Abstract
Objective:
Decades of marginalization have led Palestinian refugees living in Lebanon to experience multigenerational poverty and food insecurity. The Healthy Kitchens, Healthy Children programme implemented and examined the impact of a two-pronged intervention that employed women through community kitchens to deliver a subsidized healthy daily school snack to elementary-school children in Palestinian refugee camps in Lebanon. We describe the rationale, study design, theorized impact pathways, and discuss lessons learned.
Design:
The programme was quasi-experimental. We conducted formative and process evaluation of both components of the intervention to elucidate the pathways to programme impact.
Setting:
Palestinian refugee camps in Lebanon.
Participants:
Thirty-three women participated in the kitchens and provided subsidized snacks to 714 children.
Results:
Snacks were healthy, traditional Palestinian recipes designed by women and a nutritionist. Participation fluctuated but eventually increased after modifying the meals to ensure acceptability by children. The main challenges to sustainability related to the need for subsidization of the meals and the lack of school policies around the regulation of sales of school food, which together led to fluctuations in programme participation.
Conclusions:
The study provides lessons learned on the potential of this model to improve the human capital of two generations of protracted refugees. The availability of schools as a constant market for these social enterprises offers an opportunity for sustainable livelihood generation and food security gains. Challenges to sustainability remain and could be addressed through social (subsidies to support the programme) and structural (policies to restrict unhealthy food sales) measures.
Keywords: Food security, Protracted refugee population, School nutrition programme, Community kitchens, Women’s empowerment
Some of the most marginalized populations in the Middle East are Palestinian refugees(1). In Lebanon, Palestinians are a protracted refugee population who experience significant social, political and economic exclusion(2). In this context, the UN Relief and Works Agency for Palestine refugees (UNRWA) provides them with education, health care and other welfare(3,4). Despite this support, Palestinian refugees still suffer from high levels of poverty and food insecurity(3). About 62 % of households reported being food insecure in 2015 and this was associated with poor educational status, poor mental health status and poor self-rated health(3). Food insecurity is more common in households with female heads and results in poor-quality diets, particularly a reduction in fruit, vegetable, dairy and meat and chicken consumption(3). The nutritional profile of this population includes high rates of adult overweight and associated non-communicable diseases, an under-5 stunting rate of 13 % and high anaemia levels in schoolchildren(5,6). There is a significant gender differential in employment rate, with female employment at 16·9 % in 2015, while that of males was 69·2 %. This is likely related to cultural factors and time constraints due to family obligations(3). Nevertheless, women have an unused potential to contribute to reversing their household’s food insecurity.
Combinations of short-term and long-term actions that are complementary have been shown to be most effective at alleviating food insecurity in various settings(7). Two types of intervention have individually found some success in addressing food insecurity: community kitchens and school feeding programmes(8–10). The Healthy Kitchens, Healthy Children programme (HKHC) brings together concepts from both of these interventions that could lead to beneficial synergies in addressing the underlying causes and potential consequences of food insecurity in Palestinian refugees.
In brief, community kitchens are defined as community-based cooking programmes which aim to enhance food skills, increase self-efficacy, decrease food insecurity and break social isolation(9). Most commonly, participants in community kitchens are trained in budgeting, menu planning, food hygiene, cooking skills, and may also receive nutrition education. Community kitchens are collaborative and participatory and have the potential to foster social support(11).
School feeding programmes are food assistance programmes that aim to alleviate short-term hunger in children, provide nutritious food, and improve cognitive and educational outcomes. They act as a social safety net and have been described as providing income transfer to households in the form of food(12) and offsetting household food-related concerns(13). A systematic review of the effects of school feeding programmes found small but significant effects on height in younger children, school attendance and school performance (specifically in mathematics), with greater positive effects in disadvantaged children(14).
The HKHC programme established community kitchens as social enterprises and linked these with a school food programme. We hypothesized that women participating in Healthy Kitchens would generate income and have increased self-reliance, social engagement and support(9,15). This support would lead to improvements in participants’ mental health(16) and financial income would lead to improvements in food security; all enhancing women’s empowerment. Through a change in children’s (as well as parents’ and teachers’) knowledge, and healthy food availability, children participating in the school food programme would have improvements in diet, school attendance and performance(14).
In the present paper we describe the design and process of this programme, as well as key findings from the formative and process evaluation. The programme’s theory of change is outlined in Fig. 1; however, the testing of these hypotheses and results of the impact evaluations are beyond the scope of the present paper and are presented elsewhere. We conclude with lessons learned and key reflections from implementing such a programme in a setting with long-term political and economic constraints.
Fig. 1.

Healthy Kitchens, Healthy Children programme impact pathway. Grey boxes represent features of the school nutrition intervention component, white boxes represent features of the Healthy Kitchens component and hatched boxes represent features of both components (CBO, community-based women’s organization; CK, community kitchen)
Methods
The HKHC programme was quasi-experimental in design with two components: (i) the establishment of two community kitchens (Healthy Kitchens (HK)) as social enterprises; linked to (ii) a community-based school nutrition intervention. The design of the HKHC programme was informed by a previous pilot study which showed that it was feasible to supply schoolchildren with healthy meals cooked by a women’s cooperative(17).
Figure 1 displays the HKHC programme impact pathway. It details the inputs, activities, outcomes and hypothesized theory of change of the two separate and complementary components of the programme: HK and the school nutrition intervention. This programme impact pathway guided the formative and process evaluation(18,19) and will inform the analysis of the impact of the programme.
Healthy Kitchens component
Intervention design
To establish the HK, we identified already existing community-based women’s organizations (CBO) willing to participate and whose community centres were in close proximity to UNRWA elementary schools. Informed consent was sought from all CBO members. In order to reach enough women who were able to commit to the time requirements of the programme, a convenience sample of fifty-one women was recruited to the CBO intervention.
We renovated and equipped the kitchens with the necessary items to increase their capacity to produce food on a larger scale and to ensure food safety and hygiene. A week-long training for women covered three main topics: (i) Entrepreneurship, including business planning, production, marketing, finance and organization; (ii) Food safety and hygiene, with hands-on training and correction of practices; and (iii) Interactive nutrition education sessions on the importance of fruits and vegetables, iron-rich foods and reducing the fat, sugar and salt content of diets. Each participating CBO was then paired with a local intervention school facilitated by UNRWA. Responsibilities of the CBO included procurement of raw materials, the safe preparation and delivery of meals, payment of salaries to working members and the management of profits and excess food produced.
Formative evaluation
Prior to the intervention, several meetings were held with the women to discuss work schedules and types of snacks acceptable to schoolchildren. Focus group discussions were held with women to compile and detail culturally appropriate recipes. These were then modified and standardized to ensure that they met the World Food Programme dietary guidelines for light mid-morning school snacks(20,21).
Outcome evaluation
At the beginning (baseline) and the end (endline) of the school year, a questionnaire was administered to women who consented to participate in the programme. Sociodemographic and economic data were collected. Household food security was measured using the Arab Family Food Security Scale(22). The Household Dietary Diversity Score was adapted to include examples of foods consumed by this population(23). Additional modules assessed mental health, level of social support and empowerment(24,25). These data will be presented elsewhere.
Community-based school nutrition intervention
Intervention design
This component was designed as a quasi-experimental school-based intervention with a matched pair design and 8-month follow-up of children aged 5–15 years. Schools were matched on gender distribution and geographic quarter (a proxy for socio-economic status). Four UNRWA schools (two matched pairs) were selected based on convenience. One school from each pair was then randomly allocated to the school nutrition intervention arm (subsidized healthy food sold at school plus nutrition education) and the second to the control arm (nutrition education alone). We conducted the study in two refugee camps in Beirut: two all-girls’ schools in year 1 and two co-ed schools in year 2. With the assistance of the school administration and parents’ committees we invited parents to attend a presentation of the programme which described the rationale and design of the intervention, the logistics and costs of participating. Families receiving assistance from the UNRWA social welfare programme were exempt from the costs of the snacks to encourage participation and ensure no child who wanted to participate was excluded.
We also informed existing school canteens and explored potential collaboration with them. Canteens are usually small structures with basic equipment that sell packaged processed products and sometimes Middle Eastern dough breads (manakish) to school students.
Healthy snacks were sold to students at a subsidized price in the two intervention schools, 5 d/week during recess. Supplemental Fig. S1 (see online supplementary material) shows the rotating 4-week menu. The recipes aimed slightly below the World Food Programme criteria for one mid-morning snack of approximately 25 % of average energy, 30 % of protein and 10 % of fat requirements for children aged 6–12 years(20,21). Recipes were also designed to reduce saturated fat, sugar and salt content of the diet and increase dietary diversity. The dietary composition of the recipes was verified using Nutritionist Pro software v5.1.0 (Axxya Systems, San Bruno, CA, USA). Supplemental Table S1 (see online supplementary material) shows the recipes and nutritional composition of a 5 d sample menu and Table 1 includes the average nutritional content of the 20 d cycling menu. The rationale for offering a mid-morning snack is that it would provide nutrition during the school day especially to students who skipped breakfast and would replace the high-energy, low-nutrient-density snack that children purchased from canteens at recess.
Table 1.
Average nutritional content of the snacks (aggregate of years 1 and 2) provided in the Healthy Kitchens, Healthy Children school nutrition intervention
| Average/d | % Recommended amount* | |
|---|---|---|
| Energy (kJ; 7531 kJ) | 1312·1 | 17·4 |
| Energy (kcal; 1800 kcal) | 313·6 | 17·4 |
| Carbohydrate (g; RDA = 130 g) | 45·2 | 34·7 |
| Protein (g; RDA = 34 g) | 12·7 | 37·3 |
| Fat (g; 30 % AMDR = 60 g/d) | 9·1 | 15·1 |
| Na (mg; UL = 2200 mg) | 234·2 | 10·6 |
| Vitamin A (RAE; RDA = 600 µg) | 253·0 | 42·1 |
| Fe (mg; RDA = 8 mg) | 3·4 | 42·7 |
| Folate (μg; RDA = 300 µg) | 98·0 | 32·7 |
| Zn (mg; RDA = 8 mg) | 1·3 | 16·5 |
| Vitamin D (μg; RDA = 15 µg) | 0·3 | 2·1 |
| Ca (mg; RDA = 1300 mg) | 147·2 | 11·3 |
| Vitamin C (mg; RDA = 45 mg) | 13·0 | 28·9 |
RAE, retinol activity equivalents; UL, Tolerable Upper Intake Level; AMDR, Acceptable Macronutrient Distribution Range.
These values are based on age-specific recommendations (9–13 years)(21).
The actual cost per snack averaged $US 0·94, including food, labour, packaging and transportation. The snacks were subsidized, and schoolchildren were asked to pay $US 0·25 per snack, totalling $US 5 per month for twenty snacks. Prior to the establishment of the HKHC programme, children were paying an average of $US 0·76 per day for a school snack. Participation in the healthy snack programme was completely voluntary throughout the year, allowing children to opt out at any point.
In both intervention and control schools, nutrition and health education sessions targeted students (as three half-hour sessions) and parents and teachers (three one-hour sessions). School nutrition education kits developed and evaluated during the pilot were used(17). They were tailored to each age group and involved interactive learning activities conducted in Arabic by a trained nutritionist. Topics included nutrition and healthy eating for children, the importance of breakfast, the importance of physical activity, food safety and hygiene.
Formative and process evaluation
In the first year of the programme, formative research was conducted with parents and teachers. This involved focus groups with parents to determine the best modality of payment for the school snacks (daily in cash given to children v. weekly or monthly to be paid by parents to the kitchens). Discussions were held with school administrators and teachers to make provisions for logistical arrangements of the study including location of school meal sales, timing and logistics for baseline data collection and timing of nutrition education sessions.
Process evaluation was conducted throughout the implementation of the programme and addressed participation in the programme (number of children participating per month, number of snacks sold per day), timings and logistics surrounding meals sold, delivery of nutrition education sessions (number of students/parents/teachers in attendance) and the effectiveness of the education sessions (short pre- and post-tests). Snack acceptability (low, medium, high) was measured using a three-point smiley-face scale throughout the intervention and snack waste (weighed waste) was recorded in the first and last month of the intervention. Feedback was obtained from school administrators, teachers and parents on programme implementation and on barriers for future implementation and continuation of the programme.
Outcome evaluation
Data were collected at baseline and at the 8-month time point (endline) on parents’ household food security and household dietary diversity, and on children’s dietary habits, anthropometry, Hb, breakfast recall, dietary diversity score and child-reported food security. School attendance records and test grades in mathematics and languages were collected by the school and shared with the research team. These data on impact of the school food intervention are beyond the scope of the present paper.
Results
Healthy Kitchens component
The kitchens initially trained and employed fifty-one women on a rotating basis to provide daily healthy snacks to children attending two local elementary schools. The age range of women varied from 18 to 64 years, with a median age of 41 years. However, eighteen women dropped out within the first week of the programme, once they realized the time commitment of their involvement. Thirty-three women (64·7 %) completed the study.
Work schedules
Discussions early in the development phase of the HK on the tasks, expectations and work schedule ensured sustained functioning of the kitchen. The schedule, which rotated women within teams, increased social interaction and the chance to gain experience from one another. It also organized tasks so that part of food preparation (purchasing, washing and cutting) was completed the day before, women then arrived at the kitchen early in the day, prepared food and were able to complete all tasks by 13.00 hours, to be home when their children arrived from school. A system was created whereby every woman had a substitute in a different group in case she was unable to make it to work on her assigned day and to prevent women from dropping out due to ad hoc time commitments. The resulting work schedule meant that women were working in the HK between 2 and 3 d/week.
Recipe development
The development of the monthly snack menu was participatory in nature and was an outcome of the focus groups and the ensuing trial period. Examples of modifications were the inclusion of yoghurt, deemed to be more culturally acceptable than milk; substitutions of fruits by season; changes in the shape of dough-based snacks to make them easier to hold and consume; and substituting rice with bulgur wheat, among others. The nutritionist worked with the women to adapt the recipes based on recommended nutrient content. In both refugee camps, the nutritionist visited local markets and primary distributors to assess food safety issues along the supply chain. There was a 2-month-long trial-and-error period to fine tune the recipes and develop a work schedule for each recipe to accommodate preparation and cooking in the short time allocated before recess, as all foods were prepared fresh daily. During this period, each recipe was made at least once by the women and all procurement and preparation options were explored to meet budget limits and avoid waste. Although the recipes were designed to avoid having excessive leftovers and waste, any leftover food that was produced was divided among the women to take home.
Organization
Based on the capacity-building sessions conducted, women allocated the tasks of cooking, purchasing and budgeting among themselves, according to their varying skill sets and literacy levels. Training sessions also addressed different organizational procedures for packaging and transportation of the snacks from the HK to the schools. School staff initially hesitated to participate in the distribution of meals and in the conduct of education sessions, but after working with the principal and teachers we were able to ensure that the intervention did not provide additional workload for teachers. The women worked closely with the school administration to develop an efficient system that did not interfere with teaching time and allowed for smooth distribution; for example, meals were packed in labelled boxes by class, which were delivered to the classroom door by a kitchen employee, with a list of schoolchildren’s names for distribution.
Community-based school nutrition intervention
Programme participation and payment modality
Out of 847 children attending the intervention schools, 746 assented to participate in the school food intervention (88 %), thirty-two children were lost to follow up; therefore, a total of 714 children participated in the healthy snack programme over the two intervention years: 228 in year 1 and 486 in year 2. Of these, 110 children were identified as hardship cases and were exempt from payment (thirty-five in year 1 and seventy-five in year 2). Participation in the school nutrition intervention was monitored monthly (Fig. 2). The results from the snack acceptability sheets (Fig. 3) show the percentage of children who reported high acceptability for any of the meals per month, and these data were used to determine which snacks would remain or be removed in the next menu iteration.
Fig. 2.
Child participation rate, by month of intervention (aggregate of years 1 and 2), in the Healthy Kitchens, Healthy Children school nutrition conducted among elementary-school children (n 714) in Palestinian refugee camps in Lebanon
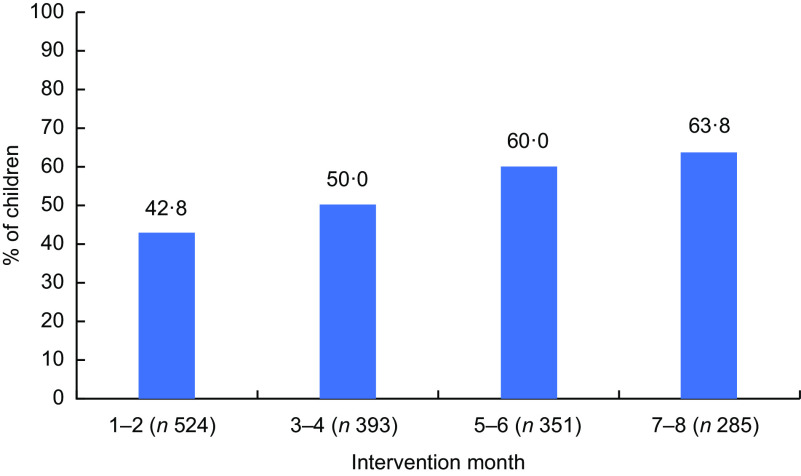
Fig. 3.
Percentage of children expressing high snack acceptability, by month of intervention (aggregate of years 1 and 2), in the Healthy Kitchens, Healthy Children school nutrition intervention conducted among elementary-school children (n 714) in Palestinian refugee camps in Lebanon
Participation decreased in the first three months as the snacks were still being tested and snack acceptability data were being collected and analysed. As snacks were adjusted and improved, participation stabilized and increased (to reach 66·7 %). The modality of payment also changed after consulting with parents and school administration in year 1. We first requested weekly payments, then changed to monthly payments and eventually allowed children and families the flexibility to pay daily, weekly or monthly to accommodate the financial situation of households. It is important to note that even though snack participation was completely voluntary, more than 55 % of children opted into the programme at any one time.
The endline survey also explored whether parents considered enrolling their children in the HKHC healthy snack programme the following academic year and how much they were willing to pay for the snacks. The results were encouraging as 90 % of participating parents in the intervention schools (i.e. parents of children who initially participated in the HKHC snacks but were not necessarily still receiving them at the time of the interview) and 95 % in the control schools responded positively (Table 2). There was variability, however, in the amount parents were willing and able to pay. Parents in the intervention schools were also asked whether children were given additional money besides the amount to cover the cost of the HKHC snacks. Seventy-seven per cent of parents reported giving an average of 1048 LBP (Lebanese pounds; $US 0·70) to their children per day.
Table 2.
Percentage of parents at endline considering enrolling their children in the Healthy Kitchens, Healthy Children school nutrition intervention the following year, by intervention group
| Intervention (n 527) | Control (n 508) | |||
|---|---|---|---|---|
| n or Mean | % or sd | n or Mean | % or sd | |
| Parents consider having their children participate next year, n and % | 475 | 90·1 | 485 | 95·5 |
| Amount willing to pay for the healthy snack, n and % | ||||
| 500 LBP ($US 0·33) | 239 | 45·4 | 139 | 27·4 |
| 750 LBP ($US 0·50) | 66 | 12·5 | 27 | 5·3 |
| 1000 LBP ($US 0·66) | 126 | 23·9 | 226 | 44·5 |
| 1500 LBP ($US 1·00) | 18 | 3·4 | 43 | 8·5 |
| Parents gave their children additional money, n and % | 385 | 77·2 | – | – |
| Amount of additional money, mean and sd (n 385) | ||||
| LBP | 1048·2 | 668·6 | – | – |
| $US | 0·70 | 0·46 | – | – |
LBP, Lebanese pound.
Educational component
Three health and nutrition education sessions were administered to each class, in all four schools; 58–68 % of children attending the sessions completed pre- and post-test questionnaires. For parent education sessions, an average of twenty parents attended two sessions in each school.
Discussion
To our knowledge, the HKHC programme is the first quasi-experimental intervention that implemented potential solutions to long-term food insecurity in protracted Palestinian refugees residing in urban refugee camps in Lebanon. If effective, this multipronged and multigenerational intervention model can be used in other settings to create food-related income-generating opportunities and improve dietary diversity of marginalized communities. The design allowed us to develop the model linking CBO to schools to deliver healthy school snacks and to test the acceptability of the meals by parents and children. As UNRWA is the main provider of services and resources for Palestinian refugees in Lebanon, the HKHC programme worked with the organization to deliver the multipronged intervention. We highlight the strengths and challenges of the HKHC experience below.
Challenges
Local environment
Identifying schools and CBO took much longer than anticipated due to the difficulty in finding schools that were able to be matched according to our inclusion criteria and also be close to CBO identified. UNRWA was instrumental in overcoming the challenges of working within such a constrained system. These initial difficulties underscore the importance of working with strong partners with community connections.
Recruitment of women to Healthy Kitchens
It is important to consider how the HKHC model and HK schedule can be modified to encourage women who live in difficult circumstances to participate. Only thirty-three of the fifty-one women recruited to the programme remained after the first week of the intervention. Addressing social constraints to participation is crucial to reduce attrition(26). The work schedule developed did address part of these issues, allowing women to return to childcare duties before the end of the school day.
School environment
At the school level, the main challenges related to: (i) the need for subsidisation of the meals; (ii) the lack of school policies around the regulation of sales of school food; which together led to (iii) fluctuations in programme participation.
1. Subsidization of meals and payment modalities
UNRWA schools have maintained their services despite funding constraints, but these constraints undoubtedly overburdened the school staff. In the second year of the intervention, a major challenge faced by one of the camps was the high influx of refugee children from neighbouring Syria who were identified as economic hardship cases(3). Schools had to accommodate doubling the number of schoolchildren within the existing school infrastructure due to the influx of Palestinian refugees from Syria who sought shelter within the Lebanon Palestinian camps(3). This was extremely challenging for the school administration and although we had agreed with UNRWA at the start of the intervention to cover the costs of the snacks for children from families with known hardship cases, this constituted a large number in year 2 (n 75). In this case, snack costs for children identified as hardship cases were provided from funds external to the HKHC intervention. The CBO that housed the HK had external funds to support orphans and children in need and were therefore able to cover the costs of their snacks.
Despite this increased pressure and the changes in payment modalities, there were no consequences for the kitchens. Numbers of children stabilized by month 3, regardless of payment modalities, with no major impact on planning for the number of meals needed per day. Since the programme was subsidized by the HKHC intervention and the CBO, the kitchens were able to cover the upfront costs of procuring ingredients and therefore not reduce or halt the production of snacks. This is extremely important with regard to sustainability in such a constrained environment with high poverty rates. For the HK to be able to cover children with hardship cases, the HK must make enough profit from paying children to subsidize the costs of hardship cases or have access to external funds. Most studies on cost-effectiveness and financial suitability of school feeding programmes have focused on national programmes(12) whereas few have explored this topic in the absence of state-led programmes. Some lessons could be learned from state-led school food programmes that vary subsidy amounts according to ability to pay(27).
2. Pre-existing canteens and the lack of school policies around the regulation of sales of school food
Within a context where policies around the regulation of unhealthy foods to children at school are lacking, we faced challenges with the pre-existing school canteens, similarly to other school feeding programmes(28). The canteens saw the intervention as competition despite our efforts to incorporate them into the model and provide solutions that addressed their concerns. Because these canteens are a source of livelihood for the individuals managing them, this reaction is understandable. Moreover, the canteens pay a proportion of profits to the schools. This relationship made it risky for the canteen owners to commit to an intervention that may be competition and affect canteen profits. To further complicate matters, there were familial, social and political relationships between canteen owners and teachers and school administrators. This led to delicate discussions and despite the involvement of UNRWA’s education department, this remained a major barrier to the sustainability of the programme. The ideal scenario would ensure that policies are in place to prohibit the sales of competitive unhealthy foods and the canteen owner could participate in the intervention by selling the healthy snacks at the canteen. Similar solutions to overcoming challenges with school canteens in school feeding programmes have been discussed(29). The income lost from these restrictions could be compensated through a salary from working with the HK.
3. Fluctuations in programme participation
Maintaining high participation in the healthy snacks was a recurrent challenge during both intervention years, partly resulting from the need for subsidization and the lack of regulation of sales of food discussed above. Another factor that could explain the drop in participation in month 3 was the fact that winter vacation occurred in the middle of December and parents were confused about what the payment schedule was around these holidays. Better communication between the programmes ahead of holidays could remove ambiguity over payments and food delivery, allowing for uninterrupted participation in the healthy snacks. The subsequent rise in participation could be attributed to the flexible payment modality, as well as improved communication and the participatory approach of the HKHC intervention. However, it is important to note that the number of children returning the acceptability sheets decreased over time, pointing to the possibility that only those who enjoyed the meals continued to receive and rate them. This decrease could also be due to survey fatigue(30).
Nutrition and health education sessions were well attended by children, as these were conducted during the school day, whereas it was difficult to obtain high attendance rates for parent education sessions; a common challenge in school programmes that address both the school and home environment(31). As parent sessions were also held during school hours, parents had obligations that prevented them from attending, including work and taking care of younger children at home. Exploring alternative ways of involving parents in school nutrition programmes is needed for students to receive consistent messages and to create a home environment conducive to healthy eating(29,31–33).
Strengths
Despite the challenges, the HKHC model had many strengths. Working with UNRWA and recruiting CBO that were well respected was important in ensuring recruitment of women and continuation of the HK beyond the study. The participatory approach of designing the kitchen work schedule with the women allowed their work schedules to be compatible with their duties and responsibilities at home. The participatory menu development also proved to be successful based on acceptability and participation rates.
Another key success of the HKHC model was to re-introduce traditional Palestinian food to schoolchildren. Processed foods are widely available, palatable and cheap, making it challenging to convince children not to consume them. Working with the women and monitoring the children’s acceptability of the snacks allowed us to provide traditional snacks that were acceptable(10). Anecdotal evidence indicated that after eating these foods at school, children requested these traditional foods from their parents at home. This stands in contrast to the decline in preparation of these traditional foods from many homes. A further strength of the intervention was involving school teachers and principals and having them act as role models for healthy eating habits(34). Eating with peers is very prominent in Palestinian culture, and being able to share the experience of eating the healthy snacks with peers and teachers encouraged children to participate, reinforcing the message that support and participation of school staff is crucial in such an intervention model(34).
Limitations
The HKHC intervention also had some limitations. Although the snacks were highly accepted, children continued to buy other foods from the school canteens, including processed foods. Children consuming more energy than usual as a result of the snack was a concern that we attempted to address in the design of the meals, but the snacks may have needed to be larger to prevent children from purchasing extra food. Moreover, although the subsidized snack cost less than the average pocket money given to children for school snacks, children ended up spending the same amount of money on school snacks compared with the previous year. Despite income transfer to the family being a commonly cited potential outcome of school feeding programmes, it has not been included in systematic reviews of the effects of school feeding programmes(35). If income transfer and improved food security are to be seen as an outcome of a school nutrition programme, the right balance between the size and cost of the meal should be further examined. Substitution (i.e. a subsequent reduction in food consumed at home) has been reported in some studies(36) but this finding did not appear to counterbalance the energy content of the school meal. However, several studies do report improvements in knowledge about nutrition and healthy food practices as well as increased dietary diversity(15,37–39).
Key lessons learned
The HKHC intervention was designed to be context specific and thus all aspects of the intervention were tailored to address logistical and cultural realities of living in an urban refugee camp in Beirut, Lebanon. However, the lessons learned and the key take-away messages can be applied to other similar contexts.
First, understanding the local political context and the dynamics of different institutions is crucial for programme success. Identifying key actors early on facilitates the process of establishing partnerships which are crucial for successful implementation and sustainability(12). Second, strong communication between HK and schools is instrumental to a functional intervention. Multiple meetings should be held between HK staff, school administration and teachers prior to and during the intervention to ensure the school staff are not overburdened by the intervention. Working with administrations and existing canteens (or equivalents) to create healthy food environments within the schools that do not deter children from participating in healthy meals is very important in ensuring buy-in from students(40). Designing snacks that are healthy, filling and acceptable to students is crucial to prevent children from purchasing other foods(10).
School feeding programmes show small positive effects on some nutrition and education outcomes; however, in many developing countries, school feeding programmes are highly reliant on external funding and are criticized for their lack of effectiveness and sustainability when they are not integrated into publicly funded educational policies(12). For a school feeding programme to persist, it should have an ‘exit strategy’ which implies that it should be able to transition from an externally supported programme to a national programme(12). The World Food Programme has set several standards to ensure quality and sustainability of school feeding programmes, which include stable funding and budgeting, a strategy for local production and sourcing, and strong community partnerships, among others(41). In the context of Palestinian refugees in Lebanon, it is unrealistic to plan for integration of such programmes into publicly funded educational policies of the Lebanese government or UNRWA. Consequently, it is essential to find alternative means to resume, sustain and support programmes that have the potential to improve food security and health status of Palestinian refugees in Lebanon. There is also a need for data on cost-effectiveness of the modality of the HKHC model and compare it with other potential designs(12). The HK are now still operating, with links to Palestinian nursery schools, orphanages and summer camps. Current activities are partly subsidized by a profit-generating catering business that has helped sustain the operations.
Conclusions
In conclusion, the HKHC model has the potential to advance the human capital of two generations of protracted refugees in Lebanon through its two-pronged design. The availability of schools as a constant market for these social enterprises offers an opportunity for sustainable livelihood generation and food security gains. If effective, this multigenerational intervention model can be used in other settings to create food-related income-generating opportunities and improve dietary diversity of marginalized communities. However, due to the economic precarity commonly experienced by protracted refugee communities, sufficient funding is required to establish and sustain such programmes. Moreover, funding should be able to cover formative, process and impact evaluations of the programme to truly understand what dimensions of the intervention are successful and how they can be improved to better suit the needs of the population.
Acknowledgements
Acknowledgements: The authors would like to acknowledge the Women Program Association and Baraem Association for setting up the Healthy Kitchens and running the kitchens for the school year. In addition, the authors would like to thank Reem Talhouk for her support in costing the healthy snacks and Ali Basma for his architecture support for the refurbishment of the kitchens. Finally, the authors would like to thank UNRWA for its crucial and continuous support of the kitchens and for its assistance with data collection. Financial support: This research was supported by a grant from The Nestlé Foundation (Lausanne, Switzerland) for the study of problems of nutrition in the world. The funder had no role in the study design, analysis or writing of this article. Conflict of interest: None. Authorship: N.R.S. and H.G. designed the study presented here and designed the study evaluations; A.R.M., J.C. and Z.J. conducted the field research; Z.J. analysed the data and performed statistical analysis; J.C. drafted the manuscript and had final responsibility for submitting this article for publication; H.G., N.R.S., Z.J. and J.C. interpreted the results and provided critical intellectual feedback to revise the manuscript. All authors read and approved the final manuscript. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the Institutional Review Boards of the American University of Beirut and the University of Maryland. Written informed consent was obtained from all subjects prior to participation and subjects had the right to withdraw from the study at any time without any penalty or loss of benefits.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980019003161.
click here to view supplementary material
References
- 1. Shiblak A (1996) Residency status and civil rights of Palestinian refugees in Arab countries. J Palestine Stud 25, 36–45. [Google Scholar]
- 2. Knudsen A & Hanafi S (2010) Palestinian Refugees: Identity, Space and Place in the Levant. London: Routledge. [Google Scholar]
- 3. Chaaban J, Salti N, Ghattas H et al . (2016) Survey on the Socioeconomic Status of Palestine Refugees in Lebanon 2015. Beirut: American University of Beirut and the United Nations Relief and Works Agency for Palestine Refugees in the Near East. [Google Scholar]
- 4. Sabatinelli G, Pace-Shanklin S, Riccardo F et al. (2009) Palestinian refugees outside the occupied Palestinian territory. Lancet 373, 1063–1065. [DOI] [PubMed] [Google Scholar]
- 5. UNICEF (2012) The State of the World’s Children 2012: Children in An Urban World. New York: UNICEF. [Google Scholar]
- 6. United Nations Relief and Works Agency for Palestine Refugees in the Near East (2017) Health Department Annual Report 2017. Amman: UNWRA. [Google Scholar]
- 7. Beerlandt H & Huysman S (1999) Manual for Bottom-Up-Approach in Food Security Interventions: Analysis of Target Groups. Rome: International Fund for Agricultural Development. [Google Scholar]
- 8. Engler-Stringer R & Berenbaum S (2007) Exploring food security with collective kitchens participants in three Canadian cities. Qual Health Res 17, 75–84. [DOI] [PubMed] [Google Scholar]
- 9. Iacovou M, Pattieson DC, Truby H et al. (2013) Social health and nutrition impacts of community kitchens: a systematic review. Public Health Nutr 16, 535–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kristjansson E, Gelli A, Welch V et al. (2016) Costs, and cost-outcome of school feeding programmes and feeding programmes for young children. Evidence and recommendations. Int J Educ Dev 48, 79–83. [Google Scholar]
- 11. Loopstra R & Tarasuk V (2013) Perspectives on community gardens, community kitchens and the Good Food Box program in a community-based sample of low-income families. Can J Public Health 104, e55–e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bundy D, Burbano C, Grosh ME et al. (2009) Rethinking School Feeding: Social Safety Nets, Child Development, and the Education Sector. Washington, DC: The World Bank. [Google Scholar]
- 13. Bartfeld JS & Ahn H-M (2011) The School Breakfast Program strengthens household food security among low-income households with elementary school children. J Nutr 141, 470–475. [DOI] [PubMed] [Google Scholar]
- 14. Galloway R, Kristjansson E, Gelli A et al. (2009) School feeding: outcomes and costs. Food Nutr Bull 30, 171–182. [DOI] [PubMed] [Google Scholar]
- 15. Fano TJ, Tyminski SM, Flynn MA (2004) Evaluation of a collective kitchens program using the population health promotion. Can J Diet Pract Res 65, 72–80. [DOI] [PubMed] [Google Scholar]
- 16. Racine S & St-Onge M (2009) Les cuisines collectives: une voie vers la promotion de la santé mentale. Can J Commun Ment Health 19, 37–62. [PubMed] [Google Scholar]
- 17. Batal M, Ghattas H & Abou-Ezze R (2013) A school feeding program based on the ecohealth approach: a case study from rural Lebanon. Presented at Experimental Biology 2013, Boston, MA, USA, 20–24 April 2013.
- 18. Habicht J-P, Victora C & Vaughan JP (1999) Evaluation designs for adequacy, plausibility and probability of public health programme performance and impact. Int J Epidemiol 28, 10–18. [DOI] [PubMed] [Google Scholar]
- 19. Leroy JL & Menon P (2008) From efficacy to public health impact: a call for research on program delivery and utilization in nutrition. J Nutr 138, 628–629. [DOI] [PubMed] [Google Scholar]
- 20. World Food Programme (2000) School Feeding Handbook. Rome: WFP. [Google Scholar]
- 21. US Department of Health and Human Services & US Department of Agriculture (2015) 2015–2020 Dietary Guidelines for Americans, 8th ed. https://health.gov/dietaryguidelines/2015/resources/2015-2020_Dietary_Guidelines.pdf (accessed November 2019).
- 22. Sahyoun NR, Nord M, Sassine AJ et al . (2014) Development and validation of an Arab family food security scale. J Nutr 144, 751–757. [DOI] [PubMed] [Google Scholar]
- 23. Kennedy G, Ballard T & Dop MC (2011) Guidelines for Measuring Household and Individual Dietary Diversity. Rome: FAO. [Google Scholar]
- 24. George LK, Blazer DG, Hughes DC et al. (1989) Social support and the outcome of major depression. Br J Psychiatry 154, 478–485. [DOI] [PubMed] [Google Scholar]
- 25. Veit CT & Ware JE (1983) The structure of psychological distress and well-being in general populations. J Consult Clin Psychol 51, 730–742. [DOI] [PubMed] [Google Scholar]
- 26. Buvinić M & Furst-Nichols R (2014) Promoting women’s economic empowerment: what works? World Bank Res Obs 31, 59–101. [Google Scholar]
- 27. US Department of Agriculture, Food and Nutrition Service (2018) National School Lunch Program. https://www.fns.usda.gov/nslp/national-school-lunch-program-nslp (accessed November 2019).
- 28. Kain J, Uauy R, Vio F et al. (2004) School-based obesity prevention in Chilean primary school children: methodology and evaluation of a controlled study. Int J Obes Relat Metab Disord 28, 483–493. [DOI] [PubMed] [Google Scholar]
- 29. Drummond C & Sheppard L (2011) Examining primary and secondary school canteens and their place within the school system: a South Australian study. Health Educ Res 26, 739–749. [DOI] [PubMed] [Google Scholar]
- 30. Porter SR, Whitcomb ME & Weitzer WH (2004) Multiple surveys of students and survey fatigue. New Dir Inst Res 2004, issue 121, 63–73. [Google Scholar]
- 31. Blom-Hoffman J, Wilcox KR, Dunn L et al . (2008) Family involvement in school-based health promotion: bringing nutrition information home. School Psych Rev 37, 567–577. [PMC free article] [PubMed] [Google Scholar]
- 32. Briggs M, Fleischhacker S & Mueller CG (2010) Position of the American Dietetic Association, School Nutrition Association, and Society for Nutrition Education: comprehensive school nutrition services. J Nutr Educ Behav 42, 360–371. [DOI] [PubMed] [Google Scholar]
- 33. Pérez-Rodrigo C & Aranceta J (2001) School-based nutrition education: lessons learned and new perspectives. Public Health Nutr 4, 131–139. [DOI] [PubMed] [Google Scholar]
- 34. Habib-Mourad C, Ghandour LA, Moore HJ et al . (2014) Promoting healthy eating and physical activity among school children: findings from Health-E-PALS, the first pilot intervention from Lebanon. BMC Public Health 14, 940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Jomaa LH, McDonnell E & Probart C (2011) School feeding programs in developing countries: impacts on children’s health and educational outcomes. Nutr Rev 69, 83–98. [DOI] [PubMed] [Google Scholar]
- 36. Powell CA, Walker SP, Chang SM et al. (1998) Nutrition and education: a randomized trial of the effects of breakfast in rural primary school children. Am J Clin Nutr 68, 873–879. [DOI] [PubMed] [Google Scholar]
- 37. Spence F & Van Teijlingen ER (2005) A qualitative evaluation of community-based cooking classes in Northeast Scotland. Int J Health Promot Educ 43, 59–63. [Google Scholar]
- 38. Tarasuk V & Reynolds R (1999) A qualitative study of community kitchens as a response to income-related food insecurity. Can J Diet Pract Res 60, 11–16. [PubMed] [Google Scholar]
- 39. Marquis S, Thomson C & Murray A (2001) Assisting people with a low income: to start and maintain their own community kitchens. Can J Diet Pract Res 62, 130–132. [PubMed] [Google Scholar]
- 40. Briefel RR, Wilson A & Gleason PM (2009) Consumption of low-nutrient, energy-dense foods and beverages at school, home, and other locations among school lunch participants and nonparticipants. J Am Diet Assoc 109, 2 Suppl., S79–S90. [DOI] [PubMed] [Google Scholar]
- 41. World Food Programme (2009) Feed Minds, Change Minds – School Feeding: Highlights and New Directions. Rome: WFP. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980019003161.
click here to view supplementary material