Abstract
Introduction
The COVID-19 pandemic forced numerous pain clinics to suspend their services. For chronic pain patients, even a temporary closure and inability to connect with their healthcare providers may result in adverse outcomes. There are serious concerns regarding worsening of physical and emotional suffering and a surge in substance abuse. Therefore, telemedicine, also called telehealth, would seem to be a reasonable alternative to in-person clinic visits during the lockdowns. However, it remains unclear whether a telemedicine consultation is adequate for diagnostic purposes and subsequent intervention planning.
Methods
This study was conducted as an open-label cohort study on new patients referred to an interdisciplinary community pain clinic focused on image-guided interventions. The primary outcome was to determine whether a video consultation was sufficient to make an initial diagnosis and plan subsequent interventions. Secondary variables included technical feasibility, patient satisfaction, calculated nonincurred cost and time-saving. Video consultations were performed using a secure videoconference system consistent with routine clinic practice.
Results
Sixty-five participants were recruited, and 49 (75.4%) completed the study. Patients for whom interventional approaches were not recommended elected not to continue with clinic visits. The intra-observer agreement rate between the telemedicine and in-person encounter was 93.9% (95% CI 87.2-100) for the diagnostic codes and treatment plan. The median satisfaction score from the telemedicine encounter was seven on a scale of 0–7, and it remained 6 when the remote care experience was later compared with the in-person visit. There were considerable savings in travel time and expenses.
Discussion
The study experimentally validated the ability of telemedicine encounters to establish a diagnosis and formulate an interventional pain management plan of care. The validity of virtual consultation for complex pain care remains to be determined. It is unreasonable to expect telemedicine to completely replace clinic visits in the foreseeable future. However, judicious use of technology may facilitate timely scheduling, save time and resources, and improve satisfaction without jeopardizing the quality of care.
Keywords: Chronic pain, Telemedicine, Interventional pain management
1. Introduction
The early use of telemedicine dates back to the 1990s. It has evolved tremendously since then. The COVID-19 pandemic swiftly influenced an upswing in the utilization of telemedicine. On March 16, 2020, the Ontario Ministry of Health announced increased resources for telemedicine and the approval of new billing codes enabling physicians to continue providing routine healthcare services by video and telephone, including assessment of possible COVID-19 symptoms [1]. While some healthcare providers (HCPs) were able to resort to telemedicine options quickly, others elected to suspend their services. Even temporary closure of ambulatory services and inability to connect with HCPs may result in adverse outcomes for chronic pain patients. There are serious concerns about worsening physical and emotional suffering and a surge in substance abuse. Conceivably, delays in chronic pain management may trigger psychosocial complications, such as depression, isolation, ineffective coping mechanisms (including substance abuse), and social isolation [2,3]. Therefore, telemedicine appears to an attractive and reasonable alternatives to in-person clinic visits to continue chronic pain services.
Although telemedicine had not been broadly utilized in Ontario before the COVID pandemic, the technology has been available for at least 20 years [4]. A 2012 literature review of 141 randomized controlled trials in which telemedicine interventions of various kinds had been tested in 37,695 patients identified publication biases, non-inferiority to standard care, and cost-saving [5]. In addition to common chronic conditions (e.g., asthma, COPD, diabetes, heart failure, hypertension), telemedicine has been implemented to manage multiple sclerosis, Parkinson's disease, orthopedic problems, etc. [[6], [7], [8]]. Even though telemedicine is not a newcomer in chronic pain management, in Ontario it has been primarily utilized for case discussions and education (e.g., ECHO project), and a limited number of practicing physicians) [9]. Other small research projects concerning direct patient-healthcare provider interactions emphasized a positive experience with ease of access, high satisfaction, and significant cost saving [10,11]. Limited evidence is available concerning outcomes of telemedicine care [12]. Conceivably, HCPs may be reluctant to commit to a diagnosis and treatment plan without physical face-to-face encounter and hands-on examination.
Formal training in pain medicine includes a physical assessment as part of the evaluation and ultimate formulation of a working diagnosis [13]. The initial consultation culminates in recommendations, including medications, diagnostic and/or therapeutic interventional procedures, counseling, and allied health approaches. Due to the complexity of some cases, several in-person visits may be necessary to complete interviews, psychological tests, and other evaluations. Patients from remote geographic areas are the most disadvantaged group dealing with cumbersome, expensive, and time-consuming arrangements to attend their appointments. During times of crisis, such as the ongoing pandemic, clinic visits become even more impractical and discouraged unless they are absolutely necessary.
To our knowledge, there have been no publications experimentally addressing the applicability of telemedicine in diagnosing chronic pain problems and providing accurate recommendations concerning the next step, particularly as it applies to image-guided interventions.
2. Material and methods
From March 20, 2020, Silver Pain Center's clinic policy changed, and all non-procedural in-clinic visits were halted to comply with the recommended avoidance of non-essential visits and prevention of possible COVID-19 spread. The clinic has continued to provide telemedicine care and in-clinic procedural services.
The study was planned as an open-label cohort study on chronic pain patients newly referred to our interdisciplinary community outpatient clinic. The primary outcome was to determine whether video consultations were sufficient to formulate working diagnosis and plan subsequent interventions. Secondary variables included technical feasibility, patient satisfaction, and nonincurred cost and time-saving.
The protocol was approved by an independent ethics review board (Veritas Inc, IRB Tracking Number: 16552-15:11:3913-04-2020) and registered with ClinicalTrials.gov (NCT04370717) on May 1, 2020. The published literature was reviewed using PubMed search engine and full access to the manuscripts was feasible through the University of Toronto online library services. Other resources were accessed online (e.g., government publications).
Following the IRB approval of the study protocol on May 8, 2020, all consecutive eligible candidates were offered to participate, and enrollment continued for 12 months. Eligibility was determined by assessing the inclusion and exclusion criteria. All patients who gave consent to participate in telemedicine consultation were recruited. Because of the mandatory closure of non-essential in-clinic visits, patients who were not interested or excluded were only able to have initial consultations by telephone. Exclusion criteria were based on factors deemed non-reconcilable for the remote visits. Patients who were non-English speakers and had no one in their household to help with translation were excluded. Patients who did not have compatible telecommunication devices or were illiterate in basic telecommunication skills with no help at home were excluded as well. Other non-eligibility criteria included the inability to complete online self-assessment forms and study questionnaires, unwillingness to make a follow-up visit, and changing pain complaints (e.g., a patient referred for back pain but identified headaches on the pre-consultation intake form).
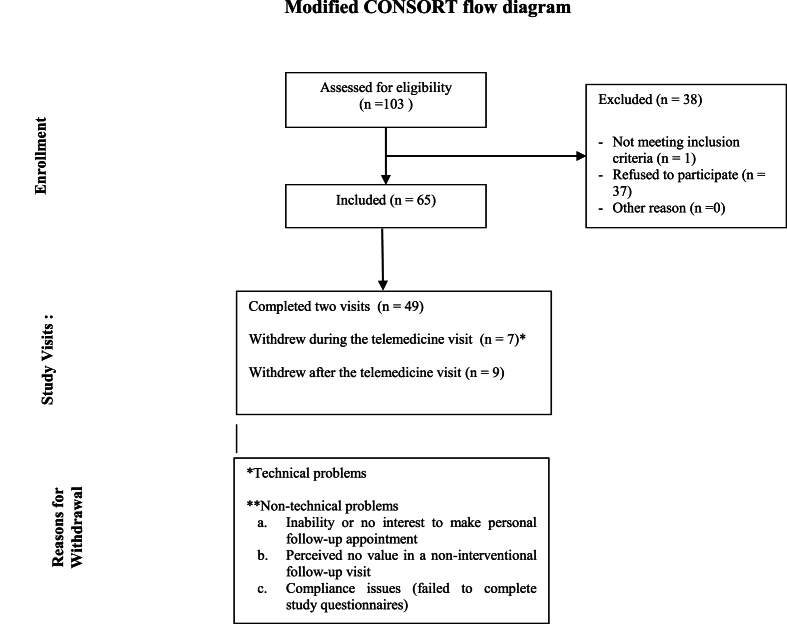
The first participant was recruited on May 12, 2020. A total of 103 candidates were approached, and 65 were enrolled. 37 candidates declined to participate, and one was excluded based on the eligibility criteria (Fig. 1). The main reasons for voluntary non-participation were perceived technical issues, busy schedule, and inconvenience.
Fig. 1.
A modified CONSORT diagram of the study recruitment of subjects.
Patients who expressed their interest in participating in the study received the informed consent form and had unlimited time to review it and contact the research coordinator to obtain more information. Patients were required to electronically sign the informed consent form, complete other routine clinic documents, and send the package via DocuSign to the clinic patient care coordinator. The standard questionnaires included the Brief Pain Inventory Short Form (BPI-SF), the Patient Health Questionnaire (PHQ-4), McGill Pain Questionnaire Short Form (MPQ-SF), Pain Catastrophizing Scale Short Form (PCS-SF), and Somatic Symptom Scale (SSS-8) [14].
Video consultations were performed using an approved videoconference system (Ontario Telemedicine Network or Medeo). Ontario Telemedicine Network (OTN) is a proprietary of Ontario Health and funded by the Ontario Ministry of Health for use by Ontario physicians. Medeo is a platform of QHR technologies, one of Canada's providers of electronic medical record solutions. Both options are secure and protect personal health information. Physicians completed patient consultations using laptop or desktop computers. Patients were able to select from multiple options, including desktop or laptop computers, tablets and smartphones. Both platforms offer web-based and application interfaces. Telemedicine consultations were scheduled and conducted without modifications from the routine clinic practice. A structured history taking and an abbreviated physical examination, based on the World Academy of Pain Medicine United webinar series, were implemented [15]. The participating physicians were not limited to a strict protocol and each case was approached based on clinical judgment. The case report included ICD-10-CA codes and a plan of care. ICD-10-CA is a Canadian edition of the ICD-10 coding system that is being used for billing purposes. The 3-point scale measured the primary outcome, whereas 1 means the diagnosis remained unchanged; 2 means the diagnosis remained within the same ICD-10-CA category; 3 means diagnosis changed to another ICD-10-CA category. The same coding was used for the plan of care, whereas 1 represented the exact planned procedure was performed, 2 – the procedure was slightly modified (e.g., bilateral instead of unilateral, vertebral level within the same segment), and 3 – totally different procedure was done, or it was cancelled.
Secondary outcomes included the following.
-
1.
Feasibility: (a) patients' acceptance of telemedicine, (b) dropout rates and causes of dropouts (medical or technical reasons), (c) participants' satisfaction with video quality and sound quality (patients were asked if they were “satisfied” with the video quality and sound quality after each telemedicine consultation; “Yes” or “No, why not?“), (d) technical errors with the telemedicine equipment, and (e) specialist consultation time in minutes.
-
2.
Patient satisfaction from the telemedicine visit was recorded using a 7-point Likert score (0, completely dissatisfied to 7, completely satisfied)
-
3.
Calculated cost-saving included (a) cost of travel in Canadian dollars, (b) estimated loss of income, (c) saved travel distance in kilometres and travel time in hours as estimated by Google Maps.
After one week, patients received an electronic satisfaction survey.
An in-person follow-up and/or procedural visit was subsequently scheduled. During this visit, the same physician completed physical examination, documented the diagnosis, and either proceeded to treatment or modify the care plan. The research coordinator entered the diagnostic and procedural codes in the case report form.
2.1. Statistical analysis
A simple rate was computed for the primary outcome of the intra-observer agreement between telemedicine and in-patient visits for both ICD-10-CA coding diagnosis and treatment. The 95% confidence interval for our sampling error was calculated using the standard error based on the number of participants (n).
For psychosocial metrics, we compiled descriptive statistics. The values were based on ordinal tests that are not normally distributed, and therefore reported as medians and interquartile ranges. To compare participants that withdrew from the study with those that completed the study, we performed Mann-Whitney U testing for this non-parametric data.
Monetary costs, time spent, and distances traveled were reported as both mean (SD) and median (IQR) to report the best measure of central tendency.
Data was collected in Excel v. 16.5. All outcomes were performed using IBM SPSS, build 1.0.0.1508, 2020 subscription.
3. Results
Sixty-five participants were recruited and 49 (75.4%) completed the study. Seven (10.3%) withdrew due to technical problems encountered during a telemedicine appointment. Nine (13.2%), withdrew for reasons unrelated to technical issues (Fig. 1). Of 65 enrolled patients, 22 were identified as males and 43 as females. The mean age was 52 (24–74). Patients who withdrew due to technical issues were slightly older with a mean age of 58 (35–73) versus 53 (24–74) for those who completed the telemedicine visit; however, the difference did not reach statistical significance. When comparing participants that completed the study with those that withdrew, there were no significant differences in their psychosocial characteristics. This was done with Mann-Whitney U testing due to the non-normal distribution of responses for all metrics, which were ordinal. (Table 1, Table 2). Overall, the study participants exhibited moderate degree of pain-related disability (mean PDI of 47 [9–70]), moderate anxiety and depression (mean PHQ4 of 5.74 [0–12]), high somatic orientation (mean SSS-8 of 14.75 [[2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25]]), and catastrophizing (mean PCL-C 11 [[2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16]]).
Table 1.
Mann-Whitney U test, Complete vs. Withdrawna Participants.
| Completed |
Withdrawn |
sig. | |||
|---|---|---|---|---|---|
| Mean Rank | N | Mean Rank | n | ||
| NRS | 34.4 | 49 | 26.2 | 15 | 0.13 |
| BPI-SF, relief in last 24H | 33.3 | 49 | 32.2 | 16 | 0.84 |
| BPI-SF Total | 34.1 | 49 | 29.6 | 16 | 0.40 |
| PHQ-4 | 30.9 | 49 | 39.5 | 16 | 0.11 |
| PCS-SF | 33.9 | 49 | 30.3 | 16 | 0.51 |
| SSS-8 | 32.7 | 49 | 33.8 | 16 | 0.85 |
| MPQ-SF Sensory | 34.5 | 49 | 28.5 | 16 | 0.27 |
| MPQ-SF Affective | 33.9 | 49 | 30.2 | 16 | 0.50 |
| Satisfaction | 28 | 49 | 23.3 | 6 | 0.44 |
Includes Technical and Non-technical Withdrawals Legends needed.
Table 2.
Mann-Whitney U test, Complete vs. Withdrawna Participants.
| Completed |
Withdrawn |
sig. | |||
|---|---|---|---|---|---|
| Mean Rank | n | Mean Rank | n | ||
| NRS | 31.2 | 49 | 20.2 | 9 | 0.07 |
| BPI-SF, relief in last 24H | 30.4 | 49 | 24.6 | 9 | 0.34 |
| BPI-SF Total | 30.6 | 49 | 23.4 | 9 | 0.24 |
| PHQ-4 | 28.6 | 49 | 34.6 | 9 | 0.33 |
| PCS-SF | 29.7 | 49 | 28.4 | 9 | 0.84 |
| SSS-8 | 29.5 | 49 | 29.3 | 9 | 0.97 |
| MPQ-SF Sensory | 30.6 | 49 | 23.5 | 9 | 0.25 |
| MPQ-SF Affective | 20.3 | 49 | 24.9 | 9 | 0.38 |
| Satisfaction | 28 | 49 | 23.3 | 6 | 0.44 |
Includes only Non-technical Withdrawals List the reason for withdrawal.
3.1. Primary outcome
Based on the ICD-10-CA coding agreement, only three patients (6.1%) differed between their telemedicine and in-clinic assessments or the recommended treatment. Two patients with a matching diagnosis underwent an intervention that was different from the initially planned procedure. Another patient who was diagnosed with gonarthrosis was found to have a patellofemoral problem during the physical appointment. This patient received the same planned intraarticular injection. There was an additional patient with correctly diagnosed spondylosis and mechanical back pain who came to the clinic with a sore throat, which added a new diagnostic code. Because his pain-related diagnosis and plan of care remained the same, this case was not considered discrepant. Therefore, with an n of 49, the agreement rate was 93.9% (95% CI 87.2-100) for both the diagnostic codes and treatment plan. The median scores for psychosocial parameters of these patients are displayed in Table 3.
Table 3.
Psychosocial Charactersitics of Participans and Satisfaction Scores
| Assessment Scores | Median | IQR |
|---|---|---|
| NRS | 7 | (7 - 8) |
| BPI-SF, % relief in last 24H | 30 | (10 - 50) |
| BPI-SF | 52 | (40 - 58.5) |
| PHQ-4 | 5 | (2 - 8.5) |
| PCS-SF | 12 | (8.5 - 14) |
| SSS-8 | 15 | (11 - 18.5) |
| MPQ-SF Sensory | 19 | (10 - 23) |
| MPQ-SF Affective | 6 | (2 - 9) |
| Telemedicine Satisfaction | 7 | (6 -7) |
| Telemedicine vs. Clinic Satisfaction | 6 | (6 -7) |
3.2. Secondary outcome
The median satisfaction score from the telemedicine encounter was 7/7 on the scale of 0–7. Once it was compared with in-person visit experience, it reduced to 6/7. The median travel time saving was 0:38 h with untraveled median distance of 50.1 km. The median cost saving was CAD 40.20 for travel expenses, and CAD 0.00 for a loss of income. This was because 65.3% of participants reported no income loss. On the other hand, the mean nonincurred income loss was CAD 142.00. Zero dollars was the minimum reported total, and CAD 2000.00 was the maximum reported non incurred lost income. Table 4 summarizes these findings.
Table 4.
Travel and Cost Saving
| Quality Metrics | Mean | SD | Median | IQR |
|---|---|---|---|---|
| Saved Travel Cost (CAD) | 40.2 | 78.8 | 20 | (7.25-25.00) |
| Income Not Lost (CAD) | 142.1 | 345 | 0 | (0.00 - 153.00) |
| Saved Distance (km) | 87.9 | 102.8 | 50.1 | (27.8 - 98.2) |
| Saved Travel Time (h:mm) | 1:04 | 1:01 | 0:38 | (0:27 - 1:17) |
4. Discussion
While there is mixed evidence on the effectiveness of telemedicine to make accurate diagnoses, most studies suggest a positive correlation. The results of this study were congruent with a clinical impression of the accuracy and effectiveness of telemedicine consultations in an outpatient interventional pain clinic. Patients recruited in the study represented typical demographics of chronic pain sufferers, with more females and older age. Patients who completed their telemedicine visits and then withdrew their consent for the subsequent clinic/research visit were similar in their demographics and psychosocial patterns, with only a slight trend for a lower pain intensity (NRS) of those who elected not to pursue a subsequent clinic visit (31.2 vs 20.2 p=0.07).
Recently published commentary discouraged the use of telemedicine methods for new chronic pain patients [16]. The authors offered the opinion statements based on their personal experiences, consideration of key aspects of chronic pain care, and limited literature review, but not. on experimental data. While there is ongoing deliberation on whether or not telemedicine can replace in-clinic evaluation of chronic pain problems, other disciplines generally support the validity of remote visits. Contrary to the above mentioned publication, Russell et al. confirmed the effectiveness of a telerehabilitation assessment of ankle disorders using telemedicine. In their study that was published twelve years ago, 93.3% agreement rate between in-person and remote diagnosis of ankle disorders was reported. A high level of inter- and intra-rater reliability was found, even when a complex anatomical assessment was involved [17]. Subsequently, the same group demonstrated the accuracy and reliability of an online musculoskeletal physiotherapy assessment of the knee complex using telerehabilitation compared to a traditional face-to-face assessment. Primary pathoanatomical diagnoses were in exact agreement in 67% of cases and were similar in 89%. The pathology system was found to be in agreement in 17 out of 18 cases (94%) [18]. Palacín-Marín et al. conducted a pilot study suggesting that a telerehabilitation system may be helpful in assessing individuals with chronic low back pain. The α reliability between face-to-face and telerehabilitation evaluations was more than 0.80 for 7 of the 9 outcome measures [19]. Another study indicated that patients with chronic musculoskeletal spinal conditions could achieve clinically meaningful improvements in their condition when accessing care via telerehabilitation [20]. The article concluded that telerehabilitation should be considered for individuals unable to access relevant in-person services; however, non-inferiority remained inconclusive and required further exploration [20]. Even more affirmative conclusions, more focused on the diagnostic accuracy and decision-making, were highlighted in two studies concerning general orthopedic and spine patients [21,22]. Surgical and interventional plans were rarely changed following the telemedicine consultations. These publications evaluated the accuracy and effectiveness of assessing semi-objective components (e.g., range of motion, provocation tests) to reach diagnostic conclusions.
Pain assessment may be different and more challenging. Early attempts to introduce telemedicine were hampered by the fear of promoting services that were deemed to be more convenient to healthcare providers while abandoning non-technology savvy patients with less access to the necessary resources. Initially in Ontario, community telemedicine sites employed on-site nurses or nurse practitioners to facilitate patient encounters. The earliest review article published in 2012 accurately predicted an expansion of telemedicine pain services and called for developing telemedicine pain services to fit patient needs, not technological advances [23]. The explosion of smartphone technologies and affordable wireless connectivity enabled the use of video communication, without facilitators, directly between physicians and patients.
The present study provides satisfactory experimental evidence concerning consultation accuracy of telemedicine examinations and diagnosis. As long as HCPs are trained in virtual communications, including remote physical examination, and patients have access to audio-video resources and minimally required logistical arrangements, establishing a working diagnosis and recommending a care plan can be achieved. Conversely, technological illiteracy, unstable cellular or Wi-Fi connection, and the lack of telecommunication devices in households would result in the inability to conduct meaningful and productive clinical encounters on the patient side. Although non-English speakers were excluded for convenience, our daily experience supports the use of telemedicine for these individuals if a family member can facilitate translation. Aside from training and experience, HCPs must have a secure privacy-compliant telemedicine platform and administrative support. The latter is necessary for electronic consent collection, scheduling, and administering pre-consultation questionnaires.
All appointments in this study were conducted via either the Ontario Telemedicine Network of Ontario Health or Medeo videoconferencing service of the existing electronic medical records system (Accuro ® EMR, QHR Technologies, Canada). Telephone appointments were not considered due to the inability to conduct telemedicine physical examination and a perceived high risk of misunderstanding and misinterpretation. Despite the widespread use of telephones in daily life and the range of possible benefits that telephones offer for routine follow-up encounters, their role in medical practice remains, for many clinicians, controversial [24]. Furthermore, the telephone connection is not secure and does not allow the identification of the speaker. Experimental research also does not support using telephone-based interventions for managing chronic pain [25]. Taking into account all the above-mentioned reasons, telephone encounters were considered insufficient to serve as a tool for telemedicine consultations, but, nevertheless, were offered to patients who were unable or disinterested in the videocommunications as as personal consultations were not allowed. Most patients were satisfied with the quality and content of their telemedicine appointments and were almost equally pleased when compared with personal encounters. The results were congruent to the conclusions of other publications. All patients with non-acute headaches were satisfied with telemedicine visits [12]. A study that examined telemedicine during the COVID-19 pandemic in sports and musculoskeletal medicine found that patients rated their telemedicine visit as “excellent” or “very good” across measures (91.6%–95.0%) including addressing concerns, communication, developing a treatment plan, convenience, and satisfaction [26]. In our study, participants who did not complete the visit due to technical problems were excluded from further analyses. Conceivably, they were dissatisfied with their telemedicine encounter.
Saving of time and expenses were considerable and consistent with previously published literature [6,11].
There are a few drawbacks of telemedicine consultations identified. Hands-on elements of the physical examination cannot be completed, such as manual palpation and detailed neurological examination. Reliability of patient-administered self-examination varies greatly between patients. Nonetheless, some components such as appearance, behavioral patterns, active range of motion and provocation tests can be more confidently relied upon during the telemedicine encounter.
There was evident uncertainty related to intra-observer versus inter-observer reliability. In our study, the same physician who encountered the patient via telemedicine also examined and confirmed the diagnosis and treatment plan on the subsequent clinic visit. Therefore, the absolute accuracy of the diagnosis cannot be evaluated. However, this scenario is similar to routine clinical care in which physicians typically establish a working diagnosis and continue their own workup and treatments. Physicians may err in the diagnosis and treatment options regardless of whether patients are seen in-person or virtually. To the authors’ knowledge, there are no publications addressing the inter-observer reliability of pain diagnosis.
Patients may also perceive that their participation in the study would expedite subsequent procedural appointments. After the consultation, most of those who elected to drop out confirmed that they did not see a value in making a non-procedural visit and were reluctant to be accidentally exposed to the COVID-19 virus. This consideration may be applicable only in a research setting. Nonetheless, we cannot make any conclusion concerning the diagnostic accuracy of non-interventional visits.
Patient literacy or economic barriers were the main reasons for refusing participation or early withdrawal due to telecommunication problems. These factors continue to pose significant hurdles to a broader acceptance of telemedicine for disadvantaged populations.
A wider acceptance of telemedicine is also related to physician conservatism, lack of resources, and unfavorable reimbursement policies. Medical practice liability concerns may also play a role in denying telemedicine methods. It is conceivable that some physicians do not feel comfortable deferring physical examination, fearing that inability to do so would result in misdiagnosis and mismanagement.
Notwithstanding the natural and artificial drawbacks of telemedicine-enabled chronic pain management, the restrictions placed by the COVID-19 pandemic provided the impetus towards healthcare restructuring that enabled remote evaluations, management, and treatments.
Telemedicine-focused publications have exponentially increased since the onset of the COVID-19 pandemic. One study compared a telerehabilitation program (TP) with no intervention group of women with fibromyalgia during a lockdown. The TP group improved pain intensity (p = 0.022), mechanical pain sensitivity (p < 0.05), and psychological distress (p = 0.005) compared to the Control group. The Control group showed no statistically significant changes in any variable (p > 0.05) [27].
A virtual multidisciplinary approach also seems feasible and practical. The Australian researchers confirmed that the program was significantly more effective than usual care at increasing pain self-efficacy (g = 0.69) and several secondary measures at post-treatment and follow-up, including movement-based fear avoidance and pain-related disability [28].
5. Conclusions
This study experimentally validated the ability of telemedicine encounters to establish a working diagnosis and postulate a plan of care in the interventional pain management setting. Although elimination of clinic visits and their replacement by telemedicine is not expected, the study results suggest thata judicious use of technology may facilitate timely scheduling, save time and money, and improve patient satisfaction without jeopardizing the quality of care.
Funding
The study was financially supported by the Silver Pain Clinic operational funding.
Contributorship statement
•Michael Gofeld: generated the concept and design, wrote the protocol draft and revisions, communicated with IRB, conducted the study procedures, collected data, drafted the manuscript, and submitted the manuscript.
•Kevin Smith: contributed to design and protocol, conducted the study procedures, drafted and revised the manuscript.
•Vladimir Djuric: contributed to design and protocol, conducted the study procedures, drafted and revised the manuscript.
•Faisal Motlani: contributed to design and protocol, conducted the study procedures, drafted and revised the manuscript.
•Daniel Baldor: contributed to design and protocol, generated statistical plan, analysed data and produced statistical inferences, and drafted the result section.
All authors accept full responsibility for the finished work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Conflict of interest statement
Nothing to declare pertinent to the submitted research.
Acknowledgements
The authors cordially thank Annelise Marsig (research assistant) for providing necessary support and managing the study, and the Silver Pain Centre administrative team for helping with patient education and recruitment.
References
- 1.https://news.ontario.ca/mohltc/en/2020/3/province-expanding-telehealth-ontario-resources.html
- 2.Cegla T.H., Magner A. Einfluss der Coronapandemie auf Schmerzpatienten : Welche Auswirkungen der Pandemie auf ihre Versorgung nehmen Patienten mit chronischen Schmerzen wahr? [Influence of the corona pandemic on pain patients: which impacts of the pandemic on their care do patients with chronic pain experience?] Schmerz. 2021;35:188–194. doi: 10.1007/s00482-021-00549-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Consonni M., Telesca A., Grazzi L., Cazzato D., Lauria G. Life with chronic pain during COVID-19 lockdown: the case of patients with small fibre neuropathy and chronic migraine. Neurol Sci. 2021;42:389–397. doi: 10.1007/s10072-020-04890-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ryan P., Kobb R., Hilsen P. Making the right connection: matching patients to technology. Telemed J e Health. 2003;9:81–88. doi: 10.1089/153056203763317684. [DOI] [PubMed] [Google Scholar]
- 5.Wootton R. Twenty years of telemedicine in chronic disease management – an evidence synthesis. J Telemed Telecare. 2012;18:211–220. doi: 10.1258/jtt.2012.120219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Robb J.F., Hyland M.H., Goodman A.D. Comparison of telemedicine versus in-person visits for persons with multiple sclerosis: a randomized crossover study of feasibility, cost, and satisfaction. Mult Scler Relat Disord. 2019;36 doi: 10.1016/j.msard.2019.05.001. [DOI] [PubMed] [Google Scholar]
- 7.Beck C.A., Beran D.B., Biglan K.M., et al. National randomized controlled trial of virtual house calls for Parkinson disease. Neurology. 2017;89:1152–1161. doi: 10.1212/WNL.0000000000004357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Buvik A., Bergmo T.S., Bugge E., Smaabrekke A., Wilsgaard T., Olsen J.A. Cost-effectiveness of telemedicine in remote orthopedic consultations: randomized controlled trial. J Med Internet Res. 2019;21(2) doi: 10.2196/11330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hassan S., Carlin L., Zhao J., Taenzer P., Furlan A.D. Promoting an interprofessional approach to chronic pain management in primary care using Project ECHO. J Interprof Care. 2020;9:1–4. doi: 10.1080/13561820.2020.1733502. [DOI] [PubMed] [Google Scholar]
- 10.Peng P.W., Stafford M.A., Wong D.T., Salenieks M.E. Use of telemedicine in chronic pain consultation: a pilot study. Clin J Pain. 2006;22:350–352. doi: 10.1097/01.ajp.0000169671.55276.87. [DOI] [PubMed] [Google Scholar]
- 11.Pronovost A., Peng P., Kern R. Telemedicine in the management of chronic pain: a cost analysis study. Can J Anaesth. 2009;56:590–596. doi: 10.1007/s12630-009-9123-9. [DOI] [PubMed] [Google Scholar]
- 12.Müller K.I., Alstadhaug K.B., Bekkelund S.I. Acceptability, feasibility, and cost of telemedicine for nonacute headaches: a randomized study comparing video and traditional consultations. J Med Internet Res. 2016;18(5):e140. doi: 10.2196/jmir.5221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.www.royalcollege.ca/rcsite/documents/ibd/pain-medicine-otr-e Objectives of Training in the Subspecialty of Pain Medicine.
- 14.https://ocean.cognisantmd.com/site/Site.html#eForms
- 15.https://vimeo.com/ondemand/wapmutelemedicine
- 16.Emerick T., Alter B., Jarquin S., Brancolini S., Bernstein C., Luong K., Morrisseyand S., Wasan A. Telemedicine for chronic pain in the COVID-19 era and beyond. Pain Med. 2020;21:1743–1748. doi: 10.1093/pm/pnaa220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Russell T.G., Blumke R., Richardson B., Truter P. Telerehabilitation mediated physiotherapy assessment of ankle disorders. Physiother Res Int. 2010;15:167–175. doi: 10.1002/pri.471. [DOI] [PubMed] [Google Scholar]
- 18.Richardson B.R., Truter P., Blumke R., Russell T.G. Physiotherapy assessment and diagnosis of musculoskeletal disorders of the knee via telerehabilitation. J Telemed Telecare. 2017;23:88–95. doi: 10.1177/1357633X15627237. [DOI] [PubMed] [Google Scholar]
- 19.Palacín-Marín F., Esteban-Moreno B., Olea N., Herrera-Viedma E., Arroyo-Morales M. Agreement between telerehabilitation and face-to-face clinical outcome assessments for low back pain in primary care. Spine. 2013;38:947–952. doi: 10.1097/BRS.0b013e318281a36c. [DOI] [PubMed] [Google Scholar]
- 20.Cottrell M.A., O'Leary S.P., Raymer M., Hill A.J., Comans T., Russell T.G. Does telerehabilitation result in inferior clinical outcomes compared with in-person care for the management of chronic musculoskeletal spinal conditions in the tertiary hospital setting? A non-randomised pilot clinical trial. J Telemed Telecare. 2019;27:444–452. doi: 10.1177/1357633X19887265. [DOI] [PubMed] [Google Scholar]
- 21.Crawford A.M., Lightsey H.M., Xiong G.X., Striano B.M., Greene N., Schoenfeld A.J., Simpson A.K. Interventional procedure plans generated by telemedicine visits in spine patients are rarely changed after in-person evaluation. Reg Anesth Pain Med. 2021;46:478–481. doi: 10.1136/rapm-2021-102630. [DOI] [PubMed] [Google Scholar]
- 22.Crawford A.M., Lightsey H.M., Xiong G.X., Striano B.M., Schoenfeld A.J., Simpson A.K. Telemedicine visits generate accurate surgical plans across orthopaedic subspecialties. Arch Orthop Trauma Surg. 2022;142:3009–3016. doi: 10.1007/s00402-021-03903-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McGeary D.D., McGeary C.A., Gatchel R.J. A comprehensive review of telehealth for pain management: where we are and the way ahead. Pain Pract. 2012;12:570–577. doi: 10.1111/j.1533-2500.2012.00534.x. [DOI] [PubMed] [Google Scholar]
- 24.Delichatsios H., Callahan M., Charlson M. Outcomes of telephone medical care. J. Gen Intern Med. 1998;13:579–585. doi: 10.1046/j.1525-1497.1998.00179.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rutledge T., Atkinson J.H., Chircop-Rollick T., D'Andrea J., Garfin S., Patel S., Penzien D.B., Wallace M., Weickgenant A.L., Slater M. Randomized controlled trial of telephone-delivered cognitive behavioral therapy versus supportive care for chronic back pain. Clin J Pain. 2018;34:322–327. doi: 10.1097/AJP.0000000000000555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tenforde A.S., Iaccarino M.A., Borgstrom H., et al. Telemedicine during COVID-19 for outpatient sports and musculoskeletal medicine physicians. Pharm Manag PM R. 2020;12(9):926–932. doi: 10.1002/pmrj.12422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hernando-Garijo I., Ceballos-Laita L., Mingo-Gómez M.T., Medrano-de-la-Fuente R., Estébanez-de-Miguel E., Martínez-Pérez M.N., Jiménez-Del-Barrio S. Immediate effects of a telerehabilitation program based on aerobic exercise in women with fibromyalgia. Int J Environ Res Publ Health. 2021;18:2075. doi: 10.3390/ijerph18042075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smith J., Faux S.G., Gardner T., Hobbs M.J., James M.A., Joubert A.E., Kladnitski N., Newby J.M., Schultz R., Shiner C.T., Andrews G. Reboot online: a randomized controlled trial comparing an online multidisciplinary pain management program with usual care for chronic pain. Pain Med. 2019;20:2385–2396. doi: 10.1093/pm/pnz208. [DOI] [PubMed] [Google Scholar]