Abstract
Background:
Indicated surgical management of metacarpal neck fractures varies with techniques including Kirschner wires, plate fixation, intramedullary fixation, and headless compression screws without a demonstrated superiority. This study compares intramedullary threaded nail fixation (ITN) to a locking plate construct.
Methods:
Index through small finger metacarpals were harvested from ten embalmed cadavers. After appropriate exclusion criteria, remaining metacarpals underwent neck fracture creation via three-point load to failure. Eight samples were randomly allocated to fixation with ITN fixation and six were stabilized with a 2.3mm seven-hole locking plate. Samples were then subjected to a second round of biomechanical testing using the same apparatus. Ultimate load between intact tissue and subsequently stabilized fracture was analyzed with a paired t-test. Percent change in ultimate load in intact tissue and stabilized tissue was calculated and magnitude of relative difference between the two groups was analyzed via unpaired t-tests. Statistical difference was defined by a p-value of p<0.05.
Results:
Both groups demonstrated ability to handle a biomechanical load however both were significantly weaker than intact tissue (paired t-test p ITN-fixed vs. p ITN-intact = 0.006; p plate-fixed vs. p plate-intact = 0.002). ITN samples demonstrated a higher load to failure (unpaired t-test p ITN-fixed vs. p plate-fixed = 0.039) (Figure 6).
Summary:
ITN provides a biomechanically stronger fixation constructed for vertically oriented metacarpal neck fractures compared to locking plate fixation. Both ITN and locking plate constructs provide stabilization capable of tolerating a biomechanical load; however, both fixation modalities are weaker than native tissue.
Introduction
Metacarpal fractures account for 10–40% of all hand fractures1,2 Metacarpal neck fractures represent a specific subset of metacarpal fractures with a reported incidence of 130.3 per 100,000.3 Their treatment lacks a consensus for management.3,4 Treatment algorithms vary widely; angulation alone as a guide has a wide range of reported tolerances. Classically, angular tolerance varies by involved metacarpal with up to 15 degree accepted for index and long fingers, 40 degree for ring fingers and 60 degrees for small fingers.5 Regarding the fifth metacarpal specifically, Hunter et al. reported their series of fifth metacarpal neck fractures in 1970 accepting up to 70 degree of angulation in the metacarpal neck save for any rotational mal-alignment.6 Furthermore, functional management was found to be an amenable treatment with possible benefits in return of grip strength and return to work.7
As a result of the typical load applied, the volar surface of the metacarpal sustains comminution and the fracture angulates in an apex dorsal direction.5 Generally accepted indications for operative treatment include rotational malalignment, open fractures, angulation greater than accepted norms for the individual metacarpal and concomitant or multiple neck fractures. Operative intervention hopes to preclude a prominent dorsal deformity, prominence of the metacarpal head in the volar palm, decreased grip strength and pseudoclawing.8,9
Numerous fixation techniques are reported in the literature, including Kirschner wire fixation, plate fixation, intramedullary nails and headless compression screws, yet complication rates can be as high as 36% after surgical management.10–12 In response to high rates of complication, alternative surgical techniques and implants have been sought, including the recently designed intramedullary threaded nail (ITN). Indications for ITN follow the previously described indications for operative intervention.13 Recently, Patel et al compared ITN to percutaneously placed Kirschner wire fixation and demonstrated biomechanical superiority of the ITN construct.14 Historically, biomechanical studies showed added strength with locking plate fixation, when compared to Kirschner-wire fixation or headless compression screws.15 This study aimed to determine the biomechanical stability of the newly designed ITN in the fixation of metacarpal neck fractures and to compare them to the stability of a locking plate and screw construct. Our hypothesis was that the locking plates would be biomechanically superior to ITN.
Materials and Methods
Tissue collection.
Index through small finger metacarpals were isolated from ten embalmed human cadavers. Of the eighty metacarpals available, seventy-three were successfully collected and seven were discarded due to evidence of prior fracture, callus formation, or creation of a fracture during the dissection and collection process. Forty-eight of the seventy-three harvested metacarpals were subsequently discarded due to failing to pass our exclusion criteria, which included evidence of prior osseous defects or poor cortical bone quality indicative of osteoporosis. Cortical bone quality was subjectively classified based off the translucency of the metacarpals. Some metacarpals, particularly small finger and ring metacarpals were smaller than 4.0 millimeters in diameter in the diaphysis. These could not be included in the study as this would not allow for appropriate passage of the intramedullary nail.
Metacarpal neck fracture creation.
After these exclusions, twenty-five metacarpals remained and underwent fracture creation via three-point load to failure from a previously accepted fracture model.16 Fractures were created at the metacarpal necks using a custom apparatus and a mechanical testing system (Tinius Olsen H5KS, 5000 N load cell and Horizon software) at a loading rate of 10 mm/min until overt failure (Figure 1 and Supplemental Image 1). Creation of these fracture patterns using the mechanical testing system occurred without difficulty. The ultimate load, defined as the maximum load in Newtons sustained by the tissue prior to fracture, was recorded during testing. Samples were examined after fracture to evaluate the quality of the fracture created; eleven of the twenty-five fractured metacarpals were discarded at this stage due to the presence of improper fracture morphology (e.g., comminuted or oblique rather than transverse fractures, or fractures extending beyond the metacarpal neck). This left 14 metacarpals with uniform neck fractures to be allocated to the nail or the plate fixation arm of the study.
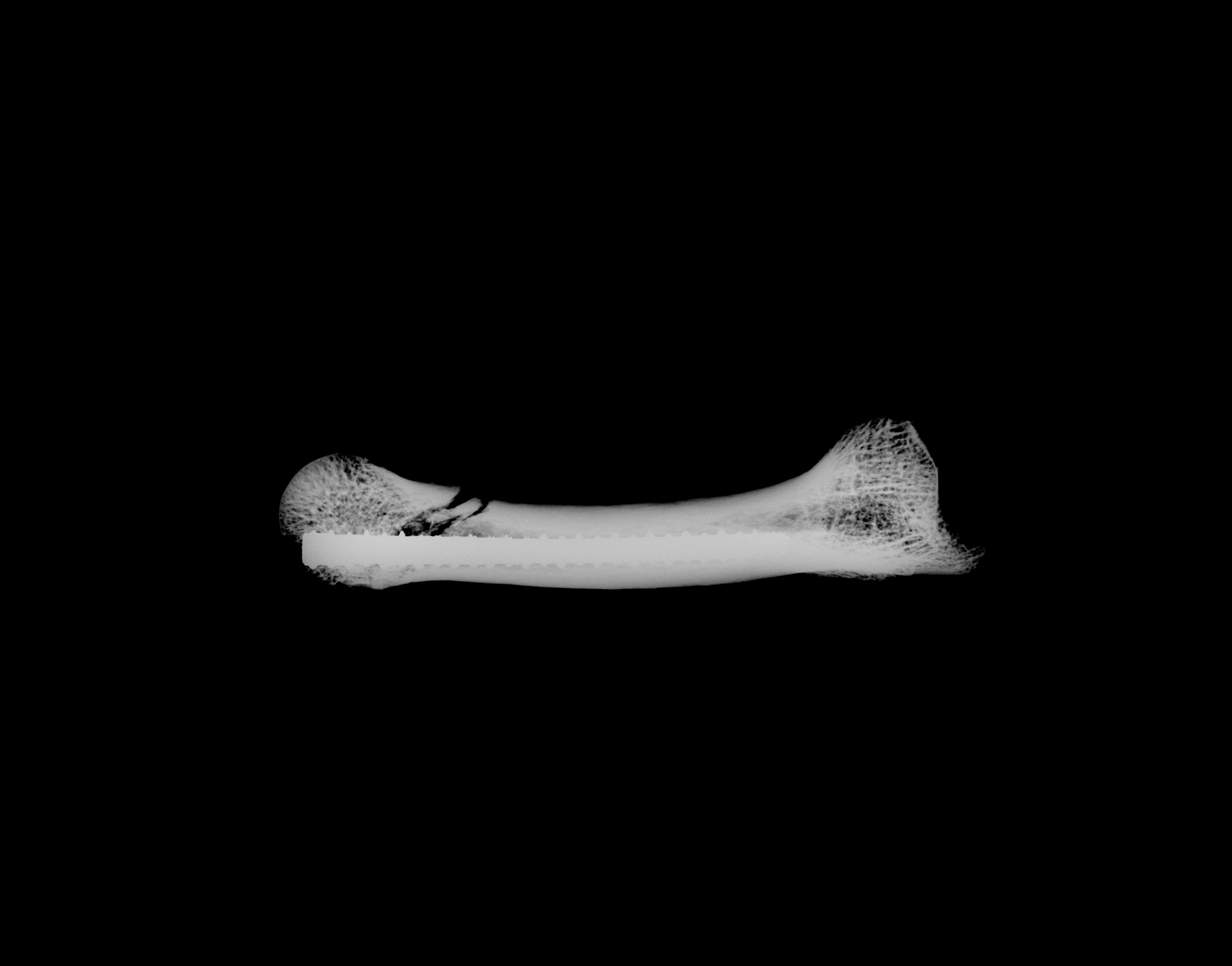
Figure 1:

Radiographic depiction of induced metacarpal neck fracture (Kubtec Parameter)
Fracture fixation and biomechanical testing.
Fracture fixation was performed by surgeons with prior surgical experience of using both the intramedullary nail as well as the locking plate and screw construct. Eight metacarpals were randomly allocated to undergo fracture fixation with ITN. Metacarpals were reduced and stabilized with an ExsoMed INnate intramedullary nail. Technique began with anatomic reduction of the fractures, after which a guidewire was inserted in a retrograde manner from the metacarpal head to the proximal portion. A drill was then reamed over the wire to allow passage of the nail and nail length was then determined using a radiographic guide. Based on the guide measurements, nails were selected from a range of lengths in 5mm increments (25mm-75mm) to ensure intramedullary placement of the implant head. Upon appropriate length selection, nails were subsequently inserted to adequate depth in standard fashion17 (Figure 2, Figure 3, and Supplemental Image 2).
Figure 2:

Posterior-anterior view of ITN construct (Kubtec Parameter)
Figure 3:
Lateral view of ITN construct (Kubtec Parameter)
The remaining six metacarpals underwent plate and screw fixation with a 2.3mm 7-hole locking plate. Fractures were first reduced with pointed reduction clamps and then plates were placed dorsally and secured with five locking screws. While metacarpal allocation between the study groups was random, the number of available devices in the locking plate group was limited to six constructs, thus only six metacarpals were able to be placed in this study arm compared to the eight in the ITN group (Figures 4 and 5).
Figure 4:

Dorsal view of plate fixation
Figure 5:

Lateral view of plate fixation
Surgical fixation in both groups were performed without any significant difficulty. Metacarpals stabilized with either nail or plate were then subjected to a second round of biomechanical testing using the same system, apparatus, and settings as initially performed on the intact tissue. The ultimate load for each fracture-stabilized metacarpal, defined as re-creation of the fracture, was recorded during testing.
Statistical analysis:
The ultimate load between the intact tissue and the subsequently stabilized fracture for each metacarpal sample was compared with a paired t-test, evaluating the strength of the repaired fractures as compared to the native (intact) tissue for both the ITN and plate-stabilized groups. In addition, the percent change in ultimate load between the fixed fractures as compared to the initially intact tissue was calculated for each sample, and the magnitude of this relative difference was compared between the ITN and plate stabilized groups via unpaired t-tests. A p-value of p<0.05 was considered to be statistically significant. Available sample sizes were underpowered to adequately assess the impact of “digit” (e.g., index finger, ring finger) on experimental outcomes.
Results
Both the ITN-fixed and plate-fixed constructs, while capable of supporting a biomechanical load, were significantly weaker than intact tissue as revealed by paired t-tests (paired t-test p ITN-fixed vs. p ITN-intact = 0.006; p plate-fixed vs. p plate-intact = 0.002). Comparison of the load to failure between the ITN and plate-fixed groups revealed that the ITN-fixed samples demonstrated higher load to failure (unpaired t-test p ITN-fixed vs. p plate-fixed = 0.039) (Figure 6). This suggests that the ITN fixation created a repaired bone construct that was closer in its mechanical strength to the native, intact tissue than those that had been fixed with a plate.
Figure 6:
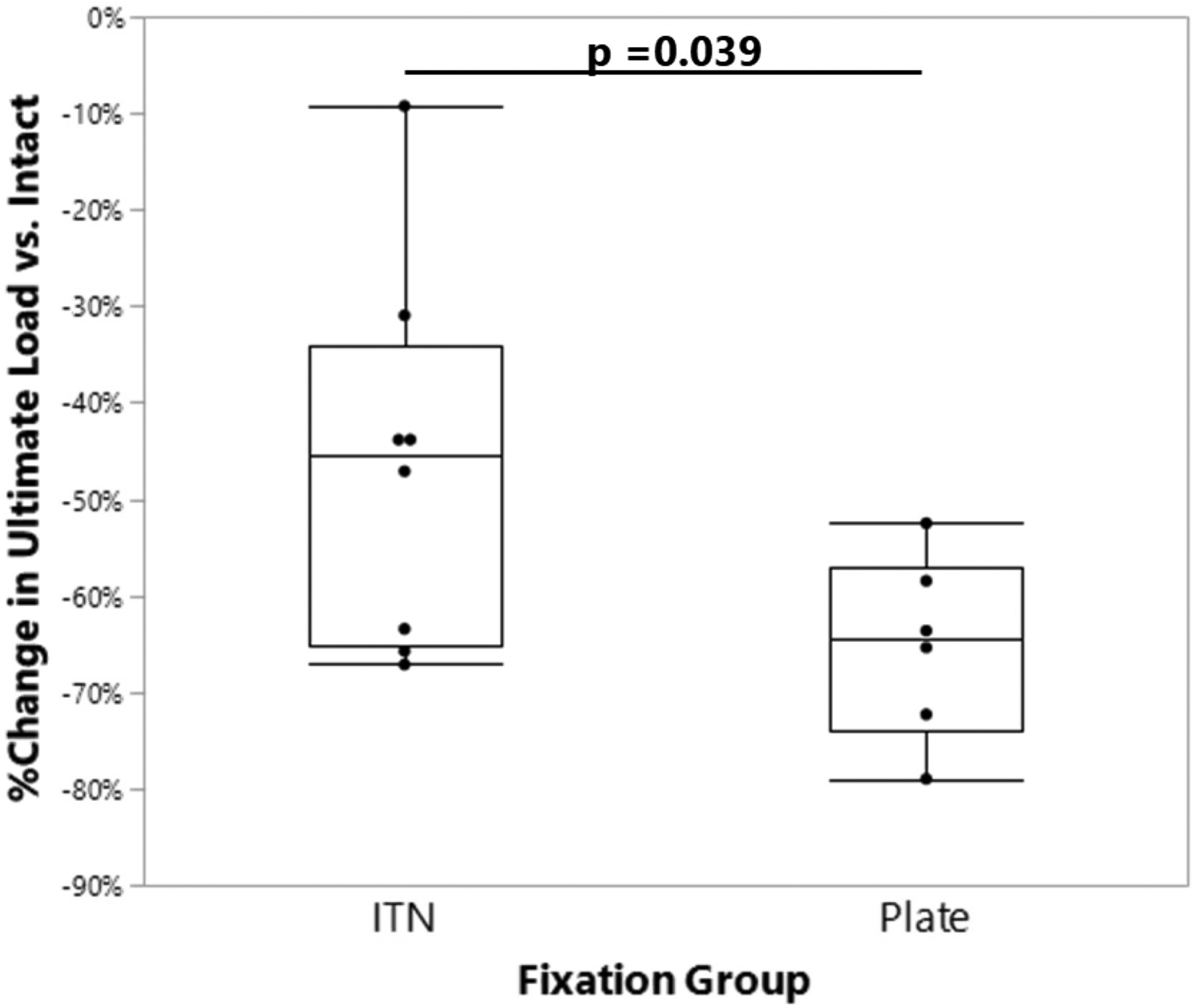
Comparison of change in ultimate load (vs. intact tissue) for each mode of fracture fixation. ITN: Intramedullary threaded nail.
Discussion
The current study evaluated the biomechanical performance of ITN compared to a dorsal plate fixation construct in a cadaveric metacarpal neck fracture model. Our hypothesis that locking plates would be biomechanically stronger and provide superior fixation stability was not supported by our results. While both the ITN-stabilized and plate-stabilized constructs were mechanically inferior when compared to intact tissue, the ITN construct was found to be stronger and more closely mimic the strength of intact tissue as compared to the locking plate model. The average load to failure of the locking plate group was 140.2N, whereas the ITN construct averaged 335.9N at load failure.
ITN fixation offers a less invasive option compared to plate fixation techniques. Previous studies have highlighted complications in patients undergoing plate fixation for metacarpal fractures, including decreased range of motion, site infection, device failure, stiffness, nonunion, delayed wound healing, and additional surgery for device removal.10–12 The clinical relevance of less invasive procedures for metacarpal neck fractures has been previously addressed by Ruchelsman et al, showing increased range of motion, improved grip strength, and decreased need for secondary surgeries with headless compression screw fixation.18 Our goal in performing this study was to determine the strength of ITN fixation while also investigating the potential advantages of this less invasive procedure and the need for further studies into such fixations.
Many factors are involved in determining the ideal fixation method of metacarpal fractures including the fracture location, relative degree of stability and/or comminution, and the amount of soft tissue involvement impacting adequate fracture coverage. In our study, the transverse neck fracture model simulated simple metacarpal neck fractures without comminution. Although our findings indicate that ITN fixation is biomechanically superior to dorsal plating of transverse metacarpal neck fractures, it is unclear how an ITN construct would perform biomechanically in the fixation of metacarpal shaft fractures or in the setting of different metacarpal neck fracture patterns including those that are oblique, spiral, or comminuted. An assessment of the biomechanical performance of ITN for the fixation of these fracture patterns was beyond the scope of our study.
Despite the results of this study, the locking plate remains a viable construct for metacarpal fractures.19 Familiarity and comfort with plate and screw procedures is a benefit for many surgeons. In addition, the dissection involved in plate and screw constructs allows for direct fracture visualization and reduction which has been shown to lead to a decreased risk of limb shortening and rotational deformity compared to other fixation methods.19 Another main benefit of plates and screws is the early mobilization and return to function allowed which has been correlated with greater patient satisfaction after surgery.20–22 This early return to activities is further supported by literature in athletes, as Etier et al cites a return to football at an average of 6.3 days following plate and screw fixation.23
There were several limitations to this study. Data relating to the age and prior bone health of cadaveric donors were not available for this study, leading to possible variance in bone density and tensile strength among specimens. However, this limitation was addressed through our experimental design, with randomized group assignments and biomechanical strength assessment longitudinally within each sample using paired t-testing. Due to the cadaveric nature of the study, the contributions of local soft tissue stability were negated, as bone samples were cleaned of soft tissues prior to fracture creation and instrumentation. To best compare the efficacy of the two fracture fixation methods, we chose to utilize monotonic testing, where the ultimate load of the intact tissue (assessed by a single load-to-failure test) could be directly compared to the ultimate load of the repaired constructs. While beyond the scope of the current study, in future work, it would be interesting to assess whether the fatigue performance of the metacarpals, both before and after creation of a fracture, would be similarly affected. Similarly, while we were unable to assess the impact of clinically relevant torsional loading, this may also be assessed in future studies. Furthermore, low numbers of testable specimens, which impacted statistical power, also remains a limitation to this study. However, despite the lower numbers of subjects, our results show statistical significance in strength with fracture fixation of the ITN as compared to plate fixation approaches.
Based on our results, we conclude that ITN fixation of metacarpal neck fractures may offer a more stable and biomechanically superior fixation than dorsal plating. However, the biomechanical stability of ITN fixation for metacarpal shaft fractures and comminuted or oblique fracture patterns is still unknown. Future studies, focusing on both biomechanical aspects and long-term clinical outcomes, are needed to assess ITN fixation for metacarpal shaft fractures as well as metacarpal neck fractures with oblique and comminuted patterns.
Supplementary Material
Funding:
Biomechanical testing of specimens was supported by NIH P01-AG036675.
Footnotes
Conflicts of Interest:
The authors have no conflicts of interest to declare. All co-authors have seen and agree with the contents of the manuscript and there is no financial interest to report. We certify that the submission is original work and is not under review at any other publication.
Contributor Information
Doyle R Wallace, Medical College of Georgia at Augusta University1.
A Luke Shiver, Medical College of Georgia at Augusta University.
Steven K Pulliam, Medical College of Georgia at Augusta University.
Bruce M Byrd, Medical College of Georgia at Augusta University.
Meghan E McGee-Lawrence, Department of Cellular Biology and Anatomy at the Medical College of Georgia.
Mark C Snoddy, Medical College of Georgia at Augusta University.
References:
- 1.Anakwe RE, Aitken SA, Cowie JG, Middleton SD, Court-Brown CM. The epidemiology of fractures of the hand and the influence of social deprivation. J Hand Surg Eur Vol. Jan 2011;36(1):62–5. doi: 10.1177/1753193410381823 [DOI] [PubMed] [Google Scholar]
- 2.Padegimas EM, Warrender WJ, Jones CM, Ilyas AM. Metacarpal Neck Fractures: A Review of Surgical Indications and Techniques. Arch Trauma Res. Sep 2016;5(3):e32933. doi: 10.5812/atr.32933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury. Aug 2006;37(8):691–7. doi: 10.1016/j.injury.2006.04.130 [DOI] [PubMed] [Google Scholar]
- 4.Tosti R, Ilyas AM, Mellema JJ, Guitton TG, Ring D. Interobserver variability in the treatment of little finger metacarpal neck fractures. J Hand Surg Am. Sep 2014;39(9):1722–7. doi: 10.1016/j.jhsa.2014.05.023 [DOI] [PubMed] [Google Scholar]
- 5.Wolfe SW. Green’s Operative Hand Surgery vol 1. Elsevier; 2017. [Google Scholar]
- 6.Hunter JM, Cowen NJ. Fifth metacarpal fractures in a compensation clinic population. A report on one hundred and thirty-three cases. J Bone Joint Surg Am. Sep 1970;52(6):1159–65. [PubMed] [Google Scholar]
- 7.Kuokkanen HO, Mulari-Keränen SK, Niskanen RO, Haapala JK, Korkala OL. Treatment of subcapital fractures of the fifth metacarpal bone: a prospective randomised comparison between functional treatment and reposition and splinting. Scand J Plast Reconstr Surg Hand Surg. Sep 1999;33(3):315–7. doi: 10.1080/02844319950159299 [DOI] [PubMed] [Google Scholar]
- 8.Kamath JB, Harshvardhan, Naik DM, Bansal A. Current concepts in managing fractures of metacarpal and phalangess. Indian J Plast Surg. May 2011;44(2):203–11. doi: 10.4103/0970-0358.85341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thurston AJ. Pivot osteotomy for the correction of malunion of metacarpal neck fractures. J Hand Surg Br. Oct 1992;17(5):580–2. doi: 10.1016/s0266-7681(05)80247-5 [DOI] [PubMed] [Google Scholar]
- 10.Creighton JJ Jr., Steichen JB. Complications in phalangeal and metacarpal fracture management. Results of extensor tenolysis. Hand Clin. Feb 1994;10(1):111–6. [PubMed] [Google Scholar]
- 11.Kollitz KM, Hammert WC, Vedder NB, Huang JI. Metacarpal fractures: treatment and complications. Hand (N Y). Mar 2014;9(1):16–23. doi: 10.1007/s11552-013-9562-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Page SM, Stern PJ. Complications and range of motion following plate fixation of metacarpal and phalangeal fractures. J Hand Surg Am. Sep 1998;23(5):827–32. doi: 10.1016/s0363-5023(98)80157-3 [DOI] [PubMed] [Google Scholar]
- 13.Tobert DG, Klausmeyer M, Mudgal CS. Intramedullary Fixation of Metacarpal Fractures Using Headless Compression Screws. J Hand Microsurg. Dec 2016;8(3):134–139. doi: 10.1055/s-0036-1593390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patel M, Castañeda P, Campbell DH, Putnam JG, McKee MD. Threaded Intramedullary Nails Are Biomechanically Superior to Crossed K-wires for Metacarpal Neck Fractures. Hand (N Y). Apr 9 2021:15589447211003182. doi: 10.1177/15589447211003182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jones CM, Padegimas EM, Weikert N, Greulich S, Ilyas AM, Siegler S. Headless Screw Fixation of Metacarpal Neck Fractures: A Mechanical Comparative Analysis. Hand (N Y). Mar 2019;14(2):187–192. doi: 10.1177/1558944717731859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Avery DM, Klinge S, Dyrna F, Pauzenberger L, Lam D, Cote M, DiVenere J, Obopilwe E, Mazzocca A, Rodner C. Headless Compression Screw Versus Kirschner Wire Fixation for Metacarpal Neck Fractures: A Biomechanical Study. The Journal of Hand Surgery Am. Mar 2017;42(5):392e1–e6. doi: 10.1016/j.jhsa.2017.02.013 [DOI] [PubMed] [Google Scholar]
- 17.Boulton CL, Salzler M, Mudgal CS. Intramedullary cannulated headless screw fixation of a comminuted subcapital metacarpal fracture: case report. J Hand Surg Am. Aug 2010;35(8):1260–3. doi: 10.1016/j.jhsa.2010.04.032 [DOI] [PubMed] [Google Scholar]
- 18.Ruchelsman D, Tejwani N, Kwon Y, Egol K. Open reduction and internal fixation of capitellar fractures with headless screws. J Bone Joint Surg Am. Jun 2008;90(6):1321–9. [DOI] [PubMed] [Google Scholar]
- 19.Wong KP, Hay RA, Tay SC. Surgical outcomes of fifth metacarpal neck fractures--a comparative analysis of dorsal plating versus tension band wiring. Hand Surg. 2015;20(1):99–105. doi: 10.1142/s0218810415500148 [DOI] [PubMed] [Google Scholar]
- 20.Zhu X, Zhang H, Wu J, Wang S, Miao L. Pin vs plate fixation for metacarpal fractures: a meta-analysis. J Orthop Surg Res. Nov 19 2020;15(1):542. doi: 10.1186/s13018-020-02057-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Souer JS, Mudgal CS. Plate fixation in closed ipsilateral multiple metacarpal fractures. J Hand Surg Eur Vol. Dec 2008;33(6):740–4. doi: 10.1177/1753193408090101 [DOI] [PubMed] [Google Scholar]
- 22.Greeven AP, Bezstarosti S, Krijnen P, Schipper IB. Open reduction and internal fixation versus percutaneous transverse Kirschner wire fixation for single, closed second to fifth metacarpal shaft fractures: a systematic review. Eur J Trauma Emerg Surg. Apr 2016;42(2):169–75. doi: 10.1007/s00068-015-0507-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Etier BE, Scillia AJ, Tessier DD, et al. Return to play following metacarpal fractures in football players. Hand (N Y). Dec 2015;10(4):762–6. doi: 10.1007/s11552-015-9769-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


