Highlights
-
•
Educational initiatives should contextualize concussion disclosure to promote success.
-
•
Interventions should promote stakeholder and team-based support networks.
-
•
Several key contextual factors, in addition to knowledge and attitudes, should be considered to improve concussion disclosure.
-
•
Supportive sport culture and the presence of medical professionals aid in disclosure.
-
•
Stigma, interpersonal pressure, and a lack of support may prevent successful disclosure.
Keywords: Education, Medical professional presence, Mixed methodological research, Reporting, Sport culture
Abstract
Background
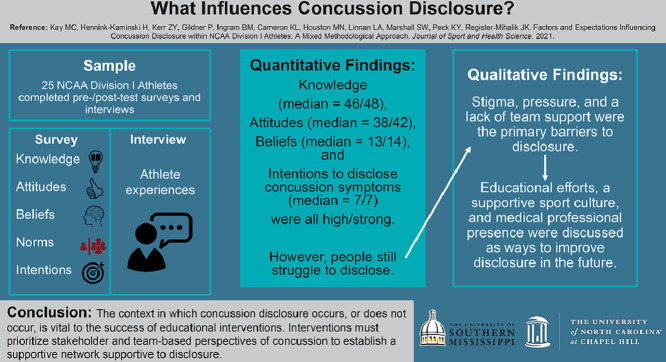
Participation in sports is associated with many benefits to all aspects of health; however, it also comes with the risk of injury, particularly concussions. Self-disclosure and care seeking following a concussion are especially important because of the lack of outwardly visible signs and/or symptoms. Although recent research has explored factors affecting concussion disclosure, use of isolated methodologies limits the ability to contextualize how disclosure or nondisclosure occurs. Therefore, the purpose of this study was to describe the factors and expectations of National Collegiate Athletic Association (NCAA) athletes that may influence concussion disclosure.
Methods
This mixed-methods convergent parallel research study included 25 NCAA Division I athletes representing 13 sports, all of whom completed a concussion-education session with pre-/post-test surveys and a semistructured interview. Eligible athletes were at least 18 years old and on an NCAA roster. The surveys focused on previous concussion-related disclosure behaviors, knowledge, attitudes, beliefs, norms, and intentions about disclosing concussion. Interviews focused on the athletes’ experiences related to concussion disclosure. Survey data were analyzed using descriptive statistics and Mann-Whitney U tests. Interviews were analyzed using a Consensual Qualitative Research tradition.
Results
Participants had good concussion knowledge (median = 46.0), positive attitudes (median = 38.0), strong beliefs (median = 13.0), and strong intentions to disclose concussion symptoms (median = 7.0). None of the constructs differed by participants’ gender. Although quantitative findings were mostly positive, interview data highlighted factors that may explain why some participants are successful in disclosing concussions and why others may find disclosure difficult. Educational efforts, sport culture, and medical professional presence were the primary facilitators discussed by participants. Stigma, pressure, and a lack of team support were perceived as disclosure barriers.
Conclusion
The context in which concussion disclosure occurs or does not occur is vital to the success of educational interventions. Interventions must prioritize stakeholder- and team-based perspectives on concussion to establish a network supportive to disclosure.
Graphical Abstract
1. Introduction
Participation in sports is associated with many physical, mental, and social health benefits for children and adults. Despite its benefits, risks exist, primarily in the form of injury. Concussions are one of the many injuries that can occur during sport participation.1, 2, 3 Within collegiate sports, concussions make up approximately 8% of all sport-related injuries.4 However, reports indicate that up to 50% of all concussions are never disclosed.5, 6, 7, 8, 9
Injury disclosure is especially important for concussions because they show few outwardly visible signs, making it difficult for others to recognize.10 Health care providers are trained to identify potential concussions, but they are not always present when concussions occur. Additionally, without outwardly visible signs and/or symptoms, it is important for athletes and teammates to be well-informed and honest about what they are experiencing in order to receive timely and proper care.11 Role expectations regarding concussion disclosure and care, as well as which responsibilities lie with which individuals in the athletic environment, have not been heavily explored in current literature; however, these factors may help optimize concussion-disclosure interventions.
Recent research highlights various factors associated with individuals’ willingness to disclose concussions. Factors including gender,12 concussion history,13 knowledge,9 attitudes,14,15 and perceived norms15 can influence concussion disclosure both positively and negatively. These factors fit within the Socio-Ecological Model, which provides a framework that highlights the interactive relationships among intrapersonal, interpersonal, community, and policy-level factors.16 However, much of this research relied on the use of exclusively qualitative or quantitative data, making it difficult to discern the relationship of factors between independent studies using differing sampling and analytical techniques. A mixed methodological approach allows for greater understanding of the issue at hand by presenting quantitative data with respect to the problem and qualitative data with respect to why the problem may or may not exist. Therefore, the purpose of this study was to use a mixed methodological approach to describe the factors and expectations of National Collegiate Athletic Association (NCAA) athletes that may influence concussion disclosure.
2. Methods
To assess the context in which NCAA athletes were more or less likely to disclose concussions, this study employed a single-cohort mixed methodological convergent parallel design, which used surveys in combination with a semistructured interview protocol. This particular study was part of a larger investigation into the design and efficacy of an innovative concussion-education platform meant to improve knowledge, attitudes, beliefs, norms, and intentions in both military cadets and athletes. The Institutional Review Board of the University of North Carolina at Chapel Hill approved the study prior to data collection. All participants signed a written informed consent document and provided verbal permission to audio-record their interviews.
2.1. Participants
Twenty-five NCAA Division I athletes (n = 13 females; age = 20.1 ± 0.8 years, mean ± SD) representing 13 sports participated in this study during the fall of 2017. Persons enrolled at the participating institution who were on a current athletic roster were eligible to participate. Most participants were Caucasian (n = 20, 80%), non-Hispanic (n = 21, 84%), non-first year students (n = 23, 92%), without histories of concussion (n = 16, 64%), and they had been previously exposed to concussion education (n = 23, 92%) (Table 1).
Table 1.
Participants’ demographics.
| Variable | n (%) |
|---|---|
| Gender | |
| Male | 12 (48) |
| Female | 13 (52) |
| Race | |
| Caucasian | 20 (80) |
| African American | 5 (20) |
| Academic year | |
| Freshman | 2 (8) |
| Sophomore | 2 (8) |
| Junior | 12 (48) |
| Senior | 8 (32) |
| Graduate student | 1 (4) |
| Sport | |
| Collision | |
| Football | 5 (20) |
| High/medium contact | |
| Basketball (women) | 1 (4) |
| Cheerleading (women) | 3 (12) |
| Lacrosse (women) | 1 (4) |
| Soccer (women) | 1 (4) |
| Wrestling (men) | 1 (4) |
| Low/non-contact | |
| Baseball | 1 (4) |
| Cross country/track and field (men) | 3 (12) |
| Cross country/track and field (women) | 2 (8) |
| Diving (women) | 1 (4) |
| Fencing (women) | 1 (4) |
| Golf (men) | 1 (4) |
| Rowing (women) | 1 (4) |
| Softball (women) | 2 (8) |
| Swimming (men) | 1 (4) |
| Socioeconomic status proxy | |
| At least 1 parent with a bachelor's degree | 18 (72) |
| Previous concussion history | |
| Yes | 9 (36) |
| No | 16 (64) |
| Previous concussion education | |
| Yes | 23 (92) |
| No | 2 (8) |
2.2. Instrumentation
The quantitative survey consisted of closed-ended items regarding demographics, previous concussion-related disclosure behaviors, knowledge, attitudes, beliefs, norms, and intentions toward disclosing concussion. It was adapted from a previous survey to better reflect a college-aged population. It included an additional section on general consequences, fewer belief/social norm items, as well as additional items about school-related and social impacts of concussion.15,17 The survey was validated for face and content validity after the revisions. One item included 3 subquestions that were used to assess previous concussion-related disclosure behaviors; each subquestion was rated as a yes/no with respect to lifetime experience with each behavior. Knowledge (identification of concussive symptoms and consequences) was assessed by 48 questions; the resulting scale ranged from 0 to 48 (higher score = better knowledge). Attitudes (e.g., difficulty of reporting; when someone would/would not report) were assessed with 6 questions rated on a 7-point Likert scale (1 = strongly disagree to 7 = strongly agree); the resulting scale ranged from 6 to 42 (higher scores = more positive attitudes). Beliefs were assessed by 2 questions (level of control and whether or not someone should report) rated on a 7-point Likert scale (1 = strongly disagree to 7 = strongly agree); the resulting scale ranged from 2 to 14 (higher scores = greater alignment with sports safety). Last, intention was assessed via a single question (“When I experience concussive symptoms, I intend to report them”) on a 7-point Likert scale (1 = strongly disagree to 7 = strongly agree).
The qualitative interview was semistructured and consisted of 7 open-ended questions related specifically to concussion experience, knowledge, attitudes, and disclosure. These questions asked about experiences participants have had with disclosing concussions as well as their perceptions of factors that may impact their ability and/or willingness to disclose a potential concussive injury. The interview questions and protocol were developed based on previous research and in consultation with content, clinical, and methodological experts.15,17 The interview protocol was revised for question content and clarity based on feedback.
2.3. Procedures
After expressing interest in participating during an in-person recruitment session, participants were contacted via e-mail by a research assistant. Researchers contacted interested participants on a first-come, first-served basis, making an attempt to balance the number of participants between males and females. Upon receipt of response confirming their interest, the research assistant scheduled a time for each participant to come to the research laboratory to complete testing. Upon arriving, participants did the following: (1) signed a written informed consent document; (2) completed a pretest questionnaire; (3) took the online concussion-education platform; (4) completed a post-test questionnaire (excluding demographics); and (5) participated in the semistructured interview. The educational platform and post-test questionnaire were related specifically to the larger investigation and were not included as a part of this study. To protect participants’ confidentiality, the resulting interview audio file was transcribed, and any identifying material was removed at the end of each testing session.
2.4. Data analysis
Specific quantitative and qualitative analyses are described in detail below. Once the quantitative and qualitative analyses were completed, findings were integrated to support the larger issue regarding the context of concussion disclosure. Integration occurred via a joint display array (Table 2) where quantitative and qualitative data were presented in tandem.
Table 2.
Attitudes, beliefs, and intention joint display array.a
| Variable | Median (IQR) | Qualitative findings |
|---|---|---|
|
Knowledge (range: 0 (poor) to 48 (ideal)) (See Table 3 for specific items) |
46.0 (39.5–47.5) | Previous experience with concussion improves ability to recognize and understand symptoms Lack of visible signs and symptoms prevents honest disclosure Education is emphasized only in contact sports |
| Attitudes (range: 6 (poor) to 42 (ideal)) | 38.0 (32.0–39.5) | Stigma makes disclosing more difficult External pressure from coaches to keep playing Internal pressure from fear of losing starting spot, not wanting to let team down Need team support to make individual decisions Need to create a culture of support and encouragement Peer leadership (team captains) to set example for difficult decisions |
| Reporting concussion symptoms is: | ||
| Harmful (1)–beneficial (7) | 7.0 (6.5–7.0) | |
| Cowardly (1)–brave (7) | 6.0 (4.5–7.0) | |
| Extremely difficult (1)–extremely easy (7) | 5.0 (3.0–7.0) | |
| Bad (1)–good (7) | 7.0 (6.0–7.0) | |
| Unimportant (1)–important (7) | 7.0 (7.0–7.0) | |
| Shameful (1)–prideful (7) | 5.0 (4.0–7.0) | |
| Beliefs (total range: 2 (poor) to 14 (ideal)) | 13.0 (12.5–14.0) | Participants feel they have control but may accept that coaches also have a large, if not larger, influence over disclosure decisions Coaches should not have a role in the decision to report Medical professionals serve as a liaison between coach and athlete, improving disclosure |
| I have control over reporting concussion symptoms Range = 1 (strongly disagree) to 7 (strongly agree) |
7.0 (6.0–7.0) | |
| I should report concussive symptoms Range = 1 (strongly disagree) to 7 (strongly agree) |
7.0 (7.0–7.0) | |
| Intention (range: 1 (none) to 7 (always)) | 7.0 (6.0–7.0) | Athletic trainer presence is essential to willingness to report Open communication creates an environment of trust Athletic trainers’ job is to watch and notice, making intention not a factor |
| When I experience concussive symptoms, I intend to report them | 7.0 (6.0–7.0) |
Abbreviation: IQR = interquartile range.
Quantitative variables consist of scores from the pretest questionnaire.
2.4.1. Quantitative
Quantitative analyses were conducted using SAS Version 8 (SAS Institute, Cary, NC, USA). Researchers examined the data using the Shapiro-Wilk normality test. Given that data were non-normally distributed, medians and frequencies were reported for all demographic and construct (knowledge, attitudes, beliefs, norms, and intention) variables. Mann-Whitney U tests compared each construct by gender to confirm or dispute influences supported in previous literature. An a priori alpha level of 0.05 dictated all statistical significance.
2.4.2. Qualitative
Qualitative analyses followed a consensual qualitative research tradition that is based in grounded theory and phenomenology. This approach allows researchers to understand and analyze participants’ experiences and circumstances. This method specifically requires the use of multiple researchers to establish consensus, creating a rigorous methodological approach to data analyzation.18 The research team consisted of 3 individuals, ranging from novice to expert with respect to their experience with qualitative research. Previous literature supports the use of a novice in order to bring new perspectives to data analysis and reduce researcher bias.18 An additional research team member with qualitative experience served as an auditor to ensure all aspects of data analysis were considered, thereby further reducing researcher bias.18 The auditor had no role in data collection, consensus, or management.
The consensual qualitative research approach uses 4 progressive stages, including: (1) identification of key words; (2) establishment of categories/themes; (3) cross-analyzation of multiple transcripts’ keywords, categories, and themes; and (4) establishment of data frequency.18 This approach also centers on the consensus of the research team. Individual team members coded Stage 1, Stage 2, and Stage 3 independently before meeting as a group to establish consensus with respect to the identified categories and themes. In the event of disagreement, the auditor was consulted to ensure all viewpoints were considered before forming a consensus decision. At this point, a consensus codebook was established. This consensus codebook was then used by research team members who individually coded interviews. After each interview was coded, the research team met once again to discuss coding decisions and ensure consensus for all data placement. Finally, frequency was established for each category and theme. For the purpose of this study, a category/theme was considered general if applied to at least 23 participant cases, typical if applied to between 13 and 22 cases, variant if applied to between 4 and 12 cases, and rare if applied to fewer than 4 cases. Frequency is used in this approach to ensure ease of interpretation for those who may be unfamiliar with qualitative research analyses.18
3. Results
In general, participants did not discuss significant personal hardships involving concussion disclosure; however, they did discuss factors that may explain why they have been successful and why others may have difficulty. Of the 9 individuals (36%) reporting at least 1 concussion, 78% of them stated that they reported their concussion at the time of injury, that it was diagnosed, and that it was caused by sport participation. The factors assessed by this study included concussion-related knowledge, attitudes, beliefs, and intentions to disclose a potential injury. No gender differences were observed with respect to any of the 4 factors within the survey (Table 3). The interviews resulted in 5 primary themes; 2 were related to educational platform feedback and were not included in the current study. The 3 remaining themes were as follows: (1) perceptions and satisfaction with concussion education; (2) factors influencing disclosure; and (3) role expectations in concussion (Table 4). All qualitative data from the 3 included themes were reviewed for their relevance and were included as part of the corresponding survey domain.
Table 3.
Mann-Whitney U tests of differences between gender on outcome variables.a
| Variable | Mean | SD | Median | IQR | p |
|---|---|---|---|---|---|
| Knowledge score | 44.0 | 4.7 | 46.0 | 39.5–47.5 | |
| Male | 46.5 | 39.0–48.0 | 0.804 | ||
| Female | 46.0 | 41.5–47.0 | |||
| Attitude score | 35.8 | 5.1 | 38.0 | 32.0–39.5 | |
| Male | 38.0 | 31.0–42.0 | 0.494 | ||
| Female | 35.0 | 32.0–39.0 | |||
| Belief score | 13.0 | 1.5 | 13.0 | 12.5–14.0 | |
| Male | 13.5 | 12.3–14.0 | 0.977 | ||
| Female | 13.0 | 12.5–14.0 | |||
| Intention score | 6.6 | 0.7 | 7.0 | 6.0–7.0 | |
| Male | 7.0 | 6.0–7.0 | 0.422 | ||
| Female | 7.0 | 6.0–7.0 |
Abbreviation: IQR = interquartile range.
Quantitative variables consisted of scores from the pretest questionnaire.
Table 4.
Overarching study codebook.
| Theme | Category |
|---|---|
| Perceptions and satisfaction with concussion education | Channels |
| Source | |
| Message | |
| Initial education | |
| Continuing education | |
| Factors influencing disclosure | Intrapersonal |
| Interpersonal | |
| Physical environment | |
| Perceptions and knowledge of concussion | |
| Role expectations in concussion | Individual |
| Teammates | |
| Coaches | |
| Medical professionals | |
| Other |
3.1. Knowledge
The quantitative data suggest that participating NCAA athletes had relatively high concussion-related knowledge levels (median = 46.0, IQR : 39.5–47.5). This knowledge included symptoms, consequences of suffering a concussion in general, consequences of returning to play too soon after a concussion, and consequences of suffering multiple concussions. Visible signs/symptoms related to concussion (i.e., trouble balancing, difficulty concentrating, difficulty remembering, etc.) were most often correctly identified by participants (Table 5). Emotional symptoms (i.e., being more emotional, irritable, and sad) were less often correctly identified, with identification ranging from 68% to 80% of participants. Overall, participants understood the consequences of sustaining concussions, returning to play too soon, and suffering multiple concussions with respect to their likelihood of sustaining another injury, suffering brain damage, and possibly experiencing trouble performing daily activities. Participants also knew that at least 1 bad thing can happen in each of the 3 areas. Less frequently identified consequences of suffering a concussion or returning from a concussion too soon included impacts on school and social activities. Additionally, participants struggled to identify the possible consequences of suffering multiple concussions.
Table 5.
Knowledge constructs (range : 0–48).
| Variable | T/F | n (%correct) |
|---|---|---|
| Symptoms | ||
| Blurry vision | T | 25 (100) |
| Confusion | T | 25 (100) |
| Difficulty concentrating | T | 25 (100) |
| Difficulty remembering | T | 25 (100) |
| Trouble balancing | T | 25 (100) |
| Dizziness | T | 24 (96) |
| Feeling in a fog | T | 24 (96) |
| Headache | T | 24 (96) |
| Not feeling right | T | 24 (96) |
| Sensitivity to noise | T | 24 (96) |
| Sensitivity to light | T | 24 (96) |
| Skin rash | F | 24 (96) |
| Nausea | T | 23 (92) |
| Pressure in head | T | 23 (92) |
| Drowsiness | T | 22 (88) |
| Feeling slowed down | T | 22 (88) |
| Fatigue | T | 21 (84) |
| Joint pain | F | 21 (84) |
| Being more emotional | T | 20 (80) |
| Irritability | T | 18 (72) |
| Nervousness | T | 18 (72) |
| Trouble falling asleep | T | 18 (72) |
| Sadness | T | 17 (68) |
| Neck pain | T | 15 (60) |
| General consequences | ||
| I don't know what might happen | F | 25 (100) |
| More likely to sustain another concussion | T | 25 (100) |
| No bad things can ever happen | F | 25 (100) |
| Skin rash | F | 25 (100) |
| Trouble with school | T | 25 (100) |
| Brain damage | T | 23 (92) |
| Difficulty with everyday activities | T | 23 (92) |
| Difficulty with social activities | T | 21 (84) |
| Consequences of returning to play too soon | ||
| I don't know what might happen | F | 25 (100) |
| No bad things can ever happen | F | 25 (100) |
| Skin rash | F | 25 (100) |
| More likely to sustain another concussion | T | 24 (96) |
| Brain damage | T | 23 (92) |
| Difficulty with everyday activities | T | 23 (92) |
| Trouble with school | T | 21 (84) |
| Difficulty with social activities | T | 20 (80) |
| Consequences of suffering multiple concussions | ||
| Difficulty with everyday activities | T | 25 (100) |
| Difficulty with social activities | T | 25 (100) |
| No bad things can ever happen | F | 25 (100) |
| Skin rash | F | 25 (100) |
| Brain damage | T | 24 (96) |
| I don't know what might happen | F | 24 (96) |
| Trouble with school | T | 24 (96) |
| More likely to sustain another concussion | T | 20 (80) |
Note: Quantitative variables consist of scores from the pretest questionnaire.
Abbreviations: F = false; T = true.
In the qualitative interviews, 1 participant commented, “People don't realize how little things can turn into something big”, when discussing the potential long-term consequences of nondisclosed and/or improperly managed concussions. The qualitative interviews also highlighted that participants believed several factors affected concussion-related knowledge and the behaviors related to overall concussion knowledge. Several participants discussed how previous experience with concussion can impact your knowledge and understanding of symptoms as well as your ability to recognize an injury in yourself or others. One track and field athlete stated,
If I were to disclose a concussion in the future, I would want to know how it feels and all the symptoms of it.
Another participant discussed the invisibility of signs and symptoms, with a second participant providing further emphasis on how that impacts their decision to tell a person in authority about the situation. One football player said,
With a concussion, it's not like a hurt knee where you can see it. We know that guys have concussions, and they're faking it.
Despite loss of consciousness occurring in only a small subset of concussed patients, the visibility of losing consciousness sparks action. A baseball player mentioned,
If I saw one of my teammates get knocked out, I'm not going to just let him wake up and tell someone later. I'm going to go get a coach or someone (who can help).
Last, participants discussed the role of grass-roots sport culture and the perception that only those participating in contact sports need to be educated about concussion-related dangers. One football player said,
I think it's all about how you're educated at a young age. That's probably how you'll respond when you're older.
A diver emphasized,
I think it's really important (concussion education). I think it's important for all athletes to be educated.
3.2. Attitudes
Participants generally had positive attitudes toward concussion-related disclosure behaviors (median = 38.0, IQR : 32.0–39.5). This study included assessments of thoughts and emotions caused by reporting concussion symptoms. Participants generally felt that reporting concussion symptoms was beneficial (median = 7.0, IQR : 6.5–7.0), good (median = 7.0, IQR : 6.0–7.0), and important (median = 7.0, IQR : 7.0–7.0); however, there were greater discrepancies in whether or not reporting was brave (median = 6.0, IQR : 4.5–7.0), prideful (median = 5.0, IQR : 4.0–7.0), or easy (median = 5.0, IQR : 3.0–7.0). Table 2 displays the connections between quantitative and qualitative findings.
Specifically, participants mentioned several factors that could impact personal and peer attitudes concerning concussion disclosure and nondisclosure. They addressed the presence of stigma, pressure (external and internal), and sport culture. Regarding stigma, several athletes addressed the role of “faking” concussions and how the appearance of removing yourself from participation comes off as “weak”. Pressure was highlighted by 1 football player and 1 track and field athlete:
In college there are always the guys behind you trying to take your spot, and if you're out, he's getting the reps while you sit on the sideline. I think that has a lot to do with it (not disclosing).
I think we're in it for the win, and whatever has to happen to get that (win) has to happen.
Another football player highlighted the desire for support and a positive culture surrounding health in general:
You're supposed to have everyone's back. That's not just on the field or when you're out on the weekends. It's their overall health, and I think that needs to be established as a team.
However, in 1 circumstance, a football player discussed the difficulty of taking the initiative as a teammate to report another teammate's struggle. He said,
It's not my job to tell someone else about my teammate. I know I probably should tell someone, but I don't take responsibility for that. It's up to my teammate to do something.
3.3. Beliefs
Beliefs addressed 2 primary concussion-related factors, both of which were rated highly by participants. The first factor evaluated their level of perceived control over reporting concussion symptoms (median = 7.0, IQR : 6.0–7.0), and the second asked whether or not they felt they should report concussive symptoms (median = 7.0, IQR : 7.0–7.0). The participants understood the importance of reporting and felt confident in being able to report; however, approximately 25% of athletes chose not to report. Table 2 displays the connections between quantitative and qualitative findings.
Some of the influential discussions surrounding beliefs included the role of coaches and medical professionals. Specifically, coaches were mentioned as having a primary influence on decision making about reporting concussion symptoms. Participants argued that coaches should not have a role in the decision to remove an individual from play, but that did not take away from the fact that coaches influenced everyone around them. One rower noted,
I guess if there was more education about it, especially with coaches (that would be helpful). Everyone wants the coaches to be on their side, and the coaches have a big influence on whether someone reports an injury.
A cheerleader mentioned coaches’ having a positive influence on reporting by stating,
Our coaches are really open with us. So that's the main thing. Just being able to feel comfortable to tell them.
Last, participants highlighted how medical professionals, specifically athletic trainers, can improve disclosure by acting as a liaison between coaches and athletes. By having a medical professional advocate for student athletes, the student athlete is less hesitant to speak up in a time of need. A wrestler stated,
We're supposed to bypass our coach. If we're sick or hurt we don't have to tell the coach. We're not coming to practice as long as we've talked to the (athletic) trainer.
Ultimately, participants desired the presence of an individual, such as an athletic trainer, who can advocate for their health and who would have the authority to remove someone from play, particularly in scenarios where other influencing factors might be stronger (such as a game). A rower summed up the importance of this role by saying,
Being around enough to know how someone acts normally and then if they're not acting normally, having the authority to tell them to stop.
3.4. Intentions
The last component addressed the intentions of athletes to report experiencing concussion-related signs and/or symptoms. Participants had strong intentions to disclose (median = 7.0, IQR : 6.0–7.0), and they voiced several factors that may contribute to their intentions. Table 5 displays the connections between quantitative and qualitative findings.
Qualitatively, participants described the role of the athletic trainer as a primary influence on their intention to disclose. Specifically, having an athletic trainer is vital to ensuring that people are willing to report; their continued presence and communication allow for a sense of trust among athletes and staff. One softball player highlighted this by saying,
I guess if they (medical professionals) are there more consistently, that would build the relationship with the players. You know that they're always going to be there, so you feel more trusting with them.
Participants also mentioned that their perception of the athletic trainer’s job is to watch and notice these injuries, taking intention out of the equation entirely. As they perceived it, athletic trainers should be able to recognize these injuries to the point where the athletes themselves do not need to speak up. One football player explicitly stated,
I feel like the athletic trainers should be watching. It's their job to notice. They should take the action to pull them off the field (as opposed to the athlete coming off and telling them).
4. Discussion
This study aimed to explore factors influencing concussion disclosure. By using a mixed methodological approach, the research team highlighted confirmatory/discordant findings with respect to previous literature and provided context examining how the factors mattered. Previous literature has found that knowledge,9 attitudes,14,15 and beliefs/perceived norms15 influence concussion-disclosure behaviors; however, the contexts as well as the relationships among factors remain unclear. Guided by the socioecological model, participants provided clarity about the context in which these factors are important. In general, participants were knowledgeable about concussion, had positive or safe attitudes toward concussion, strong beliefs toward concussion behaviors, and the intention to disclose concussion symptoms. Despite previous research that found gender differences within concussion-disclosure behavior,12 the findings from this study did not differ by gender. Even though participants had primarily positive quantitative findings, the context provided through qualitative research displays the complexities concerning concussion care-seeking and disclosure behaviors.
4.1. Knowledge
Participants had high levels of knowledge related to the symptoms and consequences of suffering a concussion. Across previous research with collegiate athletes, concussion knowledge is consistently on the higher end of the spectrum.19,20 It is important to note that the majority of concussion-education legislation was implemented between 2009 and 2014. Therefore, collegiate athletes should have been exposed previously to concussion education at the high school level, which may have led to higher knowledge scores. Despite having strong knowledge overall, participants struggled with identifying the emotional symptoms and social and academic consequences of concussion. Outwardly visible symptoms, such as a loss of balance, tend to be more easily recognized. It is common for collegiate athletes to fail to recognize emotional changes as symptoms of concussion, while endorsing other symptoms that are, in fact, inaccurate.20,21 This misunderstanding of concussion may significantly hinder the ability of athletes to disclose their injuries because they do not truly understand the factors that are considered symptoms of concussion. Additionally, there is a significant stigma associated with mental health symptomology.22,23 Many of the lesser known concussion-related symptoms may be indicative of mental health status. Thus, it is possible that student athletes associate these symptoms only with mental health status and not also with concussion; however, further research is needed. Previous experience may also play a role within this sample regarding the perception of concussion history's effect on concussion knowledge and behaviors. Ironically, previous concussion history seems to have inconsistent effects on concussion knowledge.13,21
Although prior research has focused on quantitative data, the addition of the qualitative research methods in this study allowed our research team to further identify and explore the quantitative findings. Participants indicated that they wanted to know what a concussion feels like and what to expect in order to better understand how to recognize the injury. Even with high levels of symptom-recognition knowledge, participants felt that concussions are misunderstood. This is an important distinction. There has to be a baseline level of knowledge to be able to recognize and subsequently disclose an injury; knowledge in and of itself is not enough to prompt action. Therefore, future educational initiatives should prioritize symptom recognition alongside athletes’ understanding of the concussion experience. The educational process should incorporate lived experiences in order to create comprehensive knowledge-based outcomes. As such, future research should prioritize exploration of perceived knowledge and confidence in symptom recognition.
4.2. Attitudes
In general, participants had positive attitudes toward concussion, which the literature posits as a common factor influencing intentions to disclose concussion.12,13,24,25 Participants felt that disclosing concussions was an important, beneficial, and good behavior. Although there was consensus about concussion disclosure’s being a positive action overall, there was greater discrepancy regarding whether or not it is the brave thing to do and whether or not the action of disclosing was easy or difficult. Having positive attitudes is an important step to prioritizing future concussion disclosure, but previous research suggests that having positive attitudes is not enough to produce action.19,26, 27, 28 There may be discrepancies between the intention to disclose and actual disclosure behaviors following injury, and there are many reasons why an individual may not act, even when the benefits of acting are recognized.
Much of the qualitative discussion regarding attitudes in this study revolved around 3 primary areas: stigma, pressure, and the culture of sport. Participants also specifically highlighted the negative connotation associated with “faking” concussions and the detrimental effect that can have on team dynamics. Approximately one-quarter of collegiate athletes have felt pressure from at least 1 source (coaches, parents, teammates, and/or fans) to avoid disclosing a concussion.29 Previous research examining disclosure motivation highlights both internal and external forms of pressure, including someone trying to take an individual's spot on the team, not wanting to let others down, and not wanting to come out of the practice or game.12,19 Our participants expressed that these factors contributed to the culture of sport and to the pressure they experienced; they also specifically highlighted how these factors intersect to create an overall lack of support regarding concussion disclosure. The intersection of personal expectations and perceived team-based or stakeholder expectations creates an atmosphere where pressure and cultural implications can be internalized, if not explicitly stated. It is important to build a network of support within the athletics community in order to go beyond positive attitudes to elicit actual disclosure.
4.3. Beliefs
Participants strongly believed that they should report concussion symptoms and that they had control over being able to report them. However, the overall findings show that following through with disclosing a concussion is difficult. In addition, even with strong intentions to disclose, the decision to act on intention may be delayed or may not occur at all.15 Two primary areas were suggested for optimizing follow-through. First, participants highlighted the role of the coach in decision making. Whether verbalized or perceived, coaches have influence over the decisions their athletes make; such decisions may be related to injury disclosure, abuse disclosure, external activities, school, and more.29, 30, 31 In the presence of negative team-based relationships, athletes may not feel comfortable disclosing injuries, which potentially puts them at risk of future and further injury occurrence.32,33 In contrast, positive sport cultures, which include supportive teammates and coaches, appear to facilitate the disclosure process.34,35 Participants also discussed the role of medical professionals in making concussion disclosure follow-through easier. Specifically, having access to an athletic trainer while suffering a concussion makes it easier to decide to disclose it in the moment rather than waiting to report it.36, 37, 38 Also, if athletes have a relationship with the medical professional, it is even more likely that they would be willing to disclose injuries.39 Based on the findings of studies concerning coachs’ influence, it is not surprising that athletes may be hesitant to report directly to a coach in the absence of medical professionals.
The qualitative data related to beliefs support the notion that simply knowing what steps to take does not mean individuals will take them. If roadblocks exist to disclosure, such as a lack of medical professional presence or a coach with differing beliefs, it is unlikely that participants will take the step to act. Additionally, having a medical professional present may lend to higher levels of perceived behavioral control. As such, prioritizing medical professional presence during athletic activity (practices and competitions) and creating a team culture supportive of disclosure are vital steps toward successful concussion-disclosure behavior among athletes. Additionally, the interviews highlighted how participants sometimes misinterpret the role of athletic trainers, thinking they should be able to recognize all concussions, thereby rendering self-disclosure unnecessary. Although ideal, it is unrealistic to expect an athletic trainer to identify every single concussion, particularly in the absence of visible signs and/or symptoms. Athletic trainers or other medical professionals may not always be present at the concussive event or injury. Therefore, an important part of educational intervention for student athletes is making sure they understand that the potential “invisibility” of concussion and lack of immediate medical access highlight the need for them to encourage teammates who have sustained a concussion to seek care promptly.
4.4. Intentions
Regardless of the individual factors influencing concussion disclosure, there is a high level of agreement among participants and in the concussion literature that athletes intend to make the appropriate decision and disclose concussion symptoms.15,24,40,41 It is important to note that in this study all athletes had access to athletic trainers. As seen above, the relationship between athletic trainers and athletes can positively influence attitudes, norms, and thoughts related to concussion disclosure.
One unique aspect of the current study's approach to assessing intention is how it highlighted that participants’ strong intention to disclose may exist because they do not expect to have to make the decision themselves. Participants felt it was athletic trainers who ultimately hold the power to remove someone from play. In theory, athletic trainers are responsible for the health and safety of athletes, but athletic trainers are not capable of monitoring every single athlete at every single moment. Athletic trainers also feel subject to pressure (whether perceived or verbalized), fear of job loss, and discomfort, particularly when housed under an athletics model of employment rather than a medical model of employment.42,43 Employing athletic trainers within a medical model (vs.within athletics) is the gold standard for administrative operations, providing adequate medical supervision with less pressure and influence from external sources.42,44 It is unfair to expect athletic trainers to be able to identify symptoms not outwardly visible in all patients, but it is important for athletic trainers to serve as patient advocates and help to create a supportive environment that prioritizes concussion disclosure.45 That said, athletes need to take an active role in the disclosure process, which should be facilitated, as opposed to hindered, by the interpersonal influence of coaches, teammates, and even parents. Educational initiatives could promote a higher level of athlete involvement by encouraging self-efficacy and confidence among athletes to see something and say something. This would help the athletic trainers to improve recognition efforts, provide athletes with a sense of responsibility regarding decision making, and cultivate team-based norms supportive of concussion disclosure.
4.5. Limitations and future research
Study limitations include the potential for participants’ recall bias and bias stemming from participants’ originating from only 1 NCAA institution. Qualitative data analysis frequently raises questions regarding researcher bias; however, the methodology used in this study aimed to reduce research subjectivity. Participants were from a convenience sample, so participation bias may exist; however, the current study's findings still may serve as a foundation for improved contextual understanding concerning concussion care seeking and care in the collegiate population. Only 2 participants had sustained a concussion during the previous academic year, so it may have been more difficult for most others to remember details about their experiences. Also, there were only a few participants per sport, and the sports had various levels of contact. The NCAA mandates concussion education regardless of contact level, but those participating in sports with greater contact during childhood may have been exposed to more extensive concussion education in the past. Additionally, although including a few participants from a variety of sports helped to reduce the influence of specific sport cultures, thereby providing a more generalized understanding, it is likely that nuances exist within each sport-specific environment. Last, participants were interviewed after completing the educational platform. That would not influence their pretest survey responses, but it may have provided information participants could consider while answering the interview questions. Future research should purposefully sample members of teams from various sports in order to examine the contexts of disclosure as they relate to sport-specific norms. Such research should also focus on the optimization of concussion-education programming for collegiate athletes, and it should revolve around recognition of the responsibility to disclose concussions and the delineation of the roles of individuals involved (such as athletic trainers, coaches, and the athletes themselves). It should also address the cultural implications of concussion, as opposed to focusing strictly on knowledge.
5. Conclusion
Knowledge, attitudes, beliefs, and intentions all influence disclosure decisions in some capacity. Previous research supports this notion, but the current study provides greater context regarding how and why these influences may occur. Knowledge, attitudes, beliefs, and intentions are all important to consider when designing concussion education; however, prioritizing supportive social and physical environments conducive to disclosure may be the most important. By having access to athletic trainers and having positive team dynamics and supportive relationships, concerns about the influence of knowledge, attitudes, beliefs, and intentions may lessen. The present study, in line with other work,46 highlights that concussion education should be ongoing, inclusive, and far-reaching in order to address cultural implications of concussion as well as the baseline knowledge required to recognize that an injury has occurred. To optimize future disclosure, concussion education should involve all stakeholders (i.e., coaches, athletic trainers, and athletes) and address individual-level and team/school-level beliefs and perceived norms. Specifically, education should include delineation of the roles of all involved, including medical professionals, coaches, teammates, and players (with the consideration that many concussions take place in the absence of a medical professional). Additionally, education should target the mental and social consequences of concussion, as opposed to focusing solely on physical impacts.
Acknowledgments
Acknowledgments
This work was supported by the National Collegiate Athletic Association–Department of Defense (NCAA–DOD) Mind Matters Research Challenge Award. The funding agency had no role in the study design, data collection, analysis and interpretation of the data, in the writing of the report, or in the decision to submit the article for publication.
Authors’ contributions
MCK was involved in project design, data collection, data analysis, and manuscript drafting; HHK was involved in project design and data analysis; PG was involved in project design, data collection, and data analysis; BMI was involved in data collection and manuscript drafting; ZYK, KLC, MNH, LAL, SWM, and KYP were involved in project design; JKRM was involved in project design, data analysis, and manuscript drafting. All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
Supplementary materials
References
- 1.Kerr ZY, Marshall SW, Dompier TP, Corlette J, Klossner DA, Gilchrist J. College sports-related injuries–United States, 2009–10 through 2013–14 academic years. MMWR Morb Mortal Wkly Rep. 2015;64:1330–1336. doi: 10.15585/mmwr.mm6448a2. [DOI] [PubMed] [Google Scholar]
- 2.Bryan MA, Rowhani-Rahbar A, Comstock RD, Rivara F. Seattle Sports Concussion Research Collaborative. Sports- and recreation-related concussions in US youth. Pediatrics. 2016;138 doi: 10.1542/peds.2015–4635. [DOI] [PubMed] [Google Scholar]
- 3.Rosenthal JA, Foraker RE, Collins CL, Comstock RD. National high school athlete concussion rates from 2005–2006 to 2011–2012. Am J Sports Med. 2014;42:1710–1715. doi: 10.1177/0363546514530091. [DOI] [PubMed] [Google Scholar]
- 4.Dompier TP, Kerr ZY, Marshall SW, et al. Incidence of concussion during practice and games in youth, high school, and collegiate American football players. JAMA Pediatr. 2015;169:659–665. doi: 10.1001/jamapediatrics.2015.0210. [DOI] [PubMed] [Google Scholar]
- 5.Kroshus E, Baugh CM. Concussion education in U.S. collegiate sport: What is happening and what do athletes want? Health Educ Behav. 2016;43:182–190. doi: 10.1177/1090198115599380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kerr ZY, Evenson KR, Rosamond WD, Mihalik JP, Guskiewicz KM, Marshall SW. Association between concussion and mental health in former collegiate athletes. Inj Epidemiol. 2014;1:28. doi: 10.1186/s40621-014-0028-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Llewellyn T, Burdette GT, Joyner AB, Buckley TA. Concussion reporting rates at the conclusion of an intercollegiate athletic career. Clin J Sport Med. 2014;24:76–79. doi: 10.1097/01.jsm.0000432853.77520.3d. [DOI] [PubMed] [Google Scholar]
- 8.Torres Colón GA, Smith S, Fucillo J. Concussions and risk within cultural contexts of play. Qual Health Res. 2017;27:1077–1089. doi: 10.1177/1049732316669339. [DOI] [PubMed] [Google Scholar]
- 9.Delaney JS, Lamfookon C, Bloom GA, Al-Kashmiri A, Correa JA. Why university athletes choose not to reveal their concussion symptoms during a practice or game. Clin J Sport Med. 2015;25:113–125. doi: 10.1097/JSM.0000000000000112. [DOI] [PubMed] [Google Scholar]
- 10.McCrory P, Meeuwisse W, Dvořák J, et al. Consensus statement on concussion in sport: The 5th International Conference on Concussion in Sport held in Berlin, October 2016. Br J Sports Med. 2017;51:838–847. doi: 10.1136/bjsports-2017-097699. [DOI] [PubMed] [Google Scholar]
- 11.Moreau MS, Langdon JL, Buckley Thomas A. The lived experience of an in-season concussion amongst NCAA Division I student-athletes. Int J Exerc Sci. 2014;7:62–74. [Google Scholar]
- 12.Kerr ZY, Register-Mihalik JK, Kroshus E, Baugh CM, Marshall SW. Motivations associated with nondisclosure of self-reported concussions in former collegiate athletes. Am J Sports Med. 2016;44:220–225. doi: 10.1177/0363546515612082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Register-Mihalik JK, Valovich McLeod TC, Linnan LA, Guskiewicz KM, Marshall SW. Relationship between concussion history and concussion knowledge, attitudes, and disclosure behavior in high school athletes. Clin J Sport Med. 2017;27:321–324. doi: 10.1097/JSM.0000000000000349. [DOI] [PubMed] [Google Scholar]
- 14.Cranmer GA, LaBelle S. Using the disclosure decision-making model to understand high school football players’ disclosures of concussion symptoms. Int J Sport Commun. 2018;11:241–260. [Google Scholar]
- 15.Register-Mihalik JK, Cameron KL, Kay MC, et al. Determinants of intention to disclose concussion symptoms in a population of U.S. military cadets. J Sci Med Sport. 2019;22:509–515. doi: 10.1016/j.jsams.2018.11.003. [DOI] [PubMed] [Google Scholar]
- 16.Bronfenbrenner U. Toward an experimental ecology of human development. Am Psychol. 1977;32:513–531. [Google Scholar]
- 17.Register-Mihalik JK, Guskiewicz KM, McLeod TCV, Linnan LA, Mueller FO, Marshall SW. Knowledge, attitude, and concussion-reporting behaviors among high school athletes: A preliminary study. J Athl Train. 2013;48:645–653. doi: 10.4085/1062-6050-48.3.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hill CE, Knox S, Thompson BJ, Williams EN, Hess SA, Ladany N. Consensual qualitative research: An update. J Couns Psychol. 2005;52:196–205. [Google Scholar]
- 19.Conway FN, Domingues M, Monaco R, et al. Concussion symptom underreporting among incoming national collegiate athletic association Division I college athletes. Clin J Sport Med. 2020;30:203–209. doi: 10.1097/JSM.0000000000000557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fedor A, Gunstad J. Limited knowledge of concussion symptoms in college athletes. Appl Neuropsychol Adult. 2015;22:108–113. doi: 10.1080/23279095.2013.860604. [DOI] [PubMed] [Google Scholar]
- 21.Cusimano MD, Zhang S, Topolovec-Vranic J, Hutchison MG, Jing R. Factors affecting the concussion knowledge of athletes, parents, coaches, and medical professionals. SAGE Open Med. 2017;5 doi: 10.1177/2050312117694794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smith RA, Applegate A. Mental health stigma and communication and their intersections with education. Commun Educ. 2018;67:382–393. doi: 10.1080/03634523.2018.1465988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pedersen ER, Paves AP. Comparing perceived public stigma and personal stigma of mental health treatment seeking in a young adult sample. Psychiatry Res. 2014;219:143–150. doi: 10.1016/j.psychres.2014.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kroshus E, Baugh CM, Daneshvar DH, Viswanath K. Understanding concussion reporting using a model based on the theory of planned behavior. J Adolesc Health. 2014;54:269–274. doi: 10.1016/j.jadohealth.2013.11.011. e2. [DOI] [PubMed] [Google Scholar]
- 25.Register-Mihalik JK, Linnan LA, Marshall SW, McLeod TCV, Mueller FO, Guskiewicz KM. Using theory to understand high school aged athletes’ intentions to report sport-related concussion: Implications for concussion education initiatives. Brain Inj. 2013;27:878–886. doi: 10.3109/02699052.2013.775508. [DOI] [PubMed] [Google Scholar]
- 26.Register-Mihalik JK, Marshall SW, Kay MC, et al. Perceived social norms and concussion-disclosure behaviours among first-year NCAA student-athletes: Implications for concussion prevention and education. Res Sports Med. 2021;29:1–11. doi: 10.1080/15438627.2020.1719493. [DOI] [PubMed] [Google Scholar]
- 27.Sullivan L, Molcho M. Gender differences in concussion-related knowledge, attitudes and reporting-behaviours among high school student-athletes. Int J Adolesc Med Health. 2018;33:1. doi: 10.1515/ijamh-2018-0031. [DOI] [PubMed] [Google Scholar]
- 28.Kerr ZY, Register-Mihalik JK, Marshall SW, Evenson KR, Mihalik JP, Guskiewicz KM. Disclosure and non-disclosure of concussion and concussion symptoms in athletes: Review and application of the socio-ecological framework. Brain Inj. 2014;28:1009–1021. doi: 10.3109/02699052.2014.904049. [DOI] [PubMed] [Google Scholar]
- 29.Kroshus E, Garnett B, Hawrilenko M, Baugh CM, Calzo JP. Concussion under-reporting and pressure from coaches, teammates, fans, and parents. Soc Sci Med. 2015;134:66–75. doi: 10.1016/j.socscimed.2015.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chrisman SP, Quitiquit C, Rivara FP. Qualitative study of barriers to concussive symptom reporting in high school athletics. J Adolesc Health. 2013;52:330–335. doi: 10.1016/j.jadohealth.2012.10.271. e3. [DOI] [PubMed] [Google Scholar]
- 31.Baugh CM, Meehan WP, Kroshus E, McGuire TG, Hatfield LA. College football players less likely to report concussions and other injuries with increased injury accumulation. J Neurotrauma. 2019;36:2065–2072. doi: 10.1089/neu.2018.6161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pensgaard AM, Ivarsson A, Nilstad A, Solstad BE, Steffen K. Psychosocial stress factors, including the relationship with the coach, and their influence on acute and overuse injury risk in elite female football players. BMJ Open Sport Exerc Med. 2018;4 doi: 10.1136/bmjsem-2017-000317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jowett S. What makes coaches tick? The impact of coaches’ intrinsic and extrinsic motives on their own satisfaction and that of their athletes. Scand J Med Sci Sports. 2008;18:664–673. doi: 10.1111/j.1600-0838.2007.00705.x. [DOI] [PubMed] [Google Scholar]
- 34.Chase MA, Magyar TM, Drake BM. Fear of injury in gymnastics: Self-efficacy and psychological strategies to keep on tumbling. J Sports Sci. 2005;23:465–475. doi: 10.1080/02640410400021427. [DOI] [PubMed] [Google Scholar]
- 35.Malinauskas R. College athletes’ perceptions of social support provided by their coach before injury and after it. J Sports Med Phys Fitness. 2008;48:107–112. [PubMed] [Google Scholar]
- 36.Pierpoint LA, LaBella CR, Collins CL, Fields SK. Dawn Comstock R. Injuries in girls’ soccer and basketball: A comparison of high schools with and without athletic trainers. Inj Epidemiol. 2018;5:29. doi: 10.1186/s40621-018-0159-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Echlin PS, Johnson AM, Riverin S, et al. A prospective study of concussion education in 2 junior ice hockey teams: Implications for sports concussion education. Neurosurg Focus. 2010;29:E6. doi: 10.3171/2010.9.FOCUS10187. [DOI] [PubMed] [Google Scholar]
- 38.Urban JE, Cheramie EK, Kopacki M, et al. Presence of athletic trainers in a youth football organization: A single institution's experience. Athl Train Sports Health Care. 2017;9:53–57. [Google Scholar]
- 39.Phillips J. The relationship between the athlete and the athletic trainer and how it effects concusison reporting. Electronic Theses and Dissertations Paper 116. Georgia Southern University; Statesboro, Georgia. 2010.
- 40.Kroshus E, Garnett BR, Baugh CM, Calzo JP. Social norms theory and concussion education. Health Educ Res. 2015;30:1004–1013. doi: 10.1093/her/cyv047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Register-Mihalik JK, Marshall SW, Kay MC, et al. Perceived social norms and concussion-disclosure behaviours among first-year NCAA student-athletes: Implications for concussion prevention and education. Res Sports Med. 2021;29:1–11. doi: 10.1080/15438627.2020.1719493. [DOI] [PubMed] [Google Scholar]
- 42.Eason CM, Mazerolle SM, Goodman A. Organizational infrastructure in the collegiate athletic training setting, part III: Benefits of and barriers in the medical and academic models. J Athl Train. 2017;52:35–44. doi: 10.4085/1062-6050-51.12.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Goodman A, Mazerolle SM, Eason CM. Organizational infrastructure in the collegiate athletic training setting, part II: Benefits of and barriers in the athletics model. J Athl Train. 2017;52:23–34. doi: 10.4085/1062-6050-51.12.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Baugh CM, Kroshus E, Lanser BL, Lindley TR, Meehan WP. Sports medicine staffing across national collegiate athletic association division I, II, and III schools: Vidence for the medical model. J Athl Train. 2020;55:573–579. doi: 10.4085/1062-6050-0463-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wilkerson G. Patient-centered care and conflict of interests in sports medicine-athletic training. Int J Athl Ther Train. 2012;17:1–3. [Google Scholar]
- 46.Kroshus E, Cameron KL, Coatsworth JD, et al. Improving concussion education: Consensus from the NCAA–Department of Defense Mind Matters Research and Education Grand Challenge. Br J Sports Med. 2020;54:1314–1320. doi: 10.1136/bjsports-2020-102185. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.