Abstract
Jejunal diverticula are rare, and small bowel diverticular disease resulting in volvulus can lead to severe complications; as symptoms are non-specific, many patients are misdiagnosed and treated wrongly for other conditions. When a small bowel volvulus is detected, urgent surgical treatment is needed to avoid troublesome difficulties. We present the case of a 36-year-old woman who presented to the emergency room with an acute abdomen due to small bowel obstruction. After further testing, a volvulus was detected and promptly treated. Jejunal diverticula that caused a small bowel volvulus was the final diagnosis.
INTRODUCTION
Since the first descriptions by Somerling and Sir Asley Cooper, jejunal diverticulum has been recognized as a rare pathology (0.2–7% of the adult population) [1–3]. Clinically, they can be asymptomatic or present with nonspecific gastrointestinal symptoms [2]. Other rarer presentations can be due to complications like hemorrhage, perforation, intussusception, volvulus, malabsorption and small bowel obstruction [1, 2]. Complete resection of the affected bowel segment is the treatment of choice [3]. We present the case of a 36-year-old patient with a long history of nonspecific gastrointestinal symptoms misdiagnosed as irritable bowel syndrome. Suddenly, she presented to the emergency room with bowel obstruction, and a small bowel volvulus (SBV) caused by jejunal diverticula was the final diagnosis.
CASE PRESENTATION
The patient is a 36-year-old woman with a history of recurrent episodes of diarrhea, flatulence, mild abdominal pain and constipation since her teenage years; however, at all medical visits, these symptoms were never investigated, no additional tests were performed and she was treated as dyspepsia and irritable bowel syndrome for years.
Suddenly, she presented with severe pain in her upper abdomen. At first, it was mild and was accompanied by nausea, vomits and inability to pass gas or stool. As time passed, the pain became unbearable; therefore, she was brought to the emergency room by her family.
On clinical evaluation, a dehydrated patient with severe abdominal pain with tenderness was encountered; her vitals were normal, but a 5 x 5 cm non-painful mobile mass was detected on her upper abdomen. No other masses or lymph nodes were seen at that time. Due to this, abdominal computed tomography (CT) was requested, revealing dilated small bowel loops >6 cm with thickened wall, whirl sign and a small amount of free liquid in her abdomen (Fig. 1A and B).
Figure 1.
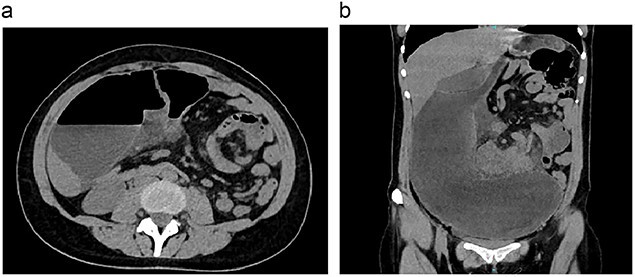
(a) CT, showing bowel loops distended. (b) CT, the volvulus of the small bowel is seen.
With these findings, surgical consultation was required, and after obtaining consent, surgery was decided.
On laparotomy, about 400 ccs of inflammatory liquid was discovered; also, 200 cm away from the ileocecal valve, about 60 cm of bowel was extremely dilated, reaching 13 cm and was volvulated in a 270-degree fashion, completely obstructing the bowel with signs of ischemia. With these findings, complete bowel resection of the ileum was completed and a side-to-side isoperistaltic anastomosis with a mechanical stapler was performed without complications; a drain was placed, and surgery was completed without complications (Fig. 2).
Figure 2.

Surgery, small bowel volvulus is completely removed.
Pathology reported a 3.8 x 1.5 cm true jejunal diverticula that caused a SBV. The wall of the small bowel was thickened and had multiple areas of ischemia. No signs of malignancy or any compromise of the lymph nodes were detected (Fig. 3A and B).
Figure 3.
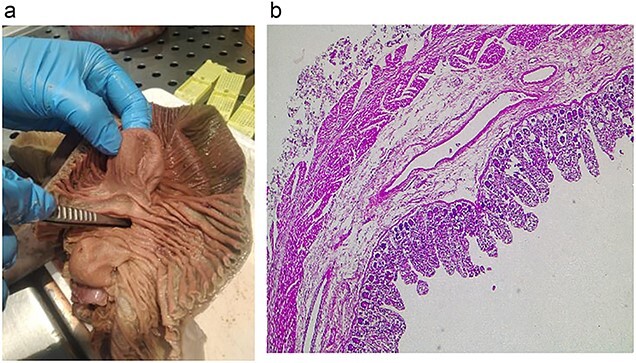
(a) Pathology, the lumen of the diverticulum is shown. (b) Pathology, the diverticulum is seen with all bowel layers.
Her postoperative course was unremarkable, she completed a course of antibiotics and after a full diet was initiated, she was discharged without complications. On follow-ups, she is doing well.
DISCUSSION
SBV is defined as the twisting of the small bowel around its mesenteric axis [1, 2]. If untreated, it can lead to severe complications, including bowel obstruction, ischemia, infarction, perforation and death [1]. This complication is usually found in the neonatal period and is extremely rare in adults (0.2–1.3%) [3, 4]. SBV can be categorized as primary or secondary [1, 2]. Primary SBV occurs in patients with no congenital malrotation, bands or postoperative adhesions [1, 4]. It is believed to be due to the absence of food during daylight hours and the consumption of a single, large, high-fiber meal at night [1, 5]. Secondary SMB often occurs in older patients and is caused by postoperative adhesions, tumors, pregnancy, hematoma and diverticulums [1].
Jejunal diverticula are the intestine’s outpouchings arising from the jejunum’s antimesenteric border [2]. They can be categorized as true when it involves all bowel wall layers [2, 3]. Alternatively, when they are formed by the mucosa and submucosa without any smooth muscle layer, they are referred to as false diverticula [2, 4]. Jejunal and ileal diverticula are extremely rare compared with other diverticulums of the gastrointestinal tract and occur in <1% of the population [1, 5]. The etiology of jejunal diverticulosis is still under research [1]. However, it is believed that jejunal diverticula are caused by a combination of abnormal peristalsis, intestinal dyskinesia and high segmental intraluminal pressures. They are also most commonly seen in patients with connective tissue diseases such as systemic lupus erythematosus around the sixth decade of life [2, 4, 6]. Jejunal diverticula symptoms are nonspecific since patients may be completely asymptomatic (80% of the patients) or present with symptoms clinically indistinguishable from bowel obstruction, acute abdomen, hemorrhage or malabsorption due to the bacterial overgrowth within the diverticulum (can appear in up to 10% of cases) [1, 7]. As a result, these chronic clinical manifestations may be misdiagnosed as dyspepsia and irritable bowel syndrome, which delays the correct diagnosis [2, 5], as it happened to our patient. Edwards et al. have described a triad in such patients as; flatulent dyspepsia, epigastric pain and flatulence 1 or 2 h after meals [8].
Complications, including inflammation, obstruction, perforation, hemorrhage and malabsorption, occur in 10–30% of cases, and up to 30% of these patients will need surgical intervention [1, 5].
Mechanical bowel obstruction occurs due to jejunal diverticula in up to 4.6% of cases because the segment of the bowel involved, which is fluid-filled and heavier than the uninvolved part, rotates the bowel and causes an obstruction [4]. In addition, if the diverticula is large enough, it can induce volvulus due to adhesions or because it triggers an abnormal rotation of the small bowel [2, 9]. In our case, the patient had a history of recurrent abdominal pain episodes because of the jejunal diverticula that led to obstruction and volvulus.
Diagnosing asymptomatic patients is difficult since X-rays or CTs may fail to detect jejunal diverticula and can only be revealed by radiological contrast studies [1, 5]. Other procedures like capsule endoscopy and double-balloon can also be helpful [2, 8]. When symptomatic, CT is usually the recommended imaging method as it can reveal the ‘whirl sign,’ which refers to a whirling or spiral shape of the mesenteric vessels [2, 9]. It is a sensitive marker of SBV, predicting the need for surgery [1], as was found in our patient. Asymptomatic jejunal diverticulosis does not require operative management unless complications or symptoms arise; when this happens, complete resection of the involved segment must be achieved [1, 10].
In our case, surgery was needed due to the clinical findings and the CT. However, if a more thorough diagnosis had been made, these complications might not have occurred because the diverticulum would have been detected earlier, proving that no symptoms should be overlooked.
A large subgroup of patients with a history of nonspecific gastrointestinal symptoms, such as diarrhea, pain and flatulence, may be misdiagnosed and present with an undiagnosed jejunal diverticulum. Significant clinical insight is needed in these patients, as they may benefit from early intervention to avoid the associated morbidity.
CONCLUSIONS
Even if jejunal diverticula is rare, it must always be in the differential when approaching a patient with non-specific gastrointestinal symptoms. Because of the rarity of the entity, diagnosis is often delayed, resulting in unnecessary complications like volvulus, which, if seen, must be treated with prompt surgery and resection.
Contributor Information
Gabriel A Molina, Department of General Surgery Hospital Metropolitano & Universidad San Francisco de Quito (USFQ), Quito, Ecuador.
Rommel H Ojeda, Department of General Surgery, IESS-Quito-Sur, Quito, Ecuador.
Galo Jimenez, Department of General Surgery, IESS-Quito-Sur, Quito, Ecuador.
Andrea Heredia, Department of General Surgery, IESS-Quito-Sur, Quito, Ecuador.
C Augusto Cadena, Department of General Surgery, IESS-Quito-Sur, Quito, Ecuador.
Davor Martic, School of Medicine, Pontificia Universidad Católica del Ecuador, Quito, Ecuador.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
DATA AVAILABILITY
The data underlying this article will be shared on reasonable request to the corresponding author.
References
- 1. Woods. Acquired jejunoileal diverticulosis and its complications: a review of the literature. Am Surg 2013;74:849–54. [PubMed] [Google Scholar]
- 2. Patel VA, Jefferis H, Spiegelberg B, Iqbal Q, Prabhudesai A, Harris S. Jejunal diverticulosis is not always a silent spectator: a report of 4 cases and review of the literature. World J Gastroenterol 2008;14:5916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kassahun WT. Complicated small-bowel diverticulosis: a case report and review of the literature. World J Gastroenterol 2007;13:2240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Johnson KN, Fankhauser GT, Chapital AB, Merritt MV, Johnson DJ. Emergency management of complicated jejunal diverticulosis. Am Surg 2014;80:600–3. [PubMed] [Google Scholar]
- 5. Hu J-L. Midgut volvulus due to jejunal diverticula: a case report. World J Gastroenterol 2012;18:5826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chou CK, Mark C-W, Wu R-H, Chang J-M. Large diverticulum and volvulus of the small bowel in adults. World J Surg 2004;29:80–2. [DOI] [PubMed] [Google Scholar]
- 7. Li X-B, Guan W-X, Gao Y. Multislice computed tomography angiography findings of chronic small bowel volvulus with jejunal diverticulosis. Jpn J Radiol 2010;28:469–72. [DOI] [PubMed] [Google Scholar]
- 8. Mohi RS, Moudgil A, Bhatia SK, Seth K, Kaur T. Complicated Jejunal diverticulosis: small bowel volvulus with obstruction. Iran J Med Sci 2016;41:548–51. [PMC free article] [PubMed] [Google Scholar]
- 9. Porter HW. A case of a chronic volvulus of the jejunum due to multiple jejunal diverticula. Br J Surg 1946;34:218–9. [DOI] [PubMed] [Google Scholar]
- 10. Igwe PO, Ray-Offor E, Allison AB, Alufohai EF. Volvulus complicating jejunal diverticulosis: a case report. Int J Surg Case Rep 2015;9:61–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.


