Abstract
Objective:
Food security has been suggested to be a risk factor for depression, stress and anxiety. We therefore undertook a systematic review and meta-analysis of available publications to examine these associations further.
Design:
Relevant studies were identified by searching Web of Science, Embase, Scopus and PubMed databases up to January 2019.
Setting:
OR was pooled using a random-effects model. Standard methods were used for assessment of heterogeneity and publication bias.
Participants:
Data were available from nineteen studies with 372 143 individual participants from ten different countries that were pooled for the meta-analysis.
Results:
The results showed there was a positive relationship between food insecurity (FI) and risk of depression (OR = 1·40; 95 % CI: 1·30, 1·58) and stress (OR = 1·34; 95 % CI: 1·24, 1·44) but not anxiety. Subgroup analysis by age showed that subjects older than ≥65 years exhibited a higher risk of depression (OR = 1·75; 95 % CI: 1·20, 2·56) than younger participants (OR = 1·34; 95 % CI: 1·20, 1·50), as well as a greater risk of depression in men (OR = 1·42; 95 % CI: 1·17, 1·72) than women (OR = 1·30; 95 % CI: 1·16, 1·46). Finally, subgroup analysis according to geographical location illustrated that food insecure households living in North America had the highest risk of stress and anxiety.
Conclusions:
The evidence from this meta-analysis suggests that FI has a significant effect on the likelihood of being stressed or depressed. This indicates that health care services, which alleviate FI, would also promote holistic well-being in adults.
Keywords: Food insecurity, Depression, Stress, Anxiety, Meta-analysis, Anaemia risk, Systematic review
Food security is defined as the assured ability to acquire nutritionally adequate and safe food that meets cultural needs and acquired in a socially acceptable way(1). Conversely, food insecurity (FI) occurs as a consequence of limited resources and affects many households worldwide, thereby causing malnutrition(2). Despite considerable progress over the past 25 years in increasing global food production, nearly 795 million people worldwide remain food insecure(3). In addition, individuals experiencing FI have increased risks of weight abnormalities(4), anaemia(5), showing adverse development(6), diabetes(7), hypertension(8), asthma(9) and cancer(10).
FI not only influences nutrition and physical health but may also affect mental health. Consequently, individuals experiencing FI also demonstrate psychological distress including anxiety and depression due to lack of affordable, culturally appropriate food together with an inability to feed both themselves and their families(11). FI generates uncertainty over the ability to maintain and acquire sufficient food, thereby provoking a stress response that contributes to anxiety and depression(12). Furthermore, acquiring foods in socially unacceptable ways can induce feelings of alienation, powerlessness, shame and guilt that are associated with depression(13,14). It also magnifies socioeconomic disparities within households and communities that could increase cultural sensitivities and further adversely influence mental health(15).
A global analysis of FI found that it was associated with poorer mental health and specific psychosocial stressors across different regions(3), which persist after adjusting for confounding demographic and socioeconomic variables(11). The numerous pathways by which FI may contribute to common mental disorders and the broader social implications of FI linked to cultural norms and self-efficacy may contribute to the cross-cultural consistency of results from previous studies(13,14).
Depression, stress and anxiety are major components of the worldwide burden of disease and play a role in public concern regarding socioeconomic disparities and impacts on the economic burden to society(16). Depressive disorders are characterised by sadness, loss of interest or pleasure, feelings of guilt or low self-worth, disturbed sleep and/or appetite, feelings of tiredness and poor concentration. Anxiety-related disorders therefore refer to a group of mental disorders characterised by feelings of anxiety and fear(17) and stress as ‘a particular relationship between the person and the environment that is appraised by the person as taxing or exceeding his or her resources and endangering his or her well-being’(18). According to WHO statistics, the total number of people living with depression in the world is ~322 million, and the estimated total number of people living with anxiety disorders is currently ~264 million(19).
To date, observational studies have shown inconsistent effects of FI on depression, stress and anxiety and might not be sufficient to provide concise conclusions. Therefore, a systematic review and meta-analysis was performed to examine the associations between FI and the risk of depression, stress and anxiety.
Methods
Literature search and selection
This meta-analysis was performed in accordance with the guidelines of the ‘preferred reporting items for systematic reviews and meta-analyses’(20). A systematic literature search was undertaken using the Web of Science, Embase, Scopus and PubMed databases from inception up to January 2019. Search strategies used defined subject headings and keywords and did not use language and date restrictions. Our systematic search was conducted by using the relevant search terms (see Supplementary Table 1). The references cited in the retrieved review articles were also searched manually.
Eligibility criteria
Studies were included in the final analysis if they met the following criteria: (i) were observational and reported on the association between FI and depression, stress and anxiety risk and (ii) provided multivariable-adjusted OR with corresponding 95 % CI of FI with depression, stress and anxiety risk. Studies were excluded if: (i) the information could not be extracted; (ii) they were case reports, animal studies, editorials, conference papers, reviews or letters; (iii) they did not report FI as exposure and depression, stress or anxiety risk as an outcome; (iv) participants were under 18 years (i.e. children and adolescents) and (v) they were abstracts with inadequate information and/or dissertations.
Study selection
The titles and abstracts of all articles retrieved in the initial search were evaluated independently by three reviewers. In the next step, following further evaluation of the full texts, articles not meeting the eligibility criteria were excluded by using an online form, with a hierarchical approach based on study design, population or exposure and outcome. The reference lists of relevant review articles identified during this process were also examined to include any additional studies. Full-text articles were retrieved if the citation was considered eligible and subjected to a second evaluation for relevance by the same reviewers. Any disagreements were discussed and resolved by consensus.
Data collection
For all selected studies, two reviewers (SM and AB) extracted data separately using a standard data extraction form. They discussed any discrepancies and sought the assessment of a fourth reviewer (AP) for resolution. Extracted information included relevant study characteristics (name of the first author, year, database, geographical area, study, sample size), population characteristics (age range or mean age, male sex, race/ethnicity), exposure (criteria for, method of FI assessment, level of FI measurement, method of mental health assessment, most fully adjusted OR estimate and the adjusted covariates for calculating OR) and the studies main findings.
Quality assessment for individual studies
Two reviewers (SM and AB) assessed the quality of each selected study using the Newcastle-Ottawa scale (adapted for cross-sectional studies)(21). This scale awards a maximum of ten stars to each study as follows: five stars relate to the selection (representativeness of the sample, sample size, non-respondents and ascertainment of the exposure), two stars to comparability (controls for the effect or factors) and three stars to the features of the outcome (assessment of the outcome and statistical test). High-quality studies were defined as those scoring nine or ten stars. Studies with seven or eight stars were categorised as medium quality, while studies with six stars and below were identified as low quality. The quality score for each study is reported in Table 1. Moreover, the level of agreement between reviewers for data collection as well as for quality assessment was computed by the Kappa statistic or coefficient(22).
Table 1.
Description of the studies included in the meta-analysis
| First author | Database/Study design/Country | Subjects: Age(year) Population size Sex |
Race/ethnicity | Level of food insecurity measurement | Measure of food insecurity | Mental health assessment | OR (95 % CI) | Main findings | Adjusted variables | Quality score |
|---|---|---|---|---|---|---|---|---|---|---|
| Kaiser(24) | CWHS/Cross-sectional study/USA | ≥18 n 4037 (100 % female) |
Mixed | Household | FSSM | CWHS forms | Depression risk | Food insecurity increase the depression risk (OR = 1·61; 95 % CI: 1·28, 2·02) | Income as % of federal poverty ratio | +8/10 |
| Johnson(25) | NAFS/Cross-sectional /USA | 78·2 ± 8·4 n 345 |
Mixed | Household | USDA | GDS | Depression risk | Food insecurity increase the depression risk (OR = 4·9; 95 % CI: 2·0, 12·0) | Age, sex, race/ethnicity, education, marital status, living arrangement, income, and receive food stamps | +9/10 |
| Carter(11) | SoFIE/Cross-sectional /New Zealand | ≥18 n 18 955 (8740 male and 10 215 female) |
White | Household | SoFIE forms | K-10 | Stress risk | Food insecurity increase the stress risk (OR = 1·9; 95 % CI: 1·7, 2·1) | Age, sex, ethnicity, marital status, family composition, household income, labour market activity, level of education, NZ (area) deprivation | +9/10 |
| Ramsey(26) | –/Cross-sectional /Australia | ≥20 n 505 (44·5 % male and 55·5 % female) |
Mixed | Household | FSSM | SF-12 | Depression risk | Food insecurity increase the depression risk (OR = 2·89; 95 % CI: 1·29, 4·49) | equivalised household income, indigenous status and household structure | +9/10 |
| Tarasuk(27) | CCHS/Cross-sectional /Canadian | 18–64 n 77 053 |
White | Household | FSSM | CCHS | Anxiety risk | Food insecurity increase the anxiety risk (OR = 1·81; 95 % CI: 1·62, 2·03) | Socio-demographic variables | +9/10 |
| Leung(28) | NHANES/Cross-sectional /USA | 20–65 n 3518 |
Mixed | Household | FSSM | DSM-IV | Depression risk | Food insecurity increase the depression risk (OR = 1·98; 95 % CI: 1·57, 2·42) | Age, sex, race/ethnicity, education, marital status, household size, poverty level, smoking status and BMI categories | +9/10 |
| Bruening(29) | NIH/Cross-sectional /USA | 18·8 ± 0·5 n 209 (38 % male and 62 % female) |
Mixed | Individual | USDA | ACHAS | Depression, stress and anxiety risk | Food insecurity increase the depression risk (OR = 2·97; 95 % CI: 1·58, 5·60), but not stress risk (OR = 1·42; 95 % CI: 0·77, 2·60) and anxiety risk (OR = 1·49; 95 % CI: 0·99, 6·66) | Sex, age, race/ethnicity, meal plan, Pell grant status, highest parental education and the clustering of students within residence halls | +9/10 |
| Chung(30) | KNHANES/Cross-sectional/Korea | 20–64 n 5862 (2278 male and 3584 female) |
Asian | Household | USDA | DSM-IV | Depression and stress risk | Food insecurity increase the stress risk (OR=1·52; 95 % CI: 1·15, 2·01), but not depression risk (OR = 1·26; 95 % CI: 0·89, 1·78) | Sex, age, income, education, alcohol use, smoking status, physical activity, marital status and recipients of food assistance | +9/10 |
| Pryor(31) | TEMPO/longitudinal study/France | 18–35 n 1991 (38 male and 62 % female) |
Mixed | Household | USDA | MINI | Depression risk | Food insecurity increase the depression risk (RR = 2·01; 95 % CI: 1·01, 4·02) | Unadjusted | +7/10 |
| Maharaj(35) | –/Cross-sectional/South Africa | 18–75 n 335 (178 male and 157 female) |
African | Household | 12-month Food Security Scale | HSC-25 | Depression and anxiety risk | Food insecurity increase the depression risk (OR = 4·51; 95 % CI: 2·01, 10·09) and anxiety risk (OR = 4·52; 95 % CI: 2·09, 9·80) | Sex and age | +8/10 |
| Vilar-Compte(32) | –/Cross-sectional/Mexico | ≥65 n 329 (15·2 % male and 84·8 % female) |
Hispanic | Household | ELCSA | GDS-5 | Depression risk | Food insecurity increase the depression risk (OR = 2·84; 95 % CI: 1·77, 4·54) | Unadjusted | +7/10 |
| Hudin(34) | FELDA/Cross-sectional/Malaysia | 69·7 ± 6·0 n 289 (58 male and 238 female) |
Asian | Household | Food Security Tool for Elderly (2003) | GDS and DUSOC | Depression and stress risk | Food insecurity increase the depression risk (OR = 11·132; 95 % CI: 5·294, 23·40) and stress risk (OR = 2·47; 95 % CI: 1·18, 5·15) | Unadjusted | +7/10 |
| Tseng(36) | NHIS/Cross-sectional/USA | ≥18 n 18 456 (8740 male and 10 215 female) |
Mixed | Household | USDA | K-6 | Stress risk | Food insecurity increase the stress risk (OR = 3·1; 95 % CI: 2·3, 4·0) | Age, race/ethnicity, education, income, health insurance, smoking status, presence of a chronic disease in parent or child, marital status, and employment status |
+9/10 |
| Bruening(37) | SPARC/USA | ≥18 n 1138 (11 261 female; 7195 male) |
Mixed | Individual | USDA | ACHAS | Depression, stress and anxiety risk | Food insecurity increase the depression (OR = 1·98; 95 % CI: 1·34, 2·91) and stress risk (OR = 1·69; 95 % CI: 1·16, 2·46), but not anxiety risk (OR = 1·20; 95 % CI: 0·55, 2·59) | Sex, race/ethnicity, Pell grant status and residence hall group | +9/10 |
| Gregorio(38) | EpiDoC/Cross-sectional/Portugal | ≥18 n 10 661 (49·64 % female; 50·36 % male) |
White | Household | USDA | HRQoL | Depression and anxiety risk | Food insecurity increase the depression risk (OR = 1·50; 95 % CI: 1·09, 2·59) and but not anxiety risk (OR = 0·79; 95 % CI: 0·52, 1·21) | Age group, sex, educational level, employment status and NUTS II | +9/10 |
| Scanlon(39) | –/Cross-sectional/USA | ≥18 n 189 (100 % male) |
African–American | Household | USDA | CES-D | Depression risk | Food insecurity did not increase the depression risk (OR = 2·36; 95 % CI: 0·89, 6·29) | Age, education, ASPD, depression score and BPD symptom severity score; criminal justice – involvement history, relationship factors | +9/10 |
| Tong(40) | HOPE HOME/Cross-sectional/USA | ≥50 n 350 |
Mixed | Household | FSSM | CES-D | Depression risk | Food insecurity increase the depression risk (OR = 3·01; 95 % CI: 1·69, 5·38) | Age and education | +8/10 |
| Wattick(41) | –/Cross-sectional/USA | ≥18 n 1956 |
Mixed | Household | USDA | HRQOL | Depression and stress risk | Food insecurity increase the depression (OR = 2·19; 95 % CI: 1·58, 2·79) risk and stress (OR = 2·33; 95 % CI: 1·47, 3·71) risk | Unadjusted | +7/10 |
| Lee(42) | CHS/Cross-sectional/Korea | ≥18 n 225 965 (65 % female; 49 % male) |
Asian | Individual | USDA | CHS | Depression risk | Food insecurity increase the depression risk (RR = 2·33; 95 % CI: 1·47, 3·71) | Sex, residence, chronic disease, drinking status, smoking status, exercise, sleep duration, social network and BMI | +9/10 |
CWHS, California Women’s Health Survey; FSSM, Household Food Security Survey Module; NAFS, Nutrition and Function Study, SoFIE, Survey of Families, Income and Employment; CCHS, Canadian Community Health Survey; ACHAS, American College Health Association survey; KNHANES, Korea National Health and Nutritional Examination Survey; TEMPO, Trajectoires Épidémiologiques en Population; MINI, Mini-International Neuropsychiatric Interview; GDS-5, Geriatric Depression Scale; MHI-5, Mental Health Inventory; PHQ, Patient Health Questionnaire; FIES SM-I, Food Insecurity Experience Scale Survey Module for Individuals; FELDA, Felda Land Development Authority; NHIS, National Health Interview Survey; SPARC, Social impact of Physical Activity and nutRition in College; EpiDoC, Epidemiology of Chronic Diseases Cohort Study; HRQoL, health-related quality of life; CES-D,Centers for Epidemiologic Studies–Depression; CHS, Community Health Survey; ACHAS, American College Health Association survey; HRQOL, health-related quality of life; NEI, Negative Experience Index; and PEI, positive experience index; HSC, Hopkins Symptom Checklist, K-10: Kessler-10 scale.
Statistical analysis
To analyse the relationship between FI and adult depression, stress and anxiety risk, the fully adjusted risk estimates for depression, stress and anxiety risk were pooled. To accurately examine and explore the possible sources of heterogeneity among studies, subgroup analysis was performed based on age (18–65 and ≥65 years), sex (female, male and mixed), level of FI(23) (mild, moderate and severe) or continent (North America, Europe, Asia and others). Additionally, FI with hunger was considered as severe FI level in the pooling process. Pooled OR (and 95 % CI) was estimated using a weighted random-effect model (the DerSimonian-Laird approach). Heterogeneity among the studies was assessed by Cochran Q and I2 statistics (I2 = (Q-df)/Q × 100 %; I2 < 25 %, no heterogeneity; I2 = 25–50 %, moderate heterogeneity; I2 = 50–75 %, large heterogeneity, I2 > 75 %, extreme heterogeneity). The heterogeneity was considered significant if either the Q statistic had P < 0·1 or I2 > 50 %. Begg’s test and Egger’s test were conducted to evaluate publication bias (P < 0·05 was considered representative of statistical significance). Also, the trim-and-fill approach was used to obtain an adjusted effect size which took publication bias into account. All statistical tests for this meta-analysis were performed with STATA (version 14.0; Stata Corporation) and the statistical software package IBM SPSS statistics (version 23.0; SPSS, Inc.).
Results
Our systematic literature search produced 2627 publications, after the exclusion of duplicates from the different databases. From these, 2535 publications were excluded because they did not meet study eligibility criteria, leaving ninety-two articles for full-text assessment (Fig. 1). Ultimately, nineteen studies were included in the qualitative synthesis(11,24–42), and they all met the eligibility criteria for the quantitative synthesis(11,24–32,34–42). Eighteen studies used a cross-sectional approach(11,24–30,32,34–42) and one used a longitudinal approach(31). The risk ratios of 372 143 individuals in these studies were pooled for the meta-analysis. Sixteen studies(24–26,28–32,34,35,37–42) measured depression risk (n 257 685), seven(11,29,30,34,36,37,41) reported stress risk (n 41 914) and five(27,29,35,37,38) measured anxiety risk (n 89 496). From these, fifteen studies reported their results as maximally adjusted ORs(11,24–30,35–40,42), whilst the four others did not adjust for any covariates(31,32,34,41). These studies were published between 2007 and 2019 and conducted in the United States(24,25,28,29,36,37,39–41), Mexico(32), New Zealand(11), Canada(27), Malaysia(34), Portugal(38), South Africa(35), France(31), Korea(30,42) and Australia(26). Table 1 summarises the characteristics of the studies included. Quality assessment of each selected study was assessed using the Newcastle-Ottawa scale and showed that all studies included were of high (n 12) quality(11,25–30,36–39,42) and seven of medium quality(24,31,32,34,35,40,41) (Supplementary Table 2). In addition, our results suggested that the level of agreement between reviewers for data collection as well as for quality assessment was appropriate (κ = 0·759).
Fig. 1.
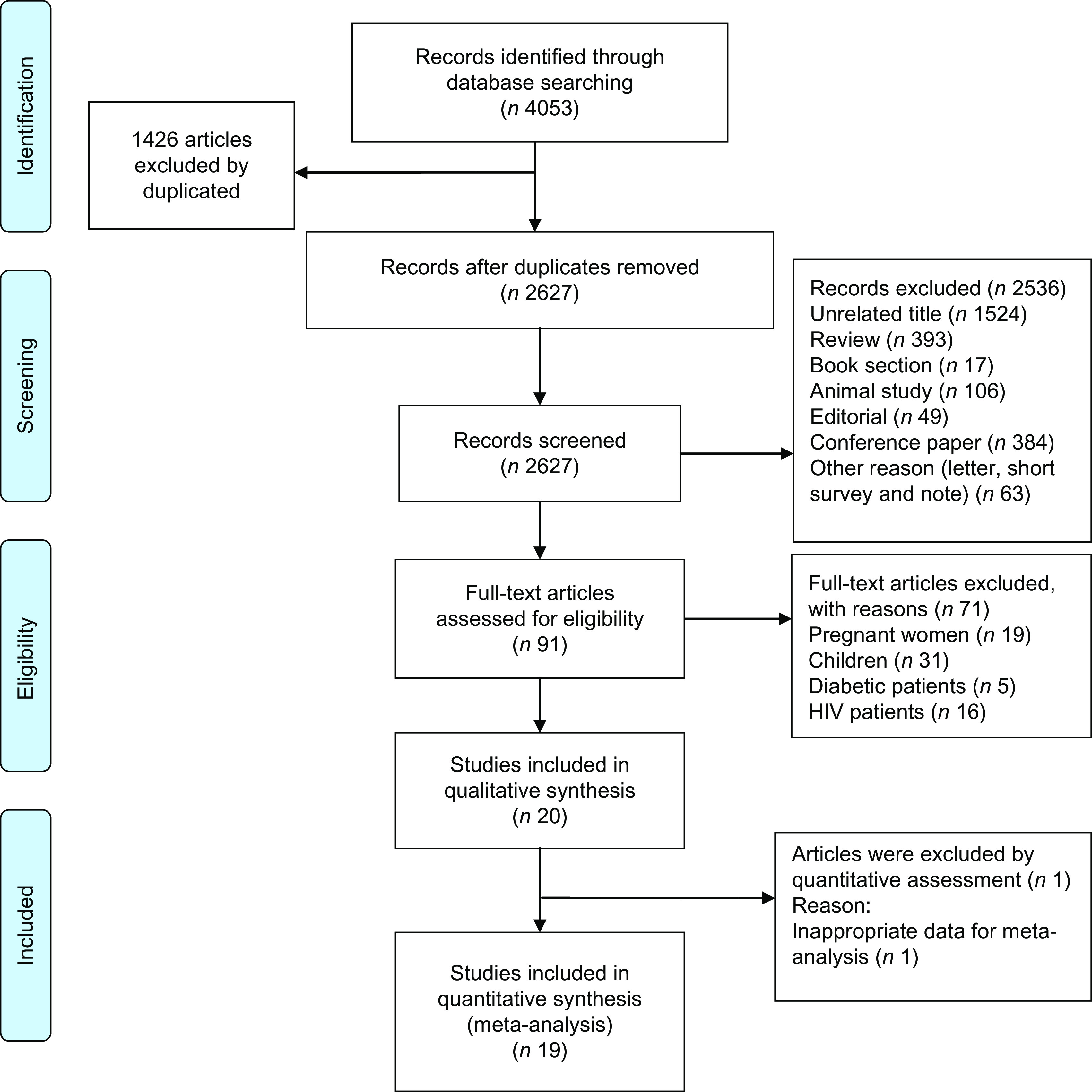
PRISMA flowchart describing the study’s systematic literature search and study selection
Quantitative synthesis
The study-specific, maximally adjusted, ORs results were pooled to examine the associations between FI and the risk of depression, stress and anxiety among adults.
Depression
As shown in Fig. 2 when all ORs were combined with the random-effects model, FI increases the risk of depression among adults (OR = 1·40; 95 % CI: 1·30, 1·58). A high heterogeneity was found amongst studies (I2 = 86·6 %, P < 0·001). For detecting the potential sources of heterogeneity, the subgroup analysis was based on age (18–65 and ≥65 years), sex (female, male and mixed), level of FI (mild, moderate and severe) or continent (North America, Europe, Asia) (Table 2). Subgroup analysis by age showed that FI for adults ≥65 years was associated with a higher risk of depression (OR = 1·75; 95 % CI: 1·20, 2·56, I2 = 93·79 %, P < 0·001) than in younger participants (i.e. <18–65 years) (OR = 1·34; 95 % CI: 1·20, 1·50, I2 = 79·0 %, P < 0·001) (Table 2). Subgroup analysis by sex revealed that FI increased the risk of depression in women (OR = 1·30; 95 % CI: 1·16, 1·46, I2 = 40·4 %, P = 0·18) and men (OR = 1·42; 95 % CI: 1·17, 1·72, I2 = 0·0 %, P = 0·78) (Table 2). In addition, subgroup analysis demonstrated that risk of depression increased with the magnitude of FI from moderate (OR = 1·45; 95 % CI: 1·40, 1·51, I2 = 0·0 %, P = 0·65) or severe (OR = 1·77; 95 % CI: 1·71, 1·83, I 2 = 0·0 %, P = 0·57) levels but not at a mild level (OR = 1·09; 95 % CI: 0·89, 1·36, I 2 = 0·0 %, P = 0·37) (Table 2). Finally, subgroup analysis according to continent illustrated that FI increased the risk of depression in studies conducted in North America (OR = 1·38; 95 % CI: 1·28, 1·50, I2 = 37·7 %, P = 0·12), Europe (OR = 1·31; 95 % CI: 1·04, 1·64, I2 = 31·3 %, P = 0·22) or Asia (OR = 1·44; 95 % CI: 1·04, 2·00, I2 = 93·7 %, P < 0·001). Subgroup analysis including sex, level of FI or continent attenuated heterogeneity (Table 2).
Fig. 2.
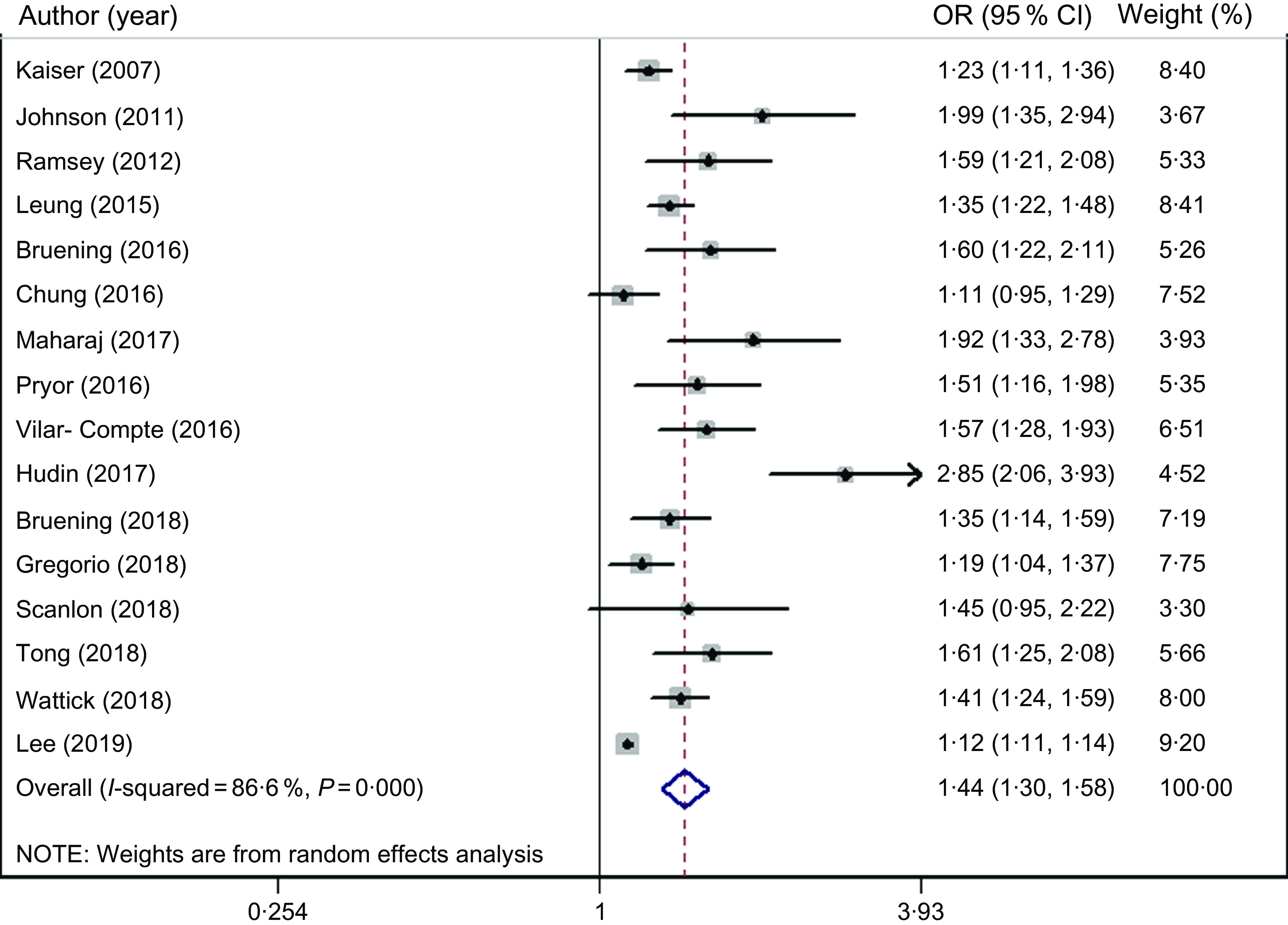
Forest plot showing odds ratio with 95 % confidence interval of the association between food insecurity and depression risk
Table 2.
Subgroup analysis to assess the association between food insecurity and mental disorders
| Subgrouped by | No. of individuals | No. of studies | OR* | 95 % CI | I 2 (%) | P for heterogeneity |
|---|---|---|---|---|---|---|
| Depression | ||||||
| Age (years) | ||||||
| 18–65 | 30 401 | 9 | 1·34 | 1·20, 1·50 | 79·0 | <0·001 |
| ≥65 | 5730 | 4 | 1·75 | 1·20, 2·56 | 93·0 | <0·001 |
| Sex | ||||||
| Women | 5054 | 3 | 1·30 | 1·16, 1·46 | 40·4 | 0·18 |
| Men | 1012 | 3 | 1·42 | 1·17, 1·72 | 0·0 | 0·78 |
| Mixed | 251 503 | 13 | 1·48 | 1·31, 1·66 | 87·7 | <0·001 |
| Food insecurity degree | ||||||
| Mild | 7165 | 2 | 1·09 | 0·89, 1·36 | 0·0 | 0·37 |
| Moderate | 1419 | 2 | 1·45 | 1·40, 1·51 | 0·0 | 0·65 |
| Severe | 1377 | 3 | 1·77 | 1·71, 1·83 | 0·0 | 0·57 |
| Continent | ||||||
| North America | 11 742 | 8 | 1·38 | 1·28, 1·50 | 37·7 | 0·12 |
| Europe | 12 652 | 2 | 1·31 | 1·04, 1·64 | 31·30 | 0·22 |
| Asia | 234 807 | 3 | 1·44 | 1·04, 2·00 | 93·7 | <0·001 |
| Stress | ||||||
| Sex | ||||||
| Women | 10 475 | 3 | 1·41 | 1·33, 1·49 | 0·0 | 0·44 |
| Men | 8530 | 3 | 1·46 | 1·15, 1·85 | 83·0 | 0·003 |
| Mixed | 155 324 | 5 | 1·80 | 1·43, 2·17 | 59·3 | 0·04 |
| Continent | ||||||
| North America | 21 768 | 4 | 1·38 | 1·21, 1·57 | 52·5 | 0·09 |
| Asia | 6151 | 2 | 1·26 | 1·06, 1·51 | 31·5 | 0·22 |
| Anxiety | ||||||
| Continent | ||||||
| North America | 78 500 | 3 | 1·29 | 1·23, 1·35 | 0·0 | 0·54 |
| Others | 10 996 | 2 | 1·30 | 0·62, 2·73 | 80·7 | <0·001 |
Calculated by random-effects model.
Stress
As shown in Fig. 3, FI significantly increased the risks of stress in adults (OR = 1·34; 95 % CI: 1·24, 1·44). A moderate heterogeneity was found between studies (I2 = 47·3 %, P = 0·07). For detecting the potential sources of heterogeneity, subgroup analysis was run based on the sex (female, male and mixed) and continent (North America and Asia). Subgroup analysis by sex indicated that FI increased the risks of stress among women (OR = 1·41; 95 % CI: 1·33, 1·49, I2 = 0·0, P = 0·44) and men (OR = 1·46; 95 % CI: 1·15, 1·85, I2 = 83·0 %, P = 0·003) and in both North America (OR = 1·38; 95 % CI: 1·21, 1·57, I2 = 52·5 %, P = 0·09) and Asia (OR = 1·26; 95 % CI: 1·06, 1·51, I2 = 31·5 %, P = 0·22) (Table 2).
Fig. 3.
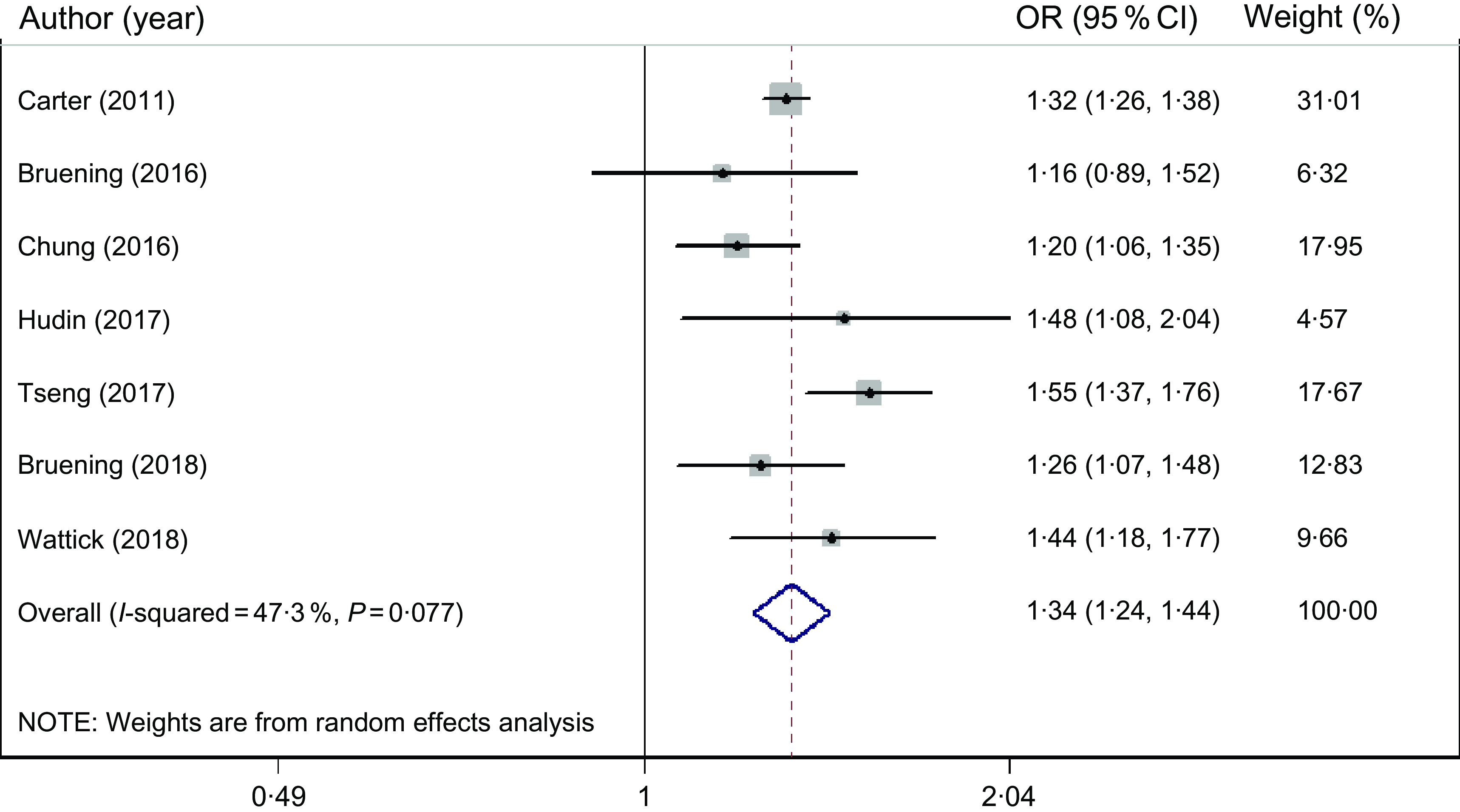
Forest plot showing odds ratio with 95 % confidence interval of the association between food insecurity and stress risk
Anxiety
No significant association existed between FI and anxiety risk (OR = 1·22; 95 % CI: 0·98, 1·52). A high heterogeneity was found amongst studies (I2 = 80·7 %, P < 0·001) (Fig. 4). However, subgroup analysis based on continent indicated FI increased the risk of anxiety in North America (OR = 1·29; 95 % CI: 1·23, 1·35, I2 = 0·0 %, P = 0·54), but not other countries (OR = 1·30; 95 % CI: 0·62, 2·73, I2 = 80·7 %, P < 0·001). Subgroup analysis by continent attenuated heterogeneity (Table 2). We did not conduct further subgroup analysis for association between FI and anxiety risk because of the small number of studies.
Fig. 4.
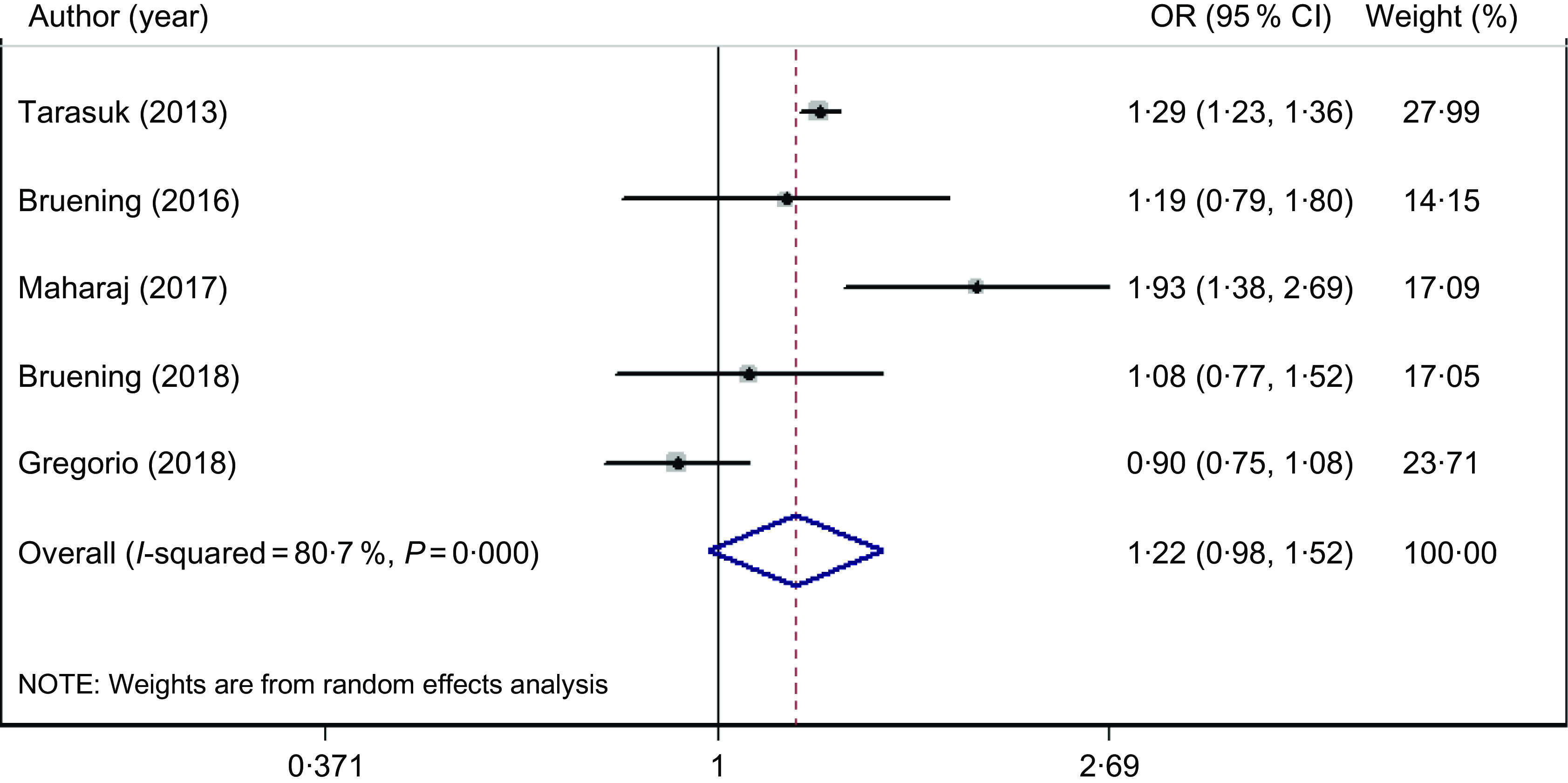
Forest plot showing odds ratio with 95 % confidence interval of the association between food insecurity and anxiety risk
Sensitivity analysis and publication bias
Sensitivity analysis revealed that the results were not affected by any one study. There was no evidence of publication bias for studies assessing the association between FI, the risk of stress (P = 1 for Begg’s test and P = 0·54 for Egger’s test) and anxiety (P = 1 for Begg’s test and P = 0·71 for Egger’s test). Although the result from the Begg’s test indicated publication bias for studies examining the association between FI and the risk of depression (P = 0·001), it was not confirmed by the Egger’s test (P = 0·24). The trim-and-fill approach showed that for depression risk is skewed to the right (Supplementary Fig. 1), indicating that six studies with negative results or reverse associations might not have been published (Supplementary Fig. 2).
Discussion
FI has received increasing attention worldwide, with more than 1 billion people estimated to have inadequate access to enough safe and nutritious food to meet their dietary needs for an active and healthy life(43). Although, the impact of FI on nutritional status, growth and development is well described(44), less is known about the non-nutritional impacts, such as on mental health. Therefore, the purpose of our review was to critically assess the associations between FI and the risks of depression, stress and anxiety among adults in cross-sectional studies. At present, this is the only meta-analysis in this context. The articles we have included illustrate that FI contributes to elevated depression in all subjects especially amongst Asians as well adults aged ≥65 years. It was notable that higher FI increased the risk for depressive symptoms. FI in older people might be due several factors including limited financial resources, mobility and transportation. Also, depression can affects ones perception of FI, which is likely to affect responses to FI questions(45).
A simple explanation for the existence of the positive relationship between degree of FI and depressive symptoms is that having insufficient food and nutrients undermines social relationships because of feelings of deprivation and alienation(46). Consequently, the most severe FI can be found alongside the most depressive symptoms. FI also increased the risk of stress in all subjects, especially those in North America for which, subgroup analysis found that it was associated with increased risk of anxiety. Current findings suggest that this continent might be more strongly related to the onset of psychological disorder risk than others, due in part to the large number of studies from North American (i.e. 9 of 19).
Some mixed findings that were apparent with respect to depression, stress and anxiety, which may depend on publication bias or a sample size effect. More studies were found on depression, compared with anxiety (n 5) and stress (n 7), and would impact on the statistical power of the meta-analysis. FI is also a broad and complex concept(15), and gathering such data is challenging and can result in measurement errors and misclassifications. In addition, most studies used different assessment tools for FI and mental health. The differences in the adjusted variables included in each study might also affect the results. Moreover, some mediators, such as demographic, socioeconomic, lifestyle and clinical variables, therapy support and genetic background, can all be confounding factors for FI(47,48). Therefore, these factors might affect any inconsistencies.
Our results for depression and stress were in line with a previous review showing an association between FI and symptoms of common mental disorders(15). Another review in children indicated that FI was linked to poorer intellectual, behavioural and psycho-emotional development(12), as did a study on women in high-income countries(49).
Pathways linking FI and poor mental health are likely to be both behavioural and biological and mediated centrally as fundamental changes occur in the hippocampus with depression(50). FI will also contributes to nutrient deficiency(51) and inadequate energy intake(52). Individuals with FI tend to consume a diet that is high in fat, refined sugars and Na and low in fruit, vegetables and fibre, leading to excess carbohydrate intake and decreased micronutrient consumption(51). Psychological problems also occur from a diet with a high-energy density and poor nutrient content(4,53) that can lead to overeating when food is readily available and cause adverse metabolic effects(4,54), as well as lower physical activity(4,55) and poor weight management(4,56). FI also results in an increased psycho-emotional burden by undermining social relationships because of feelings of deprivation and alienation leading to low self-efficacy and a deep sense of helplessness(46). Even when individuals are consuming adequate food and energy, with FI they may experience anxiety or stress because they are not eating in a culturally unacceptable way(57,58).
Like all studies, ours is not without limitations, which in the case of meta-analysis includes reporting, and personal bias, together with observational biases that could be inherent in the original studies. Although, observational studies make important contributions to the knowledge of the distribution and causes of diseases, possible sources of error and bias include selection, and information bias, measurement errors, plus confounding factors. In addition, it is a snapshot of the population that can change overtime and include Neyman bias (prevalence–incidence bias)(59). Moreover, the inherent methodologic limitations of cross‐sectional studies make it impossible to draw causal links with the variables recorded(59). Lastly, the studies included different tools used for assessing mental health, and although each of these has their own validity and reliability, the comparability of these measures is an important consideration that should be addressed.
We observed a high percentage of heterogeneity that may be due to the small number of studies (less than ~10 studies) for anxiety(60). Furthermore, we did not undertake an assessment of the grey literature and only worked with studies written in English. We were not able to assess the impact of other potential bias including demographic, lifestyle and clinical variables and genetic background. Due to high heterogeneity, subgroup analyses had to be undertaken, which reduced our statistical power. Despite these limitations, the strength of our study was its sensitivity, subgroup analysis and assessment of age, sex, level of FI with continent on the overall effect sizes, together with the high quality of most studies included. In addition, we tried to minimise any biases in the review process by performing a comprehensive search of the literature and also by conducting and reporting the review by adhering to the PRISMA guidelines. Lastly, the studies included used different tools for assessing FI, notably HFIAS and HFSSM. So, although the different measures of FI each have their own validity and reliability, the comparability of these measures should be studied further.
Implications for practice
The evidence from this meta-analysis suggests that FI has a significant effect on the likelihood of experiencing stress and depression, but not anxiety. Interventions that improve FI may reduce the burden of stress and depression and its subsequent impact on the family and society. However, identifying the direction of causality is important from an applied perspective because if FI precedes poor mental health, then interventions to promote food security could promote mental health. If poor mental health precedes FI, then mental health interventions should might do include information on food security.
Implications for research
To better understand FI and its association with mental health, future longitudinal studies, with other types of statistical analysis such as structural equation modelling with clearly defined, and validated tools for FI assessment are required. These should be more rigorous, with testable definitions of FI. Indeed, current tools available for measuring FI are subjective, rather limited in scope, with a majority assessing only one dimension (i.e. food access). To more accurately assess the true burden of FI, new tools should be adapted or developed to assess all four dimensions including food access, availability, utilisation and stability over time. Furthermore, assessment of associated variables such as demographic, socioeconomic, lifestyle and clinical variables, as well as differences in therapy would strengthen the assessment of potential pathways determining FI. Although, gathering data on actual nutritional intake is challenging(15), traditional dietary assessment methods (food records, FFQ, 24 h recalls, diet history with interviewer-assisted data collection) or new technology-based dietary assessment methods (web-based and mobile device applications) along with measuring FI are necessary. These could determine whether FI households are consuming diets that differ from food secure households and thus contribute to poor mental health.
Conclusion
In conclusion, this meta-analysis suggested that FI contributes to elevated depression in all subjects, especially amongst Asians and ≥65-year-old adults. It was notable that a higher degree of FI increased the risk for depressive symptoms. Based on our findings, FI also increased the risk of stress in all subjects, especially those in North America. These results indicate that health care services, which alleviate FI, would also promote holistic well-being. Implementing strategies to reduce the risk of mental disorders, especially in food insecure regions, through improving the bioavailability of complementary foods and following dietary guidelines should now be integrated into programmes designed to alleviate poverty. Furthermore, longitudinal and in-depth qualitative studies with longer follow-up periods are warranted to assess the possible relationship between household food security and adult mental health.
Acknowledgements
Acknowledgements: The authors thank the directors of the Kermanshah University of Medical Sciences for allowing them to conduct a systematic review and meta-analysis of the association between food insecurity and mental health. Financial support: None. Conflict of interest: The authors declare that they have no conflict of interest. Authorship: S.M. and A.P. designed the research; S.M., A.P., A.B. and C.J. conducted the research; S.M. and H.M. performed statistical analysis; S.M., M.M., A.G. and M.S. wrote the paper; S.M. and M.M. had primary responsibility for final content. All authors read and approved the final manuscript. Ethics of human subject participation: Not applicable.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S136898001900435X.
click here to view supplementary material
References
- 1. Anderson SA (1990) Core indicators of nutritional state for difficult-to-sample populations. J Nutr 120, 1559–1600. [DOI] [PubMed] [Google Scholar]
- 2. Shen X, Gao X, Tang W et al. (2015) Food insecurity and malnutrition in Chinese elementary school students. Br J Nutr 114, 952–958. [DOI] [PubMed] [Google Scholar]
- 3. Jones AD (2017) Food insecurity and mental health status: a global analysis of 149 countries. Am J Prev Med 53, 264–273. [DOI] [PubMed] [Google Scholar]
- 4. Moradi S, Mirzababaei A, Dadfarma A et al. (2019) Food insecurity and adult weight abnormality risk: a systematic review and meta-analysis. Eur J Nutr 58, 45–61. [DOI] [PubMed] [Google Scholar]
- 5. Moradi S, Arghavani H, Issah A et al. (2018) Food insecurity and anaemia risk: a systematic review and meta-analysis. Public Health Nutr 21, 3067–3079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Moradi S, Mirzababaei A, Mohammadi H et al. (2019) Food insecurity and the risk of undernutrition complications among children and adolescents: a systematic review and meta-analysis. Nutr 62, 52–60. [DOI] [PubMed] [Google Scholar]
- 7. Seligman HK, Bindman AB, Vittinghoff E et al. (2007) Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999–2002. J General Internal Med 22, 1018–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pérez-Escamilla R, Villalpando S, Shamah-Levy T et al. (2014) Household food insecurity, diabetes and hypertension among Mexican adults: results from Ensanut 2012. Salud Publica Mexico 56, Suppl. 1, s62–s70. [DOI] [PubMed] [Google Scholar]
- 9. Kirkpatrick SI, McIntyre L & Potestio ML (2010) Child hunger and long-term adverse consequences for health. Arch Pediatr Adolesc Med 164, 754–762. [DOI] [PubMed] [Google Scholar]
- 10. Gany F, Lee T, Ramirez J et al. (2014) Do our patients have enough to eat? Food insecurity among urban low-income cancer patients. J Health Care Poor Underserved 25, 1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Carter KN, Kruse K, Blakely T et al. (2011) The association of food security with psychological distress in New Zealand and any gender differences. Social Sci Med 72, 1463–1471. [DOI] [PubMed] [Google Scholar]
- 12. Whitaker RC, Phillips SM & Orzol SM (2006) Food insecurity and the risks of depression and anxiety in mothers and behavior problems in their preschool-aged children. Pediatr 118, e859–e868. [DOI] [PubMed] [Google Scholar]
- 13. Nanama S & Frongillo EA (2012) Altered social cohesion and adverse psychological experiences with chronic food insecurity in the non-market economy and complex households of Burkina Faso. Social Sci Med 74, 444–451. [DOI] [PubMed] [Google Scholar]
- 14. Bernal J, Frongillo EA & Jaffe K (2016) Food insecurity of children and shame of others knowing they are without food. J Hunger Environ Nutr 11, 180–194. [Google Scholar]
- 15. Weaver LJ & Hadley C (2009) Moving beyond hunger and nutrition: a systematic review of the evidence linking food insecurity and mental health in developing countries. Ecol Food Nutr 48, 263–284. [DOI] [PubMed] [Google Scholar]
- 16. Ponda MP, Liang Y, Kim J et al. (2017) A randomized clinical trial in vitamin D–deficient adults comparing replenishment with oral vitamin D3 with narrow-band UV type B light: effects on cholesterol and the transcriptional profiles of skin and blood. Am J Clin Nutr 105, 1230–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dew MA, Rosenberger EM, Myaskovsky L et al. (2015) Depression and anxiety as risk factors for morbidity and mortality after organ transplantation: a systematic review and meta-analysis. Transplant 100, 988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Araiza AM & Lobel M (2018) Stress and eating: definitions, findings, explanations, and implications. Social Personality Psychol Compass 12, e12378. [Google Scholar]
- 19. Organization WH (2017) Depression and Other Common Mental Disorders: Global Health Estimates. Geneva: World Health Organization. [Google Scholar]
- 20. Moher D, Liberati A, Tetzlaff J et al. (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339, b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Modesti PA, Reboldi G, Cappuccio FP et al. (2016) Panethnic differences in blood pressure in Europe: a systematic review and meta-analysis. PLoS One 11, e0147601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Landis JR & Koch GG (1977) The measurement of observer agreement for categorical data. Biom 33, 159–174. [PubMed] [Google Scholar]
- 23. Coates J, Swindale A & Bilinsky P (2007) Household Food Insecurity Access Scale (HFIAS) for Measurement of Food Access: Indicator Guide. Washington, DC: Food and Nutrition Technical Assistance Project, Academy for Educational Development, 34. [Google Scholar]
- 24. Kaiser L, Baumrind N & Dumbauld S (2007) Who is food-insecure in California? Findings from the California Women’s Health Survey, 2004. Public Health Nutr 10, 574–581. [DOI] [PubMed] [Google Scholar]
- 25. Johnson CM, Sharkey JR & Dean WR (2011) Indicators of material hardship and depressive symptoms among homebound older adults living in North Carolina. J Nutr Gerontology Geriatrics 30, 154–168. [DOI] [PubMed] [Google Scholar]
- 26. Ramsey R, Giskes K, Turrell G et al. (2012) Food insecurity among adults residing in disadvantaged urban areas: potential health and dietary consequences. Public Health Nutr 15, 227–237. [DOI] [PubMed] [Google Scholar]
- 27. Tarasuk V, Mitchell A, McLaren L et al. (2013) Chronic physical and mental health conditions among adults may increase vulnerability to household food insecurity. J Nutr 143, 1785–1793. [DOI] [PubMed] [Google Scholar]
- 28. Leung CW, Epel ES, Willett WC et al. (2015) Household food insecurity is positively associated with depression among low-income supplemental nutrition assistance program participants and income-eligible nonparticipants. J Nutr 145, 622–627. [DOI] [PubMed] [Google Scholar]
- 29. Bruening M, Brennhofer S, van Woerden I et al. (2016) Factors related to the high rates of food insecurity among diverse, Urban College freshmen. J Acad Nutr Diet 116, 1450–1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chung HK, Kim OY, Kwak SY et al. (2016) Household food insecurity is associated with adverse mental health indicators and lower quality of life among Koreans: results from the Korea National Health and Nutrition Examination Survey 2012–2013. Nutrients 8, E819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Pryor L, Lioret S, Van Der Waerden J et al. (2016) Food insecurity and mental health problems among a community sample of young adults. Social Psychiatry Psychiatric Epidemiol 51, 1073–1081. [DOI] [PubMed] [Google Scholar]
- 32. Vilar-Compte M, Martinez-Martinez O, Orta-Aleman D et al. (2016) Functional limitations, depression, and cash assistance are associated with food insecurity among older urban adults in Mexico city. J Health Care Poor Underserved 27, 1537–1554. [DOI] [PubMed] [Google Scholar]
- 33. Weigel MM, Armijos RX, Racines M et al. (2016) Association of household food insecurity with the mental and physical health of low-income urban Ecuadorian women with children. J Environ Public Health 2016, 5256084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hudin RS, Shahar S, Ibrahim N et al. (2017) Influence of socio-economic and psychosocial factors on food insecurity and nutritional status of older adults in FELDA settlement in Malaysia. J Clin Gerontology Geriatrics 8, 35–40. [Google Scholar]
- 35. Maharaj V, Tomita A, Thela L et al. (2017) Food insecurity and risk of depression among refugees and immigrants in South Africa. J Immigr Minor Health 19, 631–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tseng KK, Park SH, Shearston JA et al. (2017) Parental psychological distress and family food insecurity: sad dads in hungry homes. J Dev Behav Pediatr: JDBP 38, 611–618. [DOI] [PubMed] [Google Scholar]
- 37. Bruening M, van Woerden I, Todd M et al. (2018) Hungry to learn: the prevalence and effects of food insecurity on health behaviors and outcomes over time among a diverse sample of university freshmen. Int J Behav Nutr Physical Activity 15, 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Gregorio MJ, Rodrigues AM, Graca P et al. (2018) Food insecurity is associated with low adherence to the mediterranean diet and adverse health conditions in Portuguese adults. Front Public Health 6, 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Scanlon FA, Scheidell JD, Cuddeback GS et al. (2018) Depression, executive dysfunction, and prior economic and social vulnerability associations in incarcerated African American men. J Correct Health Care 24, 295–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Tong M, Tieu L, Lee CT et al. (2019) Factors associated with food insecurity among older homeless adults: results from the HOPE HOME study. J Public Health (Oxford, England) 41, 240–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wattick R, Hagedorn R & Olfert M (2018) Relationship between diet and mental health in a young adult Appalachian College population. Nutrients 10, 957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lee YS & Kim TH (2019) Household food insecurity and breakfast skipping: their association with depressive symptoms. Psychiatry Res 271, 83–88. [DOI] [PubMed] [Google Scholar]
- 43. Barrett CB (2010) Measuring food insecurity. Sci (New York, NY) 327, 825–828. [DOI] [PubMed] [Google Scholar]
- 44. Cook JT, Frank DA, Berkowitz C et al. (2004) Food insecurity is associated with adverse health outcomes among human infants and toddlers. J Nutr 134, 1432–1438. [DOI] [PubMed] [Google Scholar]
- 45. Wolfe WS, Frongillo EA & Valois P (2003) Understanding the experience of food insecurity by elders suggests ways to improve its measurement. J Nutr 133, 2762–2769. [DOI] [PubMed] [Google Scholar]
- 46. Palar K, Kushel M, Frongillo EA et al. (2015) Food insecurity is longitudinally associated with depressive symptoms among homeless and marginally-housed individuals living with HIV. AIDS Behavior 19, 1527–1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Franklin B, Jones A, Love D et al. (2012) Exploring mediators of food insecurity and obesity: a review of recent literature. J Community Health 37, 253–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Miraghajani M, Feizi A, Esmaillzadeh A et al. (2019) The relationship between dairy food intake and psychological distress among Iranian adults: results from a large cross-sectional population-based study. J Public Health 27, 781–789. [Google Scholar]
- 49. Maynard M, Andrade L, Packull-McCormick S et al. (2018) Food insecurity and mental health among females in high-income countries. Int J Environ Res Public Health 15, E1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Althoff RR, Ametti M & Bertmann F (2016) The role of food insecurity in developmental psychopathology. Prev Med 92, 106–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Melchior M, Chastang J-F, Falissard B et al. (2012) Food insecurity and children’s mental health: a prospective birth cohort study. PLoS One 7, e52615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Meza A, Altman E, Martinez S et al. (2019) “It’s a Feeling That One Is Not Worth Food”: a qualitative study exploring the psychosocial experience and academic consequences of food insecurity among college students. J Acad Nutr Diet 119, 1713–1721. e1711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Lang UE, Beglinger C, Schweinfurth N et al. (2015) Nutritional aspects of depression. Cell Physiol Biochem 37, 1029–1043. [DOI] [PubMed] [Google Scholar]
- 54. Suzuki A, Sakurazawa H, Fujita T et al. (2016) Overeating at dinner time among Japanese workers: is overeating related to stress response and late dinner times? Appetite 101, 8–14. [DOI] [PubMed] [Google Scholar]
- 55. Rebar AL, Stanton R, Geard D et al. (2015) A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health Psychol Rev 9, 366–378. [DOI] [PubMed] [Google Scholar]
- 56. Jung SJ, Woo HT, Cho S et al. (2017) Association between body size, weight change and depression: systematic review and meta-analysis. Br J Psychiatry 211, 14–21. [DOI] [PubMed] [Google Scholar]
- 57. Piaseu N, Belza B & Shell-Duncan B (2004) Less money less food: voices from women in urban poor families in Thailand. Health Care Women Int 25, 604–619. [DOI] [PubMed] [Google Scholar]
- 58. Piaseu N & Mitchell P (2004) Household food insecurity among urban poor in Thailand. J Nursing Scholarship 36, 115–121. [DOI] [PubMed] [Google Scholar]
- 59. Arab A & Rafie N (2018) Dietary patterns and semen quality: a systematic review and meta-analysis of observational studies. Andrology 6, 20–28. [DOI] [PubMed] [Google Scholar]
- 60. Sterne JA, Sutton AJ, Ioannidis JP et al. (2011) Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 343, d4002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S136898001900435X.
click here to view supplementary material


