The self-inflating resuscitator or bag-valve-mask (BVM) is a basic but essential part of an anaesthetist's toolkit for resuscitation. It is used in situations ranging from preoxygenation of the lungs, emergency ventilation for respiratory failure and cardiopulmonary resuscitation. This article outlines the key design features of the BVM important for its use in clinical practice.
History
Like the modern ventilator, the BVM resuscitator was developed during the polio epidemic in 1953. The combination of the mass demand for manual ventilation and lack of oxygen supplies led to the need for a bag that could ventilate and entrain its own air. Using bicycle spokes to create an internal spring, a non-rebreathing valve and an anaesthetic reservoir bag, Dr Henning Ruben created the prototype self-inflating bag.1,2 Together with Dr Holger Hesse, in 1953 they developed the first self-inflating, portable, manual ventilator that could be used without electricity or oxygen supply—the Artificial Mask Bag Unit (AMBU)—and marked a revolution in resuscitation.
Design of the BVM resuscitator
There are many different proprietary brands of BVM produced such as Ambu and Laerdal, but the common basic design (Fig. 1) consists of the following.
-
(i)
Oxygen reservoir bag (e.g. Laerdal Silicone Resuscitator: adult model: 2600 ml; paediatric model 600 ml).3 This will fill if there is adequate oxygen supply from the oxygen inlet (e.g. 15 L min−1), and ensures that the patient is breathing the maximum fractional inspired oxygen concentration (Fio2) available.
-
(ii)
Oxygen inlet to connect to an oxygen source.
-
(iii)Intake valve, which is made up of three soft flap valves:
-
a.The intake disc membrane. This ensures gas is only delivered forward to the patient during manual ventilation, but not backward into the reservoir bag.
-
b.The inlet reservoir flap valve. This is essential for the self-inflating property of the resuscitator. During spontaneous breathing, if the oxygen supply flow cannot meet the patient's inspiratory flow and the oxygen reservoir bag has been emptied, this valve will open and entrain room air. This situation can also occur during manual ventilation if the tidal volume and ventilation rate are high and the oxygen supply flow is inadequate. In such case, when the ventilation bag recoils in the expiratory phase, the valve will open and entrain room air.4
-
c.The outlet reservoir flap valve. With increasing oxygen flow, pressure will build up in the oxygen reservoir bag, and at a certain threshold the valve will open to atmosphere. This prevents the patient from being exposed to dangerous pressures caused by excessive flow from the oxygen source.
-
a.
-
(iv)
Ventilation bag (e.g. Laerdal Silicone Resuscitator: adult model 1600 ml paediatric model 500 ml), which the user compresses to provide ventilation.3 This bag recoils automatically during expiration and refills itself from an attached oxygen source or room air or both. Because of the large volume of the bag, it is not uncommon for inexperienced operators to generate excessively high volumes and flows during manual ventilation, which can result in gastric insufflation and high intrathoracic pressures with associated cardiovascular effects and barotrauma. To address this, some models are designed with a smaller ventilation bag or incorporated with a modified valve at the outlet of the ventilation bag to limit the peak inspiratory flow.5,6
- (v)
-
(vi)
Pressure relief valve at the inspiratory port of the patient valve. This is usually found in paediatric models to prevent excessive pressure being applied.
-
(vii)
Positive end-expiratory pressure (PEEP) valve may be attached to the expiratory port of the patient valve in some models.
Fig 1.
A schematic diagram of the basic design and the functions of individual flap valves inside the intake valve of a bag-valve-mask resuscitator. Entrained room air flow is represented by the orange dashed arrow. Oxygen flows are represented by the blue dashed arrows. Photos of the dissembled intake valve and patient valve of a Laerdal Silicone Resuscitator are included.
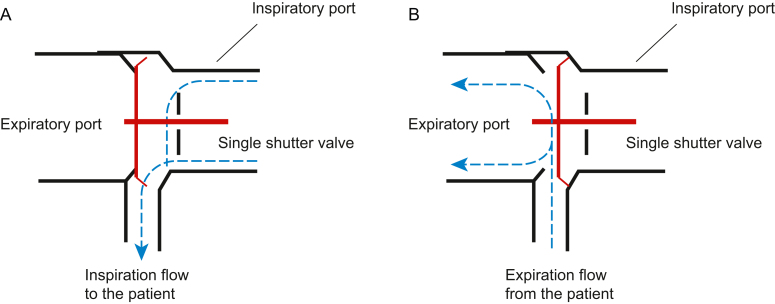
Fig 2.
A schematic diagram of a single shutter valve, represented by Ambu® SPUR II disposable resuscitator (www.ambu.com), showing its position in inspiration (A) and expiration (B) in response to gas flow (blue dashed arrows).
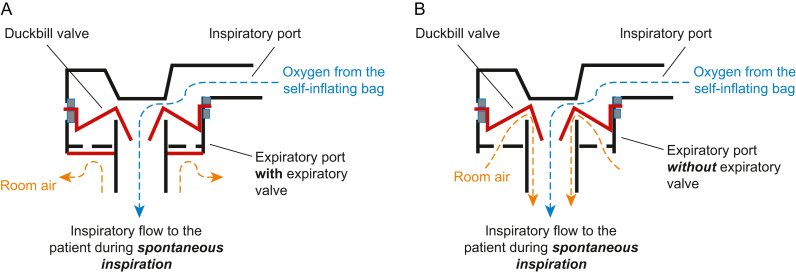
Fig 3.
A schematic diagram of a duckbill valve with (A) and without (B) an expiratory valve, showing potential entrainment of room air (orange dashed arrows) through the expiratory port, during spontaneous inspiration.
Reusable and disposable BVMs
Both reusable and disposable single-use BVMs are available. Reusable models can be dissembled and the parts individually cleaned and disinfected after use using different methods such as steam autoclaving, chemical disinfection (e.g. Cidex OPA) and pasteurisation.3 However, repeated cleaning and disinfection may degrade the materials, with risk of device malfunction. Re-assembling errors can also occur after disinfection and lead to serious adverse effects.7
In contrast, advantages of disposable models over reusable models include eliminating the risks of cross-contamination of highly infectious pathogens (e.g. Ebola) between patients and reassembling errors. They are also more convenient in settings that lack disinfection facilities (e.g. community medical clinics). However, single-use BVMs contribute to creation of plastic medical waste and add to the environmental impacts of healthcare.
Patient valve
The patient valve consists of an inspiratory port, an expiratory port, a patient connector and non-rebreathing soft valves to allow unidirectional inspiratory and expiratory flow (Fig 2, Fig 3). During expiration, the soft valves direct gas out of the expiratory port to prevent rebreathing. The specific designs and configurations of these soft valves used are important in the performance of each device. Two commonly used ones are discussed below.
The Ambu single shutter valve
The Ambu single shutter valve is a flap valve (Fig. 2). During inspiration, fresh gas flow from the self-inflating bag pushes the valve forward, opening the inspiratory port. This movement simultaneously closes the expiratory port. This is important because it prevents entrainment of room air from the expiratory port if the patient is taking negative pressure spontaneous breaths. At the end of inspiration, the flap returns to its original position, opening the expiratory port simultaneously, and allowing expired gas to exit.
The duckbill valve
The duckbill valve (Fig. 3) or lip valve is used in Laerdal resuscitators, and other brands.3,8, 9, 10 The inspiratory valve is shaped like a duck's bill directed towards the patient, which opens during inspiration. When the patient expires, the duckbill valve closes and gas is directed around the duckbill and out via the expiratory port.
Factors affecting oxygen delivery
Manual ventilation
During manual ventilation, the delivered oxygen concentration varies depending on the oxygen flow and the delivered tidal volume and ventilatory rate. For instance, at 8 L min−1 oxygen flow, the Laerdal Silicone Resuscitator Adult model manufacturer's specifications suggest it can deliver almost 100% oxygen concentration if the delivered tidal volume is 400 ml and ventilation rate is 12 per minute during manual ventilation.3 However, the fraction of delivered oxygen (Fdo2) decreases to 68% if delivered tidal volume and bag cycling rate are increased to 600 ml×24 per minute, because of the entrainment of room air.3,4 This is less of an issue at higher oxygen flows of 15 L min−1, where it has been shown that Fdo2 can exceed 95% across a wide range of tidal volumes and ventilatory rates during manual ventilation.3,4 Knowledge of this relationship allows titration of delivered oxygen concentration across a range of flows, for example to maximise delivered oxygen, or conversely in situations where avoidance of hyperoxia is desired such as post-cardiac arrest.
Spontaneous breathing
BVMs are commonly used in the resuscitation of spontaneously breathing patients, because of the assumption that they can deliver a high Fdo2 at high oxygen flow. However, the specific design of the patient valve in different models can affect its performance. One of the main causes for this variability in performance is whether or not air can be entrained via the exhaust port during negative pressure spontaneous inspiration8, 9, 10, 11(Fig. 3). This can be prevented by closing the expiratory port during spontaneous inspiration by movement of the Ambu single shutter valve (Fig. 2) as stated before, or by an additional expiratory disc valve (Fig. 3) in the case of the duckbill design. Studies in mechanical lung simulators and healthy volunteers have suggested that duckbill models without an expiratory valve can have worse oxygen delivery performance if inspiration is spontaneous, especially in settings of respiratory distress with high peak inspiratory flow.8, 9, 10, 11 To alleviate this issue, anaesthetists can consider adding a PEEP valve to the exhaust port in certain models to improve delivered Fio2.11
Comparing the BVM resuscitator with the Mapleson C breathing system
The Mapleson C breathing system (Waters system) is a flow-dependent system commonly used as an alternative for ventilation and oxygenation outside of the operating theatre. In comparison with a BVM, the advantages of the Mapleson C breathing system are that the absence of an inspiratory valve makes it easier to breathe through and is more efficient for preoxygenation.2 Experienced practitioners may also prefer the Mapleson C breathing system during positive pressure ventilation as it gives a better impression of lung and chest wall compliance.12 However, during situations of respiratory distress, minute ventilation is expected to be high, and thus requiring significant oxygen flow in order to prevent rebreathing.
A major advantage of the BVM is that it will enable ventilation of the lungs even without a supply of supplementary oxygen. The non-rebreathing valves at the patient's valve side also prevent rebreathing even when the oxygen fresh gas flow is low. This is useful when there is no or limited oxygen supply, such as in a prehospital setting. However, because of its self-inflating properties there is minimal feedback on the volume delivered to guide adequacy of ventilation if there is leak at the patient-facemask interface. In contrast, when using the flow-dependent Mapleson C breathing system, a poor seal will easily be detected by the collapsed reservoir bag. Errors in the set-up of the valves, for example when re-assembling after disinfection, can also cause serious adverse effects.7
Conclusions
More than 50 years since its invention, the BVM remains an essential tool in our daily practice. Knowledge of its design aids our use and understanding of its performance and limitations.
Acknowledgements
We thank Dr Jonathan CH Cheung for his help in investigating the structure of the bag-valve-mask resuscitators detailed in our article.
Declaration of interests
The authors declare that they have no conflicts of interest.
Biographies
Christopher Pak-to LeeMBBS is a resident in the Department of Anaesthesia and Intensive Care at Prince of Wales Hospital, and an honorary clinical tutor at the Chinese University of Hong Kong. His interests include resuscitation and promoting ‘green ICU’ practices.
Yu-Yeung YipFHKCA (IC) FHKCA FHKAM FCICM FANZCA is a consultant in the Department of Anaesthesia and Intensive Care at Prince of Wales Hospital, and an honorary associate professor at the Chinese University of Hong Kong. He is the Hong Kong director and a member of the Basic Assessment and Support in Intensive Care (BASIC) collaboration. His interests include airway management, e-learning and critical care echocardiography.
Matrix codes: 1B03, 1B04, 1C02, 2A01, 2C02, 3A01
References
- 1.Fahey D.G. The self-inflating resuscitator--evolution of an idea. Anaesth Intensive Care. 2010;38(Suppl 1):10–15. doi: 10.1177/0310057X100380S102. [DOI] [PubMed] [Google Scholar]
- 2.Baskett P., Zorab J. The resuscitation greats. Henning Ruben MD, FFARCS(I), FFARCS. The Ruben valve and the AMBU bag. Resuscitation. 2003;56:123–127. doi: 10.1016/s0300-9572(02)00350-7. [DOI] [PubMed] [Google Scholar]
- 3.Laerdal. LSR User Guide (EN). Available from https://laerdal.com/hk/ProductDownloads.aspx?productId=264 (accessed 17 January 2023).
- 4.Young P., Pilcher J., Patel M., et al. Delivery of titrated oxygen via a self-inflating resuscitation bag. Resuscitation. 2013;84:391–394. doi: 10.1016/j.resuscitation.2012.08.330. [DOI] [PubMed] [Google Scholar]
- 5.Dörges V., Ocker H., Hagelberg S., Wenzel V., et al. Optimisation of tidal volumes given with self-inflatable bags without additional oxygen. Resuscitation. 2000;43:195–199. doi: 10.1016/s0300-9572(99)00148-3. [DOI] [PubMed] [Google Scholar]
- 6.Wagner-Berger H.G., Wenzel V., Stallinger A., et al. Decreasing peak flow rate with a new bag-valve-mask device: effects on respiratory mechanics, and gas distribution in a bench model of an unprotected airway. Resuscitation. 2003;57:193–199. doi: 10.1016/s0300-9572(03)00032-7. [DOI] [PubMed] [Google Scholar]
- 7.Munford B.J., Wishaw K.J. Critical incidents with nonrebreathing valves. Anaesth Intensive Care. 1990;18:560–574. doi: 10.1177/0310057X9001800428. [DOI] [PubMed] [Google Scholar]
- 8.Nimmagadda U., Salem M.R., Joseph N.J., et al. Efficacy of preoxygenation with tidal volume breathing. Comparison of breathing systems. Anesthesiology. 2000;93:693–698. doi: 10.1097/00000542-200009000-00018. [DOI] [PubMed] [Google Scholar]
- 9.Mills P.J., Baptiste J., Preston J., Barnas G.M. Manual resuscitators and spontaneous ventilation--an evaluation. Crit Care Med. 1991;19:1425–1431. doi: 10.1097/00003246-199111000-00020. [DOI] [PubMed] [Google Scholar]
- 10.Grauman S., Johansson J., Drevhammar T. Large variations of oxygen delivery in self-inflating resuscitation bags used for preoxygenation - a mechanical simulation. Scand J Trauma Resusc Emerg Med. 2021;29:98. doi: 10.1186/s13049-021-00885-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yip Y.Y., Lee C.P.T., Cheung J.C.H. Raising the awareness for insufficient oxygen delivery from self-inflating resuscitation bags lacking expiratory valve during preoxygenation. Hong Kong J Emerg Med. 2022;30:61–63. [Google Scholar]
- 12.Stafford R.A., Benger J.R., Nolan J. Self-inflating bag or Mapleson C breathing system for emergency pre-oxygenation? Emerg Med J. 2008;25:153–155. doi: 10.1136/emj.2007.050708. [DOI] [PubMed] [Google Scholar]