Abstract
Objectives
CAD/CAM hybrid materials have become increasingly utilized in restorative dentistry. However, their low tensile bond strength (TBS) may lead to the detachment of minimally invasive restorations. When prepared, an experimental enamel-based biopolymer prosthesis provided a honeycomb-like interfacial layer with luting adhesives leading to a higher TBS than Ni–Cr–Be based alloy, lithium disilicate-based ceramic, and cured-resin-composite. This study aimed to compare TBSs of dental veneers fabricated from experimental biopolymer and commercial hybrid materials bonded to enamel using two different luting adhesives.
Methods
Laminate veneers (4 × 4 mm) 1 mm thick were prepared from commercial CAD/CAM blocks: VITA ENAMIC, SHOFU Block HC, KATANA AVENCIA, and an experimental biopolymer. The flat bonding surface of the veneers was ground to 600-grit, followed by 50-μm alumina air-abrading for standardization. Each veneer was fixed on flat ground bovine enamel using either Super-Bond C&B or RelyX™ U200 resin (n = 10). The surface treatment and bonding procedures were treated as recommended by the manufacturers. All bonded specimens were stored in water at 37 °C for 24 h before tensile testing with a universal testing machine at a cross-headed speed of 1.0 mm/min. The fractured surface was examined with a stereomicroscope and scanning electron microscope. TBS data were statistically analyzed using two-way ANOVA and Tukey's HSD test (α = 0.05).
Results
Experimental biopolymer veneers demonstrated the highest mean TBS with cohesive failure in the luting agents. Adhesive failure at the veneer side interface was found in other groups. There was no significant difference between the two luting agents.
Conclusion
The results indicate that the experimental biopolymer veneer bonded to enamel provided the best retention. The TBS at the enamel-resin interface is higher than at the veneer-resin interface for all commercial CAD/CAM hybrid materials.
Clinical significance
An experimental enamel-based biopolymer veneer can provide better retention than CAD/CAM hybrid materials in clinical treatment.
Keywords: Dental veneer, CAD/CAM hybrid Ceramics, Tensile bond strength, Enamel-based biopolymer, Luting adhesives, Hybrid materials, Prosthesis retention
1. Introduction
Restorative materials such as ceramic and resin composite restorations have become popular due to their aesthetic qualities. However, dental ceramics have several limitations because of their hardness and brittleness. Their extreme hardness may promote wear on the opposing enamel [1,2], and their brittleness makes restorations prone to fracture. Porcelain fracture is a common failure that can occur with dental ceramic restorations or fixed partial dentures [[3], [4], [5]]. All-ceramic crowns had an 11.024 times greater risk of needing renewal than metal crowns in function up to 15 years. The cause of failure was always from ceramic fracture [3].
Porcelain laminate veneers are one of the most popular cosmetic and minimally invasive of dental treatments. They are 0.5–1.00 mm thick, tooth-colored, and made for patients who desire to improve their appearance. These veneers can change the color, contour, shape, and size of the teeth they cover and bond to using luting adhesives. A thin layer of enamel (0.5–1.00 mm) is removed to provide space for each veneer which will protect the prepared enamel or dentin after bonding with resin adhesives [6].
In dentistry, CAD/CAM (Computer-aided design/Computer-aided manufacturing) technology has become increasingly utilized and popular. It was created with various benefits in mind, including speed, quality control, lower marginal discrepancy after cementation, and repeatability [7,8]. A new CAD/CAM hybrid material combines the benefits of ceramic and polymer features, such as increased flexural capability, less abrasiveness, and improved color stability and durability [9,10]. Air-abrasion, hydrofluoric acid, and silanization of CAD/CAM hybrid material can significantly increase the tensile bond strength [[11], [12], [13], [14]]. The bonding characteristics vary depending on the brands of commercial CAD/CAM hybrid materials, which have different microstructures and chemical composition characteristics [11,15]. Commercial brands of hybrid materials, such as polymer-infiltrated ceramic network (PICN) material (VITA ENAMIC), Zirconia-silica ceramic (SHOFU Block HC), and resin nanoceramic (Lava Ultimate), have been introduced to the market.
A dental prosthesis fabricated using an experimental hybrid material, an enamel-based biopolymer, provided a microhardness value and color similar to human enamel. Furthermore, surface treatment with 50 μm alumina blasting and phosphoric acid etching of this biopolymer can create a honeycomb-like interfacial layer when using Super-Bond C&B luting cement, leading to a higher TBS than that of air-blasted lithium disilicate-based ceramic, based metal alloy, and cured resin composite [16]. According to these properties, an experimental enamel-based biopolymer can be the selected material for a CAD/CAM dental laminate veneer. For the long-term clinical survival of laminate veneers, developing durable materials with strong adhesive properties and ease of preparation is essential.
The study hypothesis was that a honeycomb-like interface of an experimental enamel-based biopolymer might improve dental veneer retention compared with commercial CAD/CAM hybrid materials. This research aimed to evaluate the tensile bond strength of the different microstructures of hybrid material veneers bonded on bovine enamel surfaces.
2. Materials and methods
The Faculty Executive Committee, Faculty of Dentistry, Chulalongkorn University, Bangkok, Thailand, approved the study protocol. Fig. 1 shows a schematic workflow of the principal experimental procedures.
Fig. 1.
A schematic workflow of experimental procedures.
2.1. Preparation of laminate veneers and tooth surface
A laminate veneer, 4 mm × 4 mm, and 1 mm thick, was prepared from commercial CAD/CAM hybrid materials and an experimental enamel-based biopolymer blocks using a sectioning machine (Isomet, Buehler, Lake Bluff, IL) and a diamond disk. The main compositions of four hybrid materials (VITA ENAMIC, SHOFU Block HC, KATANA AVENCIA, Experimental biopolymer), two luting adhesives with ceramic primers (Super-Bond C&B with Universal Ceramic Primer; RelyX™ U200 with RelyX Ceramic Primer) used in this study were listed in Table 1. The veneers’ bonding surfaces of each group (n = 20) were ground flat for surface standardization with 400-grit and 600-grit silicon carbide (Si–C) abrasive papers in a polishing machine (Minitech 233, Presi, Le Locle, Switzerland) under water cooling. After air-abrading with 50 μm alumina procedures, all veneers were ultrasonically cleaned in distilled water for 15 min and then air-dried. All specimens in each group were randomly divided into two subgroups for two different types of resin cement. The G power program calculated a sample size of 10 (n = 10) for each group.
Table 1.
Main compositions and manufacturers of commercial hybrid materials, the experimental biopolymer, luting adhesives, and ceramic primers.
| Material | Manufacturer | Composition |
|---|---|---|
| VITA ENAMIC | Vita Zahnfabrik, Germany | 86 wt% feldspar ceramic |
| Polymer: UDMA, TEGDMA | ||
| SHOFU Block HC | Shofu Inc., Kyoto, Japan | 61 wt% zirconium silicate, silicon dioxide |
| Polymer: UDMA, TEGDMA | ||
| KATANA AVENCIA | Kuraray Noritake Dental, Niigata, Japan | 62 wt% alumina filler (20 nm), silica filler (40 nm) |
| Polymer: UDMA, TEGDMA | ||
| Experimental biopolymer | – | 90 wt% bovine enamel |
| Polymer: PMMA | ||
| Super-Bond C&B | Sun Medical, Moriyama, Japan | Monomer: MMA, 4-META; Catalyst: TBB |
| Polymer: PMMA | ||
| RelyX™ U200 | 3M-ESPE St. Paul, MN, USA | Base paste: Methacrylate monomers containing phosphoric acid group, silanated fillers, initiator components, stabilizers |
| Catalyst paste: Methacrylate monomers, alkaline (basic) fillers, silanated fillers, initiator components, stabilizers, pigment | ||
| Universal Ceramic Primer | Sun Medical, Moriyama, Japan | Liquid A: Methacrylic monomer, others |
| Liquid B: Methacrylic monomer, silane coupling agent | ||
| RelyX Ceramic Primer | 3M-ESPE St. Paul, MN, USA | Ethyl alcohol, water, methacryloxypropyltrimethoxysilane |
UDMA = Urethane dimethacrylate; TEGDMA = Triethylene glycol dimethacrylate; PMMA = Poly(methyl methacrylate); MMA = Methyl methacrylate; 4-META = 4-methacryloyloxyethyl trimellitate anhydride; TBB = Tri-n-butyl borane.
The labial aspect of a bovine tooth was sectioned into 4 mm wide, 4 mm long, and 2 mm thick with a diamond disk using a low-speed handpiece and each slab was then embedded in a polyvinyl chloride (PVC) tube with dental stone. The enamel surfaces of all blocks were ground flat for surface standardization with 400-grit and 600-grit silicon carbide (Si–C) abrasive paper in a polishing machine under wet conditions. After polishing, the substrate surfaces were ultrasonically cleaned in distilled water for 15 min and then air-dried. The surface treatment, bonding, and luting steps were treated following the manufacturer's recommendation (Table 2).
Table 2.
Enamel and veneer bonding surface treatment for each luting adhesive.
| Bonding surface | Super-Bond C&B | RelyX™ U200 |
|---|---|---|
| Enamel block | 65% Phosphoric acid (Red activator) 30s, rinse 10s, air-dried 10s | 37% Phosphoric acid 15s, rinse 10s, air-dried 10s |
| VITA ENAMIC | 5% Hydrofluoric acid (HF) for 60s rinse 10s, air-dried 10s, and Universal Ceramic Primer application | 5% Hydrofluoric acid (HF) for 60s rinse 10s, air-dried 10s, and RelyX Ceramic Primer application |
| SHOFU Block HC | Air-blasting with 50-μm aluminum oxide particles perpendicular to the surface from a distance of 10 mm. for 10s at 2 bar pressure before Universal Ceramic Primer was applied | Air-blasting with 50-μm aluminum oxide particles perpendicular to the surface from a distance of 10 mm. for 10s at 2 bar pressure before RelyX Ceramic Primer was applied |
| KATANA AVENCIA | Air-blasting with 50-μm aluminum oxide particles perpendicular to the surface from a distance of 10 mm. for 10s at 2 bar pressure before Universal Ceramic Primer was applied | Air-blasting with 50-μm aluminum oxide particles perpendicular to the surface from a distance of 10 mm. for 10s at 2 bar pressure before RelyX Ceramic Primer was applied |
| Experimental biopolymer | 65% Phosphoric acid (Red activator) 30s, rinse 10 s, air-dried 10s | 65% Phosphoric acid (Red activator) 30s, rinse 10s, air-dried 10s |
2.2. Luting procedure
The bonding interface of 3.0 mm in diameter was standardized using polyethylene tape. The veneer specimens were bonded to the conditioned bovine enamel surfaces using either Super-Bond C&B (Sun Medical, Moriyama, Japan) or RelyX™ U200 (3M-ESPE St. Paul, MN, USA) according to the manufacturer's instructions. Veneer fixing was performed under a constant perpendicular load of 1 kg for 10 min using a customized tool. The Super-Bond C&B groups were left to set in self-curing mode while the RelyX™ U200 groups were light-cured for 40 s with an LED light curing unit (EliparTrilight™ S10, 3M-ESPE St. Paul, MN, USA). The bonded specimens were stored in distilled water at 37 °C for 24 h in an incubator (Contherm 160 M, Contherm Scientific Ltd, Korokoro, Lower Hutt, New Zealand) following the ISO/TS 11405 standard method.
2.3. Tensile bond strength test
All bonded specimens were fixed to a customized metallic tool, placed accurately in a universal testing machine (SHIMADZU, EZ-S 500 N model, Japan), and loaded in tension at a cross-headed speed of 1.0 mm/min until failure occurred following the ISO/TS 11405 guidance. The debonded surface of post-measurement specimens was observed under a stereomicroscope (Olympus Stereo Microscopes, SZ61, Japan) at 40 × magnification to determine the failure patterns and then followed by scanning electron microscope analysis (FEI Quanta 250, OR, USA). Four fractured specimens from the experimental biopolymer group were randomly selected to examine the veneer-resin interfacial layer. Each fractured specimen was sectioned to prepare two 1 mm thick specimens for a polished and a chemical challenge with 6 mol/L Hydrocholic acid (HCl) for 30s specimens. The veneer-luting resin interface of fractured experimental biopolymer was wet abraded from #400 to #2000 grit abrasive papers and polished with 0.05 μm alumina paste. All specimens were ultrasonically cleaned and prepared for SEM examination at × 1500 to × 6000 magnifications to visualize the characteristics of the interface [16].
2.4. Statistical analysis
Statistical analysis was performed using SPSS version 22.0 (SPSS Inc, Chicago, Illinois). First, a two-way analysis of variance (two-way ANOVA) was used to compare the mean tensile strength among groups at a 95% confidence level (α = 0.05), followed by Tukey's HSD post-hoc test to compare between groups.
3. Results
3.1. Tensile bond strength (TBS)
The means and standard deviations (SD) of tensile bond strength and failure modes are summarized in Table 3. Two-way ANOVA showed no statistically significant interaction between hybrid materials and luting agents (p > 0.05). No statistically significant differences in tensile bond strengths were found between the two types of luting resin. One-way ANOVA was used for statistical analysis of veneer material types. The highest mean bond strength was observed for the experimental biopolymer group, while the lowest was observed for SHOFU Block HC groups, regardless of resin adhesives.
Table 3.
Mean values and standard deviations (MPa) of tensile bond strength and mode of failure (number of specimens) for all groups.
| Veneer Material | VITA ENAMIC | SHOFU Block HC | KATANA AVENCIA | Experimental Biopolymer | ||||
|---|---|---|---|---|---|---|---|---|
| Luting resin | Mean ± SD | AV/C/M/AE | Mean ± SD | AV/C/M/AE | Mean ± SD | AV/C/M/AE | Mean ± SD | AV/C/M/AE |
| Super-Bond C&B | 9.01 ± 3.04AC | 7/0/3/0 | 5.34 ± 1.33B | 10/0/0/0 | 8.19 ± 3.59BC | 6/0/4/0 | 12.09 ± 2.08A | 0/10/0/0 |
| RelyX™ U200 | 7.14 ± 2.86B | 7/0/3/0 | 6.00 ± 1.98B | 10/0/0/0 | 7.02 ± 2.90B | 7/0/3/0 | 11.06 ± 2.40A | 0/10/0/0 |
A, B, C Different superscript letters indicate significantly different at p < 0.05.
Failure mode: AV = adhesive failure at the veneer side interface, C = cohesive failure within the luting resin, M = mixed failure of AV and C, AE = adhesive failure at the enamel side interface.
In Super-Bond C&B adhesive group, the experimental biopolymer had the highest mean value (12.09 ± 2.08 MPa), followed by VITA ENAMIC (9.01 ± 3.04 MPa), KATANA AVENCIA (8.19 ± 3.59 MPa), and SHOFU Block HC (5.34 ± 1.33 MPa) respectively. However, there was no significant difference between the experimental biopolymer and VITA ENAMIC.
In RelyX™ U200 adhesive group, the experimental biopolymer showed the significantly highest value (11.06 ± 2.40 MPa), followed by VITA ENAMIC (7.14 ± 2.86 MPa), KATANA AVENCIA (7.02 ± 2.90 MPa), and SHOFU Block HC (6.00 ± 1.98 MPa) respectively.
3.2. Failure mode
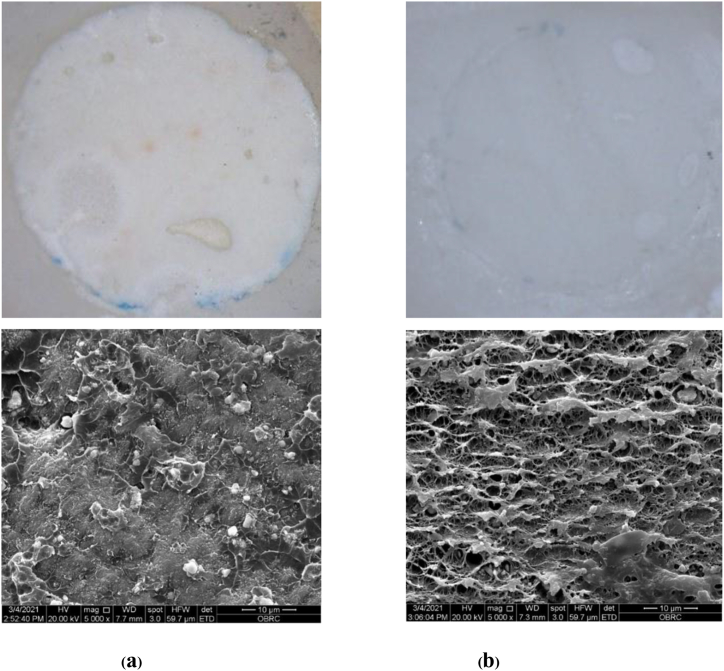
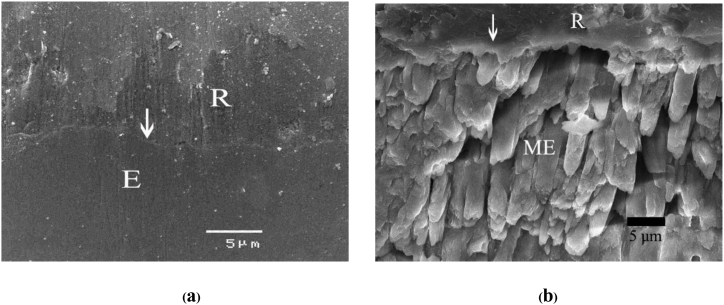
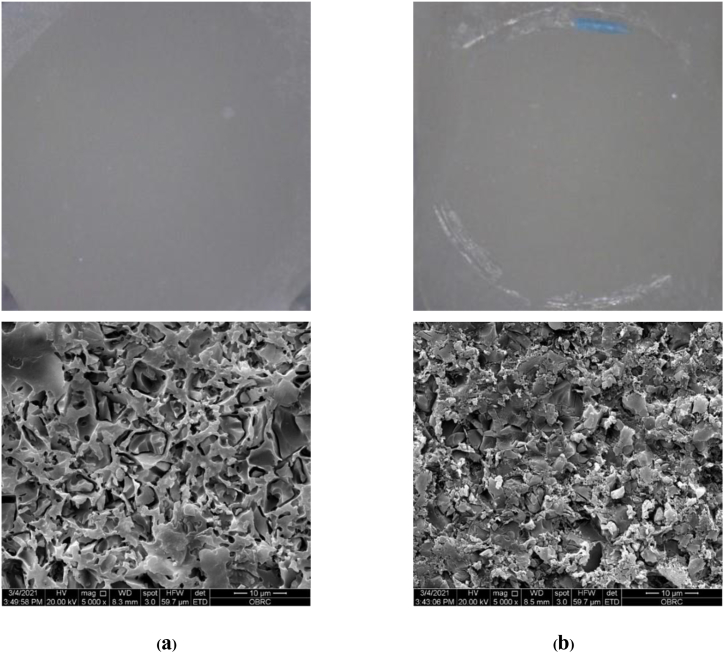
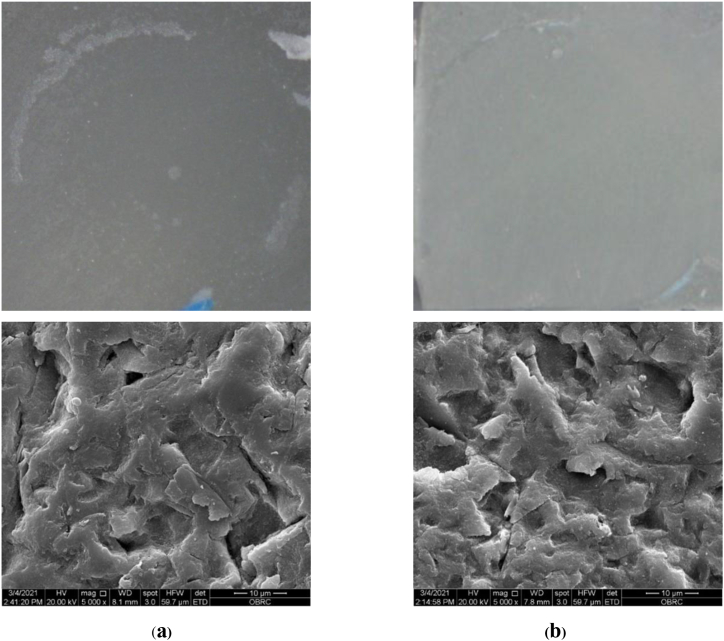
The analysis of failure modes indicated cohesive failure in the cured luting resin (C) for all experimental biopolymer specimens (Fig. 2a and b). A 2–3 μm interfacial layer was found between the experimental biopolymer and luting resin (Fig. 3a and b). Adhesive failure at the veneer side interface (AV) was the most common failure that occurred in VITA ENAMIC (Fig. 4a and b) and KATANA AVENCIA (Fig. 5a and b) groups for both luting agents. Adhesive failure (AV) was found in all SHOFU Block HC specimens (Fig. 6a and b). For all specimens no adhesive failure at the enamel side interface (AE) was seen. Cohesive failure within luting resin, mixed failure, and adhesive failure at the veneer side interface were associated with the highest, higher, and lowest TBS, respectively.
Fig. 2.
Stereomicroscope and SEM images of the fractured surface in experimental biopolymer specimens bonded with (a) Super-Bond C&B, (b) RelyX™ U200 demonstrating the cohesive failure in cured luting resin (C). (original × 40 and × 5000 for Stereomicroscope and SEM, respectively).
Fig. 3.
SEM micrographs of fractured experimental biopolymer bonded with Super-Bond C&B demonstrating the consistent thickness of the hybrid layer (arrowed) at the veneer-luting resin interface in (a) polished and (b) after soaking in 6 mol/L HCl for 30s (original × 3500 and × 6000, respectively; E = experimental biopolymer, R = resin, ME = modified experimental biopolymer).
Fig. 4.
Stereomicroscope and SEM images of the fractured surface in VITA ENAMIC specimens bonded with (a) Super-Bond C&B, (b) RelyX™ U200 demonstrating the adhesive failure at the veneer side interface (AV). (Original × 40 and × 5000 for Stereomicroscope and SEM, respectively).
Fig. 5.
Stereomicroscope and SEM images of the fractured surface in KATANA AVENCIA specimens bonded with (a) Super-Bond C&B, (b) RelyX™ U200 demonstrating the adhesive failure at the veneer side interface (AV). (Original × 40 and × 5000 for Stereomicroscope and SEM, respectively).
Fig. 6.
Stereomicroscope and SEM images of the fractured surface in SHOFU Block HC specimens bonded with (a) Super-Bond C&B, (b) RelyX™ U200 demonstrating the adhesive failure at the veneer side interface (AV) with the dislodgement of filler particles (original × 40 and × 5000 for Stereomicroscope and SEM, respectively).
4. Discussion
Experimental enamel-based biopolymer veneers provided the highest mean tensile bond strength with cohesive failure in both luting agent types (Table 3, Fig. 2a and b). This result suggests that the experimental biopolymer surface treatment using either 65% phosphoric acid etching for 30s or 37% phosphoric acid etching for 15s, rinsed with water, and air-dried 10s could create the permeability needed for luting adhesives to fully impregnate into the micro-spaces as well as that of conditioned bovine enamel. The honeycomb-like pattern interface between experimental enamel-based biopolymer and Super-Bond C&B has been shown in Fig. 3b and reported earlier [16]. The study's results support the hypothesis.
Adhesive failure at the veneer side interface was mainly found (70%) with VITA ENAMIC and KATANA AVENCIA (60%–70%) specimens with lower TBS compared with the experimental biopolymer (Table 3, Fig. 4, Fig. 5b). These results imply that the micro space created either with 5% hydrofluoric acid etching for 60s of VITA ENAMIC or air-blasting with 50-μm aluminum oxide for KATANA AVENCIA produced either less undercut or only partial infiltration with primers and luting resin therefore, mixed failure was found in fewer specimens (30% and 30%–40%, respectively).
CAD/CAM VITA ENAMIC is composed of 86% feldspathic ceramic network and an infiltrated resin (UDMA, TEGDMA), while KATANA AVENCIA contained 62% alumina (20 nm) and silica (40 nm) fillers dispersed in UDMA and TEGDMA resin matrix [7,9]. On the other hand, the experimental biopolymer, composed of 90% bovine enamel and infiltrated with PMMA resin, was more accessible to etch, had higher permeability, and had more undercut irregularity. Therefore, Super-Bond C&B, the PMMA resin using TBB for auto-polymerization, and RelyX™ U200, the light-cured resin-composite, containing 4-META/MMA and methacrylate with phosphoric acid group monomers, respectively could easily penetrate these micro-undercuts. Furthermore, the cohesive failure in resin (Fig. 2a and b) and the honeycomb-like hybrid layer (Fig. 3b) suggests that the phosphoric acid etched experimental biopolymer provides sufficient permeability for those monomers to highly impregnate, resulting in the highest TBS compared with other CAD/CAM commercial hybrid materials.
The SHOFU Block HC group had the lowest TBS with adhesive failure at the veneer side interface in all specimens (Table 3, Fig. 6). It contained 61% nano-filler zirconium metallic glass as an inorganic part in the form of large spherical particles 1–10 μm and silicon dioxide dispersed in UDMA and TEGDMA polymer matrix [17]. The SEM micrograph of the SHOFU Block HC fractured surface demonstrated the dislodgement of filler particles in both luting agents (Fig. 6a and b). This result suggests that air-blasting on the SHOFU Block HC veneer surface creates the least undercut irregularity, and its exposed filler particles after air-blasting are not well attached to the resin matrix, resulting in the easy detachment.
Therefore, inorganic and resin compositions and microstructures of the four hybrid materials tested in this study affected the TBS of laminate veneers regardless of resin luting agents. Air-blasting with alumina or etching with hydrofluoric acid increased bond strength by improving mechanical interlocking and increasing wettability and surface area [11]. According to the surface preparation techniques recommended by the manufacturers, SHOFU Block HC and KATANA AVENCIA were suggested for air abrasion. In contrast, hydrofluoric acid was recommended for VITA ENAMIC, followed by a silane coupling agent [12,18,19]. For etchable feldspathic ceramic, which is the inorganic scaffold of VITA ENAMIC, conditioning with hydrofluoric acid is required. Air abrasion with alumina particles is not suitable for glass ceramic surfaces because it may cause microcracks in the ceramic surface, resulting in prosthesis mechanical failure [11,20]. Resin matrix and inorganic fillers like zirconia and alumina in SHOFU Block HC and KATANA AVENCIA cannot easily be etched; thus, the air abrasion method is more effective.
Several investigations have indicated that a silane coupling agent advised by the manufacturers is useful for enhancing bonding ability by chemically bonding between silica-based inorganic fillers and resin matrix [7,20,21]. However, the silanization effect depended on the microstructure and the amount of inorganic content [11,14,22]. For the VITA ENAMIC glass-ceramic network, the silanization process may contribute to the tight bonding of the material with the resin adhesives. In contrast, a chemical bond with silane did not occur in the SHOFU Block HC surface due to the inorganic part, which is mainly composed of zirconium silicate fillers [23]. In addition, pre-test failure that occurred in SHOFU Block HC specimens has been reported in a previous study [13].
Sandblasting was recommended as a surface preparation procedure for the SHOFU Block HC and KATANA AVENCIA. This approach can improve bond strength by exposing filler particles and improving micro-mechanical retention at the roughened surface [24]. The exposed silica filler particles in KATANA AVENCIA can be reachable for silanization of the ceramic primer, which might help to improve bonding with mixed adhesive and cohesive failure in some specimens. However, the SEM micrograph revealed the dislodgement of filler particles from the SHOFU Block HC fractured surface (Fig. 6a and b), which might be from the air blasting, as reported earlier [15,25]. When air-blasting is at 2 bar pressure, the material surface is damaged, creating a 1–10 μm gap between the filler particles and resin matrix. Due to the manufacturing process, inorganic filler particles are often treated with silane [26]. Adding silanized filler particles to the resin matrix will increase the resin composite materials' mechanical strength and improve their hydrolytic stability. However, a silane coupling agent alone may be insufficient for bonding to non-silica-based filler particles like zirconia. Because of lacking polar bonds, zirconia-filler surfaces cannot create chemical bonds with silane hydroxyl groups [27]. As a result of the decreased bond to the resin matrix, inorganic components may be dislodged after mechanical roughening. Consequently, the silane coupling agent in the primers was also less effective with fewer fillers, leading to the reduced bonding capacity and TBS value of SHOFU Block HC.
All specimens had no adhesive failure at the enamel side interface (AE). The TBS at the enamel-resin interface is higher than at the veneer-resin interface for all commercial CAD/CAM hybrid materials. The cohesive failure in luting resin of the experimental enamel-based biopolymer, which consisted of 90% hydroxyapatite by weight in a network pattern and provided the highest retention for dental veneers, created an interfacial layer (Fig. 3) similar to the hybridized enamel [[28], [29], [30]]. Hybridized enamel formed using Super-Bond C&B could provide a leakage-free interface that resists HCl acid, dye, and silver nitrate penetration [28,29] and survive under long-term cyclic loading (2,500,000 cycles) [30].
Although there was no significant difference in TBS between the luting agents on bonding the veneer to enamel (Table 3), the complete hybridized cementum/dentin margin/interface without dye or silver nitrate penetration, and a higher TBS than the prosthesis-cement interface could be formed using Super-Bond C&B [28,[30], [31], [32]]. In contrast, RelyX™ U200 provided adhesive failure at the dentin-cement interface [33]. The six months’ water storage statistically significantly reduced the micro-tensile bond strength of dentin bonding that had an adhesive failure at demineralized dentin [34]. Although exposed collagen in the demineralized dentin is gradually hydrolyzed, the mini-dumbbell-shaped bonded specimens help detect this demineralized dentin, the defect, remaining under prosthesis within 24 h water storage showing the significantly lower TBS [32]. Therefore, in clinical veneer cases with margins on cementum/dentin, Super-Bond C&B may provide better retention.
Furthermore, phosphoric acid etching is a simple and safe method for conditioning a veneer surface, making the experimental biopolymer hybrid material retain the highest. Intraoral repairing of fractured veneer using hydrofluoric acid or sandblasting surface treatment risks causing soft tissue irritation or damaging the veneer surface [11,20,35]. This study result suggests safer intraoral repairing with higher retention of experimental biopolymer than other tested commercial CAD/CAM hybrid materials. However, this in-vitro study compared the TBS of dental veneers after 24 h water storage, which is the first screening test to show the potential for bonding the biopolymer as an indirect restorative material to enamel. Thus to predict long-term clinical retention, a long-term thermocycling test is required.
5. Conclusions
Within the scope of this investigation, achieving high retention of dental veneers was dependent on the types of veneer material and the surface preparation techniques. Regardless of luting resin agents, an inorganic scaffold or network provides better adhesion than the inorganic fillers dispersed in a resin matrix of hybrid materials. The phosphoric etched experimental enamel-based biopolymer creates the best tensile bond strength without harming the tissues or dental veneers.
Author contribution statement
Morakot Piemjai: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Chakriya Donpinprai: Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Data availability statement
Data will be made available on request.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper
Acknowledgments
The authors would like to express their appreciation to Associate Professor John Harcourt, The University of Melbourne, for editorial suggestions.
References
- 1.Kelly J. Ceramics in restorative and prosthetic dentistry. Annu. Rev. Mater. Sci. 2003;27:443–468. [Google Scholar]
- 2.Deval P., Tembhurne J., Gangurde A., Chauhan M., Jaiswal N., Tiwari D. A Clinical comparative evaluation of the wear of enamel antagonists against monolithic zirconia and metal-ceramic crowns. Int. J. Prosthodont. (IJP) 2021;34:744–751. doi: 10.11607/ijp.6598. [DOI] [PubMed] [Google Scholar]
- 3.Piemjai M., Adunphichet N. Impact of hybrid layer formation on the 15-year survival, complications, and failures of full-coverage retainers. J. Prosthodont. Res. 2022;66:131–140. doi: 10.2186/jpr.JPR_D_20_00249. [DOI] [PubMed] [Google Scholar]
- 4.Aslam A., Khan D.A., Ahmed B. Ceramic fracture in metal-ceramic restorations: the aetiology. Dent. Update. 2017;44(5):448–456. doi: 10.12968/denu.2017.44.5.448. [DOI] [PubMed] [Google Scholar]
- 5.Competition of fracture mechanisms in monolithic dental ceramics: flat model systems. Zhang Y., Kim J.W., Bhowmick S., Thompson V.P., Rekow, editors. J. Biomed. Mater. Res. B Appl. Biomater. 2009;88(2):402–411. doi: 10.1002/jbm.b.31100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.El-Mowafy O., El-Aawar N., El-Mowafy N. Porcelain veneers: an update. Dental and Med. Probl. 2018;55(2):207–211. doi: 10.17219/dmp/90729. [DOI] [PubMed] [Google Scholar]
- 7.Davidowitz G., Kotick P. The use of CAD/CAM in dentistry. Dent. Clin. 2011;55:559–570. doi: 10.1016/j.cden.2011.02.011. ix. [DOI] [PubMed] [Google Scholar]
- 8.Ahmadi E., Hasani Tabatabaei M., Sadr S.M., Atri F. Comparison of the marginal discrepancy of PFM crowns in the CAD/CAM and lost-wax fabrication techniques by triple scanning. Dent Med Probl. 2020;57(4):417–422. doi: 10.17219/dmp/125532. [DOI] [PubMed] [Google Scholar]
- 9.Coldea A., Swain M.V., Thiel N. Mechanical properties of polymer-infiltrated-ceramic-network materials. Dent. Mater. 2013;29(4):419–426. doi: 10.1016/j.dental.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 10.Badawy R.L., El-Mowafy O., Tam L. Flexural properties of chairside CAD/CAM materials. Dental and Medical Problems. 2016;53(2):230–235. doi: 10.17219/dmp/62196. [DOI] [Google Scholar]
- 11.Elsaka S.E. Bond strength of novel CAD/CAM restorative materials to self-adhesive resin cement: the effect of surface treatments. J. Adhesive Dent. 2014;16(6):531–540. doi: 10.3290/j.jad.a33198. [DOI] [PubMed] [Google Scholar]
- 12.Peumans M., Valjakova E.B., De Munck J., Mishevska C.B., Van Meerbeek B. Bonding effectiveness of luting composites to different CAD/CAM materials. J. Adhesive Dent. 2016;18(4):289–302. doi: 10.3290/j.jad.a36155. [DOI] [PubMed] [Google Scholar]
- 13.Reymus M., Roos M., Eichberger M., Edelhoff D., Hickel R., Stawarczyk B. Bonding to new CAD/CAM resin composites: influence of air abrasion and conditioning agents as pretreatment strategy. Clin. Oral Invest. 2019;23(2):529–538. doi: 10.1007/s00784-018-2461-7. [DOI] [PubMed] [Google Scholar]
- 14.Gilbert S., Keul C., Roos M., Edelhoff D., Stawarczyk B. Bonding between CAD/CAM resin and resin composite cements dependent on bonding agents: three different in vitro test methods. Clin. Oral Invest. 2016;20(2):227–236. doi: 10.1007/s00784-015-1494-4. [DOI] [PubMed] [Google Scholar]
- 15.Yoshihara K., Nagaoka N., Maruo Y., Nishigawa G., Irie M., Yoshida Y., et al. Sandblasting may damage the surface of composite CAD-CAM blocks. Dent. Mater. 2017;33(3):e124–e135. doi: 10.1016/j.dental.2016.12.003. [DOI] [PubMed] [Google Scholar]
- 16.Piemjai M., Santiwarapan P. An enamel based biopolymer prosthesis for dental treatment with the proper bond strength and hardness and biosafety. Polymers. 2022;14:538. doi: 10.3390/polym14030538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kimmich M., Stappert C.F. Intraoral treatment of veneering porcelain chipping of fixed dental restorations: a review and clinical application. J. Am. Dent. Assoc. 2013;144(1):31–44. doi: 10.14219/jada.archive.2013.0011. [DOI] [PubMed] [Google Scholar]
- 18.Awad M.M., Albedaiwi L., Almahdy A., Khan R., Silikas N., Hatamleh M.M., et al. Effect of universal adhesives on microtensile bond strength to hybrid ceramic. BMC Oral Health. 2019;19(1):178. doi: 10.1186/s12903-019-0865-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shinagawa J., Inoue G., Nikaido T., Ikeda M., Burrow M.F., Tagami J. Early bond strengths of 4-META/MMA-TBB resin cements to CAD/CAM resin composite. Dent. Mater. J. 2019;38(1):28–32. doi: 10.4012/dmj.2017-438. [DOI] [PubMed] [Google Scholar]
- 20.Nagai T., Kawamoto Y., Kakehashi Y., Matsumura H. Adhesive bonding of a lithium disilicate ceramic material with resin-based luting agents. J. Oral Rehabil. 2005;32(8):598–605. doi: 10.1111/j.1365-2842.2005.01464.x. [DOI] [PubMed] [Google Scholar]
- 21.Blatz M.B., Sadan A., Kern M. Resin-ceramic bonding: a review of the literature. J. Prosthet. Dent. 2003;89(3):268–274. doi: 10.1067/mpr.2003.50. [DOI] [PubMed] [Google Scholar]
- 22.Yano H.T., Ikeda H., Nagamatsu Y., Masaki C., Hosokawa R., Shimizu H. Correlation between microstructure of CAD/CAM composites and the silanization effect on adhesive bonding. J. Mech. Behav. Biomed. Mater. 2020;101 doi: 10.1016/j.jmbbm.2019.103441. [DOI] [PubMed] [Google Scholar]
- 23.Özcan M. Evaluation of alternative intra-oral repair techniques for fractured ceramic fused-to-Metal restorations. J. Oral Rehabil. 2003;30:194–203. doi: 10.1046/j.1365-2842.2003.01037.x. [DOI] [PubMed] [Google Scholar]
- 24.da Costa T.R., Serrano A.M., Atman A.P., Loguercio A.D., Reis A. Durability of composite repair using different surface treatments. J. Dent. 2012;40(6):513–521. doi: 10.1016/j.jdent.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 25.Nobuaki A., Keiichi Y., Takashi S. Effects of air abrasion with alumina or glass beads on surface characteristics of CAD/CAM composite materials and the bond strength of resin cements. J. Appl. Oral Sci. 2015;23(6):629–636. doi: 10.1590/1678-775720150261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Matinlinna J.P., Lung C.Y.K., Tsoi J.K.H. Silane adhesion mechanism in dental applications and surface treatments: a review. Dent. Mater. 2018;34(1):13–28. doi: 10.1016/j.dental.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 27.Dai S., Chen Y., Yang J., He F., Chen C., Xie H. Surface treatment of nanozirconia fillers to strengthen dental bisphenol A-glycidyl methacrylate-based resin composites. Int. J. Nanomed. 2019;26(14):9185–9197. doi: 10.2147/IJN.S223392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Piemjai M., Thaveeratana A., Nakabayashi N. Marginal integrity between a prefabricated composite block and enamel, DEJ and dentin bonded by three adhesive resins. Am. J. Dent. 2010;23(5):285–291. [PubMed] [Google Scholar]
- 29.Piemjai M., Waleepitackdej O., Garcia-Godoy F. Marginal micro-seal and tensile bond strength of a biopolymer hybrid layer coupled with dental prosthesis using a primerless-wet system. Polymers. 2023;15:283. doi: 10.3390/polym15020283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pattaratiwanont R., Piemjai M., Garcia-Godoy F. Survival of posterior fixed partial dentures with minimal tooth reduction and improved esthetics: an in vitro study. J. Prosthet. Dent. 2022;127:585–592. doi: 10.1016/j.prosdent.2020.09.047. [DOI] [PubMed] [Google Scholar]
- 31.Piemjai M., Chantarawej P., Nakabayashi N. Evaluation of caries-free restorations bonded with various adhesive systems: in vitro study. Int J Dent. 2020;22 doi: 10.1155/2020/5859835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Piemjai M., Nakabayashi N. Direct tensile strength and characteristics of dentin restored with all-ceramic, resin-composite and cast metal prostheses cemented with resin adhesives. BioMed Res. Int. 2015;5:1–10. doi: 10.1155/2015/656948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Małysa A., Weżgowiec J., Danel D., Boening K., Walczak K., Więckiewicz M. Bond strength of modern self-adhesive resin cements to human dentin and different CAD/CAM ceramics. Acta Bioeng. Biomech. 2020;22(2):25–34. [PubMed] [Google Scholar]
- 34.Rêgo H.M., Alves T.S., Bresciani E., Niu L.N., Tay F.R., Pucci C.R. Can long-term dentine bonding created in real life be forecasted by parameters established in the laboratory? Sci. Rep. 2016;6 doi: 10.1038/srep37799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bajraktarova-Valjakova E., Korunoska-Stevkovska V., Georgieva S., Ivanovski K., Bajraktarova-Misevska C., Mijoska A., et al. Hydrofluoric acid: burns and systemic toxicity, protective measures, immediate and hospital medical treatment. Open Access Maced J Med Sci. 2018;6(11):2257–2269. doi: 10.3889/oamjms.2018.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.