Abstract
Bacillus anthracis is one of the most genetically homogeneous pathogens described, making strain discrimination particularly difficult. In this paper, we present a novel molecular typing system based on rapidly evolving variable-number tandem repeat (VNTR) loci. Multiple-locus VNTR analysis (MLVA) uses the combined power of multiple alleles at several marker loci. In our system, fluorescently labeled PCR primers are used to produce PCR amplification products from eight VNTR regions in the B. anthracis genome. These are detected and their sizes are determined using an ABI377 automated DNA sequencer. Five of these eight loci were discovered by sequence characterization of molecular markers (vrrC1, vrrC2, vrrB1, vrrB2, and CG3), two were discovered by searching complete plasmid nucleotide sequences (pXO1-aat and pXO2-at), and one was known previously (vrrA). MLVA characterization of 426 B. anthracis isolates identified 89 distinct genotypes. VNTR markers frequently identified multiple alleles (from two to nine), with Nei's diversity values between 0.3 and 0.8. Unweighted pair-group method arithmetic average cluster analysis identified six genetically distinct groups that appear to be derived from clones. Some of these clones show worldwide distribution, while others are restricted to particular geographic regions. Human commerce doubtlessly has contributed to the dispersal of particular clones in ancient and modern times.
Anthrax is a disease that has plagued mankind for millennia. The earliest suspected reports occur in Sanskrit manuscripts and in the biblical book of Exodus (4). More recently, anthrax played an important role in the advancement of modern microbiology with the development of Koch's postulates and of the first vaccine using an attenuated bacterial strain (12, 16). While anthrax currently affects mostly livestock and wildlife around the world, it can and does kill humans (4). Indeed, the great current interest in anthrax is due to its potential as a bioterrorism and biowarfare agent (3, 4). Bacillus anthracis spores can remain stable for decades and can be readily packaged into biological weapons (3). This same longevity may greatly influence the ecology and evolution of this pathogen. The initiating spores for an anthrax outbreak may emanate from a single long-deceased victim. This resting stage probably greatly reduces the rate of evolutionary change, and this may contribute to the extremely homogeneous nature of B. anthracis (10).
Numerous studies have demonstrated the lack of molecular polymorphism within B. anthracis (6, 7, 10). Previous analyses using amplified fragment length polymorphisms (AFLP) revealed only 30 differences among >1,000 DNA fragments (10). In addition, many of these AFLP markers have low diversity values and little discriminatory power. Comparative analysis of the protective antigen gene sequence in 25 diverse strains found only five differences across 2,500 nucleotides (18). An exception to this trend was revealed by the work of Andersen et al. (1), who sequenced a previously identified arbitrarily primed PCR marker (7). They found the vrrA open reading frame (ORF), which contained a variable-number tandem repeat (VNTR) sequence. In contrast to the extremely monomorphic nature of the genome, five different allelic states were observed in the vrrA VNTR among diverse strains (1, 7, 8). This demonstrated that even highly similar B. anthracis strains could be differentiated if polymorphic genomic regions could be identified and analyzed. Such discrimination is essential if molecular epidemiology is to aid in the understanding and control of anthrax.
Molecular typing of pathogens has long been a part of pathogen identification and control and has recently been accelerating with new technologies. Traditionally, serotyping has been extremely valuable and has often been able to identify important cellular components associated with virulence. While serotyping will continue to be an important tool, it often has limited discriminatory power, resolving pathogens into only a few types. Multilocus enzyme electrophoresis provides a multiple-factor genetic analysis, with as many as 40 genetic loci analyzed (2). Moreover, enzyme loci frequently have more than two alleles, providing increased genetic resolution per locus. However, DNA typing is more rapid and less expensive and has an even greater capacity for genetic dissection of bacterial pathogens. It is limited only by the genome size and the technology. Because most microbial genomes consist of millions of nucleotides, technology is invariably limiting. Pulsed-field gel electrophoresis (PFGE) can resolve very large and sometimes polymorphic DNA restriction fragments. PFGE typing has proven generally applicable to many pathogens and has notable successes in epidemiological tracking (14). However, this is a cumbersome technology that cannot easily handle very large sample sets. Moreover, PFGE data sets are not easily standardized for transfer throughout the public health community. Ribotyping uses restriction fragment length polymorphisms associated with rRNA genes (17) and, again, is generally applicable to all bacteria. However, it is limited by the number of ribosomal loci in the genome. Such methods often do not distinguish among closely related species, and many strains within a species show identical patterns (e.g., Bacillus cereus and B. anthracis).
Recently, PCR-based methods have become increasingly important to molecular typing efforts. These approaches include AFLPs, repetitive element polymorphisms-PCR, randomly amplified polymorphic DNA, and arbitrarily primed PCR (24, 26, 27). The power of PCR-based methods is the ease with which they can be applied to many bacterial pathogens and their multilocus discrimination. These methods have proven valuable for genetic dissection of pathogens for which other approaches have failed. However, a limitation of many PCR-based approaches is the biallelic (binary) nature of their data, frequently, the presence or absence of a marker fragment. Finally, comparative gene sequencing is becoming feasible for strain characterization and can be performed at multiple loci. In its best applications, multiple-locus sequence typing (MLST) can provide data for multiple alleles (haplotypes) spread across dispersed genomic locations (13). Nucleotide data are well understood, standardized into four defined categories, and easily analyzed using phylogenetic approaches. If sufficient nucleotide diversity is present, MLST can distinguish among both species and strains. While routine clinical MLST is still unfeasible, hybridization arrays (e.g., chip technology) could make single-nucleotide polymorphisms a mainstream approach to pathogen typing in the future (22).
One of the most recent developments in molecular typing involves the analysis of VNTR sequences (5, 11, 23). Short nucleotide sequences that are repeated multiple times often vary in copy number, creating length polymorphisms that can be detected easily by PCR using flanking primers. VNTRs appear to contain greater diversity and, hence, greater discriminatory capacity than any other type of molecular typing system (19, 23). Many bacteria have VNTRs, although development of the PCR primers for these markers is specific to each pathogen. In this report, we describe a multiple-locus VNTR analysis (MLVA) system that uses eight marker loci to discriminate among different B. anthracis isolates. Five of these markers (vrrC1, vrrC2, vrrB1, vrrB2, and CG3) were identified by the nucleotide sequence characterization of B. anthracis AFLP markers (10). One marker (vrrA) was identified previously (1), and two were identified by analysis of the pXO1 and pXO2 plasmid sequences (pXO1-aat and pXO2-at) (14). Because of the nearly monomorphic molecular nature of B. anthracis, MLVA may be the only reasonable method with which to study the diversity, evolution, and molecular epidemiology of this pathogen. Our analysis of a worldwide B. anthracis collection reveals 89 distinct MLVA genotypes that cluster into about six major genetic groups that represent worldwide clones.
MATERIALS AND METHODS
DNA preparation.
In this study, we have analyzed 426 B. anthracis isolates from around the world (Table 1). These samples include previously described samples (8, 10) plus more than 300 additional clinical and environmental isolates (Table 1). DNA from each isolate was obtained by either large-batch procedures (8, 10) or a greatly simplified approach requiring only heat lysis of a single colony. In this abbreviated protocol, B. anthracis cells were streaked onto blood agar plates and then incubated at 37°C overnight. A single colony from each plate was transferred into a microcentrifuge tube containing 200 μl of TE (Tris-HCl [pH 8.0], 1.0 mM EDTA). The colony was resuspended by vortexing or repetitive pipetting. The cellular suspension was heated to 95°C for 20 min and then cooled to room temperature. Cellular debris was removed by centrifugation at 15,000 × g for 1 min. Centrifugation was conducted inside a biosafety cabinet to contain any aerosols. The supernatant was then transferred to a new tube for storage. One microliter of the lysate contains sufficient template to support a single PCR, which means that this procedure can supply template for 200 reactions. We periodically optimize our reactions by titrating the heat lysate template concentrations using serial dilutions. Results obtained using either DNA preparation protocol gave the same MLVA results. However, the heat lysis procedure is much more rapid and easily adapted to large-scale processing of samples and was the method used for most of the samples in this study.
TABLE 1.
B. anthracis isolates
| Continent | Country | No. of isolates | No. of genotypes |
|---|---|---|---|
| Africa | Mozambique (MOZ) | 5 | 4 |
| Namibia (NAM) | 23 | 7 | |
| South Africa (SAF) | 127 | 9 | |
| Tanzania (TANZ) | 5 | 1 | |
| Zambia (ZAM) | 17 | 2 | |
| Zimbabwe (ZIM) | 4 | 2 | |
| Subtotal | 181 | 18 | |
| Asia | China | 7 | 5 |
| India | 3 | 2 | |
| Indonesia (INDO) | 5 | 4 | |
| Pakistan (PAK) | 4 | 4 | |
| S. Korea (KOR) | 4 | 2 | |
| Turkey (TURK) | 41 | 12 | |
| Subtotal | 64 | 31 | |
| Australia | 30 | 3 | |
| Europe | Croatia (CRO) | 1 | 1 |
| France (FRA) | 8 | 3 | |
| Germany (GER) | 9 | 5 | |
| Hungary (HUN) | 3 | 2 | |
| Ireland (IRE) | 1 | 1 | |
| Italy | 3 | 2 | |
| Norway (NOR) | 5 | 5 | |
| Poland (POL) | 1 | 1 | |
| Slovakia (SLO) | 3 | 2 | |
| Spain (SPA) | 2 | 1 | |
| Switzerland (SWI) | 2 | 2 | |
| United Kingdom (UK) | 19 | 10 | |
| Subtotal | 57 | 32 | |
| North America | Canada (CAN) | 51 | 7 |
| Haiti | 1 | 1 | |
| United States (USA) | 32 | 16 | |
| Subtotal | 84 | 22 | |
| South America | Argentina (ARG) | 2 | 2 |
| Brazil (BRA) | 1 | 1 | |
| Subtotal | 3 | 3 | |
| All | 419 | 89 |
MLVA PCR.
MLVA reaction primers (Table 2) were designed to provide uniquely labeled or sized amplicons for every allele at the eight VNTR loci. PCR amplification of all eight VNTR loci was routinely accomplished using four reactions. Two of the amplicons (vrrC1 and vrrC2) are significantly larger than the others and, in addition, are amplified using partially complementary primers. Likewise, vrrB1 and vrrB2 are amplified using complementary primers. Limited unique sequences in these repeated regions necessitated the overlap of these primers and thus required these amplicons to be divided into separate PCRs. Large amplicons tend to be outcompeted by small amplicons and thus require separate PCRs. These restraints led to a four-reaction design in which vrrB1 is grouped with CG3 and vrrA, vrrB2 is grouped with pXO1-aat and pXO2-at, vrrC1 is amplified alone, and vrrC2 is amplified alone.
TABLE 2.
MLVA primers used to DNA type B. anthracis
| Marker locus | Primers | Primer sequence | Dye labela | Tm (°C) |
|---|---|---|---|---|
| vrrA | vrrA-f1-fam | CAC AAC TAC CAC CGA TGG CAC A | Fam | 71.0 |
| vrrA-r1 | GCG CGT TTC GTT TGA TTC ATA C | None | 69.7 | |
| vrrB1 | vrrB1-f1-fam | ATA GGT GGT TTT CCG CAA GTT ATT C | Fam | 70.0 |
| vrrB1-r1 | GAT GAG TTT GAT AAA GAA TAG CCT GTG | None | 69.0 | |
| vrrB2 | vrrB2-f1-fam | CAC AGG CTA TTC TTT ATC AAA CTC ATC | Fam | 72.0 |
| vrrB2-r1 | CCC AAG GTG AAG ATT GTT GTT GA | None | 68.8 | |
| vrrC1 | vrrC1-f1 | GAA GCA AGA AAG TGA TGT AGT GGA C | None | 66.8 |
| vrrC1-r1-fam | CAT TTC CTC AAG TGC TAC AGG TTC | Fam | 67.5 | |
| vrrC2 | VrrC2-f1-hex | CCA GAA GAA GTG GAA CCT GTA GCA C | Hex | 70.9 |
| vrrC2-r1 | GTC TTT CCA TTA ATC GCG CTC TAT C | None | 70.6 | |
| CG3 | CG3-f1-ned | TGT CGT TTT ACT TCT CTC TCC AAT AC | Ned | 66.2 |
| CG3-r1 | AGT CAT TGT TCT GTA TAA AGG GCA T | None | 66.2 | |
| pXO1-aat | pXO1-AAT-f3-fam | CAA TTT ATT AAC GAT CAG ATT AAG TTC A | Fam | 66.3 |
| pXO1-AAT-r3 | TCT AGA ATT AGT TGC TTC ATA ATG GC | None | 66.7 | |
| pXO2-at | pXO2-AT-f1-hex | TCA TCC TCT TTT AAG TCT TGG GT | Hex | 64.4 |
| pXO2-AT-r1 | GTG TGA TGA ACT CCG ACG ACA | None | 65.8 |
PE Biosystem's 5′ fluorescent phosphoramidite dyes: 6-Fam, Hex, and Ned.
Reaction 1 contained 1× PCR buffer (20 mM Tris-HCl [pH 8.4], 50 mM KCl); 2 mM MgCl2; the four deoxynucleoside triphosphates (dNTPs; 0.2 mM each); 0.04 U of Platinum Taq DNA polymerase (Gibco-Life Technologies) per μl; 0.1 μM CG3-F1 and CG3-R1; 0.2 μM each vrrA-F1, vrrA-R1, vrrB1-F1, and vrrB1-R1; and 0.04 to 0.2 ng of template DNA per μl or simply 1 μl of the single-colony lysate.
Reaction 2 contained 1× PCR buffer; 4 mM MgCl2; dNTPs (0.2 mM each); 0.04 U of Platinum Taq DNA polymerase per μl; 0.4 μM each vrrB2-F1, vrrB2-R1, pXO1-aat-F1, pXO1-aat-R1, pXO2-at-F1, and pXO2-at-R1; and 0.04 to 0.2 ng of template DNA per μl or simply 1 μl of the single-colony lysate.
Reaction 3 contained 1× PCR buffer; 2 mM MgCl2; dNTPs (0.2 mM each); 0.04 U of Platinum Taq DNA polymerase per μl; 0.2 μM each vrrC1-F1 and vrrC1-R1; and 0.04 to 0.2 ng of template DNA per μl or simply 1 μl of the single colony lysate.
Reaction 4 contained 1× PCR buffer; 2 mM MgCl2; dNTPs (0.2 mM each); 0.04 U of Platinum Taq DNA polymerase per μl; 0.2 μM each vrrC2-F1 and vrrC2-R1; and 0.04 to 0.2 ng of template DNA per μl or simply 1 μl of the single-colony lysate.
The PCR thermocycling program for all four reactions was identical. Once the reactions were assembled, they were raised to 94°C for 5 min to activate the DNA polymerase. Thereafter, each temperature cycle was 94°C for 20 s, 60°C for 20 s, and 65°C for 20 s. These three steps were repeated 34 times. The final step was at 65°C for 5 min.
Automated genotype analysis.
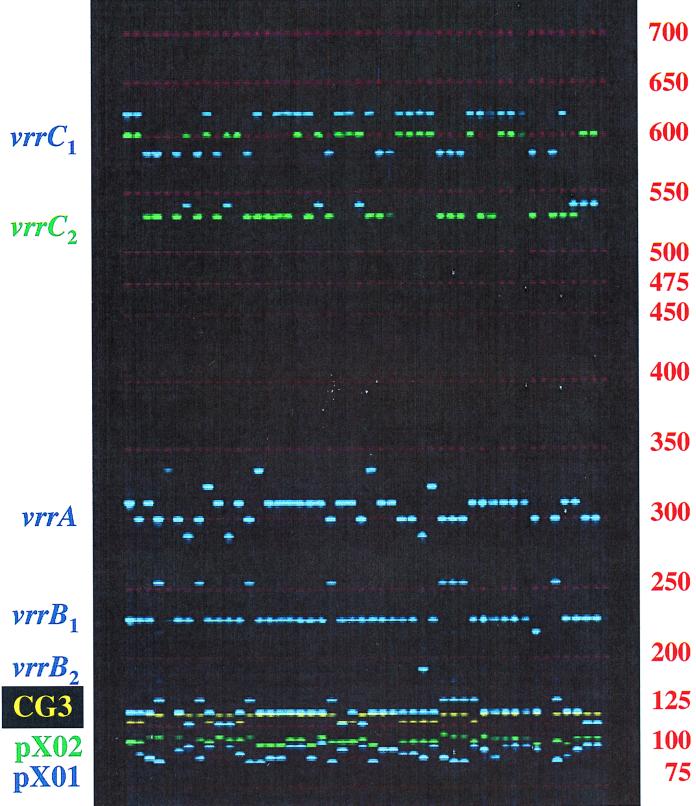
The MLVA PCR products were electrophoretically analyzed with a Perkin-Elmer Applied Biosystems 377 automated fluorescent DNA sequencer (Fig. 1). The four reactions were mixed in equal amounts prior to electrophoretic analysis, which provides relatively equal fluorescent signal from each amplicon. Genescan and Genotyper software packages (Perkin-Elmer, ABI) were used to analyze the gel images. Custom macro programs (available upon request) associated with Genotyper allow the automated scoring of alleles.
FIG. 1.
Electrophoretic analysis of MLVA fragments from different B. anthracis isolates. Fluorescent image of an ABI377 electrophoresis gel containing amplification products from 45 different B. anthracis isolates. All eight VNTR loci are present in each lane. Each marker allele is a unique size and color combination, allowing easy identification of similar-sized fragments from different alleles. The 48 isolates were chosen randomly from the worldwide diversity set shown in Table 1. Sizes are shown in bases.
The apparent electrophoretic size of DNA fragments is not always exactly the same as the size determined by DNA sequencing. This could be due to DNA conformational differences, 3′ adenine addition by the polymerase, migrational deviations of the size standard, or mass asymmetry between the amplicon strands that affect the comparison with the single-stranded standards. We have determined the actual nucleotide sequence of most marker alleles by DNA sequencing and report these values in all cases. These differences are usually only one or two nucleotides, but we recommend the use of standard genotypes selected from Fig. 2 as references.
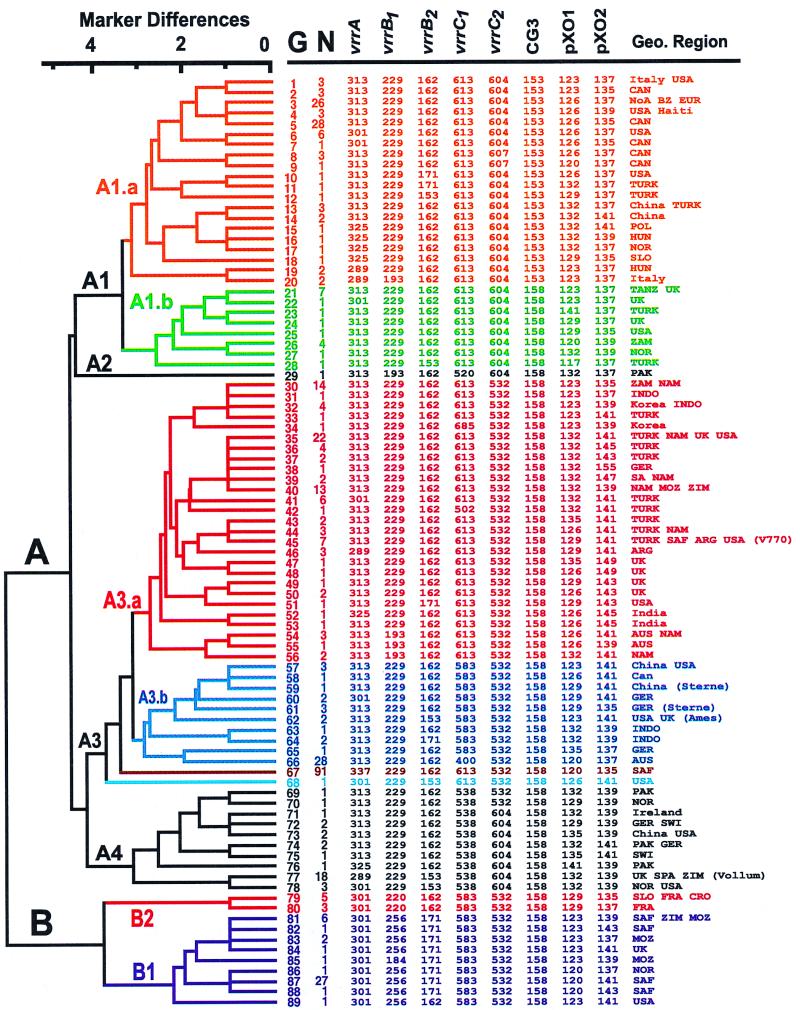
FIG. 2.
MLVA-based dendrogram and genotype scores. The eight VNTR marker loci were used to calculate a simple matching coefficient among all 89 unique MLVA genotypes. UPGMA cluster analysis was performed to identify groups of similar genotypes from the worldwide collection. The genetic distance is presented as the absolute number of differences in marker alleles among genotypes. The amplicon sizes presented are based upon nucleotide sequence determinations using the primers listed in Table 2. Country abbreviations are defined in Table 1. The vaccine strains Sterne, STI-1, and V770-NP1 are lacking the pXO2 plasmid marker and were not included in the cluster analysis. However, we have annotated the data set (see Geographical [Geo.] Region column) to indicate where these important strains match other genotypes based on analysis using seven marker loci. STI-1 did not match any of the genotypes but is related to the cluster A1.a isolates (see text for details). In addition, we have labeled the genotypes of the well-known strains Ames and Vollum. Marker alleles are presented as their sizes in nucleotides. The vrrA allele 313 corresponds to VNTR4 described previously (7, 8). G, genotype number; N, no. of isolates.
Data analysis.
Only genotypes generating data from all eight markers were included in these analyses. About 5% of the samples examined were missing one or both virulence plasmids, which precludes complete genotyping with this MLVA system. This includes the commonly used vaccine strains that lack the pXO2 plasmid. These important strains are annotated on Fig. 2 next to their seven-marker genotypic matches. Analysis of the raw genotype scores was accomplished by using a phenetic approach, unweighted pair group method arithmetic average (UPGMA) cluster analysis (26). UPGMA cluster analysis was performed with PAUP 4.0 (20) with a simple matching coefficient to estimate genetic differences. Individual marker diversity (D) was calculated as equal to 1 − Σ(allele frequency)2 (25) and based upon allele frequencies in the 89 distinct B. anthracis genotypes, not the complete 426-isolate collection.
RESULTS
MLVA.
We have developed an MLVA approach for molecular typing of B. anthracis strains. The system presented here uses eight genetic loci that provide high levels of discrimination among different isolates. These marker loci were identified by DNA sequencing of variable AFLP marker fragments (CG3, vrrB1, vrrB2, vrrC1, and vrrC2), examination of virulence plasmid sequences (pXO2-at and pXO1-aat), and from the previously described vrrA VNTR locus (1). Five of the eight MLVA markers (vrrA, vrrB1, vrrB2, vrrC1, and vrrC2) are found in ORFs and variation in repeat number does not affect the translational reading frame (data not shown). The pXO1 and pXO2 VNTR markers allow monitoring for the presence or absence of the plasmids as well as for plasmid-based variation. This plus-minus assay provides important information about virulence because the lack of either plasmid attenuates a B. anthracis strain (21). Phylogenetic comparison of nucleotide variation did not detect natural horizontal transfer among strains (18), suggesting that plasmid and chromosomal evolution in B. anthracis has been generally congruent.
While no effort was made to make the MLVA primers specific to B. anthracis templates, most sets will not support amplification from other bacterial species. A limited number of B. cereus and Bacillus thuringiensis strains have been examined using the standard reaction conditions; at most a couple, and frequently none, of the markers were amplified in reactions containing these templates (data not shown). The vrrA locus amplified most often in other species, but the resulting allele sizes did not correspond to any of the five alleles observed in B. anthracis isolates. These Bacillus species are the most closely related to B. anthracis. Therefore, this MLVA system represents a credible method of identifying B. anthracis as well as determining what strain type is present.
B. anthracis genotypes.
We used MLVA to characterize 426 B. anthracis isolates from diverse geographic locations. This analysis divided them into 89 MLVA genotypes (Fig. 2). It is clear that multiple isolates from the same anthrax outbreak frequently have identical genotypes. This reduces the number of distinguishable isolates relative to the total number of samples. In addition, many genotypes are found at multiple locations, especially within a restricted geographical region. The number of distinct genotypes collected from particular countries is reported in Table 1. The distribution may be more a function of isolate availability for this study than intrinsic diversity within a limited geographic area, so it is difficult to draw conclusions from these numbers. However, multiple genotypes are observed in all regions for which a large collection of samples are available. The Australian collection is heavily biased by 28 samples from the short 1997 Victoria outbreak. All of these are one genotype. The restricted nature of the collection may therefore explain the lack of multiple genotypes discovered to date in Australia.
VNTR marker diversity.
The discriminatory power of each MLVA marker can be estimated by the number of alleles it detects and by its diversity. These two simple descriptive statistics were determined using only the 89 B. anthracis genotypes to minimize the effect of sampling on allele frequency (Table 3). The isolate collection is biased towards numerous samples from easily accessed B. anthracis collections. This could unduly influence allele frequencies. MLVA markers average over five alleles per locus, with a range of from two to nine alleles (Table 3). The diversity index (D) is based on the number of alleles and the allele frequency. This provides a better measure of discriminatory power than allele number (25). MLVA markers have an average diversity of 0.54, with a range of 0.30 to 0.80. Note that vrrB1 has the lowest diversity (0.30) in spite of having five alleles, whereas CG3 detects only two alleles but has a diversity index of 0.38. The two plasmid-based markers have the highest diversity and greatest number of alleles, perhaps due to the simple sequence nature of their repeats (Table 3).
TABLE 3.
VNTR marker locus attributes
| Locusa | Repeat sizeb (nucleotides) | Array size (no. of repeats)
|
No. of alleles | Dc | |
|---|---|---|---|---|---|
| Smallest | Largest | ||||
| vrrA | 12 | 2 | 6 | 5 | 0.50 |
| vrrB1 | 9 | 15 | 23 | 5 | 0.32 |
| vrrB2 | 9 | 11 | 15 | 3 | 0.34 |
| vrrC1 | 36 | 4 | 12 | 6 | 0.55 |
| vrrC2 | 18 | 17 | 19 | 3 | 0.50 |
| CG3 | 5 | 1 | 2 | 2 | 0.35 |
| pXO1-aat | 3 | 4 | 11 | 8 | 0.81 |
| pXO2-at | 2 | 6 | 15 | 9 | 0.79 |
| Avg | 5.1 | 0.52 | |||
VNTR markers found in ORFs are shown in italics.
vrrB repeats are not all identical, as some contain multiple nucleotide differences. vrrC markers contain a degenerate 9-nucleotide subrepeat structure that results in fractional repeat sizes in some alleles.
D is Nei's marker diversity, which is calculated as 1 − Σ(allele frequency)2 and based solely upon the 89 unique B. anthracis genotypes.
While most of the B. anthracis allelic variation observed in this study is consistent with the repeat unit size, some alleles contain fractions of a repeat. The nucleotide structures found in vrrA, vrrB, and vrrC have evolved from simpler trinucleotide repeats, and remnants of these structures still exist within each repeat (1; unpublished data). No fractional-size alleles were observed for vrrA or vrrB among the different B. anthracis strains, but we did observe several for the vrrC markers. Nucleotide sequencing determined that these were due to insertion or deletion events within the subrepeats (see the vrrC2 alleles in genotypes 8 and 9, Fig. 2).
B. anthracis genetic relationships.
UPGMA cluster analysis reveals major genetic affiliations among the MLVA genotypes (Fig. 2). Six major clusters are apparent that may represent older clonal separations in the evolutionary history of this species. Similar major groups were identified by AFLP marker analysis (10), most of which were independent of the MLVA markers in this study.
The most obvious separation in the dendrogram is the split between the A and B genotypes (Fig. 2). The B cluster contains approximately 12% of the isolates and genotypes in this study. Cluster B is further subdivided into two groups, B1 and B2. Southern African isolates dominate (93%) group B1 and far outnumber the samples found in group B2. Only two genotypes are present in the B2 group. These are rare and collected exclusively in Europe. The B2 group is only tentatively associated with the B1 subgroup, as other analytical approaches (e.g., maximum parsimony) place B2 loosely with the A cluster (data not presented). All B genotypes are uncommon in much of the world, yet genotype 87 (Fig. 2) is an important contributor to the ongoing anthrax outbreak in Kruger National Park (K. L. Smith, V. DeVos, H. Bryden, M. E. Hugh-Jones, L. B. Price, A. Klevytska, D. T. Scholl, and P. Keim, unpublished data).
Members of the A cluster are found worldwide and can be subdivided into at least four groups (Fig. 2). Isolates in the A1 cluster are found throughout the world, but they dominate the western North America collection. The most common A1 genotypes are geographically distributed from the Canadian Wood Bison National Park (genotypes 3 and 5) to southern Texas in the United States (genotype 6). The CG3 marker locus represents a defining diagnostic marker for the A1.a group, as the 153-bp allele is only found in this group. This marker locus consists of a five-nucleotide sequence present in two copies in most strains, but only once in isolates found in cluster A1.a. This difference may not be readily reversible, and all allelic contrasts may be due to a single evolutionary event. While STI-1 was not included in the UPGMA analysis due to its lack of the pXO1 plasmid, it most closely resembles members of the A1.a group. As the sole representative from Russia in this study, it did not exactly match any of the 89 genotypes with its seven markers. However, it is clearly related to isolates from the A1.a cluster. STI-1 marker alleles (Fig. 2, allele sizes = 313, 229, 162, 613, 604, 153, 129, —) matched six of seven markers for 11 different genotypes in A1.a. In addition, STI-1 contains the CG3 153 allele that is only present in A1.a isolates. The close genetic relationship between the western North American isolates and this single Russian representative needs further research and would benefit significantly from examination of additional Russian isolates. The A1.b cluster isolates occur most commonly in Africa and only rarely in other parts of the world.
The A2 branch is represented by a single isolate from Pakistan. It is distinct from other genotypes and may represent a B. anthracis that is common in this undersampled region.
The A3 cluster is perhaps the single most important B. anthracis group due to its wide distribution and prevalence. This highly diverse cluster contains 44% of the genotypes (39 of 89) and 58% of the isolates (260 of 419) examined in this study (Fig. 2). Genotypes in this group are involved in some of the largest outbreaks that we have examined: Kruger National Park (genotype 67); Victoria, Australia (genotype 66); Turkey (genotype 35); and southern Africa (genotypes 30 and 40). Genotypes matching the well-known vaccine strains V770-NPR (genotypes 45, 46, and 49) and Sterne (genotypes 59 and 61) are also found in this cluster. The well known and highly virulent strain Ames (genotype 62) is found in A2 and is similar to Sterne at most marker alleles. The Ames strain played a central role in the United States biological warfare program before it was dismantled (David Huxsoll, personal communication).
The A4 cluster is distinct and yet underrepresented in our current collection (Fig. 2). It is notable primarily for the well-known strain Vollum (genotype 77), which was used in the British biological warfare program (Peter Turnbull, personal communication). Vollum has been studied in many laboratories, and most of the 15 isolates identical to genotype 77 are from laboratory archival collections. One sample of the Vollum 1B strain differed at the vrrA markers by one repeat from other Vollum samples. This seemingly represents an “in-laboratory” mutational event. A natural isolate matching the Vollum genotype was collected in Spain. Other closely related isolates have been found in the United States, Norway, Europe, and Asia but not in Africa.
DISCUSSION
The MLVA typing method presented in this paper represents a robust and easily transferable approach to characterizing B. anthracis isolates. The protocols presented are rapid and require only crudely isolated DNA to provide high-resolution molecular typing analysis. The individual marker alleles are uniquely identified by a combination of size and fluorescent color. Therefore, automated gel analysis is routine. Instrumentation and software to perform MLVA are widely available with the exception of the custom macro software that will be provided by the authors upon request. Standardized data are presented in this report to provide a uniform reference to all anthrax research teams (Fig. 2). Future analyses by any laboratory in the world can be easily compared to the standardized data and particular strains (Table 4) reported here. We hope that the availability of PCR primers, protocols, and a reference data set will encourage anthrax research teams to use a common genetic typing system and to share their results. In the future, combinations of data sets from around the world will lead to novel and comprehensive insights into anthrax biology.
TABLE 4.
Representatives of each B. anthracis genotype
| Genotype | Country | Original strain no. | Sourcea | SPLb no. | Genotype | Country | Original strain no. | Sourcea | SPLb no. | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Italy | 1FG | IZS | K0021 | ||||||
| 2 | Canada | 80-167C-5 | ADRI | K2284 | ||||||
| 3 | Canada | 74-412C-8 | ADRI | K7441 | ||||||
| 4 | Iowa | BA1007/#81 | USAMRIID | K8113 | ||||||
| 5 | Canada | 91-382C-1 | ADRI | K1081 | ||||||
| 6 | Texas | C93022281 | TVMDL | K2165 | ||||||
| 7 | Canada | BA0018 | USAMRIID | K8960 | ||||||
| 8 | Canada | 72-241C-A | ADRI | K1040 | ||||||
| 9 | Canada | 74-389C-52 | ADRI | K3897 | ||||||
| 10 | S. Dakota | 96-10355 | ADRDL | K1256 | ||||||
| 11 | Turkey | 2/6 | EM | K8127 | ||||||
| 12 | Turkey | 1/6 | EM | K7665 | ||||||
| 13 | China | 22/32 | CAMR | K2129 | ||||||
| 14 | China | 23/32 | CAMR | K8071 | ||||||
| 15 | Poland | 100004 | VMRI | K1340 | ||||||
| 16 | Hungary | Feb-98 | VMRI | K1347 | ||||||
| 17 | Norway | B6273/93 | CVL | K8091 | ||||||
| 18 | Slovakia | A22 | IUTSTT | K5974 | ||||||
| 19 | Hungary | Apr-98 | VMRI | K1430 | ||||||
| 20 | Italy | 2PT | IZS | K4241 | ||||||
| 21 | England | 16/32 | CAMR | K1335 | ||||||
| 22 | England | Asc 403 | CAMR | K3166 | ||||||
| 23 | Turkey | 32 | EM | K9002 | ||||||
| 24 | England | 25/32 | CAMR | K3612 | ||||||
| 25 | Florida | 14185 | ATCC | K3700 | ||||||
| 26 | Zambia | Nov-32 | CAMR | K7724 | ||||||
| 27 | Norway | B7227/83 | CVL | K8419 | ||||||
| 28 | Turkey | 14 | EM | K7948 | ||||||
| 29 | Pakistan | PAK-1 | VRI | K5135 | ||||||
| 30 | Zambia | 48/09/92 | CVLL | K0123 | ||||||
| 31 | Indonesia | Pangkep | RIVS | K1024 | ||||||
| 32 | South Korea | F-1 | DMNIH | K1072 | ||||||
| 33 | Turkey | 35 | EM | K1534 | ||||||
| 34 | South Korea | H-1 | DMNIH | K7038 | ||||||
| 35 | Namibia | 93/37 | DRM | K1285 | ||||||
| 36 | Turkey | 22 | EM | K1304 | ||||||
| 37 | Turkey | 31 | EM | K7791 | ||||||
| 38 | Germany | A30 | IUTSTT | K2484 | ||||||
| 39 | Namibia | 46 | DRM | K2223 | ||||||
| 40 | Namibia | Mar-32 | CAMR | K8025 | ||||||
| 41 | Turkey | 11 | EM | K6428 | ||||||
| 42 | Turkey | 39 | EM | K0300 | ||||||
| 43 | Turkey | 17 | EM | K1033 | ||||||
| 44 | Namibia | SA1189 | USAMRIID | K1717 | ||||||
| 45 | Argentina | ZB80 | GELAB | K8215 | ||||||
| 46 | Argentina | BB79 | GELAB | K5816 | ||||||
| 47 | United Kingdom | ASC-228 | CAMR | K9268 | ||||||
| 48 | United Kingdom | ASC-28 | CAMR | K9505 | ||||||
| 49 | United Kingdom | ASC-29 | CAMR | K3342 | ||||||
| 50 | Scotland | Dec-32 | CAMR | K2980 | ||||||
| 51 | Maryland | BA1015 | USAMRIID | K4516 | ||||||
| 52 | India | CS176(#1) | CMCH | K4342 | ||||||
| 53 | India | CS176(#5) | CMCH | K2883 | ||||||
| 54 | Namibia | 24 | DRM | K2280 | ||||||
| 55 | Australia | 29/32 | CAMR | K4834 | ||||||
| 56 | Namibia | 93/197 | DRM | K8903 | ||||||
| 57 | China | 24/32 | CAMR | K0610 | ||||||
| 58 | Canada | 9610 | ADRI | K7841 | ||||||
| 59 | China | 4 | IEM | K0006 | ||||||
| 60 | Germany | A9 | IUTSTT | K7912 | ||||||
| 61 | Germany | A41 | IUTSTT | K4921 | ||||||
| 62 | United Kingdom | Oct-32 | USAMRIID | K1694 | ||||||
| 63 | Indonesia | Bekasi | RIVS | K1938 | ||||||
| 64 | Indonesia | Dompu | RIVS | K4527 | ||||||
| 65 | Germany | A40 | IUTSTT | K1892 | ||||||
| 66 | Australia | 97-1946/2 | EMAI | K1298 | ||||||
| 67 | South Africa | K3 | KNP | K1244 | ||||||
| 68 | Ohio | 28 | USAMRIID | K2802 | ||||||
| 69 | Pakistan | BA1021 | USAMRIID | K7222 | ||||||
| 70 | Norway | B1965/77 | CVL | K8736 | ||||||
| 71 | Ireland | BA1024 | USAMRIID | K1021 | ||||||
| 72 | Germany | NMS | IUTSTT | K4433 | ||||||
| 73 | China | 28/32 | CAMR | K6410 | ||||||
| 74 | Pakistan | A67 | IUTSTT | K1129 | ||||||
| 75 | Switzerland | A66 | IUTSTT | K7615 | ||||||
| 76 | Pakistan | BA1009/ | USAMRIID | K4001 | ||||||
| 77 | United Kingdom | Vollum | CAMR | K4596 | ||||||
| 78 | Norway | B648/82 | CVL | K8822 | ||||||
| 79 | France | CNEVA 9066 | IP | K1887 | ||||||
| 80 | France | RA3 | IP | K2762 | ||||||
| 81 | South Africa | 33 | USAMRIID | K3323 | ||||||
| 82 | South Africa | BA1035 | USAMRIID | K8101 | ||||||
| 83 | Mozambique | MOZ-1 | INV | K4849 | ||||||
| 84 | United Kingdom | ASC-27 | CAMR | K9901 | ||||||
| 85 | Mozambique | 3 | INV | K2478 | ||||||
| 86 | Norway | B286/76 | CVL | K1671 | ||||||
| 87 | South Africa | K88 | KNP | K6835 | ||||||
| 88 | South Africa | 83 | USAMRIID | K3677 | ||||||
| 89 | N. Carolina | 109 | USAMRIID | K3535 |
ADRDL, Animal Disease Research and Diagnostic Laboratory, South Dakota State University; ADRI, Animal Diseases Research Institute, Alberta, Canada; ATCC, American Type Culture Collection, Manassas, Va.; CAMR, Center for Applied Microbiology and Research, Porton Down, United Kingdom; CMCH, Christian Medical College and Hospital, Tamil Nadu, India; CVL, Central Veterinary Laboratory, Oslo, Norway; CVLL, Central Veterinary Laboratory, Lusaka, Zambia; DMNIH, Department of Microbiology, National Institute of Health, Seoul, South Korea; DRM, Directorate of Resource Management, Windhoek, Namibia; EM, Enstutusu Muduriugu, Ankara, Turkey; EMAI, Elizabeth MacArthur Agricultural Institute, New South Wales, Australia; GELAB, Department Bacteriologia General, Buenos Aires, Argentina; IEM, Institute of Epidemiology and Microbiology, Changping, China; INV, Instituto Nacional de Veterinaria, Maputo, Mozambique; IP, Institut Pasteur, Paris, France; IUTSTT, Institut für Unwelt und Tierhygiene Sowie Tiermedizin mit Tierklinik, Stuttgart, Germany; IZS, Instituto Zooprofilattico Sperimentale, Teramo, Italy; KNP, Kruger National Park, South Africa; RIVS, Research Institute for Veterinary Science, Bogor, Indonesia; TVMDL, Texas Veterinary Medical Diagnostic Laboratory, College Station, Texas; USAMRIID, United States Army Medical Research Institute for Infectious Diseases, Maryland; VMRI, Veterinary Medical Research Institute, Budapest, Hungary; and VRI, Veterinary Research Institute, Lahore, Pakistan.
SPL, Special Pathogens Laboratory, Louisiana State University.
Molecular typing in many pathogenic bacterial species is accomplished without focusing on hypervariable VNTR loci. In B. anthracis, however, this has proven extremely difficult due to the homogeneous nature of all available strains (10). In this pathogen, only the most rapidly evolving genomic regions are useful for strain discrimination. VNTR loci fall into this category and have been used successfully in this study to separate B. anthracis isolates into 89 distinct genotypes. As a first approximation, one can assume that the diversity of a particular VNTR is correlated with its evolutionary rate, and in the absence of selective constraints, this would be the mutation rate. In this study, the simple di- and trinucleotide tandem repeats (pXO1-aat and pXO2-at) are the most diverse, while complex longer repeats have lower diversity (Table 3). Slip strand repair mutations by DNA polymerase are thought to occur more frequently on short repeats (23), and our data are consistent with this model. Markers of higher diversity obviously provide great discriminatory power among strains. However, it is less obvious that highly diverse markers have less power for defining older evolutionary relationships. Our MLVA markers have different diversity levels and contribute in different ways to the analysis of B. anthracis.
VNTR mutation rates are apparently fast on an evolutionary scale but slow enough that mutations are very difficult to observe in the laboratory. We have passaged a plasmid-cured strain of Ames for more than 100,000 generations and observed only a single VNTR mutation (313 to 301) in vrrA (G. Zinser and P. Keim, unpublished observations). At least in the six chromosomal loci, marker alleles appear stable to routine and even long-term handling in the laboratory. As stated above, variation in different Vollum strain (genotype 77) accessions illustrates the stability of these markers. There are 15 different Vollum examples in this study from different sources in the United States and the United Kingdom. One of these was passaged three times through rats and three times through rabbit hosts without MLVA changes. The only difference was observed in the vrrA marker (301 instead of 289) for the substrain Vollum 1B. These anecdotal and preliminary results need additional confirmation but suggest that VNTR mutation rates are slower than 10−5 and that mutational changes occur in single-repeat steps.
The existence of a limited number of B. anthracis clones can be hypothesized from the genetic similarities observed within each of the six major clusters in Fig. 2. The number and distribution of these hypothesized clones have doubtlessly been influenced by human activity. This may have started with domestication of animals but continues through modern-day international commerce. Note that not all of the putative clones are equally widespread. For example, the A3 cluster is very common and distributed across many continents, while the B1 cluster is restricted mostly to southern Africa. The A1 cluster splits into two distinctive groups, with one branch primarily North American (A1.a) and one mostly African (A1.b). These differences in cluster prevalence and distribution may be influenced by inherent biological properties (Smith et al., unpublished data) or just due to stochastic historical events.
While the biological significance of B. anthracis VNTR variation is unknown, some VNTR variation examples have pronounced effects on pathogen biology (23). Five of the eight MLVA loci in the MLVA system are found in ORFs (data not presented). Therefore, VNTR variation could easily affect the bacterial phenotype via altered translational products. Moreover, it has also been shown that extragenic VNTRs can influence adjacent gene expression (23). This provides a possible genetic role for even intergenic VNTRs. Given the extreme homogeneity of B. anthracis, VNTRs represent the only significant source for molecular variation among the strains known at this time. Whether this variation is biologically significant or only useful for diagnostic analysis of B. anthracis will be determined by future VNTR studies.
ACKNOWLEDGMENTS
This work was supported by funding from the U.S. Department of Energy (NN20-CBNP), the National Institutes of Health (RO1 GM60795), and the Cowden Endowment in Microbiology.
We thank Ms. Karen Hill, Debra Adair, Guenevier Zinser, and A. S. Kalif for excellent technical assistance. In addition, this research would have been impossible without the help and unstinting generosity of many people across the world who provided us with cultures from outbreaks and from their collections; we are extremely grateful for their patience and contributions: Argentina—Dept. Bacteriologia General, GELAB/SENASA, Buenos Aires (Luis Betancor). Australia—Elizabeth MacArthur Agricultural Institute, New South Wales (Michael Hornitzky); Princess Alexandria Hospital, Queensland (Jacqueline Harper); Yeerongpilly Veterinary Laboratory, Queensland (Rod Thomas); Department of Natural Resources & Environment, Victoria (Andrew Turner and Maria Yates). Canada—Animal Diseases Research Institute, Alberta (Jack Burchak and Greg Tiffin). China—Institute of Epidemiology & Microbiology, Changping (Xudong Liang). France—Institut Pasteur, Paris (Michelle Mock); Hôpital du Bocage, Dijon (C. Neuwirth). Germany—Institut für Umwelt und Tierhygiene Sowie Tiermedizin mit Tierklinik, Stuttgart (Reinard Bohm). Hungary—Veterinary Medical Research Institute, Budapest (Bela Nagy). India—Christian Medical College & Hospital, Tamil Nadu (M. K. Lalitha). Indonesia—Research Institute for Veterinary Science, Bogor (Sjamsul Bahri). Italy—Instituto Zooprofilattico Sperimentale, Terama (Vincenzo Caporale). Korea—Department of Microbiology, National Institutes of Health, Seoul (Ho-Hoon Kim). Mozambique—Instituto Nacional de Veterinaria, Maputo (Sara Acha). Namibia—Directorate of Resource Management, Windhoek (Pauline Lindeque). Nepal—National Zoonoses & Food Hygiene Research Centre, Kathmandu (D. D. Joshi). Norway—Central Veterinary Laboratory, Oslo (Finn Saxegaard). Pakistan—Veterinary Research Institute, Lahore (Shabbir Ahmad). Poland—Wojskowy Instytut Higieny, Pulawy (Jerzy Mierzejewski). Portugal—Regional Veterinary Diagnostic Laboratory, Evora (Patricio Nuncio and Armando Louzo). South Africa—Kruger National Park (Helena Bryden and Valerius de Vos); Onderstepoort Biological Products (Huck Jager); Onderstepoort Veterinary Institute (Maryke Henton). Tanzania—Department of Veterinary Microbiology & Parasitology, Sokoine University of Agriculture (Saddrudin Jiwa). Thailand—Department of Livestock Development, Bangkok (Vichitr Sukhapesna). Turkey—Enstitusu Muduriugu, Ankara (Metin Kerman); Infeksiyon Hastaliklari Klinigi, Erciyes Universitesi, Kayseri (Mehmet Dogany). United Kingdom—Centre for Applied Microbiology & Research, Porton (Peter Turnbull); DERA, Porton (Tony Philipps and Richard Manchee). USA—California Veterinary Diagnostic Laboratory System, California (Richard Walker); Centers for Disease Control & Prevention, Georgia (Rob Weyant); United States Army Medical Research Institute for Infectious Diseases, Maryland (Art Friedlander and John Ezzell); Veterinary Diagnostic Services, NM Dept of Agriculture, New Mexico (Linda Nims); Veterinary Diagnostic Laboratory, NDSU, North Dakota (David White); Animal Disease Diagnostic Laboratory, Oklahoma (Ronald Welsh); Animal Disease Research & Diagnostic Laboratory, SDSU, South Dakota (David Zeman); Texas Veterinary Medical Diagnostic Laboratory, Texas (Howard Whitford). Zimbabwe—Veterinary Research Laboratory, Causeway (U. Ushewokunze-Obatolu). Zambia—Central Veterinary Laboratory, Lusaka (P. M. Muyoyeta).
REFERENCES
- 1.Andersen G L, Simchock J M, Wilson K H. Identification of a region of genetic variability among Bacillus anthracis strains and related species. J Bacteriol. 1996;178:377–384. doi: 10.1128/jb.178.2.377-384.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boyd E F, Wang F S, Whittam T S, Selander R K. Molecular genetic relationships of the salmonellae. Appl Environ Microbiol. 1996;62:804–808. doi: 10.1128/aem.62.3.804-808.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eitzen E M. Use of biological weapons. In: Sidell F R, Takafuji E T, Franz D R, editors. Medical aspects of chemical and biological warfare. Washington, D.C.: Office of the Surgeon General; 1997. pp. 437–450. [Google Scholar]
- 4.Freidlander A M. Anthrax. In: Sidell F R, Takafuji E T, Franz D R, editors. Medical aspects of chemical and biological warfare. Washington, D.C.: Office of the Surgeon General; 1997. pp. 467–478. [Google Scholar]
- 5.Frothingham R, Meeker-O'Connell W A. Genetic diversity in the Mycobacterium tuberculosis complex based on variable numbers of tandem DNA repeats. Microbiology. 1998;144:1189–1196. doi: 10.1099/00221287-144-5-1189. [DOI] [PubMed] [Google Scholar]
- 6.Harrell L J, Andersen G L, Wilson K H. Genetic variability of Bacillus anthracis and related species. J Clin Microbiol. 1995;33:1847–1850. doi: 10.1128/jcm.33.7.1847-1850.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Henderson I, Yu D, Turnbull P C. Differentiation of Bacillus anthracis and other ‘Bacillus cereus group’ bacteria using IS231-derived sequences. FEMS Microbiol Lett. 1995;128:113–118. doi: 10.1111/j.1574-6968.1995.tb07509.x. [DOI] [PubMed] [Google Scholar]
- 8.Jackson P J, Walthers E A, Kalif A S, Richmond K L, Adair D M, Hill K K, Kuske C R, Andersen G L, Wilson K H, Hugh-Jones M E, Keim P. Characterization of the variable-number tandem repeats in vrrA from different Bacillus anthracis isolates. Appl Environ Microbiol. 1997;63:1400–1405. doi: 10.1128/aem.63.4.1400-1405.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jackson P J, Hugh-Jones M E, Adair D M, Green G, Hill K K, Kuske C R, Grinberg L M, Yampolskaya O V, Keim P. Molecular analysis of tissue samples from the 1979 Sverdlovsk anthrax victims: the presence of multiple Bacillus anthracis in different victims. Proc Natl Acad Sci USA. 1998;95:1224–1229. doi: 10.1073/pnas.95.3.1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Keim P, Kalif A, Schupp J M, Hill K K, Travis S E, Richmond K, Adair D M, Hugh-Jones M E, Kuske C R, Jackson P. Molecular evolution and diversity in Bacillus anthracis as detected by amplified fragment length polymorphism markers. J Bacteriol. 1997;179:818–824. doi: 10.1128/jb.179.3.818-824.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Keim P, Klevytska A, Price L B, Schupp J M, Zinser G, Okinaka R, Hill K K, Jackson P, Smith K L, Hugh-Jones M E. Molecular diversity in Bacillus anthracis. J Appl Microbiol. 1999;87:215–217. doi: 10.1046/j.1365-2672.1999.00873.x. [DOI] [PubMed] [Google Scholar]
- 12.Koch R. Die Aetiologie der Milzbrand-Krankheit, begründet auf die Entwicklungsgeschichte des Bacillus anthracis. Beitr Biol Pflanz. 1876;2:277–310. [Google Scholar]
- 13.Maiden M C, Bygraves J A, Feil E, Morelli G, Russell J E, Urwin R, Zhang Q, Zhou J, Zurth K, Caugant D A, Feavers I M, Achtman M, Spratt B G. Multilocus sequence typing: a portable approach to the identification of clones within populations of pathogenic microorganisms. Proc Natl Acad Sci USA. 1998;95:3140–3145. doi: 10.1073/pnas.95.6.3140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miettinen M K, Siitonen A, Heiskanen P, Haajanen H, Bjorkroth K J, Korkeala H J. Molecular epidemiology of an outbreak of febrile gastroenteritis caused by Listeria monocytogenes in cold-smoked rainbow trout. J Clin Microbiol. 1999;37:2358–2360. doi: 10.1128/jcm.37.7.2358-2360.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Okinaka R, Cloud K, Hampton O, Hoffmaster A, Hill K, Keim P, Koehler T M, Lamke G, Kumano S, Mahillon J, Manter D, Martinez Y, Ricke D, Svensson R, Jackson P J. Sequence and organization of pXO1, the large Bacillus anthracis plasmid harboring the anthrax toxin genes. J Bacteriol. 1999;181:6509–6515. doi: 10.1128/jb.181.20.6509-6515.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pasteur L, Chamberland R. Compte rendu sommaire des expériences faites à Pouilly-le-Fort, près Melun, sur la vaccination charbonneuse. C R Séances Acad Sci Ser III Sci Vie. 1881;92:1378–1383. [Google Scholar]
- 17.Popovic T, Kim C, Reiss J, Reeves M, Nakao H, Golaz A. Use of molecular subtyping to document long-term persistence of Corynebacterium diphtheriae in South Dakota. J Clin Microbiol. 1999;37:1092–1099. doi: 10.1128/jcm.37.4.1092-1099.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Price L B, Hugh-Jones M E, Jackson P, Keim P. Natural genetic diversity in the protective antigen gene of Bacillus anthracis. J Bacteriol. 1999;181:2358–2362. doi: 10.1128/jb.181.8.2358-2362.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Richards R I, Sutherland G R. Dynamic mutation: possible mechanisms and significance in human disease. Trends Biochem Sci. 1997;22:432–436. doi: 10.1016/s0968-0004(97)01108-0. [DOI] [PubMed] [Google Scholar]
- 20.Swofford D. PAUP—phylogenetic analysis using parsimony (and other methods), 4.0 beta version. Sunderland, Mass: Sinauer Associates, Inc.; 1999. [Google Scholar]
- 21.Thorne C B. Bacillus anthracis. In: Sonenshein A L, Hoch J A, Losick R, editors. Bacillus subtilis and other gram-positive bacteria: biochemistry, physiology, and molecular genetics. Washington, D.C.: American Society for Microbiology; 1993. pp. 113–132. [Google Scholar]
- 22.Vahey M, Nau M E, Barrick S, Cooley J D, Sawyer R, Sleeker A A, Vickerman P, Bloor S, Larder B, Michael N L, Wegner S A. Performance of the Affymetrix GeneChip HIV PRT 440 platform for antiretroviral drug resistance genotyping of human immunodeficiency virus type 1 clades and viral isolates with length polymorphisms. J Clin Microbiol. 1999;37:2533–2537. doi: 10.1128/jcm.37.8.2533-2537.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van Belkum A, Scherer S, van Alphen L, Verbrugh H. Short-sequence DNA repeats in prokaryotic genomes. Microbiol Mol Biol Rev. 1998;62:275–293. doi: 10.1128/mmbr.62.2.275-293.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vos P, Hogers R, Bleeker M, Reijans M, van de Lee T, Hornes M, Frijters A, Pot J, Peleman J, Kuiper M. AFLP: a new technique for DNA fingerprinting. Nucleic Acids Res. 1995;23:4407–4414. doi: 10.1093/nar/23.21.4407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weir B S. Genetic data analysis. Sunderland, Mass: Sinauer Associates, Inc.; 1990. [Google Scholar]
- 26.Welsh J, McClelland M. Fingerprinting genomes using PCR with arbitrary primers. Nucleic Acids Res. 1990;18:7213–7218. doi: 10.1093/nar/18.24.7213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Williams J G, Kubelik A R, Livak K J, Rafalski J A, Tingey S V. DNA polymorphisms amplified by arbitrary primers are useful as genetic markers. Nucleic Acids Res. 1990;18:6531–6535. doi: 10.1093/nar/18.22.6531. [DOI] [PMC free article] [PubMed] [Google Scholar]