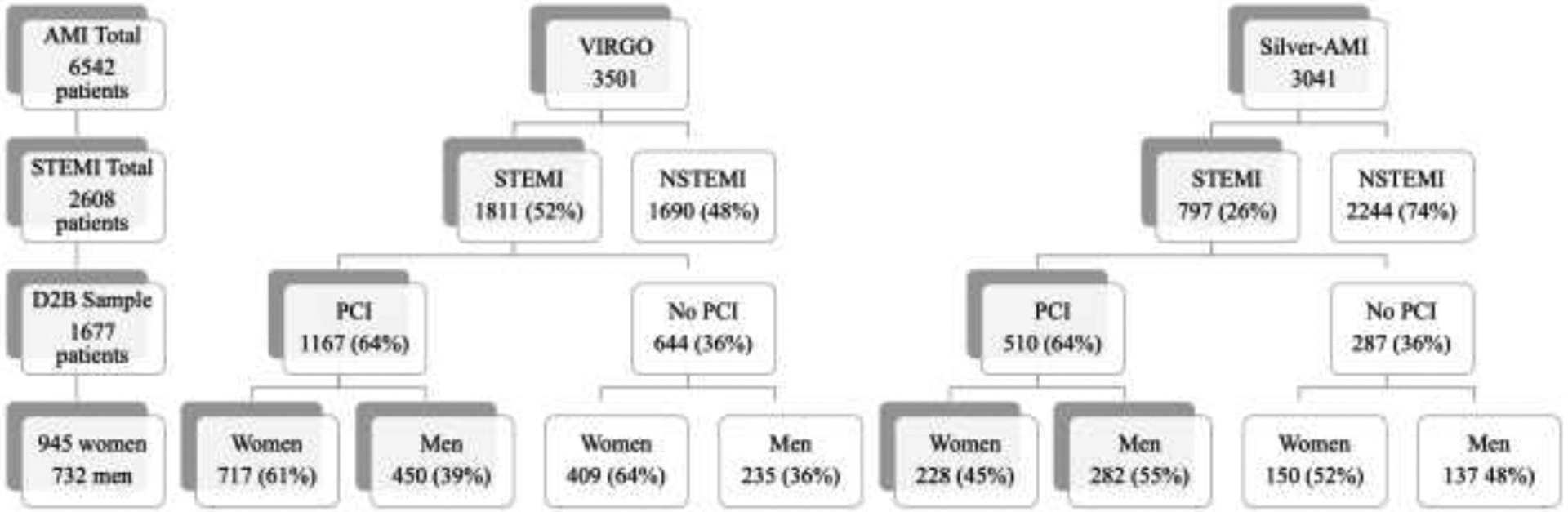
Flow chart showing selection of study patients from VIRGO and SILVER-AMI. AMI=acute myocardial infarction, STEMI=ST-elevation myocardial infarction, NSTEMI=non-ST-elevation myocardial infarction, D2B=door-to-balloon, PCI=percutaneous coronary intervention.
Baseline demographic characteristics of patients in the D2B Samples from both studies are shown in Table 2. Older patients were more likely to live alone, and young patients were more likely to have a presentation delay; otherwise, the subgroups were similar.
Table 2.
Demographic Characteristics of Patients in the D2B Sample from the VIRGO and SILVER-AMI Studies.
| VIRGO D2B Sample (1167) | SILVER-AMI D2B Sample (510) | |||
|---|---|---|---|---|
| Women (717, 61%) | Men (450, 39%) | Women (228, 45%) | Men (282, 55%) | |
| Age in years (mean ±SD) | 46.9 ± 6.2 | 47.0 ± 5.8 | 82.3 ± 5.2 | 80.7 ± 4.8 |
| Race | ||||
| White | 578 (81%) | 379 (84%) | 200 (88%) | 258 (92%) |
| Black | 108 (15%) | 41 (9%) | 25 (11%) | 11 (4%) |
| Other | 31 (4%) | 30 (7%) | 3 (1%) | 13 (5%) |
| Hispanic | 36 (5%) | 36 (8%) | 2 (1%) | 14 (5%) |
| Education | ||||
| Less than high school | 153 (21%) | 60 (13%) | 27 (12%) | 33 (12%) |
| High school graduate or GED | 413 (58%) | 268 (60%) | 115 (50%) | 113 (40%) |
| Two-year or four-year college degree | 111 (16%) | 81 (18%) | 66 (29%) | 87 (31%) |
| Graduate or post-graduate degree | 40 (6%) | 41 (9%) | 19 (8%) | 49 (17%) |
| Married or living as married/living with partner | 394 (55%) | 282 (63%) | 76 (33%) | 203 (72%) |
| Living alone | 82 (11%) | 77 (17%) | 104 (46%) | 81 (29%) |
| Presentation delay of 6 hours or more | 242 (34%) | 110 (25%) | 32 (14%) | 36 (13%) |
| Diabetes | 223 (31%) | 66 (15%) | 61 (27%) | 75 (27%) |
In the D2B Sample of the VIRGO study, there were 244 symptom phenotypes in women and 171 symptom phenotypes in men. The difference of 73 symptom phenotypes was significantly greater than the difference of 52 that would have been expected if the difference was merely due to differences in sample size (p=0.02).
In the D2B Sample of the SILVER-AMI study, there were 122 symptom phenotypes in women and 144 symptom phenotypes in men. The difference of 22 symptom phenotypes was not significantly different from the difference of 20 that would have been expected if the difference was merely due to differences in sample size (p=0.60).
The 10 top-ranked symptom phenotype subgroups from both studies are listed in Table 3. For the VIRGO D2B Sample patients, the symptom phenotypes were more broadly distributed, as only 21% of the women had one of the top 10 symptom phenotypes, as compared to 29% in men (p=0.002). The top 10 symptom phenotypes tended to be more complicated descriptions of symptoms for young women than for other subgroups, as shown in Table 3. For the SILVER-AMI D2B Sample patients, the proportion of women and men with one of the top 10 symptom phenotypes was not significantly different (34% in women versus 37% in men, p=0.47).
Table 3.
Top Ten Symptom Phenotypes in Women and Men in the D2B Samples from the VIRGO and SILVER-AMI Studies.
| VIRGO Study | SILVER-AMI Study | |||||||
|---|---|---|---|---|---|---|---|---|
| Women (%) | Men (%) | Women (%) | Men (%) | |||||
| 1 | chest pain | 1.7 | chest pain | 1.3 | chest pain, radiation | 1.3 | chest pain | 2.0 |
| 2 | chest pain, nausea/vomiting/belching, radiation, diaphoresis | 1.3 | chest pain, diaphoresis | 1.1 | chest pain | 0.7 | chest pain, radiation | 0.9 |
| 3 | chest pain, radiation, diaphoresis | 1.0 | chest pain, radiation | 1.1 | chest pain, dyspnea | 0.5 | no symptoms reported | 0.7 |
| 4 | chest pain, radiation | 0.8 | chest pain, radiation, diaphoresis | 1.0 | no symptoms reported | 0.4 | chest pain, diaphoresis | 0.7 |
| 5 | chest pain, dyspnea, diaphoresis | 0.7 | chest pain, nausea/vomiting/belching, radiation, diaphoresis | 0.7 | chest pain, radiation, dyspnea, diaphoresis | 0.4 | chest pain, radiation, diaphoresis | 0.4 |
| 6 | chest pain, nausea/vomiting/belching, diaphoresis | 0.7 | chest pain, dyspnea | 0.7 | chest pain, nausea/vomiting/belching, radiation | 0.4 | chest pain, radiation, dyspnea | 0.4 |
| 7 | chest pain, nausea/vomiting/belching, radiation, dyspnea, diaphoresis | 0.7 | chest pain, radiation, dyspnea, diaphoresis | 0.6 | chest pain, radiation, dyspnea | 0.4 | chest pain, indigestion/epigastric pain | 0.4 |
| 8 | Chest pain, light-headed, nausea/vomiting/belching, radiation, dyspnea, Diaphoresis, weakness/fatigue | 0.7 | chest pain, radiation, dyspnea | 0.5 | Radiation, diaphoresis | 0.2 | chest pain, dyspnea | 0.3 |
| 9 | chest pain, indigestion/epigastricPain, nausea/vomiting/belching, radiation, dyspnea, diaphoresis, weakness/fatigue | 0.7 | chest pain, nausea/vomiting/belching, diaphoresis | 0.5 | indigestion/epigastricpain, nausea/vomiting/belching | 0.2 | radiation | 0.2 |
| 10 | chest pain, light-headed, indigestion/epigastric Pain, nausea/vomiting/belching, radiation, anxiety/stress/agitation, Dyspnea, diaphoresis, weakness/fatigue | 0.7 | chest pain, diaphoresis, weakness/fatigue | 0.4 | chest pain, diaphoresis | 0.2 | chest pain, weakness/fatigue | 0.2 |
In the D2B Sample of the VIRGO study, the mean number of symptoms in women was 4.7 ± 2.1 in women as compared with 4.2 ± 2.0 in men (p<0.0001). In the D2B Sample of the SILVER-AMI study, the difference in mean number of symptoms in women and men was not statistically significant (3.5 ± 1.9 vs 3.2 ± 1.9, p=0.08). The mean number of symptoms was significantly greater in VIRGO than in SILVER-AMI in both women and men (p<0.0001).
Neither the main effect of sex nor that of study was statistically significant in a generalized linear model containing only these predictors of door-to-balloon times, although their interaction was statistically significant (p=0.02). Examining the simple effects of sex within study, we found that in the VIRGO study, the door-to-balloon time was significantly longer in women (mean=114.6 ± 93.5, median=86.0, IQR=79.5 minutes) than men (mean=97.8 ± 78.4, median=77.5, IQR=62.0 minutes, p=0.004), while in the SILVER-AMI study, the door-to-balloon time was not significantly different between women (mean=106.6 ± 96.2, median=76.0, IQR=73.0 minutes) and men (mean=109.2 ± 103.4, median=77.5, IQR=69.0 minutes, p=0.7116).
Adding the number of symptoms or number of symptoms other than chest pain did not yield significant effects or improve the model, regardless of whether these variables were treated as linear or categorical predictors.
When chest pain was added to the model, the interaction of sex and study became nonsignificant, effectively being replaced by an interaction of study and chest pain (p=0.008), likely because chest pain was more likely to occur in VIRGO women as compared with SILVER-AMI patients. The pattern of simple effects of chest pain on door-to-balloon time within study mirrored that of sex within study in the previous model: significantly longer in those without chest pain (mean=130.8 ± 119.7, median=91.0, IQR=80.0 minutes) than those with chest pain (mean=105.6 ± 83.8, median=82.0, IQR=67.0 minutes, p=0.03) in VIRGO but not in SILVER-AMI (without chest pain: mean=97.2 ± 58.4, median=79.5, IQR=73.0 minutes; with chest pain: mean=110.6 ± 107.5, median=76.0, IQR=70.0 minutes; p=0.11).
A model including sex, study, and delayed presentation (≥ 6 hours) produced a main effect for delay (with delay: mean=123.4 ± 100.7, median=92.0, IQR=90.5 minutes; without delay: mean=102.9 ± 88.4, median=78.0, IQR=65.0 minutes; p=0.004) with the sex by study interaction becoming marginal (p=0.06), while a model including sex, study, and history of diabetes produced a main effect for diabetes (with diabetes: mean=125.1 ± 108.4, median=94.0, IQR=82.0 minutes; without diabetes: mean=102.3 ± 85.0, median=78.0, IQR=60.0 minutes; p=0.005) and retained the sex by study interaction (p=0.02). Including both presentation delay and history of diabetes produced the best model AICC among those we examined, though only delay (p=0.02) and the sex by study interaction (p=0.03) remained significant (diabetes main effect p=0.11). Adding chest pain, the number of symptoms, or number of symptoms other than chest pain to this model did not yield significant effects or improve the model.
Further analysis of the number of symptom phenotypes in subgroups using door-to-balloon time as a dichotomous variable was unrevealing overall. No significant differences were found between study or sexes in the number of symptom phenotypes, the mean number of symptoms, or the main effects of the logistic regression model.
STEMI patients who received PCI were significantly less likely to have a presentation delay compared with STEMI patients who did not receive PCI (30.4% vs. 35.2%, p=0.04). Because presentation delay was associated with both whether patients received PCI and door-to-balloon times in the logistic regression model, we combined STEMI patients with no PCI with STEMI patients with door-to-balloon times ≥ 90 minutes. In this combined subgroup, women had significantly more symptom phenotypes than men (232 vs. 166, difference of 66 compared with expected difference of 40, p=0.01) and in VIRGO (198 vs. 109, difference of 89 compared with expected difference of 53, p<0.001), but not in SILVER-AMI (85 vs. 94, difference of −9 compared with expected difference of −6, p=0.68).
The frequencies of individual symptoms in patients in the D2B Sample from both studies are listed in Table 4. Chest pain was the dominant symptom in the D2B Sample of both studies for both women and men. In the D2B Sample, chest pain was more common in VIRGO women and men as compared with SILVER-AMI women and men and not significantly different between sexes within either study. Nausea/vomiting was more likely to occur in women as compared with men in VIRGO and in the VIRGO study patients as compared with the SILVER-AMI study patients. Radiating or other pain were more likely to occur in women as compared with men in both studies and in men in VIRGO as compared with men in SILVER-AMI. Confusion was more likely to occur in women in the VIRGO study than in the SILVER-AMI study, while anxiety/stress/agitation was more likely to occur in men in the SILVER-AMI study than in the VIRGO study. Chest pain, dyspnea, diaphoresis, and weakness/fatigue were more likely to occur in VIRGO study patients as compared with SILVER-AMI study patients but were not significantly different between sexes within each study. Other than chest pain, other presenting symptoms did not predict door-to-balloon time, whether analyzing using door-to-balloon time as a continuous variable, or as a dichotomous variable using the 90-minute cutoff.
Table 4.
Frequencies of Individual Symptoms in Patients from the D2B Samples of the VIRGO and SILVER-AMI Studies. Adjustment for multiple comparisons was made with the Hochberg procedure to preserve an overall two-sided type 1 error rate of .05.
| Symptom | VIRGO | SILVER-AMI | ||
|---|---|---|---|---|
| Women | Men | Women | Men | |
| Chest Pain | 88.3‡ | 92.4‡ | 79.4‡ | 82.6‡ |
| Dizziness/Lightheadedness | 31.7 | 28.9 | 22.4 | 22.3 |
| Indigestion/epigastric pain | 32.6 | 29.1 | 26.3 | 24.1 |
| Nausea/Vomiting | 57.5*‡ | 38.2*‡ | 36.8‡ | 25.2‡ |
| Radiating or other pain | 66.8* | 56.2*‡ | 59.6* | 44.0*‡ |
| Anxiety/agitation/palpitations | 16.5 | 10.9‡ | 19.7 | 19.1‡ |
| Dyspnea | 48.0‡ | 47.6‡ | 33.8‡ | 35.8‡ |
| Diaphoresis | 66.2‡ | 65.1‡ | 33.8‡ | 38.3‡ |
| Weakness/Fatigue | 47.4‡ | 40.7‡ | 29.8‡ | 24.8‡ |
| Confusion | 12.6‡ | 12.7 | 4.4‡ | 6.0 |
Significant (Hochberg-adjusted p<0.05) between sexes within study
Significant (Hochberg-adjusted p<0.05) between studies within sex
Discussion
Combining data from both the VIRGO and SILVER-AMI studies allowed this detailed evaluation of the relationship of symptoms and symptom complexity with door-to-balloon times in young and older patients with STEMI. Our analysis showed significantly more symptom phenotypes and more symptoms on average in the young women as compared with men in the VIRGO study. Young women in the VIRGO study had symptom combinations that were more broadly distributed over a larger number of symptom phenotype subgroups. Our analysis also showed a significant delay in the door-to-balloon times in the young women from the VIRGO study.
In contrast to the young VIRGO cohort, there was no significant difference between women and men in the older SILVER-AMI cohort in the number of symptom phenotypes, the distribution of symptom phenotypes, or average number of symptoms, and there was also no difference between women and men in door-to-balloon times in the older cohort. The findings in the D2B Sample of the SILVER-AMI cohort contrast with the prior study of the entire SILVER-AMI cohort, where there were more symptom phenotypes and more symptoms on average in women as compared with men.
The generalized linear model showed a significant interaction between sex and study as predictors of door-to-balloon times. Chest pain replaced sex as a significant predictor of door-to-balloon times and lack of chest pain correlated with longer door-to-balloon times in the VIRGO patients but not SILVER-AMI patients.
The relative lack of chest pain and the distracting effect of numerous other symptoms may have obscured the STEMI diagnosis in young women, leading to a delay in door-to-balloon time. It is important to note, however, that chest pain was a cardinal symptom in young women (occurring in 88%) and chest pain occurred more commonly in young women than in older women. It was likely the compounding effect of age and symptom recognition that caused the delay in door-to-balloon time in younger women. Multiple prior studies have shown prolonged door-to-balloon times in women,1–6 which may mostly affect young women where young age and relative lack of chest pain may work together to make the STEMI diagnosis seem less probable.
In addition to study and chest pain, a prolonged presentation time of >6 hours and a history of diabetes mellitus were also associated with prolonged door-to-balloon times in the best fitting logistic regression model. Presentation delay may have affected the door-to-balloon time, or alternatively, presentation delay and door-to-balloon time may have both been affected by another factor, such as initial recognition of STEMI. Diabetes may have affected the perception and description of symptoms or may have been a marker for peripheral vascular disease that may have delayed door-to-balloon times.
Young women had greater symptom complexity as shown by a greater number of symptom phenotypes, but the number of symptom phenotypes in subgroups could not be used in the predictive model of door-to-balloon time. To analyze the number of symptom phenotypes and door-to-balloon time, we compared the number of symptom phenotypes in subgroups divided by a 90-minute door-to-balloon cutoff. This analysis did not show a difference between door-to-balloon time subgroups in the number of symptom phenotypes. By combining the subgroup of patients with door-to-balloon times ≥ 90 minutes with STEMI patients with no PCI, however, we were able to show that women had significantly more symptom phenotypes than men overall and, in the VIRGO patients, but not in the SILVER-AMI patients, which was consistent with our overall comparison of symptom phenotypes in women and men. This finding suggests that symptom complexity could have either prolonged door-to-balloon time or reduced the chances of receiving PCI in young women with STEMI, possibly due to presentation delay.
Comparisons of the young VIRGO patients and the older SILVER-AMI patients also revealed interesting differences in the frequencies of several of the individual symptoms of AMI. Five out of 10 symptoms were more frequently reported in the young VIRGO patients, as compared with the older SILVER-AMI patients. Nausea/vomiting and diaphoresis were markedly more common in the young cohort as compared with the older cohort.
Our finding have implications for the rapid diagnosis of STEMI and efforts to improve door-to-balloon times, which may improve the outcomes of patients with STEMI.18–21 Studies have shown that expert clinicians use a diagnostic process that requires an initial step of recognizing diagnostic possibilities before proceeding to diagnostic confirmation through testing.13,22–25 For STEMI, rapid recognition leads to diagnostic confirmation by electrocardiogram and studies have shown that the time to obtaining a confirming electrocardiogram is a key determinant of door-to-balloon time.26–30 Prior studies of the VIRGO patients showed that absence of prehospital electrocardiograms and female sex were associated with prolonged door-to-balloon times, also suggesting that the lack of initial recognition of STEMI in young women contributes to prolonged door-to-balloon times.5,6
Our study has recognized limitations. The VIRGO study enrolled patients from August 2008 to January 2012 and the SILVER-AMI study enrolled patients from January 2013 to June 2018. The discordant timeframes could affect door-to-balloon times, however both studies occurred after a major nationwide initiative to address door-to-balloon times and nationally recorded door-to-balloon times were relatively stable during the two study timeframes.21,26,27 Furthermore, the study’s different timeframes would not affect inter-study comparisons between women and men. Also, the two studies used an age cutoff to define their study populations which limited the ability to use age as a continuous variable in the multivariable analysis, although the study was used as a dichotomous variable, which reflected age. Finally, our study design allowed analysis of symptoms and symptom combinations but lacked specific information about how patients would have ranked the relative severity or importance of symptoms. Despite these limitations, the VIRGO and SILVER-AMI studies provided a useful opportunity to evaluate symptom combinations in young and older STEMI patients and the relationship of symptom complexity to door-to-balloon times.
In summary, door-to-balloon times were longer in young women as compared with young men, but not in older women as compared with older men and young women had more symptom phenotypes and more symptoms on the average than men. Chest pain was a significant predictor of door-to-balloon times, and young women were significantly more likely to report symptoms other than chest pain. Clearly, symptom presentation compounded by young age affects door-to-balloon times in young women. These findings may have implications for recognizing STEMI in young women more quickly and reliably, which may improve the door-to-balloon times in women.
Funding:
The VIRGO study was supported by a National Heart, Lung, and Blood Institute grant #5RO1HL081153. IMJOVEN (the Spanish component of VIRGO was supported in Spain by a grant PI 081614 from the Fondo de Investigaciones Sanitarias del Instituto Carlos IIII, Ministry of Science and Technology, and the Centro Nacional de Investigaciones Cardiovasculares. The SILVER-AMI study was supported by a National Heart, Lung, and Blood Institute grant #RO1 HL115295 and was conducted at the Yale Claude D. Pepper Older Americans Independence Center (grant P30 AG021342).
Disclosures:
In the past three years, Harlan Krumholz received expenses and/or personal fees from UnitedHealth, Element Science, Aetna, Reality Labs, Tesseract/4Catalyst, F-Prime, the Siegfried and Jensen Law Firm, Arnold and Porter Law Firm, and Martin/Baughman Law Firm. He is a co-founder of Refactor Health and HugoHealth, and is associated with contracts, through Yale New Haven Hospital, from the Centers for Medicare & Medicaid Services and through Yale University from Johnson & Johnson. Dr. Brush receives royalties from Dementi Milestone Publishing for the book “The Science of the Art of Medicine: A Guide to Medical Reasoning.” The other authors report no disclosures.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Angeja BG, Gibson CM, Chin R, Frederick PD, Every NR, Ross AM, Stone GW, Barron HV and Participants in the National Registry of Myocardial I. Predictors of door-to-balloon delay in primary angioplasty. Am J Cardiol 2002;89:1156–61. [DOI] [PubMed] [Google Scholar]
- 2.Bloos SM, Kaur K, Lang K, Gavin N, Mills AM, Baugh CW, Patterson BW, Podolsky SR, Salazar G, Mumma BE, Tanski M, Hadley K, Roumie C, McNaughton CD and Yiadom M. Comparing the Timeliness of Treatment in Younger vs. Older Patients with ST-Segment Elevation Myocardial Infarction: A Multi-Center Cohort Study. J Emerg Med 2021;60:716–728. [DOI] [PubMed] [Google Scholar]
- 3.Choi K, Shofer FS and Mills AM. Sex differences in STEMI activation for patients presenting to the ED 1939. Am J Emerg Med 2016;34:1939–1943. [DOI] [PubMed] [Google Scholar]
- 4.Ladwig KH, Fang X, Wolf K, Hoschar S, Albarqouni L, Ronel J, Meinertz T, Spieler D, Laugwitz KL and Schunkert H. Comparison of Delay Times Between Symptom Onset of an Acute ST-elevation Myocardial Infarction and Hospital Arrival in Men and Women <65 Years Versus >/=65 Years of Age.: Findings From the Multicenter Munich Examination of Delay in Patients Experiencing Acute Myocardial Infarction (MEDEA) Study. Am J Cardiol 2017;120:2128–2134. [DOI] [PubMed] [Google Scholar]
- 5.D’Onofrio G, Safdar B, Lichtman JH, Strait KM, Dreyer RP, Geda M, Spertus JA and Krumholz HM. Sex differences in reperfusion in young patients with ST-segment-elevation myocardial infarction: results from the VIRGO study. Circulation 2015;131:1324–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gupta A, Barrabes JA, Strait K, Bueno H, Porta-Sanchez A, Acosta-Velez JG, Lidon RM, Spatz E, Geda M, Dreyer RP, Lorenze N, Lichtman J, D’Onofrio G and Krumholz HM. Sex Differences in Timeliness of Reperfusion in Young Patients With ST-Segment-Elevation Myocardial Infarction by Initial Electrocardiographic Characteristics. J Am Heart Assoc 2018;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Canto JG, Rogers WJ, Goldberg RJ, Peterson ED, Wenger NK, Vaccarino V, Kiefe CI, Frederick PD, Sopko G, Zheng ZJ and Investigators N. Association of age and sex with myocardial infarction symptom presentation and in-hospital mortality. JAMA 2012;307:813–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khan NA, Daskalopoulou SS, Karp I, Eisenberg MJ, Pelletier R, Tsadok MA, Dasgupta K, Norris CM, Pilote L and Team GP. Sex differences in acute coronary syndrome symptom presentation in young patients. JAMA Intern Med 2013;173:1863–71. [DOI] [PubMed] [Google Scholar]
- 9.Mehta LS, Beckie TM, DeVon HA, Grines CL, Krumholz HM, Johnson MN, Lindley KJ, Vaccarino V, Wang TY, Watson KE, Wenger NK, American Heart Association Cardiovascular Disease in W, Special Populations Committee of the Council on Clinical Cardiology CoE, Prevention CoC, Stroke N, Council on Quality of C and Outcomes R. Acute Myocardial Infarction in Women: A Scientific Statement From the American Heart Association. Circulation 2016;133:916–47. [DOI] [PubMed] [Google Scholar]
- 10.Lichtman JH, Leifheit EC, Safdar B, Bao H, Krumholz HM, Lorenze NP, Daneshvar M, Spertus JA and D’Onofrio G. Sex Differences in the Presentation and Perception of Symptoms Among Young Patients With Myocardial Infarction: Evidence from the VIRGO Study (Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients). Circulation 2018;137:781–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brush JE Jr., Krumholz HM, Greene EJ and Dreyer RP. Sex Differences in Symptom Phenotypes Among Patients With Acute Myocardial Infarction. Circ Cardiovasc Qual Outcomes 2020;13:e005948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brush JE Jr.. Hajduk AM, Greene EJ, Dreyer RP, Krumholz HM and Chaudhry SI. Sex Differences in Symptom Phenotypes Among Older Patients with Acute Myocardial Infarction. Am J Med 2022;135:342–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brush JE Jr.. Sherbino J and Norman GR. Diagnostic reasoning in cardiovascular medicine. BMJ 2022;376:e064389. [DOI] [PubMed] [Google Scholar]
- 14.Lichtman JH, Lorenze NP, D’Onofrio G, Spertus JA, Lindau ST, Morgan TM, Herrin J, Bueno H, Mattera JA, Ridker PM and Krumholz HM. Variation in recovery: Role of gender on outcomes of young AMI patients (VIRGO) study design. Circ Cardiovasc Qual Outcomes 2010;3:684–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dodson JA, Geda M, Krumholz HM, Lorenze N, Murphy TE, Allore HG, Charpentier P, Tsang SW, Acampora D, Tinetti ME, Gill TM and Chaudhry SI. Design and rationale of the comprehensive evaluation of risk factors in older patients with AMI (SILVER-AMI) study. BMC Health Serv Res 2014;14:506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Joint ESCAAHAWHFTFfUDoMI, Authors/Task Force Members C, Thygesen K, Alpert JS, White HD, Biomarker S, Jaffe AS, Katus HA, Apple FS, Lindahl B, Morrow DA, Subcommittee ECG, Chaitman BR, Clemmensen PM, Johanson P, Hod H, Imaging S, Underwood R, Bax JJ, Bonow JJ, Pinto F, Gibbons RJ, Classification S, Fox KA, Atar D, Newby LK, Galvani M, Hamm CW, Intervention S, Uretsky BF, Steg PG, Wijns W, Bassand JP, Menasche P, Ravkilde J, Trials, Registries S, Ohman EM, Antman EM, Wallentin LC, Armstrong PW, Simoons ML, Trials, Registries S, Januzzi JL, Nieminen MS, Gheorghiade M, Filippatos G, Trials, Registries S, Luepker RV, Fortmann SP, Rosamond WD, Levy D, Wood D, Trials, Registries S, Smith SC, Hu D, Lopez-Sendon JL, Robertson RM, Weaver D, Tendera M, Bove AA, Parkhomenko AN, Vasilieva EJ, Mendis S, Guidelines ESCCfP, Bax JJ, Baumgartner H, Ceconi C, Dean V, Deaton C, Fagard R, Funck-Brentano C, Hasdai D, Hoes A, Kirchhof P, Knuuti J, Kolh P, McDonagh T, Moulin C, Popescu BA, Reiner Z, Sechtem U, Sirnes PA, Tendera M, Torbicki A, Vahanian A, Windecker S, Document R, Morais J, Aguiar C, Almahmeed W, Arnar DO, Barili F, Bloch KD, Bolger AF, Botker HE, Bozkurt B, Bugiardini R, Cannon C, de Lemos J, Eberli FR, Escobar E, Hlatky M, James S, Kern KB, Moliterno DJ, Mueller C, Neskovic AN, Pieske BM, Schulman SP, Storey RF, Taubert KA, Vranckx P and Wagner DR Third universal definition of myocardial infarction. J Am Coll Cardiol 2012;60:1581–98.22958960 [Google Scholar]
- 17.Hurvich CM; Tsai C-L (1989), “Regression and time series model selection in small samples”, Biometrika 76 (2): 297–307, doi: 10.1093/biomet/76.2.297 [DOI] [Google Scholar]
- 18.Berger PB, Ellis SG, Holmes DR Jr.,Granger CB, Criger DA, Betriu A, Topol EJ and Califf RM. Relationship between delay in performing direct coronary angioplasty and early clinical outcome in patients with acute myocardial infarction: results from the global use of strategies to open occluded arteries in Acute Coronary Syndromes (GUSTO-IIb) trial. Circulation 1999;100:14–20. [DOI] [PubMed] [Google Scholar]
- 19.McNamara RL, Wang Y, Herrin J, Curtis JP, Bradley EH, Magid DJ, Peterson ED, Blaney M, Frederick PD, Krumholz HM and Investigators N. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol 2006;47:2180–6. [DOI] [PubMed] [Google Scholar]
- 20.Rathore SS, Curtis JP, Nallamothu BK, Wang Y, Foody JM, Kosiborod M, Masoudi FA, Havranek EP and Krumholz HM. Association of door-to-balloon time and mortality in patients > or =65 years with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Am J Cardiol 2009;104:1198–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nallamothu BK, Normand SL, Wang Y, Hofer TP, Brush JE Jr., Messenger JC, Bradley EH, Rumsfeld JS and Krumholz HM. Relation between door-to-balloon times and mortality after primary percutaneous coronary intervention over time: a retrospective study. Lancet 2015;385:1114–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Elstein AS, Shulman LS, Sprafka SA: Medical Problem Solving: An Analysis of Clinical Reasoning. Cambridge, MA: Harvard University Press; 1978. [Google Scholar]
- 23.Barrows HS, Norman GR, Neufeld VR and Feightner JW. The clinical reasoning of randomly selected physicians in general medical practice. Clin Invest Med. 1982;5:49–55. [PubMed] [Google Scholar]
- 24.Kassirer JP and Gorry GA. Clinical problem solving: a behavioral analysis. Ann Intern Med 1978;89:245–55. [DOI] [PubMed] [Google Scholar]
- 25.Pelaccia T, Tardif J, Triby E, Ammirati C, Bertrand C, Dory V and Charlin B. How and when do expert emergency physicians generate and evaluate diagnostic hypotheses? A qualitative study using head-mounted video cued-recall interviews. Ann Emerg Med 2014;64:575–85. [DOI] [PubMed] [Google Scholar]
- 26.Krumholz HM, Bradley EH, Nallamothu BK, Ting HH, Batchelor WB, Kline-Rogers E, Stern AF, Byrd JR and Brush JE Jr. A campaign to improve the timeliness of primary percutaneous coronary intervention: Door-to-Balloon: An Alliance for Quality. JACC Cardiovasc Interv 2008;1:97–104. [DOI] [PubMed] [Google Scholar]
- 27.Bradley EH, Herrin J, Wang Y, Barton BA, Webster TR, Mattera JA, Roumanis SA, Curtis JP, Nallamothu BK, Magid DJ, McNamara RL, Parkosewich J, Loeb JM and Krumholz HM. Strategies for reducing the door-to-balloon time in acute myocardial infarction. N Engl J Med 2006;355:2308–20. [DOI] [PubMed] [Google Scholar]
- 28.Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, Khot UN, Lange RA, Mauri L, Mehran R, Moussa ID, Mukherjee D, Nallamothu BK, Ting HH, American College of Cardiology F, American Heart Association Task Force on Practice G, Society for Cardiovascular A and Interventions. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol 2011;58:e44–122. [DOI] [PubMed] [Google Scholar]
- 29.Krumholz HM, Herrin J, Miller LE, Drye EE, Ling SM, Han LF, Rapp MT, Bradley EH, Nallamothu BK, Nsa W, Bratzler DW and Curtis JP. Improvements in door-to-balloon time in the United States, 2005 to 2010. Circulation 2011;124:1038–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Borden WB, Fennessy MM, O’Connor AM, Mulliken RA, Lee L, Nathan S, Nichols J and Lopez JJ. Quality improvement in the door-to-balloon times for ST-elevation myocardial infarction patients presenting without chest pain. Catheter Cardiovasc Interv 2012;79:851–8. [DOI] [PubMed] [Google Scholar]


