Abstract
Background:
Animal and experimental studies suggest circadian disruption increases colorectal cancer risk, but evidence in humans is limited. We examined night shift work, chronotype, and residential position within a time zone, proxies for circadian disruption, in relation to colorectal cancer risk.
Methods:
Participants in the Black Women’s Health Study, a prospective cohort of 59,000 Black American women established in 1995, reported history of night shift work and chronotype on follow-up questionnaires. Residential position within a time zone was estimated using participant addresses at each questionnaire cycle. Number of colorectal cancer cases and follow-up duration varied by analysis depending on timing of exposure assessment, ranging from 204 over the 2005–2018 night shift work study period to 452 over the 1995–2018 residential position study period. Cox proportional hazards regression was used to estimate multivariable-adjusted hazard ratios (HR) and 95% confidence intervals (CI).
Results:
Compared to never having worked a night shift, working a night shift for ≥10 years was associated with increased colorectal cancer risk (HR=1.64, 95% CI 1.01–2.66). However, shorter duration was not. The HR for evening vs. morning chronotype was 0.96 (95% CI 0.73–1.27). Westward position of residence within a time zone was not associated with colorectal cancer risk (HR per 5-degree longitude increase: 0.92, 95% CI 0.82–1.03).
Conclusions:
Our findings suggest a possible increased risk of colorectal cancer associated with long duration night shift work; however, results require confirmation in larger studies.
Impact:
Circadian disruption from long-term night shift work may contribute to colorectal cancer development in Black women.
Keywords: Circadian disruption, Night shift work, Chronotype, Colorectal cancer, Black Women
INTRODUCTION
Humans have an internal circadian rhythm, roughly 24-hours in length, that plays a critical role in human functioning, regulating cellular, physiological, and behavioral processes such as cell cycle progression, DNA repair, and sleep/wake and feeding/fasting timing.1 External cues, such as sunlight, help synchronize the endogenous circadian clock to the 24-hour day.1 When an individual’s internal circadian rhythm and external cues do not align, circadian disruption or misalignment can occur. This disruption can increase inflammation, cellular stress, DNA damage, and immune and metabolic dysfunction.2 In both animal and human studies, circadian disruption has been linked to chronic diseases, including cancer.1,3–6 Because the circadian system regulates cellular and physiological processes in the large bowel,7,8 circadian disruption has been studied as a potential risk factor for colorectal cancer, the third most commonly diagnosed cancer in the United States (US).
Circadian disruption can be exemplified in many ways. A commonly studied exemplification is night shift work.1 Based on experimental, animal, and human evidence, the International Agency for Research on Cancer (IARC) declared night shift work as a Group 2A probable carcinogen in 2019.9 However, IARC acknowledged that the human evidence linking night shift work to cancer incidence was limited and inconsistent, particularly for colorectal cancer. In line with their assessment, an early meta-analysis reported positive associations between ever having worked a night shift, longer duration of night shift work, and colorectal cancer incidence,10 but an updated meta-analysis reported no association.11
In addition to night shift work, seemingly innocuous factors may also lead to misalignment relevant to human health. For instance, a late chronotype (preference for evening activities rather than morning activities) is often incompatible with early work/school schedules and could lead to misalignment. Additionally, residing in the western part of a time zone, where the sun rises and sets at a later time compared to the eastern part of the time zone, can lead to misalignment between one’s internal circadian rhythm and the defined clock/social time, leading to chronic circadian disruption.12 Chronotype13–15 and residential position in a time zone5,16,17 have been associated with increased risk of some cancers, but their relationship with colorectal cancer remains unclear. No prior study, to our knowledge, has examined the relation of chronotype with colorectal cancer risk. In an ecologic study of White Americans, a 5-degree longitude increase in westward position of residence within a time zone was associated with an increased risk of colorectal cancer.16 However, the authors were unable to prospectively assess the association, control for individual-level confounding, or account for changes in residential location.
Given the limited, inconsistent evidence and methodological limitations of prior studies, further research is needed to understand the impact of circadian disruption on colorectal cancer incidence. Moreover, associations should be assessed among underrepresented racial/ethnic groups who may have greater susceptibility to circadian disruption, such as Black Americans who tend to have shorter endogenous circadian periods,18 sleep less,19 and often have less flexible work schedules.20
In the present study, we examined the relation of circadian disruption, measured as night shift work, chronotype, and residential position within a time zone, with risk of colorectal cancer within a large prospective study of Black American women with over 20 years of follow-up.
MATERIALS AND METHODS
Study Population and Design
Approximately 59,000 self-identified Black women from across the US were enrolled in the Black Women’s Health Study (BWHS) in 1995 upon receipt of a completed self-administered baseline questionnaire. Since 1995, BWHS participants have been followed through biennial questionnaires to collect data on lifestyle and behavioral factors and disease diagnoses. Participant follow-up is complete for 85% of potential person-years. Because of the timing of exposure assessment (see below), three separate analytic populations, each with distinct starts of follow-up, were defined (Supplemental Figures S1–S3).
Follow-up began in 2005 for the night shift work analysis. After excluding women who did not answer the 2005 questionnaire (n=15,845), had a prior cancer diagnosis (except non-melanoma skin cancer; n=2,520), or were missing data on night shift work (n=6,214), 34,421 BWHS participants remained in the analytic sample.
In the chronotype analysis, participants were considered for inclusion if they completed the 2015 questionnaire, which asked about chronotype (n=37,119). Available evidence indicates that chronotype is partly genetically determined,21 but is also influenced by other factors including geographic location,22 sex, and age.23 Chronotype can change with age, particularly during childhood and adolescence.24 During adulthood, chronotype tends to become earlier with increasing age. However, in women, chronotype changes relatively little after age 34.23 Therefore, in analyses that evaluated chronotype as the exposure variable, follow-up began either in 1995 or at age 35, when chronotype is expected to be more stable.23,24 Thus, BWHS participants who were ≥35 years old at study enrollment entered the chronotype analytic sample in 1995, while women who were younger than 35 at study enrollment entered into the analytic sample upon turning 35. Excluded were participants who had received a cancer diagnosis prior to 1995 or prior to turning age 35 (n=791) or who were missing data on chronotype (n=2,630). After exclusions, 33,698 women remained for analysis.
For the time zone analysis, follow-up began in 1995. Participants were excluded if they had a cancer diagnosis prior to 1995 (n=1,499) or if they were missing data on residential position at every questionnaire cycle (e.g., unable to be geocoded; n=1,098). After exclusions, 56,403 participants remained in the analytic sample.
Exposure Assessment
On the 2005 questionnaire, participants reported ever working a night shift (yes, no), as well as frequency (“Never”, “Once a year”, “A couple times a year”, “Once a month”, “Every week”) and duration (years) of night shift work. We collapsed categories “Once a year”, “A couple times a year”, and “Once a month” in frequency of night shift work analyses. Duration of night shift work was assessed in four categories (never, <5, 5–9, ≥10 years) in primary analyses and three categories (never, <5, ≥5 years) in stratified analyses.
Participants reported their chronotype in categories on the 2015 questionnaire: “Definitely a morning type”, “More of a morning type”, “Definitely an evening type”, “More of an evening type”, “Neither a morning nor evening type”. The two morning and two evening categories were collapsed to create a three-level categorical variable. Because evidence suggests that chronotype is partly determined by genetics21 and changes little after age 35 for women,23,24 we assumed chronotype assessed in 2015 reflected participants’ chronotype throughout adulthood.
Residential position within a time zone was defined as the geodesic distance, the shortest distance between two points on a sphere, between the time zone meridian and a participant’s place of residence in degrees longitude. Participants’ address at each questionnaire cycle was obtained from mailings of baseline and follow-up questionnaires and was geocoded. Using a geographic information system and the Vincenty formula,25 which accounts for the Earth’s ellipsoid shape and variations in latitude as one moves north or south of the equator, we calculated the geodesic distance between participants’ geocoded address and the meridian of the time zone in which they lived. The Eastern, Central, Mountain, and Pacific time zone meridians are located at −75 degrees, −90 degrees, −105 degrees, and −120 degrees longitude, respectively (Figure 1). Residential positions that were located west of the specified time zone meridian were assigned a positive geodesic distance value, while residential positions located east of the time zone meridian were assigned a negative value. Therefore, the progression from negative to positive distance values within a time zone represented an east to west gradient. Residential position was updated at each biennial questionnaire cycle. Assessment of restricted cubic splines showed no evidence of non-linearity. Thus, we evaluated residential position as a continuous variable per 5-degree longitude increment in distance from the time zone meridian following an east to west gradient. ArcGIS Pro 2.7.0 (Esri) was used to conduct all spatial analyses.
Figure 1. Residential position of BWHS participants in the continental US, according to time zone.
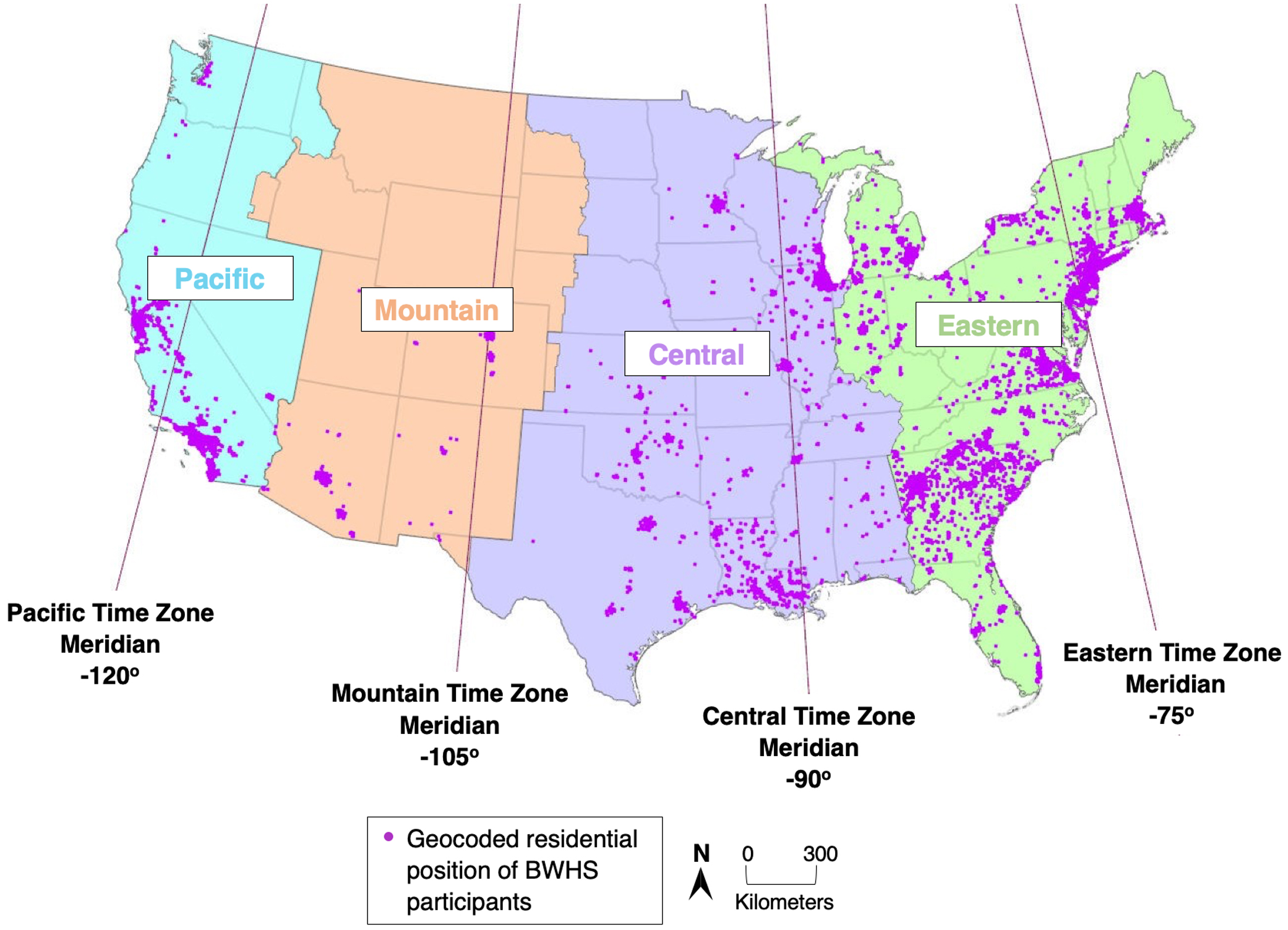
This map of the continental US depicts the four time zones (Eastern in green, Central in purple, Mountain in peach, and Pacific in blue) and the geocoded residential position of BWHS participants (purple dots) within the time zones at baseline in 1995. BWHS, Black Women’s Health Study; US, United States.
Outcome Ascertainment
Incident colorectal cancer was the outcome of interest. The International Classification of Diseases 10 (codes C18.0–C18.9 and C26.0 for colon and C19.9 and C20.0 for rectum) was used to define colon and rectal cancer. Participants self-reported colon or rectal cancer diagnoses on baseline and follow-up questionnaires. Diagnoses were also identified through linkage to state cancer registries and the National Death Index. Once participants were identified as having a colorectal cancer diagnosis, consent was obtained to access participants’ medical records and pathology reports. Diagnoses were confirmed and information on date of diagnosis and cancer subsite (colon, rectum) was collected through review of pathology reports and cancer registry data by trained study personnel who were blinded to exposure status.
Statistical Analysis
Cox proportional hazards regression was used to estimate age- and multivariable-adjusted hazard ratios (HR) and 95% confidence intervals (CI) for the separate associations of night shift work, chronotype, and residential position within a time zone with risk of colorectal cancer, overall and according to cancer subsite. Regression models in each analysis were stratified by age in one-year increments at the particular questionnaire cycle and time period, such that age was the underlying timescale.
In the night shift work analysis, participants began accruing follow-up time in 2005. In the chronotype analysis, each participant accrued follow-up time beginning in 1995 or upon turning age 35, whichever came last. In the time zone analysis, follow-up time accrual began in 1995. In all analyses, follow-up ended at the time of colorectal cancer diagnosis or diagnosis of another cancer, death, or end of the study period in 2018, whichever occurred first.
To control for potential confounding, we adjusted for the following established or suspected colorectal cancer risk factors in multivariable regression models: family history of colorectal cancer (yes, no), body mass index (BMI; <25, 25–29, 30–34, ≥35 kg/m2), smoking status (never, past, current), alcohol consumption (non-current, current 1–6, current ≥7 drinks/week), vigorous exercise (none, <5, ≥5 hours/week), and processed meat consumption (grams/day in quartiles). Education, red meat consumption, fiber intake, geographic region, neighborhood socioeconomic status, urbanicity, and sleep duration were also assessed as candidate covariates, but ultimately excluded from final regression models due to negligible changes in model estimates upon their inclusion. All covariates were updated at each questionnaire cycle. In stratified analyses, only age-adjusted results are presented because age- and multivariable-adjusted estimates were nearly identical, suggesting little evidence of confounding by covariates included in multivariable models.
Since Black Americans are more likely than other racial/ethnic groups to be diagnosed with early-onset colorectal cancer,26 we examined effect measure modification by age (<50, ≥50 years) in each analysis. Additionally, we investigated effect measure modification by US Census geographic region (Northeast, South, Midwest, West)27 in chronotype and residential position analyses since circadian disruption may vary by geography.22 We also examined effect measure modification by chronotype (morning, evening, neither a morning nor evening type) in the night shift work analysis, by BMI (<30, ≥30 kg/m2) and night shift work (never, ever) in the chronotype analysis, and by latitude (≤39, >39 degrees, median) in the time zone analysis.
Data availability
The data underlying this article cannot be shared publicly due to protection of Black Women’s Health Study participants’ privacy. The data will be shared on reasonable request to the corresponding author.
RESULTS
Table 1 displays baseline characteristics of the study population in the residential position within a time zone analysis (our largest analytic sample). The average residential position within a given time zone was 1.80 (standard deviation=4.1) degrees longitude west of the time zone meridian at study entry. The majority of participants lived in the Eastern time zone (63%). Participants were an average age of 39 years and an average BMI of 28.0 kg/m2 at study entry. None of the assessed covariates varied across quartiles of position of residence within a time zone (Supplemental Table S1). In Supplemental Table S2, baseline characteristics of the night shift work analytic sample are displayed. Approximately 43% of participants reported ever working a night shift. Of the night shift workers, 60% worked a night shift every week and 12% worked a night shift for ≥10 years. At study entry in 2005, women who ever worked a night shift were more likely to have a higher BMI, have twelve or fewer years of education, be a current smoker, and receive six or fewer hours of sleep. In the chronotype analysis, 56%, 31% and 13% of participants reported having a morning, evening, or neither morning nor evening chronotype, respectively. Population characteristics at study entry generally did not vary across chronotype categories (Supplemental Table S3).
Table 1.
Age-standardized characteristics of the study population for the residential position within a time zone analysis at baseline in 1995, N=56,403.a
| N | ||
|---|---|---|
|
| ||
| Mean (SD) | ||
| Age | 56,403 | 39.0 (10.8) |
| Body mass index, kg/m2 | 54,727 | 28.0 (6.7) |
| % | ||
| Years of education: ≤12 years | 10,721 | 19 |
| Family history of colorectal cancer | 5,185 | 9 |
| Smoking status: Current | 8,725 | 15 |
| Alcohol consumption: Current, ≥7 drinks/week | 3,778 | 7 |
| Vigorous exercise: ≥5 hours/week | 7,273 | 13 |
| Red meat consumption: Highest quartile | 12,650 | 22 |
| Processed meat consumption: Highest quartile | 12,689 | 22 |
| Total fiber intake: Highest quartile | 12,857 | 23 |
| Geographic region: | ||
| Northeast | 15,493 | 27 |
| South | 17,203 | 31 |
| Midwest | 13,273 | 24 |
| West | 10,432 | 18 |
| Sleep duration (ascertained in 2009): ≤6 hours | 16,958 | 45 |
| Night shift work (ascertained in 2005): | ||
| Never | 18,616 | 49 |
| Ever | 13,648 | 36 |
| Chronotype: | ||
| Morning | 18,568 | 33 |
| Evening | 10,434 | 18 |
| Neither morning nor evening | 4,266 | 8 |
Values are means (SD) or percentages and are standardized to the age distribution of the study population.
Night Shift Work
During the 2005–2018 study period, 204 colorectal cancer cases (150 colon, 46 rectal, 8 subsite unknown) were diagnosed among 34,421women. In both age- and multivariable-adjusted regression models, night shift work duration of ≥10 years was associated with an increased risk of colorectal cancer (multivariable-adjusted HR=1.64, 95% CI 1.01–2.66; Table 2) compared to never working a night shift. Estimates were similar for colon and rectal cancer. In contrast, compared to never working a night shift, ever having worked a night shift was not associated with overall colorectal cancer risk (multivariable-adjusted HR=1.13, 95% CI 0.86–1.50). Multivariable-adjusted HRs were 1.31 (95% CI 0.95–1.82) and 0.74 (95% CI 0.41–1.36) for colon and rectal cancer, respectively. There was no apparent trend for increased frequency of night shift work. The HR for working a weekly night shift for ≥5 years, a measure of exposure intensity, in relation to colorectal cancer risk was 1.47 (95% CI 0.94–2.28). Neither age nor chronotype modified the associations (Table 3).
Table 2.
Hazard ratios for the association between night shift work and risk of colorectal cancer, overall and by subsite.
| Overall colorectal cancer |
Colon cancer |
Rectal cancer |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Night shift work | Cases | Person-years | Age-adjusted HR (95% CI)a | MV-adjusted HR (95%CI)b | Cases | Person-years | Age-adjusted HR (95% CI)a | MV-adjusted HR (95%CI)b | Cases | Person-years | Age-adjusted HR (95% CI)a | MV-adjusted HR (95%CI)b |
|
| ||||||||||||
| Never | 108 | 225,486 | 1.00 (ref) | 1.00 (ref) | 74 | 225,445 | 1.00 (ref) | 1.00 (ref) | 29 | 225,406 | 1.00 (ref) | 1.00 (ref) |
| Ever | 96 | 168,300 | 1.17 (0.89–1.55) | 1.13 (0.86–1.50) | 76 | 168,276 | 1.35 (0.98–1.87) | 1.31 (0.95–1.82) | 17 | 168,206 | 0.76 (0.42–1.39) | 0.74 (0.41–1.36) |
| Frequency | ||||||||||||
| Once/yr to once/mo | 29 | 53,086 | 1.17 (0.78–1.77) | 1.15 (0.76–1.73) | 24 | 53,082 | 1.40 (0.88–2.22) | 1.38 (0.87–2.19) | 5 | 53,059 | 0.75 (0.29–1.95) | 0.72 (0.28–1.88) |
| Every week | 58 | 101,226 | 1.18 (0.86–1.63) | 1.13 (0.82–1.56) | 46 | 101,210 | 1.36 (0.94–1.97) | 1.31 (0.90–1.90) | 9 | 101,166 | 0.68 (0.32–1.44) | 0.66 (0.31–1.41) |
| Duration c | ||||||||||||
| <5 years | 56 | 111,235 | 1.09 (0.79–1.50) | 1.05 (0.76–1.45) | 46 | 111,223 | 1.30 (0.90–1.89) | 1.27 (0.87–1.83) | 8 | 111,175 | 0.57 (0.26–1.24) | 0.55 (0.25–1.22) |
| 5–9 year | 11 | 20,914 | 1.08 (0.58–2.02) | 1.04 (0.56–1.95) | 8 | 20,912 | 1.15 (0.55–2.38) | 1.10 (0.53–2.29) | d | – | – | – |
| ≥10 years | 20 | 20574 | 1.70 (1.05–2.75) | 1.64 (1.01–2.66) | 14 | 20567 | 1.69 (0.95–3.00) | 1.65 (0.92–2.94) | 5 | 20557 | 1.62 (0.62–4.20) | 1.63 (0.62–4.25) |
HR, Hazard ratio; CI, Confidence interval; MV, Multivariable; yr, year; mo, month.
Hazard ratios adjusted for age (continuous) and time period (continuous).
Hazard ratios additionally adjusted for family history of colorectal cancer (yes, no), body mass index (<25, 25–29, 30–34, ≥35 kg/m2), smoking status (never, past, current), alcohol consumption (non-current, current 1–6, current ≥7 drinks/week), vigorous physical activity (none, <5, ≥5 hours/week), and processed meat consumption (quartiles).
Reference group is never worked a night shift.
Hazard ratios are not presented for case counts <5.
Table 3.
Hazard ratios for the association between night shift work and risk of colorectal cancer, according to strata of age and chronotype.
| Age |
Chronotype |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| <50 years |
≥50 years |
Morning |
Evening |
Neither |
||||||
| Night shift work | Cases/PY | Age-adjusted HR (95% CI)a | Cases/PY | Age-adjusted HR (95% CI)a | Cases/PY | Age-adjusted HR (95% CI)a | Cases/PY | Age-adjusted HR (95% CI)a | Cases/PY | Age-adjusted HR (95% CI)a |
|
| ||||||||||
| Never | 22/91,893 | 1.00 (ref) | 86/133,593 | 1.00 (ref) | 46/101,220 | 1.00 (ref) | 22/53,772 | 1.00 (ref) | 7/22,407 | 1.00 (ref) |
| Ever | 17/64,009 | 1.12 (0.60–2.12) | 79/104,291 | 1.19 (0.87–1.61) | 31/70,328 | 0.97 (0.61–1.53) | 24/42,066 | 1.35 (0.75–2.42) | 6/16,288 | 1.05 (0.35–3.16) |
| Duration b | ||||||||||
| <5 years | 11/45,935 | 1.01 (0.49–2.07) | 45/65,300 | 1.11 (0.77–1.59) | 19/48,199 | 0.90 (0.53–1.55) | 16/27,724 | 1.42 (0.74–2.73) | c | – |
| ≥5 year | 5/12,880 | 1.69 (0.64–4.49) | 26/28,608 | 1.37 (0.88–2.13) | 8/15,426 | 1.08 (0.51–2.30) | 5/10,913 | 1.04 (0.39–2.77) | c | – |
PY, Person-years; HR, Hazard ratio; CI, Confidence interval.
Hazard ratios adjusted for age (continuous) and time period (continuous).
Reference group is never worked a night shift.
Hazard ratios are not presented for case counts <5.
Chronotype
During the 1995–2018 study period, 264 incident colorectal cancer cases (200 colon, 54 rectal, 10 subsite unknown) were reported among 33,698 women. Chronotype was not associated with risk of colorectal cancer in age- or multivariable-adjusted models: multivariable-adjusted HR=0.96, 95% CI 0.73–1.27 for evening vs. morning chronotype and HR=0.77, 95% CI 0.52–1.14 for neither morning nor evening vs. morning chronotype (Table 4). Multivariable-adjusted HRs for evening compared to morning chronotype were 0.90 (95% CI 0.65–1.24) and 1.48 (95% CI 0.85–2.59) for colon and rectal cancer, respectively. There was no evidence of an association between chronotype and colorectal cancer risk within strata defined by age, geographic region, BMI, or night shift work (Supplemental Table S4); however, sample sizes were small for some strata and estimates were imprecise.
Table 4.
Hazard ratios for the association between chronotype and risk of colorectal cancer, overall and by cancer subsite.
| Overall colorectal cancer |
Colon cancer |
Rectal cancer |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Exposure | Cases | Person-years | Age-adjusted HR (95% CI)a | MV-adjusted HR (95%CI)b | Cases | Person-years | Age-adjusted HR (95% CI)a | MV-adjusted HR (95%CI)b | Cases | Person-years | Age-adjusted HR (95% CI)a | MV-adjusted HR (95%CI)b |
|
| ||||||||||||
| Chronotype | ||||||||||||
| Morning | 156 | 352,888 | 1.00 (ref) | 1.00 (ref) | 119 | 352,840 | 1.00 (ref) | 1.00 (ref) | 29 | 352,754 | 1.00 (ref) | 1.00 (ref) |
| Evening | 78 | 190,913 | 0.98 (0.74–1.28) | 0.96 (0.73–1.27) | 55 | 190,886 | 0.92 (0.67–1.27) | 0.90 (0.65–1.24) | 22 | 190,853 | 1.46 (0.84–2.55) | 1.48 (0.85–2.59) |
| Neither morning nor evening | 30 | 80,984 | 0.78 (0.52–1.15) | 0.77 (0.52–1.14) | 26 | 80,981 | 0.87 (0.57–1.33) | 0.86 (0.56–1.31) | c | – | – | – |
HR, Hazard ratio; CI, Confidence interval; MV, Multivariable.
Hazard ratios adjusted for age (continuous) and time period (continuous).
Hazard ratios additionally adjusted for family history of colorectal cancer (yes, no), body mass index (<25, 25–29, 30–34, ≥35 kg/m2), smoking status (never, past, current), alcohol consumption (non-current, current 1–6, current ≥7 drinks/week), vigorous physical activity (none, <5, ≥5 hours/week), and processed meat consumption (quartiles).
Hazard ratios are not presented for case counts <5.
Residential Position within a Time Zone
Over follow-up from 1995 through 2018, 452 incident colorectal cancer cases occurred among 56,403 women. Of these, 343 were colon cancers, 99 were rectal cancers, and 10 were of unknown cancer subsite. There was no association between position of residence within a time zone and risk of colorectal cancer in age- or multivariable-adjusted regression models (multivariable-adjusted HR per 5-degree longitude increase in westward position=0.92, 95% CI 0.82–1.03; Table 5). A similar null association was found for risk of colon cancer (multivariable-adjusted HR=0.98, 95% CI 0.86–1.11). In contrast, a 5-degree longitude increase in residential position toward the western border of a time zone was associated with a 24% reduced risk of rectal cancer (multivariable-adjusted HR=0.76, 95% CI 0.59–0.98). In analyses stratified by chronotype, a 5-degree longitude increment in westward position of residence within the time zone was associated with an increased risk of colorectal cancer among women identifying as neither a morning nor evening chronotype (age-adjusted HR=1.58, 95% CI 1.01–2.47; Supplemental Table S5), but was not associated with colorectal cancer among morning or evening chronotypes. There was no evidence of effect modification by age, geographic region, or latitude.
Table 5.
Hazard ratios for the association between residential position within a time zone and risk of colorectal cancer, overall and by cancer subsite.
| Overall colorectal cancer |
Colon cancer |
Rectal cancer |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Residential position a | Cases | Person-years | Age-adjusted HR (95% CI)b | MV-adjusted HR (95%CI)c | Cases | Person-years | Age-adjusted HR (95% CI)b | MV-adjusted HR (95%CI)c | Cases | Person-years | Age-adjusted HR (95% CI)b | MV-adjusted HR (95%CI)c |
|
| ||||||||||||
| Per 5-degree longitude increment | 452 | 897,750 | 0.92 (0.83–1.03) | 0.92 (0.82–1.03) | 343 | 897,618 | 0.99 (0.87–1.12) | 0.98 (0.86–1.11) | 99 | 897,351 | 0.77 (0.59–0.99) | 0.76 (0.59–0.98) |
HR, Hazard ratio; CI, Confidence interval; MV, Multivariable.
Per 5-degree longitude increment in residential position from eastern to western border of time zone.
Hazard ratios adjusted for age (continuous) and time period (continuous).
Hazard ratios additionally adjusted for family history of colorectal cancer (yes, no), body mass index (<25, 25–29, 30–34, ≥35 kg/m2), smoking status (never, past, current), alcohol consumption (non-current, current 1–6, current ≥7 drinks/week), vigorous physical activity (none, <5, ≥5 hours/week), and processed meat consumption (quartiles).
DISCUSSION
In this study of circadian disruption and colorectal cancer incidence in a cohort of Black women, longer duration of night shift work was associated with an increased risk of colorectal cancer. Risk estimates were elevated for both colon and rectal cancer, but were imprecise due to small numbers of cases. In addition, there was evidence of a positive association between ever having worked a night shift and risk of colon, but not rectal cancer. We found no association between chronotype and risk of colorectal cancer, overall or by subsite. Residential position within a time zone was not associated with overall colorectal cancer risk. However, we observed an unexpected inverse association between residential position and risk of rectal cancer. In contrast, westward position of residence was associated with an increased risk of colorectal cancer only among women with no chronotype preference.
Biological evidence suggests a potential role of circadian disruption in carcinogenesis. Acting through a core group of clock genes, the circadian system regulates a number of cellular, physiological, and behavioral processes in the body, including cell cycle control and DNA repair.8 Circadian clock genes also promote cell apoptosis by upregulating tumor suppressor genes in response to DNA damage and cellular stress.8 The circadian system also plays a role in immune system functioning28 and regulation of the sleep/wake and feeding/fasting cycles.29,30 Further, activity in the gastrointestinal tract, such as digestive enzyme expression, gut physiology, colonic motility, metabolism, and cellular processes, exhibits diurnal patterns, indicating that the large bowel is under circadian control.7,31 In an experimental study, knocking down circadian clock proteins resulted in reduced apoptosis and accelerated cell proliferation and tumor growth in colon cancer cell lines.6 In a mouse model, circadian disruption led to dysregulation of the immune system, creating a pro-inflammatory environment.32 This may be important as inflammation has been implicated in colorectal carcinogenesis.33 Finally, disruption of the feeding/fasting34 or sleep/wake cycles17,35 could lead to immune system dysregulation, changes in gut microbiota, chronic inflammation,28 and obesity,4 all of which may play a role in colorectal cancer development.36
Despite biological evidence, prior research examining the association between circadian disruption, represented by shift work, and colorectal cancer in humans has provided conflicting results. For example, null,37,38 positive (2-fold increase in risk),39 and inverse (20% reduction in risk)40 associations have been reported in studies of night shift work and duration of night shift work in relation to colorectal cancer risk. Prior studies assessing rotating shift work, which includes night shifts, have similarly produced mixed findings, with some showing that rotating shift work,40 especially for long durations40,41 is associated with an approximately 20–35% increased risk of colorectal cancer, and others indicating no association.38,42,43 Furthermore, it is unclear whether night or rotating night shift work differentially impacts colorectal cancer risk by subsite, since positive associations have been reported for rectal cancer only44,45 and for both colon and rectal cancer.39 In the present analysis, we were unable to distinguish between permanent and rotating night shift work, the latter of which is hypothesized to be more disruptive, as individuals are unable to adapt their circadian rhythms to their ever-changing work schedules.46 However, we found that having worked a night shift for ≥10 years was associated with an increased risk of colorectal cancer, while ever having worked a night shift was associated with an elevated risk of colon cancer only. Given inconsistencies in prior literature, further research is needed to confirm our findings.
Chronotype has been hypothesized to be an indicator of susceptibility to circadian disruption,35 leading some to examine it as a potential cancer risk factor. For example, having an evening chronotype has been associated with an increased risk of breast,14,15,47 prostate,13 and endometrial cancer48 in some, but not all49 studies. To our knowledge, chronotype has not been previously examined with respect to colorectal cancer. The null association observed in the present study may suggest that chronotype is not a risk factor for colorectal cancer. An alternative explanation is exposure misclassification, as chronotype was ascertained at only a single timepoint and that single measurement was assumed to be reflective of chronotype throughout adulthood. Other potential explanations are limited study power, which may have hindered the ability to observe an association, and the possibility that chronotype may only be an indicator of susceptibility to circadian disruption, rather than an independent cause of circadian disruption.35
Findings from previous studies suggest that residential position may be a risk factor for cancer, as increasing westward residential position within a time zone has been positively associated with overall,16 breast,16,17,50 liver,5,16 and other cancer types.16 In a US study, a 5-degree longitude increase in residential position toward the western border of a time zone was associated with a 4% increased risk of colorectal cancer among women.16 In another study, living in areas with later sunset times was suggestively associated with an increase in colorectal cancer incidence.17 Overall results from the present analysis do not support previous evidence of a positive association between residential position and colorectal cancer. Differences in study design and lower statistical power may partially explain the divergence in findings. Another possibility is that residential position within a time zone may not be an adequate measure of circadian disruption in this study population. The apparent inverse association with rectal cancer was unexpected and may represent a chance finding.
There are some limitations to the present study. First, statistical power was limited in some analyses, particularly rectal cancer-specific models, due to a relatively small number of cases. Second, we did not have data on type of night shift work (e.g., permanent vs. rotating) or job type, which may influence intensity of circadian disruption exposure. Third, exposure misclassification is possible since chronotype was ascertained once in 2015 and applied to earlier timepoints. Fourth, given the retrospective nature of the chronotype analysis, there is a potential for recall bias. However, chronotype is not a known risk factor for colorectal cancer, so recall bias may be unlikely. Fifth, the analysis may be susceptible to survival bias because participants had to survive long enough to report their chronotype in 2015. Examination of covariate distributions at baseline among those included vs. excluded from the analysis did not reveal appreciable differences, suggesting that the two populations are similar. To further examine the potential for survival bias, we assessed characteristics of colorectal cancer cases included in the chronotype analysis (n=264) vs. cases who were excluded due to missing data on chronotype (n=306). There was a similar proportion of tumors located in the colon and rectum among cases included vs. excluded. As expected, excluded cases were older at diagnosis (mean age: 58.9 vs. 56.8 years) and were more likely to have late stage disease (percentage of stage 4 cancers: 20.6% vs. 3.8%) compared to included cases. If chronotype was associated with later stage disease, and hence colorectal cancer survival, failure to include these cases may result in a downward bias, which could explain the observed lack of association. Given that we cannot determine the relationship between chronotype and colorectal cancer risk among those excluded from the present analysis, we cannot rule out the potential for survival bias. However, the likelihood that chronotype impacted colorectal cancer survival seems small. Sixth, in the time zone analysis, place of residence may not be indicative of where participants spend most of their time. Thus, residential position within a time zone may not accurately reflect exposure to circadian disruption. Lastly, we were unable to assess associations by colorectal cancer molecular subtype, which may be an important consideration given that colorectal cancer risk factors can vary by molecular subtype.51
Despite some limitations, there are important strengths of this study. First, this study was conducted in a large prospective cohort of Black women, who are often underrepresented in scientific research. Analyses included incident medically confirmed colorectal cancer cases. Detailed data obtained from biennial questionnaires permitted the assessment and control of individual-level covariates. By using residential position within a time zone, we were able to objectively measure circadian disruption. Moreover, the association between residential position and colorectal cancer risk was prospectively assessed by measuring residential position prior to cancer diagnosis. Lastly, we comprehensively assessed circadian disruption in multiple ways, rather than using a single measurement.
In summary, in this study of circadian disruption in Black women, long-duration night shift work was associated with an increased risk of colorectal cancer, and colon cancer in particular, although the estimate of association was imprecise. Chronotype and residential position within a time zone were not associated with colorectal cancer risk. Given biological plausibility and limited epidemiologic investigation, further research on circadian disruption markers presented in this study, as well as other markers, is needed to elucidate the role of circadian disruption in colorectal cancer incidence.
Supplementary Material
ACKNOWLEDGEMENTS
This study, along with L.E. Barber, J.R. Palmer, and K.A. Bertrand, were supported by the National Institutes of Health (R01CA058420 and U01CA164974). J.R. Palmer also received support from the Karin Grunebaum Cancer Research Foundation. Data on colorectal cancer pathology were obtained from several state cancer registries (AZ, CA, CO, CT, DE, DC, FL, GA, IL, IN, KY, LA, MD, MA, MI, NJ, NY, NC, OK, PA, SC, TN, TX, VA). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute, the National Institutes of Health or the state cancer registries. We thank participants and staff of the BWHS for their contributions. The study protocol for the BWHS was approved by the Boston University Medical Center IRB and the IRBs of participating cancer registries, as required.
Abbreviations list:
- BMI
body mass index
- BWHS
Black Women’s Health Study
- US
United States
Footnotes
Conflicts of Interest: The authors declare no potential conflicts of interest.
REFERENCES
- 1.Baron KG, Reid KJ. Circadian misalignment and health. Int Rev Psychiatry. 2014;26(2):139–154. doi: 10.3109/09540261.2014.911149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Samuelsson LB, Bovbjerg DH, Roecklein KA, Hall MH. Sleep and circadian disruption and incident breast cancer risk: An evidence-based and theoretical review. Neurosci Biobehav Rev. 2018;84:35–48. doi: 10.1016/j.neubiorev.2017.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blask DE, Brainard GC, Dauchy RT, Hanifin JP, Davidson LK, Krause JA, Sauer LA, Rivera-Bermudez MA, Dubocovich ML, Jasser SA, Lynch DT, Rollag MD, Zalatan F. Melatonin-depleted blood from premenopausal women exposed to light at night stimulates growth of human breast cancer xenografts in nude rats. Cancer Res. 2005;65(23):11174–11184. doi: 10.1158/0008-5472.CAN-05-1945 [DOI] [PubMed] [Google Scholar]
- 4.Roenneberg T, Allebrandt KV, Merrow M, Vetter C Social jetlag and obesity. Curr Biol. 2012;22(10):939–943. doi: 10.1016/j.cub.2012.03.038 [DOI] [PubMed] [Google Scholar]
- 5.Vopham T, Weaver MD, Vetter C, Hart JE, Tamimi RM, Laden F, Bertrand KA. Circadian misalignment and hepatocellular carcinoma incidence in the United States. Cancer Epidemiol Biomarkers Prev. 2018;27(7):719–727. doi: 10.1158/1055-9965.EPI-17-1052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zeng ZL, Wu MW, Sun J, Sun YL, Cai YC, Huang YJ, Xian LJ. Effects of the biological clock gene Bmal1 on tumour growth and anti-cancer drug activity. J Biochem. 2010;148(3):319–326. doi: 10.1093/jb/mvq069 [DOI] [PubMed] [Google Scholar]
- 7.Mazzoccoli G, Vinciguerra M, Papa G, Piepoli A. Circadian clock circuitry in colorectal cancer. World J Gastroenterol. 2014;20(15):4197–4207. doi: 10.3748/wjg.v20.i15.4197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sancar A, Lindsey-Boltz LA, Kang TH, Reardon JT, Lee JH, Ozturk N. Circadian clock control of the cellular response to DNA damage. FEBS Lett. 2010;584(12):2618–2625. doi: 10.1016/j.febslet.2010.03.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.IARC Monographs Vol 124 group. Carcinogenicity of night shift work. Lancet Oncol. 2019;20(8):1058–1059. doi: 10.1016/S1470-2045(19)30455-3 [DOI] [PubMed] [Google Scholar]
- 10.Wang X, Ji A, Zhu Y, Liang Z, Wu J, Li S, Meng S, Zheng X, Xie L. A meta-analysis including dose-response relationship between night shift work and the risk of colorectal cancer. Oncotarget. 2015;6(28):25046–25060. doi: 10.18632/oncotarget.4502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dun A, Zhao X, Jin X, Wei T, Gao X, Wang Y, Hou H. Association between night-shift work and cancer risk: Updated systematic review and meta-analysis. Front Oncol. 2020;10(June):1–15. doi: 10.3389/fonc.2020.01006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roenneberg T, Kumar CJ, Merrow M. The human circadian clock entrains to sun time. Curr Biol. 2007;17(2):44–45. doi: 10.1016/j.cub.2006.12.011 [DOI] [PubMed] [Google Scholar]
- 13.Dickerman BA, Markt SC, Koskenvuo M, Hublin C, Pukkala E, Mucci LA, Kaprio J. Sleep disruption, chronotype, shift work, and prostate cancer risk and mortality: A 30-year prospective cohort study of Finnish twins. Cancer Causes Control CCC. 2017;27(11):1361–1370. doi:doi: 10.1007/s10552-016-0815-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hansen J, Lassen CF. Nested case-control study of night shift work and breast cancer risk among women in the Danish military. Occup Environ Med. 2012;69(8):551–556. doi: 10.1136/oemed-2011-100240 [DOI] [PubMed] [Google Scholar]
- 15.Ramin C, Devore EE, Pierre-Paul J, Duffy JF, Hankinson SE, Schernhammer ES. Chronotype and breast cancer risk in a cohort of US nurses. Chronobiol Int. 2013;30(9):1181–1186. doi: 10.3109/07420528.2013.809359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gu F, Xu S, Devesa SS, Zhang F, Klerman EB, Graubard BI, Caporaso NE. Longitude position in a time zone and cancer risk in the United States. Cancer Epidemiol Biomarkers Prev. 2017;26(8):1306–1311. doi: 10.1158/1055-9965.EPI-16-1029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Giuntella O, Mazzonna F. Sunset time and the economic effects of social jetlag : evidence from US time zone borders. J Health Econ. 2019;65:210–226. doi: 10.1016/j.jhealeco.2019.03.007 [DOI] [PubMed] [Google Scholar]
- 18.Eastman CI, Tomaka VA, Crowley SJ. Circadian rhythms of European and African-Americans after a large delay of sleep as in jet lag and night work. Sci Rep. 2016;6(36716):20–22. doi: 10.1038/srep36716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Carnethon MR, De Chavez PJ, Zee PC, Kim KYA, Liu K, Goldberger JJ, Ng J, Knutson KL. Disparities in sleep characteristics by race/ethnicity in a population-based sample: Chicago Area Sleep Study. Sleep Med. 2016;18:50–55. doi: 10.1016/j.sleep.2015.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Golden L Limited access: Disparities in flexible work schedules and work-at-home. J Fam Econ Iss. 2008;29(1):86–109. doi: 10.1007/s10834-007-9090-7 [DOI] [Google Scholar]
- 21.Jones SE, Lane JM, Wood AR, Van Hees VT, Tyrrell J, Beaumont RN, Jeffries AR, Dashti HS, Ruth KS, Tuke MA, Yaghootkar H, Sharp SA, Harrison JW, Dawes A, Byrne EM, Tiemeier H, Allebrandt KV, Bowden J, Ray DW, Freathy RM, Murray A, Mazzotti DR, Gehrman PR, Team 23andMe Research, Lawlor DA, Frayling TM, Rutter MK, Hinds DA, Saxena Richa & Weedon Michael N.. Genome-wide association analyses of chronotype in 697,828 individuals provides new insights into circadian rhythms in humans and links to disease. Nat Commun. 2019;10(1). doi: 10.1038/s41467-018-08259-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roenneberg T, Merrow M. Entrainment of the Human Circadian Clock. Cold Spring Harb Symp Quant Biol. 2007;72:293–299. doi:doi: 10.1101/sqb.2007.72.043 [DOI] [PubMed] [Google Scholar]
- 23.Fischer D, Lombardi DA, Marucci-Wellman H, Roenneberg T. Chronotypes in the US – Influence of age and sex. PLoS One. 2017;12(6):1–17. doi: 10.1371/journal.pone.0178782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Roenneberg T, Kuehnle T, Pramstaller PP, Ricken J, Havel M, Guth A, Merrow M. A marker for the end of adolescence. Curr Biol. 2004;14(24):1–2. doi: 10.1016/j.cub.2004.11.039 [DOI] [PubMed] [Google Scholar]
- 25.Thomas CM, Featherstone WE. Validation of Vincenty’s Formulas for the Geodesic Using a New Fourth-Order Extension of Kivioja’s Formula. J Surv Eng. 2005;131(1):20–26. doi: 10.1061/(ASCE)0733-9453(2005)131:1(20) [DOI] [Google Scholar]
- 26.Siegel RL, Miller KD, Goding Sauer A, Fedewa SA, Butterly LF, Anderson JC, Cercek A, Smith RA, Jemal A. Colorectal cancer statistics, 2020. CA Cancer J Clin. 2020;70(3):145–164. doi: 10.3322/caac.21601 [DOI] [PubMed] [Google Scholar]
- 27.United States Census Bureau. Geographic Levels. Published 2021. Accessed September 22, 2022. https://www.census.gov/programs-surveys/economic-census/guidance-geographies/levels.html
- 28.Comas M, Gordon CJ, Oliver BG, Stow NW, King G, Sharma P, Ammit AJ, Grunstein RR, Phillips CL. A circadian based inflammatory response – implications for respiratory disease and treatment. Sleep Sci Pract. 2017;1(1):1–19. doi: 10.1186/s41606-017-0019-2 [DOI] [Google Scholar]
- 29.Roenneberg T, Wirz-Justice A, Merrow M. Life between clocks: Daily temporal patterns of human chronotypes. J Biol Rhythms. 2003;18(1):80–90. doi: 10.1177/0748730402239679 [DOI] [PubMed] [Google Scholar]
- 30.Cassone VM, Stephan FK. Central and peripheral regulation of feeding and nutrition by the mammalian circadian clock: Implications for nutrition during manned space flight. Nutrition. 2002;18(10):814–819. doi: 10.1016/s0899-9007(02)00937-1 [DOI] [PubMed] [Google Scholar]
- 31.Hoogerwerf WA. Role of biological rhythms in gastrointestinal health and disease. Rev Endocr Metab Disord. 2009;10(4):293–300. doi: 10.1007/s11154-009-9119-3 [DOI] [PubMed] [Google Scholar]
- 32.Castanon-Cervantes O, Wu M, Ehlen JC, Paul K, Gamble KL, Johnson RL, Besing RC, Menaker M, Gewirtz AT, Davidson AJ. Dysregulation of Inflammatory Responses by Chronic Circadian Disruption. J Immunol. 2010;185(10):5796–5805. doi: 10.4049/jimmunol.1001026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Long AG, Lundsmith ET, Hamilton KE. Inflammation and Colorectal Cancer. Curr Color Cancer Rep. 2017;13(4):341–351. doi: 10.1007/s11888-017-0373-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mazri FH, Manaf ZA, Shahar S, Ludin AFM. The association between chronotype and dietary pattern among adults: A scoping review. Int J Env Res Public Heal. 2020;17(68):1–33. doi: 10.3390/ijerph17010068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Juda M, Vetter C, Roenneberg T. Chronotype modulates sleep duration, sleep quality, and social jet lag in shift-workers. J Biol Rhythms. 2013;28(2):141–151. doi: 10.1177/0748730412475042 [DOI] [PubMed] [Google Scholar]
- 36.Keum N, Wu K, Giovannucci E, Hunter DJ. Colorectal Cancer. In: Adami HO, Hunter D, Lagiou P, Mucci L, eds. Textbook of Cancer Epidemiology. 3rd ed. University Press Scholarship; Online; 2018:1–65. doi: 10.1093/oso/9780190676827.003.0011 [DOI] [Google Scholar]
- 37.Walasa WM, Carey RN, Si S, Fritschi L, Heyworth JS, Fernandez RC, Boyle T. Association between shiftwork and the risk of colorectal cancer in females: a population-based case-control study. Occup Environ Med. 2018;75(5):344–350. doi: 10.1136/oemed-2017-104657 [DOI] [PubMed] [Google Scholar]
- 38.McNeil J, Heer E, Willemsen RF, Friedenreich CM, Brenner DR. The effects of shift work and sleep duration on cancer incidence in Albertàs Tomorrow Project cohort. Cancer Epidemiol. 2020;67(July 2019):101729. doi: 10.1016/j.canep.2020.101729 [DOI] [PubMed] [Google Scholar]
- 39.Parent MÉ, El-Zein M, Rousseau MC, Pintos J, Siemiatycki J. Night work and the risk of cancer among men. Am J Epidemiol. 2012;176(9):751–759. doi: 10.1093/aje/kws318 [DOI] [PubMed] [Google Scholar]
- 40.Papantoniou K, Castaño-Vinyals G, Espinosa A, Turner MC, Alonso-Aguado MH, Martin V, Aragonés N, Pérez-Gómez B, Pozo BM, Gómez-Acebo I, Ardanaz E, Altzibar JM, Peiro R, Tardon A, Lorca JA, Chirlaque MD, García-Palomo A, Jimenez-Moleon JJ, Dierssen T, Ederra M, Amiano P, Pollan M, Moreno V, Kogevinas M. Shift work and colorectal cancer risk in the MCC-Spain case–control study. Scand J Work Environ Heal. 2017;43(3):250–259. doi: 10.5271/sjweh.3626 [DOI] [PubMed] [Google Scholar]
- 41.Schernhammer ES, Laden F, Speizer FE, Willett WC, Hunter DJ, Kawachi I, Fuchs CS, Colditz GA. Night-Shift Work and Risk of Colorectal Cancer in the Nurses’ Health Study. JNCI. 2003;95(11):825–828. doi: 10.1093/jnci/95.11.825 [DOI] [PubMed] [Google Scholar]
- 42.Schwartzbaum J, Ahlbom A, Feychting M. Cohort study of cancer risk among male and female shift workers. Scand J Work Environ Heal. 2007;33(5):336–343. doi: 10.5271/sjweh.1150 [DOI] [PubMed] [Google Scholar]
- 43.Wichert K, Rabstein S, Stang A, Erbel R, Eisele L, Arendt M, Keimer A, Dragano N, Hoffmann W, Lerch MM, Roskoden FC, Schmidt CO, Völzke H, Jöckel KH, Brüning T, Behrens T. Associations between shift work and risk of colorectal cancer in two German cohort studies. Chronobiol Int. 2020;37(8):1235–1243. doi: 10.1080/07420528.2020.1782930 [DOI] [PubMed] [Google Scholar]
- 44.Papantoniou K, Devore EE, Massa J, Strohmaier S, Vetter C, Yang L, Shi Y, Giovannucci E, Speizer F, Schernhammer ES. Rotating Night Shift work and Colorectal Cancer Risk in the Nurses’ Health Studies. Int J Cancer. Published online 2018. doi:doi: 10.1002/ijc.31655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shi Y, Liu L, Hamada T, Nowak JA, Giannakis M, Ma Y, Song M, Nevo D, Kosumi K, Gu M, Kim SA, Morikawa T, Wu K, Sui J, Papantoniou K, Wang M, Chan AT, Fuchs CS, Meyerhardt JA, Giovannucci E, Ogino S, Schernhammer ES, Nishihara R, Zhang X. Night-shift work duration and risk of colorectal cancer according to IRS1 and IRS2 expression. Cancer Epidemiol Biomarkers Prev. 2020;29(1):133–140. doi: 10.1158/1055-9965.EPI-19-0325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Haus EL, Smolensky MH. Shift work and cancer risk: Potential mechanistic roles of circadian disruption, light at night, and sleep deprivation. Sleep Med Rev. 2013;17(4):273–284. doi: 10.1016/j.smrv.2012.08.003 [DOI] [PubMed] [Google Scholar]
- 47.Hurley S, Goldberg D, Von Behren J, DeHart JC, Wang S, Reynolds P. Chronotype and postmenopausal breast cancer risk among women in the California Teachers Study. Chronobiol Int. 2019;36(11):1504–1514. doi: 10.1080/07420528.2019.1658113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Von Behren J, Hurley S, Goldberg D, DeHart JC, Wang SS, Reynolds P. Chronotype and risk of post-menopausal endometrial cancer in the California Teachers Study. Chronobiol Int. Published online 2021:1–11. doi: 10.1080/07420528.2021.1912073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lozano-Lorca M, Olmedo-Requena R, Vega-Galindo MV, Vázquez-Alonso F, Jiménez-Pacheco A, Salcedo-Bellido I, Sánchez MJ, Jiménez-Moleón JJ. Night shift work, chronotype, sleep duration, and prostate cancer risk: Caplife study. Int J Env Res Public Heal. 2020;17(6300):1–17. doi: 10.3390/ijerph17176300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Borisenkov MF. Latitude of residence and position in time zone are predictors of cancer incidence, cancer mortality, and life expectancy at birth. Chronobiol Int. 2011;28(2):155–162. doi: 10.3109/07420528.2010.541312 [DOI] [PubMed] [Google Scholar]
- 51.Wang L, He X, Ugai T, Haruki K, Lo CH, Hang D, Akimoto N, Fujiyoshi K, Wang M, Fuchs CS, Meyerhardt JA, Zhang X, Wu K, Chan AT, Giovannucci EL, Ogino S, Song M. Risk Factors and Incidence of Colorectal Cancer According to Major Molecular Subtypes. JNCI Cancer Spectr. 2021;5(1):1–10. doi: 10.1093/jncics/pkaa089 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article cannot be shared publicly due to protection of Black Women’s Health Study participants’ privacy. The data will be shared on reasonable request to the corresponding author.


