Abstract
Introduction:
Ocular manifestations are seen in several autoimmune disorders including spondyloarthritis (SpAs). Though acute anterior uveitis (AAU) is the hallmark of SpAs, episcleritis and scleritis are also seen. Genetic and geographical factors impact the prevalence of AAU; however, available evidence support that HLA-B27 positivity is closely associated with it.
Objective:
The current narrative review is focused on clinical features of AAU and its management.
Methods:
For the purpose of this narrative review; literature search covered MEDLINE, Google scholar and EMBASE databases and included articles published in English language from January 1980 till April 2022 using the following keywords: “Ankylosing spondylitis”, “Spondyloarthritis”, “Eye manifestations”, “Ocular”, “Uveitis” and “Arthritis”.
Conclusion:
Patients with SpA may suffer from different ocular complications with uveitis being the most common one. Biological therapy is a promising medical strategy enabling in achieving therapeutic goals with minimal adverse effects. An effective management strategy for patients with AAU associated with SpA could be formulated by the collaboration between ophthalmologists and rheumatologists.
Keywords: ankylosing spondylitis, uveitis, spondyloarthritis, eye manifestations, ocular, arthritis
INTRODUCTION
Spondyloarthritis (SpA) is an umbrella term for a group of autoimmune rheumatic diseases comprising psoriatic arthritis, reactive arthritis, SpA related to inflammatory bowel diseases (IBD) and ankylosing spondylitis (AS) that affects the spine and peripheral joints. They have an estimated global incidence of 1%.1 Non-radiographic axial SpA is also common; a cross-sectional survey conducted in Asian patients with inflammatory back pain found that 36.46% of them met its classification criteria.2 The exact aetiopathogenesis of this condition is not yet fully understood; however, involvement of immune mediators on the background of several genetic, familial and environmental predispositions are considered important.
Autoimmune disorders such as SpAs exert pernicious systemic and ocular effects. Peripheral manifestations, especially inflammation of entheses (enthesitis) and fingers and toes (dactylitis) are the hallmark of SpA. Ocular problems are frequently encountered in SpA, of which uveitis is the hallmark which is reported in almost 40% of the patients. Uveitis can be infectious or non-infectious, and can be a part of either a systemic disease (rheumatological or otherwise) or a local process. Literature reports a higher recurrence rate, bilateral involvement and frequent posterior synechiae in patients with rheumatological disease associated uveitis than those without.3 The presentation of ocular manifestation varies in every individual ranging from mild to severe. Untreated uveitis increases the risk of further complications of chronic ocular inflammation resulting in blindness. Precise diagnosis with prompt treatment by ophthalmologist in collaboration with rheumatologist may mitigate the distressing ocular sequelae and complications. In a meta-analysis by Turk et al., type of ocular involvement in childhood and adult SpA was noted to be similar.4 However, occurrence of uveitis was less frequent in adult-onset PsA compared to child-onset PsA.4
In this narrative review we have appraised the various ocular manifestations of SpA; particularly Acute Anterior Uveitis (AAU) and present some perspectives on its management.
SEARCH STRATEGY
For the purpose of this narrative review, literature search covered MEDLINE, Google scholar and EMBASE databases and included articles published in English language from January 1980 till April 2022 using the following keywords: “Ankylosing spondylitis”, “Spondyloarthritis”, “Eye manifestations”, “Ocular”, “Uveitis”, and “Arthritis”. Table 1 lists some of the more relevant studies based on the search.
Table 1.
Some of the important studies of uveitis associated with SpA.
| Study [Reference] | Study Design | Diagnosis/Number of patients | Study outcomes |
|---|---|---|---|
| Vale et al., 20186 | Observational retrospective study | SpA/153 | Uveitis predominantly occurred in men, and more frequently in HLA-B27 positive patients |
| Mitulescu et al., 20187 | Retrospective study | SpA/67 | Patients with AAU and inflammatory back pain should be referred to a rheumatology unit. |
| Ninan et al., 20178 | Hospital based cross sectional | Seronegative /SpA | Uveitis percentage was 16.3%, AS was commonest occurring in 69.3% and 78.3% patients were HLA-B27 positive |
| Das et al., 201510 | Retrospective study | Uveitis of varying etiologies/343 | Changing pattern of uveitis in a tertiary institute was reported with highest number of HLA-B27 associated uveitis. |
| Lee et al., 201711 | Retrospective, interventional case series | AS/91 | Men preponderance (70%), average onset in the fourth decade, and unilateral manifestation (87.9%) was observed |
| Bouzid et al. 202031 | Retrospective study | SpA/101 | First-line sulfasalazine reduced uveitis relapses |
| van Denderen et al., 201434 | Randomized controlled trial | AS/77 | Adalimumab treatment. significantly reduced the number of acute uveitis attacks, and the number of attacks per patient |
| Rudwaleit et al., 201637 | Randomized, double-blind and placebo-controlled RAPID-axSpA (NCT01087762) | axial SpA/218 | Certolizumab Pegol reduced uveitis flares |
| Calvo-Río et al., 201638 | Multi-center randomized trial | SpA/15 | Golimumab is predicted to be useful therapeutic option in refractory SpA-related uveitis |
EPIDEMIOLOGY
The International Uveitis Study Group has classified uveitis according to the location, clinical course, and distribution.5,6 Depending upon the location of inflammation in tissue whether anterior or posterior to the lens it is labelled as anterior or posterior uveitis. Clinically it is classified by aetiology as infectious, non-infectious, and masquerade (heterogeneous group of eye diseases that mimic chronic intraocular inflammation).5 An unsatisfactorily extended delay of 5 to 10 years is generally observed among the first occurrence of SpA symptoms including uveitis and its diagnosis. This delay may be attributed to the lack of awareness regarding SpA and requirement of there being radiographic sacroiliitis grade 2 bilaterally or grade 3 or 4 unilaterally for its classification.
Acute anterior uveitis is the most common extra-articular manifestation in SpA which might be acute or chronic.6,7,8 It is the most frequent type of Uveitis prevalent globally though infectious causes are more common in the developing countries.9
The epidemiologic variations of uveitis depends on the type of SpA, disease duration and presence of HLA-B27 gene.10 Gender and ethnic variations are strong factors behind the epidemiological pattern seen. Male preponderance is observed with SpA associated uveitis with differences in clinical presentations in both genders; however, no definitive reason for these differences has been established as yet.11,12
From Europe an urban multi-ethnic population were investigated to explore the epidemiological spectrum of uveitis and reported 25% had immune associated uveitis.13 An observational survey in France which included 902 patients with SpA showed uveitis prevalence of 32.2% with recurrence rate of 52.3%.14 Factors independently associated with uveitis in this survey were noted to be the presence of HLA-B27 gene and disease duration for ≥ 10 years (P<0.0001).14 A systematic literature review has found an overall incidence of 32.7% of uveitis in patients with SpA with disease duration of 17.7±1.0 years.15
A strong co-relation exists between HLA-B27 gene and AAU; nevertheless, cases of undiagnosed SpA are common in patients with AAU, primarily in those who carry the HLA-B27 gene.16 Current evidence suggests that AAU linked with the HLA-B27 has a less favourable prognosis and prone to frequent relapses.17 In this context it is important to emphasise that the classification criteria proposed by the Assessment in Spondyloarthritis International Society (ASAS) of axial-SpA includes presence of HLA-B27 as a part of the clinical arm.18
CLINICAL ASPECTS
Ocular involvement in SpA includes the sclera, episclera, the uveal tract, and other adjacent structures including vitreous humour, retina, optic nerve, and vessels. Uveitis in SpA indicates severity of the disease and can be bilateral too. Its characteristic feature is the “ping-pong” pattern meaning uveitis can affect alternatively one or the other eye.5
Blurred vision is the main symptom of AAU caused by ciliary spasm and presence of cells and/or flare in the anterior chamber of the eye; while pain, redness and watering are the other symptoms. Episodes of photophobia (due to ciliary muscle spasm secondary to inflammation in anterior chamber), circumcorneal injection (due to engorgement of episcleral vessels around ciliary body) and keratic precipitates, hypopyon (inflammatory cells in the anterior chamber of the eye), pupillary membrane (formed by the inflamed aqueous) and hyphema (blood cells in the anterior chamber) have also been reported.9
Persistence of uveitis leads to the development of posterior synechiae (adhesions between the lens and the iris). Secondary glaucoma can occur either as a part of the disease process or due to the excessive use of topical steroids. Other manifestations such as cataract and iris atrophy may also occur, though latter is the cardinal feature of herpetic anterior uvieitis.5
A multicentric Ibero-American cohort study demonstrated that 20% of patients with SpA had AAU, emphasizing that it is the commonest complication of SpA.19 Another finding from this study revealed that psoriatic arthritis was inversely related to AAU; however, it has been reported that uveitis is more deceptive in outbreak, chronic, posteriorly located and active bilaterally in PsA, when compared with other SpAs.20
Rudwaleit and colleagues compared patients with non-radiographic axial SpA and AS and did not find statistically significant differences in the prevalence of AAU, HLA-B27 and disease activity.21 Previous studies have shown that men are more prone to develop SpA-associated AAU, at an early age than women.12,22 However, rates of ocular manifestation and visual acuity were not predisposed to the gender.12
Another study from Taiwan has found that more than 90% of the patients with AS display the HLA-B27 positivity with the high proportion of the HLA-B*2704 subtype. It also reported an early disease onset and more relapses in HLA-B27-associated AAU.23 Although, HLA-B27 positivity is a key factor responsible for the incidence of SpA in patients with AAU, a wide range of incidence has been reported due to clinical and methodological differences including study design, classification criteria used for SpA, interobserver variability in radiography readings, and duration of follow-up.24
This variability of AAU among the different types of SpA was highlighted by several studies. Its higher prevalence in AS is perhaps a reflection of the higher frequency of HLA-B27-positive patients with AS.22 Among patients with psoriatic arthritis and IBD also a wide range of AAU prevalence associated with HLA-B27has been reported.25 Furthermore, a meta-analysis reported AAU as the most common (25.8%) extraarticular manifestation in patients with AS followed by psoriasis (9.3%) and IBD (6.8%).26
In ophthalmological settings, patients with AAU should be taken into consideration for the probability of a SpA diagnosis, especially in the presence of chronic back pain. Similarly, in rheumatological settings, presence of AAU in SpA is an useful indicator of a disease flare or suboptimal treatment. In accordance with the Assessment in Spondyloarthritis International Society/European League Against Rheumatism (ASAS-EULAR) recommendations for axial SpA, a rheumatologist can be the lead coordinator in a multidisciplinary network due to his/her thorough knowledge of the entire range of SpA.27 In this context, an algorithm called Dublin Uveitis Evaluation Tool (DUET) has been proposed to direct the ophthalmologists and physicians for timely referrals of patients with AAU to rheumatologists that will facilitate early detection of SpA.28
MANAGEMENT
Early and accurate diagnosis for appropriate management of AAU is imperative to prevent morbidity and enhance the quality of life caused by poor eyesight and other complications. Management of AAU comprises local and systemic therapies depending on the gravity of problem and response to the treatment. The aetiology, anatomic site, type of onset, potential ophthalmic and systemic risks of drugs should be critically understood for accomplishing therapeutic success. The major goal of the treatment of SpA associated AAU is relief from acute attack and the prevention of relapses.
The treatment of uveitis is achieved through several strategies comprising of:
Topical therapy
This is the standard treatment approach for symptomatic relief of an acute attack of AAU. A cycloplegic agent is used in combination with steroids that may be used systemically, topically, or by subconjunctival injection. Topical cycloplegics used with topical steroids prevents the formation of posterior synechiae.29 Furthermore, advances in the drug delivery systems has led to the development of intravitreal implants delivering steroids or other compounds. Systemic glucocorticoids (such as prednisolone or prednisone) are administered when topical treatment is ineffective and especially for bilateral uveitis.
Systemic NSAIDs
Systemic NSAIDs inhibit prostaglandins and are used in mild conditions and inflammations non-responsive to topical therapy. They have been found to be an ideal alternative to glucocorticoids and are capable of reducing uveitis attacks.29
Conventional synthetic disease-modifying antirheumatic drugs (csDMARDs)
The use of methotrexate in non-infectious uveitis has been found to decrease the rate of AAU flares during the withdrawal of systemic glucocorticoids.30 There is paucity in the data regarding treatment of AAU using sulfasalazine and leflunomide. A study by Bouzid et al. Has reported a reduction in uveitis relapses in a series of 101 patients with recurrent uveitis.31 Azathioprine is moderately effective in the treatment of non-infectious uveitis. There is evidence of systemic cyclosporine for treating intermediate and posterior uveitis which is comparable to systemic glucocorticoids.30
Biologic and targeted synthetic DMARDs
Biologic DMARDs are recombinant DNA based therapies that consist of bioengineered soluble receptors, monoclonal antibodies, and cytokines that are responsible for expressing the pro and anti-inflammatory components of the immune system. An important pro-inflammatory cytokine TNF alpha is therapeutically very effective in treating several rheumatic diseases and their ocular manifestations. TNF antagonists including infliximab and adalimumab have been reported to reduce the frequency of AAU.32–34 A meta-analysis estimated the frequency of uveitis in patients with AS who were treated with infliximab and etanercept therapies and concluded that infliximab was more effective than etanercept.35 When Etanercept was indirectly compared to other monoclonal TNF antagonists, it showed higher AU flare rates. Several studies suggest that monoclonal antibodies are more effective than soluble receptors for the treatment of uveitis. Therefore, Etanercept is not recommended for treatment of spondyloarthritis with uveitis.35
Infliximab or adalimumab also may be used as glucocorticoids-sparing treatment for patients with chronic uveitis associated with SpA.36 Experience with other biologics in AAU such as Certolizumab and Golimumab is growing.37,38
FUTURE PERSPECTIVES
Despite advanced therapies available for the treatment of uveitis, challenges persist. Although, there is an upsurge in the randomized controlled trials evaluating treatment interventions in SpA, there is a scarcity of data from head-to-head studies especially in the context of ocular manifestations. Such comparative data would provide better evidence required for clinical decision-making and healthcare economic assessments. Several biologic therapies have shown excellent results in patients with AAU associated with SpA. More evidence is needed to determine the efficacy of biologic therapy consisting of anti-TNF alpha in patients with AAU.
CONCLUSION
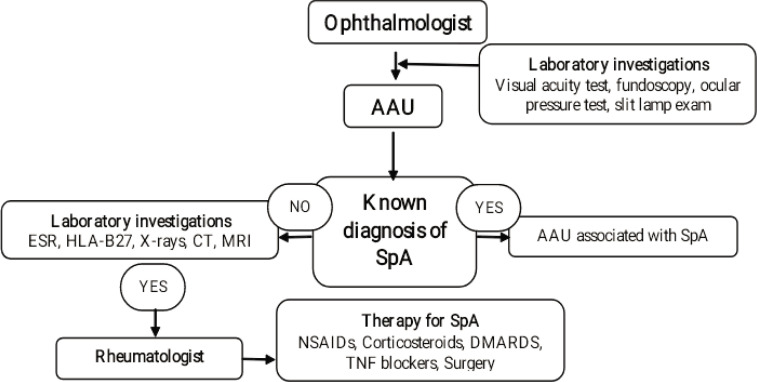
Patients with SpAs may suffer from different ocular complications with uveitis being the most common one. Genes, gender, and geographical factors are the key factors impacting the epidemiological pattern of uveitis. Biological therapy is a promising medical strategy enabling us to achieve therapeutic goals accurately with minimal adverse effects. An effective management strategy for patients with AAU associated with SpA can be achieved by due collaboration between ophthalmologists and rheumatologists (Figure 1).28
Figure 1.
Management of uveitis in SpA. A collaborative approach of rheumatologist and ophthalmologist (based on Haroon M. et al.)28
CONFLICT OF INTEREST
The authors declare no conflict of interest.
FUNDING
None.
REFERENCES
- 1.Shah A, Paramesparan K, Rennie WJ. Peripheral seronegative spondyloarthritis-Updates on critical criteria. Indian J Musculoskelet Radiol 2019;1:101–7. [Google Scholar]
- 2.Burgos-Varga R, Wei JC, Rahman MU, Akkoc N, Haq SA, Hammoudeh M, et al. The prevalence and clinical characteristics of nonradiographic axial spondyloarthritis among patients with inflammatory back pain in rheumatology practices: A multinational, multicenter study. Arthritis Res Ther 2016;18:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tseng ST, Yao TC, Huang JL, Yeh KW, Hwang YS. Clinical manifestations in uveitis patients with and without rheumatic disease in a Chinese population in Taiwan. J Microbiol Immunol Infect 2017;50:798–804. [DOI] [PubMed] [Google Scholar]
- 4.Turk M, Hayworth J, Nevskaya T, Pope J. The frequency of uveitis in patients with adult versus childhood spondyloarthritis. RMD Open 2020;6:e001196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Agrawal RV, Murthy S, Sangwan V, Biswas J. Current approach in diagnosis and management of anterior uveitis. Indian J Ophthalmol 2010;58:11–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vale IMS, Pereira IA, de Souza MM. Analysis of the frequency of uveitis in spondyloarthritis patients and associations with clinical parameters of the disease. Revista Brasileira de Oftalmologia 2018;77:80–4. [Google Scholar]
- 7.Mitulescu CT, Popescu CC, Oprea CL, Predețeanu D, Istrate S, Ciuluvică R, et al. A referable clinical pattern of spondyloarthritis-associated uveitis. Rom J Ophthalmol 2018;62:155–61. [PMC free article] [PubMed] [Google Scholar]
- 8.Ninan F, Mathew J, Philip SS, John D, Danda D, John SS. Uveitis of spondyloarthritis in Indian subcontinent: A cross sectional study. IJAM 2017;4. [Google Scholar]
- 9.Muñoz-Fernández S, Martín-Mola E. Uveitis. Best Pract Res Clin Rheumatol 2006;20:487–505. [DOI] [PubMed] [Google Scholar]
- 10.Das D, Bhattacharjee H, Das K, Tahiliani PS, Bhattacharyya P, Bharali G, et al. The changing patterns of uveitis in a tertiary institute of Northeast India. Indian J Ophthalmol 2015;63:735–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee JH, Choi M, Rim THT, Lee SC, Lee CS. Clinical characteristics and prognostic factors in ankylosing spondylitis associated uveitis. Ocul Immunol Inflamm 2019;27:64–9. [DOI] [PubMed] [Google Scholar]
- 12.Smith WM. Gender and spondyloarthropathy-associated uveitis. J Ophthalmol 2013;2013:928264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Llorenç V, Mesquida M, Sainz de la Maza M, Keller J, Molins B, Espinosa G, et al. Epidemiology of uveitis in a Western urban multiethnic population. The challenge of globalization. Acta Ophthalmol 2015;93:561–7. [DOI] [PubMed] [Google Scholar]
- 14.Canouï-Poitrine F, Lekpa FK, Farrenq V, Boissinot V, Hacquard-Bouder C, Comet D, et al. Prevalence and factors associated with uveitis in spondylarthritis patients in France: Results from an observational survey. Arthritis Care Res (Hoboken) 2012;64:919–24. [DOI] [PubMed] [Google Scholar]
- 15.Zeboulon N, Dougados M, Gossec L. Prevalence and characteristics of uveitis in the spondyloarthropathies: A systematic literature review. Ann Rheum Dis 2008;67:955–9. [DOI] [PubMed] [Google Scholar]
- 16.Jakob E, Reuland MS, Mackensen F, Harsch N, Fleckenstein M, Lorenz HM, et al. Uveitis subtypes in a German interdisciplinary uveitis center-analysis of 1916 patients. J Rheumatol 2009;36:127–36. [DOI] [PubMed] [Google Scholar]
- 17.Power WJ, Rodriguez A, Pedroza-Seres M, Foster CS. Outcomes in anterior uveitis associated with the HLA-B27 haplotype. Ophthalmology 1998;105:1646–51. [DOI] [PubMed] [Google Scholar]
- 18.Rudwaleit M, van der Heijde D, Landewé R, Listing J, Akkoc N, Brandt J, et al. The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part II): Validation and final selection. Ann Rheum Dis 2009;68:777–83. [DOI] [PubMed] [Google Scholar]
- 19.Sampaio-Barros PD, Pereira IA, Hernández-Cuevas C, Berman A, Burgos-Vargas R, Gutierrez MA, et al. An analysis of 372 patients with anterior uveitis in a large Ibero-American cohort of spondyloarthritis: The RESPONDIA group. Clin Exp Rheumatol 2013;31:484–9. [PubMed] [Google Scholar]
- 20.Queiro R, Torre JC, Belzunegui J, González C, De Dios JR, Unanue F, et al. Clinical features and predictive factors in psoriatic arthritis-related uveitis. Semin Arthritis Rheum 2002;31:264–70. [DOI] [PubMed] [Google Scholar]
- 21.Rudwaleit M, Haibel H, Baraliakos X, Listing J, Märker-Hermann E, Zeidler H, et al. The early disease stage in axial spondylarthritis: Results from the German Spondyloarthritis Inception Cohort. Arthritis Rheum 2009;60:717–27. [DOI] [PubMed] [Google Scholar]
- 22.Braakenburg AM, de Valk HW, de Boer J, Rothova A. Human leukocyte antigen-B27-associated uveitis: Long-term follow-up and gender differences. Am J Ophthalmol 2008;145:472–9. [DOI] [PubMed] [Google Scholar]
- 23.Ho HH, Chen JY. Ankylosing spondylitis: Chinese perspective, clinical phenotypes, and associated extra-articular systemic features. Curr Rheumatol Rep 2013;15:344. [DOI] [PubMed] [Google Scholar]
- 24.Cantini F, Nannini C, Cassarà E, Kaloudi O, Niccoli L. Uveitis in Spondyloarthritis: An Overview. J Rheumatol Suppl 2015;93:27–9. [DOI] [PubMed] [Google Scholar]
- 25.Cantini F, Niccoli L, Nannini C, Kaloudi O, Bertoni M, Cassarà E. Psoriatic arthritis: A systematic review. Int J Rheum Dis 2010;13:300–17. [DOI] [PubMed] [Google Scholar]
- 26.Stolwijk C, van Tubergen A, Castillo-Ortiz JD, Boonen A. Prevalence of extra-articular manifestations in patients with ankylosing spondylitis: A systematic review and meta-analysis. Ann Rheum Dis 2015;74:65–73. [DOI] [PubMed] [Google Scholar]
- 27.van der Heijde D, Ramiro S, Landewé R, Baraliakos X, Van den Bosch F, Sepriano A, et al. 2016 update of the ASAS-EULAR management recommendations for axial spondyloarthritis. Ann Rheum Dis 2017;76:978–91. [DOI] [PubMed] [Google Scholar]
- 28.Haroon M, O’Rourke M, Ramasamy P, Murphy CC, FitzGerald O. A novel evidence-based detection of undiagnosed spondyloarthritis in patients presenting with acute anterior uveitis: the DUET (Dublin Uveitis Evaluation Tool). Ann Rheum Dis 2015;74(11):1990–5. [DOI] [PubMed] [Google Scholar]
- 29.Gupta N, Agarwal A. Management of uveitis in spondyloarthropathy: Current Trends. Perm J 2018;22:17–041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gómez-Gómez A, Loza E, Rosario MP, Espinosa G, Morales JMGR, Herreras JM, et al. Efficacy and safety of immunomodulatory drugs in patients with anterior uveitis: A systematic literature review. Medicine (Baltimore) 2017; 96: e8045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bouzid N, Jamilloux Y, Chapurlat R, Pradat P, De Parisot A, Kodjikian L, et al. Impact of systemic treatments on the course of HLA-B27-associated uveitis: A retrospective study of 101 patients. PLoS ONE 2020;15:e0230560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guignard S, Gossec L, Salliot C, Ruyssen-Witrand A, Luc M, Duclos M, et al. Efficacy of tumor necrosis factor blockers in reducing uveitis flares in spondyloarthropathy: A retrospective study. Ann Rheum Dis 2006;65:1631–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Braun J, Baraliakos X, Listing J, Sieper J. Decreased incidence of anterior uveitis in patients with ankylosing spondylitis treated with the anti-tumor necrosis factor agents infliximab and etanercept. Arthritis Rheum 2005;52:2447–51. [DOI] [PubMed] [Google Scholar]
- 34.van Denderen JC, Visman IM, Nurmohamed MT, Suttorp-Schulten MS, van der Horst-Bruinsma IE. Adalimumab significantly reduces the recurrence rate of anterior uveitis in patients with ankylosing spondylitis. J Rheumatol 2014;41:1843–8. [DOI] [PubMed] [Google Scholar]
- 35.Ming S, Xie K, He H, Li Y, Lei B. Efficacy and safety of adalimumab in the treatment of non-infectious uveitis: A meta-analysis and systematic review. Drug Des Devel Ther 2018;12:2005–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Calvo Zorrilla I, Guerrero Basterretxea E, Ibarguengoitia O, Montero D, Garcia Vivar ML, Ruíz Lucea E, et al. Frequency and pattern of the uveitis in spondyloarthritis with biological therapy. Arthritis Rheumatol 2018;70. [Google Scholar]
- 37.Rudwaleit M, Rosenbaum JT, Landewé R, Marzo-Ortega H, Sieper J, van der Heijde D, et al. Observed incidence of uveitis following certolizumab pegol treatment in patients with axial spondyloarthritis. Arthritis Care Res (Hoboken) 2016;68:838–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Calvo-Río V, Blanco R, Santos-Gómez M, Rubio-Romero E, Cordero-Coma M, Gallego-Flores A, et al. Golimumab in refractory uveitis related to spondyloarthritis. Multicenter study of 15 patients. Semin Arthritis Rheum 2016;46(1):95–101. [DOI] [PubMed] [Google Scholar]