Abstract
Objective:
To investigate the relationships between children’s food and drink choices at school lunch for children who consume high and low sugar intakes at home.
Design:
Children’s food and drink consumption at home was assessed using diet diaries over three consecutive days. Children were classified as ‘high’ or ‘low’ sugar consumers at home using the WHO recommendation that free sugars should be less than 10 % of their daily total energy intake. A purposive sample of children was then selected and observed during school lunch, recording food selections, food left on plates and content of packed lunches.
Setting:
Six primary schools in Newham and Kent, England.
Participants:
Parents and children aged 6–7 years.
Results:
Seventy-one parents completed diet diaries. From the seventy-one, thirty-nine children were observed during school lunch. Twenty children were high sugar consumers, nineteen children were low sugar consumers; thirty-one children had a school meal. Eleven of the fifteen children (73 %) who had school meals and who were high sugar consumers selected a high-sugar dessert rather than fruit. Only five of the sixteen (31 %) children who had school meals and were low sugar consumers at home chose a high-sugar dessert. Most of the children who had packed lunches had sweet items, despite school policies.
Conclusions:
Children who consumed high sugar intake at home tended to select foods high in sugar for school meals or had packed lunches containing high-sugar foods. The implications for public health programmes include healthy eating workshops and implementing school food policies.
Keywords: Children, School lunch, Dietary, Sugar
There is an increased focus on children’s dietary habits spurred by the rise in child obesity and tooth decay( 1 ). The UK National Child Measurement Programme found that 33 % of children aged 10–11 years were obese or overweight in 2016( 2 ). Similarly, approximately a third (31 %) of 5-year-olds and nearly half (46 %) of 8-year-olds had experienced tooth decay in their primary (baby) teeth. The frequent consumption of foods and drinks containing free sugars is a common risk factor for both child obesity and tooth decay in children( 3 , 4 ). The Scientific Advisory Committee on Nutrition reported in 2015 that high sugar intake increases the risk of developing type 2 diabetes, weight gain and tooth decay in children( 5 ). Free sugars (FS) are mono- and disaccharides added to food or drinks; or sugars naturally present in honey, syrups and fruit juices excluding sugars in milk( 6 ). The Scientific Advisory Committee on Nutrition recommended that FS intake in the UK should account for no more than 5 % of a person’s daily energy intake( 5 ). The WHO guidelines also recommended restricting FS in children’s diets to less than 10 % of their daily total energy intake( 7 ). However, data from national nutrition surveys in England show that children’s consumption of FS exceeds these recommendations( 8 ). Children aged 4–10 years and 11–18 years consumed an average of 15 and 16 % of their energy intake from FS in 2012. Developing strategies to support healthy eating requires a deeper understanding of the factors that influence children’s food choices.
Children spend a significant amount of their time outside the home environment in school, which means that they have access to foods or drinks available outside the home environment( 9 ). However, few studies have explored the relationship between dietary habits at home and food choices outside the home environment. The Department for Education in England reported that one million primary-school children (85 %) have school meals across England( 10 ).
The two key factors that influence what children eat at school are the availability of food options in the school meals and what parents decide to include in children’s packed lunches. A study of primary-school children in England found that sugar and total carbohydrate contents in foods consumed by children who had packed lunches were higher than those eating school meals( 11 ). Although studies have explored children’s food choices in school lunch, no studies have looked at the relationship between children’s food consumption both at home and at school.
Several studies examining food consumption have used an ethnographic approach, which involved participant observations of children as the main methodology( 12 , 13 ). The advantage of participant observations is that it provides a visual and objective assessment of behaviour rather than beliefs or perceptions( 14 ). The purpose of the school meal and packed lunch observation in the present study was to assess children’s food selection and choices outside the home environment at school. The present study addressed the research question: is there a relationship between children’s FS consumption at home and their food choices and consumption at school lunch?
Methods
Mixed-methods study design
The present study used a mixed-methods explanatory design( 15 ) which involved both quantitative and qualitative research methods in two sequential phases. In phase 1, quantitative data were collected to assess children’s food and drink consumption at home using a parent-reported 3 d food diary, including one weekend day. These data were input into INTAKE24( 16 ), an online dietary assessment method. INTAKE24 is specifically designed to include the portion size of foods and is linked to the National Diet and Nutrition Survey Nutrient Databank( 17 ). The data were analysed to determine children’s sugar consumption at home and then used to select children to take part in a qualitative study, which included non-participant observation of children’s school lunch. The classification of children into ‘high’ and ‘low’ sugar consumers at home was based on the percentage of energy that FS contributed to their daily energy intake as compared with the recommendation that FS should be less than 10 %( 7 ). Children who had low sugar intake at home had FS intake that was less than 10 % of their energy intake, while children who had high sugar intake at home had FS intake that exceeded 10 % of their energy intake. Following this classification, all the children who were high or low sugar consumers at home were selected to take part in a qualitative study, which included non-participant observation of children’s school lunch.
Study population
The study population comprised children attending primary schools in Kent and Newham in England and their parents/carers. These areas were selected to study families from both low and middle socio-economic groups in an inner city, ethnically diverse urban population living in the capital city of London, in the borough of Newham; and from a suburban, less diverse population outside London, in Kent. Newham and Kent were selected to represent two contrasting areas in England. Newham is in the top 20 % of deprived areas in England; more than a quarter (28 %) of children live in low-income households. In contrast, Kent is ranked among the 50 % least deprived areas in England with 15 % of children living in poverty( 18 , 19 ).
Sample selection: schools
State-maintained (government-funded) primary schools in Kent and Newham were the setting for the present study. A list of primary schools in Kent and Newham was obtained and categorised based on the number of children within the school and the percentage of children whose first language was English. Schools with large numbers and fewer non-English speaking children were prioritised to maximise the opportunities for a good response from parents. Seventy-six schools were approached using an invitation letter sent to the head teachers asking them for permission to involve their school. Six schools agreed to participate; three schools in Newham and three schools in Kent.
Sample selection: participants
The participants were Year 2 children aged 6–7 years attending the six primary schools and their parents who gave their positive consent for their child to participate. Sample size requirements for participant observation studies are not based on a priori calculation but on data saturation when no new themes emerge from the observations( 20 ). Guidance on ethnographic studies that include non-participant observations estimate that twenty-five to fifty observations are often sufficient to obtain thematic saturation( 21 ).
Quantitative assessment of children’s dietary intake at home
Parents/carers who attended the six schools were asked to complete a 24 h diet diary over three days noting their child’s food and drink intake; and to complete a demographic questionnaire. Three consecutive days were preselected to include one weekend day and two weekdays. The purpose of collecting dietary information on at least one day in the weekend was to take account of variations in children’s diets, including on special occasions that occur more frequently at weekends. The diet diaries had instructions for recording foods and drinks with details of the amount, portion size and brand name provided to their child, and the amount of food and drink left after the meal or snack.
The data collected in the diet diaries were entered into INTAKE24( 16 ) which computes the daily intake based on nutrient groups analysed to calculate FS intake and total energy intake. INTAKE24 is a validated method to be used by parents of younger children to assess dietary intake( 16 ).
Each child was classified based on the daily dietary intake using the WHO recommendation. Extreme (or deviant) sampling( 22 ) was then used to identify the children who consumed high sugar intake (daily total energy percentage from FS exceeded 10 %) or low sugar intake (daily total energy percentage from FS less than 10 %).
Description of food availability in the schools selected
Schools provided a range of food options including set meals, fruit, vegetables and dessert such as cakes, pudding, flavoured yoghurt, ice cream and custard. The content of school meals varied depending on the schools’ fixed main course menus. Table 1 shows the main differences and similarities between the school menus and the availability of FS-containing foods (dessert) in all six schools. The study was carried out during the summer term of 2016 and the analysis was based on the summer term menus (Table 1). All participating schools in Newham and Kent offered vegetables and fruit at school meals. Fish was usually served on Fridays in schools and the majority of schools offered a vegetarian option. Vegetables were also available in all menus including sweetcorn, salad, peas and mixed vegetables.
Table 1.
A summary of the school menus and food availability for the school meals at the six schools in Newham and Kent, England, that participated in the study in May–July 2016
| School number (area) | Set main meal | Desserts provided | School food policy |
|---|---|---|---|
| School 1 (Newham) |
|
Fruit, flavoured yoghurt, chocolate cake, banana cake with custard, chocolate ice cream, cheesecake, apple pie with custard and jelly | No food policy for both school meals and packed lunches |
| School 2 (Newham)* |
|
Only dessert options were fruit or yoghurt | Policy is based on the Eatwell Plate and is reviewed every 3 years (for school meals and packed lunch) |
| School 3 (Newham)* |
|
Pudding, fruit flapjack, syrup sponge with custard, jelly, ice cream, apple pie and chocolate muffins | Policy is based on the Eatwell Plate (for school meals and packed lunch) |
| School 4 (Kent) |
|
Pudding, fruit, sticky toffee (custard), chocolate tart, ice cream, carrot cake and jelly | Policy is based on the Nutritionist resource (for school meals and packed lunch) |
| School 5 (Kent) |
|
Fruit, cake, jelly, cookies, iced finger bun and mousse | No policy for both school meals and packed lunches |
| School 6 (Kent) |
|
Fruit, ice cream, fruit yoghurt, chocolate mousse, tutti-frutti cake, cheesecake and raspberry cake | Policy is based on the Eatwell Plate and Change4Life (for packed lunch) |
Healthy Schools in London.
All six schools provided healthy drinks for children (water and milk). Only one school offered only fruit or yoghurt for dessert. Other schools served different sugar-containing dessert options. In Kent, one school had three options for lunch, either school meals, packed lunch or catering option, which included sandwiches. Only milk and water were available as drinks for children who had school meals in all schools; while children with packed lunches brought either apple or orange juice.
School food policies
Two of the three schools in Newham had Healthy School status( 23 ) (Table 1), which meant they followed specific requirements as part of the ‘Healthy Schools in London’ Programme. One of these requirements was having a school food policy. Two schools in Kent had food policies based on the Eatwell Plate, ChangeforLife and Nutritionist resource( 24 ).
School lunch observations
A qualitative researcher carried out the observations in the school on the purposive sample of children who were categorised as high and low sugar consumers. This researcher was aware of whether the child was categorised as a low or high sugar consumer during the participant observations. Each child was observed individually based on his/her sugar classification. Detailed information about children’s food choices and observation data were written up in field notebooks. The notes were then transferred into a descriptive narrative on a digital file.
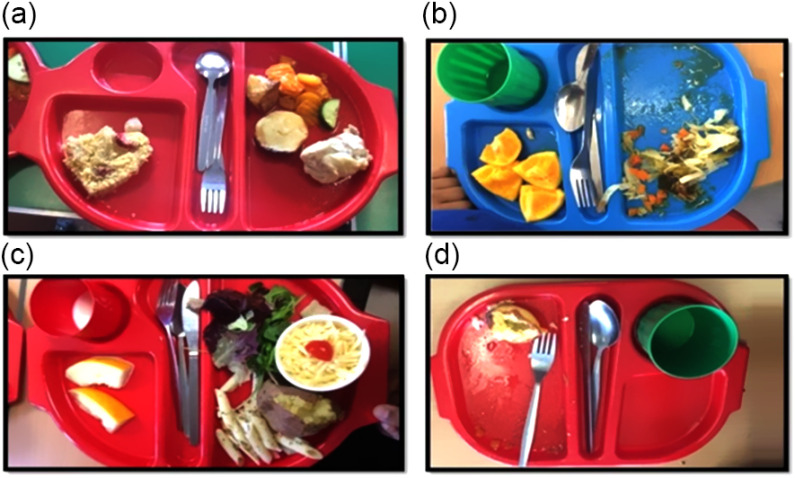
The non-participant observation of school lunches used an observation checklist developed to record the observations of both school meals and packed lunches. This checklist recorded food content, food left on the plate, the interaction between children in terms of food choices and the contribution of FS. Photographs of the foods available at school lunch and photographs of the children’s plates were taken to provide a visual record of the content of school meals or packed lunches and the content of the food left on the plate.
Data analysis
Children’s diet diaries were analysed using the statistical software package IBM SPSS Statistics version 22.0 to calculate their daily FS intake and total energy intake. Conventional content analysis( 25 ) was used to analyse the data gathered during school lunch observations from the observation checklists, photographs and school menus. Thirty-one children who had a school meal and eight children who had a packed lunch were included in the analysis.
Results
Description of study population
One hundred and thirty-four families agreed to participate in the study and were invited to complete a 3 d diet diary. Of those parents, seventy-one parents completed the 3 d diet diaries (thirty-eight children in Newham and thirty-three children in Kent). Forty-three parents out of seventy-one (60 %) completed the demographic questionnaire. Nearly half of the mothers (46 %) and fathers (49 %) had a university degree, while 40 % of mothers and 28 % of fathers had completed further education at college.
Thirty-nine children were purposively sampled to take part in the school lunch observations. The mean age of the children was 7·2 (sd 0·2) years. Twenty children were observed in Kent and nineteen in Newham. Most of the parents of the thirty-nine children who were observed either had completed further education or had a university degree (90 %).
Assessment of children’s macronutrient and sugar intakes at home
Thirty-nine children were selected for school lunch observations. Table 2 shows the daily mean intakes of energy, carbohydrate, total sugars, fat, saturated fat, protein and FS of the thirty-nine children. The mean energy intake of the 6–7-year-old children was 8079 kJ/d (1931 kcal/d; 7481 kJ/d (1788 kcal/d) in Newham and 8673 kJ/d (2073 kcal/d) in Kent). Children in Kent consumed more FS (75 g/d) than children in Newham (49 g/d; Table 2). The FS consumption and the energy percentage from FS were measured for meals and snacks at home (excluding reported FS from lunches during weekdays). Twenty children were categorized as high sugar consumers (total energy from FS was ≥10 %) and nineteen as low sugar consumers (total energy from FS was <10 %). The mean daily sugar intake was 56 g/d for high sugar consumers and 12 g/d for children who had low sugar intake. The total energy from FS was 17 % for children in the high sugar group and 5 % for children in the low sugar group. The analysis of diet diaries showed that the mean intake of fruits and vegetables at home in children who had low sugar intake was higher than that of the children who had high sugar intake (Table 3).
Table 2.
Mean daily macronutrient intakes of 6–7-year-old children who participated in the study in Newham and Kent, England, based on 3 d food diaries reported by parents in May–July 2016
| Macronutrient | Children in Newham (n 19) |
Children in Kent (n 20) |
All children (n 39) |
|||
|---|---|---|---|---|---|---|
| Mean | sd | Mean | sd | Mean | sd | |
| Energy (kJ) | 7481 | 1992 | 8673 | 3824 | 8079 | 3000 |
| Energy (kcal) | 1788 | 476 | 2073 | 914 | 1931 | 717 |
| Carbohydrate (g) | 232 | 63 | 286 | 118 | 255 | 92 |
| Fat (g) | 68 | 29 | 83 | 60 | 76 | 48 |
| Saturated fat (g) | 26 | 10 | 34 | 23 | 30 | 18 |
| Protein (g) | 73 | 26 | 75 | 28 | 74 | 27 |
| Total sugars (g) | 101 | 43 | 142 | 73 | 123 | 51 |
| Free sugars (g) | 49 | 31 | 75 | 60 | 63 | 50 |
Table 3.
Mean daily fruit and vegetables intakes at home of 6–7-year-old children who participated in the study in Newham and Kent, England, based on the 3 d food diaries reported by parents in May–July 2016
| Fruit and vegetable intakes | Children in Newham (n 19) |
Children in Kent (n 20) |
All children (n 39) |
|||
|---|---|---|---|---|---|---|
| Mean | sd | Mean | sd | Mean | sd | |
| Fruit (g) | 150 | 101 | 94 | 47 | 120 | 80 |
| Vegetables (g) | 40 | 31 | 43 | 87 | 41 | 66 |
| All children who had low sugar intake at home*
(n 19) |
All children who had high sugar intake at home†
(n 20) |
All children (n 39) |
||||
| Mean | sd | Mean | sd | Mean | sd | |
| Fruit (g) | 123 | 93 | 118 | 58 | 120 | 80 |
| Vegetables (g) | 52 | 72 | 35 | 53 | 41 | 66 |
Children had free sugar intake that was less than 10 % of their energy intake at home.
Children had free sugar intake exceeding 10 % of their energy intake at home.
Description of school lunch process
Children who had school lunches usually sat at the same table and talked to each other. The food choices of children who sat together were similar. The time taken for children to finish eating their school lunches ranged from 10 to 15 min. All the schools followed the same system during school lunch, whereby the class teachers stood in front of the dining area to oversee the children who selected their own food items. Children chose items from the salad bar, as well as a main dish option and a dessert. Children who had school meals usually sat at the same table; children with packed lunches also sat together. All six schools had the same size of coloured plate, but the amount of food allocated to children varied in each school determined by the serving staff. Two schools in Kent served small food portions compared with other schools. After the meal, some teaching assistants checked the food remaining on children’s plates and encouraged the children to finish their food.
School meals food selection and consumption by children who consumed high and low sugar intakes at home
Seventeen (89 %) out of the nineteen children in Newham had a school meal, while fourteen out of the twenty children (70 %) in Kent had a school meal. Table 4 shows the school lunch dessert selections and foods consumed by children in Newham and Kent. In Newham, the sugar-containing desserts were mainly flavoured yoghurts while in Kent the sugar-containing desserts were puddings.
Table 4.
The dessert selections and foods consumed at lunch by 6–7-year-old children who had school meals in Newham and Kent, England, May–July 2016
| Food selection at school lunch | Children who had high sugar intake at home* | Children who had low sugar intake at home† | ||||||
|---|---|---|---|---|---|---|---|---|
| Children in Newham (n 8) |
Children in Kent (n 7) |
Children in Newham (n 9) |
Children in Kent (n 7) |
|||||
| n | % | n | % | n | % | n | % | |
| Number and % of children who selected desserts containing free sugars | 6 | 75 | 5 | 71 | 3 | 33 | 2 | 29 |
| Number and % of children who selected desserts not containing free sugars | 2 | 25 | 2 | 29 | 6 | 67 | 5 | 71 |
| Number and % of children who selected vegetables | 3 | 38 | 4 | 57 | 8 | 88 | 7 | 100 |
| Number and % of children who left vegetables on the plate | 2 | 25 | 3 | 43 | 7 | 77 | 2 | 29 |
Children had intake of free sugars at home that exceeded 10 % of their energy intake.
Children had intake of free sugars at home that was less than 10 % of their energy intake.
Eleven of the fifteen children who had high sugar intake at home selected a dessert with a high FS content rather than fruit when it was available. Figure 1(a) shows an example of the foods selected at school lunch by a child who was a high sugar consumer at home. In contrast, only five of the sixteen children categorised as a low sugar consumer at home selected a high-sugar dessert at school lunch (Fig. 1(c)). Children who had a low sugar intake at home selected mainly flavoured yoghurts as their chosen dessert at school, while children who had a high sugar intake at home tended to select sweetened desserts at school such as ice cream, cake, custard, pudding, flapjack and chocolate mousse. The food left on the plate of children with high sugar intake at home included fruit and vegetables. Eight children with high sugar intake at home left fruit and vegetables on their plates (Fig. 1(b)). Children with low sugar intake at home selected more fruit at school lunch but like children who had high sugar intake at home, they also left some vegetables on their plates (Fig. 1(d)).
Fig. 1.
Photographs illustrating the foods selected and the food left on the plate in school meals by four different children, who had high or low sugar intake at home, from the sample of 6–7-year-old children in Newham and Kent, England, May–July 2016. (a) Photograph of food selected as a school meal by a child who had high sugar intake at home: strawberry flapjack. (b) Photograph of food left on the plate of a child who had high sugar intake at home: fruit and vegetables. (c) Photograph of food selected as a school meal by a child who had low sugar intake at home: fruit, vegetables, cheese and pasta. (d) Photograph of food left on the plate of a child who had low sugar intake at home: mainly vegetables.
Packed lunch content of children who consumed high and low sugar intakes at home
Eight children had packed lunches. The content of packed lunches was usually a sandwich, fruit and a dessert (e.g. sweets or sweet biscuits), but there were differences in food content between the children. Schools had guidance that recommended avoiding unhealthy options such as sweets, confectionery and crisps and encouraging a healthy alternative instead such as bread sticks or low-sugar snack bars. Four of six schools had some restrictions on confectionery and sweets as a part of their packed lunch polices. Despite this, four of the five children who had high sugar intake at home had either sweets or sweet biscuits in their packed lunches, while all three children who had low sugar intake at home had fruit in their packed lunches. Seven of eight children had small cartoons of fruit juice and only one child had a water bottle in their packed lunch. Children left fruit and sandwiches in their packed lunches.
Discussion
The present study compared the school meal selection and content of packed lunches in children with high and low sugar intakes in heterogeneous school environments in Newham and Kent, England. While recognising the relatively small purposive sample size, the study suggests that there could be a trend in the relationship between children’s sugar consumption at home and their choices and consumption at school. More children who had high sugar intake at home selected foods that were high in sugar at school rather than fruit, while children who had low sugar intake at home were less likely to pick foods that were high in sugar at school lunch. This relationship may be influenced by children’s learned food preferences. A preference for sweet taste is universally present in neonates, along with an aversion to sour and bitter tastes( 26 – 28 ). Both cross-sectional studies and longitudinal studies demonstrate a preference towards sweet taste in children( 29 , 30 ). Children have an unlearned preference for sweet and salty foods and an innate dislike of sour and bitter tastes( 31 ). This innate preference for sugar-containing foods and drinks can further develop during childhood through repeated exposure to sweetened foods( 32 ). Experience can also enhance taste preferences; earlier experiences of a particular food eaten at home are the major determinants for developing children’s food acceptance patterns.
The findings in our study showed that children who had low sugar intake at home consumed more fruits and vegetables than high-sugar foods during school lunch. However, both children with high and low sugar intakes at home left fruit and vegetables on their plates at school lunch. Current evidence recommends that children eat at least five portions of a variety of fruit and vegetables each day( 24 ). Previous research has also shown the benefit of providing fruit and vegetables at school during early school years( 33 , 34 ). A recent systematic review assessed the effect of school food environment policies on children’s dietary habits and found that school food environment policies improved targeted dietary behaviours( 35 ). Our study suggests that offering children only fresh fruit and yoghurt as dessert options at school lunch could support children to reach their daily fruit and vegetable consumption recommendations, while also reducing their intake of FS( 36 ). To support this objective, fresh fruit dessert options in school meals and school food policy should follow the Eatwell Guide( 24 ) and sugar swaps ideas.
Previous studies have shown that repeated exposure to vegetables at a younger age may be effective in encouraging children to eat more fruit and vegetables, especially before the onset of neophobia( 37 ). When the repeated exposure to vegetables strategy was used, younger children were less fussy about their food choices, enjoyed food more and reported lower satiety responsiveness( 37 ). However, findings from interviews and focus groups with children suggested that their perceptions about fruit and vegetables change over time through cognitive development( 38 ). The participant observation in our study showed that fruit and vegetables were available to all children. This highlights the role that catering staff could have to encourage children to consume those fruit and vegetables, to facilitate higher consumption through repeated exposure and encouragement.
The school lunch observations showed that the majority of children had a school meal. Since 2014, government-funded schools in England provide every child in reception (aged 4–5 years), Year 1 and Year 2 with a hot lunchtime meal under the Universal Infant Free School Meals policy. A recent cross-sectional study assessed the effect of the Universal Infant Free School Meals policy in schools and found that it increased the uptake of school meals from over a third (38 %) of children in 2013–14 to 80 % in 2015–16, evident across most schools( 39 ). School meals are a communal experience creating opportunities to encourage healthy eating at lunchtime( 40 , 41 ).
Our study found that the minority of children had a packed lunch. One school in Kent allowed crisps and sweet snacks such as cake or chocolate-coated biscuits and fruit juice to be brought to school in packed lunches. A study in English primary schools that compared the food and nutrient intakes of children eating school dinners and packed lunches found that the sugar content of packed lunches was higher than that of school dinners( 11 ). Our findings agreed with Golley et al. that children having school meals were no longer consuming drinks other than milk or water, confectionery or savoury snacks compared with children who had packed lunch( 42 ). Children’s eating behaviour at home, such as feeding practices, parenting style( 43 ) and parental autonomy, may contribute to parents’ lunch packing decisions. A qualitative study of 7–8-year-old children in Wales found that some children preferred packed lunches because they had greater control over what they ate at school lunch( 44 ). Parents often capitulated to their children’s preference for unhealthy options in packed lunches, which could explain the high sugar content of food items in packed lunches identified in our study.
The findings from the present study suggest that reducing children’s high-sugar choices at school also needs to take account of and aim to reduce their sugar choices and intake in the home environment. Similarly, recent studies have considered food choices outside the home environment, when high-sugar snacking is common at home( 45 , 46 ). A cross-sectional study examined the association between the home availability of sugar-sweetened beverages and total sugar-sweetened beverage consumption and found that when sugar-sweetened beverages were available at school, adolescents’ sugar-sweetened beverage consumption was higher among those with more frequent availability of sugar-sweetened beverages in the home. A systematic review investigated the association between the family environment and children’s fruit and vegetable consumption( 47 ). The findings highlighted the importance of targeting the family environment for the promotion of healthy eating behaviours among children and adolescents. There is a need for a whole-family approach in interventions as well as trying to reduce high-sugar options at school.
Families’ food choices at home strengthen children’s preference for sugary foods and parents are usually in charge of limiting children’s sugar consumption by controlling access to foods( 48 ). Therefore, there is an opportunity to change children’s food preferences by supporting families with tools that encourage healthy food choices. One example is the using sugar swaps ideas such as the Change4 Life Public Health initiative in the UK (http://www.nhs.uk/Change4Life). The Change4Life programme encourages families and schools to promote healthy eating workshops that involve parental education highlighting the need to restrict FS consumption at home.
While it is possibly easier to monitor and regulate the nutritional content of school meals, there also needs to be clearer guidance for packed lunches to support parents to improve the quality of foods brought from home at lunchtime( 49 ). Schools are encouraged to promote healthy eating workshops that involve parental education highlighting the fact of controlling FS consumption at home. Experiential learning healthy eating workshops for both parents and primary-school children have been shown to reduce children’s sugar consumption( 50 , 51 ).
Strength and limitations
This was a mixed-methods study, which included participant observations based on a qualitative research methodology reflecting the small purposive sample size. This inductive and explorative study generated hypotheses from the trends that were observed about the relationship between children’s sugar intakes at home and at school. However, as with all qualitative research studies, one should be cautious about generalising the present study’s findings to different settings. Transferability needs to be established in a given context.
Several methods were used to ensure the quality and convey rigour and trustworthiness in the present study( 52 ), including the time spent in the field and using photographs and a checklist to verify the observations. One limitation of the study was only observing the lunch period on one occasion. Although the observations were carried out by a researcher who knew the child’s status, the coding and analysis were carried out by multiple coders (K.B., V.M. and C.P.). This is consistent with qualitative data analysis, which conveys credibility by using multiple coders to reduce biases( 53).
Conclusions
The present exploratory study suggested that children who consumed high sugar intake at home selected foods that were high in sugar in their school lunch meal or had packed lunches that also included high-sugar items. School lunch creates opportunities to influence children’s common food choices but requires change at the school organisation, policy and family levels. The findings from the study reinforce the conceptualised relationship between children’s food choices in the school and home environments. The study highlighted the importance of school polices, which should contain guidance on both school meals and packed lunches. Implications for future public health programmes include healthy eating workshops for families, both parents and children; and clearer guidance that promotes healthier packed lunches.
Acknowledgements
Acknowledgements: The authors would like to thank all the families who participated in this study. Thanks are expressed to Professor Paula Moynihan for her advice on using the INTAKE24 software to analyse free sugars. Financial support: K.B. is supported by a King Abdulaziz University PhD scholarship. King Abdulaziz University had no role in the design, analysis or writing of this article. Conflict of interest: None. Authorship: K.B., V.M. and C.P. conceptualised the study and contributed to the design of the quantitative analysis; K.B. and V.M. planned and analysed the non-participant school lunch observations. K.B. conducted all of the quantitative analysis and carried out the school lunch observations. K.B., V.M. and C.P. interpreted the findings for the manuscript. K.B., V.M. and C.P. drafted the manuscript; all authors provided feedback. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the Queen Mary Ethics of Research Committee (QMERC2015/61). Written informed consent was obtained from all subjects.
References
- 1. Craig R & Mindell J (2015) Health Survey for England 2015. Leeds: Health and Social Care Information Centre. [Google Scholar]
- 2. NHS Digital (2016) National Child Measurement Programme, England 2015 to 2016 school year. http://www.content.digital.nhs.uk/searchcatalogue?productid=23381&q=national+child+measurement+programme&sort=Relevance&size=10&page=1#top (accessed July 2018).
- 3. Moynihan P & Petersen PE (2004) Diet, nutrition and the prevention of dental diseases. Public Health Nutr 7, 201–226. [DOI] [PubMed] [Google Scholar]
- 4. Department of Health (2016) Childhood obesity: a plan for action. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/546588/Childhood_obesity_2016__2__acc.pdf (accessed September 2018).
- 5. Scientific Advisory Committee on Nutrition (2015) Carbohydrates and Health [Public Health England, editor]. London: TSO; available at http://www.gov.uk/government/uploads/system/uploads/attachment_data/file/445503/SACN_Carbohydrates_and_Health.pdf (accessed July 2018).
- 6. World Health Organization (2015) Guideline: Sugars Intake for Adults and Children. Geneva: WHO; available at http://apps.who.int/iris/bitstream/10665/149782/1/9789241549028_eng.pdf (accessed July 2018). [PubMed]
- 7. World Health Organization (2014) WHO opens public consultation on draft sugars guideline. http://www.who.int/mediacentre/news/notes/2014/consultation-sugar-guideline/en/ (accessed July 2018). [PubMed]
- 8. Bates B, Lennox A, Prentice A et al. (2014) National Diet and Nutrition Survey: Results from Years 1–4 (combined) of the Rolling Programme (2008/2009–2011/12). London: Public Health England and Food Standards Agency; available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/594361/NDNS_Y1_to_4_UK_report_full_text_revised_February_2017.pdf (accessed July 2018).
- 9. Amini M, Dadkhah-Piraghaj M, Abtahi M et al. (2014) Nutritional assessment for primary school children in Tehran: an evaluation of dietary pattern with emphasis on snacks and meals consumption. Int J Prev Med 5, 611. [PMC free article] [PubMed] [Google Scholar]
- 10. Department of Education (2014) New data shows 1.3 million more infants eating free school meals. https://www.gov.uk/government/news/new-data-shows-13-million-more-infants-eating-free-school-meals (accessed July 2018).
- 11. Rogers I, Ness A, Hebditch K et al. (2007) Quality of food eaten in English primary schools: school dinners vs packed lunches. Eur J Clin Nutr 61, 856–864. [DOI] [PubMed] [Google Scholar]
- 12. Kremer-Sadlik T, Morgenstern A, Peters C et al. (2015) Eating fruits and vegetables. An ethnographic study of American and French family dinners. Appetite 89, 84–92. [DOI] [PubMed] [Google Scholar]
- 13. Lloyd-Williams F, Bristow K, Capewell S et al. (2011) Young children’s food in Liverpool day-care settings: a qualitative study of pre-school nutrition policy and practice. Public Health Nutr 14, 1858–1866. [DOI] [PubMed] [Google Scholar]
- 14. Tugault-Lafleur CN, Black JL & Barr SI (2017) A systematic review of methods to assess children’s diets in the school context. Adv Nutr 8, 63–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Creswell JW & Clark VLP (2007) Designing and Conducting Mixed Methods Research, 1st ed. Thousand Oaks, CA: Sage Publications. [Google Scholar]
- 16. Foster E, Delve J, Simpson E et al. (2014) Comparison study: INTAKE24 vs Interviewer led recall. Final report. https://intake24.co.uk/assets/papers/Intake24-Comparison-report.pdf (accessed July 2018).
- 17. Foster E, Matthews J, Lloyd J et al. (2008) Children’s estimates of food portion size: the development and evaluation of three portion size assessment tools for use with children. Br J Nutr 99, 175–184. [DOI] [PubMed] [Google Scholar]
- 18. Public Health England (2017) Health Newham Profile. https://fingertips.phe.org.uk/profile/health-profiles/area-searchresults/E12000007?search_type=list-child-areas&place_name=London (accessed July 2018).
- 19. Ministry of Housing, Communities & Local Government (2015) The English Index of Multiple Deprivation 2015 (IMD2015): Headlines Findings of Kent. https://www.gov.uk/government/statistics/english-indices-of-deprivation-2015 (accessed July 2018).
- 20. Morse JM (2000) Determining Sample Size: Qualitative Health Research, 1st ed. Thousand Oaks, CA: Sage Publications. [Google Scholar]
- 21. Moser A & Korstjens I (2018) Series: Practical guidance to qualitative research. Part 3: Sampling, data collection and analysis. Eur J Gen Pract 24, 9–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Patton MQ (2005) Qualitative Research. Chichester: John Wiley & Sons Ltd. [Google Scholar]
- 23. Healthy Schools London Programme (2013) Healthy Schools in London. http://www.healthyschools.london.gov.uk/ (accessed July 2018).
- 24. Public Health England (2016) The Eatwell Guide: How does it differ to the eatwell plate and why? London: Public Health England; available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/528201/Eatwell_guide_whats_changed_and_why.pdf (accessed July 2018).
- 25. Hsieh H-F & Shannon SE (2005) Three approaches to qualitative content analysis. Qual Health Res 15, 1277–1288. [DOI] [PubMed] [Google Scholar]
- 26. Desor J, Maller O & Andrews K (1975) Ingestive responses of human newborns to salty, sour, and bitter stimuli. J Comp Physiol Psychol 89, 966–970. [DOI] [PubMed] [Google Scholar]
- 27. Scaglioni S, Arrizza C, Vecchi F et al. (2011) Determinants of children’s eating behavior. Am J Clin Nutr 94, 6 Suppl., 2006S–2011S. [DOI] [PubMed] [Google Scholar]
- 28. Wardle J, Guthrie C, Sanderson S et al. (2001) Food and activity preferences in children of lean and obese parents. Int J Obes Relat Metab Disord 25, 971–979. [DOI] [PubMed] [Google Scholar]
- 29. Mennella JA, Pepino MY & Reed DR (2005) Genetic and environmental determinants of bitter perception and sweet preferences. Pediatrics 115, e216–e222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Desor J & Beauchamp GK (1987) Longitudinal changes in sweet preferences in humans. Physiol Behav 39, 639–641. [DOI] [PubMed] [Google Scholar]
- 31. Birch LL & Fisher JO (1998) Development of eating behaviors among children and adolescents. Pediatrics 101, 539–549. [PubMed] [Google Scholar]
- 32. Ventura AK & Mennella JA (2011) Innate and learned preferences for sweet taste during childhood. Curr Opin Clin Nutr Metab Care 14, 379–384. [DOI] [PubMed] [Google Scholar]
- 33. Anderson A, Porteous L, Foster E et al. (2005) The impact of a school-based nutrition education intervention on dietary intake and cognitive and attitudinal variables relating to fruits and vegetables. Public Health Nutr 8, 650–656. [DOI] [PubMed] [Google Scholar]
- 34. Moore L & Tapper K (2008) The impact of school fruit tuck shops and school food policies on children’s fruit consumption: a cluster randomised trial of schools in deprived areas. J Epidemiol Community Health 62, 926–931. [DOI] [PubMed] [Google Scholar]
- 35. Micha R, Karageorgou D, Bakogianni I et al. (2018) Effectiveness of school food environment policies on children’s dietary behaviors: a systematic review and meta-analysis. PLoS One 13, e0194555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Knai C, Pomerleau J, Lock K et al. (2006) Getting children to eat more fruit and vegetables: a systematic review. Prev Med 42, 85–95. [DOI] [PubMed] [Google Scholar]
- 37. Caton SJ, Blundell P, Ahern SM et al. (2014) Learning to eat vegetables in early life: the role of timing, age and individual eating traits. PLoS One 9, e97609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Zeinstra GG, Koelen MA, Kok FJ et al. (2007) Cognitive development and children’s perceptions of fruit and vegetables; a qualitative study. Int J Behav Nutr Phys Act 4, 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sellen P, Huda N, Gibson S et al. (2018) Evaluation of Universal Infant Free School Meals. http://dera.ioe.ac.uk/30988/1/UIFSM-evaluation-7.pdf (accessed July 2018).
- 40. Independent (2017) The health cost of cutting free school lunches will be far greater than the price of them. https://www.independent.co.uk/life-style/health-and-families/the-health-cost-of-cutting-free-school-lunches-will-be-far-greater-than-the-price-of-them-a7756881.html (accessed July 2018).
- 41. Evans C, Mandl V, Christian M et al. (2016) Impact of school lunch type on nutritional quality of English children’s diets. Public Health Nutr 19, 36–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Golley R, Pearce J & Nelson M (2011) Children’s lunchtime food choices following the introduction of food-based standards for school meals: observations from six primary schools in Sheffield. Public Health Nutr 14, 271–278. [DOI] [PubMed] [Google Scholar]
- 43. Ventura AK & Birch LL (2008) Does parenting affect children’s eating and weight status? Int J Behav Nutr Phys Act 5, 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Warren E, Parry O, Lynch R et al. (2008) ‘If I don’t like it then I can choose what I want’: Welsh school children’s accounts of preference for and control over food choice. Health Promot Int 23, 144–151. [DOI] [PubMed] [Google Scholar]
- 45. Cho D & Kim S (2018) Interplay between self-efficacy and perceived availability at home and in the school neighborhood on adolescents’ fruit and vegetable intake and energy-dense, low-nutrient food and sugary drink consumption. J Nutr Educ Behav 50, 856–867. [DOI] [PubMed] [Google Scholar]
- 46. Haughton CF, Waring ME, Wang ML et al. (2018) Home matters: adolescents drink more sugar-sweetened beverages when available at home. J Pediatr 202, 121–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Pearson N, Biddle SJ & Gorely T (2009) Family correlates of fruit and vegetable consumption in children and adolescents: a systematic review. Public Health Nutr 12, 267–283. [DOI] [PubMed] [Google Scholar]
- 48. Mattila ML, Rautava P, Sillanpaa M et al. (2000) Caries in five-year-old children and associations with family-related factors. J Dent Res 79, 875–881. [DOI] [PubMed] [Google Scholar]
- 49. Evans CE & Cade JE (2017) A cross-sectional assessment of food-and nutrient-based standards applied to British schoolchildren’s packed lunches. Public Health Nutr 20, 565–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Dudley DA, Cotton WG & Peralta LR (2015) Teaching approaches and strategies that promote healthy eating in primary school children: a systematic review and meta-analysis. Int J Behav Nutr Phys Act 12, 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Eisenmann JC, Gentile DA, Welk GJ et al. (2008) SWITCH: rationale, design, and implementation of a community, school, and family-based intervention to modify behaviors related to childhood obesity. BMC Public Health 8, 223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Graneheim UH & Lundman B (2004) Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today 24, 105–112. [DOI] [PubMed] [Google Scholar]
- 53. Barbour R (2001) Checklists for improving rigour in qualitative research: a case of the tail wagging the dog? BMJ 322, 1115–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]