Abstract
COVID-19 has exposed major weaknesses in the healthcare settings. The surge in COVID-19 cases increases the demands of health care, endangers vulnerable patients, and threats occupational safety. In contrast to a hospital outbreak of SARS leading to a whole hospital quarantined, at least 54 hospital outbreaks following a COVID-19 surge in the community were controlled by strengthened infection prevention and control measures for preventing transmission from community to hospitals as well as within hospitals. Access control measures include establishing triage, epidemic clinics, and outdoor quarantine stations. Visitor access restriction is applied to inpatients to limit the number of visitors. Health monitoring and surveillance is applied to healthcare personnel, including self-reporting travel declaration, temperature, predefined symptoms, and test results. Isolation of the confirmed cases during the contagious period and quarantine of the close contacts during the incubation period are critical for containment. The target populations and frequency of SARS-CoV-2 PCR and rapid antigen testing depend on the level of transmission. Case investigation and contact tracing should be comprehensive to identify the close contacts to prevent further transmission. These facility-based infection prevention and control strategies help reduce hospital transmission of SARS-CoV-2 to a minimum in Taiwan.
Keywords: Infection prevention and control, Access control, Isolation, SARS-CoV-2 testing, Case investigation, Contact tracing
Introduction
Coronavirus disease 2019 (COVID-19), emerging in December 2019 from China, has become pandemic within 3–4 months and affected more than 755 million confirmed cases, including more than 6 million deaths, as of 31 January 2023.1 COVID-19 exposed the weakness of national public health and healthcare infrastructure, and also threatened national economy and healthcare capacity. The impact of COVID-19 varied widely among countries or regions because the initial anti-epidemic interventions differed. For example, the US and Taiwan confirmed the first imported COVID-19 case on January 21, 2020. While 33 states and territories in the US had issued mandatory stay-at-home orders to control widespread community outbreaks as of April 1, 2020,2 Taiwan only reported 348 cases (1.46/100,000 population) as of April 3, 2020 and only 13.8% of them were indigenous cases.3 The Taiwan Central Epidemic Command Center (CECC) deployed containment strategies to reduce the impact of COVID-19 to a minimum,4, 5, 6, 7, 8 and achieved low excess deaths without city lockdown, workplace closures, or curfews.9 Therefore, proactive, strong, and decisive coordinated action is imperative at the global, national and institution levels.
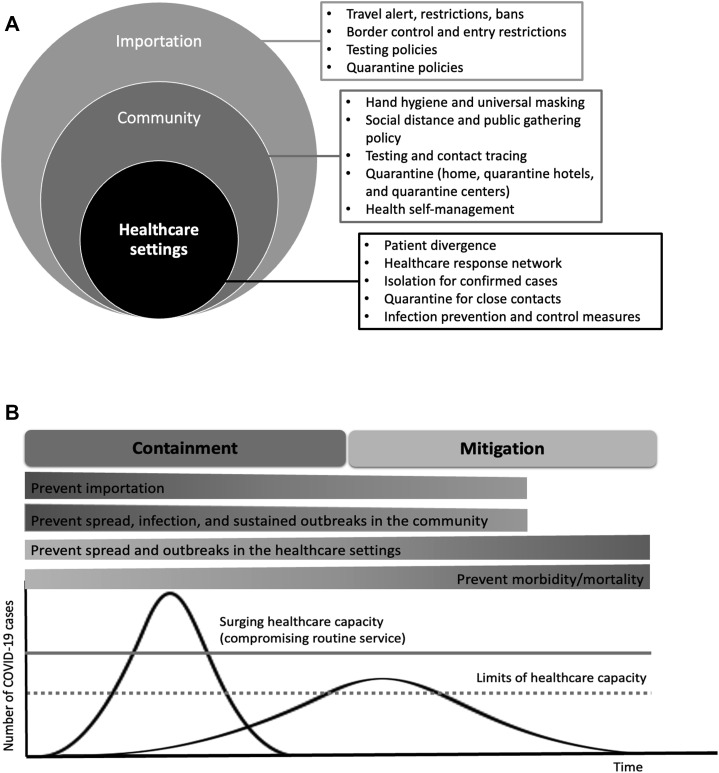
COVID-19 is highly transmissible from person to person via a respiratory route (mainly droplet transmission), direct contact of infected individuals (symptomatic, pre-symptomatic, or asymptomatic), or indirect contact of droplet- or secretion-contaminated environmental surfaces (fomite transmission).10 To effectively control the COVID-19 epidemic needs a bundle of active interventions. Fig. 1 shows the concept map of national strategies and key measures to combat COVID-19 in Taiwan. Before availability of etiology-specific resources, such as testing, vaccine, or antiviral therapy, non-pharmaceutical interventions (NPIs) are key measures for surviving at the first encounter of human and pathogen.11 The implemented NPIs include border control, which is only applicable to imported diseases, as well as transmission prevention in the community and healthcare settings.5 , 12, 13, 14 While public health measures aim to prevent and control spread of SARS-CoV-2 in the community, infection prevention and control (IPC) measures in the healthcare settings are an extension of public health interventions and important along the path of the COVID-19 pandemic. However, IPC in the healthcare settings can be a challenging and complicated task due to the segregation of vulnerable individuals who share common space and facilities. Furthermore, patients and their accompanying persons are not familiar with and prepared to do so in compliance with national and institution policies.
Figure 1.
The concept map of national strategies and key measures to combat COVID-19 in Taiwan. (A) Three tiers of containment strategies. (B) Timely adjustment by risk and resources from containment to mitigation.
In 2003, an outbreak of severe acute respiratory syndrome (SARS) in a regional hospital affecting 113 patients and 37 healthcare personnel (HCP) led to a whole hospital quarantined.15 That event was really a crisis of the Taiwanese government and the society.15 Therefore, the government and people in Taiwan become alert to the threat of emerging infectious diseases and willing to act coordinately.16 , 17 When facing a newly emerging infection with limited information, it is reassuring to have mechanisms to detect unusual events in place as a part of the IPC programs in hospitals. These mechanisms can help promptly detect the first encounter through the identification of unusual clusters of cases, as was demonstrated in a teaching hospital in Taiwan in March 2003.18 Furthermore, no HCP who involved in the care of the first five SARS cases was infected despite a substantial number of exposures which relied just on adherence to standard precautions in HCP's daily practice on the ground.18
Numerous COVID-19 outbreaks occurring in the healthcare settings can amplify transmission, endanger vulnerable patients, threaten occupational safety, and hamper the healthcare capacity.19, 20, 21, 22, 23 The surge in COVID-19 cases increases the demands of healthcare capacity while the capacity remains limited and difficult to promptly increase. In addition, hospitalized COVID-19 cases might transmit the disease to HCP and other inpatients, which would further compromise the healthcare systems. During the early phase of the COVID-19 pandemic, two case series in China estimated that the proportion of hospital-acquired SARS-CoV-2 infection was 44%.24 In a hospital in South Africa a single unsuspected COVID-19 case involved 80 HCP and 39 patients in 5 wards and an outside nursing home and dialysis unit.21 The large extent and a high mortality rate of 38.5% among infected patients underline the devastating consequences of hospital transmission of SARS-CoV-2. Moreover, the affected hospital services, wards, and buildings of hospital outbreaks had been temporarily closed to reduce transmission.21 , 22 , 25
Therefore, IPC policy, strategy and practice in the healthcare settings are paramount important for national security, HCP and patients’ health and safety, and preservation of healthcare capacity. In this article, we review the COVID-19 outbreaks in the healthcare settings and the corresponding IPC strategies to prevent intra-hospital spread of SARS-CoV-2 in Taiwan, and provide the rationale which may facilitate decision making at the institution level in the future.
Beyond personal protective equipment
Universal masking and appropriate personal protective equipment (PPE) are effective in reducing intra-hospital spread of SARS-CoV-2.26 However, a prospective cohort in the UK and the US demonstrated that HCP with adequate PPE remained at increased risk of acquiring COVID-19 and underscore the challenges in availability and appropriate use of PPE.27 Outbreak investigations have repeatedly demonstrated intra-hospital spread of SARS-CoV-2 despite fully equipped PPE.28 The findings indicate that healthcare systems should develop further IPC measures to protect HCP from COVID-19, along with ensuring PPE quality, availability, and appropriate use.
Intra-hospital spread of COVID-19 in Taiwan
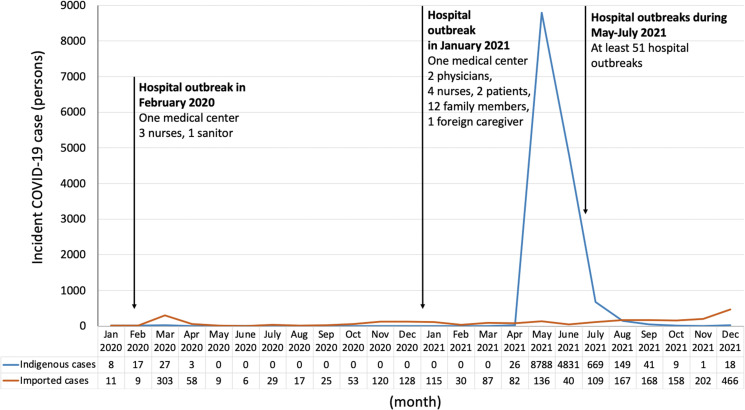
In Taiwan, the combination of NPIs and high degree of public adherence have contributed to successful COVID-19 control in the early stages of the COVID-19 pandemic.4 As of 30 April, 2021, only 1163 COVID-19 cases were reported, with >90% being imported cases.29 Nevertheless, hospital outbreaks were detected and increased parallel to the surge of COVID-19 cases in the community. Fig. 2 illustrates the number of confirmed COVID-19 cases and corresponding hospital outbreaks from January 2020 to July 2021 in Taiwan. The first intra-hospital outbreak occurred in February 2020 despite implementing triage, access control, and other measures.30 The index case, who was an inpatient without COVID-19 related symptoms and a travel, occupation, contact, and cluster (TOCC) history at admission, developed pneumonia and was diagnosed with COVID-19 by SARS-CoV-2 PCR 10 days later. A total of four HCP were infected subsequently. The second outbreak occurred at a designated COVID-19 hospital in January 2021, and involved 21 cases (6 HCPs, 2 patients and 13 accompanying persons).28 The index case triggering the investigation was a physician, who was wearing appropriate PPE while taking care of an imported case in a COVID-19 unit. The hospital immediately established the incident command team, and the Taiwan Centers for Disease Control (CDC) deployed personnel to facilitate outbreak management which included restriction of admissions and visitor access, PCR testing for all HCP, 14-day single-room quarantine of the close contacts, traffic control bundling, wards segregated based on the COVID-19 risk, and thorough environmental cleaning and disinfection.
Figure 2.
Number of COVID-19 cases by date of report and corresponding hospital outbreaks.
Following a cluster of infections in Wanhua District, Taipei City, a surge of COVID-19 cases occurred mainly in northern Taiwan during May to July 2021.31 An undiagnosed resident from Wanhua resulted in a cluster of COVID-19 cases in a nearby medical center.32 Overall, a total of 26 hospitals among 495 hospitals in Taiwan reported 54 outbreaks of COVID-19 with 512 confirmed cases between January 2020 and July 2021.19 The confirmed cases included HCP (19.5%), patients (39.3%), and accompanying persons (41.2%). The median number of affected cases per outbreak was 6 (interquartile range [IQR], 2–12), and the median outbreak duration was 12 days (IQR, 4.3–17.0). Accordingly, the Taiwan CDC has strengthened IPC strategies for preventing transmission from community to hospitals as well as within hospitals (Table 1 ). The detailed IPC measures other than PPE are described below.
Table 1.
Facility-based infection prevention and control measures beyond personal protective equipment in the context of COVID-19 in Taiwan.
| Measuresa | Comments |
|---|---|
| Patient divergence |
|
| Access control | |
| Triageb |
|
| Entry controlb |
|
| Visitor access restrictionb |
|
| Source control | |
| Isolation and quarantineb |
|
| Testing and tracing | |
| Health monitoring and surveillanceb,c |
|
| SARS-CoV-2 testing strategiesb,c |
|
| Case investigation and contact tracingb,c |
|
| Basic IPC measures | Measures implemented before and more important during the pandemic |
| Standard precaution7 |
|
| Universal vaccinationb,c | Preventive mass immunization campaign or an outbreak-response vaccination campaign60,61 |
| Partnershipb,c | The patient/public empowerment and engagement as the new normal through continuous education and encouragement residents, patients and their accompanying persons to help stop the spread of COVID-19, and keep one another safe by getting vaccinated and tested |
Abbreviations: HCP, healthcare personnel; IPC, infection prevention and control; PPE, personal protective equipment; TOCC, travel, occupation, contact, cluster.
IPC measures are designed along the path of individuals who enter and share the public space and shared facilities to protect the right, health and safety of all stakeholders (healthcare personnel, patients and their accompanying persons, and visitors). The challenges are how to translate the theory, policies, government requests, professional recommendations, stakeholders' anticipations, and frontline feedback, while considering the reality which includes the gaps and limitations of environmental, resource, and human factors. All IPC measures should be integrated into daily practice or standards of procedures, and checked and then revised to be feasible, practical, and sustainable. For hazard control, these include PPE, engineering control, and administrative control.
Measures aim to prevent transmission from community to hospitals.
Measures aim to prevent transmission within hospitals.
Information technologies are applied to facilitate IPC measures and provide user-friendly platforms.
Access control measures
Before the COVID-19 pandemic, there is no access control in the hospitals in Taiwan except during nighttime hours. The Taiwan CECC announced the access control policy to prevent the intrusion of SARS-CoV-2 into hospitals. In addition to universal masking and alcohol hand sanitizer, a triage area is established at the designated entrance (including emergency departments) to screen fever, respiratory symptoms, and history of TOCC.33 To translate this policy, sustain these measures, and expedite entry into hospitals, several novel designs or devices have been implemented. These include temperature measurement using non-contact thermal imaging cameras,34 on-site digital reading the National Health Insurance cards,35 and automated triage and appointment systems which are incorporated into the hospital's existing web-based appointment system and deployed along with its on-site counterpart to expedite entry into hospitals.36 Both automated triage and appointment systems query COVID-19 risks (international travel, confirmed cases, close contacts) through web-based database maintained by the National Health Insurance Administration, which integrates data from the Immigration Agency and CDC. Visitors or patients with relevant histories are denied registration or entry; on the other hand, they are referred to either epidemic clinics or outdoor quarantine stations of emergency departments based on their medical needs.30 , 37
The epidemic clinic is designated to provide medical service to patients who are suspected of having COVID-19 or are at risk of SARS-CoV-2 infection; therefore, it is usually located in an independent building or at the corner of one hospital building, preferably separate from other clinics and with an independent entrance and air-conditioning circuit. Since the COVID-19 pandemic, the triage of emergency departments is moved outside for screening fever, respiratory symptoms, and history of TOCC. Patients at risk for COVID-19 are diverted to the outdoor quarantine stations, where physicians visit them after wearing proper PPE. Those patients undergo SARS-CoV-2 PCR testing, medical examination, and corresponding treatment in the outdoor quarantine stations until meeting the criteria for releasing from isolation. Furthermore, a double triage and telemedicine protocol are developed to triage suspected COVID-19 cases and minimize HCP's exposure to this disease.38
Visitor access restriction
The Taiwan CECC has announced visitor restriction policies, which are applied to inpatients to limit the number of visitors and time staying at bedsides and also to those with risk for COVID-19; the policies are adjusted based on the level of community transmission.39 Exception to these restrictions are clearly defined for ethical consideration, such as key family members of patients undergoing emergent care, invasive procedures, or hospice care. Following the large-scale community outbreak, visitors are required to provide a negative SARS-CoV-2 PCR or antigen test result before entering the hospitals. Visitors could be exempted from screening for SARS-CoV-2 if they have received the full COVID-19 vaccination at least 14 days before or have a history of previous COVID-19 within three months.40
Isolation and quarantine
Integrated with early identification of confirmed cases and comprehensive contact tracing, isolation of the confirmed cases during their contagious period and quarantine of the close contacts during the incubation period are critical measures to prevent transmission and contain clusters of infectious diseases with high transmissibility such as COVID-19, particularly when pharmaceutical interventions are absent, unavailable, or limited in efficacy. This policy is aligned with the recommendations of the US Centers for Disease Control and Prevention.41 Quarantine policy was initiated at the beginning of COVID-19 pandemic in Taiwan with rolling updates according to the epidemiological evidence, resource, and feedback from the frontline execution.
To surge capacity for this mission, hospitals are required to allocate a certain proportion (up to 30% at the peak in northern Taiwan) of inpatient units or beds as isolation units to provide acute and intensive care of COVID-19 cases.37 The isolation units are generally located away from the main hospital building, with incorporating contaminated, transition, and clean zones.42 Hospitalized patients are transported through specific routes to minimize contact with other patients and HCP, and placed in adequately ventilated single rooms or negative pressure isolation rooms.41 The portable high efficiency particulate air (HEPA) cleaners have been confirmed to be effective in removing SARS-CoV-2 particles from the air, and thus are used to increase the filtration of aerosol particles in single rooms without modifying the existing ventilation systems.43 , 44 Physicians and nurses working in the isolation units receive comprehensive PPE training and are not allowed to work in other patient-care areas.
To cope with the surge in COVID-19 cases from the community or confirmed after hospitalization with the difficulty in transferring cases to other hospitals, hospitals respond accordingly by transforming routine inpatient units into dedicated COVID-19 units. A medical center near Wanhua increased the COVID-19 units from 1 unit (11 negative pressure isolation beds) to 5 units (138 beds without negative pressure designs) and ICU capacity from 1 unit (10 beds) to 4 units (58 beds) within 3 weeks in 2021.32
At the national level, the central and local governments work together to divert asymptomatic or mild COVID-19 cases in the community to preserve hospital capacity for severe cases and routine healthcare. These include home isolation or quarantine which is integrated with hospital-based supporting system sponsored by local governments. In addition, hotels are recruited and transformed into quarantine hotels for inbound traveler or into enhanced quarantine centers equipped with HCP and medical resources.45 These capacity surging and patient divergence in the community significantly relieve the burden of overstretched hospital service, which indirectly result in subsequent reduction in hospital outbreaks and preserve capacity of routine health care.
Health monitoring and surveillance
For occupational health and safety, HCP's right, and protection of vulnerable populations in the healthcare settings, early identification of SARS-CoV-2 infection among HCP has been emphasized and can be achieved through a surveillance and reporting system.46 Syndromic surveillance can be conducted using passive or active methods according to the COVID-19 transmission risk.47 A weekly passive syndromic surveillance has been routinely performed after the SARS epidemic in Taiwan; HCP self-report to the designated staff in their unit or department if they experience any predefined symptoms, such as fever, cough, and other airway symptoms. In response to the evolving COVID-19 outbreak, the systems have been rapidly scaled up, and the predefined symptoms were expanded to include dysosmia and dysgeusia as well.48 HCP measure their temperature at least once daily on arrival for their shift. Requirement to daily report their health status causes additional burden on HCP who are already stretched by the excess load of COVID-19; therefore, REDCap or other one-stop intranet platforms are developed to actively remind HCP for self-reporting travel declaration, temperature, predefined symptoms, and test results. The corresponding management for HCP with predefined symptoms are established based on their SARS-CoV-2 infection risk.46 The policies for testing, quarantine accommodation, sick paid leave are well defined and announced at the national and institution levels.
The effectiveness of enhanced surveillance and reporting systems had been evaluated between January and June, 2020 in Taiwan46 and from January to February, 2020 in Singapore.49 None of the HCP were found to be infected with COVID-19. The results highlight that a surveillance and reporting system in place can be rapidly enhanced to prevent HCP from infection during the COVID-19 outbreak.
SARS-CoV-2 PCR testing strategies
Before the etiology causing emerging infectious disease is identified and efficient testing is available and accessible, syndromic surveillance is conducted based on case definition for notification. However, the following cases may be missed by syndromic surveillance: patients with early stage of the disease, mild infections, atypical symptoms, co-morbidities, extreme age, co-infections, uncommon routes of transmission, and infections from various virus variants.30 , 50 With the advance in science and technology of viral kinetics of SARS-CoV-2, laboratory testing plays a key role in early case finding (including symptomatic, pre-symptomatic, and asymptomatic patients) and guiding risk-adjusted and transmission-based IPC measures. The national laboratory network was established and strengthened through the recruitment of medical centers and regional hospitals distributed throughout most geographical regions of the country in January 2020; later, the network expanded the available testing supply and maximized testing capacity.51
National and institutional SARS-CoV-2 PCR testing strategies have been developed and implemented since the emerging COVID-19 pandemic. The government-funded, free testing strategies are adjusted timely according to epidemiological characteristics, capacity of testing, level of transmission in the community or institutions, and turnaround time from sampling to data feedback. The target populations for SARS-CoV-2 PCR and rapid antigen testing have been expanded stepwise (Table 1). With an increasing level of community transmission, SARS-CoV-2 testing has been applied to all patients scheduled for hospital admission, surgery, dialysis or other procedures, as well as their accompanying persons. Given the higher risk of infection, HCP are recommended to be prioritized for SARS-CoV-2 testing47 following exposure to virus or periodically (e.g., weekly). The later was initially applied to HCP at high-risk units, such as triage, emergency departments, or COVID-19 units. The testing frequency depends on the level of transmission within a hospital and surrounding areas, and mass screening has been applied to all HCP periodically for outbreak management or until HCP are fully vaccinated.22 , 25 , 32 After implementing universal testing for newly admitted patients and their companions, as well as periodic testing of HCP in high-risk areas, there was a significant decrease in hospital outbreaks.19
With the advanced facility, large-scale SARS-CoV-2 PCR testing is doable. Nevertheless, self-performed rapid antigen testing is feasible and sustainable for repeated testing and can be used as an effective intervention for countries transitioning from pandemic mitigation to endemic COVID-19 though the impact of testing varies depending on test sensitivity and frequency.52 , 53 Besides, in the absence of government subsidy, the feasibility and sustainability of these testing strategies will depend on the costs of the tests.
Case investigation and contact tracing
Taiwan's response to the COVID-19 pandemic was unique in the world, as it acted promptly at the very beginning and conducted precisive contact tracing and testing to achieve very low proportion of indigenous cases using a reasonable number of testing. As of March 27, 2021, total number of COVID-19 cases per million population was 42 in Taiwan and 63 in China, and total number of tests per million population was 19,256 in Taiwan and 111,163 in China, whereas more than 90,000 cases per million population and more than 1,000,000 tests per million population were reported in the US and Israel. As of 29 January, 2023, Taiwan reported 399,263 COVID-19 cases per million population (rank 46 among 229 countries and territories), including 683 deaths per million population (rank 120), and conducted 1,259,685 tests per million population (rank 92).54
In the healthcare settings, case investigation and contact tracing should be comprehensive for the close contacts since getting infected could potentially affect many people, including those at higher risk for severe diseases and critical infrastructure workers. To achieve zero healthcare-acquired COVID-19 in a teaching hospital, infection control nurses evaluate every COVID-19 case for the potential of intra-hospital spread immediately after receiving the automated messages of positive results of SARS CoV-2 PCR or notification from the frontline HCP.46 If the case has not been reported as COVID-19 before or stayed in the hospital outside the dedicated COVID-19 units without COVID-19 specific isolation precaution, the incident event management is initiated according to the Taiwan CDC recommendations with minor modification.55
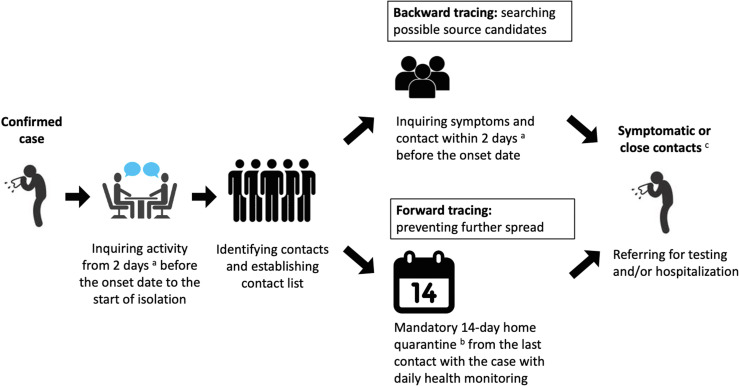
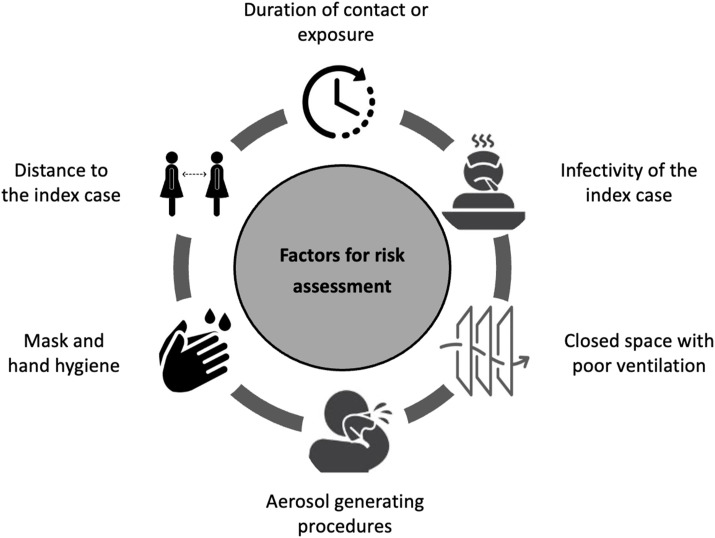
Fig. 3 shows the framework of bi-directional contact tracing and testing. The index case is placed in a single isolation room and interviewed for comprehensive information on the history of SARS-CoV-2 testing and results, date of symptom onset, potential source of illness, activity history, and the list of close contacts.41 A high-risk contact (i.e., close contact, as defined in Fig. 3) should undergo a SARS-CoV-2 PCR test and 14-day quarantine. On the other hand, low-risk contacts (i.e. risk contacts) should monitor themselves for symptoms consistent with COVID-19 for 14 days. The risks of exposure are accessed based on several factors, as described in Fig. 4 . In addition, the risks of subsequent infection following exposure vary by vaccination status and host factors.
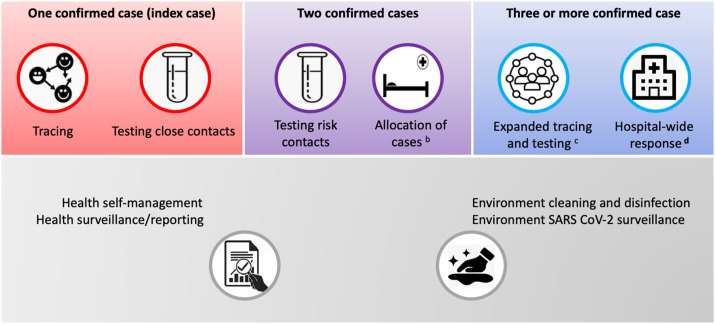
Figure 3.
The framework of bi-directional contact tracing (a) a contact elicitation window of 2 days is used to ensure more infected contacts are identified, thus day 0 is considered as 2 days prior to the date of symptom onset or specimen collection for SARS-CoV-2 testing for the index case.62,63 (b) close contacts are defined as individuals with face-to-face contact (within 2 m) for a period of ≥15 min or direct exposure to aerosols or respiratory secretions without proper personal protection equipment from 2 days before the onset date of index case to the start of isolation. (c) The quarantine period of contacts is adjusted from 14 days to balance the public health risks and benefits against the social and economic impact.
Figure 4.
Factors considered in the risk assessment for possible transmission to contacts in the absence of transmission-based isolation precaution and appropriate personal protective equipment.
In addition to those described in Table 1, other measures implemented include escalating SARS-CoV-2 testing policies, restriction or delay of scheduled admissions or procedures, segregation of wards, and traffic control bundle according to the Taiwan CDC recommendations (Fig. 5 ).55 All these intensive aggressive interventions allow the outbreak to be declared over quickly.56 To proactively prevent COVID-19 acquisition and spread in the healthcare settings, the importance of hand hygiene, environmental cleaning, and other elements of standard precaution (Table 1) cannot be overemphasized as SARS-CoV-2 may be transmitted indirectly through contaminating the hospital environment.57
Figure 5.
The core elements of responding to COVID-19 confirmed cases who are hospitalized outside of dedicated COVID-19 wards or beds, and in the absence of COVID-19 specific precaution according to the Taiwan CDC recommendations (a) the guidance was first released on February 26, 2020 by the Taiwan CDC.55 (b) Isolation of confirmed cases and quarantine of those close contract in single rooms in designated COVID-19 units or in index units after cleaning. (c) In addition to the index case, there are additional 2 confirmed cases among those close contacts or risk contacts in inpatients units or additional 3 cases in outpatients or administrative units. In this situation, risk contacts are managed as close contacts. (d) Hospital-, campus- or building-wide responses are mandatory if there are a total of 3 or more confirmed cases (including the index case), or confirmed cases are distributed across more than one unit. These responses include active monitoring of health condition, mass screening, segregation of wards, and traffic control bundle. If deemed necessary, restrictions or delays of scheduled admissions or procedures may be implemented to reallocate capacity for isolation or quarantine purposes. For example, the facility may need to allocate manpower to support the index unit(s) to manage the outbreak.
Conclusions
The early and aggressive implementation of NPIs in Taiwan has successfully contained COVID-19 prior to the widespread availability of effective vaccines and antiviral agents. In the healthcare setting, IPC measures are important during the initial phase of pandemics as well as transition to endemics since HCP and patients face higher risks of SARS-CoV-2 infection than individuals in the community. In view of the lessons learned from the SARS outbreak in 2003, hospital outbreaks of COVID-19 during community surges were controlled by strengthened, multi-pronged integrated IPC measures. In addition to appropriate use of PPE, access control, visitor restriction, dedicated isolation units, hospital-wide health surveillance and reporting system, and extensive case findings and contact tracing have been deployed during the COVID-19 pandemic. These IPC measures prevent intra-hospital spread of SARS-CoV-2 to a minimum and protect HCP and patients in Taiwan.
Funding
YC Chen was supported by National Taiwan University Hospital intramural fund (NTUH 109-P14). The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the manuscript.
Declaration of competing interest
The authors have no conflicts of interest relevant to this article.
Acknowledgments
Thanks to Dr. Hao-Hsin Wu, Taiwan Centers for Disease Control, for suggestion and preparing Figure 4, Figure 5. We are grateful to infection control personnel for their commitment and contribution and healthcare personnel for their engagement and collaboration to protect patients, caregivers, and colleagues during the COVID-19 pandemic. We also appreciate all personnel in local and central governments who involve in pandemic control to secure a safe and healthy society for three years.
References
- 1.World Health Organization. WHO coronavirus (COVID-19) dashboard. Available at: https://covid19.who.int/. [Accessed on 31 January 2023].
- 2.Moreland A., Herlihy C., Tynan M.A., Sunshine G., McCord R.F., Hilton C., et al. Timing of state and territorial COVID-19 stay-at-home orders and changes in population movement - United States, March 1-May 31, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1198–1203. doi: 10.15585/mmwr.mm6935a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chiang C.H., Chiang C.H., Chiang C.H., Chen Y.C. The practice of wearing surgical masks during the COVID-19 pandemic. Emerg Infect Dis. 2020;26:1962. doi: 10.3201/eid2608.201498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen S.C. Taiwan's experience in fighting COVID-19. Nat Immunol. 2021;22:393–394. doi: 10.1038/s41590-021-00908-2. [DOI] [PubMed] [Google Scholar]
- 5.Cheng H.Y., Li S.Y., Yang C.H. Initial rapid and proactive response for the COVID-19 outbreak - Taiwan's experience. J Formos Med Assoc. 2020;119:771–773. doi: 10.1016/j.jfma.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen Y.H., Fang C.T. Combined interventions to suppress R0 and border quarantine to contain COVID-19 in Taiwan. J Formos Med Assoc. 2021;120:903–905. doi: 10.1016/j.jfma.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cheng H.Y., Liu D.P. Early Prompt response to COVID-19 in Taiwan: comprehensive surveillance, decisive border control, and information technology support. J Formos Med Assoc. 2022 doi: 10.1016/j.jfma.2022.11.002. S0929-S6646(22)00421-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheng H.Y., Huang A.S. Proactive and blended approach for COVID-19 control in Taiwan. Biochem Biophys Res Commun. 2021;538:238–243. doi: 10.1016/j.bbrc.2020.10.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The Economist. Tracking covid-19 excess deaths across countries. Available at: https://www.economist.com/graphic-detail/coronavirus-excess-deaths-tracker. [Accessed on 31 January 2023].
- 10.Leung N.H.L. Transmissibility and transmission of respiratory viruses. Nat Rev Microbiol. 2021;19:528–545. doi: 10.1038/s41579-021-00535-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tsou H.H., Kuo S.C., Lin Y.H., Hsiung C.A., Chiou H.Y., Chen W.J., et al. A comprehensive evaluation of COVID-19 policies and outcomes in 50 countries and territories. Sci Rep. 2022;12:8802. doi: 10.1038/s41598-022-12853-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cheng H.Y., Chueh Y.N., Chen C.M., Jian S.W., Lai S.K., Liu D.P. Taiwan's COVID-19 response: timely case detection and quarantine, January to June 2020. J Formos Med Assoc. 2021;120:1400–1404. doi: 10.1016/j.jfma.2020.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ng T.C., Cheng H.Y., Chang H.H., Liu C.C., Yang C.C., Jian S.W., et al. Comparison of estimated effectiveness of case-based and population-based interventions on COVID-19 containment in Taiwan. JAMA Intern Med. 2021;181:913–921. doi: 10.1001/jamainternmed.2021.1644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Niu Z., Scarciotti G. Ranking the effectiveness of non-pharmaceutical interventions to counter COVID-19 in UK universities with vaccinated population. Sci Rep. 2022;12:13039. doi: 10.1038/s41598-022-16532-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yen M.Y., Lin Y.E., Lee C.H., Ho M.S., Huang F.Y., Chang S.C., et al. Taiwan’s traffic control bundle and the elimination of nosocomial severe acute respiratory syndrome among healthcare workers. J Hosp Infect. 2011;77:332–337. doi: 10.1016/j.jhin.2010.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen Y.C., Chang S.C., Tsai K.S., Lin F.Y. Certainties and uncertainties facing emerging respiratory infectious diseases: lessons from SARS. J Formos Med Assoc. 2008;107:432–442. doi: 10.1016/S0929-6646(08)60150-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization. Summary of probable SARS cases with onset of illness from 1 November 2002 to 31 July 2003. Available at: https://www.who.int/publications/m/item/summary-of-probable-sars-cases-with-onset-of-illness-from-1-november-2002-to-31-july-2003. [Accessed on 31 January 2023].
- 18.Chen Y.C., Chen P.J., Chang S.C., Kao C.L., Wang S.H., Wang L.H., et al. Infection control and SARS transmission among healthcare workers, Taiwan. Emerg Infect Dis. 2004;10:895–898. doi: 10.3201/eid1005.030777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu H.H., Su C.H., Chien L.J., Tseng S.H., Chang S.C. Healthcare-associated COVID-19 outbreaks: a nationwide population-based cohort study. J Hosp Infect. 2022;124:29–36. doi: 10.1016/j.jhin.2022.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lessells R., Moosa Y., de Oliveira T. Report into a nosocomial outbreak of coronavirus disease 2019 (COVID-19) at Netcare St. Augustine’s Hospital. 2020 https://www.krisp.org.za/manuscripts/StAugustinesHospitalOutbreakInvestigation_FinalReport_15may2020_comp.pdf [Accessed on 31 January 2023] [Google Scholar]
- 22.Lee U., Kim S.E., Lee S.Y., Wi H.N., Choi O., Park J.W., et al. Source analysis and effective control of a COVID-19 outbreak in a university teaching hospital during a period of increasing community prevalence of COVID-19. J Korean Med Sci. 2021;36:e179. doi: 10.3346/jkms.2021.36.e179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ponsford M.J., Ward T.J.C., Stoneham S.M., Dallimore C.M., Sham D., Osman K., et al. A systematic review and meta-analysis of inpatient mortality associated with nosocomial and community COVID-19 exposes the vulnerability of immunosuppressed adults. Front Immunol. 2021;12:744696. doi: 10.3389/fimmu.2021.744696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhou Q., Gao Y., Wang X., Liu R., Du P., Wang X., et al. Nosocomial infections among patients with COVID-19, SARS and MERS: a rapid review and meta-analysis. Ann Transl Med. 2020;8:629. doi: 10.21037/atm-20-3324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim S.W., Jo S.J., Lee H., Oh J.H., Lim J., Lee S.H., et al. Containment of a healthcare-associated COVID-19 outbreak in a university hospital in Seoul, Korea: a single-center experience. PLoS One. 2020;15 doi: 10.1371/journal.pone.0237692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Richterman A., Meyerowitz E.A., Cevik M. Hospital-acquired SARS-CoV-2 infection: lessons for public health. JAMA. 2020;324:2155–2156. doi: 10.1001/jama.2020.21399. [DOI] [PubMed] [Google Scholar]
- 27.Nguyen L.H., Drew D.A., Graham M.S., Joshi A.D., Guo C.G., Ma W., et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5:e475–e483. doi: 10.1016/S2468-2667(20)30164-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Taiwan Centers for Disease Control. Taoyuan General Hospital cluster infection incident. Available at: https://covid19.mohw.gov.tw/en/cp-5142-59029-206.html. [Accessed on 31 January 2023].
- 29.Taiwan Centers for Disease Control. Taiwan national infectious disease statistics system. Available at: https://nidss.cdc.gov.tw/en/. [Accessed on 31 January 2023].
- 30.Cheng C.W., Huang P.Y., Wu T.S., Huang C.G., Tsao K.C., Lin C.S., et al. Infection control operations of a large hospital in Taiwan to prevent nosocomial outbreaks during COVID-19 pandemic. Biomed J. 2021;44:S8–S14. doi: 10.1016/j.bj.2021.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu C.J., Yang C.Y., Chen Y.L., Wang S.S., Chu C.M., Hsieh M.H., et al. Prompt successful response to a COVID-19 outbreak: performance of community-based rapid screening station. J Formos Med Assoc. 2022;121:2356–2359. doi: 10.1016/j.jfma.2022.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huang J.H., Chang H.T., Liao C.H., Chiu K.M. Rapid response of a medical center upon the surge of COVID-19 epidemic in Taiwan. J Microbiol Immunol Infect. 2022;55:1–5. doi: 10.1016/j.jmii.2021.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.US Centers for Disease Control and Prevention. Management of visitors to healthcare facilities in the context of COVID-19: Non-US healthcare settings. Availble at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-us-settings/hcf-visitors.html. [Accessed on 31 January 2023].
- 34.Brzezinski R.Y., Rabin N., Lewis N., Peled R., Kerpel A., Tsur A.M., et al. Automated processing of thermal imaging to detect COVID-19. Sci Rep. 2021;11:17489. doi: 10.1038/s41598-021-96900-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang C.J., Ng C.Y., Brook R.H. Response to COVID-19 in Taiwan: big data analytics, new technology, and proactive testing. JAMA. 2020;323:1341–1342. doi: 10.1001/jama.2020.3151. [DOI] [PubMed] [Google Scholar]
- 36.Lu D.H., Hsu C.A., Yuan E.J., Fen J.J., Lee C.Y., Ming J.L., et al. Experiences with internet triaging of 9498 outpatients daily at the largest public hospital in Taiwan during the COVID-19 pandemic: observational study. JMIR Med Inform. 2021;9 doi: 10.2196/20994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chang Y.T., Lin C.Y., Tsai M.J., Hung C.T., Hsu C.W., Lu P.L., et al. Infection control measures of a Taiwanese hospital to confront the COVID-19 pandemic. Kaohsiung J Med Sci. 2020;36:296–304. doi: 10.1002/kjm2.12228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lin C.H., Tseng W.P., Wu J.L., Tay J., Cheng M.T., Ong H.N., et al. A double triage and telemedicine protocol to optimize infection control in an emergency department in Taiwan during the COVID-19 pandemic: retrospective feasibility study. J Med Internet Res. 2020;22 doi: 10.2196/20586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Taiwan Centers for Disease Control. Crucial policies for combating COVID-19. Available at: https://covid19.mohw.gov.tw/en/sp-timeline0-206.html. [Accessed on 31 January 2023].
- 40.Taiwan Centers for Disease Control Hospitals in Taiwan to conditionally allow visitation and adjust screening measures for inpatients and individuals accompanying inpatients in cities with risks. 2021. https://www.cdc.gov.tw/En/Bulletin/Detail/p1Xr9ABkqY8yVaAEcuscSQ?typeid=158 Starting August 24. [Accessed on 31 January 2023]
- 41.US Centers for Disease Control and Prevention. Interim guidance on developing a COVID-19 case investigation and contact tracing plan: Overview. Availble at: https://www.cdc.gov/coronavirus/2019-ncov/php/contact-tracing/contact-tracing-plan/overview.html. [Accessed on 31 January 2023].
- 42.Yen M.Y., Schwartz J., Chen S.Y., King C.C., Yang G.Y., Hsueh P.R. Interrupting COVID-19 transmission by implementing enhanced traffic control bundling: implications for global prevention and control efforts. J Microbiol Immunol Infect. 2020;53:377–380. doi: 10.1016/j.jmii.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Conway Morris A., Sharrocks K., Bousfield R., Kermack L., Maes M., Higginson E., et al. The removal of airborne SARS-CoV-2 and other microbial bioaerosols by air filtration on COVID-19 surge units. Clin Infect Dis. 2021;75:e97–e101. doi: 10.1093/cid/ciab933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lindsley W.G., Derk R.C., Coyle J.P., Martin S.B., Jr., Mead K.R., Blachere F.M., et al. Efficacy of portable air cleaners and masking for reducing indoor exposure to simulated exhaled SARS-CoV-2 aerosols - United States. MMWR Morb Mortal Wkly Rep. 2021;2021(70):972–976. doi: 10.15585/mmwr.mm7027e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tsai H.W., Hung F.M., Liao C.H., Lin H.F. Hotel-based quarantine center as a rapid response to COVID-19 outbreak, New Taipei, Taiwan, May to July 2021. J Formos Med Assoc. 2022;121:1351–1353. doi: 10.1016/j.jfma.2022.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pan S.C., Hsu M.C., Chang H.H., Wang J.T., Lai Y.L., Chen P.C., et al. Prospective health surveillance for COVID-19 among health care workers at a university medical center in Taiwan, January to June 2020. J Formos Med Assoc. 2021;121:613–622. doi: 10.1016/j.jfma.2021.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.World Health Organization Prevention, identification and management of health worker infection in the context of COVID-19. 2020. https://www.who.int/publications/i/item/10665-336265 [Accessed on 31 January 2023]
- 48.Sheng W.H., Liu W.D., Wang J.T., Chang S.Y., Chang S.C. Dysosmia and dysgeusia in patients with COVID-19 in northern Taiwan. J Formos Med Assoc. 2021;120:311–317. doi: 10.1016/j.jfma.2020.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Htun H.L., Lim D.W., Kyaw W.M., Loh W.J., Lee L.T., Ang B., et al. Responding to the COVID-19 outbreak in Singapore: staff protection and staff temperature and sickness surveillance systems. Clin Infect Dis. 2020;71:1947–1952. doi: 10.1093/cid/ciaa468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Miller M.B., Ooi E.E., Rhoads D.D., Kulldorff M., Anderson D.E., Lee H., et al. As Omicron takes hold and other new variants arise, COVID-19 testing remains the universally agreed tool to effect transition from pandemic to endemic state. Front Public Health. 2022;10:883066. doi: 10.3389/fpubh.2022.883066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Taiwan Centers for Disease Control. Adequate testing capacity and precisely locate potentially infected individuals. Available at: https://covid19.mohw.gov.tw/en/cp-4788-53906-206.html. [Accessed on 31 January 2023].
- 52.Koo J.R., Cook A.R., Lim J.T., Tan K.W., Dickens B.L. Modelling the impact of mass testing to transition from pandemic mitigation to endemic COVID-19. Viruses. 2022;14:967. doi: 10.3390/v14050967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pham T.M., Tahir H., van de Wijgert J., Van der Roest B.R., Ellerbroek P., Bonten M.J.M., et al. Interventions to control nosocomial transmission of SARS-CoV-2: a modelling study. BMC Med. 2021;19:211. doi: 10.1186/s12916-021-02060-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Worldometer. COVID-19 coronavirus pandemic. Available at: https://www.worldometers.info/coronavirus/#countries. [Accessed on 31 January 2023].
- 55.Taiwan Centers for Disease Control. Responding to covid-19 cases in the healthcare setting. Available at: https://www.cdc.gov.tw/Category/MPage/I92jtldmxZO_oolFPzP9HQ. [Accessed on 31 January 2023].
- 56.Akhmetzhanov A.R., Jung S.M., Cheng H.Y., Thompson R.N. A hospital-related outbreak of SARS-CoV-2 associated with variant Epsilon (B.1.429) in Taiwan: transmission potential and outbreak containment under intensified contact tracing, January-February 2021. Int J Infect Dis. 2021;110:15–20. doi: 10.1016/j.ijid.2021.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bak A., Mugglestone M.A., Ratnaraja N.V., Wilson J.A., Rivett L., Stoneham S.M., et al. SARS-CoV-2 routes of transmission and recommendations for preventing acquisition: joint British Infection Association (BIA), Healthcare Infection Society (HIS), Infection Prevention Society (IPS) and Royal College of Pathologists (RCPath) guidance. J Hosp Infect. 2021;114:79–103. doi: 10.1016/j.jhin.2021.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.World Health Organization. Avoid the Three Cs. Available at: https://www.who.int/brunei/news/infographics–-english. [Accessed on 31 January 2023].
- 59.US Centers for Disease Control and Prevention. Standard precautions for all patient care. Available at: https://www.cdc.gov/infectioncontrol/basics/standard-precautions.html. [Accessed on 31 January 2023].
- 60.Wu U.I., Wang J.T., Chang S.C., Chuang Y.C., Lin W.R., Lu M.C., et al. Impacts of a mass vaccination campaign against pandemic H1N1 2009 influenza in Taiwan: a time-series regression analysis. Int J Infect Dis. 2014;23:82–89. doi: 10.1016/j.ijid.2014.02.016. [DOI] [PubMed] [Google Scholar]
- 61.World Health Organization. Framework for decision-making: implementation of mass vaccination campaigns in the context of COVID-19: Interim guidance. Available at: https://apps.who.int/iris/bitstream/handle/10665/332159/WHO-2019-nCoV-Framework_Mass_Vaccination-2020.1-eng.pdf. [Accessed on 31 January 2023].
- 62.Hart W.S., Maini P.K., Thompson R.N. High infectiousness immediately before COVID-19 symptom onset highlights the importance of continued contact tracing. Elife. 2021;10 doi: 10.7554/eLife.65534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cheng H.Y., Jian S.W., Liu D.P., Ng T.C., Huang W.T., Lin H.H. Contact tracing assessment of COVID-19 transmission dynamics in Taiwan and risk at different exposure periods before and after symptom onset. JAMA Intern Med. 2020;180:1156–1163. doi: 10.1001/jamainternmed.2020.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]