Abstract
Objective
This study examined psychopathology and weight over 4 years following bariatric surgery in adolescents with obesity, as compared to a nonsurgical group. The role of psychological dysregulation in relation to psychopathology in the 2–4 year “maintenance phase” following surgery was also examined.
Methods
Adolescent participants (122 surgical and 70 nonsurgical) completed height/weight and psychopathology assessments annually for 4 years, with dysregulation assessed at Year 2. Analyses examined the association of “High” and “Low” psychopathology with weight over time using logistic regression. Mediation analyses in the surgical group examined indirect effects of dysregulation on percent weight loss through Year 4 psychopathology.
Results
There were lower odds of “High” internalizing symptoms in the surgical group versus the nonsurgical group from baseline (presurgery) to Year 4 (OR = .39; p < .001; 42.3% “High” internalizing in surgical; 66.7% in nonsurgical) and during the 2–4 year maintenance phase (OR = .35, p < .05; 35.1% “High” internalizing in surgical; 60.8% in nonsurgical). There was a significant mediation effect in the surgical group: higher dysregulation was associated with greater Year 4 internalizing symptoms (β = .41, p < .001) which in turn was associated with less Year 4 percent weight loss (β = −.27, p < .05).
Conclusions
While the surgical group was less likely to experience internalizing symptoms, internalizing psychopathology was related to less percent weight loss in this group. Internalizing symptoms mediated the relationship between dysregulation and percent weight loss in the surgical group. Postoperative mental health follow-up is needed for adolescents into young adulthood.
Keywords: adolescent, bariatric surgery, dysregulation, internalizing, psychopathology
Introduction
Drivers of obesity are multifaceted and reflect interactions of environmental influences, genetic risk, individual factors, and systemic inequities (Swinburn et al., 2011). Certainly, a multitude of factors affect overweight and obesity in youth from a developmental systems perspective (e.g., social-contextual factors, experiences of adversity, and access to resources; Bohnert et al., 2020). Severe obesity remains a public health concern for youth, due to associated medical and psychological comorbidities and their likely persistence into young adulthood (Armstrong et al., 2019) without effective intervention. Bariatric surgery has been established as an effective treatment for improving weight, overall health, and quality of life in adolescents with severe obesity (Inge et al., 2017), with 60% of adolescent patients of Roux-en-Y gastric bypass maintaining a weight loss of 20% over 5 years, at minimum (Inge et al., 2017). While this is an overall net improvement, the variability in sustained weight loss for the remaining 40% of patients in the study warrants further investigation. Specifically, there is a critical need to understand the influence of psychological factors on adolescent weight trajectories following bariatric surgery to inform responsive follow-up care that sustains benefits.
Prospective longitudinal follow-up of adolescent psychosocial health following bariatric surgery has mainly come from two research groups: (a) the Adolescent Morbid Obesity Study (AMOS) in Sweden, a national study of Roux-en-Y gastric bypass surgery (Järvholm et al., 2020); and (b) an initial small single site series and subsequent larger multisite series within the U.S., led by Zeller, Inge, and colleagues. The evidence from these groups thus far indicates that while postoperative psychopathology trajectories of psychopathology following surgery vary for some (Zeller et al., 2017), psychopathology tends to persist for a sizable subgroup of adolescents. Following surgery, research shows improvements in anxiety, depression, and self-concept for adolescents in the short-term (i.e., 4 months postsurgery; Järvholm et al., 2012). Continued improvements in depressive symptoms, health-related quality of life, anxiety, anger, and disruptive behavior (Järvholm et al., 2015) occur within the first year following surgery, with deceleration around 6 months (Zeller et al., 2009) and stabilization (Järvholm et al., 2016) or “rebound” of symptoms at Year 2 (Zeller et al., 2011). Approximately, one-third of adolescents presented with symptomatic psychopathology at 2 years following surgery (Hunsaker et al., 2018), and findings continue to point to the persistent nature of psychopathology 5 years following surgery (Järvholm et al., 2020). Trajectories of psychopathology remain largely understudied in the 2–4 years of follow-up window, an important period that determines potential persistent psychopathology symptoms for adolescents. This fits with the known risk for emerging psychopathology in the transition from adolescence into young adulthood, as over half of the adults with a lifetime prevalence of a psychiatric diagnosis report onset in adolescence (by age 14) or young adulthood (by age 24; Kessler et al., 2005). These 2–4 years may also be when individuals experience weight recurrence (Inge et al., 2017; Zeller et al., 2011). This is coupled with persistent psychopathology and related risk factors that emerge for adolescents 2 years following the procedure (Hunsaker et al., 2018). Thus, the 2–4 years postsurgery appear to be an important “maintenance phase” that may be a turning point for both psychopathology and some weight recurrence (Majid et al., 2022).1 It remains unclear how these observed trajectories of persistent psychopathology relate to weight change trajectories following adolescent bariatric surgery, especially after 2 years. Examination of this time period in a surgical group in conjunction with a nonsurgical group may elucidate the specific needs of both groups of adolescents with severe obesity.
Adolescence is a period of heightened vulnerability where various factors, such as dysregulation, can pose an increased risk to developing psychopathology (McLaughlin et al., 2011). Dysregulation, defined generally as difficulty regulating or managing processes of cognition, emotion, and/or behavior, is a key component of psychopathology (Beauchaine, 2015; McLaughlin et al., 2011) and a potential risk factor for obesity in youth (Javaras et al., 2020). Factors found to impact postsurgery outcomes in adult patients include aspects of dysregulation, such as emotion dysregulation, affect intensity, and effortful control (Lavender et al., 2020). Recent work has conceptualized dysregulation as a dispositional factor (i.e., stable rather than fluctuating) that can be related to greater challenges in adherence to postsurgery recommendations and less optimal long-term postsurgical outcomes in adults (Lavender et al., 2020). Our previous work showed that greater dysregulation was related to suicidality 4 years following surgery (Zeller et al., 2020) but it is not fully understood how dysregulation may impact postsurgery outcomes. The type of dysregulation (i.e., affective, cognitive, or behavioral) may also have differential influences on aspects of psychopathology and eating behavior (i.e., internalizing vs. externalizing; Gowey et al., 2016; Lavender et al., 2020; McLaughlin et al., 2011). As dysregulation and psychopathology are closely linked and associated with weight-related outcomes, further investigation of these pathways is needed to understand these potential risk factors for adolescents undergoing bariatric surgery.
Present Study
A better understanding of behavioral and dispositional factors related to persistent presentations of psychopathology and weight gain/recurrence is needed to inform clinical follow-up to maintain the physical and psychological well-being for adolescents postbariatric surgery, with particular attention to the 2–4 year period. Using a prospective observational design, the aims of the present study were to examine: change or persistence of psychopathology from presurgery/baseline through 4 years postsurgery/follow-up (Aim 1), associations between psychopathology status with BMI over time (Aim 2), and dysregulation as an indirect predictor of weight loss outcomes via psychopathology in the surgical group (Aim 3). We hypothesized that the majority of adolescents in both the surgical and nonsurgical groups would maintain their psychopathology status over time (i.e., persistently low/high), a small subgroup would experience changes in psychopathology status (i.e., remitting or deteriorating), and more participants in the surgical group would meet criteria for “Low” psychopathology status at Year 4 as compared to the nonsurgical group (Aim 1). We also hypothesized that “High” psychopathology status would be associated with less primary weight loss and more weight recurrence by Year 2 and Year 4 in the surgical group, and greater weight gain in the nonsurgical group (Aim 2). Finally, we hypothesized that higher dysregulation at Year 2 would be predictive of lower percent weight loss in the surgical group, and this effect would be mediated by psychopathology (internalizing and externalizing) at Year 4 (Aim 3).
Methods
Participants and Procedures
Participants in the present study were part of the TeenView ancillary studies conducted in collaboration with the Teen Longitudinal Assessment of Bariatric Surgery consortium (Teen-LABS), a prospective longitudinal study collecting clinical and laboratory data on adolescents undergoing bariatric surgery at five sites in the US (Inge et al., 2016). Participants were invited to participate in a series of ancillary studies (i.e., the TeenView series) examining psychosocial variables from baseline, and over years of follow-up. The TeenView studies were designed with a comparator group of demographically similar adolescents with severe obesity presenting for nonsurgical behavioral weight management at the Teen-LABS sites. The surgical and nonsurgical groups were followed over the same years (Zeller et al., 2019). All procedures, recruitment and enrollment strategies, and eligibility criteria for Teen-LABS and the TeenView studies were approved by respective institutional review boards and have been previously described (Hunsaker et al., 2018; Inge et al., 2016; Zeller et al., 2019, 2020). Participants provided written consent at each study phase.
Constructs and Measures
Psychological Dysregulation
The Dysregulation Inventory is a 92-item self-report measure completed at Year 2 that assesses affective, behavioral, and cognitive dysregulation, as well as Total psychological dysregulation (Mezzich et al., 2001). Example subscale items are: Affective Dysregulation:“I just cannot calm down faster than most people”; Behavioral Dysregulation: “I jump into situations before I think it through”; Cognitive Dysregulation: “I have trouble changing the way I do things, even when I am doing them wrong”. Cronbach’s alpha reflected good internal consistency reliability: Cognitive (α = .83); Affective (α = .93); Behavioral (α = .93).
Body Mass Index and Weight Change
Height and weight were obtained at each time point (Baseline, Years 1, 2, 4) and used to calculate body mass index (BMI). Year 1 BMI was only used in the growth curve analyses. For descriptive purposes, percent weight change was calculated as ([weightfollow-up − weightbaseline]/weightbaseline) × 100, with weight gain represented as positive values and weight loss as negative. For Aim 3 analyses with the surgical sample, percent weight change was recalculated for ease of interpretation as ([weightbaseline − weightfollow-up]/weightbaseline) × 100, with higher values indicating greater weight loss. For the surgical sample, weights were set to missing for participants identified as pregnant (n = 2 at Y1, n = 5 at Y2, n = 11 at Y4). Pregnancy data were not available for the nonsurgical sample.
Psychopathology
Psychopathology was measured through the Achenbach Youth Self-Report and Adult Self-Report (YSR for ≤18 years/ASR for ≥19; Achenbach & Rescorla, 2001). The Internalizing and Externalizing broadband scales at baseline, Year 2, and Year 4 were used in the present study. T-scores on the YSR/ASR scales can fall in the Normal, Borderline, or Clinical range with a T-score >60 used as a cutoff indicating symptomotology in the Borderline clinical range (Achenbach & Rescorla, 2001; Hunsaker et al., 2018; Järvholm et al; 2020). Borderline clinical cutoffs (T-score > 60) were used to create 4 status groupings of symptom presentation across timepoints (Baseline, Year 2, and Year 4) and for the maintenance phase (Year 2 and Year 4). Persistently high psychopathology: borderline or clinical range symptoms at baseline and at either 2 or 4 years; Persistently low psychopathology: normal range symptoms at presurgery/baseline, 2 and 4 years. Remitting psychopathology: borderline or clinical range symptoms at presurgery/baseline, then normal range at 2 and 4 years; Deteriorating psychopathology: normal range symptoms at presurgery/baseline, then borderline or clinical range at either 2 or 4 years. From these categories, two status groupings were defined: (a) Low: Persistently lowandremitting combined; (b) High: Persistently highanddeteriorating combined. For the maintenance phase, groupings were consistent with the definitions above applied to the specific timeframe (e.g., Persistently high: borderline or clinical range at Year 2 and Year 4).
Demographics
Demographic information was obtained via parent/self-report at baseline and follow-up: adolescent age/date of birth, sex assigned at birth, race/ethnicity, and maternal education.
History of Child Maltreatment
The Child Trauma Questionnaire–Short Form (CTQ) is a 28-item measure completed only at baseline that was used to include history of child maltreatment (i.e., emotional, physical, sexual abuse, and emotional or physical neglect) as a covariate in the present study (Bernstein et al., 2003) as this has been associated with greater psychosocial burden in adolescents undergoing bariatric surgery (Zeller et al., 2015). This measure has good criterion-related validity in adolescence. Higher scores indicate greater severity of reported child maltreatment, with established score ranges (Bernstein et al., 2003). For the purposes of this study, a “0” on this measure indicated no maltreatment scales in the moderate clinical range, and a “1” indicated at least one maltreatment scale in the moderate clinical range.
Mental Health Treatment
As part of the parent Teen-LABS protocol at Year 4, the surgical group self-reported use of psychiatric medication (i.e., antidepressants, mood stabilizers, and stimulants) dichotomized as 0 = none or 1 = any, use of outpatient mental health treatment and/or psychiatric hospitalization in the previous 12 months. This information was not collected in the nonsurgical group.
Data Analysis
Preliminary analyses were run in SPSS and hypothesis testing was conducted in Mplus. Chi-square and t-tests were used for attrition analyses. Missing data were handled via maximum likelihood estimation in Mplus (Version 7.11). The nesting of participants within the five sites was controlled for in hypothesized analyses via specialized variable and analysis commands in Mplus (i.e., ‘Cluster = site’ and ‘Type = Complex’) to avoid possible Type-1 errors. Preliminary analyses compared cohorts (surgical vs. nonsurgical) on demographic factors. Covariates in analyses for Aims 1, 2, and 3 included sex, race/ethnicity, age, caregiver education, baseline BMI, and history of child maltreatment. Data are made available upon request.
Study aim analyses are described here. Aim 1: Descriptive statistics were run to determine psychopathology status grouping, in each of the 4 groups, then dichotomized to “High” (i.e., persistently high or deteriorating symptoms) and “Low” (i.e., persistently low or remitting symptoms) for internalizing and externalizing symptoms. Logistic regressions were run to test whether group (surgical vs. nonsurgical) was associated with psychopathology status when controlling covariates. Aim 2: Growth curve models were estimated using structural equation modeling to test whether change in BMI over time (baseline, Years 1, 2, and 4) varied by psychopathology status, using a time by group interaction. These analyses were completed separately for the surgical and nonsurgical groups and controlled for the specified covariates. Aim 3: For the surgical group only, mediation analyses examined the indirect effects of dysregulation (Year 2) on percent weight change through psychopathology (internalizing, externalizing at Year 4, run separately). Similar analyses were not completed with the nonsurgical group due to small sample size. To maximize statistical power, correlations between potential covariates and outcomes were run to determine covariates to include in mediation models, with sex emerging as the only significant covariate. In addition, psychopathology (internalizing and externalizing) was included in these models as a continuous variable.
Results
At baseline, participants (n = 192) were a mean age of 16.6 years old, 79.7% Female, and 60.9% White. There were no significant differences between the surgical (n = 122) and nonsurgical (n = 70) groups across sex, race/ethnicity, or caregiver education at baseline. Participants in the surgical group were slightly older (M age = 16.9) than participants in the nonsurgical group (M age = 16.1). Relative to nonsurgical, the surgical group had a higher baseline BMI (p < .001), but by Year 4 a lower BMI (p < .001) and a greater percent weight change (i.e., loss; p < .001). As in previous work, reported rates of child maltreatment history were significantly higher in the nonsurgical group (Zeller et al., 2015), and this was included as a covariate in analyses. In the surgical group, 19 participants who were in the study at Year 2 did not participate at Year 4: 1 was ineligible (deceased), 4 declined, and 14 were unable to be located. Attrition analyses indicated that those who participated at Year 2 but not Year 4 did not significantly differ by surgical versus nonsurgical group, race, age, or baseline BMI. However, those who participated at Year 4 were more likely to be female than male (n = 134 vs. 25; chi-square: χ2 = 8.65; p < .05) and have higher total psychopathology T-scores (M = 51.6 at Y4 vs. 45.9 at Y2; t = −2.82; p < .01). See Table I and Supplementary Table 4 and 5 for descriptive statistics of participant characteristics and psychopathology status groupings, respectively.
Table I.
Demographic Characteristics of Adolescent Participants
| Demographic characteristics | Total | Surgical | Nonsurgical | |
|---|---|---|---|---|
| Mean ± SD n (%) | Mean ± SD n (%) | Mean ± SD n (%) | p a | |
| Baseline | n = 192 | n = 122 | n = 70 | |
| Age | 16.61 ± 1.39 | 16.91 ± 1.33 | 16.10 ± 1.38 | <.001 |
| Sex assigned at birth (% female) | 153 (79.7%) | 97 (79.5%) | 56 (80.0%) | .96 |
| Race/Ethnicity | ||||
| White | 117 (60.9%) | 79 (64.8%) | 38 (54.3%) | .15 |
| Black | 52 (27.1%) | 24 (19.7%) | 28 (40.0%) | |
| Hispanic | 13 (6.8%) | 9 (7.4%) | 4 (5.7%) | |
| Non-hispanic biracial | 10 (5.2%) | 10 (8.2%) | 0 (0%) | |
| Caregiver education (% < high school graduation)b | 79 (42.2%) | 48 (40.0%) | 31 (46.3%) | .41 |
| Child maltreatment historyc | 48 (25.3%) | 20 (10.5%) | 28 (14.7%) | <.001 |
| BMI (presurgery/baseline) | 50.06 ± 8.01 | 52.09 ± 8.40 | 46.53 ± 5.83 | <.001 |
| Surgical procedure | ||||
| Roux-en-Y gastric bypass | — | 78 (63.9%) | — | — |
| Sleeve gastrectomy | — | 41 (33.6%) | — | — |
| Adjustable gastric band | — | 3 (2.5%) | — | — |
| Year 1 | n = 171 | n = 114 | n = 57 | |
| BMI | 40.04 ± 9.29 | 36.08 ± 7.89 | 47.89 ± 6.46 | <.001 |
| % change in weight | — | −30.91 ± 8.54 | 4.86 ± 9.60 | <.001 |
| Year 2 | n = 192 | n = 122 | n = 70 | |
| BMId | 40.75 ± 10.52 | 36.27 ± 8.71 | 48.84 ± 8.53 | <.001 |
| Psychiatric medication | 46 (24.5%) | 24 (12.8%) | 22 (11.7%) | .09 |
| % change in weighte | — | −30.01 ± 11.36 | 7.35 ± 10.70 | <.001 |
| Year 4 | n = 159 | n = 103 | n = 56 | |
| Age | 20.96 ± 1.39 | 21.17 ± 1.36 | 20.52 ± 1.39 | .01 |
| BMIf | 42.02 ± 11.49 | 39.04 ± 10.66 | 48.05 ± 10.83 | <.001 |
| % change in weightg | — | −24.12 ± 15.78 | 6.08 ± 17.40 | <.001 |
| Psychiatric medicationh | — | 21 (21.4%) | — | — |
| Psychiatric hospitalizationh | — | 3 (3.1%) | — | — |
| Outpatient mental healthh | — | 18 (18.4%) | — | — |
| In school or workingi | 128 (78.0%) | 88 (53.7%) | 40 (24.4%) | .24 |
| Living with parent(s) or other relativesj | 117 (71.3%) | 76 (46.3%) | 41 (25.0%) | .52 |
Note. BMI = body mass index.
p-values are based on two-tailed independent t-tests when examining mean values and on Chi-square tests when examining percentages. p-value for Race/Ethnicity based on examination of White versus other race/ethnicity groupings, due to sample size in respective groups.
Missing for n = 2 surgical and n = 3 nonsurgical.
Child maltreatment based on report on Child Trauma Questionnaire-Short Form completed at baseline; frequencies and percents indicate at least one maltreatment scale in the moderate clinical range.
Missing for n = 10 surgical and n = 8 nonsurgical; n = 5 self-report nonsurgical.
((weight24-months − weightpresurgery/baseline)/weightpresurgery/baseline)*100; Missing for n = 6 surgical and n = 8 nonsurgical.
Missing for n = 4 nonsurgical and n = 11 surgical; n = 52 self-report nonsurgical, n = 5 self-report surgical.
((weight48-months − weightpresurgery/baseline)/weightpresurgery/baseline)*100; Missing for n = 4 nonsurgical.
Missing for n = 6 surgical.
Missing for n = 1 nonsurgical.
Missing for n = 3 surgical and n = 1 nonsurgical.
Aim 1 (Psychopathology Status by Surgical/Nonsurgical Group)
Most participants remained in the same psychopathology status grouping across timepoints. Participants in the surgical group generally had persistently low psychopathology while those in the nonsurgical group generally had more deterioration in psychopathology (Supplementary Table 4). Results of logistic regressions to determine associations of group (surgical vs. nonsurgical) with psychopathology status (“high” vs. “low”) indicated that participants in the surgical group had significantly lower odds of high internalizing status relative to the nonsurgical group both across all timepoints (baseline to Year 4; OR = .39; p < .001; e.g., 42.3% high internalizing for surgical; 66.7% high internalizing for nonsurgical) and during the 2–4 years of maintenance phase (OR = 0.35, p < .05; e.g., 35.1% high internalizing for surgical; 60.8% high internalizing for nonsurgical). There were no significant associations between group with externalizing status, either across all timepoints or in the 2–4 year maintenance phase (Table II).
Table II.
Associations of Surgical Group (Surgical vs. Nonsurgical) With Psychopathology Status
| Surgical (%) | Nonsurgical (%) | OR | 95% CI OR | B | p | |
|---|---|---|---|---|---|---|
| Baseline to Year 4 | ||||||
| High internalizing | 42.3 | 66.7 | 0.39 | 0.24–0.66 | −0.92 | <.001 |
| High externalizing | 25.8 | 43.1 | 0.68 | 0.26–1.79 | −0.38 | 0.44 |
| Year 2 to Year 4 maintenance phase | ||||||
| High internalizing | 35.1 | 60.8 | 0.35 | 0.19–0.64 | −1.07 | .001 |
| High Externalizing | 19.6 | 35.3 | 0.64 | 0.30–1.37 | −0.44 | 0.25 |
Note. OR = odds ratio. CI = confidence interval. Results of logistic regression analyses reflect likelihood of surgical group experiencing high psychopathology symptoms, as compared to nonsurgical group. Logistic regressions controlled for sex, race/ethnicity, age, caregiver education, baseline BMI, and history of child maltreatment. Bolded values indicate significant associations.
Aim 2 (Changes in BMI over Time by Psychopathology Status)
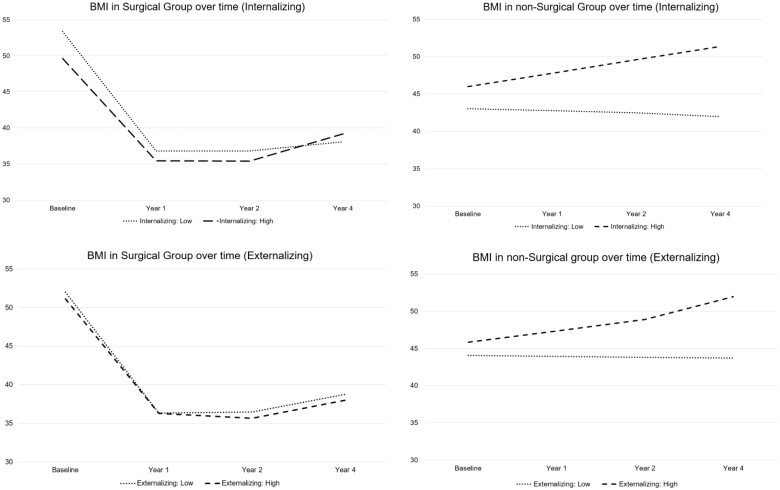
Growth curve models were used to test for changes in BMI over time (baseline, Years 1, 2, and 4) by psychopathology status for the surgical and nonsurgical groups separately (Figure 1). For the surgical group, the slope of BMI over time was quadratic, with all results for the status by time interaction for slope nonsignificant, indicating that change in BMI did not differ between high versus low psychopathology status (internalizing and externalizing). Moreover, intercepts did not differ significantly by psychopathology status, indicating that surgical participants of high- and low-status groups had similar BMI at baseline. For the nonsurgical group, no quadratic effects were found so models were rerun testing for linear effects which were also nonsignificant. For internalizing and externalizing psychopathology, status by time interactions for BMI slope and status differences for intercepts were nonsignificant, indicating that BMI did not differ by high versus low internalizing or externalizing status.
Figure 1.
Slopes of BMI for surgical and nonsurgical groups from Baseline to Year 4. Regression equations for surgical group: Internalizing (low): Y = 3.95x2 − 22.33x + 57.78; Internalizing (high): Y = 3.83x2 − 21.02x + 55.05; Externalizing (low): Y = 3.99x2—22.36x + 58.88; Externalizing (high): Y = 3.88x2 − 22.05x + 56.08. Regression equations for nonsurgical group: Internalizing (low): Y = −.27x + 43.05; Internalizing (high): Y = 1.79X + 46.01; Externalizing (low): Y = −.12x + 44.07; Externalizing (high): Y = 1.53x + 45.84.
Aim 3 (Direct and Indirect Effects of Dysregulation on Percent Weight Loss)
Results of mediation models for the surgical group are presented in Table III and Supplementary Figure 2. There was a significant direct effect of dysregulation at Year 2 on internalizing symptoms at Year 4 (β = .41, p < .001), a significant direct effect of internalizing symptoms at Year 4 on percent weight loss at Year 4 (β = −.27, p < .05), and a total significant indirect effect of dysregulation on percent weight loss though internalizing psychopathology (β = −.11, p < .05). Internalizing symptoms attenuated the association of dysregulation and percent weight loss by 85%. Models examining externalizing symptoms as a mediator included a significant direct effect of dysregulation at Year 2 on externalizing symptoms at Year 4 (β = .51, p < .001), but no significant associations with percent weight loss or a significant indirect effect.
Table III.
Mediation Analyses Testing the Indirect Effects of Dysregulation (Year 2) on Percent Weight Loss Through Psychopathology (Internalizing and Externalizing) at Year 4 for Adolescents who Underwent Bariatric Surgery
| β (standardized) |
Indirect effect (B, 95% CI) | ||||
|---|---|---|---|---|---|
| Mediational models | a | b | c | R 2 | |
| Dysregulation/percent weight loss through internalizing | .405*** | −.265* | .129 | −.047* (−.484 to .153) | .164** |
| Dysregulation/percent weight loss through externalizing | .507*** | −.132 | .090 | −.030 (−.083 to .114) | .257* |
Note. Mediation models controlled for sex. Models demonstrated acceptable model fit (SRMR: .021–.053) Internalizing, Externalizing, and Total Psychopathology symptoms were measured continuously at Year 4. Dysregulation measured at Year 2. Pathways: a = (dysregulation → psychopathology); b = (psychopathology → percent weight loss); c = (dysregulation → percent weight loss).
p < .05.
p < .01.
p < .001.
Discussion
The purpose of this study was to understand trajectories of psychopathology and weight change following bariatric surgery for adolescents, with specific attention to the role of dysregulation during the 2–4 years postsurgery period. Overall, results indicate that persistent internalizing psychopathology appears to play an important role in the 4 years following surgery for this age group. While the focus is on the surgical group, the inclusion of a nonsurgical group provides a unique view of longitudinal trajectories of adolescents with obesity who have undergone bariatric surgery compared with those who have not had bariatric surgery.
Extending our work at Year 2 (Hunsaker et al., 2018), the majority of adolescents in both groups maintained their psychopathology status (e.g., High vs. Low) over time, when followed longer. Adolescents in the surgical group were less likely to experience deteriorating psychopathology across all timepoints (0–4 years) and during the maintenance phase (2–4 years), as compared to those in the nonsurgical group. Moreover, internalizing psychopathology specifically was more persistent in the nonsurgical group as compared to the surgical group, both in the maintenance phase and across all timepoints. In other words, participants in the surgical group were significantly more likely to meet the criteria for “low” psychopathology at Year 4 as compared to the nonsurgical group. These findings fit with the existing evidence that psychopathology tends to persist for youth with overweight and obesity (Xie et al., 2013) as well as those who have undergone bariatric surgery (Hunsaker et al., 2018). Even after some initial improvements in internalizing symptoms within the year following surgery, the current findings further support the majority of evidence suggesting symptoms tend to increase again at longer-term follow-up (e.g., 2 years and on; Herget et al., 2014; Järvholm et al., 2016). It is possible that improvements in weight-related and health-related quality of life attributable to bariatric surgery improved some internalizing symptoms in the surgical group, yet these symptoms continue to emerge as persistent in the nonsurgical group who likely did not observe similar improvements in quality of life (Trooboff et al., 2019). These findings may also point to the persistent nature of internalizing symptoms generally, regardless of weight-related factors.
For the surgical group, change in BMI (across all timepoints and in the 2–4 years of maintenance period) was unrelated to psychopathology status; therefore the second hypothesis was not supported. It is possible that the expected associations of higher psychopathology symptoms with less weight loss and more weight gain in the 2–4 year maintenance phase was not observed due to the strong and expected effect of bariatric surgery on trends in BMI. This suggests that any effects of psychopathology in the surgical group were not enough to influence weight trajectories on a group level. Moreover, a trend of accelerated weight loss in the first year, continued decelerated weight loss in the second year, and some weight recurrence in the second year and on, can overall be expected regardless of psychopathology (Zeller et al., 2017). In contrast, though nonsignificant, participants with “High” total psychopathology symptoms in the nonsurgical group experienced more weight gain over time than those with “Low” total psychopathology symptoms. These findings fit with the current literature linking psychopathology with obesity and increased weight trajectories in youth (Bohnert et al., 2020). Moreover, this may especially be expected if individuals had low engagement with both behavorial weight management and mental health resources, or experienced eating-related psychopathology, such as loss of control eating (Decker et al., 2022; Hunsaker et al., 2018). Still, it is important to acknowledge that psychopathology may play a minimal role in weight trajectories overall for some adolescents.
As expected, psychological dysregulation at Year 2 and psychopathology were closely related. For the surgical group only, dysregulation on its own was not significantly related to percent weight loss; rather, internalizing psychopathology was a sole significant mediator that carried the effect of dysregulation at Year 2 on percent weight loss. Internalizing psychopathology attenuated the relationship between dysregulation and percent weight loss by 85%. Results support the conceptualization of psychological dysregulation as a more stable, dispositional factor that can influence both psychopathology and weight-related outcomes (Lavender et al., 2020). In other words, dysregulation on its own can be considered less predictive of BMI change. Rather, dysregulation may be a “personality factor” of interest that can influence persistent psychopathology, which may have more robust effects on weight trajectories following bariatric surgery in adolescents. Future work should focus on more specific application of dysregulation measurement and treatment in the context of obesity treatment.
Study Strengths and Limitations
The use of a nonsurgical comparison group is a strength of this study, allowing comparisons of longitudinal trajectories of adolescents who have undergone bariatric surgery with those with severe obesity who did not undergo bariatric surgery. The study is limited by sample size, which placed restrictions on some analyses, including the ability to detect differences in the surgical versus nonsurgical groups in the relationships of interest. The lack of diversity in the sample is an important limitation to this study as well as the existing literature in adolescent bariatric surgery. The sample is predominantly White and female, which limits generalizability to other demographics that continue to be underserved in obesity treatment and reflects the disparities in adolescent bariatric surgery (Bouchard et al., 2022). For example, Lopez et al. (2017), provide an excellent model for studying bariatric surgery outcomes in more diverse patient populations, continuing to find that Black and Hispanic/Latinx adolescents undergo bariatric surgery at lower rates as compared to White adolescents due to race/ethnicity-based disparities. This study also found that adolescent males had higher BMI and rates of obstructive sleep apnea and dyslipidemia preoperatively, but surgery outcomes did not differ for male versus female adolescents (Lopez et al., 2017). Overall, there are still a range of individual factors that affect weight trajectories even while controlling for all relevant covariates. Past literature also suggests that dysregulation may manifest differently in adolescents as compared to young adults (Gowey et al., 2016), which was not explored in the present study. Additionally, reported use of psychiatric medications at Year 4 was limited to the surgical group only; therefore we could not control for this as a covariate throughout the analyses. We did not have information on rates of diagnosed mental health conditions in this study, and future studies should include a clinical interview to determine diagnoses. The present study also used the broadband scales of Internalizing and Externalizing psychopathology as a first step to examine the trajectories of interest. Future work should look at more specific subscales (e.g., anxiety and depression) to better understand the relationships between psychopathology symptom presentation and weight trajectories.
Clinical Implications
Findings from our research team (Hunsaker et al., 2018, Zeller et al., 2017) and the AMOS study (Järvholm et al., 2015) were the first to provide evidence that mental health symptomology may not improve on its own after adolescent bariatric surgery. Continued research indicates that along with benefits for weight-related health and quality of life, bariatric surgery may introduce psychological challenges for adolescents. Particularly, persistent internalizing psychopathology and risk for suicidality should be assessed long-term postoperatively beyond the 2–4 year maintenance phase (Zeller et al., 2020). Indeed, there is a tendency for psychopathology symptoms to improve following surgery, yet deteriorate again as postoperative years progress, confirming the need for long-term access to mental health services for adolescents transitioning to young adulthood. It may be impactful for future work to examine whether surgery is a particularly beneficial option for adolescents and young adults with both severe obesity and internalizing symptoms, as well as provide adolescents the services to sustain these improvements. Adolescents with severe obesity who did not undergo surgery may be at risk for psychopathology and additional work should focus on meeting the needs of this group through screening and access to mental health services. It is apparent that adolescents vary in trajectories of psychopathology and need for mental health services, and simultaneously, resources for long-term mental health follow-up remain limited. More universal implementation of a psychopathology screening and triage process during medical follow-up appointments for adolescent bariatric surgery may be needed. Moreover, there is a need to focus psychological assessment, treatment, and referral efforts especially to support needs of youth from diverse backgrounds presenting in the context of weight management.
It is also important to acknowledge that psychopathology was elevated in both the surgical and nonsurgical groups, and points to the need for screening, preventive efforts, and treatment access for all youth with obesity. The important role of a pediatric psychologist in bariatric surgery evaluation and consultation is detailed by Burton et al. (2020), who also acknowledge the need for services to expand to additionally focus on intervention for psychopathology in the context of adolescent bariatric surgery. Though implications are focused on adolescent bariatric surgery, findings from the present study may inform both continued research questions and clinical priorities for adolescents with severe obesity who have and have not undergone bariatric surgery as they transition into young adulthood.
Supplementary Material
Footnotes
See Majid et al. (2022) regarding existing definitions of weight recurrence, their limitations, and current recommendation to use “weight recurrence” in place of “weight regain.”
Contributor Information
Carolina M Bejarano, Division of Behavioral Medicine & Clinical Psychology, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA.
Marissa Gowey, Independent Scholar, Birmingham, AL, USA.
Jennifer Reiter-Purtill, Division of Behavioral Medicine & Clinical Psychology, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA.
Sanita Ley, Division of Behavioral Medicine & Clinical Psychology, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA; Department of Pediatrics, University of Cincinnati College of Medicine, Cincinnati, OH, USA.
James E Mitchell, Department of Clinical Neuroscience, School of Medicine and Health Sciences, University of North Dakota, Grand Forks, North Dakota, USA.
Meg H Zeller, Division of Behavioral Medicine & Clinical Psychology, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA; Department of Pediatrics, University of Cincinnati College of Medicine, Cincinnati, OH, USA.
Supplementary Data
Supplementary data can be found at: https://academic.oup.com/jpepsy.
Funding
The TeenView ancillary studies (R01DK080020 and R01DA033415; PI: Zeller) were conducted in collaboration with the Teen-LABS Consortium, funded by cooperative agreements with the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): U01DK072493, UM1DK072493, and UM1DK095710 (University of Cincinnati). The first author’s effort was supported by an NIH post-doctoral training grant (T32 DK063929).
Conflicts of interest: None declared.
Author Contributions
Carolina Bejarano (Conceptualization [equal], Formal analysis [equal], Writing—original draft [lead], Writing—review & editing [lead]), Marissa Gowey (Conceptualization [equal], Supervision [equal], Writing—original draft [supporting], Writing—review & editing [supporting]), Jennifer Reiter-Purtill (Conceptualization [equal], Data curation [equal], Formal analysis [lead], Investigation [equal], Project administration [equal], Supervision [equal], Visualization [equal], Writing—original draft [supporting], Writing—review & editing [supporting]), Sanita Ley (Supervision [equal], Writing—original draft [supporting], Writing—review & editing [supporting]), James Mitchell (Investigation [equal], Supervision [equal], Writing—original draft [supporting], Writing—review & editing [supporting]), and Meg H. Zeller (Conceptualization [equal], Data curation [equal], Formal analysis [equal], Funding acquisition [equal], Investigation [equal], Methodology [equal], Supervision [equal], Writing—original draft [equal], Writing—review & editing [equal]).
References
- Achenbach T. M., Rescorla L. (2001). Manual for the Aseba School-Age Forms & Profiles: An Integrated System of Multi-informant Assessment. ASEBA. [Google Scholar]
- Armstrong S. C., Bolling C. F., Michalsky M. P., Reichard K. W., Haemer M. A., Muth N. D., Rausch J. C., Rogers V. W., Heiss K. F., Besner G. E., Downard C. D., Fallat M. E., Gow K. W., Facs M. D., SECTION ON OBESITY, SECTION ON SURGERY (2019). Pediatric metabolic and bariatric surgery: Evidence, barriers, and best practices. Pediatrics, 144(6) 10.1542/peds.2019-3223 [DOI] [PubMed] [Google Scholar]
- Beauchaine T. P. (2015). Future directions in emotion dysregulation and youth psychopathology. Journal of Clinical Child and Adolescent Psychology: The Official Journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53, 44(5), 875–896. 10.1080/15374416.2015.1038827 [DOI] [PubMed] [Google Scholar]
- Bernstein D. P., Stein J. A., Newcomb M. D., Walker E., Pogge D., Ahluvalia T., Stokes J., Handelsman L., Medrano M., Desmond D., Zule W. (2003). Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect, 27(2), 169–190. 10.1016/S0145-2134(02)00541-0 [DOI] [PubMed] [Google Scholar]
- Bohnert A. M., Loren D. M., Miller A. L. (2020). Examining childhood obesity through the lens of developmental psychopathology: Framing the issues to guide best practices in research and intervention. The American Psychologist, 75(2), 163–177. [DOI] [PubMed] [Google Scholar]
- Bouchard M. E., Tian Y., Linton S., De Boer C., O'Connor A., Ghomrawi H., Abdullah F. (2022). Utilization trends and disparities in adolescent bariatric surgery in the United States 2009–2017. Childhood Obesity (Print), 18(3), 188–196. [DOI] [PubMed] [Google Scholar]
- Burton E. T., Mackey E. R., Reynolds K., Cadieux A., Gaffka B. J., Shaffer L. A. (2020). Psychopathology and adolescent bariatric surgery: A topical review to support psychologists in assessment and treatment considerations. Journal of Clinical Psychology in Medical Settings, 27(2), 235–246. [DOI] [PubMed] [Google Scholar]
- Decker K. M., Reiter‐Purtill J., Bejarano C. M., Goldschmidt A. B., Mitchell J. E., Jenkins T. M., Helmrath M., Inge T. H., Michalsky M. P., Zeller M. H. (2022). Psychosocial predictors of problematic eating in young adults who underwent adolescent bariatric surgery. Obesity Science & Practice, 8(5), 545–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gowey M. A., Reiter-Purtill J., Becnel J., Peugh J., Mitchell J. E., Zeller M. H, TeenView Study Group. (2016). Weight-related correlates of psychological dysregulation in adolescent and young adult (AYA) females with severe obesity. Appetite, 99, 211–218. 10.1016/j.appet.2016.01.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herget S., Rudolph A., Hilbert A., Blüher S. (2014). Psychosocial status and mental health in adolescents before and after bariatric surgery: A systematic literature review. Obesity Facts, 7(4), 233–245. 10.1159/000365793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunsaker S. L., Garland B. H., Rofey D., Reiter-Purtill J., Mitchell J., Courcoulas A., Jenkins T. M., Zeller M. H. (2018). Correlates among adolescents who did or did not undergo weight loss surgery. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 63(2), 142–150. 10.1016/j.jadohealth.2017.12.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inge T. H., Courcoulas A. P., Jenkins T. M., Michalsky M. P., Helmrath M. A., Brandt M. L., Harmon C. M., Zeller M. H., Chen M. K., Xanthakos S. A., Horlick M., Buncher C. R, Teen-LABS Consortium (2016). Weight loss and health status 3 years after bariatric surgery in adolescents. New England Journal of Medicine, 374(2), 113–123. 10.1056/nejmoa1506699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inge T. H., Jenkins T. M., Xanthakos S. A., Dixon J. B., Daniels S. R., Zeller M. H., Helmrath M. A. (2017). Long-term outcomes of bariatric surgery in adolescents with severe obesity (FABS-5+): A prospective follow-up analysis. The Lancet. Diabetes & Endocrinology, 5(3), 165–173. 10.1016/s2213-8587(16)30315-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Javaras K. N., Armstrong J. M., Klein M. H., Essex M. J., Davidson R. J., Goldsmith H. H. (2020). Sex differences in the relationship between childhood self‐regulation and adolescent adiposity. Obesity (Silver Spring, MD), 28(9), 1761–1769. 10.1002/oby.22926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Järvholm K., Bruze G., Peltonen M., Marcus C., Flodmark C.-E., Henfridsson P., Beamish A. J., Gronowitz E., Dahlgren J., Karlsson J., Olbers T. (2020). 5-year mental health and eating pattern outcomes following bariatric surgery in adolescents: a prospective cohort study. The Lancet. Child & Adolescent Health, 4(3), 210–219. 10.1016/s2352-4642(20)30024-9 [DOI] [PubMed] [Google Scholar]
- Järvholm K., Karlsson J., Olbers T., Peltonen M., Marcus C., Dahlgren J., Gronowitz E., Johnsson P., Flodmark C.-E. (2015). Two‐year trends in psychological outcomes after gastric bypass in adolescents with severe obesity. Obesity (Silver Spring, MD), 23(10), 1966–1972. 10.1002/oby.21188 [DOI] [PubMed] [Google Scholar]
- Järvholm K., Karlsson J., Olbers T., Peltonen M., Marcus C., Dahlgren J., Gronowitz E., Johnsson P., Flodmark C.-E. (2016). Characteristics of adolescents with poor mental health after bariatric surgery. Surgery for Obesity and Related Diseases: Official Journal of the American Society for Bariatric Surgery, 12(4), 882–890. 10.1016/j.soard.2016.02.001 [DOI] [PubMed] [Google Scholar]
- Järvholm K., Olbers T., Marcus C., Mårild S., Gronowitz E., Friberg P., Johnsson P., Flodmark C.-E. (2012). Short‐term psychological outcomes in severely obese adolescents after bariatric surgery. Obesity (Silver Spring, MD), 20(2), 318–323. 10.1038/oby.2011.310 [DOI] [PubMed] [Google Scholar]
- Kessler R. C., Berglund P., Demler O., Jin R., Merikangas K. R., Walters E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602. [DOI] [PubMed] [Google Scholar]
- Lavender J. M., King W. C., Kalarchian M. A., Devlin M. J., Hinerman A., Gunstad J., Marcus M. D., Mitchell J. E. (2020). Examining emotion-, personality-, and reward-related dispositional tendencies in relation to eating pathology and weight change over seven years in the Longitudinal Assessment of Bariatric Surgery (LABS) study. Journal of Psychiatric Research, 120, 124–130. 10.1016/j.jpsychires.2019.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez O. N., Jupiter D. C., Bohanon F. J., Radhakrishnan R. S., Bowen-Jallow K. A. (2017). Health disparities in adolescent bariatric surgery: Nationwide outcomes and utilization. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 61(5), 649–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majid S. F., Davis M. J., Ajmal S., Podkameni D., Jain-Spangler K., Guerron A. D., King N., Voellinger D. C., Northup C. J., Kennedy C., Archer S. B. (2022). Current state of the definition and terminology related to weight recurrence after metabolic surgery: Review by the POWER Task Force of the ASMBS. Surgery for Obesity and Related Diseases, 18(7), 957–963. 10.1016/j.soard.2022.04.012 [DOI] [PubMed] [Google Scholar]
- McLaughlin K. A., Hatzenbuehler M. L., Mennin D. S., Nolen-Hoeksema S. (2011). Emotion dysregulation and adolescent psychopathology: A prospective study. Behaviour Research and Therapy, 49(9), 544–554. 10.1016/j.brat.2011.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mezzich A. C., , TarterR. E., , GiancolaP. R., & , Kirisci L. (2001). The Dysregulation Inventory: A New Scale to Assess the Risk for Substance Use Disorder. Journal of Child & Adolescent Substance Abuse, 10(4), 35–43. 10.1300/J029v10n04_04 [DOI] [Google Scholar]
- Swinburn B. A., Sacks G., Hall K. D., McPherson K., Finegood D. T., Moodie M. L., Gortmaker S. L. (2011). The global obesity pandemic: Shaped by global drivers and local environments. Lancet (London, England), 378(9793), 804–814. 10.1016/s0140-6736(11)60813-1 [DOI] [PubMed] [Google Scholar]
- Trooboff S. W., Stucke R. S., Riblet N. B., Kulkarni A. S., Anand R., Casey A., Hofley M. A. (2019). Psychosocial outcomes following adolescent metabolic and bariatric surgery: A systematic review and meta-analysis. Obesity Surgery, 29(11), 3653–3664. 10.1007/s11695-019-04048-3 [DOI] [PubMed] [Google Scholar]
- Xie B., Ishibashi K., Lin C., Peterson D. V., Susman E. J. (2013). Overweight trajectories and psychosocial adjustment among adolescents. Preventive Medicine, 57(6), 837–843. 10.1016/j.ypmed.2013.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeller M. H., Brown J. L., Reiter-Purtill J., Sarwer D. B., Black L., Jenkins T. M., McCracken K. A., Courcoulas A. P., Inge T. H., Noll J. G, Teen-LABS Consortium (2019). Sexual behaviors, risks, and sexual health outcomes for adolescent females following bariatric surgery. Surgery for Obesity and Related Diseases, 15(6), 969–978. 10.1016/j.soard.2019.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeller M. H., Modi A. C., Noll J. G., Long J. D., Inge T. H. (2009). Psychosocial functioning improves following adolescent bariatric surgery. Obesity, 17(5), 985–990. 10.1038/oby.2008.644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeller M. H., Noll J. G., Sarwer D. B., Reiter-Purtill J., Rofey D. L., Baughcum A. E., Peugh J., Courcoulas A. P., Michalsky M. P., Jenkins T. M., Becnel J. N. & TeenView Study Group and in Cooperation With Teen-LABS Consortium. (2015). Child maltreatment and the adolescent patient with severe obesity: Implications for clinical care. Journal of Pediatric Psychology, 40(7), 640–648. 10.1093/jpepsy/jsv011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeller M. H., Pendery E. C., Reiter-Purtill J., Hunsaker S. L., Jenkins T. M., Helmrath M. A., Inge T. H. (2017). From adolescence to young adulthood: Trajectories of psychosocial health following Roux-en-Y gastric bypass. Surgery for Obesity and Related Diseases, 13(7), 1196–1203. 10.1016/j.soard.2017.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeller M. H., Reiter-Purtill J., Jenkins T. M., Kidwell K. M., Bensman H. E., Mitchell J. E., Courcoulas A. P., Inge T. H., Ley S. L., Gordon K. H., Chaves E. A., Washington G. A., Austin H. M., Rofey D. L. (2020). Suicidal thoughts and behaviors in adolescents who underwent bariatric surgery. Surgery for Obesity and Related Diseases, 16(4), 568–580. 10.1016/j.soard.2019.12.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeller M. H., Reiter-Purtill J., Ratcliff M. B., Inge T. H., Noll J. G. (2011). Two-year trends in psychosocial functioning after adolescent Roux-en-Y gastric bypass. Surgery for Obesity and Related Diseases, 7(6), 727–732. 10.1016/j.soard.2011.01.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.