Abstract
Objective
Spine awake surgery (SAS) aims to achieve faster recovery times, better outcomes, and a lesser economic impact on society. Our drive to establish SAS was to improve patient outcomes and health economics during the COVID-19 pandemic. After a systematic review and to the best of our knowledge, SAS, the Oxford Protocol, is the first protocolized pathway that aims to train bespoke teams performing SAS safely, efficiently, and in a standardized repeatable fashion. A pilot study was designed around newly derived protocols and simulated training to determine if SAS is a safe and implementable pathway to improve patient outcomes and health economics.
Methods
We assessed a cohort of 10 patients undergoing one-level lumbar discectomies and decompressions, analyzing the related costs, length of stay, complications, pain management, and patient satisfaction.
Results
The age range of our patients was 46–84 years. Three discectomies and 7 central canal stenosis decompressions were performed. Eight patients were discharged on the same day. All patients gave positive feedback about their experience of SAS. A significant cost saving was made compared to a general anesthesia (GA) overnight stay across the group. No on day cancellations occurred due to lack of bed availability. No patient needed analgesia in the recovery room or needed additional analgesia over and above the SAS e-prescription take home package.
Conclusions
Our early experience and journey reinforce our drive to push forward and expand on this process. It aligns with the international literature which highlights this approach as safe, efficient, and economical.
Key words: Health economics, Patient benefits, Patient journey, Spine awake surgery
Introduction
Spine swake surgery (SAS) should not be viewed as a modification of a specific surgical procedure but as a patient journey and a change in the paradigm of spine surgery. In order to carry out a successful procedure with all the benefits of SAS, one must adopt a holistic, multidisciplinary approach to the patient journey.
In this narrative we would like to share our experience setting up a Spine Awake Service in a large institute. This encompasses conception, governance, training, human factors considerations and changes in patient pathways.
SAS is relatively new, having been little known in neurosurgical and orthopedic practice in the recent past. It aims to achieve faster recovery times, better outcomes, and a lesser economic impact on society. The scope of procedures available under SAS range from lumbar decompressions, discectomies, instrumented procedures and functional spinal neurosurgery1, 2, 3, 4
The advent of the COVID-19 pandemic has dramatically impacted surgical practice in hospitals worldwide, leading to a backlog of cases that will be increasingly hard to tackle if we do not modify our practice.5 , 6
Also, to be considered are the higher risks of inpatient COVID-19 infection and staff shortages during this unexpected new era of medicine.7 SAS may provide a solution to these issues.
Our drive to establish SAS was to reap all the benefits of improved patient outcomes and health economics especially in light of the COVID-19 pandemic. It was also designed to improve theatre efficiency and to tackle long waiting lists. We assessed an early cohort of 10 patients undergoing one-level lumbar discectomies and decompressions, analyzing the related costs, length of stay, complications, pain management, and patient satisfaction.
After a systematic review of the literature and to the best of our knowledge, SAS The Oxford Protocol offers the first protocolized pathway that aims to train bespoke teams performing spine awake surgeries safely, efficiently and in a standardized and repeatable fashion.
Our Philosophy
It became very clear early on that implementing a change of such magnitude was a far greater challenge than merely performing a familiar surgical procedure under regional anesthesia. The challenges presented themselves in the form of changing established mind sets and practices, governance, training, and addressing the changes brought on by the COVID-19 pandemic.
We started by approaching an overseas team for advice and remote mentorship. This enabled us to develop our own pathway and protocols which were appropriate to our patient demographic and institutional set up.
We summarize this journey in 3 points.
-
1.
Stakeholder buy-in: We defined an overarching team goal and gave each member a rudimentary idea of their role within the team. We then allowed each member to develop their own protocols that best suited their working environments and most effectively contributed to achieving the teams' overall objective.8 , 9
-
2.Crosspollination: There are 2 arms to our approach to crosspollination.
- Cross cover: Though every member has specific tasks, during times of need, other members of the team may undertake basic tasks on their behalf. We achieved this through whole team simulated training which led to a clear understanding of each other's roles and responsibilities. This enables time efficiency and avoids miscommunication during surgery.
- Overarching understanding of patient journey: Multidisciplinary team training (including nonoperating theatre team members) allows every team member to be fully informed about every step of the patient pathway. Hence any team member can communicate to the patient clearly and uniformly about any step along the entire pathway. This is essential to develop patient trust and relieve anxiety.
-
3
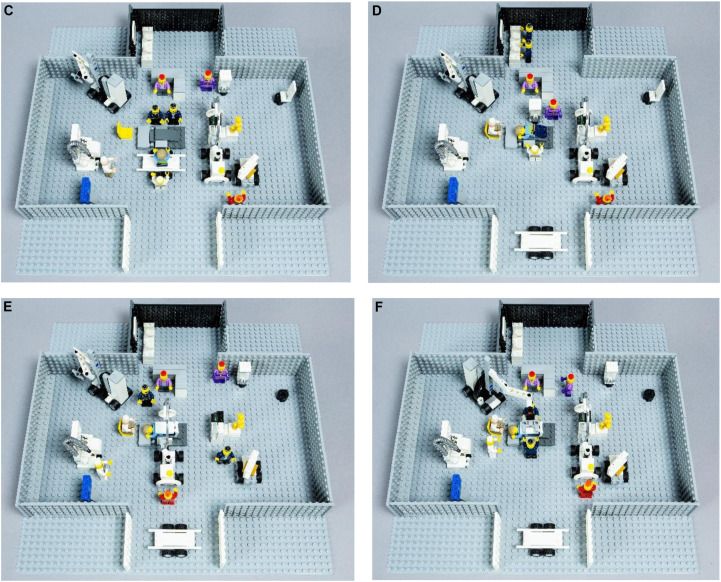
Simulated training using transferrable skills from high consequence industry to improve theatre choreography: The time critical nature of SAS, along with the well-being of the patient is crucial. To develop a more collaborative mentality amongst all the staff, we likened SAS to ‘24 hours of Le Mans’ pit-stop. An expert in pit-stop dynamics was invited to mentor us through this process. We began by looking at each individual role and breaking this down into exact movements and tasks within the operating theatre. Elements of Lean Six Sigma were combined10 , 11 and used to demonstrate how a collaborative effort can improve team performance by removing waste and reducing variation. Everyone was encouraged to create their own checklist and workflow. We used visual aids in the form of Lego models (Figure 1A-F) and recorded training sessions to demonstrate and improve the choreography.
Figure 1.
(A) Theater layout: 1. Operating table. 2. Ancillary theatre equipment. 3. C-arm. 4. X-ray monitor. 5. Trolley. 6. Portable computer. 7. Anesthetic machine. 8. Operating microscope. 9. Scrub table. 10. Ultrasound machine. 11. Scrub room. (B) The operating team: 1. SAS patient. 2. Surgeon. 3. Surgical assistant. 4. Anesthetist. 5. Anesthetic assistant. 6. Scrub nurse. 7. Scrub assistant. 8. Radiographer. (C) Spinal anesthetic. (D) Positioning and TLIP block. (E) Draping and level check. (F) Surgery.
Protocols were developed and presented to the Hospital New Procedures/Technology Advisory Committee and approvals were obtained to begin simulated training and recruit patients via the hospital governance structure.
In addition to our institution's standard protocols, we also designed the following steps as outlined in Table 1 .
Table 1.
SAS Oxford Protocol Steps
| Patient Selection |
|
| Preoperative Assessment |
|
| Day Care admission |
|
| Operative Stage |
|
| |
| |
| Recovery |
|
| |
| Adjuncts |
|
|
The spinal top-up is a mixture of 0.5% bupivacaine and fentanyl that is made available to the surgeon for direct intrathecal injection in the surgical field should the operation take longer than the spinal anaesthetic is effective for. It allows a controlled, incremental top-up of the spinal anaesthetic, and ensures the patient remains pain-free and comfortable throughout the procedure.
Nuances of SAS
Anesthetic Nuances
Although surgery under spinal anesthesia is commonplace it is rare that this takes place in the prone position. There is and should be caution when considering undertaking this. Special attention must be given to patient comfort and positioning, level, depth and duration of spinal anesthesia, emergency airway management, as well as conversion to general anesthesia (GA) in critical situations. The novelty of this situation led us to develop our own protocols and training to address this.
Spinal Anaesthetic
To improve efficiency, an intravenous fluid pre-load is administered on the ward prior to the patient arriving in theatre.
The spinal anesthetic is performed at a level above the lumbar pathology. In our experience, performing the spinal below the level of a tight stenosis may lead to an inadequate spread of the block due to alterations of CSF flow dynamics across the stenosis.
The spinal is performed in a sitting position using 1.8-2.5 ml 0.5% heavy bupivacaine with 15 μg of fentanyl (Figure 2). The patient then lies flat on the trolley and the level of the block is checked. Once an adequate level has been established the patient turns prone onto the operating table and the level is rechecked. Appropriate head up or down positioning is used to control the level of the block.
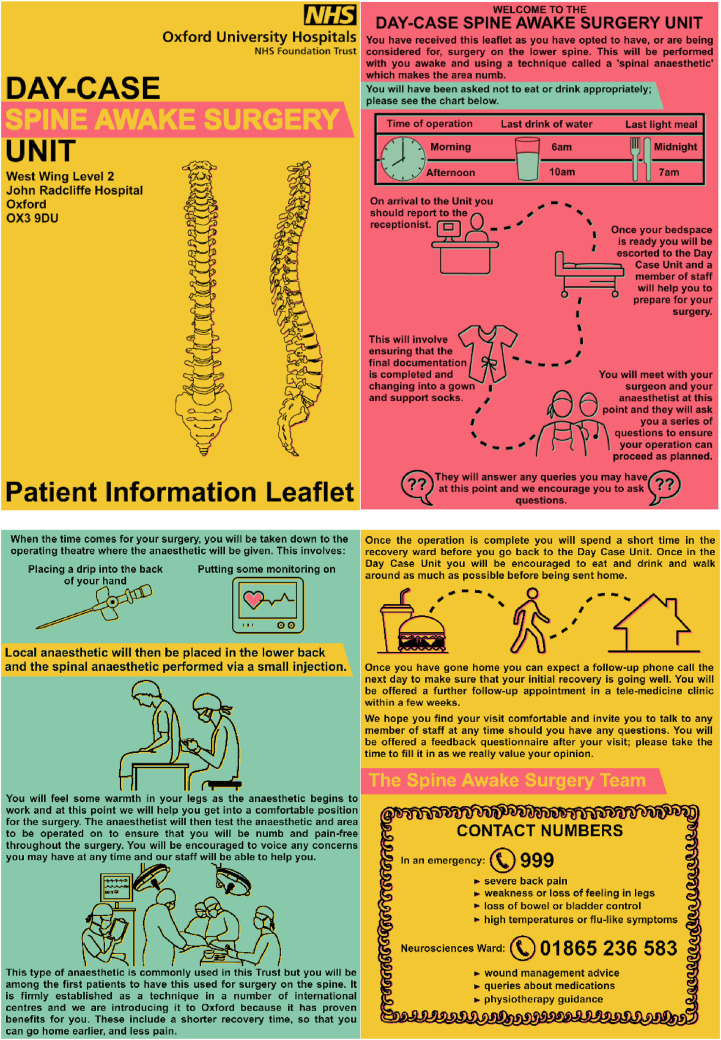
Figure 2.
Patient information leaflet.
Thoraco-Lumbar Inter-fascial Plane Block (TLIP)
Using ultrasound guidance, the planes between the subcutaneous tissues and Multifidus and between Multifidus and Longissimus are identified. Up to a total of 40 ml 0.25% bupivacaine (depending on the patient's weight and maximum safe dose calculations) is then injected bilaterally into these planes. At this point the final check of the spinal anesthetic is performed and surgery can commence.
Adjuncts to Spinal Anesthesia
Prior to coming to the operating theatre, the patient is given 10 mg Oxycodone, 2 mg Diazepam and 4 mg Ondansetron. Near the end of surgery 1 g IV Paracetamol is infused. The patient is offered further Paracetamol, Oxycodone, Diazepam, Ondansetron and 10 ml BD Lactulose on the Day Unit and to take home for 5 days.
Surgical Nuances
SAS may be daunting for surgeons and leads to considerations outside the paradigm of conventional spine surgery. Spine surgeons are not formally trained in dealing with SAS and it is essential that due thought, simulated training, and mentorship be undertaken prior to performing SAS.
The main factors to be taken into consideration are as follows.
Time Constraints Related to Regional Anesthesia
SAS, like other surgeries under regional anesthesia is a time constrained procedure. In our experience return of sensory function usually occurs around 90–120 minutes from onset of sensory block. To harness maximal length and depth of the regional anesthetic, it is paramount that time taken from delivery of anesthetic to incision is optimized. We generally achieve this in 12–16 mins. The stages include transfer from supine to prone position, delivery of TLIP block and local anesthetic to the incision site, painting/draping, positioning of operating equipment and Fluoroscopic level check.
We approached this stage as if undertaking a racing car pit stop, utilizing principles of lean six sigma and theatre choreography as described above.
Patient Positioning, Comfort, and Movement During Surgery
Detailed attention must be given to patient positioning, not only for comfort but to allow the best possible surgical access. SAS surgery has significant benefits over a general anesthetic as it does not expose the patient to complications such as pressure ulcers, compressive ocular damage, or limb plexopathy. As patients can position their lower body before complete onset of block and regain sensory function within 90 minutes, the risk of pressure related cutaneous complications is overall extremely low. We perform the procedure on pillows and achieve lumbar flexion via angulation of the operating table. This allows a good balance between patient comfort and surgical access. Patients should be counselled to inform a designated member of the team if they would like to reposition themselves or feel an urge to cough or sneeze. In our experience these situations are easily managed with good preoperative counselling and due intraoperative diligence.
Use of Minimally Invasive Techniques to Reduce Postoperative Pain and Enhance Recovery
Surgical technique for lumbar surgery varies widely from open nonmagnified procedures to full endoscopic techniques. We advocate the use of techniques that reduce tissue dissection and avoid removal of midline structures. The senior author of this paper also performs full endoscopic spine surgery and plans to adopt this technique with SAS.
Surgical Strategies to Deal with Intraoperative Complications
Complications such as CSF leaks, bleeding, break-through pain, and return to the supine position in an emergency should be planned for. We have developed protocols and conducted simulated training to successfully manage these situations.
All equipment to deal with such complications should be accounted for at the World Health Organization (WHO) check list and present in theatre before the start of the procedure. This ensures swift resolution should a complication arise. In case of a cerebrospinal fluid (CSF) leak, patient should be positioned head down to reduce risk of low-pressure headaches.
Team Decorum
Although one regularly assumes a professional decorum in theatre, special attention must be paid during SAS to ensure patient comfort and allay any anxieties. Human factors such as communication (both verbal and nonverbal), noise levels from equipment and alarms should be addressed. This is essential and is relevant to an awake patient in an unfamiliar environment with limited field of vision while in a prone position.
Early Outcomes
At the time of writing, we have performed 10 SAS procedures. The details are outlined in Table 2 .
Table 2.
SAS Procedures. Patient Cohort
| Patient | Age | Gender | Comorbidities | Procedure | Complications | Day of Discharge | Patient Satisfaction |
|---|---|---|---|---|---|---|---|
| 1 | 46 | M | None | L5/S1 MD | None | Same | TS |
| 2 | 75 | M | COPD | L4/5 CCD | Return to theatre for adjacent segment disc | Same | TS |
| Asthma | |||||||
| HTN | |||||||
| T2DM | |||||||
| High BMI | |||||||
| 3 | 73 | F | Liver disease | L3/4 CCD | Extension of decompression intraoperatively | Same | SS |
| 4 | 51 | M | High BMI OSA on CPAP | L4/5 MD | None | Same | TS |
| 5 | 84 | M | HTN Asbestosis | L4/5 MD | None | Same | TS |
| 6 | 61 | F | T2DM HTN | L3/4 CCD | None | Same | TS |
| 7 | 78 | M | HTN | L4/5 CCD | None | Same | TS |
| 8 | 49 | F | Asthma Anxiety | L5/S1 MD | None | Day 1 | SS |
| 9 | 78 | F | Renal disease | L3/4 CCD | CSF leak repaired intraoperatively | Day 3 | TS |
| HTN | |||||||
| CVA | |||||||
| TIAs | |||||||
| AF | |||||||
| 10 | 83 | F | CVA | L4/5 CCD | None | Same | TS |
| HTN | |||||||
| AF |
Satisfaction score: Totally satisfied, somewhat satisfied, neither satisfied nor dissatisfied, somewhat dissatisfied, totally dissatisfied.
MD, Microscopic discectomy; CCD, Central canal decompression; TS, Totally satisfied; SS, Somewhat satisfied.
The age range of our patients was 46–84 years. There were 3 discectomies and 7 central canal stenosis decompressions. Eight patients were discharged on the same day whilst 2 stayed overnight (one due to anxiety, another due to a TIA). All patients gave positive feedback about their experience of SAS. A cost saving of £84,800 was made compared to a general anesthetic overnight stay across the group. No on day cancellations occurred due to lack of bed availability. No patient needed analgesia in the recovery room or needed additional analgesia over and above the SAS e-prescription take home package.
Discussion
Regional anesthesia over general anesthesia has been embraced in many specialties of surgical practice with proven benefits to patient outcome.12, 13, 14, 15, 16, 17, 18, 19, 20
When considering the option of awake surgery for the different specialties and for spine surgery specifically, much emphasis is given to cost-effectiveness,21, 22, 23, 24, 25, 26, 27 lesser postoperative hospital stay,24 , 26 , 28 patient reported outcome,24 , 26 , 29, 30, 31, 32 peri- and postoperative complications.24 , 26, 27, 28 , 30 , 32 , 33 Spinal awake surgery is relatively new, having been known in the neurosurgical and orthopedic practice for 20 years. It aims, like for other surgical specialties, to faster recovery times, better outcomes and a lesser economic impact on society. The range of spinal procedures available under local anesthesia is ample, ranging from single-level decompressions and discectomies to cervical anterior procedures, instrumented lumbar procedures and functional spinal neurosurgery.1, 2, 3, 4 , 34 , 35
The advent of the recent COVID-19 pandemic has dramatically impacted surgical practice and patient outcome36 in hospitals around the world and in the United Kingdom, leading to the necessity of adapting elective surgical lists to the emergency, therefore raising ethical and medical issues37 and leading to a significant backlog of cases every year.5 , 6
As elective surgical practice is trying to resume in the NHS,38 spinal practice is being affected, as for other specialties, in the management of its elective surgery lists counteracted by an increase of urgent referrals that we think represents a symptom of the case backlog that has been accumulated.39 Elective spine cases have decreased, as compared to the prepandemic age40 and the necessity to reinstate such lists, in order to buffer the current backlog, is of paramount importance.41 The cost of reinstating elective surgery after the emergency is estimated to be high42 , 43 and under these circumstances, SAS could bring an important contribution to the different health systems around the world.
Conclusions
In modern medical practice, efforts are continually being made to improve clinical outcomes and health economics. SAS is a novel approach that delivers on both these fronts. We would encourage adopting this practice; however, we feel that this should not be stepped into without full preparation. The ground up team building allows members to design their own tailored protocols, engenders enthusiasm and encourages individual thought and reflective practice.
Our early experience and journey reinforce our drive to push forward and expand on this process. It aligns with the international literature which highlights this approach as safe, efficient, and economical. In the future, we hope to perform a wider range of lumbar spine surgeries including fusions and full endoscopic spine surgery.
In time, we feel that SAS could offer an alternative patient journey which can be adopted to suit many different settings whilst still offering numerous benefits.
CRediT authorship contribution statement
Paolo Rizzo: Conceptualization, Methodology, Formal analysis, Writing – review & editing, Investigation, Patient information leaflet. Helen Hann: Conceptualization, Methodology, Formal analysis, Writing – review & editing, Investigation, Patient information leaflet, Figures. Ben Coombs: Conceptualization, Methodology, Formal analysis, Writing – review & editing, Investigation, Patient information leaflet. Ali Asgar Hatim Ali: Conceptualization, Methodology, Formal analysis, Writing – review & editing, Data and tables. Amanda Stretton: Conceptualization, Methodology, Formal analysis, Writing – review & editing, Contribution to manuscript, Participation in the concept. Murtuza Sikander: Conceptualization, Methodology, Formal analysis, Writing – review & editing, Writing – original draft, Figures.
Acknowledgments
We would like to thank the following for their help during this project.
Alok Sharan, Dan Nicola, SAS team, Neurosciences management team, Healthshare, Rob Wheal and LEGO.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Fiani B., Reardon T., Selvage J., et al. Awake spine surgery: an eye-opening movement. Surg Neurol Int. 2021;12:222. doi: 10.25259/SNI_153_2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Garg B., Ahuja K., Sharan A.D. Awake spinal fusion. J Clin Orthop Trauma. 2020;11:749–752. doi: 10.1016/j.jcot.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garg B, Ahuja K, Mehta N, Sharan AD. Awake spinal fusion. JBJS Rev. 2021;9 doi: 10.2106/JBJS.RVW.20.00163. [DOI] [PubMed] [Google Scholar]
- 4.Wang M.Y., Grossman J. Endoscopic minimally invasive transforaminal interbody fusion without general anesthesia: initial clinical experience with 1-year follow-up. Neurosurg Focus. 2016;40:E13. doi: 10.3171/2015.11.FOCUS15435. [DOI] [PubMed] [Google Scholar]
- 5.Macdonald N., Clements C., Sobti A., Rossiter D., Unnithan A., Bosanquet N. The building backlog of NHS elective cases post Covid-19. Br J Surg. 2020;107:e377–e378. doi: 10.1002/bjs.11817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Macdonald N., Clements C., Sobti A., Rossiter D., Unnithan A., Bosanquet N. Tackling the elective case backlog generated by Covid-19: the scale of the problem and solutions. J Public Health. 2020;42:712–716. doi: 10.1093/pubmed/fdaa155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rickman H.M., Rampling T., Shaw K., et al. Nosocomial transmission of coronavirus disease 2019: a retrospective study of 66 hospital-acquired cases in a London Teaching hospital. Clin Infect Dis. 2021;72:690–693. doi: 10.1093/cid/ciaa816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Esmail L., Moore E., Rein A. Evaluating patient and stakeholder engagement in research: moving from theory to practice. J Comp Eff Res. 2015;4:133–145. doi: 10.2217/cer.14.79. [DOI] [PubMed] [Google Scholar]
- 9.Pandi-Perumal S.R., Akhter S., Zizi F., et al. Project stakeholder management in the clinical research environment: how to do it right. Front Psychiatry. 2015;6:71. doi: 10.3389/fpsyt.2015.00071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Laureani A., Antony J. Standards for lean six sigma certification. Int J Prod Perform Manag. 2011;61:110–120. [Google Scholar]
- 11.Salah S., Rahim A., Carretero J. The integration of Six Sigma and lean management. Int J Lean Six Sigma. 2010;1:249–274. [Google Scholar]
- 12.Chandran D., Woods C.M., Schar M., Ma N., Ooi E.H., Athanasiadis T. Cost analysis of injection laryngoplasty performed under local anaesthesia versus general anaesthesia: an Australian perspective. J Laryngol Otol. 2018;132:168–172. doi: 10.1017/S0022215117001384. [DOI] [PubMed] [Google Scholar]
- 13.Donauer K., Bomberg H., Wagenpfeil S., Volk T., Meissner W., Wolf A. Regional vs. general anesthesia for total knee and hip replacement: an analysis of postoperative pain perception from the international PAIN OUT Registry. Pain Pract. 2018;18:1036–1047. doi: 10.1111/papr.12708. [DOI] [PubMed] [Google Scholar]
- 14.Haugen T.W., Andera L.N., LaMadrid A.B. Awake thyroidectomy. Laryngoscope. 2020;130:685–690. doi: 10.1002/lary.28196. [DOI] [PubMed] [Google Scholar]
- 15.Hausman M.S., Jr., Jewell E.S., Engoren M. Regional versus general anesthesia in surgical patients with chronic obstructive pulmonary disease: does avoiding general anesthesia reduce the risk of postoperative complications? Anesth Analg. 2015;120:1405–1412. doi: 10.1213/ANE.0000000000000574. [DOI] [PubMed] [Google Scholar]
- 16.Kiss G., Claret A., Desbordes J., Porte H. Thoracic epidural anaesthesia for awake thoracic surgery in severely dyspnoeic patients excluded from general anaesthesia. Interact Cardiovasc Thorac Surg. 2014;19:816–823. doi: 10.1093/icvts/ivu230. [DOI] [PubMed] [Google Scholar]
- 17.Macfarlane A.J.R., Vlassakov K., Elkassabany N. Regional anesthesia for vascular surgery: does the anesthetic choice influence outcome? Curr Opin Anaesthesiol. 2019;32:690–696. doi: 10.1097/ACO.0000000000000781. [DOI] [PubMed] [Google Scholar]
- 18.MacNeill A.L., Mayich D.J. Wide-awake foot and ankle surgery: a retrospective analysis. Foot Ankle Surg. 2017;23:307–310. doi: 10.1016/j.fas.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 19.Romanzi A., Boleso N., Di Palma G., et al. Awake major abdominal surgeries in the COVID-19 era. Pain Res Manag. 2021;2021 doi: 10.1155/2021/8763429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wong H.Y., Pilling R., Young B.W.M., Owolabi A.A., Onwochei D.N., Desai N. Comparison of local and regional anesthesia modalities in breast surgery: a systematic review and network meta-analysis. J Clin Anesth. 2021;72 doi: 10.1016/j.jclinane.2021.110274. Erratum in: J Clin Anesth. 2021 Dec;75:110491. [DOI] [PubMed] [Google Scholar]
- 21.Agarwal P., Pierce J., Welch W.C. Cost analysis of spinal versus general anesthesia for lumbar diskectomy and laminectomy spine surgery. World Neurosurg. 2016;89:266–271. doi: 10.1016/j.wneu.2016.02.022. [DOI] [PubMed] [Google Scholar]
- 22.Cullen S., Wrafter P.F., Jones D., et al. Plastic surgery procedure unit: a streamlined care model for minor and intermediate procedures: a cost-benefit analysis. J Plast Reconstr Aesthet Surg. 2021;74:192–198. doi: 10.1016/j.bjps.2020.08.100. [DOI] [PubMed] [Google Scholar]
- 23.Eseonu C.I., Rincon-Torroella J., ReFaey K., Quiñones-Hinojosa A. The cost of brain surgery: awake vs asleep craniotomy for perirolandic region tumors. Neurosurgery. 2017;81:307–314. doi: 10.1093/neuros/nyx022. [DOI] [PubMed] [Google Scholar]
- 24.Finsterwald M., Muster M., Farshad M., Saporito A., Brada M., Aguirre J.A. Spinal versus general anesthesia for lumbar spine surgery in high risk patients: perioperative hemodynamic stability, complications and costs. J Clin Anesth. 2018;46:3–7. doi: 10.1016/j.jclinane.2018.01.004. [DOI] [PubMed] [Google Scholar]
- 25.Lalonde D.H. Latest advances in wide awake hand surgery. Hand Clin. 2019;35:1–6. doi: 10.1016/j.hcl.2018.08.002. [DOI] [PubMed] [Google Scholar]
- 26.Turel M.K., Bernstein M. Outpatient neurosurgery. Expert Rev Neurother. 2016;16:425–436. doi: 10.1586/14737175.2016.1158104. [DOI] [PubMed] [Google Scholar]
- 27.Walcott B.P., Khanna A., Yanamadala V., Coumans J.V., Peterfreund R.A. Cost analysis of spinal and general anesthesia for the surgical treatment of lumbar spondylosis. J Clin Neurosci. 2015;22:539–543. doi: 10.1016/j.jocn.2014.08.024. [DOI] [PubMed] [Google Scholar]
- 28.Zorrilla-Vaca A., Healy R.J., Mirski M.A. A comparison of regional versus general anesthesia for lumbar spine surgery: a meta-analysis of randomized studies. J Neurosurg Anesthesiol. 2017;29:415–425. doi: 10.1097/ANA.0000000000000362. [DOI] [PubMed] [Google Scholar]
- 29.Baenziger B., Nadi N., Doerig R., et al. Regional versus general anesthesia: effect of anesthetic techniques on clinical outcome in lumbar spine surgery: a prospective randomized controlled trial. J Neurosurg Anesthesiol. 2020;32:29–35. doi: 10.1097/ANA.0000000000000555. [DOI] [PubMed] [Google Scholar]
- 30.De Rojas J.O., Syre P., Welch W.C. Regional anesthesia versus general anesthesia for surgery on the lumbar spine: a review of the modern literature. Clin Neurol Neurosurg. 2014;119:39–43. doi: 10.1016/j.clineuro.2014.01.016. [DOI] [PubMed] [Google Scholar]
- 31.Galitzine S., Wilson K., Edington M., Burumdayal A., McNally M. Patients' reported experiences and outcomes following surgical excision of lower limb osteomyelitis and microvascular free tissue reconstruction under 'awake' epidural anaesthesia and sedation. Surgeon. 2021;19:193–199. doi: 10.1016/j.surge.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Leon-Rojas J.E., Ekert J.O., Kirkman M.A., Sewell D., Bisdas S., Samandouras G. Experience with awake throughout craniotomy in tumour surgery: technique and outcomes of a prospective, consecutive case series with patient perception data. Acta Neurochir. 2020;162:3055–3065. doi: 10.1007/s00701-020-04561-w. [DOI] [PubMed] [Google Scholar]
- 33.Lee J.K., Park J.H., Hyun S.J., Hodel D., Hausmann O.N. Regional anesthesia for lumbar spine surgery: can it be a standard in the future? Neurospine. 2021;18:733–740. doi: 10.14245/ns.2142584.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Garg B., Ahuja K., Khanna P., Sharan A.D. Regional anesthesia for spine surgery. Clin Spine Surg. 2021;34:163–170. doi: 10.1097/BSD.0000000000001096. [DOI] [PubMed] [Google Scholar]
- 35.Kai-Hong Chan A., Choy W., Miller C.A., Robinson L.C., Mummaneni P.V. A novel technique for awake, minimally invasive transforaminal lumbar interbody fusion: technical note. Neurosurg Focus. 2019;46:E16. doi: 10.3171/2019.1.FOCUS18510. [DOI] [PubMed] [Google Scholar]
- 36.Sudhan M.D., Singh R.K., Yadav R., et al. Neurosurgical outcomes, protocols, and Resource management during Lockdown: early institutional experience from one of the World's largest COVID 19 Hotspots. World Neurosurg. 2021;155:e34–e40. doi: 10.1016/j.wneu.2021.07.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Macleod J., Mezher S., Hasan R. Surgery during COVID-19 crisis conditions: can we protect our ethical integrity against the odds? J Med Ethics. 2020;46:505–507. doi: 10.1136/medethics-2020-106446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Davies P.S., Sinnerton R.J., MacInnes A., et al. Re-starting elective orthopaedic services in NHS Tayside during the COVID-19 pandemic. Surgeon. 2021;19:e230–e236. doi: 10.1016/j.surge.2020.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zahra W., Karia M., Rolton D. The impact of COVID-19 on elective and trauma spine service in a district general hospital. Bone Jt Open. 2020;1:281–286. doi: 10.1302/2046-3758.16.BJO-2020-0059.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Riley J., Verma R. Spinal surgery during the COVID-19 pandemic: the experience in a tertiary referral centre. J Spine Surg. 2021;7:62–67. doi: 10.21037/jss-20-643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McCabe R., Schmit N., Christen P., et al. Adapting hospital capacity to meet changing demands during the COVID-19 pandemic. BMC Med. 2020;18:329. doi: 10.1186/s12916-020-01781-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fowler A.J., Dobbs T.D., Wan Y.I., et al. Resource requirements for reintroducing elective surgery during the COVID-19 pandemic: modelling study. Br J Surg. 2021;108:97–103. doi: 10.1093/bjs/znaa012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Oussedik S., MacIntyre S., Gray J., McMeekin P., Clement N.D., Deehan D.J. Elective orthopaedic cancellations due to the COVID-19 pandemic: where are we now, and where are we heading? Bone Jt Open. 2021;2:103–110. doi: 10.1302/2633-1462.22.BJO-2020-0161.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]