Abstract
Background
This study examines whether living in US states with (1) restrictive reproductive rights and (2) restrictive abortion laws is associated with frequent mental health distress among women.
Methods
We operationalize reproductive rights using an overall state-level measure of reproductive rights as well as a state-level measure of restrictive abortion laws. We merged data from the 2018 Behavioral Risk Factor Surveillance System (BRFSS) with these state-level exposure variables and other state-level information. We used multilevel logistic regression to assess the relationship between these two measures and the likelihood of reporting 14 or more days of frequent mental health distress. We also tested whether associations differed across race, household income, education, and marital status.
Results
In the adjusted models, a standard deviation-unit increase in the reproductive rights score was significantly associated with decreased odds of reporting frequent mental health distress (OR = 0.95, 95% CI = 0.91, 0.99). Women in states with very hostile abortion restrictions had higher odds of frequent mental health distress. Associations between state-level abortion restrictions were larger among women 25–34 years old and women with a high school degree. For example, women aged 25–34 years residing in moderate (OR = 1.54, 95% CI = 1.14, 2.04), hostile (OR = 1.59, 95% CI = 1.15, 2.18), and very hostile (OR = 1.29, 95% CI = 1.02, 1.64) states were more likely to report frequent mental health distress than women living in states with less restrictive abortion policies.
Conclusion
We found the association between state-level restrictions on reproductive rights and abortion access and frequent mental health distress differed by age and socioeconomic status. These results suggest abortion rights restrictions may contribute to mental health inequities among women.
Keywords: Reproductive rights, Policy, Mental health, Women
Highlights
-
•
State-lelve measures of reproductive rights and abortion access are associated with frequent mental health distress among women in the US.
-
•
The strongest associations were noted among women aged 25-34 and women who were HS graduates.
-
•
Policies restricting reproductive rights may impact the mental health of women in the general US population.
1. Introduction
The United States Supreme Court overturned the 1973 Roe v. Wade decision in July 2022, removing the constitutional right to first-trimester abortion in the US. As a result, states now have the legal authority to implement partial or outright bans on abortions, leading to large geographical variability in reproductive care accessibility. Even before Roe was overturned, states varied significantly in policies about reproductive access and women's reproductive autonomy (Bentele et al., 2018).
State laws and regulations on reproduction may impede pregnant people's ability to obtain care and, in turn, affect health. An emerging body of research has found significant associations between living in restrictive reproductive states and poor maternal and infant health (Fuentes et al., 2016; Gerdts et al., 2016; Roberts et al., 2015). For example, babies born in states with restrictive reproductive rights have increased odds of low birthweight, pre-term birth, and higher mortality risk (Pabayo et al., 2020; Sudhinaraset et al., 2020; Wallace et al., 2017). In addition, states with restrictive reproductive rights have higher maternal mortality rates (Addante et al., 2021) and higher infant mortality rates (Krieger et al., 2015).
While this body of research on state-level reproductive restrictions on maternal and infant adverse outcomes is compelling, it is important to extend this research to examine the potential effects among all women. The adverse effects of living in states with restrictive reproductive rights may not be restricted to only pregnant people. The freedom to decide if, when, and how often to reproduce is necessary for women's optimal health (Ross & Solinger, 2017). Barriers to accessing comprehensive reproductive healthcare created by restrictive policies will likely increase psychosocial stress and contribute to frequent mental health distress, independent of a person's pregnancy status. For example, a World Health Organization (WHO) report summarized evidence that certain contraceptive methods may be associated with higher psychological distress leading them to argue that government policies that restricts women's contraceptive options may be an upstream determinant of mental health (WHO, 2009). Studies specifically focusing on abortion found that women who were denied an abortion had elevated anxiety and loss of self-esteem in the short-term (Biggs et al., 2017; Foster, 2020).
As a social determinant of health, laws and policies can potentially have positive or negative health effects (Mishori, 2019). The sexual and reproductive justice framework (SRJ) provides an overarching framework that can be applied to investigate the role of restrictive reproductive legislation in our society. SRJ emphasizes that women should have 1) the right to decide if and when to have a baby and the conditions under which to give birth, 2) the right to decide not to have a baby and the options for preventing or ending a pregnancy, and 3) the right to parent existing children with the necessary social supports in safe environments and healthy communities (Ross & Solinger, 2017). The SRJ framework acknowledges that legislation directly influences larger, contextual factors, which shape our sexual health options and, by extension, our overall health.
In addition, the SRJ framework recognizes reproductive policies as a broad category that extends beyond laws that limit abortion access. Restrictive reproductive policies that may potentially impact health include restrictions on sexual education and Medicaid coverage of family planning services because they affect larger issues of bodily autonomy. In addition, SRJ acknowledges that reproductive policies are often inequitable and disproportionately affect specific groups. Previous research has supported this SRJ presumption with research finding that restrictions on reproductive rights disproportionately burden low-income women and women of color (Goyal et al., 2020; Redd et al., 2021). In addition, women's knowledge of reproductive restrictions differed by marital status (Lara, Holt, Peña, & Grossman, 2015; Gallo et al., 2021) which suggests the effect of reproductive restrictions on behavior and health may also differ by marital status.
Using the SRJ framework to guide our research, this study uses state-level variation in policy to examine the following two questions: 1) Do women living in states with highly restricted reproductive rights have higher odds of frequent mental health distress compared with women living in states with less restricted reproductive rights, and 2) Do women living in states with prohibitive abortion policies have higher odds of frequent mental health distress compared with those in states that are less prohibitive. We hypothesize all women living in states with highly restrictive reproductive rights will have worse mental health distress compared with those living in less restrictive states. Similarly, we theorize all women living in states with greater prohibitive abortion policies will have worse mental health distress compared with those living in less restrictive states. State-level reproductive policies are likely to have a direct effect on the mental health of reproductive age women and indirect effects on the mental health of women who are not of reproductive age. We also examine whether associations differ by marital status, race/ethnicity, income, and education, as restrictions on reproductive rights are known to disproportionately burden women of color and those from lower socioeconomic backgrounds (Goyal et al., 2020; Redd et al., 2021).
2. Methods
We used data collected and made available by the Centers for Disease Control and Prevention (CDC) in the 2018 Behavioral Risk Factor Surveillance System (BRFSS) Study. BRFSS is a cross-sectional telephone survey administered annually since 1984. The study population includes non-institutionalized individuals aged 18 and older with access to a landline or cellular telephone. CDC aggregates the BRFSS surveys collected from all fifty states and the District of Columbia to produce an annual dataset. BRFSS participants answer questions about their self-reported health behaviors, health conditions, and use of preventive health services (CDC, 2019). BRFSS data are commonly used by local, state, and federal governments as well as academic researchers to assess the prevalence of health conditions and health care use in the US adult population. BRFSS data is publicly available online (CDC, 2019). We restricted our sample to participants whose biological sex was female from the 2018 BRFSS Study with complete information on the outcome and on individual-level potential confounders.
We merged our state-level exposure variables described below with the 2018 BRFSS survey data using the state of residence. All analyses were conducted on the newly created dataset that contains the merged survey data and the state-level exposure variables described in detail below.
2.1. Exposures
We operationalize reproductive access using an overall state-level measure of reproductive rights and a state-level measure specifically for access to abortion services. Our two state-level exposures of interest were an overall measure of reproductive rights and a more specific state-level measure of access to abortion services in 2017–2018. Both of these measures were created from data compiled by the Guttmacher Institute. Guttmacher Institute states that it, in turn, compiled these state indicators from data provided by the CDC, Guttmacher Institute, NARAL Pro-Choice America, and the National Center for Lesbian Rights. More information on these specific laws used to create our exposure measure is available on the Guttmacher Institute website (Guttmacher Institute, 2018). More details about both of these exposures are included in the Appendix Table A.
The overall measure of state-level reproductive rights score is a composite index based on nine indicators and developed by the Institute for Women's Policy Research (IWPR): mandatory parental consent or notification laws for minors receiving abortions; waiting periods for abortions; restrictions on public funding for abortions; percent of women living in counties with at least one abortion provider; pro-choice governors or legislators; Medicaid expansion or state Medicaid family planning eligibility expenses; coverage of infertility treatments; same-sex marriage or second-parent adoption for individuals in a same-sex relationship; and mandatory sex education (Hess et al., 2015). Each indicator reflects a specific gender-related aspect of reproduction, contributing to the face validity of the IWPR index as a reproductive rights measure. The IWPR composite index has been used in a previous study to measure the association between state-level reproductive rights and maternal and infant health outcomes (Sudhinaraset et al., 2020).
Our study assigned a score of 0 or 1 to each indicator. The IWPR index score is a tally of the indicators. A higher score on this index indicates greater reproductive access. IWPR was Z-standardized to account for variations in enacted restrictive abortion policies between states and improved the interpretation of the measure. We interpret the parameter estimates as a change given one standard deviation's (SD) increase in a state's reproductive access.
For our second primary exposure, we determined access to abortion services for each US state based on the presence of restrictive state laws and policies reported by the Guttmacher Institute (Guttmacher Institute, 2018). We coded policies using a binary 0/1 coding scheme to indicate if a restrictive policy was in effect in a given state. Laws included physician and hospital requirements, such as the requirement for an abortion by a licensed physician, the presence of a second physician, or whether abortion was required to be performed in a hospital. Forty-three states have gestational limits prohibiting abortions after a specified point in pregnancy. In addition, the prohibition of using state funds when federal funds are available has been enacted in 33 states and the District of Columbia. Twelve US states restrict coverage of abortion in private insurance plans. Forty-five states allow individual healthcare providers to refuse to participate in abortion services. Seventeen states have state-mandated counseling, during which pregnant individuals may be informed of a purported link between abortion and breast cancer, the ability of a fetus to feel pain, and long-term mental health consequences for the patient. Waiting period laws require a person seeking an abortion to wait a specified time period, such as 24 h, between receiving counseling and undergoing the procedure. Parental involvement laws vary across states but typically require the consent or notification of one or both parents 24–48 h in advance though some states allow grandparents or other relatives to substitute for parents. We summed the indicators to compute a total composite index for each state, reflecting the cumulative impact of multiple abortion restrictions. We categorized the composite index as supportive, moderate, hostile, or very hostile. We considered a state supportive of abortion rights if it had none or one of the above restrictions, a moderate state if it had 2–3 restrictions, a hostile state if it had 4–5, and a very hostile state if it had 6–10 restrictions.
2.2. Outcome
Our main outcome was frequent mental health distress. BRFSS asks respondents “Now thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good?” This question is part of the CDC Health-Related Quality of Life (CDC HRQOL– 4). Those who reported 14+ days when mental health was not good were categorized as having frequent mental health distress and those who reported 13 or fewer days were categorized as not having frequent mental health distress. This 14-day cut-off for frequent mental distress is widely accepted as the cutoff to identify individuals who experienced frequent mental health distress in the previous month (CDC, 1998; CDC, 2004; Dwyer-Lindgren et al., 2017; Quinn et al., 2023). Participants who said they did not know, were unsure, refused, or had a missing response were excluded from the investigation. This measure has shown acceptable test-retest relatability and strong internal validity in several populations, languages, and settings (Moriarty et al., 2003).
2.3. Individual-level covariates
Individual-level potential confounders from BRFSS include age (categorical variable in ten year groups from 18 to 64 with 65 and over as the reference group), education (less than high school, high school, some college, and college graduate or more (reference group)), race and ethnicity (White non-Hispanic (reference group), Black non-Hispanic, Hispanic, Asian non-Hispanic, Native non-Hispanic, Other non-Hispanic), and marital status (single versus married/coupled (reference group)). We used tertile cut-offs to categorize total annual household income into low (less than $35,000), medium ($35,000 to $75,000), and high (greater than $75,000 (reference group)).
2.4. Area-level covariates
The number of reproductive restrictions ranged from one to four. Our fully adjusted models included the following potential state-level confounders – region, Gini coefficient, median household income, proportion Black, proportion poor, and total state population. Previous studies have used these state-level confounders to examine the association between reproductive policies and individual-level birth and maternal outcomes (Addante et al., 2021; Sudhinaraset et al., 2020). All state-level potential confounders’ information was from the US Census. We coded the region variable using the standard Census regional categories. In our analyses, we chose New England as the reference group for the Census regional variable because the New England region was a priori generally believed to have fewer restrictive reproductive policies than other regions. The other state-level characteristics were measured as continuous variables. We applied a z-transformation to the continuously measured state-level variables to account for their skewed distributions.
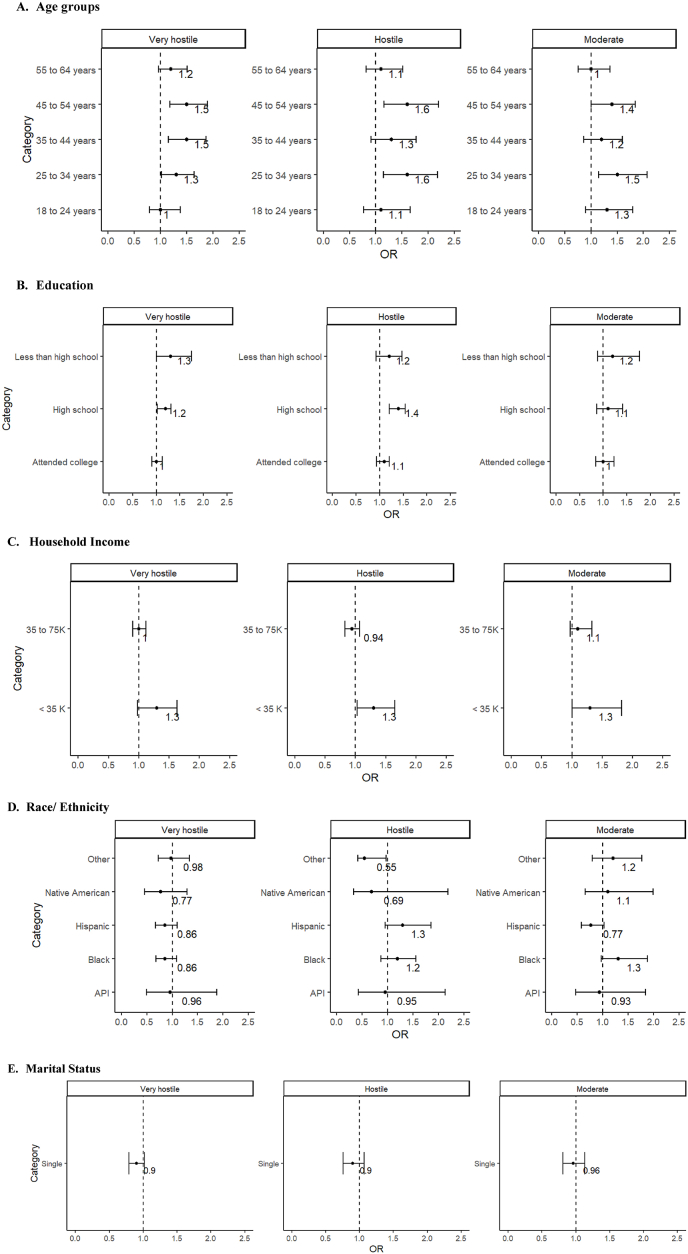
2.5. Statistical analyses
We used multilevel logistic regression to assess the relationship between reproductive rights and access to abortion services with the likelihood of reporting 14 or more days of frequent mental health distress. Multilevel models account for the clustering of BRFSS respondents within states and the District of Columbia. We adopted a series of models for this investigation. First, we estimated a state-level intercept-only model, which allowed for calculating the overall predicted probability and the plausible value range. This range is similar to the intraclass correlation coefficient (ICC), enabling us to calculate the degree of variability of the proportion of respondents reporting frequent mental health distress across states. For example, the range presents the proportions of women reporting 14 or more days of frequent mental health distress across US states in the previous 30 days. Second, we added state-level and individual-level covariates to the models (Table 2, Table 3). Third, we tested exposure and age, race, household income, education, and marital status in cross-level interaction terms to determine whether associations were heterogeneous across socio-demographic groups (Fig. 1). For all models, to obtain estimates generalizable to the US general population, 2018 BRFSS sampling weights were used. Analyses were conducted using Stata v. 14.0. Ethical approval was obtained from the Institutional Review Board of the University of Alberta (Ref: Pro00123816).
Table 2.
The relationship between state-level reproductive rights score and odds for frequent mental health distress, 2018 BRFSS a.
| Unadjusted OR (95% CI) | Adjusted OR (95%CI) | |
|---|---|---|
| State-level Characteristics | ||
| Reproductive rights score (z-transformed) | 0.98 (0.95, 1.02) | 0.95 (0.91, 0.99) |
| Region: Middle Atlantic vs. New England | 1.12 (0.92, 1.38) | |
| Region: South Atlantic vs. New England | 0.93 0.77,1.12) | |
| Region: East North Central vs. New England | 0.81 (0.68, 0.97) | |
| Region: East South Central vs. New England | 0.93 (0.76, 1.12) | |
| Region: West North Central vs. New England | 0.99 (0.77, 1.27) | |
| Region: West South Central vs. New England | 0.88 (0.69, 1.13) | |
| Region: Mountain vs. New England | 0.88 (0.75, 1.04) | |
| Region: Pacific vs. New England | 1.06 (0.89, 1.25) | |
| Proportion of black residents (z-transformed) | 0.98 (0.92, 1.04) | |
| Population size (z-transformed) | 0.98 (0.95, 1.02) | |
| Median income (z-transformed) | 0.98 (0.92, 1.04) | |
| Proportion in Poverty (z-transformed) | 1.04 (0.98, 1.10) | |
| Individual-level characteristics | ||
| Age: 18–24 years vs. 65 or greater | 3.37 (3.01, 3.77) | |
| Age: 25–34 years vs. 65 or greater | 2.93 (2.67, 3.23) | |
| Age: 35–44 years vs. 65 or greater | 2.68 (2.43, 2.96) | |
| Age: 45–54 years vs. 65 or greater | 2.81 (2.55, 3.09) | |
| Age: 55–64 years vs. 65 or greater | 2.35 (2.15, 2.58) | |
| Education: Less than high school vs. Completed college | 1.79 (1.59, 2.01) | |
| Education: High school vs. Completed college | 1.35 (1.24, 1.46) | |
| Education: Attended college vs. Completed college | 1.46 (1.36, 1.57) | |
| Household Income: Less than 35K vs. > 75K | 2.54 (2.32, 2.77) | |
| Household Income: 35–75K vs. > 75K | 1.55 (1.42, 1.69) | |
| Race: Black NH vs. White NH | 0.65 (0.59, 0.72) | |
| Race: Hispanic vs. White NH | 0.54 (0.48, 0.61) | |
| Race: Asian NH vs. White NH | 0.49 (0.37, 0.63) | |
| Race: Native NH vs. White NH | 0.85 (0.68, 1.07) | |
| Race: Other NH vs. White NH | 1.32 (1.15, 1.52) | |
| Marital status: Single vs. Married/Coupled | 1.40 (1.31, 1.49) | |
Model estimates that are statistically significant at p<0.05 levels are in bold.
Table 3.
The relationship between state-level abortion restriction measure and odds for frequent mental health distress, 2018 BRFSS a.
| Unadjusted OR (95% CI) | Adjusted OR (95% CI) | |
|---|---|---|
| State-level Characteristics | ||
| Abortion restrictions (ref: supportive) | Reference | Reference |
| Moderate | 1.05 (0.96,1.16) | 1.13 (1.03,1.25) |
| Hostile | 1.29 (1.11, 1.50) | 1.11 (0.98,1.26) |
| Very Hostile | 1.23 (1.12, 1.36) | 1.14 (1.01,1.29) |
| Region: Middle Atlantic vs. New England | 1.18 (1.03,1.35) | |
| Region: South Atlantic vs. New England | 0.93 (0.82, 1.05) | |
| Region: East North Central vs. New England | 0.83 (0.71, 0.97) | |
| Region: East South Central vs. New England | 0.93 (0.81,1.07) | |
| Region: West North Central vs. New England | 1.01 (0.86, 1.18) | |
| Region: West South Central vs. New England | 0.90 (0.77, 1.05) | |
| Region: Mountain vs. New England | 0.89 (0.79, 0.99) | |
| Region: Pacific vs. New England | 1.13 (0.98, 1.29) | |
| Proportion of black residents (z-transformed) | 0.98 (0.94, 1.02) | |
| Population size (z-transformed) | 0.98 (0.96, 1.01) | |
| Median income (z-transformed) | 0.97 (0.92, 1.02) | |
| Proportion in Poverty (z-transformed) | 1.04 (0.99, 1.09) | |
| Individual-level characteristics | ||
| Age: 18–24 years vs. 65 or greater | 3.37 (2.98, 3.80) | |
| Age: 25–34 years vs. 65 or greater | 2.93 (2.45, 3.52) | |
| Age: 35–44 years vs. 65 or greater | 2.68 (2.35, 3.07) | |
| Age: 45–54 years vs. 65 or greater | 2.81 (2.45, 3.22) | |
| Age: 55–64 years vs. 65 or greater | 2.35 (2.10, 2.63) | |
| Education: Less than high school vs. Completed college | 1.79 (1.61, 1.99) | |
| Education: High school vs. Completed college | 1.35 (1.26,1.44) | |
| Education: Attended college vs. Completed college | 1.46 (1.39, 1.54) | |
| Household Income: Less than 35K vs. > 75K | 2.54 (2.18, 2.95) | |
| Household Income: 35–75K vs. > 75K | 1.55 (1.48, 1.62) | |
| Race: Black NH vs. White NH | 0.65 (0.58, 0.73) | |
| Race: Hispanic vs. White NH | 0.54 (0.47, 0.63) | |
| Race: Asian NH vs. White NH | 0.49 (0.43, 0.56) | |
| Race: Native NH vs. White NH | 0.85 (0.66, 1.10) | |
| Race: Other NH vs. White NH | 1.32 (1.13, 1.54) | |
| Marital status: Single vs. Married/Coupled | 1.40 (1.31, 1.50) | |
Model estimates that are statistically significant at p<0.05 levels are in bold.
Fig. 1.
OR interaction terms and 95% CI for state-level abortion rights categorical score and sociodemographic characteristics.
3. Results
The analytic dataset included 235,016 women from 50 states and the District of Columbia who responded to the 2018 BRFSS. We excluded participants with missing data on the number of days with mental distress and any covariates, resulting in a case-complete dataset of 185,825 women (79.1%). Participants who were missing data were less likely to be from households with medium household incomes ($35,000 to $75,000 (OR = 0.60, 95% = 0.49,0.74)), and high household incomes (greater than $75,000 (OR = 0.47,95% CI = 0.34,0.62)), compared with those from households with low household incomes (less than $35,000). Participants with missing data were less likely to be Non-Hispanic Black (OR = 0.72, 95% CI = 0.57,0.92) or Hispanic (OR = 0.61, 95% CI: 0.45, 0.81). Participants with missing data were likelier to have less than a high school education (OR = 2.10, 95% CI: 1.51,2.91) or a high school diploma (OR = 1.50, 95% CI:1.09, 2.08).
Table 1 summarizes sample characteristics and gives weighted percentages of the respondents with complete data. A majority of the women were White non-Hispanic (64.3%), followed by Hispanic (15.2%) and Black non-Hispanic (12.6%). Approximately 15% of females in our analytical sample reported frequent mental health distress. The number of state-level abortion restrictions ranged from one to four. The reproductive rights score ranged from 0.23 to 6.28 before it was transformed into a Z-score (Appendix Table 2).
Table 1.
Characteristics of US women participating in the 2018 Behavioral Risk Factor Surveillance System (BRFSS) (n = 185,825) and US states (50 states and the District of Columbia).
| Individual Level Characteristics | Unweighted n | Weighted % |
|---|---|---|
| Age, years | ||
| 18-24 | 8365 | 10.6 |
| 25-34 | 19,536 | 18.0 |
| 35-44 | 23,680 | 17.0 |
| 45-54 | 29,778 | 16.8 |
| 55-64 | 40,014 | 17.4 |
| 65 and older | 64,452 | 20.3 |
| Education | ||
| Less than High School | 11,342 | 10.9 |
| High School | 46,848 | 25.2 |
| Some College | 54,354 | 33.3 |
| College | 73,281 | 30.6 |
| Household Income | ||
| Less than 35K | 73,226 | 39.8 |
| 35K–75K | 55,116 | 27.4 |
| Greater than 75K | 57,483 | 32.9 |
| Race/Ethnicity | ||
| White Non-Hispanic | 143,071 | 64.3 |
| Black Non-Hispanic | 17,407 | 12.6 |
| Hispanic | 12,964 | 15.2 |
| Asian Non-Hispanic | 3555 | 5.0 |
| Native Non-Hispanic | 3525 | 1.0 |
| Other Non-Hispanic | 5303 | 2.0 |
| Marital Status | ||
| Married/Coupled | 98,217 | 54.8 |
| Single | 87,608 | 45.2 |
| Frequent mental health distress | ||
| Yes | 24,785 | 15.0 |
| No | 161, 040 | 85.0 |
| State Level Characteristics (n = 51) | Mean (SD) | Median | Range |
|---|---|---|---|
| Gini Coefficient | 0.468(0.02) | 0.468 | 0.427-0.524 |
| State Median Income, USD | 58,143(9820) | 56,565 | 41,754-78,9945 |
| Proportion Black | 10.9 | 6.9 | 0.6-46.8 |
| Proportion Poor | 22.5(13.1) | 23.0 | 1.0 -45.0 |
| State Population | 6,332,183 (7,235,904) | 4,438,182 | 584,215-39,167,117 |
The intercept-only model indicated that the overall predicted probability of having frequent mental health distress in the past month was 15.3% (results not shown). Also, it confirmed the presence of significant variability in the percentage of women having frequent mental health distress in the past month. For example, the overall predictive probability of reporting frequent mental health distress in the previous month was 11.3%–20.4% across US states.
Table 2 reports the association between the state-level reproductive rights score and the likelihood of reporting frequent mental health distress. In the unadjusted model, no association was observed between the reproductive rights score and the likelihood of reporting frequent mental health distress in the previous month (OR = 0.98, 95% CI = 0.95, 1.02). After adjusting for individual-level and area-level confounders, an SD-unit increase in the reproductive rights score was significantly associated with decreased odds of reporting frequent mental health distress (OR = 0.95, 95% CI = 0.91, 0.99).
As shown in Tables 2 and in the fully adjusted model the East North Central region was associated with lower odds of reporting frequent mental health distress (OR = 0.81, 95% CI = 0.68, 0.97). Women in all age categories less than 65 had higher odds of frequent mental health distress compared to those 65 and older (e.g., 18–24 years vs. ≥65 (OR = 3.37, 95% CI = 3.01, 3.77). Women with less than a college degree had higher odds of frequent mental health distress compared with those who had a college degree (ex. Less than HS vs. College OR = 1.79, 95% CI = 1.59, 2.01). Black, Hispanic, and Asian individuals had lower odds of frequent mental health distress compared with White individuals (Black NH vs. White NH OR = 0.65, 95% CI = 0.59, 0.72; Hispanic vs. White NH OR = 0.54, 95% CI = 0.48, 0.61; Asian NH vs. White NH OR = 0.49, 95% CI = 0.37, 0.62). However, women who identified as Other race category had higher odds of frequent mental health distress compared to White NH women (OR = 1.32, 95% CI = 1.15, 1.52). Participants who reported an annual household income of less than $75,000 vs. $75,000 also had higher odds of frequent mental health distress (Less than 35K vs. greater than $75K OR = 2.54, 95% CI = 2.32, 2.77; 3k-75K vs. greater than $75K OR = 1.55, 95% CI = 1.55, 95% CI = 1.42, 1.69). Finally, being single vs. being married/coupled had higher odds of frequent mental health distress (OR = 1.40, 95% CI = 1.31, 1.49). In a series of sub-analyses, we added interaction terms between key sociodemographic characteristics that had been decided a priori to our models that adjusted for potential individual- and state-level confounders. However, none of the interaction terms in the fully adjusted models were statistically significant (results not shown), indicating that the association between the state-level reproductive rights score and odds of frequent mental health distress did not differ across race, age, marital status, household income, or educational status of the female participants.
Table 3 shows the associations between abortion restrictions at the state level and the likelihood of reporting frequent mental health distress among women. Crude analyses indicated that women who lived in states hostile (OR = 1.29, 95% CI = 1.11, 1.50) or very hostile (OR = 1.23, 95% CI = 1.12, 1.36) to abortion access were more likely to report frequent mental health distress than were women who lived in states that were supportive of abortion access. When controlling for individual-level and state-level characteristics, compared with those who lived in states that were supportive of abortion access, those residing in moderate (OR = 1.13, 95% CI = 1.03, 1.25) or very hostile (OR = 1.14, 95% CI = 1.01, 1.29) states were more likely to report frequent mental health distress.
Table 3 also indicates other sociodemographic characteristics were associated with frequent mental distress. Individual-level characteristics associated with higher odds of frequent mental health distress included younger age groups compared with those 65 and older (e.g., Ages 18 to 24 vs. ≥ 64 OR = 3.37, 95% CI = 2.98, 3.80); those with self-reported income less than $75,000 compared with $75,000 (e.g., Less than 35K vs. vs. ≥ 75K OR = 2.54, 95% CI = 2.18, 2.95); being single vs. married/couples (OR = 1.40, 95% CI = 1.31, 1.50); and having less than college degree vs. college degree (e.g., Less than high school vs. Completed College OR = 1.79, 95% CI = 1.61, 1.99). Women who identified as Other race also had increased odds of frequent mental health distress (OR = 1.32,95% CI = 1.13, 1.54). Characteristics associated with lower odds of frequent mental health distress included living in the East North Central vs. New England (OR = 0.83, 95% CI = 0.71, 0.97) and living in the Mountain region vs. New England (OR = 0.89, 95% CI = 0.79, 0.99). Black, Asian, and Hispanic women also had lower odds of frequent mental health distress status compared with their White counterparts (Black NH vs. White NH OR = 0.65, 95% CI = 0.58, 0.73; Hispanic vs. White NH OR = 0.54, 95% CI = 0.47, 0.63; Asian NH vs. White NH OR = 0.49, 95% CI = 0.43, 0.56).
Fig. 1 shows the interaction term between sociodemographic variables in the association between state-level abortion access and mental health across sociodemographic groups. Fig. 1A summarizes the interaction terms between state-level abortion access and specific age categories. We found no statistical association between abortion restrictions and frequent mental health distress among women aged 18 to 24 or older than 55 years. However, among women aged 25–34 years, compared with those living in states supportive of access to abortion, those residing in moderate (OR = 1.54, 95% CI = 1.14, 2.04), hostile (OR = 1.59, 95% CI = 1.15, 2.18), or very hostile states (OR = 1.29, 95% CI = 1.02, 1.64) were more likely to report frequent mental health distress. Among women aged 35–44 years (OR = 1.47, 95% CI = 1.15, 2.18), only those living in states very hostile to abortion access were significantly more likely to report frequent mental health distress. Among women aged 45–54 years, those living in moderate (OR = 1.35, 95% CI = 1.00, 1.84), hostile (OR = 1.60, 95% CI = 1.16, 2.20), or very hostile states (OR = 1.50, 95% CI = 1.18, 1.90) were significantly more likely to report frequent mental health distress.
Similar heterogeneous relationships were observed across levels of education categories (Fig. 1B) and income categories (Fig. 1C). For example, among women with less than a high school education, compared with those living in states with supportive abortion access, those living in states with very hostile (OR = 1.32, 95% CI = 1.00, 1.74) policies to abortion access were more likely to report frequent mental health distress. Among women with a high school degree, those living in states with hostile (OR = 1.36, 95% CI = 1.20, 1.54) and very hostile (OR = 1.16, 95% CI = 1.02, 1.31) policies towards abortion access were more likely to report frequent mental health distress. Among women with less than $35,000 household income, compared with those who lived in states supportive of abortion access, those residing in moderate (OR = 1.34, 95% CI = 1.00, 1.82), hostile (OR = 1.30, 95% CI = 1.03, 1.65), or very hostile states (OR = 1.26, 95% CI = 0.98, 1.63) were more likely to report frequent mental health distress (Fig. 1C). Associations between access to abortion and mental health were not heterogeneous across racial/ethnic categories or by marital status (Fig. 1C–D).
4. Discussion
Our study is unique because it examines the associations between restrictive reproductive rights environments and mental health status in the general female population. Previous studies in this area have focused on pregnant people or abortion restrictions (Biggs et al., 2017). Our study found that restrictive reproductive policies may be detrimentally associated with women's mental health beyond that of pregnant individuals. Our findings highlight the importance of taking a broad view of reproductive policies and not focusing solely on abortion restrictions or the effects only to pregnant people.
Results show that residing in states with greater reproductive rights was associated with decreased odds of frequent mental health distress among women. The association between the state-level reproductive rights score and odds of frequent mental health distress did not differ across female participants’ race, age, income, marital status, or educational status.
However, our results using the exposure measure of state-level abortion restrictions did indicate possibly more complex relationships. Residence in states with more abortion restrictions was associated with higher odds of frequent mental health distress among women. We found even women residing in moderate states with 2–3 abortion restrictions had higher odds of frequent mental health distress than those living in supportive states. There may be a threshold effect where the social and political climate in states with two restrictions is enough to create an environment associated with frequent mental health distress among females. Alternatively, the mix of different restrictions may explain the similar odds ratios for moderate and very hostile compared with supportive states.
Furthermore, our results suggest that state-level abortion restrictions may exacerbate socioeconomic and age disparities in mental health. Women in younger age groups and those with lower socioeconomic status (i.e., lower income or less than high school education) had higher odds of frequent mental health distress if they resided in a state that was not supportive of abortion access. By contrast, women with higher socioeconomic status (i.e., high school graduates) only experienced higher odds of frequent mental health distress if they lived in states with hostile or very hostile policies. Our results support previous reports that women with lower socioeconomic status (i.e., less income or less education) have historically encountered structural challenges in carrying out their reproductive decisions (Ogbu-Nwobodo et al., 2022). State restrictions on reproductive rights and abortion restrictions may contribute to and further perpetuate age and socioeconomic status disparities in mental health. State-level restrictions add to the structural imbalance of power that women with low socioeconomic status and younger women encounter.
There may be multiple complex pathways through which living in areas with restrictive reproductive rights may adversely affect the mental health of women. One possible mechanism may be the psychological loss of control all women may experience living under restrictive reproductive laws and policies. For example, a previous cross-sectional study in Ireland reported that a sense of general control mediated the relationship between political disenfranchisement and psychological well-being (Msetfi et al., 2018). Another possible mechanism may be the additional physical barriers women living in states with more restrictive reproductive policies may face as they seek high-quality, legal medical care and advice about sexual health. For example, studies have found that women living in states with restrictive reproductive policies travel farther, pay higher out-of-pocket costs, and experience greater stigma accessing legal contraceptive options (Barr-Walker et al., 2019; Margo et al., 2016). However, further research is needed to identify how policies affect women's mental health.
Laws and policies are a major structural determinant of population health in their ability to limit who can access health services and through what means (Dingake, 2017, Dingake, 2017). Historically, reproductive restrictions have raised overwhelming barriers for those with fewer resources. The heterogeneity of age and socioeconomic status in our sub-analyses may reflect particular groups’ inability to overcome such psychological and physical barriers created by restrictive reproductive policies. For example, women in lower socioeconomic groups may have limited resources to address obstacles to quality reproductive services, such as cost or distance. They may consequently be more affected by reproductive restrictions than women with higher socioeconomic status. By contrast, women with more abundant resources may have other options that offset the mental health burden of abortion restrictions and, perhaps, the resulting adverse mental health outcomes. In this manner, reproductive restrictions may exacerbate socioeconomic disparities in mental health.
These results should be interpreted in light of the study's limitations. First, we could not establish causality because our study uses cross-sectional data. Future longitudinal studies should examine changes in mental health measures before and after policies leading to reproductive restrictions. Researchers should take advantage of recently passed policies to conduct natural experiments to determine the potential adverse impact on health outcomes among women. Second, our outcome is based on self-reports of the number of days when the respondent's mental health was “not good”. Perceptions of health may differ by race and ethnicity because of cultural differences (Bombak, 2013). Therefore, there may be misclassification errors associated with the outcome that differ by race and ethnicity. Thirdly, we did not have information that may help explain the mechanisms involved. For example, we hypothesize that perceptions of control mediate the association between state-level reproductive restrictions and mental health. However, BRFSS does not measure perceived control. Another limitation is that BRFSS measured biological sex (females and males); thus, we limited our investigation to those identified as women at birth rather than all people who could be pregnant. Although gender and sex are intrinsically and reciprocally linked, we cannot study the complexity of the non-binary nature of gender. In addition, a higher proportion of BRFSS participants excluded from this study due to missing data were racial minorities, had annual household incomes less than $35,000, and had less than high school education. This may limit the generalizability of our study results. In addition, the missingness may also lead to measurement error and potential bias toward the null, as previous studies have indicated that people of low SES are more affected by state restrictions (Goyal et al., 2020; Redd et al., 2021). Finally, our exposure variables are composite indices based on multiple indicator policies and laws. Several of the individual indicator policies may not considerably influence our mental health outcome, which would contribute to measurement error. However, if our composite exposure variables contained such indicators, our results would be biased toward the null.
Despite these limitations, our study has several key strengths. First, our study uses a nationally representative sample and examines the associations between state-level reproductive rights and abortion access and mental health among all women. In addition, our analysis accounted for the structure of the data by using multilevel models to reflect the association between state-level restrictions and the odds of frequent mental health distress at the individual level.
State-level legislation restricted reproductive access increased dramatically in the last decade (Nash et al., 2020) and the amount and intensity of these restrictions are poised to expand in the post-Roe context. The escalation of restrictive sexual health policies in the US will likely impact the health of pregnant individuals and women in general. As put forth in the SRJ framework, having the autonomy to make reproductive and sexual health decisions is a necessary condition for justice and the well-being for women (Ross & Solinger, 2017). Future studies should assess the effects of specific reproductive policies. In addition, future research needs to incorporate women's lived experiences in response to such policies to fully understand how the growing intensification of reproductive policies affects all women.
Author statement
All persons who meet authorship criteria are listed as authors. All authors certify that they have participated in the components of the work including participation in the concept, design, analysis, writing, or revision of the manuscript.
Ethical statement
This study was reviewed and considered human subjects exempt by the Institutional Review Board at the University of Alberta. All authors of this study do not have any financial disclosures to report.
Financial statement
All authors report no financial funding was associated with this study.
Funding
This study did not receive any specific grant support from any funding agencies. However, RP holds a Tier II Canada Research Chair (CRC) in Social and Health Inequities and CB is a recipient of the Women and Children's Health Research Institute (WCHRI) Graduate Studentship Award. Open access fees were paid from RP’s CRC research stipend.
Declaration of competing interest
On behalf of all authors, I would like report that we have no conflict of interest.
Appendix Table A. State-level measure of reproductive rights score and access to abortion services and specific policies used to create each score
| Global Measure | Policy/Population indicator |
|---|---|
| Reproductive rights score | Coverage of infertility treatment |
| Reproductive rights score | Medicaid expansion or state Medicaid plan allows for family planning eligibility expenses |
| Reproductive rights score | Mandatory sex education in schools |
| Reproductive rights score | Law allowing same-sex marriage or second-parent adoption for individuals in a same-sex relationship |
| Reproductive rights score | Percent of women living in counties with at least one abortion provider |
| Reproductive rights score | Proc-choice governor or legislator |
| Reproductive rights score | Restriction on public funding for abortion |
| Abortion services | Laws with specified physician and hospital requirements |
| Abortion services | Laws prohibiting abortions after a specified point during the gestational period |
| Abortion services | Laws prohibiting intact dilation and extraction |
| Abortion services | Laws that allow individual healthcare providers to refuse to participate in abortion services |
| Abortion services | Laws prohibiting use of state funds in cases when federal funds are available |
| Abortion services; Reproductive Rights | Mandatory Parental or notification laws |
| Abortion services | State restrictions on abortion coverage in private insurance plans |
| Abortion services | State-mandated counseling before abortion services |
| Abortion services; Reproductive Rights | Waiting period laws requiring a person seeking an abortion to wait a specified time period between receiving counseling and undergoing the procedure |
Appendix Table B. Reproductive Rights Score and Number of Abortion Restrictions for each US state
| State | Reproductive Rights Score | Number of Abortion Restrictions |
|---|---|---|
| Alabama | 1.91 | 4 |
| Alaska | 2.83 | 2 |
| Arizona | 3.36 | 4 |
| Arkansas | 1.72 | 4 |
| California | 5.24 | 1 |
| Colorado | 3.71 | 2 |
| Connecticut | 5.95 | 1 |
| Delaware | 3.82 | 2 |
| District of Columbia | 5.50 | 1 |
| Florida | 2.79 | 4 |
| Georgia | 2.85 | 3 |
| Hawaii | 6.00 | 1 |
| Idaho | 0.81 | 3 |
| Illinois | 4.78 | 2 |
| Indiana | 1.89 | 4 |
| Iowa | 3.83 | 3 |
| Kansas | 0.76 | 4 |
| Kentucky | 2.43 | 4 |
| Louisiana | 1.62 | 4 |
| Maine | 3.53 | 1 |
| Maryland | 6.14 | 1 |
| Massachusetts | 4.74 | 2 |
| Michigan | 1.66 | 4 |
| Minnesota | 4.68 | 2 |
| Mississippi | 2.09 | 4 |
| Missouri | 1.68 | 4 |
| Montana | 5.04 | 1 |
| Nebraska | 0.59 | 4 |
| Nevada | 4.44 | 2 |
| New Hampshire | 3.55 | 2 |
| New Jersey | 6.08 | 1 |
| New Mexico | 5.02 | 1 |
| New York | 5.59 | 1 |
| North Carolina | 3.01 | 4 |
| North Dakota | 2.27 | 4 |
| Ohio | 2.99 | 4 |
| Oklahoma | 1.95 | 4 |
| Oregon | 6.28 | 1 |
| Pennsylvania | 2.53 | 3 |
| Rhode Island | 4.63 | 3 |
| South Carolina | 3.07 | 4 |
| South Dakota | 0.23 | 4 |
| Tennessee | 1.42 | 4 |
| Texas | 2.19 | 4 |
| Utah | 2.16 | 4 |
| Vermont | 6.15 | 1 |
| Virginia | 2.24 | 4 |
| Washington | 5.20 | 1 |
| West Virginia | 4.35 | 3 |
| Wisconsin | 1.90 | 4 |
| Wyoming | 2.21 | 2 |
Data availability
The data is publicly available. We have shared a link to the publicly available data in our paper.
References
- Addante A.N., Eisenberg D.L., Valentine M.C., Leonard J., Maddox K.E.J., Hoofnagle M.H. The association between state-level abortion restrictions and maternal mortality in the United States, 1995-2017. Contraception. 2021;104:496–501. doi: 10.1016/j.contraception.2021.03.018. [DOI] [PubMed] [Google Scholar]
- Barr-Walker J., Jayaweera R.T., Ramirez A.M., Gerdts C. Experiences of women who travel for abortion: A mixed methods systematic review. PLoS One. 2019;14 doi: 10.1371/journal.pone.0209991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentele K.G., Sager R., Aykanian A. Rewinding Roe v. Wade: Understanding the accelerated adoption of state-level restrictive abortion legislation, 2008–2014. Journal of Women, Politics & Policy. 2018;39:490–517. [Google Scholar]
- Biggs M.A., Upadhyay U.D., McCulloch C.E., Foster D.G. Women's mental health and well-being 5 Years after receiving or being denied an abortion: A prospective, longitudinal cohort study. JAMA Psychiatry. 2017;74:169–178. doi: 10.1001/jamapsychiatry.2016.3478. [DOI] [PubMed] [Google Scholar]
- Bombak A.E. Self-rated health and public health: A critical perspective. Frontiers in Public Health. 2013;1:15. doi: 10.3389/fpubh.2013.00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC Self-reported frequent mental distress among adults--United States, 1993-1996. MMWR. Morbidity and mortality weekly report. 1998;47:326–331. [PubMed] [Google Scholar]
- CDC Self-reported frequent mental distress among adults--United States, 1993-2001. MMWR. Morbidity and mortality weekly report. 2004;53:963–966. [PubMed] [Google Scholar]
- CDC . Centers for Disease Control; 2019. The behavioral risk factor surveillance System (BRFSS) overview: BRFSS 2018. [Google Scholar]
- Dingake O.B.K. The rule of law as a social determinant of health. Health Hum Rights. 2017;19:295–298. [PMC free article] [PubMed] [Google Scholar]
- Dingake O.B.K. The rule of law as a social determinant of health. Health Hum Rights. 2017;19(2):295–298. [PMC free article] [PubMed] [Google Scholar]
- Dwyer-Lindgren L., Mackenbach J.P., van Lenthe F.J., Mokdad A.H. Self-reported general health, physical distress, mental distress, and activity limitation by US county, 1995-2012. Population Health Metrics. 2017;15:16. doi: 10.1186/s12963-017-0133-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster D.G. Scribner; New York: 2020. The turnaway study. [Google Scholar]
- Fuentes L., Lebenkoff S., White K., Gerdts C., Hopkins K., Potter J.E., et al. Women's experiences seeking abortion care shortly after the closure of clinics due to a restrictive law in Texas. Contraception. 2016;93:292–297. doi: 10.1016/j.contraception.2015.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo M.F., Casterline J.B., Chakraborty P., Norris A., Bessett D., Turner A.N. Passage of abortion ban and women's accurate understanding of abortion legality. American Journal of Obstetrics and Gynecology. 2021;225(1):63.e61–63.e68. doi: 10.1016/j.ajog.2021.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerdts C., Fuentes L., Grossman D., White K., Keefe-Oates B., Baum S.E., et al. Impact of clinic closures on women obtaining abortion services after implementation of a restrictive law in Texas. American Journal of Public Health. 2016;106:857–864. doi: 10.2105/AJPH.2016.303134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goyal V., Brooks I.H.M., Powers D.A. Differences in abortion rates by race–ethnicity after implementation of a restrictive Texas law. Contraception. 2020;102:109–114. doi: 10.1016/j.contraception.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hess C., Milli J., Hayes J., Hegewisch A., Mayayeva Y., Román S., et al. Institute for Women’s Policy Research; Washington, DC: 2015. The status of women in the states: 2015. [Google Scholar]
- Institute G. 2018. State policy brief: An overview of abortion laws available. [Google Scholar]
- Krieger N., Gruskin S., Singh N., Kiang M.V., Chen J.T., Waterman P.D., et al. Reproductive justice and the pace of change: Socioeconomic trends in US infant death rates by legal status of abortion, 1960-1980. American Journal of Public Health. 2015;105:680–682. doi: 10.2105/AJPH.2014.302401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara D., Holt K., Peña M., Grossman D. Knowledge of abortion laws and services among low-income women in three United States cities. Journal of Immigrant and Minority Health. 2015;17(6):1811–1818. doi: 10.1007/s10903-014-0147-z. [DOI] [PubMed] [Google Scholar]
- Margo J., McCloskey L., Gupte G., Zurek M., Bhakta S., Feinberg E. Women's pathways to abortion care in South Carolina: A qualitative study of obstacles and supports. Perspectives on Sexual and Reproductive Health. 2016;48:199–207. doi: 10.1363/psrh.12006. [DOI] [PubMed] [Google Scholar]
- Mishori R. The social determinants of health? Time to focus on the political determinants of health. Medical Care. 2019;57:491–493. doi: 10.1097/MLR.0000000000001131. [DOI] [PubMed] [Google Scholar]
- Moriarty D.G., Zack M.M., Kobau R. The Centers for Disease control and prevention's healthy days measures–population tracking of perceived physical and mental health over time. Health and Quality of Life Outcomes. 2003;1:1–8. doi: 10.1186/1477-7525-1-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Msetfi R., Jay S., O'Donnell A.T., Kearns M., Kinsella E.L., McMahon J., et al. Restricted reproductive rights and risky sexual behaviour: How political disenfranchisement relates to women's sense of control, well-being and sexual health. Journal of Health Psychology. 2018;23:252–262. doi: 10.1177/1359105317736784. [DOI] [PubMed] [Google Scholar]
- Nash E., Mohammed L., Cappello O., Naide S. 2020. State policy trends 2020: Reproductive health and rights in a year like no other. [Google Scholar]
- Ogbu-Nwobodo L., Shim R.S., Vinson S.Y., Fitelson E.M., Biggs M.A., McLemore M.R., et al. Mental health implications of abortion restrictions for historically marginalized populations. New England Journal of Medicine. 2022;387:1613–1617. doi: 10.1056/NEJMms2211124. [DOI] [PubMed] [Google Scholar]
- Pabayo R., Ehntholt A., Cook D.M., Reynolds M., Muennig P., Liu S.Y. Laws restricting access to abortion services and infant mortality risk in the United States. International Journal of Environmental Research and Public Health. 2020;17:3773. doi: 10.3390/ijerph17113773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn D.A., Hollis B.F., Dichter M.E., Blosnich J.R. Recent and frequent mental distress among women with a history of military service, 2003–2019. The Journal of Behavioral Health Services & Research. 2023;50:119–127. doi: 10.1007/s11414-022-09825-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redd S.K., Rice W.S., Aswani M.S., Blake S., Julian Z., Sen B., et al. Racial/ethnic and educational inequities in restrictive abortion policy variation and adverse birth outcomes in the United States. BMC Health Services Research. 2021;21:1139. doi: 10.1186/s12913-021-07165-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts S.C., Fuentes L., Kriz R., Williams V., Upadhyay U.D. Implications for women of Louisiana's law requiring abortion providers to have hospital admitting privileges. Contraception. 2015;91:368–372. doi: 10.1016/j.contraception.2015.02.001. [DOI] [PubMed] [Google Scholar]
- Ross L., Solinger R. Univ of California Press; 2017. Reproductive justice: An introduction. [Google Scholar]
- Sudhinaraset M., Vilda D., Gipson J.D., Bornstein M., Wallace M.E. Women's reproductive rights policies and adverse birth outcomes: A state-level analysis to assess the role of race and nativity status. American Journal of Preventive Medicine. 2020;59:787–795. doi: 10.1016/j.amepre.2020.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace M.E., Evans M.G., Theall K. The status of women's reproductive rights and adverse birth outcomes. Women's Health Issues. 2017;27:121–128. doi: 10.1016/j.whi.2016.12.013. [DOI] [PubMed] [Google Scholar]
- WHO . 2009. Mental health aspects of women's reproductive health: A global review of the literature. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data is publicly available. We have shared a link to the publicly available data in our paper.