Abstract
Objective:
To deepen understanding of the relationship between food insecurity, acculturation, and diagnosis of CHD and related health outcomes among immigrant adults.
Design:
Using cross-sectional, nationally representative data from the National Health Interview Survey 2011 to 2015, we address two research questions. First, what is the relationship of household food insecurity and acculturation with: CHD, angina pectoris, heart attack, self-rated poor health and obesity? Second, what is the association of food insecurity with these health outcomes over years of living in the USA? We estimate multivariate logistic regressions without (question 1) and with (question 2) an interaction term between food insecurity and acculturation for CHD and related health outcomes.
Setting:
USA.
Participants:
Low-income immigrant adults.
Results:
Food insecurity and acculturation are both associated with diagnosis of CHD and related health outcomes among immigrant adults. Food insecurity and acculturation are associated with the health of female immigrants more than males. Also, the differences by food security status in the probability of having several poor health outcomes (self-rated heath, obesity, women’s angina pectoris) are largest for those in the USA for less than 5 years, decrease for those who have lived in the USA for 5–14 years, and are larger again for those in the USA for 15 or more years.
Conclusions:
Recent and long-term food-insecure immigrants are more vulnerable to CHD and related health outcomes than those in the USA for 5–14 years. Further research is needed to understand why.
Keywords: Food security, Acculturation, Healthy immigrant effect, Cardiometabolic health, Heart-related health
The immigrant population in the USA has increased significantly over the last several decades. Immigrants were 14 % of the US population in 2013, up from 8 % in 1990( 1 ). Research on the determinants of immigrant health shows that US immigrants tend to have a combination of good health and low socio-economic status upon their arrival, but this health advantage over their socio-economic native-born peers tends to decline the longer they live in the USA.† Acculturation, then, measured by the number of years living in the USA,‡ is associated with poorer health. Exposure to the US environment often leads immigrants to adopt American lifestyles and dietary behaviours( 6 ). These dietary and behavioural changes can have important health implications for immigrants over time, especially for the food insecure.
Households are considered food secure if they have access at all times to the foods necessary for all members to enjoy an active, healthy life( 7 ). Food insecurity entails having difficulty consistently obtaining adequate food because of limited economic resources. Many factors make immigrants more likely to experience food insecurity than the native-born population( 8 – 13 ). For example, their immigrant status may affect their access to federal assistance programmes( 8 , 14 – 16 ). Low-wage employment, limited education (i.e. lack of a high-school diploma), job insecurity, language barriers and marginal social standing can be common among immigrants( 11 ). These economic constraints can lead to uncertain access to food and may also contribute to health inequalities( 17 – 19 ).
Food insecurity is associated with a range of negative health outcomes among native-born US adults. These include chronic diseases such as stroke, cancer and asthma( 19 – 21 ) and cardiometabolic conditions such as CHD, diabetes, obesity and hypertension( 22 – 29 ). Food insecurity also makes managing these conditions difficult( 22 ). For example, due to the higher cost of whole grains, lean proteins and fresh produce, which are a critical part of preventing and managing such conditions, they are less often consumed in the diets of the food insecure( 22 , 24 , 30 ).
Most research on food security and heart-related health has not distinguished immigrants from the native born, whether it is directed at adults( 20 ) or children( 31 ). Yet their relative advantage over their socio-economic peers, in terms of health condition upon arrival, and their deterioration over years of living in the USA, suggest that food insecurity may affect the health of immigrants differently from the population overall. Using repeated cross-sectional data from the National Health Interview Survey (NHIS) from 2011 to 2015, we address two research questions. First, what is the relationship of household food insecurity and acculturation with diagnosis of CHD and related health outcomes, namely angina pectoris, heart attack, self-rated poor health and obesity? These health conditions are relevant to public health policy given their preventability and their prevalence, cost and morbidity in the USA( 5 , 20 , 32 ). Second, what is the association of food insecurity with CHD and related outcomes over years of living in the USA?
To answer these questions, we first estimate a series of multivariate logistic regression models examining the associations of household food insecurity and acculturation separately with each of the five health outcomes. Second, we estimate the logistic regressions with an interaction term between food insecurity and acculturation. We also examine heterogeneity across the severity of food insecurity to see if the relationships between household food insecurity and CHD and related outcomes change with the severity of food insecurity. Identifying the relationships of food insecurity and acculturation with CHD and related health outcomes among immigrant adults is an important step towards the development of appropriate health intervention strategies.
Data
The analyses in the present paper use pooled cross-sectional data from the 2011 to 2015 waves of the NHIS, an in-person health survey of the civilian non-institutionalized population of the USA conducted by the US Census Bureau for the National Center for Health Statistics. The sampling strategy follows a multistage area probability design that, when weighted, results in a nationally representative sample. The NHIS collects detailed information on demographics and topics including health status and limitations, injuries, health-care access and utilization, health insurance coverage, immigration status, and income and assets. Beginning in 2011, the US Department of Agriculture sponsored the inclusion of the ten-item, adult 30 d food security module in the NHIS.
The sample consists of working-age immigrant adults aged 18 to 64 years in households at or below 300 % of the federal poverty line. Following Gregory and Coleman-Jensen( 20 ), we exclude retirement-age respondents because of their differences in time allocation, income and health insurance from working-age adults. We also exclude higher-income households to compare food-insecure households with other low-income non-food-insecure households with similar resource constraints. Our interest is the heart-related health outcomes of immigrants and not the comparison between immigrants and other groups, such as US-born non-Hispanic Whites. Therefore, we exclude US-born persons from the sample.
A total of 171 910 individuals were interviewed by NHIS in 2011–2015. We limit the sample to households for whom the sample person is an immigrant born outside the territorial USA (excluding 141 174 observations), is a working-age adult (excluding 3856 observations), is not a pregnant woman (excluding 1648 observations), lives in a household that has income less than or equal to 300 % of the federal poverty line (excluding 8996 observations), and is not missing information on the food security module questions, health conditions or control variables (excluding 737 observations). The final sample consists of 15 499 immigrant adults at or below 300 % of the federal poverty line.
Dependent variables
We examine five diet-related health outcomes: CHD, angina pectoris, heart attack, self-rated poor health and obesity. Clinical management and prevention of these diagnosed conditions include dietary recommendations( 22 ). While self-rated health is not technically classified as a heart-related health condition, we include it here since it is commonly used in the literature as an important health measure and highly correlated with the other heart-related health outcomes. Also, while the other measures are based on a diagnosis from a doctor, self-rated poor health allows respondents to give their subjective interpretation of how they feel and is not dependent on health-care access/utilization.
Self-rated health is measured by the individual’s response to the following question: ‘Would you say your health in general is excellent, very good, good, fair or poor?’ Self-rated poor health is a binary measure equal to 1 if the respondent reported his or her health was fair or poor, and 0 if the respondent reported his or her health was good, very good or excellent. Following National Institutes of Health clinical guidelines, we define obesity as BMI of 30 kg/m2 or above. Self-reported measures of height and weight are often misreported but maintaining a sample of non-elderly adults (18–64 years) and reporting results separately by gender should minimize the effects of reporting bias( 6 ). CHD, angina pectoris or heart attack are binary variables based on diagnosis by a medical professional.
Food insecurity
The focal explanatory variable in the present study is household food insecurity. We obtain this variable from the ten-item US Adult Food Security Survey Module examining the household’s circumstances regarding food access over the past 30 d. Each question asks about the household’s circumstances or behaviours when having difficulty meeting their basic food needs due to a lack of economic resources. The sum of affirmed responses from the survey module provides the measure of the household’s food security status( 7 , 33 ). Households are then categorized into four groups: high food security, marginal food security, low food security and very low food security. For the analyses, we first use a binary measure of the household’s severity of food insecurity. Food insecurity is coded as 1 if a household experienced low or very low food security within the past 30 d; 0 otherwise. This measure captures experiences related to food insecurity that range in severity from reducing the quality and variety of food to experiencing physiological hunger. In subsequent analysis, we use a categorical version of food security status that includes the four groups: high food security, marginal food security, low food security and very low food security.
Acculturation
The NHIS provides a categorical measure for length of US residence: less than 1 year, 1–4 years, 5–9 years, 10–14 years, and 15 years or more. To maintain appropriate sample size and variation in food security status (i.e. no immigrant in the ‘less than 1 year’ category reported being food insecure), we combined and recoded the first two categories as 0–4 years. Thus, the categorical measure of years in the USA includes the four groups: 0–4 years, 5–9 years, 10–14 years, and 15 years or more. Consistent with previous research (e.g. Antecol and Bedard and Commodore-Mensah et al.( 2 , 5 )), this information provides the primary measure of acculturation.
Other control variables
Research shows gender plays an important role for both food insecurity and CHD and related health outcomes( 34 ). Women are particularly sensitive to food insecurity since they often act as household managers of food issues, sometimes depriving themselves in times of scarcity to feed other household members( 34 – 39 ). This behaviour can create health inequalities between women and men. Thus, in addition to the analysis using the total sample, we also decompose the sample by gender. The analysis includes additional controls for many demographic and socio-economic determinants of immigrant health: age, age-squared,* race and ethnicity, education level, marital status, size of family, number of children, any elderly persons present in household, the individual’s employment status, log household income,† citizenship status, health insurance coverage status and region of US residence. We use the individual’s ability to speak English well as a second marker of acculturation. English is an indicator variable equal to 1 if the individual speaks English well or very well.
The NHIS also collects information on the individual’s region of birth. This variable categorizes respondents’ region of birth in the following nine regions: Mexico, Central America, Caribbean Islands (MCC); South America (SA); Europe (EU); Russia and former Soviet Union areas (RSA); Africa (AF); the Middle East (ME); Indian subcontinent (IND); Central Asia (CA); and Southeast Asia (SEA). MCC is the largest immigrant group in the USA, making up roughly 68 % of the sample.
Econometric methods
The overall goal is to answer the following two research questions. First, what is the relationship of household food insecurity and acculturation with CHD and related health outcomes? To answer this question, we estimate a series of multivariate logistic regression models examining the associations of household food insecurity and acculturation separately with each of the five health outcomes.‡ Second, how is food insecurity associated with these health outcomes over years of living in the USA? This step involves estimating the logistic regressions with an interaction term between food insecurity and acculturation. This reveals whether living longer in the USA moderates the relationship between food insecurity and poor heart-related health.
Consider the following model:
| (1) |
where
 and
and
 are latent binary variables representing the utility associated with an individual’s underlying health outcome and his or her household’s food security status, respectively. The βs represent the estimated regression coefficients; x
i contains exogenous variables to control for the common determinants of heart-related health outcomes y
i
, as described above; years represents the categorical measure of length of US residence (acculturation);
are latent binary variables representing the utility associated with an individual’s underlying health outcome and his or her household’s food security status, respectively. The βs represent the estimated regression coefficients; x
i contains exogenous variables to control for the common determinants of heart-related health outcomes y
i
, as described above; years represents the categorical measure of length of US residence (acculturation);
 contains the interaction term of household food insecurity with the measure of length of USA residence; and
contains the interaction term of household food insecurity with the measure of length of USA residence; and
 represents unobserved individual heterogeneity. Thus, the probability that an immigrant adult experiences CHD or a related health outcome is:
represents unobserved individual heterogeneity. Thus, the probability that an immigrant adult experiences CHD or a related health outcome is:
| (2) |
where F (·) is the logistic cumulative distribution function
| (3) |
where
 and
and
 is assumed to be distributed with var (ε) = π2/3. We estimate these probabilities using maximum likelihood. Since the data are observational and cross-sectional, endogeneity may be of concern and causality cannot be inferred without strong assumptions. However, the findings reveal strong associations between the variables of interest.
is assumed to be distributed with var (ε) = π2/3. We estimate these probabilities using maximum likelihood. Since the data are observational and cross-sectional, endogeneity may be of concern and causality cannot be inferred without strong assumptions. However, the findings reveal strong associations between the variables of interest.
Results
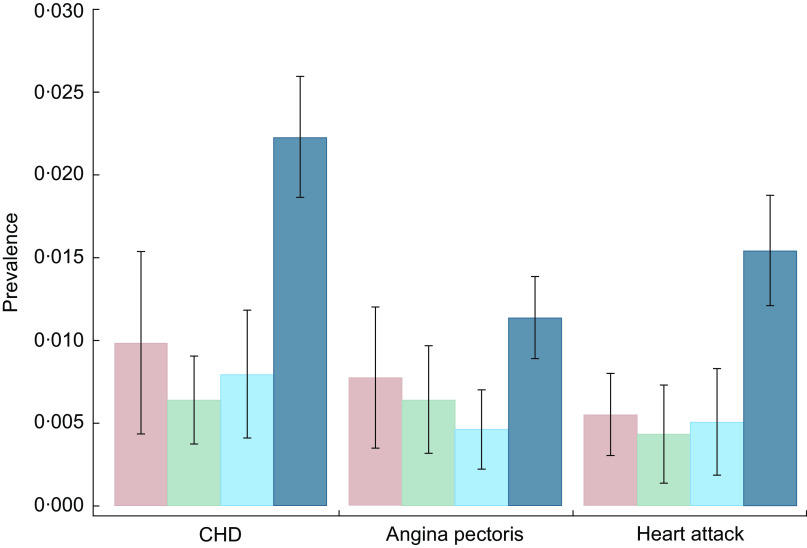
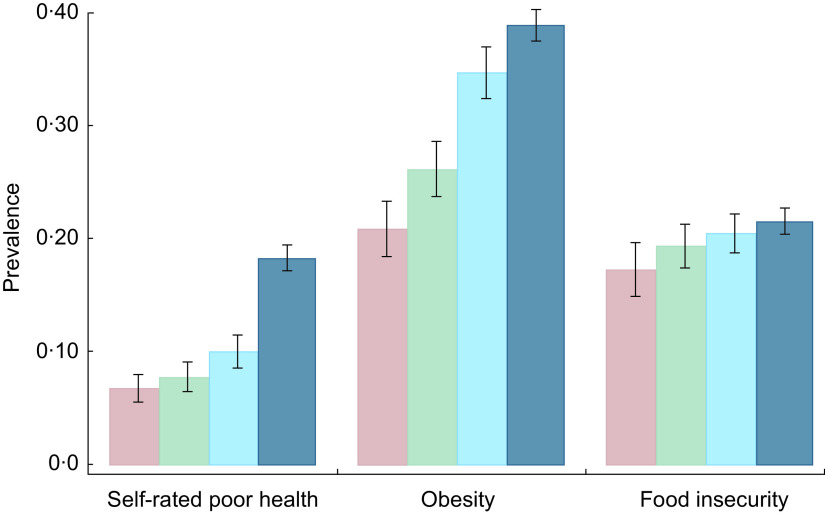
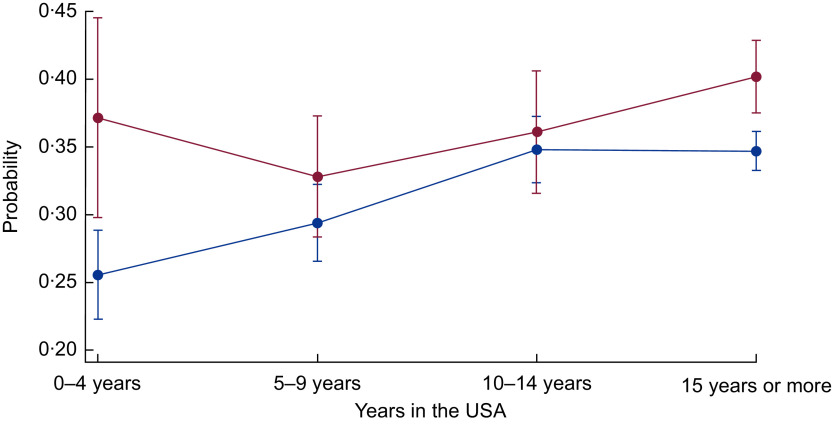
Figures 1 and Fig. 2 show the prevalence of CHD, angina pectoris and heart attack (Fig. 1) and self-rated poor health, obesity and food insecurity (Fig. 2) over years of living in the USA. In the sample of low-income immigrant adults, 15 years or more in the USA is associated with a higher prevalence of all poor health and food insecurity indicators. Interestingly, for CHD, angina pectoris and heart attack, the prevalence rates are lower among those with 5–14 years in the USA than among those with 0–4 years in the USA.
Fig. 1.
Prevalence of CHD, angina pectoris and heart attack over years of living in the USA ( , 0–4 years;
, 0–4 years;  , 5–9 years;
, 5–9 years;  , 10–14 years;
, 10–14 years;  , 15 years or more) among low-income, working-age immigrant adults. Data source is the pooled National Health Interview Survey 2011–2015. Values are proportions, with their se represented by vertical bars. Estimates account for complex survey design and confidence intervals are estimated at the 95 % level
, 15 years or more) among low-income, working-age immigrant adults. Data source is the pooled National Health Interview Survey 2011–2015. Values are proportions, with their se represented by vertical bars. Estimates account for complex survey design and confidence intervals are estimated at the 95 % level
Fig. 2.
Prevalence of self-rated poor health, obesity and food insecurity over years of living in the USA ( , 0–4 years;
, 0–4 years;  , 5–9 years;
, 5–9 years;  , 10–14 years;
, 10–14 years;  , 15 years or more) among low-income, working-age immigrant adults. Data source is the pooled National Health Interview Survey 2011–2015. Values are proportions, with their se represented by vertical bars. Estimates account for complex survey design and confidence intervals are estimated at the 95 % level
, 15 years or more) among low-income, working-age immigrant adults. Data source is the pooled National Health Interview Survey 2011–2015. Values are proportions, with their se represented by vertical bars. Estimates account for complex survey design and confidence intervals are estimated at the 95 % level
Table 1 shows significant heterogeneity in the prevalence of food insecurity and CHD and related health outcomes by region of birth. The prevalence of food insecurity is highest for those born in MCC (24·6 %), followed by AF (21·9 %), EU (16·1 %) and SA (15·9 %). The prevalence of CHD is highest for immigrants from ME (3·2 %). Angina pectoris is highest among immigrants from EU (1·7 %), and heart attack is most prevalent among immigrants from ME (2·5 %). Self-rated poor health is highest for those born in MCC or ME (both 15·3 %). Lastly, the prevalence of obesity is highest for immigrants from MCC (41·2 %).
Table 1.
Prevalence of CHD and related outcomes and food insecurity for low-income, working-age immigrant adults in the USA by region of birth
| Total sample | MCC | SA | EU | RSA | AF | ME | IND | CA | SEA | |
|---|---|---|---|---|---|---|---|---|---|---|
| Food insecurity | 0·206 | 0·246 | 0·159 | 0·161 | 0·098 | 0·219 | 0·099 | 0·088 | 0·058 | 0·133 |
| se | 0·005 | 0·006 | 0·015 | 0·017 | 0·031 | 0·022 | 0·028 | 0·013 | 0·010 | 0·011 |
| CHD | 0·016 | 0·016 | 0·013 | 0·028 | 0·003 | 0·003 | 0·032 | 0·021 | 0·011 | 0·011 |
| se | 0·001 | 0·001 | 0·004 | 0·007 | 0·003 | 0·002 | 0·011 | 0·007 | 0·004 | 0·004 |
| Angina pectoris | 0·009 | 0·009 | 0·005 | 0·017 | 0·006 | 0·001 | 0·010 | 0·011 | 0·006 | 0·007 |
| se | 0·001 | 0·001 | 0·003 | 0·007 | 0·005 | 0·001 | 0·005 | 0·005 | 0·00 | 0·00 |
| Heart attack | 0·011 | 0·011 | 0·007 | 0·015 | 0·006 | 0·008 | 0·025 | 0·014 | 0·010 | 0·007 |
| se | 0·001 | 0·001 | 0·003 | 0·005 | 0·006 | 0·005 | 0·010 | 0·005 | 0·005 | 0·003 |
| Self-rated poor health | 0·138 | 0·153 | 0·089 | 0·131 | 0·117 | 0·083 | 0·153 | 0·099 | 0·096 | 0·134 |
| se | 0·004 | 0·005 | 0·012 | 0·018 | 0·033 | 0·012 | 0·028 | 0·015 | 0·013 | 0·011 |
| Obesity | 0·342 | 0·412 | 0·243 | 0·335 | 0·223 | 0·313 | 0·282 | 0·152 | 0·103 | 0·142 |
| se | 0·005 | 0·006 | 0·015 | 0·022 | 0·054 | 0·022 | 0·035 | 0·017 | 0·013 | 0·014 |
| Number of observations | 15 499 | 9949 | 906 | 779 | 240 | 684 | 410 | 658 | 761 | 1112 |
Data source is the pooled National Health Interview Survey 2011–2015. Coefficients are proportions, with se given in the following row. All estimates account for complex survey design. Analysis sample includes households at or below 300 % of the federal poverty line. The immigrants’ region of birth are the following nine possible regions: Mexico, Central America, Caribbean Islands (MCC); South America (SA); Europe (EU); Russia and former Soviet Union areas (RSA); Africa (AF); the Middle East (ME); Indian subcontinent (IND); Central Asia (CA); and Southeast Asia (SEA).
Table 2 shows descriptive statistics for our sample of low-income immigrant adults and their households. The sample is evenly split between female and male respondents. The majority of the sample is Hispanic (65·1 %) and married or with a domestic partner (65·2 %). About 40 % of the sample has no high-school diploma. A minority of the sample are US citizens (38·7 %) and 30·4 % speak English well. About 8% of respondent households include a senior adult. A slight majority of respondents have health insurance (54·4 %). A majority of respondents have been in the USA for 15 years or more (54·6 %) and most are employed (67·7 %). The average age of respondents is 40 years, with about four members in the household and one child on average.
Table 2.
Descriptive statistics of the sample population of low-income, working-age immigrant adults in the USA
| Categorical explanatory variable | Frequency (n) | Proportion or se |
|---|---|---|
| Female | 7807 | 0·504 |
| se | 0·005 | |
| Ethnicity | ||
| Hispanic | 10 097 | 0·651 |
| se | 0·008 | |
| Non-Hispanic White | 1585 | 0·102 |
| se | 0·005 | |
| Non-Hispanic Black | 1271 | 0·082 |
| se | 0·004 | |
| Non-Hispanic Asian or Other | 2545 | 0·164 |
| se | 0·006 | |
| Marital status | ||
| Married or domestic partner | 10 110 | 0·652 |
| se | 0·005 | |
| Widowed, separated or divorced | 1954 | 0·126 |
| se | 0·00 | |
| Never married | 3434 | 0·222 |
| se | 0·005 | |
| Education status | ||
| High-school dropout | 6133 | 0·395 |
| se | 0·007 | |
| High-school graduate/GED | 4000 | 0·258 |
| se | 0·005 | |
| More than high school | 5366 | 0·347 |
| se | 0·007 | |
| US citizen | 5996 | 0·387 |
| se | 0·007 | |
| Speaks English well | 4707 | 0·304 |
| se | 0·005 | |
| At least one senior in household | 1282 | 0·083 |
| se | 0·003 | |
| Health insurance coverage | 8434 | 0·544 |
| se | 0·007 | |
| Years in the USA | ||
| 0–4 years | 1718 | 0·111 |
| se | 0·004 | |
| 5–9 years | 2294 | 0·148 |
| se | 0·004 | |
| 10–14 years | 3022 | 0·195 |
| se | 0·004 | |
| 15 years or more | 8464 | 0·546 |
| se | 0·006 | |
| Person is employed | 10 486 | 0·677 |
| se | 0·005 | |
| Continuous explanatory variable | Mean | |
| Age (years) | 39·7 | |
| se | 0·158 | |
| Size of family | 3·8 | |
| se | 0·024 | |
| Number of children | 1·3 | |
| se | 0·017 | |
| Log household income | 10·7 | |
| se | 0·019 | |
| Number of observations | 15 499 | |
GED, General Educational Development.
Data source is the pooled National Health Interview Survey 2011–2015. Coefficients are proportions, with their se given in the following row. All estimates account for complex survey design. Analysis sample includes households at or below 300 % of the federal poverty line.
Associations of food insecurity and acculturation with CHD and related outcomes
Next, we present OR from multivariate logistic regressions of household food insecurity and acculturation v. CHD and related health outcomes (without using the interaction term between food insecurity and acculturation). Estimation results for each of the five health outcomes appear in the top panels of Tables 3 and 4 among the full sample and in the sample divided by gender.* The interaction effects shown in the bottom panels are discussed in the next section. Overall, the results show a strong association between food insecurity and poor heart-related health, just as the stress from food insecurity and/or diet sensitivity of the conditions examined would suggest. Table 3 shows that food insecurity is associated with 57 % higher odds of being diagnosed with CHD, 81 % higher odds of angina pectoris and more than doubled odds of heart attack. For all three heart outcomes, the relationship with food insecurity is stronger for women and not significant for men. Number of years in the USA (acculturation) is statistically significant only for angina pectoris for the female sub-sample. The symbol † signifies where female coefficients are statistically significantly different from male coefficients. Gender differences in food insecurity are statistically significant for angina pectoris, heart attack and obesity; while gender differences in acculturation are statistically significant for angina pectoris, self-rated poor health and obesity. Female immigrants in the US for 5 years or more are less likely to have been diagnosed with angina pectoris than those in the US for less than 5 years (OR = 0·436, 0·202 and 0·325 for 5–9 years, 10–14 years and 15 years or more, respectively).
Table 3.
Results from multivariate logistic regressions of household food insecurity and acculturation v. CHD, angina pectoris and heart attack among low-income, working-age immigrant adults in the USA
| Variable | CHD | Angina pectoris | Heart attack | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Full sample | Female | Male | Full sample | Female | Female – interaction model | Male | Full sample | Female | Male | |
| Food insecurity | 1·565*** | 1·857*** | 1·339 | 1·812*** | 2·502***,† | 3·059 | 1·192 | 2·197*** | 4·046***,† | 1·453 |
| se | 0·227 | 0·396 | 0·309 | 0·299 | 0·637 | 2·118 | 0·285 | 0·448 | 1·327 | 0·371 |
| Years in the USA (Ref.: 0–4) | ||||||||||
| 5–9 years | 0·885 | 1·030 | 0·652 | 0·992 | 0·436*,† | 0·705 | 2·454 | 1·290 | 1·732 | 0·413 |
| se | 0·355 | 0·586 | 0·404 | 0·379 | 0·205 | 0·417 | 1·505 | 0·548 | 1·324 | 0·361 |
| 10–14 years | 0·908 | 1·099 | 0·667 | 0·608 | 0·202***,† | 0·349 | 2·107 | 1·290 | 1·053 | 1·228 |
| se | 0·383 | 0·562 | 0·399 | 0·245 | 0·112 | 0·227 | 1·267 | 0·579 | 0·883 | 0·868 |
| 15 years or more | 1·130 | 1·100 | 1·032 | 0·706 | 0·325***,† | 0·299*** | 1·787 | 1·778 | 1·193 | 1·969 |
| se | 0·404 | 0·613 | 0·505 | 0·229 | 0·120 | 0·135 | 0·972 | 0·708 | 0·981 | 1·188 |
| Interaction | ||||||||||
| Food insecurity × 5–9 years | – | – | – | – | – | 0·269 | – | – | – | – |
| se | – | – | – | – | – | 0·246 | – | – | – | – |
| Food insecurity × 10–14 years | – | – | – | – | – | 0·100** | – | – | – | – |
| se | – | – | – | – | – | 0·114 | – | – | – | – |
| Food insecurity × 15 years or more | – | – | – | – | – | 1·099 | – | – | – | – |
| se | – | – | – | – | – | 0·814 | – | – | – | – |
| Interaction F statistic | – | – | – | – | – | 3·58 | – | – | – | – |
| Interaction P value | – | – | – | – | – | 0·014 | – | – | – | – |
| Number of observations | 15 499 | 7807 | 7691 | 15 499 | 7807 | 7807 | 7691 | 15 499 | 7807 | 7691 |
Data source is the pooled National Health Interview Survey 2011–2015. Dependent variables are CHD, angina pectoris and heart attack, respectively. Coefficients are OR, with se given in the following row. All estimates account for complex survey design. Each regression also adjusts for age, age-squared, marital status, education level, size of family, number of children in the household, elderly person indicator, employment status, log household income, and year and region fixed effects. Reference categories (Ref.) are: in the USA for 0–4 years, White non-Hispanic, single/never married, more than a high-school education, 2011 and Northwest. Analysis sample includes households at or below 300 % of the federal poverty line.
Significant at the 10 % level.
Significant at the 5 % level.
Significant at the 1 % level.
Female coefficient statistically different from the male coefficient.
Table 4.
Results from multivariate logistic regressions of household food insecurity and acculturation v. self-rated poor health and obesity among low-income, working-age immigrant adults in the USA
| Variable | Self-rated poor health | Obesity | ||||||
|---|---|---|---|---|---|---|---|---|
| Full sample | Full sample – interaction model | Female | Male | Full sample | Full sample – interaction model | Female | Male | |
| Food insecurity | 2·801*** | 4·651*** | 2·931*** | 2·704*** | 1·260*** | 1·785*** | 1·336***,† | 1·204** |
| se | 0·180 | 1·127 | 0·249 | 0·252 | 0·065 | 0·346 | 0·096 | 0·088 |
| Years in the USA (Ref.: 0–4) | ||||||||
| 5–9 years | 1·253* | 1·387* | 1·038 | 1·517* | 1·117 | 1·226* | 1·041 | 1·188 |
| se | 0·164 | 0·255 | 0·183 | 0·359 | 0·115 | 0·137 | 0·144 | 0·182 |
| 10–14 years | 1·497*** | 1·867*** | 1·219 | 1·818*** | 1·422*** | 1·600*** | 1·166† | 1·706*** |
| se | 0·212 | 0·358 | 0·229 | 0·419 | 0·132 | 0·160 | 0·146 | 0·241 |
| 15 years or more | 1·761*** | 2·130*** | 1·363*,† | 2·320*** | 1·478*** | 1·591*** | 1·453*** | 1·475*** |
| se | 0·234 | 0·376 | 0·231 | 0·554 | 0·137 | 0·166 | 0·186 | 0·200 |
| Interaction | ||||||||
| Food insecurity × 5–9 years | – | 0·734 | – | – | – | 0·664* | – | – |
| se | – | 0·228 | – | – | – | 0·151 | – | – |
| Food insecurity × 10–14 years | – | 0·529** | – | – | – | 0·596** | – | – |
| se | – | 0·156 | – | – | – | 0·125 | – | – |
| Food insecurity × 15 years or more | – | 0·575** | – | – | – | 0·722 | – | – |
| se | – | 0·143 | – | – | – | 0·147 | – | – |
| Interaction F statistic | – | 2·11 | – | – | – | 2·31 | – | – |
| Interaction P value | – | 0·099 | – | – | – | 0·077 | – | – |
| Number of observations | 15 499 | 15 499 | 7807 | 7691 | 15 499 | 15 499 | 7807 | 7691 |
Data source is the pooled National Health Interview Survey 2011–2015. Dependent variables are self-rated poor health and obesity, respectively. Coefficients are OR, with se given in the following row. All estimates account for complex survey design. Each regression also adjusts for age, age-squared, marital status, education level, size of family, number of children in the household, elderly person indicator, employment status, log household income, and year and region fixed effects. Reference categories are: in the USA for 0–4 years, White non-Hispanic, single/never married, more than a high-school education, 2011 and Northwest. Analysis sample includes households at or below 300 % of the federal poverty line.
Significant at the 10 % level.
Significant at the 5 % level.
Significant at the 1 % level.
Female coefficient statistically significantly different from male coefficient.
Table 4 shows that food insecurity is associated with a much higher likelihood of reporting poor health for both women and men (OR = 2·931 and 2·704, respectively). Food insecurity is also associated with a higher likelihood of being obese for both women and men (OR = 1·336 and 1·204, respectively) with an OR of 1·260 for the full sample. Length of time in the USA is significantly associated with both self-rated poor health and obesity. Among women, only those in the USA for 15 years or more are significantly more likely to report poor health than those in the USA less than 5 years (OR = 1·363). Among men, respondents in the USA for 5 or more years are more likely to report poor health than those in the USA for less than 5 years, with a higher likelihood of poor health for each increasing time category (OR = 1·517, 1·818 and 2·320 for 5–9 years, 10–14 years and 15 years or more, respectively). For obesity, female immigrants in the USA for 15 years or more are more likely to be obese than those in the USA less than 5 years (OR = 1·453). Male immigrants in the USA for 10 or more years are more likely to be obese than immigrants in the USA for less than 5 years (OR = 1·706 and 1·475 for 10–14 years and 15 years or more, respectively).
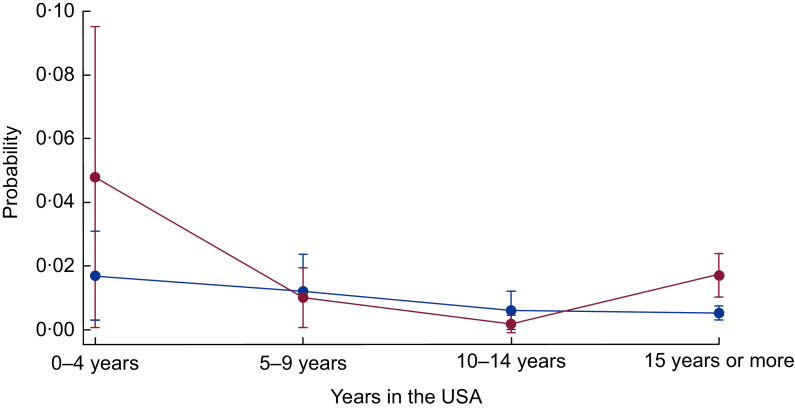
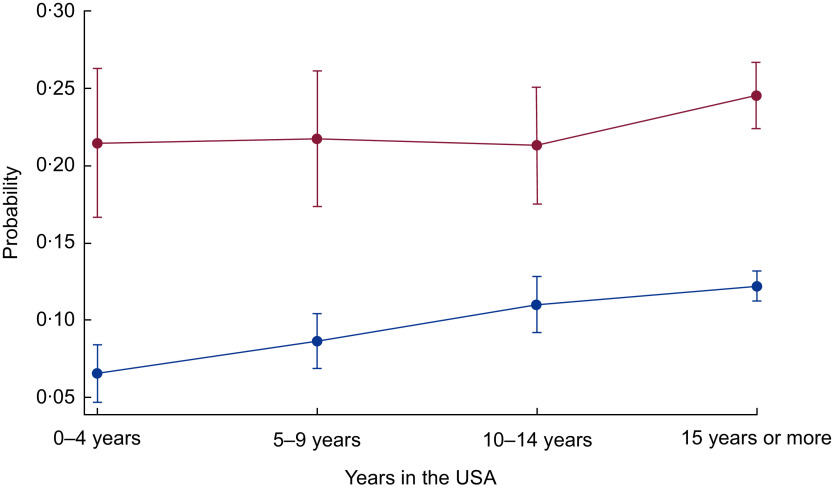
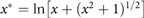
Association of food insecurity with CHD and related outcomes over years in the USA
Next, in the bottom panels of Tables 3 and 4, we present the interactive associations of food insecurity and years in the USA on the health of immigrants. Specifically, since the dependent variable is measured in the odds metric (multiplicative effect), the interaction term is considered to be a ratio of OR. We present the results of the interaction models for those outcomes where food insecurity or acculturation were statistically significant without interaction terms (Tables 3 and 4). Table 3 shows that the interaction of food insecurity and acculturation is statistically significant for angina pectoris among female immigrants (interaction P value = 0·014). When the interaction is included, food insecurity alone is no longer statistically significant, nor are the OR for 5–9 years or 10–14 years in the USA. Those who are food insecure and in the county for 10–14 years are less likely to be diagnosed with angina pectoris (OR = 0·100). As depicted in Fig. 3, for female immigrants in the USA for less than 5 years or more than 15 years, food insecurity is related to a higher probability of angina pectoris, but not for those in the USA for 5–14 years. Table 4 shows the interaction between food insecurity and time in the USA is statistically significant for poor health and obesity for the full sample (interaction P value = 0·099 and 0·077, respectively). The interaction for poor health suggests that being food insecure somewhat reduces the higher likelihood of poor health for those in the USA for more than 10 years (OR = 0·529–0·575). As shown in Fig. 4, the difference in the probability of poor health by food security status is wider for newly arrived immigrants, narrows for those who have lived in the USA for 5–14 years, but is larger again for those in the USA for 15 or more years. Similarly, for obesity, food insecurity has an attenuating effect on the higher likelihood of obesity among those in the USA from 5 to 14 years (OR = 0·596–0·664). Figure 5 shows the gap in the probability of obesity by food security status is greatest for those in the USA less than 5 years, and for those in the USA for 15 years or more. Generally, Figs 3 to 5 show that the difference in probability of poor health, obesity and women’s angina pectoris by food security status narrows from 5 to 14 years, but is widest for those in the USA less than 5 years and those in the USA more than 15 years. Thus, more recent and long-term food-insecure immigrants are more vulnerable to CHD and related health outcomes than those in the USA for 5–14 years.
Fig. 3.
Probability of angina pectoris over years of living in the USA by food security status ( , food secure;
, food secure;  , food insecure) among low-income, working-age immigrant women. Data source is the pooled National Health Interview Survey 2011–2015. Values are probabilities, with their se represented by vertical bars. Estimates account for complex survey design and confidence intervals are estimated at the 95 % level
, food insecure) among low-income, working-age immigrant women. Data source is the pooled National Health Interview Survey 2011–2015. Values are probabilities, with their se represented by vertical bars. Estimates account for complex survey design and confidence intervals are estimated at the 95 % level
Fig. 4.
Probability of self-rated poor health over years of living in the USA by food security status ( , food secure;
, food secure;  , food insecure) among low-income, working-age immigrant adults. Data source is the pooled National Health Interview Survey 2011–2015. Values are probabilities, with their se represented by vertical bars. Estimates account for complex survey design and confidence intervals are estimated at the 95 % level
, food insecure) among low-income, working-age immigrant adults. Data source is the pooled National Health Interview Survey 2011–2015. Values are probabilities, with their se represented by vertical bars. Estimates account for complex survey design and confidence intervals are estimated at the 95 % level
Fig. 5.
Probability of obesity over years of living in the USA by food security status ( , food secure;
, food secure;  , food insecure) among low-income, working-age immigrant adults. Data source is the pooled National Health Interview Survey 2011–2015. Values are probabilities, with their se represented by vertical bars. Estimates account for complex survey design and confidence intervals are estimated at the 95 % level
, food insecure) among low-income, working-age immigrant adults. Data source is the pooled National Health Interview Survey 2011–2015. Values are probabilities, with their se represented by vertical bars. Estimates account for complex survey design and confidence intervals are estimated at the 95 % level
Heterogeneity across the severity of food insecurity
In this section we ask a follow-up question: Does the relationship between household food insecurity and CHD and related health outcomes change with the severity of food insecurity? It is possible that the most severe cases drive the association between food insecurity and poor heart-related health. Table 5 shows the OR using the categorical version of food security status which includes the four groups: high food security, marginal food security, low food security and very low food security. For each logistic model, we compare high food security with the results in each other category.
Table 5.
Results from multivariate logistic regressions of categorical food security status v. CHD and related health outcomes among low-income, working-age immigrant adults in the USA
| CHD | Angina pectoris | Heart attack | Self-rated poor health | Obesity | |
|---|---|---|---|---|---|
| Food security status (Ref.: high food security) | |||||
| Marginal food security | 1·505* | 2·172*** | 0·698†,‡ | 1·878†,‡ | 1·227*** |
| se | 0·342 | 0·467 | 0·206 | 0·151 | 0·080 |
| Low food security | 1·827*** | 2·035*** | 2·213*** | 2·638***,§ | 1·339*** |
| se | 0·337 | 0·434 | 0·550 | 0·199 | 0·086 |
| Very low food security | 1·497* | 2·549*** | 1·795** | 4·786*** | 1·267*** |
| se | 0·330 | 0·649 | 0·490 | 0·452 | 0·100 |
| Years in the USA (Ref.: 0–4) | |||||
| 5–9 years | 0·883 | 0·993 | 1·286 | 1·265* | 1·117 |
| se | 0·354 | 0·380 | 0·551 | 0·166 | 0·115 |
| 10–14 years | 0·904 | 0·610 | 1·286 | 1·509*** | 1·425*** |
| se | 0·380 | 0·247 | 0·579 | 0·216 | 0·133 |
| 15 years or more | 1·130 | 0·710 | 1·787 | 1·776*** | 1·486*** |
| se | 0·402 | 0·228 | 0·723 | 0·236 | 0·138 |
| Number of observations | 15 472 | 7793 | 7679 | 15 472 | 7793 |
Data source is the pooled National Health Interview Survey 2011–2015. Dependent variables are CHD, angina pectoris, heart attack, self-rated poor health and obesity, respectively. Coefficients are OR, with se given in the following row. All estimates account for complex survey design. Each regression also adjusts for age, age-squared, marital status, education level, size of family, number of children in the household, elderly person indicator, employment status, log household income, and year and region fixed effects. Reference categories (Ref.) are: in the USA for 0–4 years, White non-Hispanic, single/never married, more than a high-school education, 2011 and Northwest. Analysis sample includes households at or below 300 % of the federal poverty line.
Significant at the 10 % level.
Significant at the 5 % level.
Significant at the 1 % level.
Marginal food security is statistically significantly different from the low food security category.
Marginal food security is statistically significantly different from the very low food security category.
Low food security is statistically significantly different from the very low food security category.
Overall, the results in Table 5 show that each category of food insecurity is strongly associated with CHD and related health outcomes among the study sample. However, the probability of CHD and related outcomes do not increase as the severity of food insecurity worsens – except for poor health. The highest likelihood of CHD, heart attack and obesity is among those with low food security (OR = 1·339–2·213). Low food security primarily signals a reduction in dietary quality or variety. The highest likelihood of angina pectoris is for those with very low food security. Very low food security means not only a reduction in dietary quality, but also a reduction in dietary quantity. The increasing severity of food insecurity is more linearly related to self-rated poor health: OR = 1·878 for marginal food security, OR = 2·638 for low food security and OR = 4·786 for very low food security.
Table 5 also shows whether the differences between marginal, low and very low food security are statistically significant (†, ‡ and §). The symbol † shows comparison tests between respondents in marginal and low food secure households; the symbol ‡ shows comparison tests between respondents in marginal and very low food secure households; and the symbol § shows comparison tests between respondents in low and very low food secure households. Differences are statistically significant only for the heart attack and poor health models. For the odds of a heart attack, marginal food security is statistically different from low and very low food security. The odds of poor health are statistically different across each of the food security categories.
Robustness and sensitivity analysis
We also check the robustness and sensitivity of the results (see appendices). First, we examine whether BMI mediates the results discussed above and include it as a covariate in the models for all outcomes, except obesity (Appendix 1 and Appendix 2). The coefficient for BMI is statistically significant and positive (OR greater than 1) in models for CHD, heart attack and poor health. However, the results for food insecurity and years in the USA are substantively unchanged from the models that do not include BMI (see Tables 3 and 4). There is no evidence that the relationship between food insecurity and health outcomes, or time in USA and health outcomes, operates through obesity.
Second, since immigrants from the MCC region represent a large majority of the sample (68 %), we test whether the results change if these individuals were dropped from the sample (Appendix 3 and Appendix 4). The biggest effect of dropping the MCC respondents from the sample is that fewer coefficients are significant, most likely due to the loss in sample size and statistical power. In general, the directions of the coefficients and magnitude are the same whether the whole sample is used or only non-MCC immigrants. The only substantive change in results is for the male model for angina pectoris outcome. The coefficient for food insecurity changes direction and is statistically significant in the non-MCC immigrant male model, indicating that food insecurity is associated with a lower likelihood of being diagnosed with angina pectoris for non-MCC immigrant men.
In all robustness and sensitivity checks, we find that generally the relationships between food insecurity, acculturation, and CHD and related outcomes do not change appreciably. The magnitude and direction of the food insecurity and acculturation coefficients remain relatively the same. Thus, the results are robust across chosen variables and samples.
Discussion
Using repeated cross-sectional data from the NHIS from 2011–2015, we address two research questions. First, what is the relationship of household food insecurity and acculturation with diagnosis of CHD and related health outcomes, namely angina pectoris, heart attack, self-rated poor health and obesity? Second, what is the association of food insecurity with these health outcomes over years of living in the USA? Overall, we find that both food insecurity and acculturation are strongly associated with CHD and related health outcomes among working-age immigrant adults (research question 1). This is not surprising since diet sensitivity is a common factor among these conditions and food insecurity increases the difficulty of following a healthy diet, given limitations on money to afford healthy foods and time to cook healthy meals( 22 , 29 , 44 ). This also corresponds to previous research linking length of US residence with negative health outcomes among immigrant adults( 10 , 45 , 46 ) and suggests that dietary acculturation may increase over time in the USA. For example, previous research consistently shows a strong association between acculturation and unhealthy food intake, such as higher saturated fat, sugar and cholesterol( 10 , 47 – 49 ).
We also find significant gender heterogeneity in these relationships, where food insecurity is associated with CHD and related outcomes of female immigrants more than male. One explanation for these findings is that the determinants of heart-related health outcomes are gender specific( 34 , 50 , 51 ). Women may also be more susceptible to negative impacts of food insecurity. For example, Martin and Lippert( 38 ) find that mothers are at greater risk for obesity than child-free women, or men regardless of parenthood status, because mothers often prioritize their children’s access to healthy food over their own.
Lastly, we find a significant interactive association between food insecurity and years in the USA for self-rated health, obesity and women’s angina pectoris. Generally, the significant interactions suggest that food insecurity is associated more strongly with CHD and related outcomes for immigrants in the USA for less than 5 years or those in the USA for 15 years or more, than those in the USA for 5–14 years. This is an important finding and provides further detail on the relationship between food insecurity, acculturation and health than previous literature. For example, Ryan-Ibarra et al.( 51 ) found among Californian immigrant women that food insecurity was associated with a higher prevalence of obesity for those in the USA for 10 years or longer, but was statistically insignificant for those in the USA for less. Using a nationally representative sample and our more granular categorical version of years in the USA provides more information about those in the USA from 5 to 14 years, than using a simple binary measure. It is worth noting that in earlier analyses when we used a dichotomous measure of time in the USA (less than 15 years; 15 years or more) our findings were similar to those of Ryan-Ibarra and colleagues. We found it was important to model time in the USA with more categories because there were important differences over time that were masked otherwise. Future research using a continuous measure of time in the USA may provide even further insights into these relationships.
There are several possible reasons why food insecurity has a greater association with poor health for those in the USA for under 5 years. First, having recently migrated, immigrants would most likely be under more stress than those who immigrated 5 or more years ago; stress from the move and stress from adapting to a new environment( 52 ). For example, linguistic isolation (inability to speak English well) and abrupt changes to nutritional sources have been shown to increase obesity and poor health among immigrants( 53 – 55 ). However, living in immigrant enclaves with Spanish-speaking neighbours and options to acquire traditional foods is associated with healthy dietary patterns among Hispanic immigrants( 53 ). Hence, it may take some time for recent immigrants to find their enclave. Another likely reason why food insecurity plays a bigger role in determining health for immigrants in the USA for less than 5 years is their ineligibility for federal assistance programmes. Legal immigrants must wait 5 years before being eligible for federal programme benefits, unless they have children or are disabled( 56 , 57 ). This means that immigrants in the USA for less than 5 years may be unable to participate in food assistance programmes such as the Supplemental Nutrition Assistance Program (SNAP) and the Special Supplemental Nutrition Program for Women, Infants, and Children.
For immigrants in the USA for 15 years or more, we find consistent evidence with the existing literature, in that acculturation is associated with poorer health outcomes and that food insecurity may be an important pathway through which this occurs( 55 ). While immigration might initially take place with the goal of increasing welfare over time, in fact years of residence in the USA correlate with declining health outcomes among immigrant adults from various backgrounds and countries of origin( 58 – 60 ). For example, Koya and Egede( 61 ) found that acculturation predicts increased rates of tobacco use, hyperlipidaemia and obesity. Similarly, Oza-Frank and Narayan( 60 ) found that length of time in the USA correlates with higher diabetes prevalence, independent of age and obesity. Adoption of health-related behaviours, such as unhealthy diets and sedentary lifestyles of the dominant culture, can strongly affect immigrant health over time( 6 , 45 , 62 – 65 ). Immigrants’ dietary acculturation in the USA typically involves increases in consumption of energy-dense, processed foods and animal products, and decreases in consumption of fruits, vegetables and whole grains( 46 , 66 , 67 ). Research on the level of dietary acculturation also shows a link between increased acculturation and chronic disease risk factors( 47 , 48 , 66 – 70 ).
It is possible that immigrants in the USA for 5–14 years have relatively less stress and have figured out how to navigate US systems and found friends and neighbours they can rely on in times of need but have not fully acculturated to poorer diets. Further research is needed using different data and alternative health measures to understand more fully how years in the USA interact with food insecurity.
Limitations
The results of the present study should be interpreted in the context of several limitations. First, measures of CHD and related health outcomes in the NHIS are self-reported and subject to reporting bias. However, the survey is nationally representative, has been extensively validated and is the key data source for information on the nation’s health. Second, the pooled cross-sectional nature of the data limits the analyses. Cross-sectional data do not allow for the examination of longitudinal change of health over time and may conflate cohort effects with the effects of time in the USA. Longitudinal data would allow the analysis to address the effects of acculturation more directly, by taking into account the life experiences of immigrants before migration and by controlling for socio-economic, demographic and cultural confounders; similar limitations have characterized other acculturation-related research( 48 , 69 ). For example, since we are limited by the categories of years of US residence (0–4 years, 5–9 years, 10–14 years, 15 years or more), we must treat each category as if health characteristics remain constant within. However, some immigrants may arrive with greater exposure to American lifestyle behaviours than others and selection processes differ in important ways( 71 – 75 ). Third, due to data limitations we are unable to examine the direct mechanisms of the impact of food insecurity on immigrant health. It is unclear whether food insecurity is related to CHD and related health outcomes due to dietary impacts, stress or other factors. Also noteworthy is that the food security module in the NHIS has only a 30 d recall period. Longitudinal data with multiple observations of food insecurity and health may show a more complex relationship among health, food insecurity and time in the USA. However, the short recall period for food insecurity offers advantages in terms of reliability and still reveals strong associations with contemporaneous food insecurity and dynamic health outcomes.
Policy implications
The present study is relevant to contemporary questions about how public health policy might affect health outcomes in the USA. First, the associations between food insecurity and CHD and related health outcomes suggest reducing food insecurity may save health-care costs. Second, the results are relevant to a recent call for clinical screenings of food insecurity( 76 ). Knowing the food security status of immigrant patients who are suffering from or predisposed to CHD and related outcomes may be important to helping them manage these conditions( 22 ). Third, recent research has shown that SNAP participation significantly reduces the likelihood of reporting poor health in low-income households( 77 , 78 ). SNAP is one vehicle to reducing food insecurity, but there are rules that prevent some immigrants from receiving SNAP( 79 ). Future research could examine the possible effects of SNAP on the heart-related health of immigrants over years of US residence. Understanding the relationships between food insecurity, acculturation, and CHD and related health outcomes among immigrants can inform the development of public health and nutrition assistance programmes for the entire US population.
Acknowledgements
Acknowledgements: The authors wish to thank Maria S. Floro, Christian Gregory, Michele Ver Ploeg, Natalia Radchenko, Alison Jacknowitz and Walter Park for their insightful comments and helpful feedback. The findings and conclusions in this publication are those of the authors and should not be construed to represent any official US Department of Agriculture or US Government determination or policy. Financial support: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. Conflict of interest: M.D.S. and A.C.-J. have no conflicts of interest. Authorship: M.D.S. designed the study with input from A.C.-J. M.D.S. conducted the data analysis and developed the first draft of the manuscript. A.C.-J. critically reviewed and revised the manuscript. Final revisions were made by M.D.S. Both authors read and approved the final version of the paper. Ethics of human subject participation: Not applicable.
Appendix 1. Robustness and sensitivity analysis: results from multivariate logistic regressions, controlling for BMI, of household food insecurity and acculturation v. CHD, angina pectoris and heart attack among low-income, working-age immigrant adults in the USA
| Variable | CHD | Angina pectoris | Heart attack | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Full sample | Female | Male | Full sample | Female | Male | Full sample | Female | Male | |
| Food insecurity | 1·558*** | 1·841*** | 1·354 | 1·809*** | 2·485*** | 1·195 | 2·193*** | 3·837*** | 1·453 |
| se | 0·225 | 0·394 | 0·314 | 0·298 | 0·634 | 0·285 | 0·442 | 1·216 | 0·370 |
| Years in the USA (Ref.: 0–4) | |||||||||
| 5–9 years | 0·874 | 1·013 | 0·657 | 0·985 | 0·430* | 2·441 | 1·280 | 1·636 | 0·413 |
| se | 0·353 | 0·578 | 0·409 | 0·377 | 0·201 | 1·494 | 0·549 | 1·283 | 0·361 |
| 10–14 years | 0·903 | 1·085 | 0·675 | 0·608 | 0·200*** | 2·103 | 1·305 | 1·030 | 1·229 |
| se | 0·382 | 0·558 | 0·404 | 0·246 | 0·110 | 1·262 | 0·587 | 0·902 | 0·870 |
| 15 years or more | 1·134 | 1·095 | 1·047 | 0·708 | 0·324*** | 1·782 | 1·821 | 1·225 | 1·970 |
| se | 0·406 | 0·613 | 0·514 | 0·230 | 0·120 | 0·967 | 0·743 | 1·040 | 1·189 |
| BMI | 1·007** | 1·005 | 1·011* | 1·004 | 1·004 | 1·004 | 1·012* | 1·016** | 1·000 |
| se | 0·003 | 0·004 | 0·006 | 0·003 | 0·005 | 0·006 | 0·007 | 0·008 | 0·006 |
| Number of observations | 15 499 | 7807 | 7691 | 15 499 | 7807 | 7691 | 15 499 | 7807 | 7691 |
Data source is the pooled National Health Interview Survey 2011–2015. Dependent variables are CHD, angina pectoris and heart attack, respectively. Coefficients are OR, with se given in the following row. All estimates account for complex survey design. Each regression also adjusts for age, age-squared, marital status, education level, size of family, number of children in the household, elderly person indicator, employment status, log household income, and year and region fixed effects. Reference categories (Ref.) are: in the USA for 0–4 years, White non-Hispanic, single/never married, more than a high-school education, 2011 and Northwest. Analysis sample includes households at or below 300 % of the federal poverty line.
Significant at the 10 % level.
Significant at the 5 % level.
Significant at the 1 % level.
Appendix 2. Robustness and sensitivity analysis: OR from multivariate logistic regressions, controlling for BMI, of household food insecurity and acculturation v. self-rated poor health among low-income, working-age immigrant adults in the USA
| Variable | Self-rated poor health | ||
|---|---|---|---|
| Full sample | Female | Male | |
| Food insecurity | 2·800*** | 2·914*** | 2·727*** |
| se | 0·182 | 0·252 | 0·256 |
| Years in the USA (Ref.: 0–4) | |||
| 5–9 years | 1·251* | 1·046 | 1·495* |
| se | 0·166 | 0·189 | 0·353 |
| 10–14 years | 1·499*** | 1·224 | 1·824** |
| se | 0·214 | 0·232 | 0·424 |
| 15 years or more | 1·778*** | 1·380* | 2·346*** |
| se | 0·239 | 0·239 | 0·570 |
| BMI | 1·010*** | 1·009*** | 1·011*** |
| se | 0·002 | 0·002 | 0·003 |
| Number of observations | 15 499 | 7807 | 7691 |
Data source is the pooled National Health Interview Survey 2011–2015. Dependent variable is self-rated poor health. Coefficients are OR, with se given in the following row. All estimates account for complex survey design. Each regression also adjusts for age, age-squared, marital status, education level, size of family, number of children in the household, elderly person indicator, employment status, log household income, and year and region fixed effects. Reference categories (Ref.) are: in the USA for 0–4 years, White non-Hispanic, single/never married, more than a high-school education, 2011 and Northwest. Analysis sample includes households at or below 300 % of the federal poverty line.
Significant at the 10 % level.
Significant at the 5 % level.
Significant at the 1 % level.
Appendix 3. Robustness and sensitivity analysis: results from multivariate logistic regressions, dropping Mexican immigrants from the sample, of household food insecurity and acculturation v. CHD, angina pectoris and heart attack among low-income, working-age immigrant adults in the USA
| Variable | CHD | Angina pectoris | Heart attack | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Full sample | Female | Male | Full sample | Female | Male | Full sample | Female | Male | |
| Food insecurity | 1·476 | 1·784 | 1·404 | 1·102 | 3·071** | 0·314** | 2·101** | 5·985*** | 1·020 |
| se | 0·434 | 0·751 | 0·585 | 0·411 | 1·692 | 0·167 | 0·759 | 3·404 | 0·518) |
| Years in the USA (Ref.: 0–4) | |||||||||
| 5–9 years | 1·218 | 1·105 | 0·896 | 0·630 | 0·175* | 1·090 | 0·882 | 0·636 | 0·123 |
| se | 0·807 | 1·361 | 0·856 | 0·455 | 0·159 | 1·133 | 0·736 | 0·792 | 0·162 |
| 10–14 years | 1·186 | 1·134 | 1·013 | 0·781 | 0·206 | 1·314 | 1·392 | 0·886 | 0·537 |
| se | 0·914 | 1·552 | 0·781 | 0·548 | 0·225 | 1·155 | 1·057 | 1·199 | 0·642 |
| 15 years or more | 2·619 | 3·599 | 1·598 | 0·607 | 0·358 | 0·537 | 2·769* | 0·745 | 2·462 |
| se | 1·627 | 4·510 | 1·162 | 0·408 | 0·325 | 0·443 | 1·675 | 0·930 | 2·256 |
| Number of observations | 5844 | 2868 | 2681 | 5844 | 2868 | 2681 | 5844 | 2868 | 2681 |
Data source is the pooled National Health Interview Survey 2011–2015. Dependent variables are CHD, angina pectoris and heart attack, respectively. Coefficients are OR, with se given in the following row. All estimates account for complex survey design. Each regression also adjusts for age, age-squared, marital status, education level, size of family, number of children in the household, elderly person indicator, employment status, log household income, and year and region fixed effects. Reference categories (Ref.) are: in the USA for 0–4 years, White non-Hispanic, single/never married, more than a high-school education, 2011 and Northwest. Analysis sample includes households at or below 300 % of the federal poverty line and excludes individuals born in Mexico.
Significant at the 10 % level.
Significant at the 5 % level.
Significant at the 1 % level.
Appendix 4. Robustness and sensitivity analysis: results from multivariate logistic regressions, dropping Mexican immigrants from the sample, of household food insecurity and acculturation v. self-rated poor health and obesity among low-income, working-age immigrant adults in the USA
| Variable | Self-rated poor health | Obesity | ||||
|---|---|---|---|---|---|---|
| Full sample | Female | Male | Full sample | Female | Male | |
| Food insecurity | 3·728*** | 4·320*** | 3·236*** | 1·442*** | 1·603*** | 1·301 |
| se | 0·499 | 0·763 | 0·633 | 0·154 | 0·220 | 0·226 |
| Years in the USA (Ref.: 0–4) | ||||||
| 5–9 years | 1·223 | 0·879 | 1·855 | 1·083 | 1·019 | 1·175 |
| se | 0·297 | 0·257 | 0·820 | 0·181 | 0·240 | 0·292 |
| 10–14 years | 2·357*** | 1·746* | 3·308*** | 1·403** | 1·161 | 1·712** |
| se | 0·593 | 0·542 | 1·334 | 0·225 | 0·265 | 0·408 |
| 15 years or more | 3·169*** | 2·191*** | 5·018*** | 1·736*** | 1·514* | 2·075*** |
| se | 0·707 | 0·644 | 1·817 | 0·279 | 0·358 | 0·478 |
| Number of observations | 5844 | 2868 | 2681 | 5844 | 2868 | 2681 |
Data source is the pooled National Health Interview Survey 2011–2015. Dependent variables are self-rated health and obesity, respectively. Coefficients are OR, with se given in the following row. All estimates account for complex survey design. Each regression also adjusts for age, age-squared, marital status, education level, size of family, number of children in the household, elderly person indicator, employment status, log household income, and year and region fixed effects. Reference categories (Ref.) are: in the USA for 0–4 years, White non-Hispanic, single/never married, more than a high-school education, 2011 and Northwest. Analysis sample includes households at or below 300 % of the federal poverty line and excludes individuals born in Mexico.
Significant at the 10 % level.
Significant at the 5 % level.
Significant at the 1 % level.
Footnotes
See Antecol and Bedard( 2 ) for an excellent review.
Acculturation is formally defined as the process of cultural and psychological adjustment that occurs because of contact between two or more cultures( 3 , 4 ). Researchers (e.g. Commodore-Mensah et al.( 5 )) have often used length of residence in the USA as a proxy for acculturation, as we do here.
We chose a polynomial age specification after also testing linear and spline specifications.
Household income x* was transformed using the inverse hyperbolic sine transformation,
We also estimated binary choice with endogenous treatment models but found similar results. Additionally, these two-stage models showed that the correlation coefficient (ρ) of the errors between the two equations was consistently statistically insignificant. This validates the use of a single-equation non-linear probability model since it is more statistically efficient (i.e. it involves only one set of se). As a robustness check, we followed this analysis with a non-parametric bounds approach( 40 – 43 ). The non-parametric bounds estimates provided empirical support for the robustness of the logistic regressions – providing similar results – and for the validity of self-reported food security status. Results are available from the authors upon request.
After testing the estimated coefficients, we found evidence that the covariates varied significantly by gender, justifying the gender-separated models.
References
- 1. Trevelyan E, Gambino C, Gryn T et al. (2016) Characteristics of the US Population by Generational Status: 2013. Washington, DC: US Census Bureau. [Google Scholar]
- 2. Antecol H & Bedard K (2015) Immigrants and immigrant health. In Handbook of the Economics of International Migration. vol. 1A: The Immigrants, pp. 271–314 [Chiswick BR and Miller PW, editors]. Amsterdam: Elsevier. [Google Scholar]
- 3. Berry JW, Phinney JS, Sam DL et al. (2006) Immigrant youth: acculturation, identity, and adaptation. Appl Psychol 55, 303–332. [Google Scholar]
- 4. Sam DL & Berry JW (2010) Acculturation: when individuals and groups of different cultural backgrounds meet. Perspect Psychol Sci 5, 472–481. [DOI] [PubMed] [Google Scholar]
- 5. Commodore-Mensah Y, Ukonu N, Obisesan O et al. (2016) Length of residence in the United States is associated with a higher prevalence of cardiometabolic risk factors in immigrants: a contemporary analysis of the National Health Interview Survey. J Am Heart Assoc 5, e004059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kaushal N (2009) Adversities of acculturation? Prevalence of obesity among immigrants. Health Econ 18, 291–303. [DOI] [PubMed] [Google Scholar]
- 7. Coleman-Jensen A, Rabbitt M, Gregory C et al. (2017) Household Food Security in the United States in 2016. Washington, DC: US Department of Agriculture, Economic Research Service. [Google Scholar]
- 8. Borjas GJ (2004) Food insecurity and public assistance. J Public Econ 88, 1421–1443. [Google Scholar]
- 9. Chilton M, Black MM, Berkowitz C et al. (2009) Food insecurity and risk of poor health among US-born children of immigrants. Am J Public Health 99, 556–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Okafor M-TC, Carter-Pokras OD & Zhan M (2014) Greater dietary acculturation (dietary change) is associated with poorer current self-rated health among African immigrant adults. J Nutr Educ Behav 46, 226–235. [DOI] [PubMed] [Google Scholar]
- 11. Quandt SA, Shoaf JI, Tapia J et al. (2006) Experiences of Latino immigrant families in North Carolina help explain elevated levels of food insecurity and hunger. J Nutr 136, 2638–2644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rabbitt MP, Smith MD & Coleman-Jensen A (2016) Food Security Among Hispanic Adults in the United States, 2011–2014. Washington, DC: US Department of Agriculture, Economic Research Service. [Google Scholar]
- 13. Sano Y, Garasky S, Greder KA et al. (2011) Understanding food insecurity among Latino immigrant families in rural America. J Family Econ Issues 32, 111–123. [Google Scholar]
- 14. Bitler M & Hoynes HW (2011) Immigrants, Welfare Reform, and the US Safety Net. Cambridge, MA: National Bureau of Economic Research. [Google Scholar]
- 15. Fix ME, Capps R & Kaushal N (2009) Immigrants and welfare: overview. In Immigrants and Welfare: The Impact of Welfare Reform on America’s Newcomers, pp. 1–36 [Fix ME, editor]. New York: Russell Sage Foundation. [Google Scholar]
- 16. Skinner C (2012) State immigration legislation and SNAP take-up among immigrant families with children. J Econ Issues 46, 661–682. [Google Scholar]
- 17. Gundersen C & Ziliak JP (2015) Food insecurity and health outcomes. Health Aff (Millwood) 34, 1830–1839. [DOI] [PubMed] [Google Scholar]
- 18. Hadley C, Lindstrom D, Tessema F et al. (2008) Gender bias in the food insecurity experience of Ethiopian adolescents. Soc Sci Med 66, 427–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Seligman HK & Schillinger D (2010) Hunger and socioeconomic disparities in chronic disease. N Engl J Med 363, 6–9. [DOI] [PubMed] [Google Scholar]
- 20. Gregory CA & Coleman-Jensen A (2017) Food Insecurity, Chronic Disease, and Health Among Working-Age Adults. Economic Research Report no. ERR-235. Washington, DC: US Department of Agriculture, Economic Research Service. [Google Scholar]
- 21. Seligman HK, Laraia BA & Kushel MB (2010) Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr 140, 304–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Berkowitz SA, Berkowitz TSZ, Meigs JB et al. (2017) Trends in food insecurity for adults with cardiometabolic disease in the United States: 2005–2012. PLoS One 12, e0179172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ford ES (2013) Food security and cardiovascular disease risk among adults in the United States: findings from the National Health and Nutrition Examination Survey, 2003–2008. Prev Chronic Dis 10, E202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gundersen C & Ziliak J (2014) Food insecurity and health outcomes among multigenerational households (805.11). FASEB J 28, 805–811. [Google Scholar]
- 25. Mahmoodi MR, Najafipour H, Mohsenpour MA et al. (2017) The relationship between food insecurity with cardiovascular risk markers and metabolic syndrome components in patients with diabetes: a population-based study from Kerman coronary artery disease risk study. J Res Med Sci 22, 118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Morales ME & Berkowitz SA (2016) The relationship between food insecurity, dietary patterns, and obesity. Curr Nutr Rep 5, 54–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Saiz AM, Aul AM, Malecki KM et al. (2016) Food insecurity and cardiovascular health: findings from a statewide population health survey in Wisconsin. Prev Med 93, 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Seligman HK, Bindman AB, Vittinghoff E et al. (2007) Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999–2002. J Gen Intern Med 22, 1018–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Seligman HK, Jacobs EA, López A et al. (2012) Food insecurity and glycemic control among low-income patients with type 2 diabetes. Diabetes Care 35, 233–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Berkowitz SA, Gao X & Tucker KL (2014) Food-insecure dietary patterns are associated with poor longitudinal glycemic control in diabetes: results from the Boston Puerto Rican Health study. Diabetes Care 37, 2587–2592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Coleman-Jensen A, McFall W & Nord M (2013) Food Insecurity in Households with Children: Prevalence, Severity, and Household Characteristics, 2010–11. Washington, DC: US Department of Agriculture, Economic Research Service. [Google Scholar]
- 32. Mozaffarian D (2016) Dietary and policy priorities for cardiovascular disease, diabetes, and obesity: a comprehensive review. Circulation 133, 187–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bickel G, Nord M, Price C et al. (2000) Guide to Measuring Household Food Security: Revised 2000. Alexandria, VA: US Department of Agriculture, Food and Nutrition Service. [Google Scholar]
- 34. Hanson KL, Sobal J & Frongillo EA (2007) Gender and marital status clarify associations between food insecurity and body weight. J Nutr 137, 1460–1465. [DOI] [PubMed] [Google Scholar]
- 35. DeVault ML (1994) Feeding the Family: The Social Organization of Caring as Gendered Work. Chicago, IL: University of Chicago Press. [Google Scholar]
- 36. Kirk MC & Gillespie AH (1990) Factors affecting food choices of working mothers with young families. J Nutr Educ 22, 161–168. [Google Scholar]
- 37. Martin KS & Ferris AM (2007) Food insecurity and gender are risk factors for obesity. J Nutr Educ Behav 39, 31–36. [DOI] [PubMed] [Google Scholar]
- 38. Martin MA & Lippert AM (2012) Feeding her children, but risking her health: the intersection of gender, household food insecurity and obesity. Soc Sci Med 74, 1754–1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Olson CM (2005) Food insecurity in women: a recipe for unhealthy trade-offs. Top Clin Nutr 20, 321–328. [Google Scholar]
- 40. Gundersen C, Kreider B & Pepper J (2012) The impact of the National School Lunch Program on child health: a nonparametric bounds analysis. J Econ 166, 79–91. [Google Scholar]
- 41. Millimet DL & Roy M (2015) Partial identification of the long-run causal effect of food security on child health. Empir Econ 48, 83–141. [Google Scholar]
- 42. Almada L, McCarthy I & Tchernis R (2016) What can we learn about the effects of food stamps on obesity in the presence of misreporting? Am J Agric Econ 98, 997–1017. [Google Scholar]
- 43. Smith MD (2018) Essays on food security, health, and immigration. Doctoral Dissertation, American University.
- 44. Berkowitz SA, Baggett TP, Wexler DJ et al. (2013) Food insecurity and metabolic control among US adults with diabetes. Diabetes Care 36, 3093–3099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Akresh IR (2007) Dietary assimilation and health among Hispanic immigrants to the United States. J Health Soc Behav 48, 404–417. [DOI] [PubMed] [Google Scholar]
- 46. Satia JA (2010) Dietary acculturation and the nutrition transition: an overview. Appl Physiol Nutr Metab 35, 219–223. [DOI] [PubMed] [Google Scholar]
- 47. Himmelgreen DA, Bretnall A, Perez-Escamilla R et al. (2005) Birthplace, length of time in the US, and language are associated with diet among inner-city Puerto Rican women. Ecol Food Nutr 44, 105–122. [Google Scholar]
- 48. Pérez-Escamilla R & Putnik P (2007) The role of acculturation in nutrition, lifestyle, and incidence of type 2 diabetes among Latinos. J Nutr 137, 860–870. [DOI] [PubMed] [Google Scholar]
- 49. Batis C, Hernandez-Barrera L, Barquera S et al. (2011) Food acculturation drives dietary differences among Mexicans, Mexican Americans, and non-Hispanic Whites – 3. J Nutr 141, 1898–1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Sanchez-Vaznaugh EV, Kawachi I, Subramanian S et al. (2008) Differential effect of birthplace and length of residence on body mass index (BMI) by education, gender and race/ethnicity. Soc Sci Med 67, 1300–1310. [DOI] [PubMed] [Google Scholar]
- 51. Ryan-Ibarra S, Sanchez-Vaznaugh EV, Leung C et al. (2017) The relationship between food insecurity and overweight/obesity differs by birthplace and length of US residence. Public Health Nutr 20, 671–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Goldman N, Pebley AR, Creighton MJ et al. (2014) The consequences of migration to the United States for short-term changes in the health of Mexican immigrants. Demography 51, 1159–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Park Y, Neckerman K, Quinn J et al. (2011) Neighbourhood immigrant acculturation and diet among Hispanic female residents of New York City. Public Health Nutr 14, 1593–1600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Park Y, Neckerman K, Quinn J et al. (2008) Significance of place of birth and place of residence and their relationship to BMI among immigrant groups in New York City. Int J Behav Nutr Phys Act 5, 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Kaplan MS, Huguet N, Newsom JT et al. (2004) The association between length of residence and obesity among Hispanic immigrants. Am J Prev Med 27, 323–326. [DOI] [PubMed] [Google Scholar]
- 56. Philbin MM, Flake M, Hatzenbuehler ML et al. (2018) State-level immigration and immigrant-focused policies as drivers of Latino health disparities in the United States. Soc Sci Med 199, 29–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Hoynes HW & Schanzenbach DW (2015) US Food and Nutrition Programs. Cambridge, MA: National Bureau of Economic Research. [Google Scholar]
- 58. Delavari M, Sønderlund AL, Swinburn B et al. (2013) Acculturation and obesity among migrant populations in high income countries – a systematic review. BMC Public Health 13, 458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Kaestner R, Pearson JA, Keene D et al. (2009) Stress, allostatic load, and health of Mexican immigrants. Soc Sci Q 90, 1089–1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Oza-Frank R & Narayan KV (2010) Overweight and diabetes prevalence among US immigrants. Am J Public Health 100, 661–668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Koya DL & Egede LE (2007) Association between length of residence and cardiovascular disease risk factors among an ethnically diverse group of United States immigrants. J Gen Intern Med 22, 841–846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Acevedo-Garcia D, Bates LM, Osypuk TL et al. (2010) The effect of immigrant generation and duration on self-rated health among US adults 2003–2007. Soc Sci Med 71, 1161–1172. [DOI] [PubMed] [Google Scholar]
- 63. Kimbro RT, Gorman BK & Schachter A (2012) Acculturation and self-rated health among Latino and Asian immigrants to the United States. Soc Prob 59, 341–363. [Google Scholar]
- 64. Lee S, O’Neill AH, Ihara ES et al. (2013) Change in self-reported health status among immigrants in the United States: associations with measures of acculturation. PLoS One 8, e76494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Uretsky MC & Mathiesen SG (2007) The effects of years lived in the United States on the general health status of California’s foreign-born populations. J Immigr Minor Health 9, 125–136. [DOI] [PubMed] [Google Scholar]
- 66. Ayala GX, Baquero B & Klinger S (2008) A systematic review of the relationship between acculturation and diet among Latinos in the United States: implications for future research. J Am Diet Assoc 108, 1330–1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Gilbert PA & Khokhar S (2008) Changing dietary habits of ethnic groups in Europe and implications for health. Nutr Rev 66, 203–215. [DOI] [PubMed] [Google Scholar]
- 68. Mazur RE, Marquis GS & Jensen HH (2003) Diet and food insufficiency among Hispanic youths: acculturation and socioeconomic factors in the third National Health and Nutrition Examination Survey. Am J Clin Nutr 78, 1120–1127. [DOI] [PubMed] [Google Scholar]
- 69. Pérez-Escamilla R (2010) Dietary quality among Latinos: is acculturation making us sick? J Am Diet Assoc 110, 5 Suppl., S36–S39. [DOI] [PubMed] [Google Scholar]
- 70. Steffen PR, Smith TB, Larson M et al. (2006) Acculturation to Western society as a risk factor for high blood pressure: a meta-analytic review. Psychosom Med 68, 386–397. [DOI] [PubMed] [Google Scholar]
- 71. Akresh IR & Frank R (2008) Health selection among new immigrants. Am J Public Health 98, 2058–2064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Borjas GJ (1991) Immigration and self-selection. In Immigration, Trade, and the Labor Market, pp. 29–76 [Abowd JM and Freeman RB, editors]. Chicago, IL: University of Chicago Press. [Google Scholar]
- 73. Hamilton TG & Hummer RA (2011) Immigration and the health of US black adults: does country of origin matter? Soc Sci Med 73, 1551–1560. [DOI] [PubMed] [Google Scholar]
- 74. Jasso G, Massey DS, Rosenzweig MR et al. (2005) The US New Immigrant Survey: overview and preliminary results based on the New-Immigrant Cohorts of 1996 and 2003. In Immigration Research and Statistics Service Workshop on Longitudinal Surveys and Cross-Cultural Survey Design: Workshop Proceedings, pp. 29–46 [Morgan B and Nicholson B, editors]. London: Crown Publishing. [Google Scholar]
- 75. McDonald JT & Kennedy S (2004) Insights into the ‘healthy immigrant effect’: health status and health service use of immigrants to Canada. Soc Sci Med 59, 1613–1627. [DOI] [PubMed] [Google Scholar]
- 76. Gundersen C & Seligman HK (2017) Food insecurity and health outcomes. Economists’ Voice 14, issue 1, 20170004. [Google Scholar]
- 77. Almond D, Hoynes HW & Schanzenbach DW (2011) Inside the war on poverty: the impact of food stamps on birth outcomes. Rev Econ Stat 93, 387–403. [Google Scholar]
- 78. Gregory CA & Deb P (2015) Does SNAP improve your health? Food Policy 50, 11–19. [Google Scholar]
- 79. Kaiser L (2008) Why do low-income women not use food stamps? Findings from the California Women’s Health Survey. Public Health Nutr 11, 1288–1295. [DOI] [PubMed] [Google Scholar]