Abstract
Background:
The provision of sufficient stability after maxillofacial surgery is essential for the reduction of complications and disease recurrence. The stabilization of osteotomized pieces results in rapid restoration of normal masticatory function, reduction of skeletal relapse, and uneventful healing at the osteotomy site. We aimed to compare qualitatively stress distribution patterns over a virtual mandible model after bilateral sagittal split osteotomy (BSSO) bridged with three different intraoral fixation techniques.
Methods:
This study was conducted in the Oral and Maxillofacial Surgery Department of Mashhad School of Dentistry, Mashhad, Iran, from March 2021-March 2022. The mandible computed tomography scan of a healthy adult was used to generate a 3D model; thereafter, BSSO with a 3mm setback was simulated. The three following fixation techniques were applied to the model: 1) two bicortical screws, 2) three bicortical screws, and 3) a miniplate. The bilateral second premolars and first molars were placed under mechanical loads of 75, 135, and 600N in order to simulate symmetric occlusal forces. Finite element analysis (FEA) was carried out in Ansys software, and the mechanical strain, stress, and displacement calculations were recorded.
Results:
The FEA contours revealed that stress was mainly concentrated in the fixation units. Although bicortical screws presented better rigidity than miniplates, they were associated with higher stress and displacement readings.
Conclusion:
Miniplate fixation demonstrated the most favorable biomechanical performance, followed by fixation with two and three bicortical screws, respectively. Intraoral fixation with miniplates in combination with monocortical screws can serve as an appropriate fixation arrangement and treatment option for skeletal stabilization after BSSO setback surgery.
Key Words: Bicortical, Bilateral sagittal split osteotomy, Finite element analysis, Maxillofacial surgery
INTRODUCTION
Adequate skeletal stability is required to reduce postoperative problems, achieve optimal recovery, and avoid recurrence in patients following orthognathic surgery. The stabilization of the osteotomized pieces results in uncomplicated healing at the osteotomy site, a faster return to normal masticatory function, and a reduction in skeletal relapse1. Various fixing techniques have been proposed for osteosynthesis following a mandibular fracture or orthognathic surgery. These methods differ in terms of the number, material, and angle of insertion, as well as the arrangement and layout of the fixation parts used. There are three types of intraoral fixation methods: rigid, semi-rigid/functional, and nonrigid 2 .The stabilization of bone pieces by intraoral fixation recuses the possibility of displacement owing to muscle strain. The advantages of this method include a faster recovery period and no need for mandibular (maxillomandibular) fixation 3.
Currently, bilateral sagittal split osteotomy (BSSO) is considered the mainstay of treatment for correcting severe discrepancies of the mandible 4 .In retrognathic or prognathic individuals, this surgical treatment is used for mandibular advancement or setback 5.Since its initial introduction in the early 1800s, multiple modifications have been proposed for BSSO surgery. These recent advancements foster more reliable, safe, and predictable surgical outcomes. The final surgical outcome is highly dependent on various factors, such as the density of the cortical bone, mandibular position, fixation method, and, most importantly, the surgeon’s expertise 6, 7.
Sagittal split ramus osteotomy (SSRO) and intraoral vertical ramus osteotomy (IVRO) are currently the two main leading concepts for mandibular repositioning in orthognathic surgery (Modern approaches in mandibular orthognathic surgery include SSRO and IVRO). When mandibular displacement demands the use of fixation screws and plates, SSRO is preferred over IVRO 8. This well-established approach promotes (ensures) sustained (initial, short-term) healing by allowing for extensive medullary contact between the osteotomy segments. Intraoral fixation reduces the required duration of the postoperative intermaxillary fixation (IMF) period with elastics. This approach also renders a predictable immediate postoperative occlusion. However, this method is associated with a higher incidence rate of neurovascular damage and bad split fracture compared to IVRO (and a 0.9% incidence rate of bad split osteotomy) 9 .
Rigid fixation is the standard for maxillofacial fracture treatment and is also commonly employed in orthognathic surgery 10-12. The concept of internal rigid fixation has gradually shifted from using non-rigid wires to incorporating titanium plates and screws 13. Despite its advancements and advantages, cases of irreversible nerve injury due to compression caused by the screws and plates, condylar displacement, need for reintervention and occlusal changes have been reported 14. Following SSRO, rigid internal fixation (RIF) is performed using bicortical plates, mini-plates, or a combination of both 15. Titanium plates and screws are currently regarded as the gold standard for rigid fixation in orthognathic surgery patients 16.
In vitro studies or finite element analysis (FEA) are used to assess the biomechanical stability of various fixation systems following mandibular osteotomy. The FEA is a numerical approach for solving differential equations in the fields of engineering, physics, and mathematical modeling 1, 2, 17. The FEA-based research justifies its implementation in oral and maxillofacial surgery by providing advantages, such as precise analysis of stress distribution, analysis of complex mechanical systems and nonhomogeneous structures, as well as being less time-consuming and highly cost-effective 18, 19. This method has recently become increasingly popular in the field of oral and maxillofacial surgery, especially in traumatology, zygomatic implantology, dental implantology, and orthognathic surgery 1, 2, 17. This method assesses the biomechanical responses of the bone and also the biomechanical performance of different fixation methods under the applied load conditions 1.
Although RIF has been utilized for over three decades, no census technique exists for fixation following SSRO surgery since Spiessel’s classic works, and the applied approach is typically empirical depending on the surgeon’s choice and clinical experience 14. In light of the aforementioned issues, we aimed to qualitatively compare the force distribution of three different fixation techniques, including two bicortical screws, three bicortical screws, and a miniplate, after SSRO mandibular setback surgery using FEA.
MATERIALS AND METHODS
Development of finite element model
This study was conducted in the Oral and Maxillofacial Surgery Department of Mashhad School of Dentistry, Mashhad, Iran, from March 2021-March 2022. A computed tomography (CT) image of a dentulous mandible of a healthy adult male was downloaded from the archive of Mashhad Dental School’s Oral and Maxillofacial Radiology Department in order to generate a virtual model. The CT images were recorded in the axial, sagittal, and coronal planes at 1mm intervals and outputted in digital imaging and communications in medicine (DICOM) format. After importing the DICOM file into the Mimics V.21 program (Materialise N.V., Heverlee, Belgium), a 3D model was recreated using the “Multiplanar reformatting” and “Subtraction” commands.
The geometry of miniplates/screws was based on the provided information by the manufacturer of the physical specimens (COMPACT 2.0 MF Internal Fixation System, Synthes, USA). A 3D scanner was used to scan the 5-hole straight miniplates, as well as miniscrews 7 mm and 15 mm in length (Radman Darman, Kian, Mashhad, Iran). The tridimensional model of the fixation tools was generated using Solidworks 2019 software (Dassault Systemes, Solidworks, Corp., Vélizy, France). The material was similar to commercially available titanium Ti-6Al-4V (ASTM F136-12a).
The BSSO, Epker modification, with mandibular setback of 3mm was simulated in the program. This resulted in a proximal and distal segment. The osteotomized 3D models were converted to a STP format, subjected to FEA, and assembled using three different fixation methods in ANSYS V.19.2 workbench (Swanson Analysis Inc., Houston, PA, USA). The developed fixation modalities were as follows:
Fixation in type 1: two bicortical screws placed distal to the osteotomy line
Fixation in type 2: three screws placed distal to the osteotomy line
Fixation in type 3: a precontoured miniplate secured with four screws mesial and distal to the osteotomy line
Loading and boundary conditions:
All materials were considered homogenous, isotropic, and linear-elastic. The mechanical properties and boundary conditions, including Young’s modulus and Poisson’s ratio, were obtained according to previous literary data (Table 1).
Table 1.
Structural components and component properties
| Component | Properties | Young's modulus (MPa) | Poisson's ratio |
|---|---|---|---|
| Cortical bone | Elastic, Isotropic | 13700 | 0.3 |
| Cancellous bone | Elastic, Isotropic | 1370 | 0.3 |
| Teeth | Elastic, Isotropic | 20000 | 0.3 |
| Titanium screws and plates | Elastic, Isotropic | 117000 | 0.33 |
The 3D model then meshed with structured pyramidal elements. Following mesh refinement, the mandible model consisted of 285, 934 tetrahedral elements and 486, 355 nodes. Each fixation method was loaded with six different forces. An occlusal force with magnitudes of 75, 135, and 600N were exerted onto the bilateral second premolars and first molars. The end of the cortical bone of the mandible was fixed in all simulations. A total of 18 different simulations were evaluated. The stress analysis of models was carried out using Abaqus 6.13 (Dassault Systemes Simulia Corp, 2009) for all models at various force bites.
Ethical considerations
The protocol of this qualitative (computational) study was approved by the Research and Ethics Committee of Mashhad University of Medical Sciences (IR.MUMS.DENTISTRY.REC.1400.073).
RESULTS
The entire construction withstood the given loads applied to the mandible, miniplate, and miniscrews. The maximum von Mises stress, as well as strain and dislodgment values, for different fixation techniques under different occlusal loads, are presented in Table 2. Stress and strain distribution in all fixation techniques and models are depicted in Figures 1-3.
Table 2.
Comparison of maximum stress, strain and dislodgment contours in different cases
| Fixation method, Teeth subjected to force Load magnitude(N) |
Screws/Plates | Cortical bone | Cancellous bone | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Stress (MPa) | Strain | Displacement (mm) |
Stress (MPa) | Strain | Displacement (mm) |
Stress (MPa) | Strain | Displacement (mm) |
|
| Plate, Molar 75 | 31.17 | 0.000027 | 0.0126 | 4.87 | 0.00036 | 0.030 | 0.54 | 0.00072 | 0.029 |
| Plate, Molar 135 | 56.10 | 0.000048 | 0.0227 | 8.76 | 0.00066 | 0.054 | 0.98 | 0.0013 | 0.053 |
| Plate, Molar 600 | 249.36 | 0.0021 | 0.1010 | 38.96 | 0.0029 | 0.242 | 4.36 | 0.0057 | 0.237 |
| Plate, Premolar 75 | 5.91 | 0.000051 | 0.0027 | 1.49 | 0.00011 | 0.0060 | 0.202 | 0.00015 | 0.0059 |
| Plate, Premolar 135 | 10.64 | 0.000092 | 0.0049 | 2.68 | 0.00021 | 0.0109 | 0.36 | 0.00027 | 0.0107 |
| Plate, Premolar 600 | 47.29 | 0.00041 | 0.022 | 1.92 | 0.00093 | 0.048 | 1.61 | 0.0012 | 0.047 |
| 2Screws, Molar 75 | 13.82 | 0.000011 | 0.0141 | 3.48 | 0.00031 | 0.0304 | 1.042 | 0.00076 | 0.029 |
| 2Screws, Molar 135 | 24.88 | 0.00021 | 0.025 | 6.27 | 0.00056 | 0.054 | 1.87 | 0.0013 | 0.053 |
| 2Screws, Molar 600 | 110.61 | 0.00095 | 0.112 | 27.89 | 0.0025 | 0.243 | 8.34 | 0.0060 | 0.239 |
| 2Screws, Premolar 75 | 2.65 | 0.000029 | 0.0030 | 1.48 | 0.00011 | 0.0060 | 0.194 | 0.00014 | 0.0059 |
| 2Screws, Premolar 135 | 4.78 | 0.000041 | 0.0055 | 2.66 | 0.00021 | 0.010 | 0.34 | 0.00025 | 0.0107 |
| 2Screws, Premolar 500 | 21.25 | 0.00018 | 0.024 | 11.85 | 0.00093 | 0.048 | 1.55 | 0.0011 | 0.047 |
| 3Screws, Molar 75 | 7.76 | 0.000080 | 0.0141 | 3.76 | 0.00031 | 0.030 | 0.48 | 0.0004 | 0.029 |
| 3Screws, Molar 135 | 13.98 | 0.000014 | 0.025 | 6.78 | 0.00056 | 0.054 | 0.86 | 0.00073 | 0.053 |
| 3Screws, Molar 600 | 62.15 | 0.00064 | 0.112 | 30.15 | 0.0025 | 0.243 | 3.85 | 0.0032 | 0.239 |
| 3Screws, Premolar 75 | 1.53 | 0.000016 | 0.0030 | 1.48 | 0.00011 | 0.0060 | 0.19 | 0.00014 | 0.0059 |
| 3Screws, Premolar 135 | 2.75 | 0.000029 | 0.0055 | 2.68 | 0.00021 | 0.0109 | 0.34 | 0.00026 | 0.0107 |
| 3Screws, Premolar 600 | 12.25 | 0.00012 | 0.0245 | 11.91 | 0.00093 | 0.048 | 1.54 | 0.00115 | 0.0478 |
Fig. 1.
Recorded finite element analysis contours for sagittal split ramus osteotomy simulations fixed with two bi-cortical screws
Fig. 3.
Recorded finite element analysis contours for sagittal split ramus osteotomy simulations fixed with mini-plate
FEA contours of the plate/screws
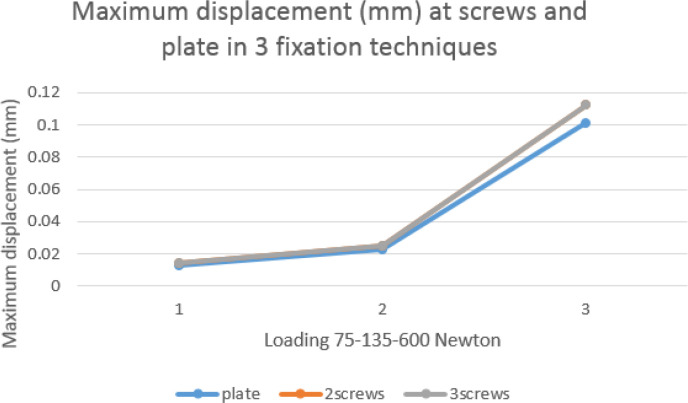
The miniplate model predicted greater von Mises stress values, compared to fixation with two or three bicortical screws, at all mechanical forces (Figure 4). Maximum displacement was equal in models fixed with either two or three bicortical screws under all occlusal loads. Nevertheless, this value was always higher than the recorded maximum displacement of the miniplate (Figure 5). The numerical results revealed the highest maximum strain values with three bicortical screws, two bicortical screws, and the miniplate in descending order (Figure 6).
Fig. 4.
Maximum von Mises stress (MPa) of the miniplate/screws in different simulation models
Fig. 5.
Maximum deformation (mm) of the miniplate/screws in different simulation models
Fig. 6.
Maximum strain of the miniplate/screws in different simulation models
FEA contours of the cortical bone
Maximum cortical bone stress presented lower values in models fixed with mini-plates compared to when bicortical screws were used (Figure 7). Cortical bone displacement was also found to be less in the miniplate fixation technique (Figure 8). Fixation with one miniplate was the simulation with the lowest strain on the cortical bone (Figure 9).
Fig. 7.
Maximum von Mises stress (MPa) of the cortical bone in different fixation techniques
Fig. 8.
Maximum displacement (mm) of the cortical bone in different fixation techniques
Fig. 9.
Maximum strain of the cortical bone in different fixation techniques
Finite element analysis contours of the cancellous bone
The cancellous mandibular bone exhibited the lowest maximum von Mises stress when the osteotomy site was fixed with miniplates (Figure 10). Minimum displacement in the cancellous bone was recognized in models fixed with miniplates (Figure 11). Miniplate fixation was also able to yield lower maximum strain levels in the cancellous bone compared to fixation with bicortical screws (Figure 12).
Fig. 10.
Maximum von Mises stress (MPa) of the cancellous bone in different fixation techniques
Fig. 11.
Maximum displacement (mm) of the cancellous bone in different fixation techniques
Fig. 12.
Maximum strain of the cancellous bone in different fixation techniques
DISCUSSION
A whole mandible was modeled in this study using the CT images of a young healthy subject. It is not possible to perform accurate simulations of the internal mandibular cortex or periodontal structures using CT scan data, which can only provide a thorough virtual model of the exterior (outer) mandibular cortex. In contrast to previously conducted studies, which tended to focus on a less sophisticated FEA model, the authors’ digital model was developed using DICOM images and Mimics software and, as a result, an exact 3D equivalent of the mandible anatomy was ultimately produced. An edentulous hemimandible with a corticocancellous structure and a total of 19845 components was created by Maurer et al. 17.
Some researchers considered the mandibular bone to be isotropic material and do not include the teeth in aims of simplification 18, 19. Stringhini et al. simulated rigid fixation on a mandibular model consisting of 1,489,170 nodes with pulp, dentin, enamel, periodontal ligament, cortical, and trabecular bone structures 4. The required computational power and dedicated (consumed) time for analysis depend on the complexity of the geometric modeling. It seems irrelevant and unnecessary to investigate the possible effect of dental and periodontal tissues on the biomechanical outcome of rigid fixation. In this commentary, our developed model only included teeth, trabecular, and cancellous bone, consisting of 285,934 tetrahedral elements and 486,355 nodes.
The adoption of appropriate material properties for each element is integral to the development of an accurate simulation model. The acquired values for Young’s modulus or Poisson’s ratio of the bone, miniplate, and miniscrews were derived from the presented values in some studies 20-22 who verified that changes in mandibular geometry or position could significantly alter the elastic properties of the mandibular bone. Mandibular bone is stiffer in length than in shear or radial measurements, and although the development of an FEA model is possible, this approach generates further complexity. The material properties were the same for all simulations, and Ti-6AI-4V alloy was used for fixative appliances.
In order to approximate symmetrical biting force, experimental loads of 75, 135, and 600N were applied to the bilateral second premolars and first molars. According to a study this was established by applying the identical load magnitudes to all of the mandibular molars and premolars and dividing the vector of force among them. In addition, earlier investigations used models with occlusal stresses of 600N or less 23. When conducting a simulation, the point of force insertion, fixation point, load magnitudes, and material properties conspire to dictate the obtained FEA results. The FEA enables the user to define the point for force insertion and fixation points according to the designed analysis; however, some limitations exist in cases of in vitro biomechanical studies.
These studies generate a virtual mandible, which is usually fixed on the mandibular ramus (rami), condyle, or a steel jig. Force is loaded onto the occlusal surface of teeth using a hydraulic pressure guide. The obtained results are reported as the amount of displacement, deformation, or failure of the utilized fixation unit. Despite the fact that most pertinent investigations used this analysis technique, it falls short of accurately replicating physiologic jaw motions. 24-26. Harada et al. used a pressure-sensitive device to measure the biting force of patients in maximum intercuspation. Forces were applied from the muscles involved in lifting the mandible during mastication, such as the masseter, temporalis, and median pterygoid muscles 27. The study by Oguz et al. applied the vector of force to the angle of the mandible in order to simulate masticatory forces of the masseter muscle 28, whereas Stringhini et al. decided to apply mechanical load in the area of insertion of the masseter, temporalis, and median pterygoid muscles 4.
In the present study, 18 simulations were analyzed and compared. The end of the cortical bone of the entire mandible was fixed in all models, and only the symphysis was able to act in the vertical plane as roller support. Since it was not possible (practical) to assess the torque effect of the mandibular condyle, this structure was not incorporated into the analysis process. Stress and displacement were identified in all simulation models. The highest recorded stress and displacement values were observed in the osteotomy bridged with three bi-cortical screws and subjected to 600N force on bilateral mandibular premolars. In this model, areas with von Mises stress of 30-60 MPa and displacement of 0.24 mm were observed. The high stress and displacement values are rationalized by the small area for force insertion, which may not be the case under clinical conditions.
The lowest amount of stress and displacement pertained to rigid miniplate fixation under a symmetric occlusal load of 75N on the mandibular molars. Greater load magnitudes led to higher amounts of stress and displacement. Stress was dissipated to other regions of the mandible-in other words, during the masticatory act, force is exerted on the fixed osteotomy site, as well as multiple structures, including the bone, teeth, and adjacent soft tissue. Considering the fact that soft tissue was not included in the assessed models, the amount of stress absorbed by hard tissues is actually less in real patients (in vivo circumstances). In agreement with the study by Stringhini et al., the performed analysis revealed that stress and displacement values were correlated 4.
Three different fixation modalities were simulated, subjected to biting forces, and then analyzed for BSSO surgery. The utilized miniplate was combined with a smaller monocortical screw; this variation is less common for mandibular fixation. The use of smaller miniplates for bridging osteotomized segments after BSSO has drawn increasing interest over the past decades. In 2010, Burm et al. established that the application of 1.2mm microplates combined with monocortical screws for the management of mandibular fractures offers acceptable (sufficient) skeletal stability in comparison with conventional 2 mm miniplates 29. Microplate intraoral fixation proved advantageous in terms of biocompatibility, high adaptability to the fracture site, minimal mass effect, and enhanced patient satisfaction. Along the same lines, Ahmad et al. used FEA to compare the efficacy of 1.5 mm and 2 mm miniplates for stabilizing mandibular symphysis fractures. The two plating systems displayed relatively similar outcomes regarding stress distribution, and no significant difference was observed 30. Yeo et al. conducted a study to compare the occurrence of neurosensory disturbances in the advanced mandible after rigid intraoral fixation with positional screws and 1.7 mm miniplates. They concluded that no method was proven superior to the other 31.
According to the obtained results, irrespective of the applied mechanical load, bi-cortical screws demonstrated lower stress values in comparison with miniplates. Previous FEA studies also confirm this finding 17-19, 24, 25. The maximum recorded stress value for the miniplates never exceeded 950 MPa (i.e., the ultimate strength of titanium alloy used in all fixation elements. Therefore, miniplates were able to endure this force without any failure 32. Stress was concentrated in the insertion site and around empty holes; moreover, maximum stress was concentrated in the superior and distal border of the third screw, as well as the inferior and mesial border of the second screw, pointing to the high pressure and tensile stress in this area.
When it comes to screws, stress dissipation patterns seem to be different. The most inferior and distal screw displayed a higher concentration of stress, and the maximum exerted stress was mainly concentrated in the area of contact (the interface) between the cortical and cancellous bone on the lingual surface of the mandible. The reason behind this finding is to some extent unclear; however, this may be attributable to the fact that this screw has to tolerate a greater amount of stress compared to when two or three screws are used. Bicortical screw fixation exhibited better rigidity compared to miniplates. Bicortical screws are fixed into both the lingual and buccal cortex of the mandible, while miniplates are only stabilized with monocortical screws. This is why miniplates are more susceptible to deflection.
The exact impact of different mandibular movements on the stress distribution behavior of the fixative appliances remains ill-defined (How stress distribution patterns in the fixative appliances will respond to different mandibular movements is unpredictable.) Miniplates are thought to tolerate (absorb) greater tensile forces and exhibit more deflection when used to stabilize osteotomized segments after mandibular advancement surgery. Our literature review revealed a paucity in studies which have investigated the correlation between the amount of mandibular displacement and the stress values for fixative appliances. Erkmen et al 33 attempted to compare different intraoral fixation methods after mandibular advancement and setback through BSSO. In a FEA study, the occlusal loads of 500 and 660N were applied, which are significantly greater than natural biting forces; therefore, the results of this study were not applicable 34.
Fixation units proved efficacious in obviating stress distribution in the mandibular bone. This finding is in line with the results of another study 24, who indicated that models with bicortical screws predicted higher stress and strain on the mandibular bone in comparison with the models which use miniplates. Due to the differences in FEA simulation and model construction, it does not seem possible to compare the exact areas of stress concentration in the mentioned study and those in the present research. This study demonstrated that a considerable amount of stress is concentrated in close proximity to the inferior-distal screw. The maximum stress is identified in the lingual trabecular bone around the screw, adjacent to the stress concentrated in the fixation unit. This may be related to the single screw located inferior to the other two.
There is usually a focal concentration of stress around the third screw, which is located in the buccal cortex of the distal segment. Nevertheless, this finding only appertains to advancement in SSRO. In the present study, with 3 mm mandibular setback, miniplate models recorded higher von Mises stress values than bicortical screws, mainly noticed around the second screw placed in the proximal osteotomy segment. In general, bone stress concentration is typically greater in the external mandibular cortex than in other regions. The relationship between bone stress concentrations around the fixation units can be related to the stress protector factor. Since metal is stiffer than bone, it becomes the primary load supporter, reducing the natural mechanical stress absorbed by the bone. This phenomenon can lead to bone adaptation to new conditions by reducing the mass and reabsorption, subsequently loosening the screws 35.
The amount of displacement of the osteotomy fragments is a reflection of the rigidity and stability of the fixation units. The highest displacement in bone elements was observed around the angle of the proximal segment where the mechanical load was exerted. The muscles in this region tend to elevate the bony segment and subsequently cause displacement. On the contrary, the distal segment is secured when the posterior teeth are locked in maximum intercuspation; moreover, the symphysis (chin) is relatively fixed and does not exhibit significant movement 36, 37.
Displacement contours illustrated that miniplate rigid fixation was able to obtain the lowest displacement values for the osteotomized fragments. Previously conducted in vitro and FEA studies also support the notion that bicortical screws provide better rigidity. Owing to the fact that bicortical screws penetrate through the buccal and lingual cortex of the proximal and distal segments, this method precludes rotation of the proximal segment. On the other hand, miniplates with monocortical screws deflect to some extent, thereby leading to lower degrees of displacement (lower displacement values) 17.
As previously mentioned, miniplates are the least rigid fixation device. According to Claes et al. 38, rigid fixative appliances minimize interfragmentary motion and inhibit the stimulation of callus formation. It is noteworthy that while flexible fixation promotes callus formation and, therefore, ameliorates bone healing, unstable fixation can possibly result in nonunion. Their animal study also reported that fracture gaps larger than 6mm lead to nonunion. This emphasizes the superiority of semi-rigid fixation, as in miniplates, over other fixation methods for the achievement of a favorable healing process.
In a medical setting, the surgeon’s choice is taken into consideration while selecting the fixing technique. According to a systematic review and meta-analysis conducted in 2016 by Al-Moraissi and Ellis, there was no statistically significant difference in skeletal stability between bicortical screws and miniplates following BSSO setback surgery. Nonetheless, as reported by the authors, bicortical plates did offer somewhat more skeletal stability than miniplate fixation, and this procedure is strongly advised (particularly promoted) in situations when the mandibular setback is larger than 6 millimeters 39.
Joss and Vassalli carried out a systematic review to investigate stability following BSSO advancement surgery with rigid fixation. The pooled results indicated that bicortical plates represented a higher rate of both long- and short-term horizontal relapse. Skeletal relapse is of multifactorial etiology and is associated with such factors as the amount of mandibular repositioning (advancement or setback), the angle of the mandibular plane, growth patterns, and faulty positioning (seating) of the condyles. They also concluded that both fixation options offer similar clinical effectiveness 40.
Among the notable limitations of this study, we can refer to the lack of data and statistical analysis of the results due to the absence of a proper statistical study, as well as the complexities of the equations due to the complex anatomy of the mandible.
Fig. 2.
Recorded finite element analysis contours for sagittal split ramus osteotomy simulations fixed with three bi-cortical screws
CONCLUSION
Despite the fact that the use of smaller fixation devices has been anecdotally successful due to less invasive surgery, reduced rates of postoperative infection, and less tissue damage, the research is still insufficient to recommend BSSO fixation with smaller-sized miniplates as a definitive treatment option (but the evidence supporting fixation with smaller sized miniplates for BSSO is still not convincing). The constructed simulation models and acquired computational data pointed out that the fixation units were located where the majority of the bone stress was centered. Miniplates had the best stress dissipation performance, whereas bicortical screws were found to be stiffer with higher stress and displacement values. The obtained FEA contours confirmed that miniplate fixation renders satisfactory stabilization of the osteotomy site after BSSO setback surgery. Nonetheless, the biomechanical efficacy of various fixation ideas after mandibular advancement was not examined in this investigation. Finally, it is suggested that miniplate fixation is the best technique for bridging osteotomy segments following BSSO setback surgery. The conclusions of this finite element analytical investigation need to be supported by additional well planned in vivo experiments.
CONFLICTS OF INTEREST
The authors declare that they have no conflict of interest.
FUNDING
No company has provided support equipment and materials, and the requested funds have been provided through the sources of research projects.
References
- 1.Hassan MK, Ring M, Stassen LF. A Finite Element Analysis Study Comparing 3 Internal Fixation Techniques in Mandibular Sagittal Split Osteotomy. Int J Otorhinolaryngol Head Neck Surg. 2018;7(05):298–305. [Google Scholar]
- 2.Ghorashi SM, Keshavarzi MM, Damercheli S, Parhiz A. The comparison of three different fixation methods on bilateral sagittal split ramus osteotomy mandibular on a 3D of fully modelled mandible by the finite element method. J Craniomaxillofac Surg. 2019;6(3):113–21. [Google Scholar]
- 3.Sukegawa S, Kanno T, Manabe Y, Matsumoto K, Sukegawa-Takahashi Y, Masui M, Furuki Y. Biomechanical Loading Evaluation of Unsintered Hydroxyapatite/poly-l-lactide Plate System in Bilateral Sagittal Split Ramus Osteotomy. Materials (Basel) 2017;10(7):764. doi: 10.3390/ma10070764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stringhini DJ, Sommerfeld R, Uetanabaro LC, Leonardi DP, Araújo MR, Rebellato NL, et al. Resistance and Stress Finite Element Analysis of Different Types of Fixation for Mandibular Orthognathic Surgery. Braz Dent J. 2016;27(3):284–91. doi: 10.1590/0103-6440201600336. [DOI] [PubMed] [Google Scholar]
- 5.Chang LR, Chen CC, Jeng SF, Chen YR, Hwang LC, Lin TS. Investigation of a Modified Novel Technique in Bilateral Sagittal Splitting Osteotomy Fixation: Finite Element Analysis and In Vitro Biomechanical Test. Biomed Res Int. 2020;2020:8707389. doi: 10.1155/2020/8707389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Böckmann R, Meyns J, Dik E, Kessler P. The modifications of the sagittal ramus split osteotomy: a literature review. Plast Reconstr Surg Glob Open. 2015;2(12):e271–e71. doi: 10.1097/GOX.0000000000000127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Monson LA. Bilateral sagittal split osteotomy. Semin Plast Surg. 2013;27(3):145–48. doi: 10.1055/s-0033-1357111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.He P, Iwanaga J, Matsushita Y, Adeeb N, Topale N, Tubbs RS, et al. A Comparative Review of Mandibular Orthognathic Surgeries with a Focus on Intraoral Vertico-sagittal Ramus Osteotomy. Cureus. 2017;9(12):e1924–e24. doi: 10.7759/cureus.1924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jung H-D, Kim SY, Park H-S, Jung Y-S. Orthognathic surgery and temporomandibular joint symptoms. Maxillofac Plast Reconstr Surg. 2015;37(1):1–11. doi: 10.1186/s40902-015-0014-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Islamoglu K, Coskunfirat OK, Tetik G, Ozgentas HE. Complications and removal rates of miniplates and screws used for maxillofacial fractures. Ann Plast Surg. 2002;48(3):265–68. doi: 10.1097/00000637-200203000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Park H-C, Kim S-G, Oh J-S, You J-S, Kim W-G. Mini-plate removal in maxillofacial trauma patients during a five-year retrospective study. J Korean Assoc Oral Maxillofac Surg. 2016;42(4):182–86. doi: 10.5125/jkaoms.2016.42.4.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rallis G, Mourouzis C, Papakosta V, Papanastasiou G, Zachariades N. Reasons for miniplate removal following maxillofacial trauma: a 4-year study. J Craniomaxillofac Surg. 2006;34(7):435–39. doi: 10.1016/j.jcms.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 13.Tamura N, Takaki T, Takano N, Shibahara T. Three-dimensional Finite Element Analysis of Bone Fixation in Bilateral Sagittal Split Ramus Osteotomy Using Individual Models. Bull Tokyo Dent Coll. 2018;59(2):67–78. doi: 10.2209/tdcpublication.2013-3000. [DOI] [PubMed] [Google Scholar]
- 14.Sato FRL, Asprino L, Noritomi PY, da Silva JVL, de Moraes M. Comparison of five different fixation techniques of sagittal split ramus osteotomy using three-dimensional finite elements analysis. Int J Oral Maxillofac Surg. 2012;41(8):934–41. doi: 10.1016/j.ijom.2012.03.018. [DOI] [PubMed] [Google Scholar]
- 15.Kuik K, Ho J, de Ruiter MHT, Klop C, Kleverlaan CJ, de Lange J, et al. Stability of fixation methods in large mandibular advancements after sagittal split ramus osteotomy: an in vitro biomechanical study. Br J Oral Maxillofac Surg. 2021;59(4):466–71. doi: 10.1016/j.bjoms.2020.09.008. [DOI] [PubMed] [Google Scholar]
- 16.Park Y-W, Kang H-S, Lee J-H. Comparative study on long-term stability in mandibular sagittal split ramus osteotomy: hydroxyapatite/poly-l-lactide mesh versus titanium miniplate. Maxillofac Plast Reconstr Surg. 2019;41(1):8–17. doi: 10.1186/s40902-019-0192-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maurer P, Holweg S, Schubert J. Finite-element-analysis of different screw-diameters in the sagittal split osteotomy of the mandible. J Craniomaxillofac Surg. 1999;27(6):365–72. doi: 10.1054/jcms.1999.0069. [DOI] [PubMed] [Google Scholar]
- 18.Chuong CJ, Borotikar B, Schwartz-Dabney C, Sinn DP. Mechanical characteristics of the mandible after bilateral sagittal split ramus osteotomy: comparing 2 different fixation techniques. J Oral Maxillofac Surg. 2005;63(1):68–76. doi: 10.1016/j.joms.2003.12.045. [DOI] [PubMed] [Google Scholar]
- 19.Ming-Yih L, Chun-Li L, Wen-Da T, Lun-Jou L. Biomechanical stability analysis of rigid intraoral fixation for bilateral sagittal split osteotomy. J Plast Reconstr Aesthet Surg. 2010;63(3):451–5. doi: 10.1016/j.bjps.2008.11.057. [DOI] [PubMed] [Google Scholar]
- 20.Nihara J, Gielo-Perczak K, Cardinal L, Saito I, Nanda R, Uribe F. Finite element analysis of mandibular molar protraction mechanics using miniscrews. Eur J Orthod. 2015;37(1):95–100. doi: 10.1093/ejo/cju017. [DOI] [PubMed] [Google Scholar]
- 22.Strait DS, Wang Q, Dechow PC, Ross CF, Richmond BG, Spencer MA, et al. modeling elastic properties in finite-element analysis: how much precision is needed to produce an accurate model? Anat Rec A Discov Mol Cell Evol Biol. 2005;283(2):275–87. doi: 10.1002/ar.a.20172. [DOI] [PubMed] [Google Scholar]
- 23.Sarkarat F, Motamedi MH, Bohluli B, Moharamnejad N, Ansari S, Shahabi-Sirjani H. Analysis of stress distribution on fixation of bilateral sagittal split ramus osteotomy with resorbable plates and screws using the finite-element method. J Oral Maxillofac Surg. 2012;70(6):1434–8. doi: 10.1016/j.joms.2011.05.017. [DOI] [PubMed] [Google Scholar]
- 24.Albougha S, Darwich K, Darwich MA, Albogha MH. Assessment of sagittal split ramus osteotomy rigid internal fixation techniques using a finite element method. Int J Oral Maxillofac Surg. 2015;44(7):823–9. doi: 10.1016/j.ijom.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 25.Sindel A, Demiralp S, Colok G. Evaluation of different screw fixation techniques and screw diameters in sagittal split ramus osteotomy: finite element analysis method. J Oral Rehabil. 2014;41(9):683–91. doi: 10.1111/joor.12188. [DOI] [PubMed] [Google Scholar]
- 26.Hsu S S P. The stability of mandibular prognathism corrected by bilateral sagittal split osteotomies: a comparison of bi-cortical osteosynthesis and mono-cortical osteosynthesis. International Journal of Oral and Maxillofacial Surgery. 2012;41(2):142–149. doi: 10.1016/j.ijom.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 27.Harada K, Watanabe M, Ohkura K, Enomoto S. Measure of bite force and occlusal contact area before and after bilateral sagittal split ramus osteotomy of the mandible using a new pressure-sensitive device: a preliminary report. J Oral Maxillofac Surg. 2000;58(4):370–3; discussion 73-4. doi: 10.1016/s0278-2391(00)90913-3. [DOI] [PubMed] [Google Scholar]
- 28.Oguz Y, Uckan S, Ozden AU, Uckan E, Eser A. Stability of locking and conventional 2 0-mm miniplate/screw systems after sagittal split ramus osteotomy: finite element analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108(2):174–7. doi: 10.1016/j.tripleo.2009.03.051. [DOI] [PubMed] [Google Scholar]
- 29.Burm JS, Hansen JE. The use of microplates for internal fixation of mandibular fractures. Plast Reconstr Surg. 2010;125(5):1485–92. doi: 10.1097/PRS.0b013e3181d51244. [DOI] [PubMed] [Google Scholar]
- 30.Ahmed SS, Bhardwaj S, Ansari MK, Farooq O, Khan AA. Role of 1 5 mm microplates in treatment of symphyseal fracture of mandible: A stress analysis based comparative study. J Oral Biol Craniofac Res. 2017;7(2):119–22. doi: 10.1016/j.jobcr.2017.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yeo XH, Ayoub A, Lee C, Byrne N, Currie WRJ. Neurosensory deficit following mandibular sagittal split osteotomy: A comparative study between positional screws and miniplates fixation. Surgeon. 2017;15(5):278–81. doi: 10.1016/j.surge.2016.07.001. [DOI] [PubMed] [Google Scholar]
- 32.Welsch G, Boyer R, Collings EW, editors Materials properties handbook: titanium alloys. ASM international. 1993 [Google Scholar]
- 33.Erkmen E, Simşek B, Yücel E, Kurt A. Comparison of different fixation methods following sagittal split ramus osteotomies using three-dimensional finite elements analysis Part 1: advancement surgery-posterior loading. Int J Oral Maxillofac Surg. 2005;34(5):551–8. doi: 10.1016/j.ijom.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 34.Erkmen E, Simşek B, Yücel E, Kurt A. Three-dimensional finite element analysis used to compare methods of fixation after sagittal split ramus osteotomy: setback surgery-posterior loading. Br J Oral Maxillofac Surg. 2005;43(2):97–104. doi: 10.1016/j.bjoms.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 35.Kröger H, Venesmaa P, Jurvelin J, Miettinen H, Suomalainen O, Alhava E. Bone density at the proximal femur after total hip arthroplasty. Clinical Orthopaedics and Related Research (1976-2007). 1998;352:66–74. [PubMed] [Google Scholar]
- 36.Oguz Y, Watanabe ER, Reis JM, Spin-Neto R, Gabrielli MA, Pereira-Filho VA. In vitro biomechanical comparison of six different fixation methods following 5-mm sagittal split advancement osteotomies. Int J Oral Maxillofac Surg. 2015;44(8):984–8. doi: 10.1016/j.ijom.2014.11.019. [DOI] [PubMed] [Google Scholar]
- 37.Peterson GP, Haug RH, Van Sickels J. A biomechanical evaluation of bilateral sagittal ramus osteotomy fixation techniques. J Oral Maxillofac Surg. 2005;63(9):1317–24. doi: 10.1016/j.joms.2005.05.301. [DOI] [PubMed] [Google Scholar]
- 38.Claes LE, Heigele CA, Neidlinger-Wilke C, Kaspar D, Seidl W, Margevicius KJ, et al. Effects of mechanical factors on the fracture healing process. Clin Orthop Relat Res. 1998;(355 Suppl):S132–47. doi: 10.1097/00003086-199810001-00015. [DOI] [PubMed] [Google Scholar]
- 39.Al-Moraissi EA, Ellis E. Stability of bicortical screw versus plate fixation after mandibular setback with the bilateral sagittal split osteotomy: a systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2016;45(1):1–7. doi: 10.1016/j.ijom.2015.09.017. [DOI] [PubMed] [Google Scholar]
- 40.Joss CU, Vassalli IM. Stability after bilateral sagittal split osteotomy advancement surgery with rigid internal fixation: a systematic review. J Oral Maxillofac Surg. 2009;67(2):301–13. doi: 10.1016/j.joms.2008.06.060. [DOI] [PubMed] [Google Scholar]