Abstract
Background
The mask mandate during the COVID-19 pandemic leads to communication challenges as sound energy gets reduced and the visual cues are lost due to the face mask. This study examines the impact of a face mask on sound energy and compares speech recognition performance between a basic and a premium hearing aid.
Methods
Participants watched four video clips (a female and a male speaker with and without a face mask) and repeated the target sentences in various test conditions. Real-ear measurement was performed to investigate the changes in sound energy in no mask, surgical, and N95 mask conditions.
Results
With the face mask on, sound energy significantly decreased for all types of masks. For speech recognition, the premium hearing aid showed significant improvement in the mask condition.
Conclusion
The findings emphasize and encourage health care professionals to actively use communication strategies, such as speaking slowly and reducing background noise, when interacting with individuals with hearing loss.
Keywords: Hearing loss, Speech perception, Mask, Hearing aid, COVID-19
1. Introduction
Hearing loss (HL) can have various symptoms and causes [1,2]. It could be caused by diseases in the ear (i.e., ear infection) and accompanied by tinnitus. It is reported in numerous studies that HL negatively affects quality of life [[3], [4], [5]]. There are multiple ways to compensate HL, but typically, the first step of hearing rehabilitation starts with hearing devices, such as hearing aids (HAs) [1,6]. A HA is a hearing device that aids individuals in hearing by amplifying sounds. The device is selected and optimized based on several factors including audiometric thresholds, family support, lifestyle, and communication needs [7]. HAs will enhance sound, but as both auditory and visual cues play a role in communication [[8], [9], [10], [11], [12], [13], [14]], it is still crucial for individuals to utilize communication strategies, such as speaking slowly and reducing background noise [15].
With the COVID-19 pandemic, due to the mask mandate, communication has become more challenging for individuals with HL [16,17]. Face masks are reported to attenuate mid-to-high frequency and individuals lose access to visual cues [[18], [19], [20], [21], [22]]. Nguyen et al. (2021) examined voice characteristics of 16 adults with and without a surgical and a KN95 mask. The participants recorded the vowel /a/, phrases in the Consensus Auditory-Perceptual Evaluation of Voice, and the Rainbow passage. Mean spectral levels in low (0–1000 Hz) and high (1–8000 Hz) frequency ranges were analyzed. While no significant effects were observed for the low frequency range, the spectral levels were reduced by 5.2 dB with the KN95 mask and by 2.0 dB with the surgical mask [20]. In 2020, Goldin and colleagues investigated the impact of various medical masks on speech signals. Using a head and torso simulator, the amount of sound attenuation was measured in four different conditions: no mask, simple mask, N95 mask 1 and N95 mask 2 [19]. Again, the N95 mask showed the most amount of sound attenuation (12 dB). The level of speech signals was decreased by 3 to 4 dB with the simple mask [19]. Brown et al. (2021) recruited 360 young and older adults to investigate the impact of face masks on speech intelligibility. The authors presented 150 sentences in which each sentence had four key words in no mask, surgical mask, black cloth mask with and without a paper filter, and cloth mask with a transparent mask. In the presence of noise, the participants' speech intelligibility significantly decreased with all types of masks [23]. Salamah et al. (2022) conducted a cross-sectional survey for 80 individuals and asked about hearing aids and communication with a face mask during the pandemic. The results showed that 40 % of the respondents reported that understanding speech is harder due to the face mask. 41.3 % of the respondents also mentioned that speech understanding is harder because they are unable to see the lip movements [16].
There are several literatures exploring communication difficulties and quality of life of individuals with HL and the benefit of hearing devices [16,17,24,25]. However, the comparison of performance between a basic and a premium hearing aid on speech performance has not been investigated yet. This study explores acoustic characteristics of a basic and a premium HA and compares their speech recognition performance in hearing-impaired listeners.
2. Material and methods
2.1. Participants
Thirty native Korean speakers with HL were enrolled in the study. The age range of the participants was from 24 to 69 years old with the mean age of 57.0 years (SD = 12.2). All participants had sensorineural HL with an asymmetry in hearing thresholds below 10 dB across testing frequencies (250, 500, 1000, 2000, 4000, and 8000 Hz) in both ears. The puretone averages were 50.4 dB in the right ear and 51.1 dB in the left ear. The average word recognition scores were 78 % in both ears. Individuals who were unable to watch TV at a distance of 1 m and those with otological pathology and neurological and mental disorders were excluded from the study. All experimental procedures were approved by Samsung Medical Center Institutional Review Board. Prior to testing, an informed consent document was obtained from the participants.
2.2. Puretone audiometry
Pure-tone audiometry was performed in a sound booth using insert earphones and an AudioStar Pro (Grason-Stadler, USA) audiometer.
2.3. Video recordings
Four video recordings were used in the study: a female speaker with and without a face mask and a male speaker with and without a face mask. A KF94 (‘Korea Filter with 94% filtration efficiency’) mask which is reported to be equivalent to N95 and FFP2 masks [26,27] was used for this study. The speakers recorded test sentences from the Korean Standard Sentences Lists for Adults (KSSL-A) which is a speech test widely used in Korea. The recordings were edited to have the female and male speakers alternating. The commercial editing tools from Adobe Systems, USA (Adobe Premiere Pro and Adobe Audition) were used.
2.4. Real-ear measurement
Following the instructions from the manufacturer [28], real-ear measurement (REM) in live mode was completed using Aurical Freefit (Natus Medical Inc., Denmark) to examine the sound pressure level (SPL) changes of sound stimuli. The testing was performed in three conditions: no mask, surgical mask, and N95 mask. Audio recordings of the KSSL-A list 1 for both speakers were used.
2.5. Speech recognition testing
The speech testing was conducted using the video recordings in a semi-anechoic chamber. Four conditions were used: no mask & no visual cues, no mask & visual cues, mask & no visual cues, and mask & visual cues. A basic (Oticon Siya 2) and a premium (Oticon More ONE) HA was used for performance comparison with additional features (i.e., noise reduction) off. The functionality of the HAs was also checked through electroacoustic testing. Wearing each set of the HAs, the participants sat on a chair located 1 m away from the loudspeaker, listened to the test sentences, and repeated them back to the tester. With the target sentences presented at 50 dBA, percent-correct scores were obtained. The testing took an hour and breaks were given as requested.
2.6. Statistical analysis
Statistical analysis was performed using SPSS version 26 (IBM Corporation, USA). As our results did not pass normality test, the Wilcoxon-signed rank test was performed. Differences in SPLs as well as speech recognition performance in test conditions were analyzed.
3. Results
3.1. The impact of face mask on sound pressure level
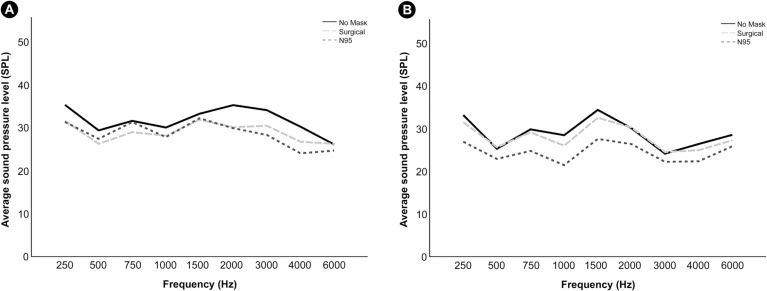
Fig. 1 illustrates the SPLs for both speakers. The mean SPLs were 31.6-, 28.9-, and 28.5-dB for the no mask, surgical, and N95 conditions, respectively for the female speaker. SPL differences between the conditions were 2.8 dB SPL (no mask – surgical) and 3.1 dB SPL (no mask – N95). For the male speaker, the mean SPL for the no mask condition was 28.9 dB. The mean SPLs for the surgical and N95 masks were 27.9- and 24.5-, respectively. SPL differences between the conditions were 0.9 dB (no mask – surgical) and 4.4 dB (no mask – N95). For both speakers, statistical significance was observed between no mask and surgical (P < 0.001) and between no mask and N95 conditions (P < 0.001). Comparing the no mask and the surgical mask condition, the maximum sound attenuation occurred at 2000 Hz (5.1 dB). Comparing the no mask and the N95 mask condition, the maximum sound attenuation was observed at 4000 Hz (6.2 dB). For the male speaker, for both conditions (no mask – surgical and no mask – N95), the SPLs decreased the most at 1000 Hz (2.5 dB for no mask – surgical and 7.0 dB for no mask – N95).
Fig. 1.
REM results of female (A) and male (B) speakers.
3.2. Performance comparison with and without visual cues
Table 1 describes performance differences between the basic and premium HAs. While the two devices did not show any statistical significance for speech recognition performance in the no mask condition regardless of the presence of the visual cues, they showed statistical significance when the speakers were wearing a mask (P = 0.014 for the no visual cues condition and P = 0.021 for the visual cues condition).
Table 1.
Statistical analysis of the HAs' speech recognition performance in the no visual cues and visual cues conditions (*P < 0.05).
| Mask | Visual cues | HAs (Inter quartile range) |
P | |
|---|---|---|---|---|
| Basic | Premium | |||
| No mask | No visual cues | 10 (0–40) | 20 (0–50) | 0.108 |
| Visual cues | 60 (20–90) | 70 (57.5–82.5) | 0.071 | |
| Mask | No visual cues | 5 (0–25) | 20 (0–40) | 0.014* |
| Visual cues | 10 (0–32.5) | 25 (7.5–50) | 0.021* | |
3.3. Speech recognition performance with and without a face mask
When the visual cues are available, both the basic and premium HA showed statistical significance on speech recognition in the no mask and mask conditions (P < 0.001 for both conditions). However, when the visual cues are unavailable, no statistical significance on speech recognition was observed in the no mask and mask conditions (p = 0.201 for the basic HA and p = 0.958 for the premium HA).
4. Discussion
This study investigates the impact of face mask on SPLs and compares speech recognition performance between the basic and the premium HA. Our findings showed that when the speakers were wearing a face mask, individuals' speech recognition performance statistically improved with the premium HA in both no visual cues and visual cues condition. Although the two HAs did not show any significance performance differences in the no visual cues condition, when the visual cues were available, the premium HA showed statistically significant speech recognition performance even if the speaker was wearing a face mask. Similar to pre-existing studies [8,10,11,14,29,30], significant improvement in speech recognition performance indicates that visual cues are helpful for communication. The authors believe that the premium HA showed better performance as it generally has more channels for signal processing and faster processing speed than the basic HA. Channel refers to different areas or groups of frequencies that HAs will process. If HAs have two channels, it means that the HAs will break the frequencies into two different ranges for processing. If HAs have 10 channels, the HAs will break the frequencies into ten different ranges for sound processing, allowing more specific adjustments or programming. The REM results also demonstrated significant reduction in SPLs with face masks. For both speakers, the lowest mean SPLs were observed with the N95 mask. The maximum attenuation of sound was observed at 2000- (no mask – surgical) and 4000 Hz (no mask – N95) for the female speaker and at 1000 Hz (no mask – surgical and no mask – N95) for the male speaker. Findings of this study are in line with previous studies that speech frequencies, which are frequencies that are critical for speech understanding, are affected by face masks [19,31,32].
In sum, these findings heighten the importance of the active use of communication strategies. Regardless of the pandemic, communication difficulty arises when visual information, such as lip movements and facial expressions, are unavailable. On a personal level, this communication difficulty can affect one-on-one conversations. On a professional level, communication difficulty could lead to poor interactions between healthcare professionals and patients and quality of care [[33], [34], [35], [36], [37], [38], [39], [40]]. Kwame and Petrucka (2021) conducted a study to identify barriers and facilitators of patient-centered care and communication. The authors reported that poor communication between healthcare professionals and patients could affect outcomes and perceptions of the quality of care [40]. Environment factors included noisy surroundings and lighting. These days, most countries are no longer enforcing the mask mandate. Even if the preventative measures are dropped for COVID-19, it is essential to keep in mind that other respiratory diseases could arise in the future, so healthcare professionals are strongly encouraged to remind themselves about communication strategies and use them when interacting with individuals with HL.
Future studies with a larger sample size as well as various listening conditions are necessary. Including a noise condition could reflect the real-world listening environment. Recruiting participants with different characteristics of HL would allow us to compare the performance between the HAs at a more specific level.
5. Conclusions
The findings of the study showed that when the speakers were wearing a face mask, individuals' speech recognition performance statistically improved with the premium HA, emphasizing the active use of communication strategies.
Ethics approval and consent to participate
All experimental procedures were approved by Samsung Medical Center Institutional Review Board. Prior to testing, an informed consent document was obtained from the participants.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Funding
This research was supported by a grant of Patient-Centered Clinical Research Coordinating Center funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI19C0481, HC19C0128).
Copyright transfer
“In consideration of the American Journal of Otolaryngology's reviewing and editing my submission, “Comparison of speech recognition performance with and without a face mask between a basic and a premium hearing aid in hearing-impaired listeners”, the author(s) undersigned transfers, assigns and otherwise conveys all copyright ownership to Elsevier Inc. in the event that such work is published in the American Journal of Otolaryngology.”
Hye Yoon Seol, Mini Jo, Heejung Yun, Jin Gyun Park, Hye Min Byun, Il Joon Moon.
CRediT authorship contribution statement
H·Y·S, M.J, J.G.P., H.M.B, and I.J.M conceptualized the study, M.J and H·Y conceived the experiments, J.G.P., H.M.B, and I.J.M reviewed the concept. M.J and H.Y conducted the experiments, and H.Y·S analyzed the results. H.Y·S wrote the main paper and all authors reviewed the manuscript.
Declaration of competing interest
No potential conflict of interest relevant to this article was reported.
Acknowledgements
The authors rented the hearing aids from Demant Korea.
References
- 1.Yueh B., Shapiro N., MacLean C.H., Shekelle P.G. Screening and management of adult hearing loss in primary care: scientific review. JAMA. 2003;289(15):1976–1985. doi: 10.1001/jama.289.15.1976. Apr 16. [DOI] [PubMed] [Google Scholar]
- 2.Lasak J.M., Allen P., McVay T., Lewis D. Hearing loss: diagnosis and management. Prim Care. 2014;41(1):19–31. doi: 10.1016/j.pop.2013.10.003. Mar. [DOI] [PubMed] [Google Scholar]
- 3.Tognola G., Mainardi A., Vincenti V., Cuda D. Benefit of hearing aid use in the elderly: the impact of age, cognition and hearing impairment. Acta Otorhinolaryngol Ital. 2019;39(6):409–418. doi: 10.14639/0392-100X-2165. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li-Korotky H.S. Age-related hearing loss: quality of care for quality of life. Gerontologist. 2012;52(2):265–271. doi: 10.1093/geront/gnr159. Apr. [DOI] [PubMed] [Google Scholar]
- 5.Punch J.L., Hitt R., Smith S.W. Hearing loss and quality of life. J Commun Disord. 2019;78:33–45. doi: 10.1016/j.jcomdis.2019.01.001. [DOI] [PubMed] [Google Scholar]
- 6.Seol H.Y., Moon I.J. Hearables as a gateway to hearing health care. Clin Exp Otorhinolaryngol. 2022;15(2):127–134. doi: 10.21053/ceo.2021.01662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dillon H. Boomerang Press; Sydney: 2012. Hearing aids. [Google Scholar]
- 8.Taitelbaum-Swead R., Fostick L. Auditory and visual information in speech perception: a developmental perspective. Clin Linguist Phon. 2016;30(7):531–545. doi: 10.3109/02699206.2016.1151938. [DOI] [PubMed] [Google Scholar]
- 9.Cienkowski K.M., Carney A.E. Auditory-visual speech perception and aging. Ear Hear. 2002;23(5):439–449. doi: 10.1097/00003446-200210000-00006. Oct. [DOI] [PubMed] [Google Scholar]
- 10.Summerfield Q. Lipreading and audio-visual speech perception. Philos Trans R Soc Lond B Biol Sci. 1992;335(1273):71–78. doi: 10.1098/rstb.1992.0009. Jan 29. [DOI] [PubMed] [Google Scholar]
- 11.Summerfield Q. Use of visual information for phonetic perception. Phonetica. 1979;36(4–5):314–331. doi: 10.1159/000259969. [DOI] [PubMed] [Google Scholar]
- 12.Massaro D.W. Mit Press; Cambridge, Mass: 1998. Perceiving talking faces: From speech perception to a behavioral principle. [Google Scholar]
- 13.Granström B., House D. Audiovisual representation of prosody in expressive speech communication. Speech Commun. 2005;46(3–4):473–484. Jul. [Google Scholar]
- 14.Seol H.Y., Kang S., Lim J., Hong S.H., Moon I.J. Feasibility of virtual reality audiological testing: prospective study. JMIR Serious Games. 2021;9(3) doi: 10.2196/26976. Aug. e26976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mckee M.M., Moreland C., Atcherson S.R., Zazove P. Hearing loss: communicating with the patient who is deaf or hard of hearing. FP essentials. 2015;434:24–28. [PubMed] [Google Scholar]
- 16.Salamah M.A., Al-Ahmadi A., Arabi S., Alsaleh W.A., Aljuwayyan A., Yousef M.F., et al. The influence of the COVID-19 pandemic on the hearing impaired. Cureus. 2022;14(11) doi: 10.7759/cureus.31348. Nov. e31348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Poon B.T., Jenstad L.M. Communication with face masks during the COVID-19 pandemic for adults with hearing loss. Cogn Res Princ Implic. 2022;7(1):24. doi: 10.1186/s41235-022-00376-8. Mar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bottalico P., Murgia S., Puglisi G.E., Astolfi A., Kirk K.I. Effect of masks on speech intelligibility in auralized classrooms. J Acoust Soc Am. 2020;148(5):2878. doi: 10.1121/10.0002450. Nov. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goldin A., Weinstein B., Shiman N. How do medical masks degrade speech perception. Hear Rev. 2020;27(5):8–9. Apr. [Google Scholar]
- 20.Nguyen D.D., McCabe P., Thomas D., Purcell A., Doble M., Novakovic D., et al. Acoustic voice characteristics with and without wearing a facemask. Sci Rep. 2021;11(1):5651. doi: 10.1038/s41598-021-85130-8. Mar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Corey R.M., Jones U., Singer A.C. Acoustic effects of medical, cloth, and transparent face masks on speech signals. J Acoust Soc Am. 2020;148(4):2371. doi: 10.1121/10.0002279. Oct. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moon I.-J., Jo M., Kim G.-Y., Kim N., Cho Y.-S., Hong S.-H., et al. How does a face mask impact speech perception? Healthcare. 2022;10(9):1709. doi: 10.3390/healthcare10091709. MDPI. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brown V.A., Van Engen K.J., Peelle J.E. Face mask type affects audiovisual speech intelligibility and subjective listening effort in young and older adults. Cogn Res Princ Implic. 2021;6(1):49. doi: 10.1186/s41235-021-00314-0. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sonnichsen R., To GL, Hohmann V., Hochmuth S., Radeloff A. Challenging times for cochlear implant users - effect of face masks on audiovisual speech understanding during the COVID-19 pandemic. Trends Hear. 2022;26 doi: 10.1177/23312165221134378. Jan-Dec. 23312165221134378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Çildir B., Tokgoz-Yilmaz S. The benefit of hearing aids in adults with hearing loss during the Covid–19 pandemic. J Surg Med. 2022;6(1):59–63. [Google Scholar]
- 26.Diagnostics devices, MFDS-regulated mask information; 2020 [cited 2022 Dec 20]. Available from: https://mfds.go.kr/eng/brd/m_65/view.do?seq=11&srchFr=&srchTo=&srchWord=mask&srchTp=7&itm_seq_1=0&itm_seq_2=0&multi_itm_seq=0&company_cd=&company_nm=&page=1.
- 27.Park S.H. Personal protective equipment for healthcare workers during the COVID-19 pandemic. Infect Chemother. 2020;52(2):165–182. doi: 10.3947/ic.2020.52.2.165. Jun. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Natus Medical Denmark ApS. Aurical® Freefit Otosuite PMM module Otosuite counseling and simulations module user guide; 2022 [cited 2022 Dec 20]. Available from: https://partners.natus.com/asset/resource/file/otometrics/asset/2021-06/7-50-1220-EN_14.PDF.
- 29.Sumby W.H., Pollack I. Visual contribution to speech intelligibility in noise. J Acoust Soc Am. 1954;26(2):212–215. [Google Scholar]
- 30.Rosenblum L.D. In: The handbook of speech perception. Pisoni D.B., Remez R.E., editors. Blackwell Publishing; Oxford: 2008. Primacy of multimodal speech perception; pp. 51–78. [Google Scholar]
- 31.Steeneken H.J., Houtgast T. Mutual dependence of the octave-band weights in predicting speech intelligibility. Speech Commun. 1999;28(2):109–123. Jun. [Google Scholar]
- 32.Giuliani N. For speech sounds, 6 feet with a mask is like 12 feet without. Leader Live. 2020 doi: 10.1044/leader.aea.25112020.26/full/. November 2. cited 2022 Dec 20. Available from: November 2. cited 2022 Dec 20. Available from: [DOI] [Google Scholar]
- 33.Eby TL, Arteaga AA, Spankovich C. Otologic and Audiologic considerations for COVID-19. Otolaryngol Head Neck Surg 2020 Jul;163(1):110–1. [DOI] [PubMed]
- 34.Pamungkasih W., Sutomo A.H., Agusno M. Description of patient acceptance of use of mask by doctor at poly out-patient care Puskesmas. Bantul Rev Primary Care Pract Edu (Kajian Praktik dan Pendidikan Layanan Primer) 2019;2(2):70–75. [Google Scholar]
- 35.Khan T., Hassali M., Al-Haddad M. Patient-physician communication barrier: a pilot study evaluating patient experiences. J Young Pharm. 2011;3(3):250–255. doi: 10.4103/0975-1483.83778. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Scheier D.B. Barriers to health care for people with hearing loss: a review of the literature. J N Y State Nurses Assoc. 2009;40(1):4–10. Spring-Summer. [PubMed] [Google Scholar]
- 37.Marler H., Ditton A. “I’m smiling back at you”: exploring the impact of mask wearing on communication in healthcare. Int J Lang Commun Disord. 2021;56(1):205–214. doi: 10.1111/1460-6984.12578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Krautscheid L.C. Improving communication among healthcare providers: preparing student nurses for practice. Int J Nurs Educ Scholarsh. 2008;5(1) doi: 10.2202/1548-923X.1647. Oct. [DOI] [PubMed] [Google Scholar]
- 39.Constand M.K., MacDermid J.C., Dal Bello-Haas V., Law M. Scoping review of patient-centered care approaches in healthcare. BMC Health Serv Res. 2014;14:271. doi: 10.1186/1472-6963-14-271. Jun. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kwame A., Petrucka P.M. A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward. BMC Nurs. 2021;20(1):158. doi: 10.1186/s12912-021-00684-2. Sep. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.