Abstract
Purpose of Review
The risk of cardiovascular complications due to SARS-CoV-2 are significantly increased within the first 6 months of the infection. Patients with COVID-19 have an increased risk of death, and there is evidence that many may experience a wide range of post-acute cardiovascular complications. Our work aims to provide an update on current clinical aspects of diagnosis and treatment of cardiovascular manifestations during acute and long-term COVID-19.
Recent Findings
SARS-CoV-2 has been shown to be associated with increased incidence of cardiovascular complications such as myocardial injury, heart failure, and dysrhythmias, as well as coagulation abnormalities not only during the acute phase but also beyond the first 30 days of the infection, associated with high mortality and poor outcomes. Cardiovascular complications during long-COVID-19 were found regardless of comorbidities such as age, hypertension, and diabetes; nevertheless, these populations remain at high risk for the worst outcomes during post-acute COVID-19. Emphasis should be given to the management of these patients. Treatment with low-dose oral propranolol, a beta blocker, for heart rate management may be considered, since it was found to significantly attenuate tachycardia and improve symptoms in postural tachycardia syndrome, while for patients on ACE inhibitors or angiotensin-receptor blockers (ARBs), under no circumstances should these medications be withdrawn. In addition, in patients at high risk after hospitalization due to COVID-19, thromboprophylaxis with rivaroxaban 10 mg/day for 35 days improved clinical outcomes compared with no extended thromboprophylaxis.
Summary
In this work we provide a comprehensive review on acute and post-acute COVID-19 cardiovascular complications, symptomatology, and pathophysiology mechanisms. We also discuss therapeutic strategies for these patients during acute and long-term care and highlight populations at risk. Our findings suggest that older patients with risk factors such as hypertension, diabetes, and medical history of vascular disease have worse outcomes during acute SARS-CoV-2 infection and are more likely to develop cardiovascular complications during long-COVID-19.
Keywords: Acute-COVID-19, Post-COVID-19, Cardiovascular manifestations, Myocardial injury, Heart failure, Dysrhythmias
Introduction
Since late December 2019, coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has spread rapidly worldwide, becoming a global pandemic [1–3] accounting for more than 753,823,259 reported cases and more than 6.8 million deaths worldwide as of February 2, 2023 [4]. SARS-CoV-2 frequently causes a respiratory infection manifesting a range of clinical presentations, from asymptomatic subclinical infection to severe viral pneumonia, acute respiratory distress syndrome (ARDS), a life-threatening form of respiratory failure that requires mechanical ventilation and admission to the intensive care unit (ICU) [5], as well as septic shock and specific organ dysfunction [1]. In addition, uncontrolled SARS-CoV-2 infection can trigger a cytokine storm resulting in multi-organ failure [6], while coagulation abnormalities have been reported in patients with COVID-19 leading to thromboembolic events [7]. For the purpose of this review, and according to the Royal College of General Practitioners, COVID-19 infection is divided into three phases: acute COVID-19, including patients with symptoms of COVID-19 infection for up to 4 weeks; subacute or ongoing symptomatic COVID-19 if symptoms persist 4–12 weeks and post-COVID-19 syndrome if symptoms persist after 12 weeks; and long COVID-19 including both ongoing symptomatic COVID-19 and post-COVID-19 syndrome [8, 9].
Given the significant association of COVID-19 with severe cardiovascular damage during the acute phase of the infection and a related increased risk of death [10, 11], there is increasing evidence that many patients with COVID-19 may experience a wide range of post-acute sequelae of cardiovascular complications. We provide herein a comprehensive review of the current literature on acute and post-acute COVID-19 cardiovascular sequelae and their pathophysiological mechanisms. Finally, we discuss therapeutic strategies for these patients during acute and long-term care and highlight populations at high risk.
Clinical Manifestation of SARS-CoV-2 During Acute and Post-COVID-19 Syndrome
Patients with acute SARS-CoV-2 infection may present with a broad spectrum of clinical manifestations, from no clinical evidence of heart disease or asymptomatic cardiac arrhythmias or dysrhythmias, to symptomatic heart disease [12]. Most patients with acute SARS-CoV-2 infection have typical symptoms of COVID-19 including dry cough, sore throat, fever, dyspnea, myalgias, headache, fatigue, diarrhea, and smell or taste abnormalities, as well as lymphopenia, neutrophilia, and bilateral ground-glass opacities on chest computed tomography (CT) scans [10, 13–15]. Even symptoms such as dyspnea are nonspecific and are evaluated as they are more likely caused by a non-cardiac condition (e.g., pneumonia) or cardiac disease. Only a small percentage of patients present with symptoms that may suggest heart disease including palpitations (9%) at 6-month follow-up [16–18] and chest pain at ~20% and 5% at 60-day and 6-month follow-up in the post-acute COVID-19 period, respectively [19]. Therefore, clinical evaluation by different diagnostic modalities such as electrocardiography (ECG), echocardiography, and cardiac magnetic resonance imaging (CMR), serum cardiac troponin, natriuretic peptide (B-type natriuretic peptide [BNP] or N-terminal pro-BNP) levels, and initial laboratory tests to assess for symptoms and signs of heart failure (HF) in addition to history and physical examination are necessary. According to guidelines [20], BNP/NT-proBNP biomarkers in COVID-19 patients should be examined as the combination of the presence or extent of pre-existing cardiac disease and the acute hemodynamic stress related to COVID-19. ECG abnormalities including ST-segment elevation or depression, T-wave depression/inversion, and Q-waves, as well as laboratory tests including troponin, BNP, and D-dimer level elevation, have been commonly reported in patients with COVID-19 [10, 21–24]. Moreover, increased levels of cardiac troponin I (cTnI), BNP, and D-dimer are related to more severe clinical outcomes and higher mortality rates [25–36].
Post-COVID-19 syndrome is poorly understood, as it affects COVID-19 survivors at all levels of disease severity and across all age ranges. Associated cardiovascular events included chest tightness, cardiac arrhythmias, palpitations, and hypotension, as well as increased heart rate, venous thromboembolic diseases, myocarditis, and acute/decompensated HF [37, 38]. The most common prevalent long-term symptom in COVID-19 is chest pain, reported in up to 20% of COVID-19 survivors at 60 days of follow-up [16, 17], while 9% and 5% reported palpitations and chest pain, respectively, at 6 months post-acute COVID-19 [39]. Cardiac damage can manifest as myocarditis, pericarditis, and rhythm abnormalities.
Myocardial Injury
As shown in meta-analyses [40, 41], the most common cardiovascular complications in COVID-19 patients was myocardial injury, at 21.2% (95% CI: 12.3–30.0%), associated with higher mortality rates (51.2% vs. 4.55%, P < 0 .001) [42], poor outcomes [1, 43, 44], and ICU admissions (risk ratio [RR] = 3.78, 95% CI: 2.07–6.89) (Table 1) [45]. Moreover, myocardial injury was reported as an independent predictor of death (hazard ratio [HR] = 2.25, 95% CI: 1.27–3.96, P = 0.005) [28]. SARS-CoV-2 infection includes direct infection and damage to the myocardium causing myocarditis [46], and indirect cardiac damage by type I and type II (secondary to hypoxemia) myocardial infarction (MI) [47]. A prospective observational cohort study in 100 patients who had recently recovered from COVID-19 illness reported that 78 patients (78%) had cardiovascular involvement as a consequence of acute infection as detected by standardized CMR, irrespective of pre-existing conditions. The most prevalent abnormality was myocardial inflammation (defined as abnormal native T1 and T2 measures), detected in 60 patients who had recently recovered from COVID-19 (60%), followed by regional scar and pericardial enhancement. In addition, patients recently recovered from COVID-19 had lower left ventricular ejection fraction (LVEF), higher left ventricle volumes, and elevated native T1 and T2 compared with healthy controls and risk factor-matched controls [48].
Table 1.
Characteristics of cardiovascular complications associated with SARS-CoV2 infection during acute and post-acute phase
| Cardiovascular Complications | Acute incidence | ICU admissions (RR) | Post-acute risk (HR) | References |
|---|---|---|---|---|
|
Myocardial injury Myocarditis Type I or II MI |
21.2% (95% CI: 12.3–30.0) 1.4% 16% (95% CI: 9.0–27.0) |
3.78 (95% CI: 2.07–6.89) 7.94 |
NA 5.38 (95% CI: 3.80–7.59) 1.66 (95% CI: 1.52–1.80) |
[42, 45, 49–54] |
|
Dysrhythmias Atrial arrhythmia AV block Sinus tachycardia Sinus bradycardia |
10.11–15.3% 9.2% (95% CI: 6.5–12.7%) 12% NA NA |
13.09 (95% CI: 7.00–24.47) NA NA NA NA |
1.69 (95% CI: 1.64–1.75) 1.71 (95% CI: 1.64–1.79) NA 1.84 (95% CI: 1.74–1.95) 1.53 (95% CI: 1.45–1.62) |
[1, 40, 41, 53–57] |
|
Heart failure RVD |
22.34% (95% CI: 14.05–33.60) 20.4% (95% CI: 17.1–24.3) |
8.9% ICU admissions OR = 1.70 (95% CI: 1.12–2.56) |
2.29 (95% CI: 2.20–2.39) | [40, 41, 48, 54, 58, 59] |
| Coagulation abnormalities | NA | |||
|
DVT PE VTE |
27% (95% CI: 21–34%) 21% (95% CI: 18–24%) 21.0–42.0% |
NA 2.25 (95% CI: 1.64–3.08) NA |
2.39 (95% CI: 2.27–2.51) 2.55 (95% CI: 2.09–3.11 3.16 (95% CI: 2.63–3.79) 1.95 (95% CI: 1.80–2.12) |
[54, 60, 61] |
| Other complications | [25, 53, 54, 62, 63] | |||
|
Pericarditis Pericardial effusion Takotsubo syndrome |
3.2% 7.2–14% 2–5.6% |
NA NA NA |
1.85 (95% CI: 1.61–2.13) NA NA |
MI: myocardial infarction; AV: atrial ventricular; RVD: right ventricular dysfunction; DVT: deep vein thrombosis; PE: pulmonary embolism; VTE: venous thromboembolism; RR: risk ratio; HR: hazard ratio; ICU: intensive care unit
Myocarditis directly caused by SARS-CoV-2 infection as diagnosed by endomyocardial biopsy, which is the gold standard method according to the European Society of Cardiology [64], is very rare [65, 66]. Although lymphocytic myocarditis was reported in 7.2% of 277 autopsies, only 1.4% met the well-established histological criteria for myocarditis [67]. On the other hand, in a cohort study, 14 out of 112 COVID-19 patients presented with symptoms related to myocardial injury, including elevated cTnI and abnormalities on echocardiography and ECG, whereas none of them met the full criteria for true myocarditis [49]. In addition, SARS–CoV-2 RNA was detected in the heart tissue of postmortem patients (5 out of 12) [68], while in another cohort study, 24 out of 39 autopsy cases (61.5%) supported the presence of SARS-CoV-2 in cardiac tissue; however, none of these tissue samples showed evidence of an influx of inflammatory cells consistent with clinical myocarditis [69]. Nevertheless, this low sensitivity could be attributed to secondary sampling error [70]. In addition, during post-acute COVID-19, only 10–20% of myocarditis is diagnosed with endomyocardial biopsy [70].
On the other hand, the frequency of type I or type II myocardial injury, as defined by elevated cTn levels > 99th percentile, in acute SARS-CoV-2 infection was 16% (95% CI: 9–27%) [50] and 24.4% during hospitalization due to COVID-19 (Table 1) [51]. Thus it is possible that myocardial injury due to SARS-CoV-2 infection is attributable to myocardial oxygen supply–demand imbalance in MI type II rather than MI type I [71, 72]. Nevertheless, this type of myocardial injury has been associated with higher mortality (RR = 7.95, P < 0.001; I2: 65%) and higher rates of ICU admissions (RR = 7.94, P = 0.01; I2: 79%) [52]. Myocardial injury was also significantly associated with a higher incidence of complications, including ARDS (58.5% vs. 14.7%, P < 0.001), acute kidney injury (8.5% vs. 0.3%, P < 0.001), electrolyte disturbance (15.9% vs. 5.1%, P = 0.003), hypoproteinemia (13.4% vs. 4.8%, P = 0.01), and coagulation disorders (7.3% vs. 1.8%, P = 0.02), compared with those without cardiac injury [43].
As reported by Xie et al. and Wang et al., survivors of COVID-19 exhibit higher risk of myocarditis (HR = 5.38, 95% CI: 3.80–7.59) 30 days after discharge and ischemic heart disease (IHD) (HR = 1.66, 95% CI: 1.52–1.80) such as acute coronary disease (HR = 2.048, 95% CI: 1.752−2.393), MI (HR = 1.979, 95% CI: 1.831−2.138), ischemic cardiomyopathy (HR = 2.811, 95% CI: 2.477−3.190), and angina (HR = 1.707, 95% CI: 1.545−1.885) (Table 1) [53, 54].
Dysrhythmias
Cardiac dysrhythmias may be the initial clinical presentation of cardiovascular manifestation of COVID-19 during acute SARS-CoV-2 infection [73], with incidence ranging from 10.11% to 15.3% as shown in meta-analyses [40, 41], and atrial arrhythmia reported at 9.2% (95% CI: 6.5–12.7%) [55]. In addition, patients with newly occurring arrhythmias were at higher risk of developing severe disease or requiring ICU admission (RR = 13.09, 95% CI: 7.00–24.47, P < 0.001) [56]. Atrioventricular (AV) block may account for up to 12% of arrhythmias seen in patients with COVID-19 [57]. In addition, the incidence of cardiac arrhythmia in patients admitted to the ICU was 44.4% [1]. Among hospitalized patients and patients admitted to the ICU, atrial fibrillation, significant bradyarrhythmias, non-sustained ventricular tachycardia (NSVT), and cardiac arrest were common findings [74] in ICU patients, with atrial arrhythmia showing a higher prevalence among patients with poor outcomes [55]. Moreover, patients with elevated troponin T (TnT) levels were associated with malignant arrhythmias, ventricular tachycardia, and fibrillation [30, 75].
Cardiac arrhythmias such as atrial fibrillation, supraventricular tachycardia, complete heart block, and ventricular tachycardia occur in patients infected with, recovering from, and after recovery from COVID-19 [76]. COVID-19 survivors were associated with increased risk of arrhythmia-related disorders as post-COVID conditions, such as atrial fibrillation and flutter (HR 1.71–2.407). Other dysrhythmias reported were tachycardia (HR = 1.682–1.84); bradycardia (HR = 1.53–1.599), and ventricular arrhythmias (HR = 1.600–1.84) (Table 1) [48, 54].
Heart Failure (HF)
Acute HF is reported as the most common complication in COVID-19 patients, with incidence of HF ranging from 14.4% (95% CI: 5.7–23.1) to 22.34% (95% CI: 14.05–33.60) [40, 41], and a high mortality rate, at 47.8% (95% CI: 41.4–54.2) (Table 1) [40]. Another study reported that among 901 admissions to an ICU due to COVID-19, 80 (8.9%) had acute HF, including 18 (2.0%) with classic cardiogenic shock (CS) and 37 (4.1%) with vasodilatory CS. The majority (n = 45) were de novo HF presentations [58], with LVEF ranging from 7.5% to 11% [49, 77]. In addition, HF is one of the most important comorbidities significantly affecting prognosis [54], with a high overall mortality rate ranging between 20% and 40% among patients with previously diagnosed HF and acute SARS-CoV-2 infection [78].
Echocardiographic evaluation in patients diagnosed with SARS-CoV-2 infection reporting a cardiac pathology within 24 hours of admission demonstrated that right ventricular (RV) dilatation and dysfunction was the most common cardiac pathology (observed in 39% of patients), followed by left ventricular (LV) diastolic dysfunction (16%) and LV systolic dysfunction (10%) [25, 79]. A systematic review and meta-analysis in 29 studies including a total of 3813 patients reported a pooled prevalence of right ventricular dysfunction (RVD) of 20.4% (95% CI: 17.1–24.3), with a high grade of heterogeneity (Table 1) [80]. In addition, RVD was associated with worse prognosis [81] and complications such as increased severity (odds ratio [OR] = 3.61, 95% CI: 2.05−6.35, P < 0.001), ICU admission (OR = 1.70, 95% CI: 1.12−2.56, P = 0.01), mechanical ventilation (MV) (OR = 1.60, 95% CI: 1.14−2.25, P = 0.007) [59], and increased all-cause death (OR = 3.32, 95% CI: 1.94–5.70) [80].
In addition, patients who recovered from COVID-19, regardless of pre-existing conditions, had lower left and right ventricular ejection fraction and higher left ventricular volume than healthy controls and risk factor–matched controls [48]. HF-related causes at 30-day readmission were significantly higher in patients with HF with reduced ejection fraction (HFrEF) (47.1%) compared with those with HF with midrange ejection fraction (HFmrEF) (0%) or those with HF with preserved ejection fraction (HFpEF) (8.6%) [82]. Moreover, patients who had recovered from COVID-19 ware associated with an increased risk of HF (HR = 2.29, 95% CI: 2.20−2.39), cardiomyopathy (HR = 1.62–2.413), cardiac arrest (HR = 1.751–2.45), and cardiogenic shock (HR = 1.988–2.43) [48, 54].
Coagulation Abnormalities
Acute SARS-CoV-2 infection has been associated with increased risk of disseminated intravascular coagulation (DIC) and thromboembolic events such as superficial vein thrombosis or so-called venous thromboembolism (VTE) and pulmonary embolism (PE) [10, 19, 83–86], even though there were no other risk factors for thrombosis in these patients [87, 88]. Meta-analysis studies reported that the prevalence of deep vein thrombosis (DVT) in patients with COVID-19 was 27% (95% CI: 21, 34%) [89], while the incidence of pulmonary embolism was 21% (95% CI: 18−24%; P < 0.001) and the incidence of pulmonary embolism in ICU and non-ICU patients was 26% (95% CI: 22−31%; P < 0.001) and 17% (95% CI: 14−20%; P < 0.001), respectively (Table 1). In addition, the predictive role of pulmonary embolism in ICU admission was reported at a diagnostic odds ratio (DOR) of 2.25 (95% CI: 1.64−3.08) [60]. The prevalence of VTE was found to be 21–42%, with VTE more common among older individuals with COVID-19 [83]. In addition, a systematic review and meta-analysis reported that the cumulative incidence of PE and DVT in patients who had recovered from COVID-19 was 1.2% (95% CI:0.9–1.4, I2: 99.8%) and 2.3% (95% CI:1.7–3.0, I2: 99.7%), respectively. Recovered COVID-19 patients presented a higher risk of PE (HR = 3.16, 95% CI: 2.63–3.79, I2: 90.1%) and DVT (HR = 2.55, 95% CI: 2.09–3.11, I2: 92.6%) compared with non-infected patients from the general population over the same follow-up period [61]. Meta-regression showed a higher risk of PE and DVT with age and with female gender, and lower risk with longer follow-up. Recovered COVID-19 patients had a higher risk of VTE (HR = 1.95, 95% CI: 1.80−2.12), which increased with aging and among females [54, 61].
Other Complications
Although limited to case reports, other complications include endocarditis, pericarditis, and Takotsubo syndrome (TTS) [90–95]. In a study of 530 hospitalized patients with COVID-19, pericardial effusion was found in 75 (7.2–14%), but only 17 patients (3.2%) fulfilled the criteria for acute pericarditis (Table 1) [62, 96]. A systematic review of a total of 33 studies (32 case reports and one case series) involving clinical data on patients with COVID-19 and pericarditis reported that pericarditis was found in 8/13 (62%) concurrently with COVID-19 and 5/13 (38%) after COVID-19 with a range from 5 to 56 days [94]. Thirteen patients (38%) were diagnosed with acute pericarditis, whereas the remainder (62%) were diagnosed with myopericarditis [94, 97]. Pericarditis, pericardial effusion, and consequent cardiac tamponade as a complication of myocarditis was also reported in a case study [92]. The most common symptoms were chest pain (68%), fever (65%), and dyspnea (56%). Pericardial friction rub was reported in four cases (two with acute pericarditis and two with myopericarditis) [94]. Diffuse ST-elevation and PR depression ECG pattern was also the most frequent among patients diagnosed with myopericarditis, while pericardial effusion and cardiac tamponade were reported in 76% and 35% of cases, respectively [94]. Although acute pericarditis is the inflammatory condition that affects the pericardium, which is most often due to viral infections, in COVID-19 patients it may be an underdiagnosed pathology. Post-acute sequelae with increased risk of pericarditis was also reported (HR = 1.85, 95% CI: 1.61–2.13) [53, 54]. On the other hand, Takotsubo syndrome (TTS), also referred to as stress-induced cardiomyopathy mimicking acute coronary syndrome [98], is a diagnosis of exclusion. During the COVID-19 pandemic, 2–5.6% (Table 1) [25, 63] were diagnosed with stress-induced cardiomyopathy, whereas before the pandemic, only 1.5–1.8% of patients in this population were diagnosed with TTS [95, 99]. While echocardiograms demonstrate segmental left ventricular dysfunction and patients present with symptoms such as shortness of breath, hypotension, and chest pain, angiography does not reveal significant coronary blockage [100–102]. Several findings, some of them very heterogeneous case reports [95], have shown an increased incidence of TTS that was significantly higher in female COVID-19 patients [95, 103, 104]. However, coronary CT is recommended rather than coronary angiography to rule out the presence of coronary artery disease and TTS [105].
Mechanisms of Cardiac Damage
Coronaviruses are a positive-sense single-stranded RNA (ssRNA) genome, 27–32 kilobases in size, enveloped by the nucleocapsid (N) protein in crown-like morphology; viral particles are 100–160 nm in diameter and present a great capacity for fast mutation and recombination (Fig. 1A) [106, 107], while the viral envelope contains the spike (S), membrane (M) and envelope (E) proteins (Fig. 1A). Infection of target cells by SARS-CoV-2 occurs when the spike (S) protein on the surface of the virus binds to a membrane-bound aminopeptidase, angiotensin-converting enzyme 2 (ACE2) [108], a protein which plays a critical role in the regulation of blood pressure and cardiovascular system homeostasis [109, 110] (Fig. 1B). Spike has a receptor-binding domain (RBD) that mediates direct contact with a cellular receptor and an S1/S2 polybasic cleavage site that is cleaved by cellular cathepsin L and the transmembrane protease serine 2 (TMPRSS2) [111]. After binding on the surface of the cell, TMPRSS2 facilitates the entry of the virus by cleaving the spike protein and promoting the fusion of the viral membrane with the membrane of the host cell [112]. Once the RNA genome of the virus is released, replication-assisting proteins are translated followed by replication of the virus in virus-induced double-membrane vesicles derived from the endoplasmic reticulum (ER) that facilitate viral replication of genomic and subgenomic RNAs translated to form the structural proteins and accessory proteins [113]. RNA replication starts with the synthesis of full-length negative-strand copies of the viral genome. These serve as templates for the production of new positive-strand genomes, which are translated to form more non-structural proteins or are packaged into newly formed virions and released [114, 115]. ACE2 protein and TMPRSS2 are mostly present in respiratory tract epithelial cells, making the lungs the main gateway for the virus [116]. Besides the lung, ACE2 expression is also found in many extrapulmonary tissues including cardiomyocytes and pericytes, leading to cardiovascular complications and partially explaining the extrapulmonary manifestation of SARS-CoV-2 infection [117, 118].
Fig. 1.
Mechanisms of myocardial damage by SARS-CoV2. A SARS-CoV-2 is a spherical viral particle consisting of three structural proteins—envelope glycoprotein, spike, and nucleocapsid protein—and a positive-sense, single-stranded RNA genome. B Infection occurs when spike protein binds to angiotensin-converting enzyme 2 (ACE2), while the transmembrane protease serine 2 (TMPRSS2) facilitates entry of the virus and the viral genome is released into the cytoplasm, followed by genomic replication/transcription and translation of viral proteins. Viral nucleocapsids are assembled in the cytoplasm, followed by budding of new particles at the membrane of the endoplasmic reticulum–Golgi intermediate compartment. Finally, viral genome and structural proteins are assembled into new viral particles and released via exocytosis. C Direct myocardial damage. Direct injury (bold arrows), through direct viral myocardial invasion and activation of inflammatory response activation. Inflammatory cells induced by SARS-CoV-2 or pro-inflammatory cytokines can cause necrosis and death of the myocardium. D Indirect injury, through interaction with ACE2, increases inflammation and endothelial dysfunction. Endothelial cell damage by SARS-CoV-2 increases the hypercoagulability state, thrombosis formation, and inflammatory response activation. Consequently, this may lead to plaque destabilization and atherothrombotic event causing type I MI. In addition, pneumonia and ARDS caused by SARS-CoV-2 and aggravated by cytokine storm exacerbate myocardial oxygen demand/supply mismatch, consequently leading to type II MI
The proposed mechanisms of myocardial injury by SARS-CoV-2 include both direct and indirect mechanisms (Fig. 1C, D). Briefly, direct mechanisms (Fig. 1C) include viral infiltration of cardiomyocytes which can lead to viral direct cell lysis and inflammatory response, consequently leading to myocardial inflammation—myocarditis. Indirect myocardial damage includes SARS-CoV-2 interaction with ACE2 , increased inflammation, cytokine storm release, and endothelial dysfunction which consequently increases hypercoagulability and thrombosis formation, leading to microvascular thrombosis, plaque destabilization, and type I MI (Fig. 1D). In addition, pneumonia and ARDS caused by SARS-CoV-2 and aggravated by cytokine storm exacerbate myocardial oxygen demand/supply mismatch, leading to type II MI. Systemic inflammation seems to be the most prominent mechanism underlying cardiovascular complications of COVID-19. Infection with SARS-CoV-2 is followed by intrinsic immune response and activation of pattern recognition receptors which will lead to the secretion of antiviral cytokines and chemokine levels [10] including interferon-c (INF-c) and pro-inflammatory cytokines including interleukin (IL)-1, IL-6, and tumor necrosis factor alpha (TNF-α) [119]. Inflammatory cells induced by SARS-CoV-2 or pro-inflammatory cytokines can cause necrosis and death of the myocardium (Fig. 1C) and fibro-fatty displacement of desmosomal proteins important for cell-to-cell adherence [120], in addition to endothelial injury and micro-thrombosis, and hypoxia due to ARDS and respiratory failure and coagulopathy activation that can lead to cardiovascular complications (Fig. 1D) [121–123]. IL-1 levels are associated with HF and death [124]. IL-1 is reported to impair cardiac contraction due to suppression of β-adrenergic receptor signaling [125, 126] and nitric oxide production, which in turn inhibits anaerobic glycolysis in cardiac myocytes [127], playing an important role in cardiovascular disease (CVD) [128]. IL-1 also induces the expression of TNF-α [129], which in turn increases concentrations of TNF-α that can impair Keap1/Nrf2 response and result in cardiomyocyte death due to severe oxidative stress [130]. In addition, IL-6 binds to the soluble IL-6 receptor and initiates subsequent signaling through engagement with 130-kDa glycoprotein [131]. Excessive synthesis of IL-6 [132] and activation of the trans-signaling pathway of IL-6 causes inflammation and oxidative stress, which further results in cardiac and cerebral injury [133]. In addition, it is likely that cytokines also increase myocardial electrical instability as a result of direct cell injury (Fig. 1C). TNF, IL-1, and IL-6 are shown to directly and indirectly promote cardiac arrhythmias by modulating cardiomyocyte ion channel expression (Fig. 2) [134, 135]. Increased levels of IL-6 and IL-10 are associated with increased risk of atrial and ventricular arrhythmias in hospitalized COVID-19 patients [136]. Moreover, IL-6 levels and infection status were directly correlated with QTc prolongation [137] and new-onset atrial fibrillation or atrial flutter regardless of patient baseline characteristics [138]. In addition, inflammatory cytokines can induce cardiac fibrosis by activating myofibroblast-driven extracellular matrix synthesis, further impairing the velocity and homogeneity of cardiac conduction (Fig. 2) [135]. Myocardial fibrosis or scarring and the resultant cardiomyopathy from viral infection can lead to re-entrant arrhythmias in post-acute COVID-19 (Fig. 2) [139]. In addition, SARS-CoV-2 may perpetuate arrhythmias due to a heightened catecholaminergic state and autonomic dysfunction after viral illness, resulting in postural orthostatic tachycardia syndrome (POTS) and inappropriate sinus tachycardia (Fig. 2), as was previously reported as a result of adrenergic modulation [140–142], while electrolyte imbalance during COVID-19 illness may increase vulnerability to various tachyarrhythmias [143].
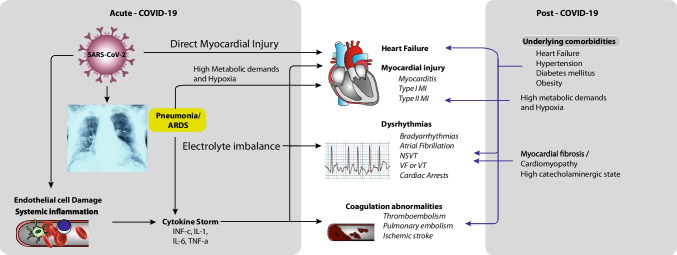
Fig. 2.
Cardiovascular manifestations of SARS-CoV-2 during acute and post-acute phase. During the acute phase (black arrows), SARS-CoV-2 infects host cells of the respiratory tract, endothelial cells, pericytes, and cardiomyocytes, leading to cardiovascular manifestations. Infection of the respiratory tract, particularly type 2 pneumocytes, leads to the development of pneumonia and ARDS, which promote the progression of systemic inflammation and immune system overreaction, leading to cytokine storm. In addition, systemic inflammation increases oxidative stress, electrolyte imbalance, and systemic endothelial dysfunction, resulting in increased incidence of coagulation abnormalities and dysrhythmias. Direct viral infection and cytokine storm may cause myocyte damage and contribute to the development of myocardial fibrosis and cardiomyopathy (black arrows), which in turn can lead to heart failure and dysrhythmias during post-acute manifestation (blue arrows). High catecholamine levels can cause autonomic dysfunction after viral illness, resulting in postural orthostatic tachycardia syndrome and inappropriate sinus tachycardia (blue arrows). In addition, underlying comorbidities in a patient after recovery from COVID-19 can increase the risk of recurrence of cardiovascular manifestations
In addition, endothelial cell injury induced by SARS-CoV-2, cytokine storm, platelets, and inflammatory cells and underlying comorbidities are considered to play a central role in immunothrombosis [7]. In general, endothelial injury is caused by aging, reactive oxygen species, an increased ratio of circulating endothelium microparticles to progenitor cells, a pro-inflammatory state, and/or a decrease in sex hormones [144, 145]. Endothelial dysfunction is also a frequent characteristic in major comorbidities which enhance the risk of SARS-CoV-2 infection and mortality, such as obesity, hypertension, diabetes, coronary artery disease, and HF [146]. The presence of viral inclusions in endothelial cells induces direct damage [147] and attraction of immune cells, resulting in widespread endothelial dysfunction and death [148]. Histological analysis revealed significant changes in endothelial morphology, including cell swelling, disruption of intercellular junctions, and cell death, in post-mortem lung tissues from patients who died from SARS-CoV-2 infection [118]. IL-1, IL-6, and tumor necrosis factor are associated with acute endothelial cell activation, while creating an amplification loop that perpetuates the cytokine storm [149, 150]. Pro-inflammatory cells, cytokines, and chemokines can activate the coagulation system and downregulate crucial physiological anticoagulant mechanisms [149]. The vascular response to hypoxia is controlled primarily by the hypoxia-inducible transcription factors (HIFs), whose target genes include several factors that regulate thrombus formation, which will all be progressively aggravated by the development of local hypoxia [151]. This in turn will establish a deleterious positive thrombo-inflammatory feedback loop [151]. The potential pathophysiological mechanisms that underlie the association between COVID-19 and development of CVD in the post-acute phase are not entirely clear [152, 153]; however, the previously discussed mechanisms in the acute phase, namely inflammatory cytokines, hypoxia induced due to respiratory changes, endothelial damage and damage to the structural integrity of the myocardium, pericardium, and conduction system due to previous infection, may also take place in the post-acute phase (Fig. 2). Moreover, as observed during long-term evaluation, survivors of SARS-CoV-2 infection have persistently increased cardiometabolic demand [154].
Post-Acute COVID-19 Management
Post-COVID is characterized by a diverse range of symptoms spanning multiple organ systems; therefore, outpatient care of COVID-19 survivors is important and should include multidisciplinary collaboration [155]. Priority should be given to groups of patients at high risk of developing post-COVID conditions; according to the Centers for Disease Control and Prevention CDC, this includes people who have experienced more severe COVID-19 illness, especially those who were hospitalized or needed intensive care; those who experience multisystem inflammatory syndrome (MIS) during or after COVID-19 illness; those who have not received a COVID-19 vaccination; and those who had underlying health conditions prior to SARS-CoV-2 infection. Such health conditions include advanced age, pre-existing respiratory disease, obesity, diabetes, hypertension, chronic CVD, chronic kidney disease, post-organ transplant, and active cancer [153, 156]. Chronic cardiovascular disease was associated with increased hospitalization due to SARS-CoV-2 infection, along with thromboembolic risk, septic shock, and higher mortality [10, 157, 158]. Hypertension, diabetes mellitus, and obesity were common comorbidities in patients with COVID-19, associated with high mortality rates [1, 10, 13, 159–161] and a greater number of long-term post-COVID symptoms [162, 163]. Even in the post-acute period, HF was associated with increased risk of mortality [82]. Despite initial theoretical concerns regarding increased levels of ACE2 and the risk of acute COVID-19 with the use of renin–angiotensin–aldosterone system (RAAS) inhibitors, treatment with angiotensin-converting enzyme inhibitors/angiotensin receptor blockers (ACEi/ARB) should be continued by patients with CVD, including treatment for HF and hypertension management [164, 165]. None of these agents affect susceptibility to SARS-CoV-2 infection or increase the risk of severe or fatal illness [166–171]. They have been shown to be safe and should be continued in patients with stable cardiovascular disease [172, 173]. On the contrary, withdrawal from guideline-directed medical therapy was associated with higher mortality in the acute to post-acute phase [174]. Therefore, discontinuation of ACE inhibitors or ARBs is not recommended [175, 176], and indiscriminate withdrawal of these drugs could harm high-risk patients [177].
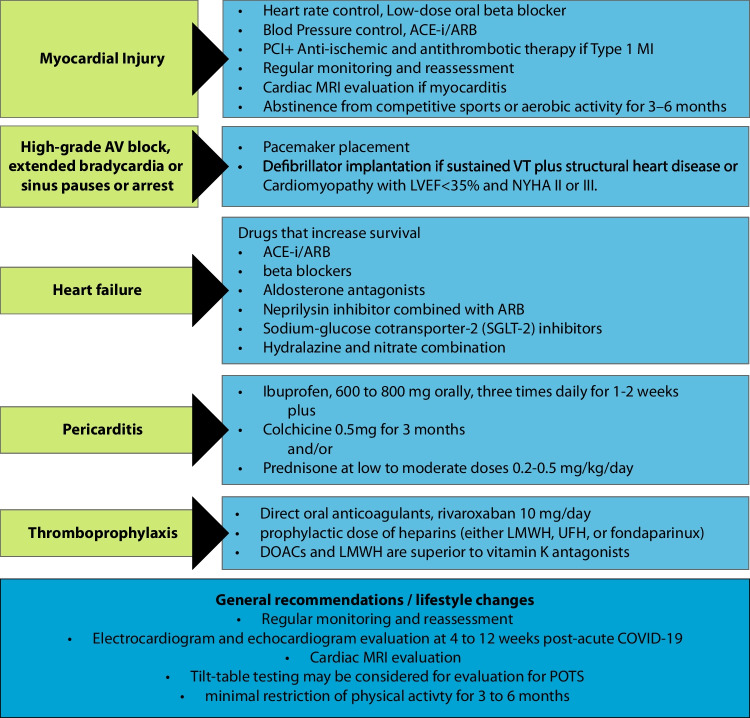
In patients who are diagnosed with myocardial injury, if necessary, heart rate should be controlled, usually by low-dose oral beta blockers and blood pressure lowering using ACEi/ARB (Fig. 3). Emphasis should be given to the management of cardiac arrhythmias such as atrial fibrillation. Low-dose oral beta blockers metoprolol or propranolol for heart rate control may be considered; low-dose (20 mg) propranolol was found to significantly attenuate tachycardia and improve symptoms in POTS, while a higher dose did not further improve, and could worsen, symptoms [178]. In addition, tilt-table testing may be considered for evaluation for POTS. Caution should be used for anti-arrhythmic agents such as amiodarone in patients with decreased pulmonary function and/or fibrotic lung disease after COVID-19 [76], since pulmonary toxicity is among the most serious adverse effects of amiodarone [179]. Outpatient follow-up is also indicated in patients who develop high-grade AV block, sinus node dysfunction, junctional bradycardia, sinus pauses, or sinus arrest during COVID-19, as these have been suggested to be poor prognostic signs [180, 181]. These patients have been managed with standard-of-care pacemaker placement [182–184], while implantable defibrillator should be considered in patients with structural heart disease, with spontaneous sustained ventricular tachycardia whether hemodynamically stable or not, ischemic or non-ischemic cardiomyopathy with LVEF less than 35% and New York Heart Association (NYHA) functional class II or III (Fig. 3). In addition, the choice of drug for patients with pericarditis should be based on the patient medical history. The nonsteroidal anti-inflammatory drug (NSAID) ibuprofen at a dose of 600–800 mg orally, three times daily for 1–2 weeks [94, 185], plus colchicine recommended at low, weight-adjusted doses for a total of 3 months is recommended to improve the response to medical therapy and to prevent recurrence [94, 186]. Corticosteroids should be avoided because they promote recurrence [187]. However, if they simply cannot be avoided and need to be used as an alternative in patients where NSAIDs and colchicine are contraindicated or added to NSAIDs and colchicine as triple therapy for patients with an incomplete response, prednisone is recommended at a low to moderate dose of 0.2–0.5 mg/kg/day or equivalent until resolution of symptoms and normalization of C-reactive protein, and then tapering should be considered (Fig. 3) [188]. Gastroprotection should be provided.
Fig. 3.
Post-acute COVID-19 management and general recommendations/lifestyle changes for cardiovascular manifestations of SARS-CoV-2 infection. PCI: percutaneous coronary intervention; ACE-i/ARB: angiotensin-converting enzyme inhibitors/angiotensin receptor blockers; MI: myocardial infarction; MRI: magnetic resonance imaging; VT: ventricular tachycardia; LVEF: left ventricular ejection fraction; NYHA: New York Heart Association classification; LMWH: low-molecular-weight heparin; DOACs: direct oral anticoagulants; UFH: unfractionated heparin; POTS: postural orthostatic tachycardia syndrome
Given the high rates of thrombotic complications in COVID-19 [189] and the high risk for thrombotic events after discharge, thromboprophylaxis should be considered; however, the indications and duration of anticoagulation therapy are unclear. For patients at high risk who are discharged after hospitalization due to COVID-19, thromboprophylaxis with direct oral anticoagulants (DOACs) should be considered for at least 35 days. In addition, patients with diabetes have an increased platelet reactivity and turnover, resulting in a pro-thrombotic state. Aspirin is recommended in patients with diabetes and CVD (recommendation IIb, level of evidence A). Rivaroxaban at a dose of 10 mg/day for 35 days improved clinical outcomes compared with no extended thromboprophylaxis [190]. As reported in a systematic review and meta-analysis, both prophylactic and full-dose heparins (low-molecular-weight heparin [LMWH], unfractionated heparin [UFH], or fondaparinux) in COVID-19 patients reduced the risk of all-cause mortality (HR = 0.63 [95% CI: 0.57–0.69] and 0.56 [95% CI: 0.47–0.66], respectively). Nevertheless, the full dose was associated with a higher risk of major bleeding (OR = 2.01, 95% CI: 1.14–3.53) compared to prophylactic dose, although there was no difference in overall mortality between the two regimens [191]. DOACs and LMWH are preferred over vitamin K antagonists, since they are patient-friendly, do not require frequent monitoring of therapeutic levels, and have low drug–drug interactions [7, 192]. However, in renal insufficiency, warfarin is preferred over DOACs, with monitoring of the international normalized ratio (INR). The Food and Drug Administration (FDA) recommends the use of rivaroxaban (10 mg daily) for 31–39 days and betrixaban (160 mg on the first day followed by 80 mg once a day) for 35–42 days [193].
Concerning general recommendations, for patients with CVD or who develop cardiac disease during acute infection, regular monitoring and reassessment are recommended [76]. ECG and echocardiographic evaluation at 4 to 12 weeks may be considered for patients during post-acute COVID-19 [9, 194]. Moreover, Holter monitoring should be used as indicated by symptoms, but it may also be reasonable to consider its use in asymptomatic patients, given the risk of a variety of arrhythmias in patients with COVID-19 [76]. Current evidence does not support the routine utilization of advanced cardiac imaging, and this should be considered on a case-by-case basis [153] unless there are abnormal findings on ECG or transthoracic echocardiogram, in which case additional investigation including stress testing or CMR should be performed [76]. In addition, intense, vigorous exercise, weightlifting, and competitive sports or aerobic activity should be avoided for 3–6 months until resolution of myocardial inflammation by CMR, or troponin normalization is recommended for patients with myocarditis due to COVID-19 (Fig. 3) [9, 195].
Conclusion
SARS-CoV-2 infection can degrade a person’s quality of life over the long term and increase the risk of cardiovascular complications regardless of age, sex, race, or cardiovascular morbidities [54]. It is now clear that patients with COVID-19 need to continue follow-up and care after hospital discharge using a multifaceted approach. Prioritization should be considered for groups at high risk, including patients who experienced severe COVID-19 illness, those with multisystem inflammatory syndrome during or after COVID-19 illness, older patients (>65 years) and those with underlying comorbidities, respiratory disease, obesity, diabetes, hypertension, chronic cardiovascular disease, chronic kidney disease, post-organ transplant, or active cancer, and people who are not yet vaccinated against COVID-19. Although the risk of SARS-CoV-2 infection or severe disease and/or death and the risk and duration of long COVID-19 symptoms have been reduced in populations with high vaccine uptake [196, 197], there are still individuals who are not yet vaccinated, and these groups remain at great risk. We would like to draw attention to patients receiving ACEi/ARBs as a treatment regimen for HF: under no circumstances should these agents be withdrawn. All hospitalized COVID-19 patients should receive thromboprophylaxis, while decisions regarding post-discharge prophylactic anticoagulation should be individualized. Finally, we suggest that optimal screening guidelines for patients after recovery from COVID-19 should be determined to prevent cardiovascular complications in a vast majority of the population. The careful documentation, investigation, and management of symptoms, and follow-up for cardiovascular complications developing during acute illness, are important.
Author Contributions
Dr. Kole and Dr. Stefanou contributed equally and should be considered co-first authors.
Conceptualization: CK, KT. Data collection and interpreting the relevant literature: CK, ES, NK, DS. Validation: CK, ES, NK. Writing—original draft preparation: CK, ES. Writing—review and editing: CK, KT. Figures 1 and 2: CK. Supervision: KT.
Funding
The authors have no relevant financial or non-financial interests to disclose.
Data Availability
This is a review article. No data and material were used for this article.
Code Availability
No software application or custom code was used in this article.
Declarations
Ethics Approval
This is a review article. No ethics approval is required.
Consent to Participate
This is a review article. No consent is required.
Consent to Publish
This is a review article. No consent is required.
Conflicts of Interest/Competing Interests
Christo Kole declares that he has no conflict of interest. Εleni Stefanou declares that she has no conflict of interest. Nikolaos Karvelas declares that he has no conflict of interest. Dimitrios Schizas declares that he has no conflict of interest. Konstantinos P. Toutouzas declares that he has no conflict of interest. The authors have no competing interests to declare that are relevant to the content of this article. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript. The authors have no financial or proprietary interests in any material discussed in this article.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Christo Kole and Εleni Stefanou contributed equally to this work.
Contributor Information
Christo Kole, Email: christo.kole@gmail.com.
Εleni Stefanou, Email: elstefanou@hotmail.com.
Nikolaos Karvelas, Email: nickkarvel@gmail.com.
Dimitrios Schizas, Email: schizasad@gmail.com.
Konstantinos P. Toutouzas, Email: ktoutouz@gmail.com
References
- 1.Wang D, Hu B, Hu C, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu F, Zhao S, Yu B, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579(7798):265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization WH. WHO Coronavirus (COVID-19) Dashboard. 2023. https://covid19.who.int/. Accessed 2 Feb 2023.
- 5.Henry BM, Lippi G. Poor survival with extracorporeal membrane oxygenation in acute respiratory distress syndrome (ARDS) due to coronavirus disease 2019 (COVID-19): Pooled analysis of early reports. J Crit Care. 2020;58:27–28. doi: 10.1016/j.jcrc.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tay MZ, Poh CM, Renia L, MacAry PA, Ng LFP. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. 2020;20(6):363–374. doi: 10.1038/s41577-020-0311-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bikdeli B, Madhavan MV, Jimenez D, et al. COVID-19 and Thrombotic or Thromboembolic Disease: Implications for Prevention, Antithrombotic Therapy, and Follow-Up: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020;75(23):2950–2973. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shah W, Hillman T, Playford ED, Hishmeh L. Managing the long term effects of covid-19: summary of NICE, SIGN, and RCGP rapid guideline. BMJ. 2021;372:n136. doi: 10.1136/bmj.n136. [DOI] [PubMed] [Google Scholar]
- 9.Hendren NS, Drazner MH, Bozkurt B, Cooper LT., Jr Description and Proposed Management of the Acute COVID-19 Cardiovascular Syndrome. Circulation. 2020;141(23):1903–1914. doi: 10.1161/CIRCULATIONAHA.120.047349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Petrilli CM, Jones SA, Yang J, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020;369:m1966. doi: 10.1136/bmj.m1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dhakal BP, Sweitzer NK, Indik JH, Acharya D, William P. SARS-CoV-2 Infection and Cardiovascular Disease: COVID-19 Heart. Heart Lung Circ. 2020;29(7):973–987. doi: 10.1016/j.hlc.2020.05.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Richardson S, Hirsch JS, Narasimhan M, et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Giacomelli A, Pezzati L, Conti F, et al. Self-reported Olfactory and Taste Disorders in Patients With Severe Acute Respiratory Coronavirus 2 Infection: A Cross-sectional Study. Clin Infect Dis. 2020;71(15):889–890. doi: 10.1093/cid/ciaa330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang L, Xie X, Tu Z, et al. The signal pathways and treatment of cytokine storm in COVID-19. Signal Transduct Target Ther. 2021;6(1):255. doi: 10.1038/s41392-021-00679-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carfi A, Bernabei R, Landi F, Gemelli Against C-P-ACSG. Persistent Symptoms in Patients After Acute COVID-19. JAMA. 2020;324(6):603–605. doi: 10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carvalho-Schneider C, Laurent E, Lemaignen A, et al. Follow-up of adults with noncritical COVID-19 two months after symptom onset. Clin Microbiol Infect. 2021;27(2):258–263. doi: 10.1016/j.cmi.2020.09.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu K, Fang YY, Deng Y, et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin Med J (Engl) 2020;133(9):1025–1031. doi: 10.1097/CM9.0000000000000744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Task Force for the management of C-otESoC. Baigent C, Windecker S, et al. European Society of Cardiology guidance for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic: part 1-epidemiology, pathophysiology, and diagnosis. Cardiovasc Res. 2022;118(6):1385–1412. doi: 10.1093/cvr/cvab342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ranard LS, Fried JA, Abdalla M, et al. Approach to Acute Cardiovascular Complications in COVID-19 Infection. Circ Heart Fail. 2020;13(7):e007220. doi: 10.1161/CIRCHEARTFAILURE.120.007220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shi S, Qin M, Cai Y, et al. Characteristics and clinical significance of myocardial injury in patients with severe coronavirus disease 2019. Eur Heart J. 2020;41(22):2070–2079. doi: 10.1093/eurheartj/ehaa408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bangalore S, Sharma A, Slotwiner A, et al. ST-Segment Elevation in Patients with Covid-19 - A Case Series. N Engl J Med. 2020;382(25):2478–2480. doi: 10.1056/NEJMc2009020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guan WJ, Ni ZY, Hu Y, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Szekely Y, Lichter Y, Taieb P, et al. Spectrum of cardiac manifestations in COVID-19: a systematic echocardiographic study. Circulation. 2020;142(4):342–353. doi: 10.1161/CIRCULATIONAHA.120.047971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18(4):844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. The Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ferrante G, Fazzari F, Cozzi O, et al. Risk factors for myocardial injury and death in patients with COVID-19: insights from a cohort study with chest computed tomography. Cardiovasc Res. 2020;116(14):2239–2246. doi: 10.1093/cvr/cvaa193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schott JP, Mertens AN, Bloomingdale R, et al. Transthoracic echocardiographic findings in patients admitted with SARS-CoV-2 infection. Echocardiography. 2020;37(10):1551–1556. doi: 10.1111/echo.14835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guo T, Fan Y, Chen M, et al. Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19) JAMA Cardiol. 2020;5(7):811–818. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Inciardi RM, Lupi L, Zaccone G, et al. Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19) JAMA Cardiol. 2020;5(7):819–824. doi: 10.1001/jamacardio.2020.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van den Heuvel FMA, Vos JL, Koop Y, et al. Cardiac function in relation to myocardial injury in hospitalised patients with COVID-19. Neth Heart J. 2020;28(7-8):410–417. doi: 10.1007/s12471-020-01458-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vasudev R, Guragai N, Habib H, et al. The utility of bedside echocardiography in critically ill COVID-19 patients: Early observational findings from three Northern New Jersey hospitals. Echocardiography. 2020;37(9):1362–1365. doi: 10.1111/echo.14825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.D'Andrea A, Scarafile R, Riegler L, et al. Right Ventricular Function and Pulmonary Pressures as Independent Predictors of Survival in Patients With COVID-19 Pneumonia. JACC Cardiovasc Imaging. 2020;13(11):2467–2468. doi: 10.1016/j.jcmg.2020.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pagnesi M, Baldetti L, Beneduce A, et al. Pulmonary hypertension and right ventricular involvement in hospitalised patients with COVID-19. Heart. 2020;106(17):1324–1331. doi: 10.1136/heartjnl-2020-317355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rath D, Petersen-Uribe A, Avdiu A, et al. Impaired cardiac function is associated with mortality in patients with acute COVID-19 infection. Clin Res Cardiol. 2020;109(12):1491–1499. doi: 10.1007/s00392-020-01683-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ahmad MS, Shaik RA, Ahmad RK, et al. "LONG COVID": an insight. Eur Rev Med Pharmacol Sci. 2021;25(17):5561–5577. doi: 10.26355/eurrev_202109_26669. [DOI] [PubMed] [Google Scholar]
- 38.Visco V, Vitale C, Rispoli A, et al. Post-COVID-19 Syndrome: involvement and interactions between respiratory, cardiovascular and nervous systems. J Clin Med. 2022;11(3). [DOI] [PMC free article] [PubMed]
- 39.Huang C, Huang L, Wang Y, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397(10270):220–232. doi: 10.1016/S0140-6736(20)32656-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhao YH, Zhao L, Yang XC, Wang P. Cardiovascular complications of SARS-CoV-2 infection (COVID-19): a systematic review and meta-analysis. Rev Cardiovasc Med. 2021;22(1):159–165. doi: 10.31083/j.rcm.2021.01.238. [DOI] [PubMed] [Google Scholar]
- 41.Sahranavard M, Akhavan Rezayat A, Zamiri Bidary M, et al. Cardiac Complications in COVID-19: A Systematic Review and Meta-analysis. Arch Iran Med. 2021;24(2):152–163. doi: 10.34172/aim.2021.24. [DOI] [PubMed] [Google Scholar]
- 42.Del Prete A, Conway F, Della Rocca DG, et al. COVID-19, Acute Myocardial Injury, and Infarction. Card Electrophysiol Clin. 2022;14(1):29–39. doi: 10.1016/j.ccep.2021.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shi S, Qin M, Shen B, et al. Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5(7):802–810. doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lombardi CM, Carubelli V, Iorio A, et al. Association of Troponin Levels With Mortality in Italian Patients Hospitalized With Coronavirus Disease 2019: Results of a Multicenter Study. JAMA Cardiol. 2020;5(11):1274–1280. doi: 10.1001/jamacardio.2020.3538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Habets MAW, Sturkenboom HN, Tio RA, et al. How often and to what extent do admitted COVID-19 patients have signs of cardiac injury? Neth Heart J. 2021;29(Suppl 1):5–12. doi: 10.1007/s12471-021-01571-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Peretto G, Sala S, Caforio ALP. Acute myocardial injury, MINOCA, or myocarditis? Improving characterization of coronavirus-associated myocardial involvement. Eur Heart J. 2020;41(22):2124–2125. doi: 10.1093/eurheartj/ehaa396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pinto DS. COVID-19: Myocardial infarction and other coronary artery disease issues. UpToDate. 2022. https://www.uptodate.com/contents/covid-19-myocardial-infarction-and-other-coronary-artery-disease-issues. Accessed 24 Nov 2021.
- 48.Puntmann VO, Carerj ML, Wieters I, et al. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19) JAMA Cardiol. 2020;5(11):1265–1273. doi: 10.1001/jamacardio.2020.3557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Deng Q, Hu B, Zhang Y, et al. Suspected myocardial injury in patients with COVID-19: Evidence from front-line clinical observation in Wuhan, China. Int J Cardiol. 2020;311:116–121. doi: 10.1016/j.ijcard.2020.03.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.De Lorenzo A, Kasal DA, Tura BR, Lamas CC, Rey HC. Acute cardiac injury in patients with COVID-19. Am J Cardiovasc Dis. 2020;10(2):28–33. [PMC free article] [PubMed] [Google Scholar]
- 51.Zou F, Qian Z, Wang Y, Zhao Y, Bai J. Cardiac Injury and COVID-19: A Systematic Review and Meta-analysis. CJC Open. 2020;2(5):386–394. doi: 10.1016/j.cjco.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gleber R, Vilke GM, Castillo EM, et al. Trends in emergency physician opioid prescribing practices during the United States opioid crisis. Am J Emerg Med. 2020;38(4):735–740. doi: 10.1016/j.ajem.2019.06.011. [DOI] [PubMed] [Google Scholar]
- 53.Wang W, Wang C-Y, Wang S-I, Wei JC-C. Long-term cardiovascular outcomes in COVID-19 survivors among non-vaccinated population: A retrospective cohort study from the TriNetX US collaborative networks. eClinicalMedicine. 2022:53. 10.1016/j.eclinm.2022.101619. [DOI] [PMC free article] [PubMed]
- 54.Xie Y, Xu E, Bowe B, Al-Aly Z. Long-term cardiovascular outcomes of COVID-19. Nature Medicine. 2022;28,3:583–590. 10.1038/s41591-022-01689-3. [DOI] [PMC free article] [PubMed]
- 55.Mulia EPB, Maghfirah I, Rachmi DA, Julario R. Atrial arrhythmia and its association with COVID-19 outcome: a pooled analysis. Diagnosis (Berl) 2021;8(4):532–535. doi: 10.1515/dx-2020-0155. [DOI] [PubMed] [Google Scholar]
- 56.Li X, Pan X, Li Y, et al. Cardiac injury associated with severe disease or ICU admission and death in hospitalized patients with COVID-19: a meta-analysis and systematic review. Critical Care. 2020;24(1):468. doi: 10.1186/s13054-020-03183-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang Y, Wang Z, Tse G, et al. Cardiac arrhythmias in patients with COVID-19. J Arrhythm. 2020;36(5):827–836. doi: 10.1002/joa3.12405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Berg DD, Alviar CL, Bhatt AS, et al. Epidemiology of Acute Heart Failure in Critically Ill Patients With COVID-19: An Analysis From the Critical Care Cardiology Trials Network. J Card Fail. 2022;28(4):675–681. doi: 10.1016/j.cardfail.2021.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Oktaviono YH, Mulia EPB, Luke K, et al. Right ventricular dysfunction and pulmonary hypertension in COVID-19: a meta-analysis of prevalence and its association with clinical outcome. Archives of Medical Science : AMS. 2021;18,5:1169–1180. 10.5114/aoms/136342. [DOI] [PMC free article] [PubMed]
- 60.Gong X, Yuan B, Yuan Y. Incidence and prognostic value of pulmonary embolism in COVID-19: A systematic review and meta-analysis. PLoS One. 2022;17(3):e0263580. doi: 10.1371/journal.pone.0263580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zuin M, Barco S, Giannakoulas G, et al. Risk of venous thromboembolic events after COVID-19 infection: a systematic review and meta-analysis. J Thromb Thrombolysis. 2023;55(3):490–498. doi: 10.1007/s11239-022-02766-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ghantous E, Szekely Y, Lichter Y, et al. Pericardial Involvement in Patients Hospitalized With COVID-19: Prevalence, Associates, and Clinical Implications. J Am Heart Assoc. 2022;11(7):e024363. doi: 10.1161/JAHA.121.024363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dweck MR, Bularga A, Hahn RT, et al. Global evaluation of echocardiography in patients with COVID-19. Eur Heart J-Cardiovasc Imaging. 2020;21(9):949–958. doi: 10.1093/ehjci/jeaa178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Caforio AL, Pankuweit S, Arbustini E, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2013;34(33):2636–2648. doi: 10.1093/eurheartj/eht210. [DOI] [PubMed] [Google Scholar]
- 65.Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tavazzi G, Pellegrini C, Maurelli M, et al. Myocardial localization of coronavirus in COVID-19 cardiogenic shock. Eur J Heart Fail. 2020;22(5):911–915. doi: 10.1002/ejhf.1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Halushka MK, Vander Heide RS. Myocarditis is rare in COVID-19 autopsies: cardiovascular findings across 277 postmortem examinations. Cardiovasc Pathol. 2021;50:107300. doi: 10.1016/j.carpath.2020.107300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wichmann D, Sperhake JP, Lutgehetmann M, et al. Autopsy Findings and Venous Thromboembolism in Patients With COVID-19: A Prospective Cohort Study. Ann Intern Med. 2020;173(4):268–277. doi: 10.7326/M20-2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lindner D, Fitzek A, Brauninger H, et al. Association of Cardiac Infection With SARS-CoV-2 in Confirmed COVID-19 Autopsy Cases. JAMA Cardiol. 2020;5(11):1281–1285. doi: 10.1001/jamacardio.2020.3551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chippa V, Aleem A, Anjum F. Post Acute Coronavirus (COVID-19) Syndrome., StatPearls [Internet]. 2022. https://www.ncbi.nlm.nih.gov/books/NBK570608/. Accessed Updated 2022 Jun 19.
- 71.Sandoval Y, Januzzi JL, Jr, Jaffe AS. Cardiac Troponin for Assessment of Myocardial Injury in COVID-19: JACC Review Topic of the Week. J Am Coll Cardiol. 2020;76(10):1244–1258. doi: 10.1016/j.jacc.2020.06.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chapman AR, Bularga A, Mills NL. High-Sensitivity Cardiac Troponin Can Be an Ally in the Fight Against COVID-19. Circulation. 2020;141(22):1733–1735. doi: 10.1161/CIRCULATIONAHA.120.047008. [DOI] [PubMed] [Google Scholar]
- 73.Kochi AN, Tagliari AP, Forleo GB, Fassini GM, Tondo C. Cardiac and arrhythmic complications in patients with COVID-19. J Cardiovasc Electrophysiol. 2020;31(5):1003–1008. doi: 10.1111/jce.14479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bhatla A, Mayer MM, Adusumalli S, et al. COVID-19 and cardiac arrhythmias. Heart Rhythm. 2020;17(9):1439–1444. doi: 10.1016/j.hrthm.2020.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Si D, Du B, Ni L, et al. Death, discharge and arrhythmias among patients with COVID-19 and cardiac injury. CMAJ. 2020;192(28):E791–E7E8. doi: 10.1503/cmaj.200879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Desai AD, Boursiquot BC, Melki L, Wan EY. Management of Arrhythmias Associated with COVID-19. Curr Cardiol Rep. 2020;23(1):2. doi: 10.1007/s11886-020-01434-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zeng L, Wang S, Cai J, et al. Clinical characteristics of COVID-19 with cardiac injury: a systematic review and meta-analysis. Epidemiol Infect. 2020;148:e266. doi: 10.1017/S0950268820002587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.John KJ, Mishra AK, Ramasamy C, et al. Heart failure in COVID-19 patients: Critical care experience. World J Virol. 2022;11(1):1–19. doi: 10.5501/wjv.v11.i1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Mahmoud-Elsayed HM, Moody WE, Bradlow WM, et al. Echocardiographic Findings in Patients With COVID-19 Pneumonia. Can J Cardiol. 2020;36(8):1203–1207. doi: 10.1016/j.cjca.2020.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Corica B, Marra AM, Basili S, et al. Prevalence of right ventricular dysfunction and impact on all-cause death in hospitalized patients with COVID-19: a systematic review and meta-analysis. Scientific Reports. 2021;11(1):17774. doi: 10.1038/s41598-021-96955-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Li Y, Li H, Zhu S, et al. Prognostic Value of Right Ventricular Longitudinal Strain in Patients With COVID-19. JACC Cardiovasc Imaging. 2020;13(11):2287–2299. doi: 10.1016/j.jcmg.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Alvarez-Garcia J, Lee S, Gupta A, et al. Prognostic Impact of Prior Heart Failure in Patients Hospitalized With COVID-19. J Am Coll Cardiol. 2020;76(20):2334–2348. doi: 10.1016/j.jacc.2020.09.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wu T, Zuo Z, Yang D, et al. Venous thromboembolic events in patients with COVID-19: a systematic review and meta-analysis. Age Ageing. 2021;50(2):284–293. doi: 10.1093/ageing/afaa259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Katsanos AH, Palaiodimou L, Zand R, et al. The Impact of SARS-CoV-2 on Stroke Epidemiology and Care: A Meta-Analysis. Ann Neurol. 2021;89(2):380–388. doi: 10.1002/ana.25967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wang M, Zhang H, He Y, et al. Association Between Ischemic Stroke and COVID-19 in China: A Population-Based Retrospective Study. Front Med (Lausanne) 2021;8:792487. doi: 10.3389/fmed.2021.792487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Luo W, Liu X, Bao K, Huang C. Ischemic stroke associated with COVID-19: a systematic review and meta-analysis. J Neurol. 2022;269(4):1731–1740. doi: 10.1007/s00415-021-10837-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Klok FA, Kruip M, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Dmytriw AA, Dibas M, Schirmer CM, et al. Age and Acute Ischemic Stroke Outcome in North American Patients With COVID-19. J Am Heart Assoc. 2021;10(14):e021046. doi: 10.1161/JAHA.121.021046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kollias A, Kyriakoulis KG, Lagou S, et al. Venous thromboembolism in COVID-19: A systematic review and meta-analysis. Vasc Med. 2021;26(4):415–425. doi: 10.1177/1358863X21995566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Amir M, Djaharuddin I, Sudharsono A, Ramadany S. COVID-19 concomitant with infective endocarditis: A case report and review of management. Int J Infect Dis. 2020;98:109–112. doi: 10.1016/j.ijid.2020.06.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kumar R, Kumar J, Daly C, Edroos SA. Acute pericarditis as a primary presentation of COVID-19. BMJ Case Reports. 2020;13(8):e237617. doi: 10.1136/bcr-2020-237617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hua A, O'Gallagher K, Sado D, Byrne J. Life-threatening cardiac tamponade complicating myo-pericarditis in COVID-19. Eur Heart J. 2020;41(22):2130. doi: 10.1093/eurheartj/ehaa253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Li K, Wu J, Wu F, et al. The Clinical and Chest CT Features Associated With Severe and Critical COVID-19 Pneumonia. Invest Radiol. 2020;55(6):327–331. doi: 10.1097/RLI.0000000000000672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Diaz-Arocutipa C, Saucedo-Chinchay J, Imazio M. Pericarditis in patients with COVID-19: a systematic review. J Cardiovasc Med. 2021;22(9):693–700. doi: 10.2459/JCM.0000000000001202. [DOI] [PubMed] [Google Scholar]
- 95.Shah RM, Shah M, Shah S, Li A, Jauhar S. Takotsubo Syndrome and COVID-19: Associations and Implications. Curr Probl Cardiol. 2021;46(3):100763. doi: 10.1016/j.cpcardiol.2020.100763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Chung MK, Zidar DA, Bristow MR, et al. COVID-19 and Cardiovascular Disease: From Bench to Bedside. Circ Res. 2021;128(8):1214–1236. doi: 10.1161/CIRCRESAHA.121.317997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Theetha Kariyanna P, Sabih A, Sutarjono B, et al. A Systematic Review of COVID-19 and Pericarditis. Cureus. 2022;14(8):e27948. doi: 10.7759/cureus.27948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zvonarev V. Takotsubo Cardiomyopathy: Medical and Psychiatric Aspects. Role of Psychotropic Medications in the Treatment of Adults with "Broken Heart" Syndrome. Cureus. 2019;11(7):e5177. doi: 10.7759/cureus.5177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Jabri A, Kalra A, Kumar A, et al. Incidence of Stress Cardiomyopathy During the Coronavirus Disease 2019 Pandemic. JAMA Netw Open. 2020;3(7):e2014780. doi: 10.1001/jamanetworkopen.2020.14780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Virani SS, Khan AN, Mendoza CE, Ferreira AC, de Marchena E. Takotsubo cardiomyopathy, or broken-heart syndrome. Tex Heart Inst J. 2007;34(1):76–79. [PMC free article] [PubMed] [Google Scholar]
- 101.Zorzi A, Baritussio A, ElMaghawry M, et al. Differential diagnosis at admission between Takotsubo cardiomyopathy and acute apical-anterior myocardial infarction in postmenopausal women. Eur Heart J Acute Cardiovasc Care. 2016;5(4):298–307. doi: 10.1177/2048872615585515. [DOI] [PubMed] [Google Scholar]
- 102.Izumo M, Akashi YJ. Role of echocardiography for takotsubo cardiomyopathy: clinical and prognostic implications. Cardiovasc Diagn Ther. 2018;8(1):90–100. doi: 10.21037/cdt.2017.07.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Dweck MR, Bularga A, Hahn RT, et al. Global evaluation of echocardiography in patients with COVID-19. Eur Heart J Cardiovasc Imaging. 2020;21(9):949–958. doi: 10.1093/ehjci/jeaa178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Giustino G, Croft LB, Oates CP, et al. Takotsubo Cardiomyopathy in COVID-19. J Am Coll Cardiol. 2020;76(5):628–629. doi: 10.1016/j.jacc.2020.05.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Citro R, Okura H, Ghadri JR, et al. Multimodality imaging in takotsubo syndrome: a joint consensus document of the European Association of Cardiovascular Imaging (EACVI) and the Japanese Society of Echocardiography (JSE) J Echocardiogr. 2020;18(4):199–224. doi: 10.1007/s12574-020-00480-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Cui J, Li F, Shi ZL. Origin and evolution of pathogenic coronaviruses. Nat Rev Microbiol. 2019;17(3):181–192. doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Lai MM, Cavanagh D. The molecular biology of coronaviruses. Adv Virus Res. 1997;48:1–100. doi: 10.1016/S0065-3527(08)60286-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Walls AC, Park YJ, Tortorici MA, et al. Structure, Function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell. 2020;181(2):281–92 e6. doi: 10.1016/j.cell.2020.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Cohen JB, Hanff TC, Bress AP, South AM. Relationship Between ACE2 and Other Components of the Renin-Angiotensin System. Curr Hypertens Rep. 2020;22(7):44. doi: 10.1007/s11906-020-01048-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Kuba K, Imai Y, Penninger JM. Angiotensin-converting enzyme 2 in lung diseases. Curr Opin Pharmacol. 2006;6(3):271–276. doi: 10.1016/j.coph.2006.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Hoffmann M, Kleine-Weber H, Schroeder S, et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell. 2020;181(2):271–80 e8. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Meng B, Abdullahi A, Ferreira I, et al. Altered TMPRSS2 usage by SARS-CoV-2 Omicron impacts infectivity and fusogenicity. Nature. 2022;603,7902:706–714. 10.1038/s41586-022-04474-x. [DOI] [PMC free article] [PubMed]
- 113.Baggen J, Vanstreels E, Jansen S, Daelemans D. Cellular host factors for SARS-CoV-2 infection. Nat Microbiol. 2021;6(10):1219–1232. doi: 10.1038/s41564-021-00958-0. [DOI] [PubMed] [Google Scholar]
- 114.Snijder EJ, van der Meer Y, Zevenhoven-Dobbe J, et al. Ultrastructure and origin of membrane vesicles associated with the severe acute respiratory syndrome coronavirus replication complex. J Virol. 2006;80(12):5927–5940. doi: 10.1128/JVI.02501-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wu HY, Brian DA. Subgenomic messenger RNA amplification in coronaviruses. Proc Natl Acad Sci U S A. 2010;107(27):12257–12262. doi: 10.1073/pnas.1000378107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Jia HP, Look DC, Shi L, et al. ACE2 receptor expression and severe acute respiratory syndrome coronavirus infection depend on differentiation of human airway epithelia. J Virol. 2005;79(23):14614–14621. doi: 10.1128/JVI.79.23.14614-14621.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Crackower MA, Sarao R, Oudit GY, et al. Angiotensin-converting enzyme 2 is an essential regulator of heart function. Nature. 2002;417(6891):822–828. doi: 10.1038/nature00786. [DOI] [PubMed] [Google Scholar]
- 118.Hamming I, Timens W, Bulthuis ML, et al. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203(2):631–637. doi: 10.1002/path.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Vabret N, Britton GJ, Gruber C, et al. Immunology of COVID-19: Current State of the Science. Immunity. 2020;52(6):910–941. doi: 10.1016/j.immuni.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Siripanthong B, Nazarian S, Muser D, et al. Recognizing COVID-19-related myocarditis: The possible pathophysiology and proposed guideline for diagnosis and management. Heart Rhythm. 2020;17(9):1463–1471. doi: 10.1016/j.hrthm.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Gustine JN, Jones D. Immunopathology of Hyperinflammation in COVID-19. Am J Pathol. 2021;191(1):4–17. doi: 10.1016/j.ajpath.2020.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Italia L, Tomasoni D, Bisegna S, et al. COVID-19 and Heart Failure: From Epidemiology During the Pandemic to Myocardial Injury, Myocarditis, and Heart Failure Sequelae. Front Cardiovasc Med. 2021;8:713560. doi: 10.3389/fcvm.2021.713560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Adeghate EA, Eid N, Singh J. Mechanisms of COVID-19-induced heart failure: a short review. Heart Fail Rev. 2021;26(2):363–369. doi: 10.1007/s10741-020-10037-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Deswal A, Petersen NJ, Feldman AM, et al. Cytokines and cytokine receptors in advanced heart failure: an analysis of the cytokine database from the Vesnarinone trial (VEST) Circulation. 2001;103(16):2055–2059. doi: 10.1161/01.CIR.103.16.2055. [DOI] [PubMed] [Google Scholar]
- 125.Van Tassell BW, Raleigh JM, Abbate A. Targeting interleukin-1 in heart failure and inflammatory heart disease. Curr Heart Fail Rep. 2015;12(1):33–41. doi: 10.1007/s11897-014-0231-7. [DOI] [PubMed] [Google Scholar]
- 126.Van Tassell BW, Toldo S, Mezzaroma E, Abbate A. Targeting interleukin-1 in heart disease. Circulation. 2013;128(17):1910–1923. doi: 10.1161/CIRCULATIONAHA.113.003199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Tatsumi T, Matoba S, Kawahara A, et al. Cytokine-induced nitric oxide production inhibits mitochondrial energy production and impairs contractile function in rat cardiac myocytes. J Am Coll Cardiol. 2000;35(5):1338–1346. doi: 10.1016/S0735-1097(00)00526-X. [DOI] [PubMed] [Google Scholar]
- 128.Buckley LF, Abbate A. Interleukin-1 blockade in cardiovascular diseases: a clinical update. Eur Heart J. 2018;39(22):2063–2069. doi: 10.1093/eurheartj/ehy128. [DOI] [PubMed] [Google Scholar]
- 129.Warner SJ, Libby P. Human vascular smooth muscle cells. Target for and source of tumor necrosis factor. J Immunol. 1989;142(1):100–109. doi: 10.4049/jimmunol.142.1.100. [DOI] [PubMed] [Google Scholar]
- 130.Shanmugam G, Narasimhan M, Sakthivel R, et al. A biphasic effect of TNF-alpha in regulation of the Keap1/Nrf2 pathway in cardiomyocytes. Redox Biol. 2016;9:77–89. doi: 10.1016/j.redox.2016.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Schumertl T, Lokau J, Rose-John S, Garbers C. Function and proteolytic generation of the soluble interleukin-6 receptor in health and disease. Biochim Biophys Acta Mol Cell Res. 2022;1869(1):119143. doi: 10.1016/j.bbamcr.2021.119143. [DOI] [PubMed] [Google Scholar]
- 132.Kang S, Tanaka T, Narazaki M, Kishimoto T. Targeting Interleukin-6 Signaling in Clinic. Immunity. 2019;50(4):1007–1023. doi: 10.1016/j.immuni.2019.03.026. [DOI] [PubMed] [Google Scholar]
- 133.Su JH, Luo MY, Liang N, et al. Interleukin-6: A Novel Target for Cardio-Cerebrovascular Diseases. Front Pharmacol. 2021;12:745061. doi: 10.3389/fphar.2021.745061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Lazzerini PE, Laghi-Pasini F, Boutjdir M, Capecchi PL. Cardioimmunology of arrhythmias: the role of autoimmune and inflammatory cardiac channelopathies. Nat Rev Immunol. 2019;19(1):63–64. doi: 10.1038/s41577-018-0098-z. [DOI] [PubMed] [Google Scholar]
- 135.Lazzerini PE, Laghi-Pasini F, Boutjdir M, Capecchi PL. Inflammatory cytokines and cardiac arrhythmias: the lesson from COVID-19. Nat Rev Immunol. 2022;22(5):270–272. doi: 10.1038/s41577-022-00714-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Guan H, Liu J, Ding J, et al. Arrhythmias in patients with coronavirus disease 2019 (COVID-19) in Wuhan, China: Incidences and implications. J Electrocardiol. 2021;65:96–101. doi: 10.1016/j.jelectrocard.2021.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Rubin GA, Desai AD, Chai Z, et al. Cardiac Corrected QT Interval Changes Among Patients Treated for COVID-19 Infection During the Early Phase of the Pandemic. JAMA Netw Open. 2021;4(4):e216842. doi: 10.1001/jamanetworkopen.2021.6842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Musikantow DR, Turagam MK, Sartori S, et al. Atrial Fibrillation in Patients Hospitalized With COVID-19: Incidence, Predictors, Outcomes, and Comparison to Influenza. JACC Clin Electrophysiol. 2021;7(9):1120–1130. doi: 10.1016/j.jacep.2021.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Liu PP, Blet A, Smyth D, Li H. The Science Underlying COVID-19: Implications for the Cardiovascular System. Circulation. 2020;142(1):68–78. doi: 10.1161/CIRCULATIONAHA.120.047549. [DOI] [PubMed] [Google Scholar]
- 140.Gubbi S, Nazari MA, Taieb D, Klubo-Gwiezdzinska J, Pacak K. Catecholamine physiology and its implications in patients with COVID-19. Lancet Diabetes Endocrinol. 2020;8(12):978–986. doi: 10.1016/S2213-8587(20)30342-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Agarwal AK, Garg R, Ritch A, Sarkar P. Postural orthostatic tachycardia syndrome. Postgrad Med J. 2007;83(981):478–480. doi: 10.1136/pgmj.2006.055046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Lau ST, Yu WC, Mok NS, et al. Tachycardia amongst subjects recovering from severe acute respiratory syndrome (SARS) Int J Cardiol. 2005;100(1):167–169. doi: 10.1016/j.ijcard.2004.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Bansal M. Cardiovascular disease and COVID-19. Diabetes Metab Syndr. 2020;14(3):247–250. doi: 10.1016/j.dsx.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Triposkiadis F, Xanthopoulos A, Butler J. Cardiovascular Aging and Heart Failure: JACC Review Topic of the Week. J Am Coll Cardiol. 2019;74(6):804–813. doi: 10.1016/j.jacc.2019.06.053. [DOI] [PubMed] [Google Scholar]
- 145.Garcia-Lucio J, Peinado VI, de Jover L, et al. Imbalance between endothelial damage and repair capacity in chronic obstructive pulmonary disease. PLoS One. 2018;13(4):e0195724. doi: 10.1371/journal.pone.0195724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.De Lorenzo A, Escobar S, Tibirica E. Systemic endothelial dysfunction: A common pathway for COVID-19, cardiovascular and metabolic diseases. Nutr Metab Cardiovasc Dis. 2020;30(8):1401–1402. doi: 10.1016/j.numecd.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Ackermann M, Verleden SE, Kuehnel M, et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19. N Engl J Med. 2020;383(2):120–128. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Levi M, van der Poll T. Coagulation and sepsis. Thromb Res. 2017;149:38–44. doi: 10.1016/j.thromres.2016.11.007. [DOI] [PubMed] [Google Scholar]
- 150.Libby P, Luscher T. COVID-19 is, in the end, an endothelial disease. Eur Heart J. 2020;41(32):3038–3044. doi: 10.1093/eurheartj/ehaa623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Gupta N, Zhao YY, Evans CE. The stimulation of thrombosis by hypoxia. Thromb Res. 2019;181:77–83. doi: 10.1016/j.thromres.2019.07.013. [DOI] [PubMed] [Google Scholar]
- 152.Farshidfar F, Koleini N, Ardehali H. Cardiovascular complications of COVID-19. JCI Insight. 2021;6. 10.1172/jci.insight.148980. [DOI] [PMC free article] [PubMed]
- 153.Nalbandian A, Sehgal K, Gupta A, et al. Post-acute COVID-19 syndrome. Nat Med. 2021;27(4):601–615. doi: 10.1038/s41591-021-01283-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Wu Q, Zhou L, Sun X, et al. Altered Lipid Metabolism in Recovered SARS Patients Twelve Years after Infection. Sci Rep. 2017;7(1):9110. doi: 10.1038/s41598-017-09536-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Nabavi N. Long covid: How to define it and how to manage it. BMJ. 2020;370:m3489. doi: 10.1136/bmj.m3489. [DOI] [PubMed] [Google Scholar]
- 156.CDC. Long COVID or Post-COVID Conditions. In: COVID-19 National Center for Immunization and Respiratory Diseases (NCIRD), Division of Viral Diseases, Centers for Disease Control and Prevention. 2022. https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html. Accessed 1 Sept 2022.
- 157.Drake TM, Riad AM, Fairfield CJ, et al. Characterisation of in-hospital complications associated with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol UK: a prospective, multicentre cohort study. Lancet. 2021;398(10296):223–237. doi: 10.1016/S0140-6736(21)00799-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Inciardi RM, Adamo M, Lupi L, et al. Characteristics and outcomes of patients hospitalized for COVID-19 and cardiac disease in Northern Italy. Eur Heart J. 2020;41(19):1821–1829. doi: 10.1093/eurheartj/ehaa388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 160.Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46(5):846–848. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Goyal P, Choi JJ, Pinheiro LC, et al. Clinical Characteristics of Covid-19 in New York City. N Engl J Med. 2020;382(24):2372–2374. doi: 10.1056/NEJMc2010419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Fernández-de-las-Peñas C, Torres-Macho J, Velasco-Arribas M, et al. Preexisting hypertension is associated with a greater number of long-term post-COVID symptoms and poor sleep quality: a case–control study. J Human Hypertens. 2022;36(6):582–584. doi: 10.1038/s41371-022-00660-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Raveendran AV, Misra A. Post COVID-19 Syndrome ("Long COVID") and Diabetes: Challenges in Diagnosis and Management. Diabetes Metab Syndr. 2021;15(5):102235. doi: 10.1016/j.dsx.2021.102235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Soler MJ, Barrios C, Oliva R, Batlle D. Pharmacologic modulation of ACE2 expression. Curr Hypertens Rep. 2008;10(5):410–414. doi: 10.1007/s11906-008-0076-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Prabhakaran D, Perel P, Roy A, et al. Management of Cardiovascular Disease Patients With Confirmed or Suspected COVID-19 in Limited Resource Settings. Glob Heart. 2020;15(1):44. doi: 10.5334/gh.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Mehta N, Kalra A, Nowacki AS, et al. Association of Use of Angiotensin-Converting Enzyme Inhibitors and Angiotensin II Receptor Blockers With Testing Positive for Coronavirus Disease 2019 (COVID-19) JAMA Cardiol. 2020;5(9):1020–1026. doi: 10.1001/jamacardio.2020.1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.de Abajo FJ, Rodríguez-Martín S, Lerma V, et al. Use of renin–angiotensin–aldosterone system inhibitors and risk of COVID-19 requiring admission to hospital: a case-population study. Lancet. 2020;395(10238):1705–1714. doi: 10.1016/S0140-6736(20)31030-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Mancia G, Rea F, Ludergnani M, Apolone G, Corrao G. Renin-Angiotensin-Aldosterone System Blockers and the Risk of Covid-19. N Engl J Med. 2020;382(25):2431–2440. doi: 10.1056/NEJMoa2006923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Fernandez-Ruiz I. RAAS inhibitors do not increase the risk of COVID-19. Nat Rev Cardiol. 2020;17(7):383. doi: 10.1038/s41569-020-0401-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Angeli F, Verdecchia P, Reboldi G. RAAS Inhibitors and Risk of Covid-19. N Engl J Med. 2020;383(20):1990–1991. doi: 10.1056/NEJMc2030446. [DOI] [PubMed] [Google Scholar]
- 171.Jarcho JA, Ingelfinger JR, Hamel MB, D'Agostino RB, Sr, Harrington DP. Inhibitors of the Renin-Angiotensin-Aldosterone System and Covid-19. N Engl J Med. 2020;382(25):2462–2464. doi: 10.1056/NEJMe2012924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Bozkurt B, Kovacs R, Harrington B. Joint HFSA/ACC/AHA Statement Addresses Concerns Re: Using RAAS Antagonists in COVID-19. J Card Fail. 2020;26(5):370. doi: 10.1016/j.cardfail.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Lopes RD, Macedo AVS, de Barros ESPGM, et al. Effect of Discontinuing vs Continuing Angiotensin-Converting Enzyme Inhibitors and Angiotensin II Receptor Blockers on Days Alive and Out of the Hospital in Patients Admitted With COVID-19: A Randomized Clinical Trial. JAMA. 2021;325(3):254–264. doi: 10.1001/jama.2020.25864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Rey JR, Caro-Codon J, Rosillo SO, et al. Heart failure in COVID-19 patients: prevalence, incidence and prognostic implications. Eur J Heart Fail. 2020;22(12):2205–2215. doi: 10.1002/ejhf.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Cardiology ACo. HFSA/ACC/AHA Statement Addresses Concerns Re: Using RAAS Antagonists in COVID-19. Am College Cardiol. 2020. https://www.acc.org/latest-in-cardiology/articles/2020/03/17/08/59/hfsa-acc-aha-statement-addresses-concerns-re-using-raas-antagonists-in-covid-19. Accessed 17 Mar 2020.
- 176.Cardiology ESo. Position Statement of the ESC Council on Hypertension on ACE-Inhibitors and Angiotensin Receptor Blockers. European Society of Cardiology. 2020. https://www.escardio.org/Councils/Council-on-Hypertension-(CHT)/News/position-statement-of-the-esc-council-on-hypertension-on-ace-inhibitors-and-ang (2020). Accessed 13 Mar 2020.
- 177.Vaduganathan M, Vardeny O, Michel T, et al. Renin-Angiotensin-Aldosterone System Inhibitors in Patients with Covid-19. N Engl J Med. 2020;382(17):1653–1659. doi: 10.1056/NEJMsr2005760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Raj SR, Black BK, Biaggioni I, et al. Propranolol decreases tachycardia and improves symptoms in the postural tachycardia syndrome: less is more. Circulation. 2009;120(9):725–734. doi: 10.1161/CIRCULATIONAHA.108.846501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Ruzieh M, Moroi MK, Aboujamous NM, et al. Meta-Analysis Comparing the Relative Risk of Adverse Events for Amiodarone Versus Placebo. Am J Cardiol. 2019;124(12):1889–1893. doi: 10.1016/j.amjcard.2019.09.008. [DOI] [PubMed] [Google Scholar]
- 180.Chinitz JS, Goyal R, Harding M, et al. Bradyarrhythmias in patients with COVID-19: Marker of poor prognosis? Pacing Clin Electrophysiol. 2020;43(10):1199–1204. doi: 10.1111/pace.14042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Azarkish M, Laleh Far V, Eslami M, Mollazadeh R. Transient complete heart block in a patient with critical COVID-19. Eur Heart J. 2020;41(22):2131. doi: 10.1093/eurheartj/ehaa307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Akhtar Z, Leung LW, Kontogiannis C, et al. Prevalence of bradyarrhythmias needing pacing in COVID-19. Pacing Clin Electrophysiol. 2021;44(8):1340–1346. doi: 10.1111/pace.14313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Al-Assaf O, Mirza M, Musa A. Atypical presentation of COVID-19 as subclinical myocarditis with persistent high-degree atrioventricular block treated with pacemaker implant. HeartRhythm Case Rep. 2020;6(11):884–887. doi: 10.1016/j.hrcr.2020.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Gupta MD, Qamar A, Mp G, et al. Bradyarrhythmias in patients with COVID-19: A case series. Indian Pacing Electrophysiol J. 2020;20(5):211–212. doi: 10.1016/j.ipej.2020.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Imazio M, Brucato A, Barbieri A, et al. Good prognosis for pericarditis with and without myocardial involvement: results from a multicenter, prospective cohort study. Circulation. 2013;128(1):42–49. doi: 10.1161/CIRCULATIONAHA.113.001531. [DOI] [PubMed] [Google Scholar]
- 186.Adler Y, Charron P, Imazio M, et al. 2015 ESC Guidelines for the diagnosis and management of pericardial diseases: The Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC) Endorsed by: The European Association for Cardio-Thoracic Surgery (EACTS) Eur Heart J. 2015;36(42):2921–2964. doi: 10.1093/eurheartj/ehv318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Imazio M, Brucato A, Cemin R, et al. A randomized trial of colchicine for acute pericarditis. N Engl J Med. 2013;369(16):1522–1528. doi: 10.1056/NEJMoa1208536. [DOI] [PubMed] [Google Scholar]
- 188.Imazio M, Brucato A, Trinchero R, Spodick D, Adler Y. Individualized therapy for pericarditis. Expert Rev Cardiovasc Ther. 2009;7(8):965–975. doi: 10.1586/erc.09.82. [DOI] [PubMed] [Google Scholar]
- 189.Gupta A, Madhavan MV, Sehgal K, et al. Extrapulmonary manifestations of COVID-19. Nat Med. 2020;26(7):1017–1032. doi: 10.1038/s41591-020-0968-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Ramacciotti E, Barile Agati L, Calderaro D, et al. Rivaroxaban versus no anticoagulation for post-discharge thromboprophylaxis after hospitalisation for COVID-19 (MICHELLE): an open-label, multicentre, randomised, controlled trial. Lancet. 2022;399(10319):50–59. doi: 10.1016/S0140-6736(21)02392-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Giossi R, Menichelli D, Pani A, et al. A Systematic Review and a Meta-Analysis Comparing Prophylactic and Therapeutic Low Molecular Weight Heparins for Mortality Reduction in 32,688 COVID-19 Patients. Front Pharmacol. 2021;12:698008. doi: 10.3389/fphar.2021.698008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Barnes GD, Burnett A, Allen A, et al. Thromboembolism and anticoagulant therapy during the COVID-19 pandemic: interim clinical guidance from the anticoagulation forum. J Thromb Thrombolysis. 2020;50(1):72–81. doi: 10.1007/s11239-020-02138-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Barkoudah E, Piazza G, Hecht TEH, et al. Extended Venous Thromboembolism Prophylaxis in Medically Ill Patients: An NATF Anticoagulation Action Initiative. Am J Med. 2020;133(Suppl 1):1–27. doi: 10.1016/j.amjmed.2019.12.001. [DOI] [PubMed] [Google Scholar]
- 194.George PM, Barratt SL, Condliffe R, et al. Respiratory follow-up of patients with COVID-19 pneumonia. Thorax. 2020;75(11):1009–1016. doi: 10.1136/thoraxjnl-2020-215314. [DOI] [PubMed] [Google Scholar]
- 195.Maron BJ, Udelson JE, Bonow RO, et al. Eligibility and Disqualification Recommendations for Competitive Athletes With Cardiovascular Abnormalities: Task Force 3: Hypertrophic Cardiomyopathy, Arrhythmogenic Right Ventricular Cardiomyopathy and Other Cardiomyopathies, and Myocarditis: A Scientific Statement From the American Heart Association and American College of Cardiology. J Am Coll Cardiol. 2015;66(21):2362–2371. doi: 10.1016/j.jacc.2015.09.035. [DOI] [PubMed] [Google Scholar]
- 196.Yek C, Warner S, Wiltz JL, et al. Risk Factors for Severe COVID-19 Outcomes Among Persons Aged >/=18 Years Who Completed a Primary COVID-19 Vaccination Series - 465 Health Care Facilities, United States, December 2020-October 2021. MMWR Morb Mortal Wkly Rep. 2022;71(1):19–25. doi: 10.15585/mmwr.mm7101a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Team. UHSAC-E. The effectiveness of vaccination against long covid: a rapid evidence briefing. 2022. https://www.icpcovid.com/sites/default/files/2022-02/Ep241-9UKHealthSecurityAgencyTheeffectivenessofvaccinationagainstlongCOVIDFeb2022.pdf. Accessed 25 Nov 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This is a review article. No data and material were used for this article.
No software application or custom code was used in this article.