Abstract
INTRODUCTION
We compared the ranking of Alzheimer's disease and related dementia (ADRD) among the leading causes of death (LCODs) between those according to the National Center for Health Statistics (NCHS) and the World Health Organization (WHO) lists by sex.
METHOD
The number of deaths in each LCOD category was obtained from CDC WONDER.
RESULTS
According to the WHO list, ADRD was the second LCOD from 2005 to 2013, the first from 2014 to 2020, and the third in 2021, respectively, for women and was the second in 2018 and 2019, the third in 2020, and the fourth in 2021, respectively, for men. According to the NCHS list, Alzheimer's disease was the fourth in 2019 and 2020 for women and was the seventh from 2016 to 2019 for men.
DISCUSSION
The ranking of ADRD among the LCODs according to the WHO list was higher than those according to the NCHS list.
Keywords: Alzheimer's disease and related dementia, leading causes of death, National Center for Health Statistics, ranking list, World Health Organization
1. INTRODUCTION
Leading causes of death (LCODs) is a commonly used health metric that provides insight into the relative impact of various diseases on population health. The National Center for Health Statistics (NCHS) in the United States publishes Deaths: Leading Causes every year, and Alzheimer's disease (AD) was the sixth LCOD for all ages and the fifth LCOD for people aged 65 years and older in 2019. 1 However, the ranking list used by the NCHS has two limitations that understate the mortality burden of Alzheimer's disease and related dementia (ADRD). First, the NCHS list uses broad categories (heart disease, cancer, and accidents) for ranking, which include heterogenous categories with different etiologies and countermeasures. For example, the cancer category includes 89 three‐character International Classification of Diseases Tenth Revision (ICD‐10) codes. By contrast, the AD category has one three‐character ICD‐10 code G30 in the NCHS list. This leads to an asymmetric comparison between cancer and AD. 2 , 3 Second, as listed on page 346 in the 2021 Alzheimer's Disease Facts and Figures, the AD category in the NCHS list does not include other dementia, resulting in the underestimation of the ADRD mortality burden. In 2019, 150,343 people died from other dementia, which was more than those who died from AD (121,499 in 2019). 4
To address the aforementioned limitations, the World Health Organization (WHO) used a modified ranking list to split broad categories into more specific categories: 9 for heart disease, 16 for cancer, and 12 for accidents. Furthermore, the WHO list provides a more comprehensive ADRD category, which includes the ICD‐10 code G30, ICD‐10 code F01 (vascular dementia), and F03 (unspecified dementia). 5 However, only the ICD‐10 code G30 is included in the NCHS list. 1 Several studies have compared the rankings of LCODs between those according to the NCHS and the WHO lists. 6 , 7 , 8 , 9 However, no study has examined the ranking of ADRD among LCODs according to the WHO list in the United States. Furthermore, the effect of the coronavirus disease 2019 (COVID‐19) pandemic on the ranking of ADRD remains unknown. Therefore, this study compared the ranking of ADRD among LCODs between those according to the WHO and the NCHS lists in the United States from 1999 to 2021.
2. METHODS
The data on the number of deaths in each category according to the NCHS and the WHO lists were obtained from the Wide‐ranging Online Data for Epidemiologic Research system maintained by the Center for Disease Control and Prevention (CDC WONDER) from 1999 to 2021. 10 We selected 1999 as the starting year because the ICD‐10 classification scheme was launched in the United States in 1999. The ranking was determined according to the number and proportion of deaths in each category. This method was used by the NCHS in annual report. 1 We used the bump chart dashboard with filters of two lists and demographic characteristics (sex and age) to visualize the yearly changes in the ranks of ADRD and AD according to two lists. The website of the dashboard can be accessed at:https://public.tableau.com/app/profile/robert.lu/viz/USADRDLeadingCOD/bumpchart
The permutation test was used to examine the differences in the rank of ADRD according to the WHO list and the rank of AD in the NCHS list for recent 10 years (from 2012 to 2021). This study used publicly available mortality data. This study was approved by the Institutional Review Board of National Cheng Kung University Hospital.
RESEARCH IN CONTEXT
Systemic Review: Our search of the PubMed database for studies on leading causes of death (LCODs) revealed fewer than 10 studies comparing the rankings of LCODs between different ranking lists. However, we did not find any study that specifically examined the differences in the ranking of Alzheimer's disease and related dementia (ADRD) as an LCOD according to different ranking lists.
Interpretation: According to the World Health Organization (WHO) list, which divides broad categories (heart disease, cancer, and accidents) into more specific categories and a broader definition of ADRD, the ranking of ADRD from 1999 to 2021 was higher than the ranking of AD based on the list used by the National Center for Health Statistics (NCHS). ADRD was the second LCOD from 2008 to 2019 according to the WHO list and AD was the sixth LCOD from 2007 to 2019 according to the NCHS list.
Future Direction: Additional studies are required to use the WHO list to reveal the ranking of ADRD as an LCOD for various racial and ethnic groups and states or counties to identify groups or regions with a relatively high mortality burden from ADRD.
3. RESULTS
We identified 60,375,303 people who died between 1999 and 2021. Of them, 2,212,174 died from ADRD and 1,991,178 died from AD. The proportion of death of 10 LCODs from 1999 to 2021 for both sexes, women, and men are illustrated in Tables S1, S2, and S3, respectively, according to the WHO list and Tables S4, S5, and S6, respectively, according to the NCHS list.
According to the WHO list, ADRD was the third LCOD from 2002 to 2004, the second from 2005 to 2013, the first from 2014 to 2020, and the third in 2021 for women (Figure 1A) and was the third LCOD between 2012 and 2017, the second in 2018 and 2019, the third in 2020, and the fourth in 2021 for men (Figure 2A).
FIGURE 1.
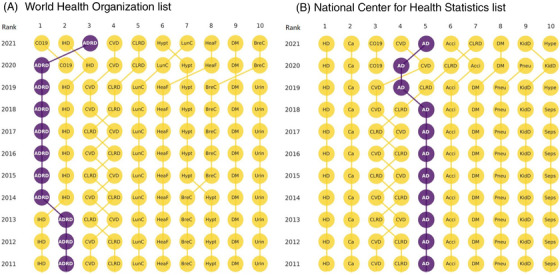
Ranking of leading causes of death in the United States according to two lists, women of all ages. (A) World Health Organization list. (B) National Center for Health Statistics list.
FIGURE 2.
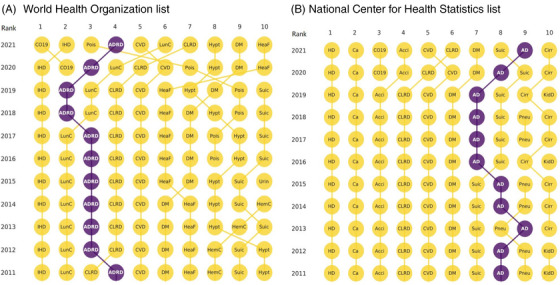
Ranking of leading causes of death in the United States according to two lists, men of all ages. (A) World Health Organization list. (B) National Center for Health Statistics list.
According to the NCHS list, AD was the fifth LCOD from 2002 to 2018, the fourth in 2019 and 2020, and the fifth in 2021 for women (Figure 1B) and was the seventh LCOD from 2016 to 2019, the eighth in 2020, and the ninth in 2021 for men (Figure 2B).
According to the permutation test, the rank of ADRD according to the WHO list was 3.5 higher than the rank of AD according to the NCHS list among women (p = 0.0001) and was 4.8 higher among men (p < 0.0001).
4. DISCUSSION
The findings of this national population‐based study, which revealed the LCODs over a 23‐year span in the United States, indicate that the ranking of ADRD among LCODs according to the WHO list was higher than that according to the NCHS list. Notably, ADRD was the first LCOD from 2014 to 2020 for women of all ages.
The first reason for the differences in ranking of ADRD among the LCODs between the two lists can be attributed to the division of broader categories (heart disease, cancer, and accidents) into more specific subcategories in the WHO list. As number of deaths in the subcategories of heart disease, cancer, and accidents decreased, the relative rank would be lower. The number of deaths in the ischemic heart disease subcategory in the WHO list was approximately two‐thirds of the number of deaths in the heart disease broad category in the NCHS list, and the number of deaths in the lung cancer subcategory in the WHO list was approximately one‐fourth of the number of deaths in the cancer broad category in the NCHS list. Therefore, the number of deaths from ADRD exceeded the number of deaths from lung cancer among women in most study years, leading to its higher ranking.
The second reason for the differences in the ranking of ADRD among LCODs was the use of a broader category for ADRD in the WHO list, which included approximately twice the number of deaths as the AD category in the NCHS list in most of the study years. This is the trade‐off between sensitivity and specificity. The NCHS approach maximizes specificity whilst sacrificing sensitivity. The WHO approach does the reverse.
Because the NCHS aimed to reflect the effect of aging on the mortality burden, the NCHS used only the number and percentage of deaths to determine the ranking of LCODs. The increase in the ranking of ADRD among LCODs over the past two decades corresponds with aging of the US society, particularly because the Baby Boomer generation began turning 65 years since 2010, making them a primary driver of increase of number of deaths from ADRD.
The findings of this study should be interpreted with caution because of the limitations. First, the ranking was determined on the basis of the number of deaths without calculating cause‐specific mortality rates. Therefore, we could not infer the increase in the ranking as the increase in the risk of death. Second, the changes in the rank of ADRD might not correspond to changes in the proportion of ADRD. For example, ADRD was the second LCOD for women in 2013 according to the WHO list, with a proportion of 12.1%, and was the first LCOD from 2014 to 2020; however, the proportions were lower than 12.1% (Table S2). Scholars have reminded us that the rankings of LCODs are just the starting point to suggest further detailed analysis of specific causes of death. 2 , 5
5. CONCLUSION
The WHO list, which overcomes some of the limitations of the NCHS list, provides a different profile of ADRD ranking, which can be a supplementary in addition to the rankings according to the NCHS list to reveal more comprehensive information regarding the ADRD mortality burden for policy decision‐making. The ranking of ADRD among the LCODs according to the WHO list was higher than those according to the NCHS list. Additional studies using the WHO list are required to examine the ranking of ADRD among LCODs for various racial and ethnic groups and states or counties and to identify states and regions with a relatively high mortality burden from ADRD.
CONFLICT OF INTEREST STATEMENT
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as potential conflicts of interest. Author disclosures are available in the supporting information.
CONSENT STATEMENT
This study used public access open data, therefore the consent was not necessary.
Supporting information
Supporting Information
Supporting Information
ACKNOWLEDGMENTS
The authors thank Ms. Pai‐Huan Lin for the data analysis. Dr. Lu was funded by the Ministry of Science and Technology, Taiwan (grant number: MOST 111‐2314‐B‐006‐030). The funders had no role in the design of the study, collection and analysis of data, decision to publish, or preparation of the manuscript.
Tai S‐Y, Chi Y‐C, Lo Y‐T, Chien Y‐W, Kwachi I, Lu T‐H. Ranking of Alzheimer's disease and related dementia among the leading causes of death in the US varies depending on NCHS or WHO definitions. Alzheimer's Dement. 2023;15:e12442. 10.1002/dad2.12442
Shu‐Yu Tai and Ying‐Chen Chi are joint first authors and contribution equally to this work.
REFERENCES
- 1. Heron M. Deaths: Leading causes for 2019. National Center for Health Statistics; 2021. Accessed on July 26, 2021. https://www.cdc.gov/nchs/data/nvsr/nvsr70/nvsr70‐09‐508.pdf. National Vital Statistics Reports. [PubMed] [Google Scholar]
- 2. Anderson RN. Coding and classifying causes of death: trends and international differences. In: Richard G Rogers RG, Crimmins EM, eds. International Handbook of Adult Mortality. Springer; 2011:467‐489. Accessed January 1, 2011. https://link.springer.com/chapter/10.1007/978‐90‐481‐9996‐9_22 [Google Scholar]
- 3. Tai SY, Lu TH. Why was COVID‐19 not the leading cause of death in the United States in 2000? Rethinking the ranking list. Am J Public Health. 2021;111:2096‐2099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Alzheimer's Association . 2021 Alzheimer's disease facts and figures. Alzheimer Dement. 2021;17(3):327–406. [DOI] [PubMed] [Google Scholar]
- 5. Becker R, Silvi J, Ma Fat D, L'Hours A, Laurenti R. A method for deriving leading causes of death. Bull World Health Org. 2006;84:297‐304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Griffiths C, Rooney C, Brock A. Leading causes of death in England and Wales: how should we group causes? Health Stat Q. 2005;28:6‐17. [PubMed] [Google Scholar]
- 7. Hsiao AJ, Chen LH, Lu TH. Ten leading causes of death in Taiwan: a comparison of two grouping lists. J Formos Med Assoc. 2015;114:679‐680. [DOI] [PubMed] [Google Scholar]
- 8. Gjertsen F, Bruzzone S, Griffiths CE. Burden of suicide presented as one of the leading causes of death: uncover facts or misrepresent statistics? J Glob Health. 2019;9(1):010401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tai SY, Cheon S, Yamaoka Y, Chien YW, Lu TH. Changes in the rankings of leading causes of death in Japan, Korea, and Taiwan from 1998 to 2018: a comparison of three ranking lists. BMC Public Health. 2022;22(1):1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. The Centers for Disease Control and Prevention . Wide‐ranging ONline Data for Epidemiologic Research (CDC WONDER). Accessed 2023. https://wonder.cdc.gov/ [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information
Supporting Information


