Abstract
The goal of this research was to determine the extent of pelvic floor dysfunction and the factors that contribute to it. The study design was community-focused and cross-sectional, and participants were chosen using a systematic random sampling technique. For data entry and cleansing, we used EPI data version 3.1 software, and for analysis, we used Statistical Package for the Social Sciences version 26. The 95% confidence interval was predicted, and the factor with a significant level less than 0.05 was chosen for multivariate logistic regression analysis. The overall Magnitude of pelvic floor dysfunction was 37.7% [(95% confidence interval (31.7-42.5)]. The most common type of pelvic floor dysfunction is overactive bladder, which was reported by 135 of all participants. Pelvic organ prolapse accounted for 92 (30.4%) of all cases, and 4 factors were found to be significantly associated with pelvic floor dysfunction. In this study, age 55 years [(AOR = 2.1; 95% CI: (1.52-6.42)], heavy labor work for more than 10 years [(AOR = 3.21; 95% CI: (1.86-5.72) grand-multipara, and being menopause [(AOR = 4.03; 95% CI: (2.20-8.27)] were linked to symptoms of pelvic floor dysfunction. The magnitude of pelvic floor dysfunction in this study was slightly higher than in Ethiopian studies. Pelvic floor dysfunction has been linked to heavy load lifting, low socioeconomic status, recurrent vaginal deliveries, chronic cough, and menopause. Screening and treatment of pelvic floor disorders should be prioritized in collaboration with regional and zonal health departments.
Keywords: symptomatic pelvic floor dysfunction, women, magnitude, risk factors, Ethiopia
What already known about this topic
Because of the sensitivity of the symptoms of pelvic floor dysfunction, women feel embarrassed and stigmatized by society, which makes it difficult for them to seek treatment. Hence, determining the magnitude of pelvic floor dysfunction and identifying risk factors was deemed critical.
What this study adds
Early detection and treatment of pelvic floor dysfunction provides a good out outcome of the interventions and prevents further complications. Community based awareness creation to screening and link to health facility to appropriate treatment options of pelvic floor disorder managements is so fundamental.
How this study might affect research, practice or policy
Because of the sensitivity issues associated with women who have symptomatic pelvic floor dysfunction, encouraging women’s health-seeking behavior regarding pelvic floor dysfunction through community-based health education is the best strategy for saving women from the complications of pelvic floor dysfunction than waiting until woman coming to health facility.
Background
Pelvic floor dysfunction (PFD) is a Gynecological health problem that contains different clinical diagnoses, and the most widespread snags are pelvic organ prolapse (POP), fecal incontinence (FI), overactive bladder, and urine incontinency. 1 The International Urogynecological Association and the International Continence Society (ICS) defined UI as an unconscious leak of urine, fecal incontinency as an uncontrolled loss of solid or liquid feces, and pelvic organ prolapse as the descent of a pelvic organ from its usual location, resulting in a bulging or protruding of the vaginal wall. 2
Cystocele, cysto-urethrocele, uterine prolapse, rectocele, and enterocele are all traditional terms for the protrusion site of pelvic organ prolapse. 3 When these terms refer to an organ, they imply that vaginal protrusion is caused by a rupture of the bladder, bladder/urethra, uterus, rectum, or small intestine. 4 Patients with pelvic organ prolapsed frequently experience stress urinary incontinence (SUI), urge urinary incontinence, urinary frequency, urgency, urinary retention, recurrent urinary tract infections, or micturition disorders. In women all over the world, symptoms range from mild discomfort to intolerable social and psychological difficulties, as well as common and devastating health complications. 5
A patient with stress urinary incontinence may complain of involuntary urine leakage during exertion, sneezing, or coughing; concurrent with these events, involuntary leakage from the urethra can be a documented sign noted by a provider. 6 Women with pelvic floor disorders, in general, have sexual problems; those with advanced pelvic organ prolapse have marital problems, and some end up divorcing due to their sexual problems. 4
Flatus incontinency, loose or solid stools that causes a social or hygiene issue is referred to as anal incontinence (AI). In addition, fecal incontinence has been linked to paradoxical contractile muscle atrophy. 7 Millions of women worldwide suffer from pelvic floor disorders; one in every 9 American women has undergone pelvic floor dysfunction surgery at some point in her life, and 30% of women are at risk of requiring another surgery for the same condition. 8
As a result of social stigma, women with pelvic floor dysfunction are frequently humiliated, embarrassed, shamed, and fearful. 9 Women who have progressive pelvic floor dysfunction and urinary incontinence have a poor body image and a lower quality of life, and some may isolate themselves from the community and avoid performing daily tasks. 10 Urine and anal incontinence are socially and emotionally crippling issues. 11 Due to a lack of underwear, disposable pads, and washing facilities, women in rural areas unable to control urinary leakage, exposing them to poor hygiene and odor issues. 12
Various studies have linked increasing age, increasing parity, and lifting heavy objects to pelvic floor dysfunction. Furthermore, anatomical prolapse and, more importantly, older age at last delivery were linked to pelvic floor dysfunction. 13 Due to social stigma and a lack of access to health care, only 17% of women with POP receive treatment in Ethiopia. 14
Objectives
To determine the magnitude of pelvic floor dysfunction among a woman residing in Ethiopia, 2022
To identify factors related with pelvic floor dysfunction among women residing in Ethiopia, 2022
Methods
Study Area and Period
This study conducted in Assosa Zone consists of 2 hospitals, 5 health centers, and 44 health posts as a whole. Sherkole refugee camp, housing 9526 displaced people from North Sudan and South Sudan, is also located in Homosha. The populations’ main means of livelihood are agrarian and semi-agrarian and some of them are traded.
This zone contains a total of 8 districts: Assosa, Bambasi, Homosha, Menge, Undulu, Sherkole, Kurmuk, and Oda Buldiglu. This study was conducted from December 26, 2021, to March 27, 2022.
Study Design, Eligibility Criteria and Sampling Procedure
A cross-sectional, community-based study was used. The source population consisted of all women who had lived in the Assosa zone for the previous 6 months. The study population consisted of women living in selected kebeles of the Assosa zone. A randomly selected woman lives in homes chosen from among the kebeles chosen as study units. Women who had lived in the area for at least 6 months were eligible. Women who were seriously ill and had severe psychiatric or cognitive problems were excluded from the survey.
The sample size was estimated by 41.1% using a single population proportion formula, with the assumptions of a 5% margin of error and 95% confidence interval; /2 = critical value = 1.96; 10% nonresponse rate; and the design effect of sampling step from an Ethiopian study. 15 Therefore, the final sample size was 818.
A multistage random sampling technique was performed. The required number of kebeles was chosen at random. Next, the determined sample (818) was proportionately assigned to each selected kebeles. Finally, a simple random sampling technique was used to select households, and a fit woman was recruited from each household. When there was more than one woman in one household who could fulfill our eligibility criteria, we used a raffle technique to select one of the women.
Operational Definitions
Symptomatic pelvic floor dysfunction (PFD): was evaluated based on whether the woman stated one or more of the indicators of urine leakage (UI), fecal incontinence (FI), and pelvic organ descent. For the purposes of the study, women with at least one of UI, FI, or pelvic organ prolapse were assumed to have pelvic floor dysfunction.2,16,17
Overactive Bladder: evaluated as to whether the woman has a sense of urgency to urinate, urine frequency, and urine leakage due to a sense of urgency. 18
Stress urine incontinency (UI): considered if the woman complains of an uncontrolled loss of urine related to both urge and stress urine leakage. 19
Anal incontinence (AI): Anal incontinence was deemed if the woman has responded with an unintentional loss of solid or liquid feces at least for a monthly for the past year. 20
Pelvic organ prolapse (POP): A pelvic organ prolapse was evaluated when the woman reported a feeling of bulging, pressure or when something seemed to be coming down through the vagina and a visible mass was bulging from the vaginal canal. 21
Income level: The amount of the annual income is determined by the sum of the individual family income.
Dependent Variables
Symptomatic Pelvic floor dysfunction
Independent Variables
Socio-demographic variables, General health conditions, Obstetric and gynecologic factors and Individual related factors.
Procedure
Data is collected using a pre-tested, structured questionnaire administered by interviewers, which is adopted after reviewing various studies and modified based on the local situation and research objective. It was created in English first, and then translated into Amharic, and then back into English to ensure consistency. Questions on pelvic floor dysfunction, health behaviors, demographic and socioeconomic factors, personal factors, general health-related factors, and obstetric and gynecological factors were included in the questionnaires.
Data Quality Assurance
The adequacy of the questionnaire in terms of content, consistency, language, and organization thoroughly checked and modified during the pretest according to standards, guidelines, and comments from investigators and data collectors to ensure data quality and relevance to the study’s objective. Data collectors are trained for 2 days on the data collection process, accuracy, and completeness. During data collection, the supervisor checked each questionnaire for completeness and logical consistency, which was then checked by the study director.
Data Processing and Analysis
The data were coded, cleaned, and entered into Epidata version 3.1 before being analyzed with SPSS Version 26. Furthermore, equality was checked. Variables with a P value of .2 or higher in bivariate logistic analysis were moved to multivariate logistic analysis. The following statistics were computed: frequency, percentages, proportions, and odds ratios. As an effect on outcome variables, adjusted odds ratios with the 95% confidence interval at a significance level less than 0.05 were calculated.
Result
Socio-Demographic Characteristics of the Participants
Eight hundred eighteen women were scheduled for interviews, and 798 participated in this study, yielding a 97.5% response rate. Participants range in age from 15 to 74 years old, with a mean age of 36 years (IQR = 18). The majority of them (78%) were married and living together, and more than half (54%) were housewives.
Fifty percent of the participants reported having done heavy labor work, and 72% lived in rural areas. They obtain water from a distance using more than 10-liter containers, collect and cut firewood, transport heavy objects to and from the market, and engage in other farming activities as heavy labor work in their daily activities (Table 1).
Table 1.
Socio-Demographic Characteristics of the Participants.
| Variable (n = 798) | Frequency | Percent % | |
|---|---|---|---|
| Age | 15-24 | 128 | 16 |
| 25-34 | 247 | 31 | |
| 35-44 | 223 | 28 | |
| 45-54 | 104 | 13 | |
| 55+ | 96 | 12 | |
| Marital status | Never married | 61 | 7.6 |
| Married and living together | 621 | 78 | |
| Divorced/separated | 88 | 11 | |
| Widowed | 27 | 3.4 | |
| Educational status | Un able to read and write | 255 | 32 |
| able to read and write | 191 | 24 | |
| Primary complete (1-8) | 136 | 17 | |
| Secondary complete (9-12) | 112 | 14 | |
| College and above | 104 | 13 | |
| Occupation | House wife | 430 | 54 |
| Employee | 112 | 14 | |
| Merchant | 176 | 22 | |
| Other (students, daily laborer) | 80 | 10 | |
| Recidenece | Urban | 223 | 28 |
| Rural | 575 | 72 | |
| Heavy labor work | Yes | 427 | 53.5 |
| No | 371 | 46.5 | |
| Monthly income | <2000 | 231 | 29 |
| 2000-2999 | 287 | 36 | |
| 3000-4999 | 168 | 21 | |
| 5000+ | 112 | 14 | |
| Heavy physical work | Yes | 399 | 50 |
| No | 303 | 38 | |
| Couldn’t estimate | 96 | 12 | |
| Duration of heavy labor work | <10 years | 120 | 30 |
| Age in years In come by Ethiopian birr (EB) | |||
General Health Condition of the Participants
Fifty percent of the participants had a history of chronic cough, diabetes, 104 were hypertensive, majority had recurrent urinary tract infections, and 16% (128) were khat users (Table 2).
Table 2.
General Health Condition of the Participants.
| Variable (n = 794) | Frequency | Percent | |
|---|---|---|---|
| Diabetes mellitus | Yes | 88 | 11 |
| No | 710 | 89 | |
| Hypertension | Yes | 104 | 13 |
| No | 694 | 87 | |
| Recurrent UTI | Yes | 167 | 21 |
| No | 630 | 79 | |
| Chronic cough | Yes | 120 | 15 |
| No | 678 | 85 | |
| Chat chewing | Yes | 128 | 16 |
| No | 670 | 84 | |
| Caffeine utilization | Yes | 702 | 88 |
| No | 96 | 12 | |
Obstetrical and Gynecological Characteristics of Participants
Seven hundred sixty-six percent (96%) ever became pregnant, 88% ever gave birth, and 59% became pregnant with a short interpregnancy interval (less than 2 years). More than a quarter (77.5%) of them had more than 4 pregnancies (Table 3).
Table 3.
Obstetrical and Gynecological Characteristics of Participants.
| Variable (n = 794) | Frequency | Percent | |
|---|---|---|---|
| Ever had pregnancy | Yes | 766 | 96 |
| No | 32 | 4 | |
| Number of pregnancy | 4 and less than | 594 | 77.5 |
| 5 and More | 249 | 32.5 | |
| Ever had child birth | Yes | 674 | 88 |
| No | 92 | 12 | |
| Mode of delivery at first child birth. | Vaginal delivery | 657 | 97.5 |
| Cesarean section | 17 | 2.5 | |
| Ever had vaginal delivery | yes | 662 | 98 |
| No | 12 | 2 | |
| Inter-pregnancy interval | <2 years | 452 | 59 |
| ≥2 years | 314 | 41 | |
| Home delivery | Ever at home | 148 | 22 |
| Never delivered | 526 | 78 | |
| Episiotomy during delivery | Yes | 252 | 38 |
| No | 410 | 62 | |
| Cesarean section delivery | Yes | 12 | 1.5 |
| No | 786 | 98.5 | |
| Number of vaginal delivery | <5 deliveries | 298 | 45 |
| ≥5deliveries | 364 | 55 | |
| Age at last delivery | ≤36 years | 485 | 72 |
| >36 years | 189 | 28 | |
| Menopause | Yes | 168 | 21 |
| No | 630 | 79 | |
Magnitude of Pelvic Floor Dysfunction
This study surveyed 4 different pelvic floor dysfunction. Among 798 participants, three hundred three 37.7% [(95% CI (31.7-42.5)] reported at least one type of pelvic floor disorder during the study period, and two hundred thirty 28.8% (22.6-37.5) reported the co-occurrence of 2 or more pelvic floor disorders. Overactive bladder is the most commonly reported form of PFD, with 135 of all participants reporting symptoms (See Figure 1).
Figure 1.
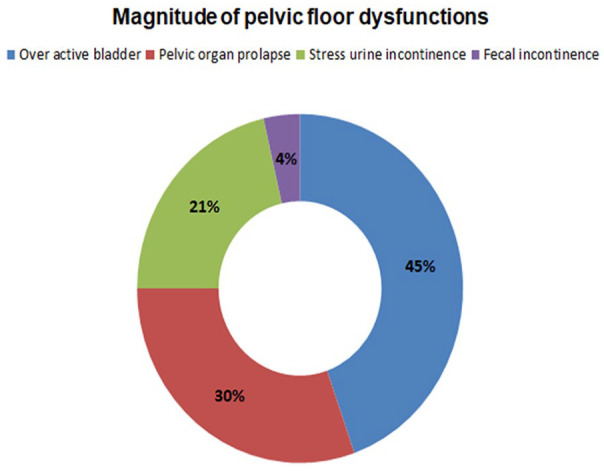
Magnitude of pelvic floor dysfunction.
Factors Associated With Pelvic Floor Dysfunction
In bivariate logistic regression, all variables were evaluated independently, and variables with a significance level of less than 0.2 were included in the multivariate logistic regression analysis. The Hosmer-Lemshow model fitness test was passed (sig. = 0.236). For collinearity detection, heavy labor work, number of childbirths, and number of vaginal deliveries were all factored into linear logistic regression. The variation inflation factor for the number of pregnancy, parity, and vaginal child birth was 3.214, 10.113, and 7.802, respectively.
As a result, the number of vaginal births was included in the regression model for further analysis with the other variables. Four variables in a multivariate logistic regression showed an effect associated with pelvic floor dysfunction. In this study, age 55 years [(AOR = 2.1; 95% CI: (1.52-6.42)], history of heavy labor work 10 years [(AOR = 3.21; 95% CI: (1.86-5.72)] and 5 vaginal child births [(AOR = 4.03; 95% CI: (2.20-8.27)] respectively (Table 4).
Table 4.
Factors Associated with Pelvic Floor Dysfunction.
| Variables (N = 798) | Pelvic floor dysfunction | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|
| Yes (%) | No (%) | |||
| Age | ||||
| 15-24 | 29 | 99 | 1 | 1 |
| 25-34 | 81 | 166 | 1.66 (1.08-4.56) | 1.17 (0.55-3.93) |
| 35-44 | 90 | 133 | 2.31 (1.04-6.39) | 1.8 (0.95-6.69) |
| 45-54 | 66 | 38 | 5.92 (0.98-10.03) | 3.34 (0.87-8.94) |
| 55+ | 42 | 48 | 2.99 (1.23-7.18) | 2.1 (1.52-6.42) |
| Educational status | ||||
| Un able to read and write | 116 | 142 | 1.05 (0.76-3.84) | 0.78 (0.35-2.09) |
| Able to read and write | 89 | 102 | 1.12 (1.08-5.39) | 1.36 (0.87-5.52) |
| Primary complete (1-8) | 56 | 80 | 0.9 (0.27-4.33) | 0.67 (0.25-9.08) |
| Secondary complete (9-12) | 49 | 63 | 1 | 1 |
| Marital status | ||||
| Never married | 11 | 50 | 0.28 (0.18-2.01 | 0.48 (0.27-6.39) |
| Married and living together | 222 | 399 | 0.69 (0.32-3.26) | 0.89 (0.46-9.41) |
| Divorced/separated | 58 | 30 | 2.42 (1.14-6.52) | 2.03 (0.95-8.04) |
| Widowed | 12 | 15 | 1 | 1 |
| Occupation | ||||
| House wife | 165 | 268 | 1.30 (0.98-2.98) | 1.86 (0.98-8.91) |
| Employee | 43 | 70 | 1.29 (0.87-2.57) | 1.02 (0.37-5.07) |
| Merchant | 73 | 104 | 1.48 (0.94-9.16) | 2.31 (0.68-8.10) |
| Other (students, daily labor) | 27 | 57 | 1 | 1 |
| Heavy labor work | ||||
| <10 years | 45 | 75 | 1 | 1 |
| ≥11 years | 201 | 78 | 4.29 (2.04 -7.08) | 3.21 (1.86-5.72) |
| History of chronic cough | ||||
| Yes | 69 | 51 | 1.71 (1.13-3.47) | 2.13 (1.95-4.28) |
| No | 299 | 379 | 1 | 1 |
| Number of vaginal delivery | ||||
| <5 deliveries | 88 | 210 | 1 | 1 |
| ≥5 deliveries | 215 | 149 | 3.44 (2.08-7.18 | 4.03 (2.20-8.27) |
| Being Menopause | ||||
| Yes | 99 | 69 | 4.67 (2.75-7.84) | 3.61 (2.04-9.98) |
| No | 148 | 482 | 1 | 1 |
Discussion
The total prevalence of pelvic floor dysfunction was found to be 37 [95% CI]. This result was lower than the results of studies conducted in Australia (47.2%) and Turkey (67.5) consecutively.22,23 The distinction may be elucidated by the difference in socio-demographic and sample size. 24 In other sayings, the magnitude of PFD in our study was greater than in studies in Bangladesh (35.5%), America (25%), Asian countries (21%), Kersa (20.5%), and Dabat (20.5%).25-28 The variation might be due to the difference in the study population, which include only post-menopausal women, a higher proportion of grand-multipara and more than 5 vaginal deliveries within this study related to studies from Saudi Arabia and Australia. 29
The magnitude of PFD in our study was greater than in previous studies conducted in Gurage Zone and Kersa, which could be attributed to differences in daily labor work and walking distance.15,27
Pelvic organ prolapse and urine incontinency were responsible for 21% and 30% of the cases, respectively. The result was slightly higher than the average magnitude found in Walker and Gunasekera review of the prevalence and risk factors of pelvic organ prolapse and incontinence in developing countries, which was 28.7% for UI and 19.7% for POP. According to the review, the prevalence of SUI ranges from 70.8% to 56.4%, with the current study falling in the middle. 30
Furthermore, this finding is consistent with a systematic review and meta-analysis conducted in LMIC countries. 31 The reason might be, the current study’s pelvic organ prolapse questions were highly correlated with the second or more severe stage of POP based on the POP quantification Test, and the questions had higher specificity. 4 In addition to the aforementioned aspects, such problems are unpleasant. As a result, most women are reluctant to discuss their health. The reason for the low proportion of symptomatic Pelvic organ prolapse compared to studies that used the target woman of pelvic organ prolapse assessment could be this. 32
According to the severity index, 8.4% had moderate to severe involuntary urine leakage, while 26% had mild incontinence. 26 The prevalence of OAB and strain urine leakage remained at 45% and 21%, respectively, with 15% of women having miscellaneous type. This finding is largely reliable, as a study published in reported an 8.7% prevalence for moderate or severe urine leakage and a 12.2% occurrence for stress urinary incontinence. 19
The magnitude of urge incontinence and miscellaneous incontinence was 1.6% and 6.9% lower, respectively, than study conducted in Spain. This difference may be because above study excluded advanced age women, women with more than 4 vaginal deliveries, and women with a history of both vaginal child birth and cesarean delivery frequently at an increased risk of pelvic floor dysfunctions. This was in line with 2 studies conducted in Ethiopia, Sweden, and a systematic review conducted in low- and middle-income countries.26,30,33,34
Heavy labor work more than 10 years and chronic cough increase intra-abdominal pressure, which is believed to play a role in the pathogenesis of PFD (particularly POP). 34 In the our study, more than 50% of the women were rural residents, and most of them do heavy labor work, such as woodworking, Carrying heavy objects from house to market and from market to house, which square measure nerve-wracking activities. 35
In our study, mothers who had 5 or more vaginal child birth were 4 times more likely to have PFD than those who did not have vaginal deliveries. This compares to a study done in the Gurage Zone which showed that repeated vaginal deliveries vaginal deliveries were associated with PFD linked to 4 or fewer vaginal deliveries. 15 Similarly, studies conducted in the US, Saint Joseph Hospital of Kinshasa and Bahirdar reported that 4 or more repeated delivery women had a higher risk of developing PFD than nulliparous woman.28,34,36 Also showed that vaginal mode of delivery was significantly associated with an increased risk of incontinence and pelvic organ Prolapse when compared with women delivered by cesarean section only. 37
The other approaching study of 5000 black women in sub-Saharan Africa found that women with a history of vaginal child birth were about 2 time more likely to report urinary incontinence. 38 The relation of frequent vaginal delivery with pelvic floor dysfunction may result from direct trauma to the pelvic muscles and connective tissue. 39 With repeated vaginal deliveries, direct injury to the pelvic muscles, connective tissue, and nerve injury from trauma and overstraining can lead to a pelvic floor disorder.
In our study, post-menopausal women stated more pelvic floor dysfunction. Menopausal women are 3 times more likely to develop pelvic floor dysfunction than their counterparts. The physiological aging process, the degenerative process and hypoestrogenism produce urogenital atrophy and weaken the supporting structures of the pelvic organs. 40 This might aggravates the risk of pelvic floor dysfunction. Reproductive hormones can be critical to normal urinary tract functions and the preservation of the connective tissues that suspends the pelvic organs. 41 This could brief the link between pelvic floor dysfunctions and being menopause. We recommend estrogen supplemental therapy for postmenopausal women. Furthermore, health institutions and other stakeholders should promote and provide health education about Kegel exercises for women. Kegel exercises can reduce the risk of pelvic floor dysfunction by strengthening the pelvic floor muscles. 42
Limitations of the Study
This study focused on interview-based pelvic floor disorder detection, which may not quantify the mild degree of pelvic organ prolapse. Therefore, researcher better give attention on clinical examination of pelvic floor dysfunction experienced care providers detect all degree of pelvic floor disorders, even though it requires high budget allocation and experienced human resources.
Conclusion and Recommendations
The magnitude of pelvic floor dysfunction was greater than other previous conducted studies in Ethiopian. Workload, frequent vaginal childbirth, chronic cough, and menopause were all related to pelvic floor dysfunction. In collaboration with regional and zonal health departments, screening and treatment of pelvic floor disorders should be prioritized.
Furthermore, health education on Kegel aerobics and support for family planning may be beneficial. We forward family planning, regular screening campaigns, and connect them to health facilities for further diagnosis and treatment of the problem to the local government and other shareholders. Provide professional education for health workers on common risk factors for pelvic floor dysfunctions, as well as social stigma reduction.
Finally, this study discovered that women with low knowledge are more affected than those knowledgeable of pelvic floor disorder and economic constraints. So, the government, in collaboration with non-governmental organizations, should prioritize community awareness and free health care provision as a project campaign.
Acknowledgments
My heartfelt thanks go to the Assosa University College of Health Science for providing me with the opportunity to conduct this research. Next, I want to thank my family for their unwavering support. Finally, I’d like to thank everyone who has helped me throughout this study, from the beginning to the end. It is clear as a result of all of this research.
Footnotes
Contributors: All authors equally contribute for all works required to conduct this research
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding was raised by Assosa University
Ethical Considerations: Before starting data collection ethical clearance taken from Ethics review Committee of institution. Having a formal letter, a supportive letter was distributed to the respective offices and kebeles. Oral and written consent was obtained after explaining the objective of the research. The information obtained from the respondents was identified by their code numbers for confidentiality. There was no risk and no direct benefit to the participants for their participation.
Consent for Publication: Not applicable for this section.
Availability of Data and Materials: The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
ORCID iD: Hunduma Dina Hambisa  https://orcid.org/0000-0002-9379-211X
https://orcid.org/0000-0002-9379-211X
References
- 1.Agarwal BK, Agarwal N.Urinary incontinence: prevalence, risk factors, impact on quality of life and treatment seeking behaviour among middle aged women. Int Surg J. 2017;4(6):1953-1958. [Google Scholar]
- 2.Rogers RG, Pauls RN, Thakar R, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for the assessment of sexual health of women with pelvic floor dysfunction. Int Urogynecol J. 2018;29(5):647-666. [DOI] [PubMed] [Google Scholar]
- 3.Prolapse PO.ACOG practice bulletin, number 214. Obstet Gynecol. 2019;134(5):126-142. [DOI] [PubMed] [Google Scholar]
- 4.Grzybowska ME, Futyma K, Wydra D.Identification of the pelvic organ prolapse/Incontinence Sexual Questionnaire-iuga revised (PISQ-IR) cutoff scores for impaired sexual function in women with pelvic floor disorders. J Clin Med. 2019;9(1):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Billecocq S.An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for the conservative and non-pharmacological management of female pelvic floor dysfunction. Prog Urol. 2019;29(4):183-208. [DOI] [PubMed] [Google Scholar]
- 6.Barber MD, Maher C.Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J. 2013;24(11):1783-1790. [DOI] [PubMed] [Google Scholar]
- 7.Zizzi PT, et al. Women’s pelvic floor muscle strength and urinary and anal incontinence after childbirth: a cross-sectional study. Rev Esc Enferm USP. 2017;51(3): 4-12. [DOI] [PubMed] [Google Scholar]
- 8.Ko KJ, Lee K-S.Current surgical management of pelvic organ prolapse: Strategies for the improvement of surgical outcomes. Investig Clin Urol. 2019;60(6):413-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Adefris M, Abebe SM, Terefe K, et al. Reasons for delay in decision making and reaching health facility among obstetric fistula and pelvic organ prolapse patients in Gondar University hospital, Northwest Ethiopia. BMC Womens Health. 2017;17(1):1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Laganà SA, Rosa LV, Rapisarda MA, et al. Pelvic organ prolapse: the impact on quality of life and psychological well-being. J Psychosom Obstet Gynaecol. 2018;39(2):164-166. [DOI] [PubMed] [Google Scholar]
- 11.Espuña-Pons M, Fillol M, Pascual AM, et al. Pelvic floor symptoms and severity of pelvic organ prolapse in women seeking care for pelvic floor problems. Eur J Obstet Gynecol Reprod Biol. 2014;177:141-145. [DOI] [PubMed] [Google Scholar]
- 12.Kim JI, Zhu D, Davila J, et al. Female sexual dysfunction as measured by low sexual frequency is associated with lower socioeconomic status: an Analysis of the National Health and Nutrition Examination Survey (NHANES), 2007-2016. J Sex Med. 2022;19(1):90-97. [DOI] [PubMed] [Google Scholar]
- 13.Dewan PJ, Agarwal A.Prevalence of pelvic organ prolapse and its relationship to associated risk factors like age, parity and mode of delivery in a rural setting in Uttar Pradesh, India. IJSS J Surg. 2021;7(5):24-28. [Google Scholar]
- 14.Borsamo A, Oumer M, Asmare Y, Worku A.Factors associated with delay in seeking treatment among women with pelvic organ prolapse at selected general and referral hospitals of southern Ethiopia, 2020. BMC Womens Health. 2021;21(1):1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beketie ED, Tafese WT, Assefa ZM, et al. Symptomatic pelvic floor disorders and its associated factors in south-central Ethiopia. PLoS One. 2021;16(7):e0254050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rogers RG, Rockwood TH, Constantine ML, et al. A new measure of sexual function in women with pelvic floor disorders (PFD): the Pelvic Organ Prolapse/Incontinence Sexual Questionnaire, IUGA-Revised (PISQ-IR). Int Urogynecol J. 2013;24(7):1091-1103. [DOI] [PubMed] [Google Scholar]
- 17.Kammerer-Doak D, Rizk DE, Sorinola O, Agur W, Ismail S, Bazi T.Mixed urinary incontinence: international urogynecological association research and development committee opinion. Int Urogynecol J. 2014;25(10):1303-1312. [DOI] [PubMed] [Google Scholar]
- 18.Hoffman BL, Bradshaw KD, Corton MM, et al. Williams Gynecology. McGraw-Hill Education; 2016. [Google Scholar]
- 19.Handa V, Brubaker L, Eckler K.Urinary Incontinence and Pelvic Organ Prolapse Associated With Pregnancy and Childbirth. UpToDate. UpToDate; 2014. [Google Scholar]
- 20.Blomquist JL, Carroll M, Muñoz A, Handa VL.Pelvic floor muscle strength and the incidence of pelvic floor disorders after vaginal and cesarean delivery. Am J Obstet Gynecol. 2020;222(1):62.e1-62.e8. [DOI] [PubMed] [Google Scholar]
- 21.Freeman A, Menees S.Fecal incontinence and pelvic floor dysfunction in women: a review. Clin Gastroenterol. 2016;45(2):217-237. [DOI] [PubMed] [Google Scholar]
- 22.Kepenekci I, Keskinkilic B, Akinsu F, et al. Prevalence of pelvic floor disorders in the female population and the impact of age, mode of delivery, and parity. Dis Colon Rectum. 2011;54(1):85-94. [DOI] [PubMed] [Google Scholar]
- 23.Zeleke BM, Bell RJ, Billah B, Davis SR.Symptomatic pelvic floor disorders in community-dwelling older Australian women. Maturitas. 2016;85:34-41. [DOI] [PubMed] [Google Scholar]
- 24.Uustal Fornell E, Wingren G, Kjølhede P. Factors associated with pelvic floor dysfunction with emphasis on urinary and fecal incontinence and genital prolapse: an epidemiological study. Acta Obstet Gynecol Scand. 2004;83(4):383-389. [DOI] [PubMed] [Google Scholar]
- 25.Islam RM, Bell RJ, Billah B, Hossain MB, Davis SR.The prevalence of symptomatic pelvic floor disorders in women in Bangladesh. Climacteric. 2016;19(6):558-564. [DOI] [PubMed] [Google Scholar]
- 26.Megabiaw B, Adefris M, Rortveit G, et al. Pelvic floor disorders among women in Dabat district, northwest Ethiopia: a pilot study. Int Urogynecol J. 2013;24(7):1135-1143. [DOI] [PubMed] [Google Scholar]
- 27.Dheresa M, Worku A, Oljira L, Mengiste B, Assefa N, Berhane Y.One in five women suffer from pelvic floor disorders in Kersa district Eastern Ethiopia: a community-based study. BMC Womens Health. 2018;18(1):1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wu JM, Vaughan CP, Goode PS, et al. Prevalence and trends of symptomatic pelvic floor disorders in US women. Obstet Gynecol. 2014;123(1):141-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Trutnovsky G, Guzman-Rojas R, Martin A, et al. Pelvic floor dysfunction—does menopause duration matter? Maturitas. 2013;76(2):134-138. [DOI] [PubMed] [Google Scholar]
- 30.Walker GJ, Gunasekera P.Pelvic organ prolapse and incontinence in developing countries: review of prevalence and risk factors. Int Urogynecol J. 2011;22(2):127-135. [DOI] [PubMed] [Google Scholar]
- 31.Islam RM, Oldroyd J, Rana J, Romero L, Karim MN.Prevalence of symptomatic pelvic floor disorders in community-dwelling women in low and middle-income countries: a systematic review and meta-analysis. Int Urogynecol J. 2019;30(12):2001-2011. [DOI] [PubMed] [Google Scholar]
- 32.Madhu C, Swift S, Moloney-Geany S, Drake MJ.How to use the pelvic organ prolapse quantification (POP-Q) system? Neurourol Urodyn. 2018;37(S6):S39-S43. [DOI] [PubMed] [Google Scholar]
- 33.Miedel A, Tegerstedt G, Mæhle-Schmidt M, Nyrén O, Hammarström M.Nonobstetric risk factors for symptomatic pelvic organ prolapse. Obstet Gynecol. 2009;113(5):1089-1097. [DOI] [PubMed] [Google Scholar]
- 34.Asresie A, Admassu E, Setegn T.Determinants of pelvic organ prolapse among gynecologic patients in Bahir dar, North West Ethiopia: a case–control study. Int J Womens Health. 2016;8:713-719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sodagar N, Ghaderi F, Ghanavati T, et al. Related Risk Factors for Pelvic Floor Disorders in Postpartum Women: A Cross-sectional Study. [Google Scholar]
- 36.Kayembe AT, et al. Factors associated with genital prolapse to Saint Joseph Hospital of Kinshasa. Pan Afr Med J. 2021;40:234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sujindra E, Himabindu N, Sabita P, Bupathy A.Determinants and treatment modalities of uterovaginal prolapse: A retrospective study. Indian J Health Sci Biomed Res. 2015;8(1):36-40. [Google Scholar]
- 38.Ojengbede OA, Morhason-Bello IO, Adedokun BO, Okonkwo NS, Kolade CO.Prevalence and the associated trigger factors of urinary incontinence among 5000 black women in sub-Saharan Africa: findings from a community survey. BJU Int. 2011;107(11):1793-1800. [DOI] [PubMed] [Google Scholar]
- 39.Hoffman BL, Bradshaw KD, Corton MM, et al. Williams Gynecology. McGraw-Hill Education; 2022. [Google Scholar]
- 40.Hoffman BL.Williams Gynecology, 3rd ed.McGraw-Hill Education; 2016. [Google Scholar]
- 41.Padubidri V, Daftary SN.Shaw's Textbook of Gynecology E-book. Elsevier Health Sciences; 2014. [Google Scholar]
- 42.Kashanian M, Ali SS, Nazemi M, Bahasadri S.Evaluation of the effect of pelvic floor muscle training (PFMT or Kegel exercise) and assisted pelvic floor muscle training (APFMT) by a resistance device (Kegelmaster device) on the urinary incontinence in women “comparison between them: a randomized trial. Eur J Obstet Gynecol Reprod Biol. 2011;159(1):218-223. [DOI] [PubMed] [Google Scholar]


